Abstract
Background
To assess initial efficacy and feasibility of a structured behavioural group training (DELFIN) for parents of children with diabetes type 1, in order to reduce parenting stress and to improve parenting skills.
Methods
A randomized controlled study was conducted between July 2008 and September 2010, at a children’s hospital in Hannover with parents of children with type 1 diabetes (2–10 yrs) (intervention group n = 37; control group n = 28). Parenting skills, parents’ psychological burden, children’s behavioural difficulties and quality of metabolic control were assessed before, 3 months after and 12 months after participating in the training program.
Results
In the intervention group parenting behaviour in conflict situations improved significantly after 3 months (Z = −3.28; p ≤ 0.001). It remained stable over 12 months (Z = −2.94; p ≤ 0.01). Depression and anxiety scores of parents decreased (Z = −1.93; p ≤ .05; Z = −2.02; p ≤ .05). Even though the outcome in the intervention group was more positive, the differences between both study arms failed to reach statistical significance. Unexpectedly parenting behaviour in the control group improved also (Z = −2.45; p ≤ .05). Anxiety as well as stress scores decreased in this group (Z = −2.02; p ≤ .05 and Z = −2.11; p ≤ .05). In both groups the initial metabolic control was good and without significant differences (A1c 7.2±0.8% vs. 7.1±0.4%; p > 0.5). It remained stable in the DELFIN group (A1c 7.1±0.8%; p > 0.5), but it increased slightly in controls (A1c 7.3±0.5%; Z = −2.79; p = .005).
Conclusions
This study has brought first evidence for the efficacy and feasibility of the program. A multicentre study with a larger sample is necessary to confirm these first results.
Keywords: Children, Parenting program, Type 1 diabetes, Randomized clinical trial, Behaviour modification
Background
The therapy of children with type 1 diabetes has experienced tremendous improvements in the recent past [1-5]. In the context of a modern evidence based insulin regimen, training courses for children and parents intend to prepare families for the diabetes self-management in every day life [2,6,7]. During the last two decades structured diabetes education programs have been scientifically evaluated and accredited nationwide in Germany [2]. There are two multisite evaluated training programs for German-speaking countries for children or adolescents above the age of six [8,9]. Furthermore, there is another multisite evaluated structured education program for parents of children with diabetes [10,11]. The main aim of these programs is to impart relevant treatment knowledge and age appropriate self-management skills. The effectiveness of these programs in imparting diabetes management skills and diabetes knowledge has been proved [11-14].
In spite of the progress of the insulin therapy, its metabolic outcome is limited by family conflicts, family dysfunction and parenting problems, e. g. diffusion of responsibilities [3,15-18]. Particularly parents of younger children perceive themselves to be excessively burdened [11,19,20]. After one year of diabetes duration a positive association between parenting stress and parental depressive symptoms was described by Patton and colleagues [21].
The specific parenting issues of parents with toddlers, pre- and elementary school children (temper tantrums, implementing prohibitions and rules, conflicts between siblings and the acquisition of skills) are exacerbated by the chronic disease [22]. Dealing with daily problems might become more complicated for the parents due to continuous requirements of the diabetes therapy and lack of social support.
On the other hand parents’ well-being and positive family functioning seem to be associated with better metabolic control [15,23]. The importance of a balanced, cooperative family atmosphere has been reviewed and documented particularly for adolescents and older children with diabetes [19,24,25]. In the ISPAD Consensus Guidelines Delamater stated that behavioural concepts could support a positive family atmosphere and thereby improve psychological and physical outcomes of children with type 1 diabetes [25]. Several national and international paediatric diabetes guidelines strongly recommend pedagogic and psychological support for parents of children with diabetes [2,4,25]. Concurrently randomized controlled trials on this topic are rare [26-28]. Some elements of (cognitive) behavioural based parenting trainings have been evaluated scientifically with first results being promising [29-33]. Most of these studies focused on diabetes specific situations and challenges. However, there is no structured concept including general relevant (cognitive) behavioural parenting strategies. Due to the close association between general and diabetes specific parenting problems a wider range of strategies may be necessary to reduce parenting stress and family conflicts. For parents of healthy children several training programs on successfully solving typical conflict situations have been developed and implemented worldwide [for a survey see [34]. Scientific studies and meta-analyses demonstrate the efficacy of behavioural parent trainings and behavioural therapy elements on family functioning [35-38].
