The development of the technique of in vitro fertilization (IVF) helped to make it possible for a couple to reproduce, to have a child, without normal sexual intercourse. Indeed this is the main point of the procedure: for there are many couples, about one in seven, who encounter difficulties in having children through normal sexual intercourse. For them, IVF provides an alternative way of creating an embryo from their gametes, with the hope that after the replacement of the embryo in the woman's uterus, a normal pregnancy follows, leading to the birth of a child. Success cannot of course be guaranteed, but the latest UK data indicate that after an IVF cycle a pregnancy is established in about 33% of cases, leading to a live birth-rate of about 25% (www.hfea.gov.uk/ivf-figures-2006.html). After the birth of Louise Brown in 1978, this technique has been used on a large scale: there are more than five million people worldwide whose conception was achieved by IVF [1]—this includes intracytoplasmic sperm injection (ICSI), which is a variant of IVF commonly used to address problems of male infertility associated with low motility of sperm.
…there are more than five million people worldwide whose conception was achieved by IVF…
In turning to consider the social and ethical significance of IVF, it is important to start from the broader context of techniques for addressing problems of infertility. IVF is not the only way of achieving reproductive success without normal sexual intercourse. What is important about human reproduction is that live sperm should encounter an oocyte in such a way that an embryo is formed and implants in a woman's uterus. Where normal sexual intercourse does not achieve this result, it is possible to place sperm, which has been collected shortly beforehand, in the vagina at the time when an egg has been released, in the hope that conception will take place. This method is widely used in animal husbandry and, since the eighteenth century at least, it has been used to facilitate human reproduction either where ordinary vaginal intercourse cannot be undertaken—for instance, after spinal injury to the man—or where the woman's cervix impedes the passage of sperm from the vagina. The technique is known as intra-uterine insemination (IUI), and it is commonly used as a first stage in assisted reproduction treatment (ART) because it is cheap and relatively non-invasive. It is also widely used for donor insemination in which sperm from a male donor is used because a woman's partner is infertile. The problem with these techniques, however, is that the success rate is relatively low: for example, in 2009 only 11% of donor insemination cycles in the UK led to a live birth as compared with 25% for IVF (www.hfea.gov.uk/1270.html). So although they remain in use because they are cheap and easy, it is IVF that has transformed the situation for couples with serious fertility problems.
Another way in which problems of infertility have been addressed is by ‘social’ solutions—these provide a couple with a child or children of whom they are not the genetic parents by adoption. Adoption is of course an old practice, often used in the ancient world to provide a male heir where a couple had no natural son. Since the nineteenth century, however, adoption has generally been used to help provide new parents for children who are orphans or have been abandoned, and this is the main source of adoptive children for couples with fertility problems. But for such couples adoption is generally not the first choice: for obvious reasons most couples have a strong preference for having some genetic link with their children.
Reproduction without sex by means of IVF, was of course preceded by sex without reproduction. Simple contraceptive devices such as the sheath (condom) are old; but it was the introduction of the contraceptive pill in 1960 that enabled women, for the first time, to take charge of their own reproductive potential. This development radically altered the position of women in society: without abstaining from sexual activity, young women were in a position to complete their education and pursue a career in ways that young men had taken for granted. This move to substantive equality between men and women was the most important social revolution of the late twentieth century, and it continues to challenge and transform relationships between men and women. But one important implication concerns reproduction: if women can start their careers without fear of pregnancy and all its complications, while still sharing their lives with men, will they also be able to have children when they have established their career and personal situation? Here the development of IVF offers some help. The difficulty for a woman in achieving pregnancy after the age of 35 is partly due to increasing irregularities in ovulation; but as long as a woman still has viable eggs in her ovaries some can be collected after stimulation by drugs, and used to create embryos by IVF. Admittedly, IVF success rates diminish once a woman is over 35 years of age and even more for those who are over 40; but there is also the possibility of using IVF with donor eggs. In this way, reproduction without sex (IVF) has helped to mitigate one consequence of sex without reproduction (contraception).
