Abstract
Background and Objective:
Depression among medical students is an area of increasing concern worldwide. This study aimed to assess the prevalence of depression and its associated factors among medical students.
Materials and Methods:
A stratified random sample of 400 students was assessed using Beck Depression Inventory by investigators. Associations between depression and class of studying, social factors like alcohol use, drug addiction, family problems, family history of depression, and staying away from home were analyzed by univariate analysis.
Results:
The overall prevalence of depression was found to be 71.25%. Among those with depression, a majority (80%) had mild and moderate degree of depression. The study showed that 46.3% (132) of the depressed were females and 53.7% (153) were males. According to cut-off scores, 115 students (29.8%) scored as normal (0-9), 111 (27.8%) as mild (10-18), 117 (29.3%) as moderate (19-29), 30 (7.5%) as severe (30-40), and 27 (6.7%) as very severe (>40) depression. The prevalence of depression was comparatively less among 1st and 2nd year medical students (57% and 50%, respectively) and the difference between the grade of depression and year of studying was found to be significant (χ2=122, P<0.001). The prevalence was significantly more among those with family problems and family history of depression.
Conclusion:
Depression is highly prevalent among medical students in this area. Our findings point to the importance of broad screening and psychiatric counseling of this vulnerable population.
Keywords: Beck Depression Inventory, depression, medical students
INTRODUCTION
Depression among medical students represents a neglected public health problem in India. It is very important to prevent the ill effects of depression on one's educational attainment and career through early detection and proper interventional measures. Few studies have been conducted at a global level to assess the prevalence of depression among medical students. All these studies have been conducted in western countries as well as in other parts of the world.[1–5] In India, epidemiological studies on depression among medical students are scanty. Clearly, depression in medical students is of paramount importance and warrants serious study.
Early onset depression among medical students interferes with psychological, social, and academic functioning, placing him or her at greater risk for problems such as substance abuse and suicidal behavior.[5] The high rate of depression among medical students is associated with numerous factors. A variety of factors which include their educational life, social factors like alcohol use, drug addiction, family problems, family history of depression, and staying away from home were associated with depression among medical students. Studies of such nature will be a useful tool to take appropriate steps like counseling for the depressed medical students. Hence, this study was undertaken to find out the prevalence and associated factors of depression among medical students.
MATERIALS AND METHODS
A cross-sectional study was conducted during January 2008 on a representative sample of medical students at an institution in Mangalore, Karnataka. The aim was to screen for depression using Beck Depression Inventory scale (BDI) and determine associated factors of depression based on a cut-off value of 10 and above.
The sample size was estimated as 400, taking prevalence as 20% and precision of 20%. In order to increase the representation of each study year in the sample, we first stratified the sample on medical students and the study years and then randomly selected the students according to proportional to the size of each stratum to get a total of 400 students. Thus, 100 medical students were selected randomly from each class from 1st to 4th year. After obtaining permission from the Head of the institution, students were approached to collect data. A departmental review board approved the study. The objectives of the study were explained to subjects before initiating the study. They were assured confidentiality and given option to refuse to participate in the study without any further questions or implications. After this, informed verbal consent was obtained from all selected participants in the study and they were asked to sign a list to confirm participation. Subjects who refused to participate in the study or if a student who was absent on the day of study and/or could not be contacted even after two visits were considered as non-respondents.
Study tool
The Beck Depression Inventory Scale (BDI) has been used for screening of depression among study population which has been tested and validated.[6,7] This is a subjective scale and used for screening purpose, which has to be further evaluated to confirm the diagnosis. We used this scale to screen for depression based on self-report.
The questionnaire is self-administered and the results are relative and dependent on how the subject answers each question. It is a 21-item measure and has been one of the most widely used screening instruments for detecting symptoms of depression. It can be administered to assess normal adults, adolescents, and individuals with psychiatric disorders (13 years of age or older).[8] It was designed to document a variety of depressive symptoms the individual experienced over the preceding week. Responses to the 21 items are made on a 4-point scale, ranging from 0 to 3 (total scores can range from 0 to 63).