On this background the DELFIN parenting program is integrating general parenting strategies and diabetes specific conflict situations. It is based on principles of behaviour therapy and includes effective strategies of other general training programs [e. g. 35–38]. These strategies are supposed to reduce parental stress, anxiety and depression as well as children’s behavioural difficulties. Thus the current study for the first time evaluates the feasibility and effectiveness of a structured behavioural parenting training for parents of toddlers, pre-school and elementary school children with type 1 diabetes. It is hypothesized that the program participation (intervention group) would induce less negative parenting behaviour in conflict situations, support positive parenting behaviour in general and reduce parents’ psychological burden (anxiety, depression and stress). In addition children’s behaviour difficulties should decrease from their parents’ perspective.
Methods
Study design and recruitment
A randomized controlled group design with the control group being wait-listed was established. Inclusion criteria for families were: child with type 1 diabetes aged 2–10 yrs; no further psychological interventions; ability to read and speak German, willingness to participate. A total of 109 families with a child with type 1 diabetes in this age range were cared for at the children’s hospital “Kinderkrankenhaus auf der Bult”.
Parents were recruited by parent-conferences, posters, flyers or direct contact via their medical practitioner or diabetes educator. Fifty eight families gave their contact details for a preliminary telephone interview. Of these six families were excluded because they either were in psychotherapy or were unable to speak German. Twelve families refused to participate: too long drive from the clinic (n = 3); too time consuming (n = 7); no adequate child care (n = 2). Three families could not be reached. Thirty seven families were assigned to the DELFIN intervention or the waiting-list control group by simple randomization with a 1:1 allocation ratio. Of the latter, four families refused to participate after randomization (one for unknown reason, one because the family started family-psychotherapy, two for expenditure of time).
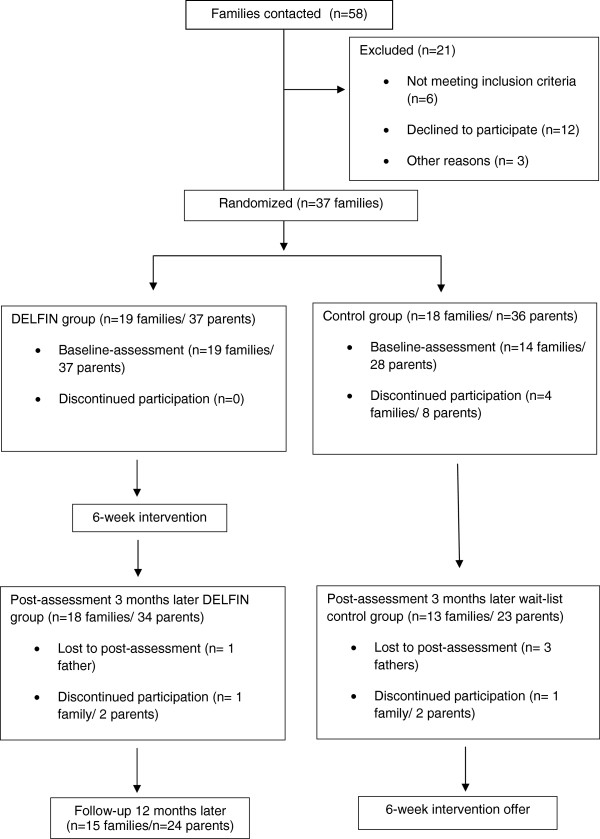
Overall 65 parents (n = 33 mothers; n = 32 fathers) completed the baseline questionnaires. Fifty seven parents completed the post-assessment 3 months later and 24 parents of the intervention group completed the follow-up assessment after 12 months. The first outcome point was chosen to give the parents opportunities to establish their new skills in daily life and to be able to detect changes in A1c. The reasons for drop-out at 3 months (n = 8, 5 of them controls) were: child in psychotherapy (n = 2); severe illness of one parent (n = 2); no more interest in the study (n = 4) (Figure 1).
Figure 1.
Schedule of enrollment, allocation and intervention.
Parents provided assent according to approved human subject procedures. Survey data was collected through a questionnaire sent to the family’s home using a prepaid envelope. Families were provided a one-time incentive of €30 for the assessment. Medical data was taken from the routine clinical care. The study was performed according to the criteria of the Helsinki II Declaration and approved by the Ethics Committee of the Hannover Medical School (Nr. 4958).