Science & Society Series on Sex and Science.
Sex is the greatest invention of all time: not only has sexual reproduction facilitated the evolution of higher life forms, it has had a profound influence on human history, culture and society. This series explores our attempts to understand the influence of sex in the natural world, and the biological, medical and cultural aspects of sexual reproduction, gender and sexual pleasure.
Putting the point this way suggests that IVF has achieved a biological and emotional separation between sex and reproduction, which was initiated by the contraceptive pill. But it is important to understand this ‘separation’ correctly. What is true is that in each direction there is the possibility of one (sex/reproduction) without the other (reproduction/sex). But it does not follow that there is not normally an intimate connection between the two, in that far and away most pregnancies are achieved by normal sexual intercourse—a situation which, for obvious reasons, is likely to remain. So what is important about IVF is not that it brings about a complete separation of reproduction from sex but that it opens up new possibilities for reproduction without sex, some of which give rise to important ethical questions.
Before discussing these new possibilities, however, we need to consider the basic morality of IVF itself. The benefit that IVF has brought is that many couples who could not otherwise have had children are now able to do so; and anyone familiar with the sadness and disappointment that accompanies the failure to have children should acknowledge that this has been a great advance in social welfare. Nonetheless there are those, most notably the moral theologians of the Catholic Church, who hold that there is something inherently wrong about IVF, so wrong that its potential benefits—which are not disputed by the critics—do not make it morally permissible. Section 2377 of the Catholic Catechism puts the position in the following way: “Techniques involving only the married couple (homologous artificial insemination and fertilization) are perhaps less reprehensible, yet remain morally unacceptable. They dissociate the sexual act from the procreative act. The act which brings the child into existence is no longer an act by which two people give themselves to one another, but one that entrusts the life and identity of the embryo into the power of doctors and biologists and establishes the domination of technology over the origin and destiny of the human person. Such a relationship of domination is in itself contrary to the dignity and equality that must be common to parents and children. Under the moral aspect procreation is deprived of its proper perfection when it is not willed as the fruit of the conjugal act, that is to say, of the specific act of the spouses’ union. Only respect for the link between the meanings of the conjugal act and respect for the unity of the human being make possible procreation in conformity with the dignity of the person” [2].
In this way, reproduction without sex (IVF) has helped to mitigate one consequence of sex without reproduction (contraception)
The central claim here seems to be that the ‘power’ of the clinicians and embryologists inherent in the practice of IVF brings about a ‘domination of technology,’ which is incompatible with ‘the dignity of the person’. Yet almost any medical intervention involves a patient entrusting himself or herself to a clinician, and even where a great deal of technology is involved, there is no reason to think that the intervention necessarily brings with it a ‘domination of technology’ that compromises the dignity of the patient. On further examination, therefore, the main reason for the claim that IVF is morally unacceptable seems to be that because the success of IVF depends on the skill and technology of clinicians and embryologists, procreation is not the direct outcome of an act of conjugal love; instead procreation, where it occurs, is a technical achievement by the clinicians and embryologists. So whereas normal sexual procreation by a married couple is an expression of conjugal love, IVF is an exercise of technical power. But once this line of thought is laid bare, it is readily seen to be unwarranted. Those who have recourse to IVF to have a child need to have a great deal of love for each other, to support each other through the trials and discomforts it entails, a love of a different type from that expressed in the ‘conjugal act’ but a strong and enduring love nonetheless. The fact that the help of clinicians and their technology is required for procreation by IVF is, for those who need it, a misfortune to which the proper response is sympathy and reassurance, not the critical judgment that their course of action is morally unacceptable.