A self-administrated questionnaire was utilized including information regarding class, social factors like alcohol use, drug addiction, family problems, family history of depression, and staying away from home. Any subject with an alcohol intake at least once in the past 12 months was considered as alcohol user for the purpose of this study. The family problem was assessed by the question that whether the family members were currently having any problem that worries the subject or not. Drug addiction was defined as repeated use of any psychoactive substance including alcohol, to the extent that the user is periodically or chronically intoxicated, shows a compulsion to take the preferred substance, and has a great difficulty in voluntarily ceasing or modifying substance use. Family history of depression was assessed based on earlier diagnosis among first or second degree relatives.
Data was entered and analyzed by using SPSS 11.0 for windows. Univariate analysis was performed and the chi- square test was used to test for the association between depression and variables. Data was expressed in terms of proportion or percentages.
RESULTS
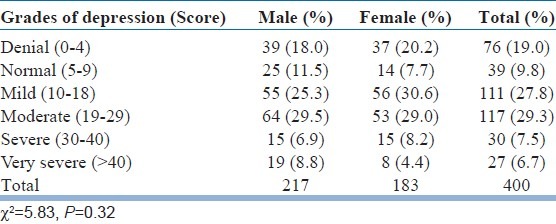
Of the 400 medical students participated in the study, 217 (54.3%) were males and 183 (45.7%) were females. The overall prevalence of depression was found to be 71.25%. Among those with depression, a majority (80%) had mild and moderate degree of depression. The prevalence of severe and profound depression was 7.5% and 6.7%, respectively. The present study showed that 46.3% (132) of the depressed were females and 53.7% (153) were males; and the association between the grade of depression and sex was not statistically significant (χ2=5.83, P=0.32). According to the cut off scores, 115 students (29.8%) scored as normal (0-9), 111 (27.8%) as mild (10-18), 117 (29.3%) as moderate (19-29), 30 (7.5%) as severe (30-40), and 27 (6.7%) as very severe (>40) depression [Table 1].
Table 1.
Grades of depression according to sex
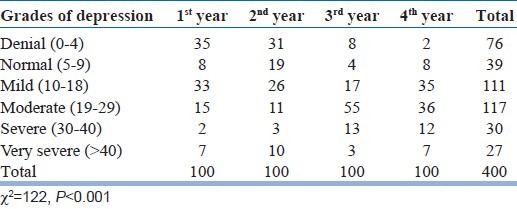
The prevalence of depression was less among 1st and 2nd year medical students (57% and 50% respectively). During the 1st and 2nd year, totally 26% of the medical students were classified to have moderate grade of depression. Among the students of the 3rd and 4th year, the prevalence of moderate depression was found to be 55% and 36%. Similarly, degree of severe and very severe depression increased from 9% during 1st year to 19% during the 4th year of the study. The difference found between the grade of depression and year of studying was statistically significant (χ2=122, P<0.001) [Table 2].
Table 2.
Grades of depression according to classes
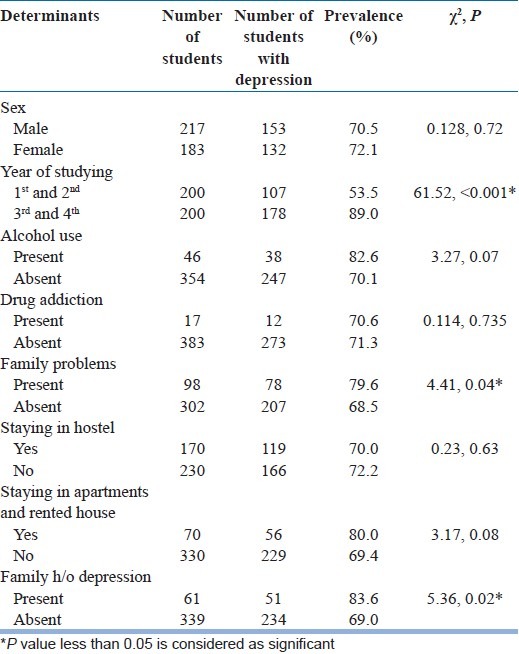
In univariate analysis, it was observed that the prevalence was high among those medical students with family problems and it was found to be significant (χ2=4.41, P=0.04). Similarly, those with family history of depression had higher prevalence compared to those students without family history of depression (χ2=5.36, P=0.02). There was no significant difference in the prevalence of depression among those with other associated factors for depression [Table 3].