DELFIN intervention
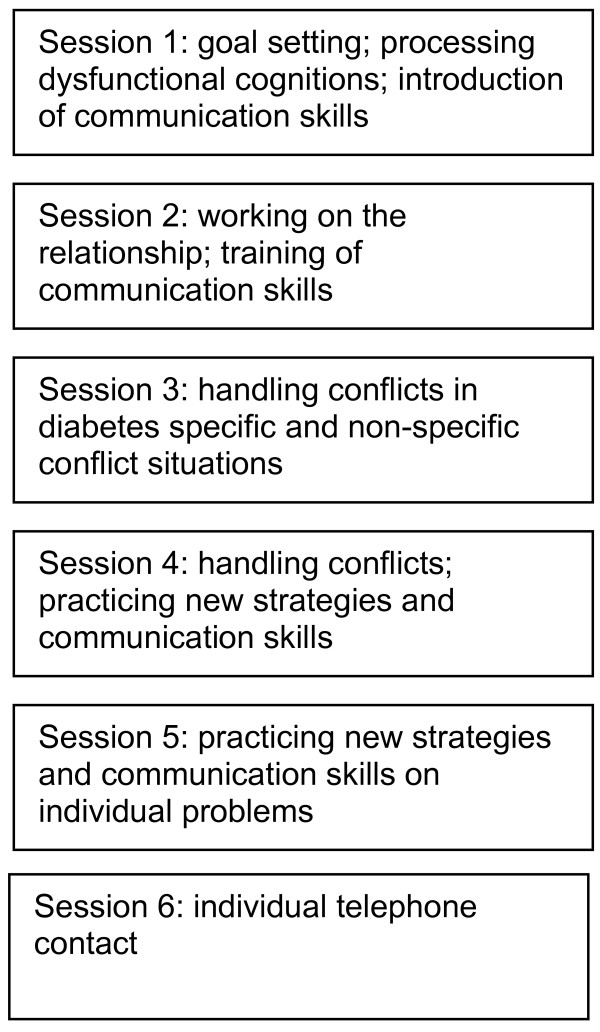
The DELFIN program (DELFIN – Das Elterntraining für Eltern von Kindern mit Diabetes Typ 1 (The parenting program for parents of children with diabetes type 1) was developed in addition to already existing accredited educational programs for children with type 1 diabetes and their parents. It is a structured group intervention for parents based on behavioural principles to strengthen their general and diabetes specific education competences. Parents are trained in groups with up to 7 families. They meet weekly for a 2 hours session over a period of 5 weeks and receive an individual phone contact the week after (see Figure 2). The parent training was run by an experienced psychologist.
Figure 2.
Structure of the DELFIN program.
The contents of the first session are the processing of dysfunctional cognitions, goal setting and theoretical discussion of communication skills. In the second session several strategies to work on a positive relationship with children are introduced. Parents practice communication skills in standardized role plays. Homework for these sessions includes among others the detection and substitution of dysfunctional cognitions and the phrasing of concrete and realistic goals.
In session 3 helpful parenting skills to solve typical family conflicts are developed. Sessions 4 and 5 focus on practical skill training with regard to the particular challenges of families with a chronically ill child (e. g. catheter insertion, injection, blood glucose measurement, dealing with high or low blood glucose, diabetes specific dysfunctional cognitions, feeling of guilt). These sessions also address general age specific parenting problems like temper tantrums or disobedience. Strategies are initially practiced in standardized role plays, later on in individual role plays. Weekly homework includes the transition of the new strategies into family routine.
Measures
Socio-demographic data
Socio-demographic data (age, sex, diabetes duration, level of parental education, distance to the clinic) were collected via a structured questionnaire.
Psychological self-report inventories
The Parenting Scale [PS; [39] was used in the German version [40] to assess parent education skills in conflict situations. It consists of 35 double sided verbalized items and delivers 3 scales: overreactivity (12 items; α = .81/.81 (mothers/fathers)), laxness (11 items; α = .71/.67) and verbosity (6 items; α = .64/.58) as well as a total score (α = .81/.75). Each item is ranked on a 7 point Likert scale with the end points describing effective parenting behaviour and ineffective behaviour, respectively. The total score as well as the subscales scores are calculated via means with higher scores indicating more ineffective parenting behaviour.
The Questions to Education Behaviour [Fragen zum Erziehungsverhalten; FZEV; [40,41] form was developed to assess positive, helping and reinforcing parental behaviour. Thirteen Items were combined to a total score (α = .85/.87) via calculation of mean. The items are assessed on a 4 point scale with higher scores indicating more positive parenting behaviour.