So far I have argued that the Catholic objection in principle to IVF fails to do justice to the situation of couples who use IVF to have children. But there is a more substantive objection to the usual practice of IVF, which is frequently urged by Catholic and other ‘conservative’ moralists. The objection arises from the fact that the collection of unfertilized eggs from a woman before IVF is a difficult and intrusive process, requiring the administration of powerful and potentially dangerous drugs to stimulate the ovaries. It is therefore standard practice to collect more eggs than are required for one cycle of IVF, and to use the extra eggs to create more embryos so that they can be frozen for use in further cycles of IVF treatment. As there is no way of knowing at the time these embryos are created, how many will be needed by the couple, it often turns out that there are some ‘spare’ embryos left over. The normal practice is that the couple decide what to do with these embryos, and most couples choose to dispose of them. It is, however, this practice of disposing of spare embryos that conservative moralists take to be reprehensible. For, they argue, each of these embryos is a completely innocent human person, someone who happens to be at an early stage in his or her life but who in fundamental respects is comparable to a newborn infant, and thus a being that merits the kind of respect and care that is appropriate to an infant, and whose status is radically violated when it is simply ‘disposed of’.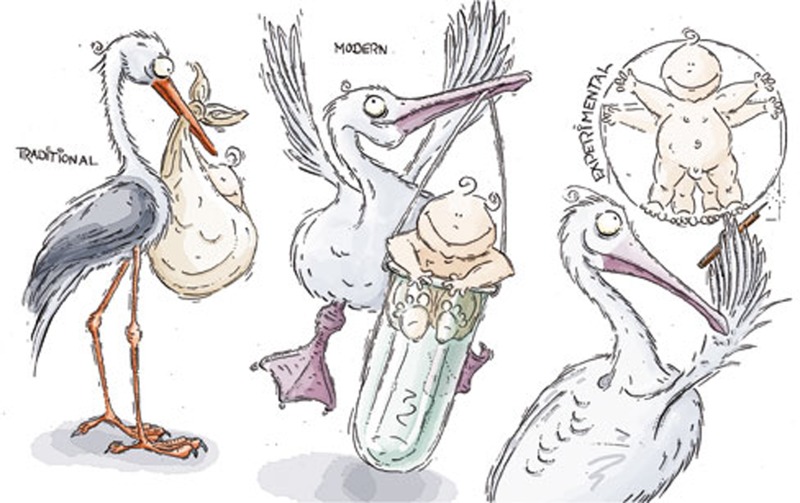
Unlike the previous point, this is not an objection to IVF as such. It is perfectly possible to perform IVF without creating spare embryos, and there are some clinics where this is routine practice. The reason for the normal practice is, as explained above, that there are good reasons for minimizing the episodes of egg collection undergone by a woman embarking on IVF treatment. One might still wonder whether one could not just freeze the extra eggs collected, rather than fertilize them before freezing them as extra embryos; for disposing of spare eggs is not as morally contentious as disposing of spare embryos. Unfortunately this option is not, at present at least, practicable because embryos survive the freezing and thawing process reasonably well, but eggs do not—although some work suggests that there are ways of achieving improved results in this regard [3]. So the issue of the status of the embryo and what it implies for our treatment of an embryo cannot be side-stepped in this way. The central issue here is whether something that has the potential to become, after implantation and successful pregnancy, a human infant and then a normal human adult has the same fundamental moral status as an infant. The main alternative view is that moral status depends on the actual capacities of the being, which starts life as an embryo, and then, if it implants, becomes a foetus and, after birth, an infant. In this latter view, the early embryo does not, at this stage of its development, have the moral status that it later acquires as it develops capacities such as sentience, consciousness and agency.