Table 3.
Prevalence of depression according to associated factors
DISCUSSION
Consistent with the economic changes in the country, medical student population is increasing every year. In this competitive era, this has enhanced the risk of developing various mental disorders like depression. Well-documented studies to determine the prevalence of depression and its associated factors among medical students are few at global level.[1–5] To the best of our knowledge, there are no studies using Beck Depression Inventory to assess depression among medical students in India, but there are some studies among adolescents.[9] There is a wide difference in prevalence rates in these studies. Since the Beck Depression Inventory is a subjective scale, it has not been used by previous studies. Other reasons include methods used for assessment, grading, and cut off used to assess depression and difference in the sample size selected for the study.
In the current study, the BDI has been utilized to detect the prevalence of depression among medical students. Although it is not designed for diagnostic purposes, its epidemiologic utility has been evaluated in several studies, which concluded that it is a reliable and valid instrument for detecting depressive disorders in non-clinical populations. Several studies support the BDI's usefulness in measuring and predicting depression in adolescent samples.[8,10]
Prevalence rates of depression are estimated to range from 15% to 66% in various studies.[1–5,11–14] Chan among Chinese medical students in Hong Kong found that around half of the medical students are depressed.[3] In contrast, a study done in Pakistan found that the prevalence rate varied from 49% to 66% among medical students.[11] Another study has shown that 39.4% of the medical students are depressed by using the instrument Depression Anxiety Stress Scale.[12] A study among adolescents in India showed the prevalence among college going girls as 29%.[9] Another study done in Iran among high school and Pre-University students found out that 34% of them were depressed according to cut- off score of BDI 16.[15] The present study has shown that the prevalence of depression is higher among medical students compared to the above studies. This is mainly because of inclusion of mild degree of depression by lower cut off for BDI score in our study. More than 3/4 of the depressed students belonged to mild to moderate degree of depression in our study. Other possibilities could include differences in the demographic structure of our students and even the increase in competition in medical field.
As the class of studying increases, the prevalence increased significantly. Our study is consistent with the findings of other studies.[1,2] In contrast to this, another study showed that prevalence is significantly higher among 1st and 2nd year medical students,[11] while it was not found to be significant in another study.[15] Although there is marginally higher prevalence among females compared to males, it was not found to be significant in comparison[1] and contrast to other studies.[14,15] It has been demonstrated that mood disorders occur more commonly among the relatives of depressed persons than in the general population.[4] It is seen that alcohol use, drug addiction, and staying away from home did not affect the prevalence of depression in our study.