The Depression-Anxiety-Stress Scale [DASS; [42] was used in the German version [43] and consists of 42 Items describing different psychological symptoms. It delivers 3 scales with 14 Items each: depressed mood (α = .93/.93), anxiety (α = .82/.85) and stress (α = .82/.86) as well as a total score (α = .96/.95). Items are assessed on a 4 point scale. Cumulative values are calculated with higher scores indicating higher psychological distress. Total value varies between 0 and 42 for each subscale and between 0 and 126 for the total score.
The parents’ version of the Strengths and Difficulties Questionnaire [SDQ; [44,45] is a brief behavioural questionnaire, assessing 4 areas of potential difficulties (emotional symptoms, hyperactivity, conduct and peer relationship problems). They are summed up to a total difficulties score (20 Items). Another scale assesses pro-social behaviour (5 Items). Each item is ranked on a 3 point scale with higher scores indicating more difficulties or positive behaviour, respectively. The range of the total difficulties score is 0–40 (cumulative value), the one of the pro-social behaviour score is 0–10.
Satisfaction with the DELFIN program was assessed via a structured questionnaire. Questions were rated on a 7 point Likert-scale with 1 being “not satisfied” and 7 being “very much satisfied”.
Biomedical data
Biomedical data was taken from the prospective medical records including A1c, frequency of acute complication (severe hypoglycaemia, DKA) and insulin regimen. A1c was measured centrally via DCATM, Siemens Healthcare Diagnostics.
Analysis
All analyses were completed using SPSS v18. Group comparisons were conducted using simple independent t-tests, Chi2-Tests, Wilcoxon-, Mann–Whitney-U-Tests or Kruskal-Wallis-H-Tests. In addition a general linear model was conducted for group x time analyses. Correlations between ordinal variables were conducted using Spearman’s p correlation coefficient. All results being significant at p < 0.05, unless otherwise stated.
Results
Socio-demographic, metabolic and psychological status at study entry
Families of the DELFIN group did not differ significantly from the controls according to age of parents, age of the index-child, number of siblings, gender of the index-child, education level of mothers or insulin delivery modality (Table 1). However, the fathers in the DELFIN group were significantly higher educated than those in the control group. All children were on intensified insulin therapy. Of those 81% (n = 27) were on CSII; the others on multiple daily injection therapy (MDI). At study entry 73% (n = 24) of the children were in good metabolic control (A1c < 7.5%), 24% (n = 8) in moderate control (A1c 7.5 - 9%) and one child was in insufficient control (A1c > 9.0%). In all but one psychological measure there were no significant differences between control and DELFIN parents. The intervention group parents scored higher on one subscale of the Parenting Scale, stating that they tend more frequently to inadequate intense reactions in parenting conflict situations than the control group parents (Z = −2.59, p = .01).
Table 1.
Sociodemografic characteristics of the sample (control = control group; DELFIN = intervention group)
| |
control |
DELFIN |
||
|---|---|---|---|---|
| Mean (SD) | Mean (SD) | t | p | |
| age mother (yrs) |
40.4 (3.8) |
39.1 (3.3) |
−1.04 |
n.s. |
| age father (yrs) |
42.4 (6.5) |
43.3 (5.5) |
0.42 |
n.s. |
| age of the index child (yrs) |
5.8 (1.9) |
6.4 (2.3) |
0.78 |
n.s. |
| number of siblings |
0.79 (0.58) |
0.95 (0.69) |
0.75 |
n.s. |
| |
N (%) |
N (%) |
Chi2 (df) |
p |
| Education level mothers |