IVF is routine and relatively commonplace, PGD is neither: although it is well established, it is expensive and time-consuming
It is not possible to pursue here all the intricacies of this debate to a reasoned conclusion. The first view has the considerable merit of simplicity, but the implication that an early embryo makes the same moral claim on us as a newborn infant is hard to accept; and the thesis that potentiality alone confers moral status does not sit well alongside the discovery of the reproductive potential inherent in almost any somatic cell. The alternative view is more complex, but coheres with our ordinary attitude to the significance of the development of a human being's capacities and abilities, which leads us, for example, not to attribute criminal responsibility to children. A compromise position, which I myself favour, recognizes that the genetic identity of an early human embryo gives the embryo a modest moral status as the blueprint for a new human life, although not the status of a person comparable with that of an infant. With this third view, it is morally legitimate to dispose of spare embryos: indeed it would be contrary to their status to require that they be somehow nurtured into human beings without parents who wanted them. But their disposal is nonetheless regrettable. Other things being equal, it would be better if the practice of IVF could be refined in such a way as to reduce the number of spare embryos created, without imposing extra risks and distress on women who already have much to endure.
I turn to consider the ethical issues, which arise from the new possibilities that are dependent on IVF. The most important of these is preimplantation genetic diagnosis (PGD or PID). This technique requires creation of embryos by IVF, and then the removal of a blastomere from each apparently ‘good’ embryo at an early stage. The isolated cell is then tested for the presence or absence of some previously identified genetic condition. This technique requires a high degree of skill and sophisticated equipment. IVF is routine and relatively commonplace, PGD is neither: although it is well established, it is expensive and time-consuming.
PGD is a method of selecting which embryos to place in a woman, and thus equally a method of rejecting embryos because they are thought to be unsuitable. It is, therefore, a way of determining which embryos are to have a chance of becoming children if they implant successfully and which embryos are not to have this chance. As such it gives rise to significant social and ethical considerations concerning the role of human intervention in determining which kinds of children are to be born or not born.
We encounter positive eugenics proper where embryos are selected on the basis of genetic predispositions that are wanted for their own sake
In the early years PGD was mainly used to enable parents to avoid having children with serious early-onset inherited disorders such as Tay–Sachs disease. Only those who hold that all human embryos have the moral status of a person will find it unacceptable that parents can take steps not to implant an embryo with the genetic basis for Tay–Sachs disease; others will judge that it is morally unacceptable that parents should be denied the opportunity to avoid having a child with Tay–Sachs disease. So with respect to these cases, the positions taken largely follow those already explored. PGD has recently been extended to conditions such as bowel cancer and breast cancer. This extension is not problematic. Human welfare generally, as well as that of future children, is enhanced by relieving families of the anxiety that they might pass on a predisposition to these aggressive hereditary cancers. But as we look forward to further developments of this kind, we need to ask what are the limits to the use of PGD?
One limit is set by genetics: once we are dealing with disorders the basis of which lies not in a single gene but in some complex multiple-gene interaction, the chances of finding an embryo with all the desired genes are much diminished. But further limits can be set by us. One issue arises from the fact that some genes giving rise to serious disorders are recessive. Where this is the case, those who ‘carry’ a copy of the affected gene do not themselves suffer from the disorder in question, but are liable to have children who do. The question that arises is whether it is acceptable to use PGD to exclude not only embryos that are liable to a serious disorder, but also those embryos that are carriers for the condition. Some argue that the disposal of embryos just because they are carriers places too low a value on the potential human life embodied in an embryo. However, once one appreciates that it is generally couples who are already using PGD to avoid having a child with a serious disorder who also wish to avoid having children who are carriers of the disorder, it is difficult to see any good reason for not permitting them to rank the embryos that are to be implanted, with those which are not carriers at all as their preferred embryos.