In this study, variables that might be related to depression, such as physical activity, duration of sleep, personal efficacy, existence of social support, conflict between career life and private life, work place phobia, were not analyzed. Also, personality characteristics that may be predictive of depression were not analyzed. Positive subjects were counseled and a psychologist and counselor took group sessions for the participants after the study. The students were also offered to consult a psychiatrist and seek help and confidentiality was assured. They were also offered services of a counselor beyond the study at their convenient time. The helpline number was informed to all the participants. The subjects with severe depression were referred to department of psychiatry for further analysis and counseling. Socio-demographic factors like education, occupation, and income of the family were not assessed due to feasibility constraints. This study gives an idea of magnitude of depression among medical students and some of its associated factors, which can be evaluated by further studies in depth by qualitative and quantitative methods. Since it is a cross-sectional study, it is hard to assess direction of influence and it precludes us from making causal inferences from our study findings. However, the sufficient sample size and using a valid scale to classify depressive symptoms of the students increases the validity of the study. Depression is highly prevalent among medical students. The fact that 7.5% and 6.7% respect of the medical students had depression of severe and very severe grade suggests the need of group counseling facilities within the medical college. Our findings point to the importance of screening of this vulnerable population and taking appropriate interventional measures to prevent the complications of depression.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared
REFERENCES
- 1.Clark DC, Zedlow PB. Vicissitude of depressed mood during four years of medical school. J Am Med Assoc. 1988;260:2521–8. [PubMed] [Google Scholar]
- 2.Levine RE, Litwins SD, Frye AW. An Evaluation of Depressed Mood in Two Classes of Medical Students. Acad Psychiatry. 2006;30:235–7. doi: 10.1176/appi.ap.30.3.235. [DOI] [PubMed] [Google Scholar]
- 3.Chan DW. Depressive symptoms and depressed mood among Chinese medical students in Hong Kong. Compr Psychiatry. 1991;32:170–80. doi: 10.1016/0010-440x(91)90010-a. [DOI] [PubMed] [Google Scholar]
- 4.Zoccolillo M, Murphy GE, Wetzel RD. Depression among medical students. J Affect Disord. 1986;11:91–6. doi: 10.1016/0165-0327(86)90065-0. [DOI] [PubMed] [Google Scholar]
- 5.Birmaher B, Ryan ND, Williamson DE, Brent DA. Childhood and adolescent depression: A review of the past 10 years, Part I. J Am Acad Child Adolesc Psychiatry. 1996;35:1427–39. doi: 10.1097/00004583-199611000-00011. [DOI] [PubMed] [Google Scholar]
- 6.Basker M, Moses PD, Russell S, Russell PS. The psychometric properties of Beck Depression Inventory for adolescent depression in a primary-care paediatric setting in India. Child Adolesc Psychiatry Ment Health. 2007;1:8. doi: 10.1186/1753-2000-1-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Beck A, Ward CH, Mendelson M, Mock J, Erbaugh J. An inventory for measuring depression. Arch Gen Psychiatry. 1961;4:561–71. doi: 10.1001/archpsyc.1961.01710120031004. [DOI] [PubMed] [Google Scholar]
- 8.Barrera M, Jr, Garrison-Jones CV. Properties of the Beck Depression Inventory as a screening instrument for adolescent depression. J Abnorm Child Psychol. 1988;16:263–73. doi: 10.1007/BF00913799. [DOI] [PubMed] [Google Scholar]
- 9.Nair MK, Paul MK, John R. Prevalence of depression among adolescents. Indian J Pediatr. 2004;71:523–4. doi: 10.1007/BF02724294. [DOI] [PubMed] [Google Scholar]
- 10.Teri L. The use of the Beck Depression Inventory with adolescents. J Abnorm Child Psychol. 1982;10:277–84. doi: 10.1007/BF00915946. [DOI] [PubMed] [Google Scholar]
- 11.Inam SNB, Saqib A, Alam E. Prevalence of anxiety and depression among medical students of private university. J Pak Med Assoc. 2003;53:44–7. [PubMed] [Google Scholar]
- 12.Vaidya PM, Mulgaonker KP. Prevalence of depression, anxiety and stress in undergraduate medical students and its correlation with their academic performance. Indian J Occup Ther. 2007;39:1–10. [Google Scholar]
- 13.Aniebue PN, Onyema GO. Prevalence of depressive symptoms among Nigerian medical undergraduates. Trop Doct. 2008;38:157–8. doi: 10.1258/td.2007.070202. [DOI] [PubMed] [Google Scholar]
- 14.Marie D, Joneborg N, Runeson B. Stress and depression among medical students: A cross sectional study. Med Educ. 2005;39:594–604. doi: 10.1111/j.1365-2929.2005.02176.x. [DOI] [PubMed] [Google Scholar]
- 15.Modabber-Nia MJ, Shodjai-Tehrani H, Moosavi SR, Jahanbakhsh-Asli N, Fallahi M. The prevalence of depression among high school and pre university adolescents: Rasht, Northern Iran. Arch Iran Med. 2007;10:141–6. [PubMed] [Google Scholar]