|
|
|
|
| Certificate of secondary education (8 grades) |
2 (14) |
1 (5) |
6.8 (3) |
n.s. |
| General certificate of secondary education (10 grades) |
6 (43) |
6 (32) |
|
|
| A-Level (13 grades) |
6 (43) |
5 (26) |
|
|
| University |
0 (0) |
7 (37) |
|
|
| Education level fathers |
|
|
|
|
| Certificate of secondary education (8 grades) |
1 (7) |
2 (11) |
9.09 (3) |
.028 |
| General certificate of secondary education (10 grades) |
6 (43) |
1 (5) |
|
|
| A-Level (13 grades) |
4 (29) |
3 (17) |
|
|
| University |
3 (21) |
12 (67) |
|
|
| |
Mean (SD) |
Mean (SD) |
t |
p |
| Diabetes duration in years |
2.6 (1.9) |
2.6 (1.6) |
−0.05 |
n.s. |
| A1C |
7.1 (0.4) |
7.2 (0.8) |
0.82 |
n.s. |
| |
N (%) |
N (%) |
Chi2 (df) |
p |
| Insulin regimen index child |
|
|
|
|
| CSII |
11 (79) |
16 (84) |
0.23 (1) |
n.s. |
| MDI |
3 (21) |
3 (16) |
|
|
| rate of severe hypoglycemia last 12 month |
0 (0) |
2 (10) |
3,22 (1) |
n.s. |
| DKA last 12 month | 0 (0) | 1 (5) | 1,56 (1) | n.s. |
Outcomes three months after intervention
Adverse parenting behaviour (Parenting-Scale, PS): After the intervention the difference between intervention and control group on the subscale “overreaction” was no longer existent due to improvements in the DELFIN group (Table 2). Compared to study entry the DELFIN parents improved their parenting behaviour on all 3 subscales as well as on the total score of the PS. Nevertheless, there were no significant time x group effects (all repeated-measure analyses with p > .05, with F (1/55) = 2.49 and p = .12 for the total score). Unexpectedly parents of the control group improved significantly on the subscale PS-verbosity (talking and discussing a lot with the child in conflict situations) and on the total score.
Table 2.
Comparison control vs. DELFIN group
|
Variable |
control |
DELFIN |
||||||
|---|---|---|---|---|---|---|---|---|
| baseline mean (SD) | post mean (SD) | Z | p ≤ | baseline mean (SD) | post mean (SD) | Z | p ≤ | |
| PS-total |
3.1 (0.6) |
3.0 (0.5) |
−2.45 |
.05 |
3.4 (0.5) |
2.9 (0.7) |
−3.28 |
.001 |
| PS-overreactivity |
3.2 (0.9) |
3.1 (0.8) |
−1.20 |
n.s. |
3.8 (0.8) |
3.4 (0.9) |
−2.58 |
.01 |
| PS-laxness |
2.7 (0.9) |
2.5 (0.8) |
−1.35 |
n.s. |
2.6 (0.6) |
2.3 (0.8) |
−2.51 |
.01 |
| PS-verbosity |
3.6 (0.8) |
3.2 (0.8) |
−2.17 |
.05 |
3.6 (0.9) |
3.0 (1.0) |
−3.06 |
.01 |
| DASS-total |
21.9 (15.4) |
17.3 (10.3) |
−2.10 |
.05 |
25.5 (15.2) |
20.0 (13.4) |
−1.93 |
.05 |
| DASS-depression |
5.2 (5.1) |
4.1 (4.1) |
−0.96 |
n.s. |
6.2 (5.8) |
4.7 (5.4) |
−1.93 |
.05 |
| DASS-anxiety |
4.9 (4.4) |
3.1 (2.8) |
−2.02 |
.05 |
4.5 (4.6) |
2.8 (2.6) |
−2.02 |
.05 |
| DASS-stress |
11.8 (6.5) |
10.0 (5.2) |
−2.11 |
.05 |
14.8 (7.6) |
12.4 (6.9) |
−1.05 |
n.s. |
| FZEV-positive parenting behavior |
1.9 (0.4) |
1.9 (0.4) |
−1.09 |
n.s. |
1.9 (0.4) |
1.9 (0.4) |
−0.22 |
n.s. |
| SDQ-total difficulties score |
8.3 (4.4) |
7.8 (4.1) |
−1.31 |
n.s. |
8.3 (4.8) |
6.9(3.9) |
−1.85 |
n.s. |
| Scores over the clinical cut-points |
n = 3 |
n = 2 |
Chi2 = 14.6 |
.01 |
n = 7 |
n = 2 |
Chi2 = 9.92 |
.01 |
| SDQ-prosocial behaviour | 7.4 (1.9) | 7.3 (1.9) | −0.73 | n.s. | 7.3 (1.6) | 7.7(1.5) | −1.92 | n.s. |
Parents’ psychological distress (Depression-Anxiety-Stress-Scale, DASS): Psychological distress (total score, depression and anxiety scale) decreased significantly in the DELFIN group (Table 2). There were no significant time x group effects (all analyses from general linear models with p > .05 and F (1/55) = .02, p = .88 for the total score). Unexpectedly in the control group a significant reduction of anxiety, stress and of the total DASS-score was observed.