So far I have discussed cases in which PGD is used to enable parents to avoid having a child with a serious genetic disorder. This use is primarily negative. What about positive uses, in which PGD is used to select a child of a specific kind? One kind of case is the ‘saviour sibling’ type, where an embryo is selected as a human leukocyte antigen (HLA) match for a sibling with a serious disorder that is best treated by a haematopoietic stem cell transfusion. This treatment requires an HLA-compatible source for the stem cells, which are provided in the cord-blood available through the birth of the ‘saviour sibling’. As the selection of the implanted embryo is guided by the medical needs of the affected child it gives rise to the objection that the resulting child's existence is being valued primarily as a means to improve the welfare of its sibling, and not for its own sake. The reply to this is that, once one appreciates the situation of a family with an affected child, there is every reason to expect the ‘saviour sibling’ to be loved and valued for its own sake, especially where its birth makes possible a treatment for its sibling. So although this use of PGD requires oversight, it is in principle acceptable.
We encounter positive eugenics proper where embryos are selected on the basis of genetic predispositions that are wanted for their own sake. Manifestly, this is a large topic, and I shall not try to address it fully here. It is in fact doubtful whether PGD is likely to be of much use for this purpose: the evidence suggests that insofar as significant abilities such as IQ have a genetic basis at all, they involve complex multiple gene–environment interactions. Still, one cannot rule out a priori some significant possibilities for the identification and selection of ‘better’ embryos, which turn out to be amenable to selection by PGD. Most of us, I am sure, can think of valuable abilities that others seem to have been granted in the genetic lottery but that we ourselves lack. It strikes me that my life, for example, would have been better had I been more musical than I am. So the question arises whether, if it were possible to select for this ability by PGD without losing other valuable abilities as a result, it would be acceptable to undertake this practice?
In thinking about this, it is important not to imagine that the use of PGD here would have enabled one's parents, so to speak, to add musical ability to the genetic predispositions of the child they were going to have anyway (oneself). Instead they would be choosing which embryo to implant on the basis of the potential musical ability of the resulting child, and thereby choosing not to have different children with all sorts of other unknown abilities. Hence the use of PGD for positive selection of this kind is surrounded by uncertainty concerning the alternatives not selected, and as a result there could be no certainty that the embryo chosen was potentially ‘the best’—if that judgement makes any sense at all. For that reason most people prefer to leave the determination of their children's genome to chance, to the genetic lottery, apart from using PGD to avoid serious disorders.
There is nothing intrinsically wrong, let alone ‘gravely immoral’, with donor conception
But this preference does not settle whether all uses of PGD for positive selection would be wrong. One area of anxiety concerns the potentially divisive social implications of a situation in which wealthy people attempt to use positive eugenic selection to create a ‘master race’. My own view is that this anxiety is not well founded, as there is no realistic prospect of genetic selection for significant abilities such as IQ. But there remains a fundamental ethical question here, namely whether it is harmful for a child that the embryo, which became that child, was selected because it had a certain genetic predisposition. Where the disposition selected is one that affects important aspects of the child's life, in a way that the child cannot later just choose to neglect, it is argued that the child's capacity to take control of his or her character is harmed by the way in which an important element of this character has been deliberately selected by the child's parents.
A hypothetical case where this consideration applies, I think, would be one in which PGD was used to select for sexuality. Deliberate determination of sexuality is quite the wrong kind of parental interference in the life of a child. A more contested case is that of sexual selection itself. Here the reasons in favour of the practice, typically involving family balancing, are easily understandable; the question is whether a child's capacity to construct a life of their own is threatened by coming to know that their sex was determined by a parental decision rather than by the genetic lottery. The issues here are subtle and speculative, and the ethical debate on them remains open.
A different group of ethical issues concerns the use of IVF in the context of donor conception. Although donor conception with sperm does not depend on IVF, the greater success of IVF as compared with donor insemination has meant that donor conception often makes use of IVF; and of course, conception with donor eggs is only possible thanks to IVF. So any study of the ethical implications of IVF needs to include reference to the ethical issues in donor conception. Here, as with IVF, we start by briefly considering the forthright condemnation of this practice in section 2376 of the Catholic Catechism: “Techniques that entail the dissociation of husband and wife, by the intrusion of a person other than the couple (donation of sperm or ovum, surrogate uterus), are gravely immoral. These techniques (heterologous artificial insemination and fertilization) infringe the child's right to be born of a father and mother known to him and bound to each other by marriage. They betray the spouses’ right to become a father and a mother only through each other” [2].