Positive parenting behaviour (Questions to Education Behaviour, FZEV): There were no significant differences regarding positive parenting behaviour (FZEV) before and after the training in both study groups. Also there were no differences between the groups (F (1/55) = .97, p = .33).
Strength and difficulties of the child (Strengths and Difficulties Questionnaire, SDQ): The psychological wellbeing of the children improved slightly in the DELFIN group, but this difference did not reach statistical significance neither within nor in between the two groups (F (1/55) = .05, p = .82 for the difficulties score and F (1/55) = .23, p = .64 for the pro-social behaviour score). However, the number of children above the cut-off for clinical problems decreased significantly in the DELFIN group (Table 2).
Metabolic control (A1c): While the good quality of control was stable after 3 months in the DELFIN group (7.2±0.8% vs. 7.1±0.8%, Z = −1.19, p > .05), the mean A1c increased significantly in the control group (7.1±0.4% vs. 7.3±0.5%, Z = −2.79, p ≤ 0.005). The interaction was significant in the group x time analysis (F (1/32) = 5.3, p = .029). This result has to be discussed with care due to the overall good metabolic control of the majority of children and the small sample size.
Effect sizes were calculated for the control and the DELFIN group (Table 3). They were moderate to high for the reduction of negative parenting behaviour in the intervention group. Comparing parenting behaviour (PS-Parenting Scale) and parent assessment of their child (SDQ) the effect sizes were higher in the intervention group than in the control group. For parents’ stress, depression and anxiety small effect sizes were observed in both study arms.
Table 3.
Effect sizes (d) for control and DELFIN group
| Variable | control | DELFIN | ||||
|---|---|---|---|---|---|---|
| |
baseline mean (SD) |
post mean (SD) |
effect size d |
baseline mean (SD) |
post mean (SD) |
effect size d |
| PS-total |
3.1 (0.6) |
3.0 (0.5) |
.18 |
3.4 (0.5) |
2.9 (0.7) |
.84 |
| PS-overreactivity |
3.2 (0.9) |
3.1 (0.8) |
.12 |
3.8 (0.8) |
3.4 (0.9) |
.48 |
| PS-laxness |
2.7 (0.9) |
2.5 (0.8) |
.24 |
2.6 (0.6) |
2.3 (0.8) |
.43 |
| PS-verbosity |
3.6 (0.8) |
3.2 (0.8) |
.51 |
3.6 (0.9) |
3.0 (1.0) |
.64 |
| DASS-total |
21.9 (15.4) |
17.3 (10.3) |
.35 |
25.5 (15.2) |
20.0 (13.4) |
.39 |
| DASS-depression |
5.2 (5.1) |
4.1 (4.1) |
.24 |
6.2 (5.8) |
4.7 (5.4) |
.27 |
| DASS-anxiety |
4.9 (4.4) |
3.1 (2.8) |
.49 |
4.5 (4.6) |
2.8 (2.6) |
.46 |
| DASS-stress |
11.8 (6.5) |
10.0 (5.2) |
.31 |
14.8 (7.6) |
12.4 (6.9) |
.33 |
| FZEV-positive parenting behaviour |
1.9 (0.4) |
1.9 (0.4) |
.00 |
1.9 (0.4) |
1.9 (0.4) |
.00 |
| SDQ-total difficulties score |
8.3 (4.4) |
7.8 (4.1) |
.12 |
8.3 (4.8) |
6.9(3.9) |
.32 |
| SDQ-prosocial behaviour | 7.4 (1.9) | 7.3 (1.9) | .05 | 7.3 (1.6) | 7.7(1.5) | .26 |
Outcomes at 12 months follow-up
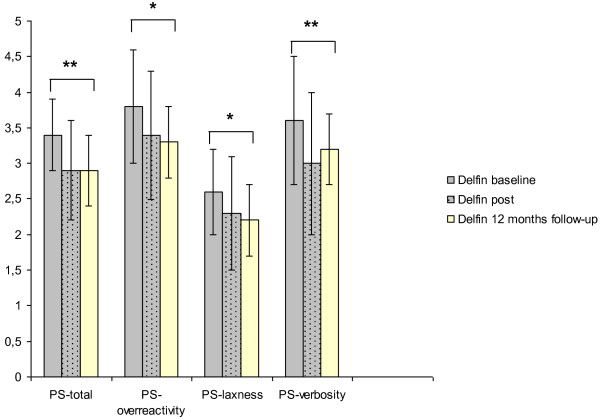
The improvement in parenting behaviour in conflict situations (PS-Scale) was stable after 12 months in the DELFIN group (Figure 3). Compared to baseline measures adverse parenting behaviour decreased significantly for the total score as well as for all 3 subscales (PS-total Z = −2.9; p ≤ 0.01; PS-overreactivity Z = −2.2; p ≤ 0.05; PS-laxness Z = −2.0; p ≤ 0.05; PS-verbosity Z = −2.4; p ≤ 0.01). After 12 months there were no significant differences compared to the measures at 3 months on the PS-Scale and all other psychological measures (all p > .05).
Figure 3.
Parenting skills of DELFIN parents baseline, 3 months after the intervention and at 12 months follow-up.
Associations between parents’ wellbeing and parenting skills
For the parents of the DELFIN group Spearman-correlations between the self-reporting measures are summarized in Table 4. Positive parenting behaviour (FZEV) was negatively associated with depression (r = −.37, p = .024) and with the tendency to accommodate the child in conflict parenting situations (EFB-laxness; r = −.43, p = .007). Parents’ psychological distress was positively associated with negative parenting behaviour (r = .37, p = .23). Particularly, the tendencies to back down and to overreact and exaggerate in conflict situations were associated with higher psychological burden (Table 4).
Table 4.
Spearman-correlations for the intervention group (n = 37)
| DASS-total | DASS-depr. | DASS-anxiet. | DASS-stress | EFB-total | EFB-overr. | EFB-laxn. | EFB-verb. | SDQ | A1C | |
|---|---|---|---|---|---|---|---|---|---|---|
| |
Rho (p) |
Rho (p) |
Rho (p) |
Rho (p) |
Rho (p) |
Rho (p) |
Rho (p) |
Rho (p) |
Rho (p) |
Rho (p) |
| FZEV-pos. behav. |
-.084 (.620) |
-.37 (.024) |
-.01 (.956) |
.04 (.815) |
-.30 (.069) |
-.27 (.106) |
-.43 (.007) |
-.04 (.797) |
.26 (.124) |
-.27 (.034) |
| DASS-total |
|
|
|
|
.37 (.023) |
.51 (.001) |
.33 (.049) |
-.01 (.971) |
.21 (.223) |
.14 (.279) |
| DASS-depr. |
|
|
|
|
.30 (.071) |
.40 (.015) |
.39 (.018) |
.017 (.919) |
.07 (.664) |
.14 (.264) |
| DASS-anxiet. |
|
|
|
|
.28 (.089) |
.43 (.009) |
.28 (.089) |
.09 (.609) |
.26 (.125) |
.05 (.711) |
| DASS-stress | .33 (.043) | .48 (.003) | .25 (.142) | -.04 (.821) | .18 (.298) | .10 (.443) |
Satisfaction with the DELFIN program
Twenty four parents completed the assessment on satisfaction with DELFIN program. Of them 22 were satisfied/very satisfied with the program (point 6–7) and 20 were satisfied/very satisfied with the support given by the trainer. The majority of parents evaluated all 5 sessions as comparably important (n = 13). Fourteen of the 19 families of the DELFIN group attended all 5 group sessions. Only 5 missed one group session (due to time strains, illness or lack of babysitter). Considering an average distance of 43.8 km (min 0.5 km - max 144.5 km) to the clinic this supports high intervention fidelity of the participants. Each family attended the individual telephone contact (session 6). All participants were regularly prepared for the sessions and had done their practical trainings (homework). In order to support intervention receipt, homework interviews were carried out with each parent at the beginning of the sessions. Implementation of new strategies to solve family conflict situations were reported by all participants. Individual situations were analyzed and suitable solutions were worked out, if problems occurred. Parents were asked to try out new solutions within the next week.
Discussion
The randomized controlled pilot study assessed the effectiveness of a behavioural training program especially for parents of young children with type 1 diabetes. The results point to improved parenting skills and slightly reduced parenting stress. The pilot study on this psychological-based concept supports the feasibility of the parenting program. The first data provide important information for conducting a larger multisite clinical trial to confirm the efficacy of the program.