This passage starts off with a contrast between the normal conception of a child by husband and wife, and the ‘intrusion’ of another person, which entails the ‘dissociation of husband and wife’. One might think that the author of this passage was thinking here of adultery; but the second sentence makes it clear that the use of donor conception is being described. As such the description is plainly inappropriate: donors do not ‘intrude’ into the conception of a child. Instead they generously offer gametes to enable a couple, who cannot have a child in any other way, to conceive a child that they go on to bring up as their own. It is strange, and sad, that when couples with problems of fertility merit support and sympathy as they work through their problems and come to terms with their need to rely on donor gametes to have children of their own, they face this undeserved and misconceived condemnation. There is nothing intrinsically wrong, let alone ‘gravely immoral’, with donor conception.
Despite the arguments of its critics, there are no principled moral objections to IVF that withstand critical scrutiny
Nonetheless, donor conception does give rise to some difficult ethical issues that continue to provoke discussion and debate, especially concerning donor anonymity and the proper level of compensation to donors for the time and trouble involved in gamete donation. On the issue of donor anonymity my own view starts from the belief that, as has been shown to be the case with young adoptees, it is greatly in the interest of donor-conceived children to be able to make contact, as young adults, with their donor so that they can discover where they have come from and thereby achieve a broader understanding of their personal identity. It is obvious that once this possibility of contact with the donor is recognized as a right, there cannot be anonymity for gamete donors. This might have implications concerning the people who are then willing to come forward as gamete donors; but with care an adequate supply of gamete donors who are content to donate without the promise of anonymity can be maintained.
One important consideration for such donors is the level of compensation for their donation. In the UK, as in Europe generally, the basic principle behind gamete donation is that it should be altruistic, since altruism provides an ethical bond between the donor and the recipient of the donation, which is appropriate to the fact that the donor's gamete is a fundamental and persisting ingredient because of its genetic constitution in the recipient's new child. Nonetheless, it is also important that those who put themselves forward to become donors should be properly compensated for the trouble and inconvenience of doing so, which is considerable in the case of women who donate eggs. What is wanted, therefore, is a level of compensation that does not leave donors feeling that their good will is being exploited, without setting it at such a high level that financial motives suffice by themselves to attract donors who lack any altruistic motivation. Within these ethical constraints, pragmatic considerations can, I think, be used to settle reasonable levels of compensation.
IVF is here to stay. It will not replace normal sexual reproduction, as most couples have no problem conceiving children through sexual reproduction; but IVF has brought great benefits to couples who cannot conceive children that way. Despite the arguments of its critics, there are no principled moral objections to IVF that withstand critical scrutiny. Some of the possibilities with which it is associated do give rise to significant ethical issues; but with adequate oversight and regulation there is no slippery slope that will drag a society that allows the use of IVF down to some dystopian future. It is time to move beyond moral criticism of IVF.

Thomas Baldwin
Footnotes
The author declares that he has no conflict of interest.
References
- ESHRE (2012) The World's Number of IVF and ICSI Babies Has Now Reached a Calculated Total of 5 Million. Press Release. Grimbergen, Belgium: European Society of Human Reproduction and Embryology. www.eshre.eu/ESHRE/English/Press-Room/Press-Releases/Press-releases-2012/5-million-babies/page.aspx/1606 [Google Scholar]
- United States Conference of Catholic Bishops (1997) Catechism of the Catholic Church. Washington DC, USA: United States Conference of Catholic Bishops [Google Scholar]
- Boldt J (2011) Current results with slow freezing and vitrification of the human oocyte. Reprod Biomed Online 23: 314–322 [DOI] [PubMed] [Google Scholar]