Recruitment, sample and participation
The high expenditure of time was the main reason for originally interested families not to participate in the program. Therefore future studies should consider alternative methods of offering such a program since the long drive to the clinic, excessive burden due to the time investment or the lack of care for the children were the most common reasons for many families not to participate in the study. Alternatively the intervention could be delivered during routine clinic visits as successfully practiced with other interventions [46]. Short-term-interventions like seminars on weekends, specific short interventions dealing with one topic or internet-based sessions may be reasonable concepts to increase the attendance. On the other hand, more than half of the parents rated all 5 group sessions as comparably important, and many of them required longer sessions. A reduction of intervention time would also mean less information and exercise for the parents and thus probably reduced efficacy of the program.
Monaghan et al. [32] developed a brief telephone-based supportive intervention for parents, which is a very economic way to run a program. The cognitive-behavioural therapy elements of the DELFIN program (e. g. dysfunctional cognitions) may be delivered via telephone contact to reduce the number of group sessions. But the important interaction between different parents on this topic would get lost. The same may be the case for the main part of the program, the behavioural therapy elements and the practical training of parental behaviour.
In addition to more flexibility in delivering and recruiting, a higher homogeneity of age in the groups could further increase the efficacy of the training. From practical experience during the sessions it has become obvious that too high heterogeneity of the children’s age is challenging for the thematic organization of the courses. This study included families with children between 2 to 10 years of age. However, the every day conflicts of parents caring for toddlers, pre-school-children or primary school children differ considerably. Due to these age-specific challenges, different educational strategies become more important and have to be customized for each subgroup. Furthermore, there are various diabetes specific conflicts depending on the cognitive developmental status of the child and its ability for self-management. Parents of pre-school-children for instance are responsible for the entire therapy and the continuous supervision. In contrast parents of older children often have to deal with insufficient adherence and autonomy conflicts.
Eligibility and performance of outcome measures
The measurements adopted in this study can be considered appropriate. In their oral feedback parents rated the assessment form as acceptable and easy to understand. In a larger trial it would be desirable to include behavioural observations, assessment by (day care) teachers and an interview with the parents. Observational data could be collected during a home visit. This would probably also increase the retention rate.
The participants of the DELFIN-program reported a reduction in adverse parenting behaviour and partial improvement of psychological wellbeing. Probably due to the small sample size, these effects were not significant compared to the control group. Another reason might be that slight reductions in psychological distress, adverse parenting behaviour and behavioural difficulties of the child were also seen in the control group. These findings may be based on the Hawthorne-effect or were probably accidental. On the other hand, parenting behaviour might improve step by step without external intervention. This hypothesis contradicts findings of other authors describing negative parental behaviour as stable [38,40]. Another explanation might be a tendency of parents’ to give socially desirable answers. This problem could be accounted for by observational data in further studies.
The reduction of negative parenting behaviour was stable after 12 months in the intervention group, indicating that parents implement new strategies in their day to day behaviour on the long run. Unfortunately no changes were detected for positive parenting behaviour. Parents of children with type 1 diabetes have to spend many hours together with their child managing diabetes therapy. Due to this it’s probably difficult for them to increase their positive parenting behaviour e.g. playing or joking with the child.
Limitations
It has to be considered that there was a self selection in this pilot sample, which might have influenced the outcome. Particularly in the control group many families refused to participate after being randomized. For them the waiting period might have been too long. Instead some of them looked for immediate psychological support and dropped out. This probably resulted in an overlap of families with a positive parenting status in the control group. Another critical point is the small sample size. A larger group of parents would allow more differentiated analysis, e. g. according to gender, participation rate, education level, child’s age and quality of metabolic control. Findings in this study are limited by conjunct observations of mothers and fathers, while other studies showed differences in parenting behaviour and outcome performance between mothers and fathers [41]. The study was performed in one German paediatric diabetes centre with an experienced multidisciplinary team caring holistically for children with diabetes and their families as standard care. Independent from this study the metabolic control of all children aged < 12 yrs is relatively good (mean centre A1c prepubertal children (n = 109) = 7.1%). In this overall positive situation it is challenging to improve the metabolic and psychological outcomes. This quite positive situation at study onset might not be representative for other pediatric diabetes units in Germany or worldwide [47].
Conclusions
This study provides preliminary evidence that parents of children with type 1 diabetes may benefit from a parenting program focussing on specific as well as unspecific conflict situations and practical training of positive parenting strategies. There was first evidence that the DELFIN program for parents of young children with type 1 diabetes tends to improve parenting behaviour and the psychological status of the parents. The program predominantly reduced negative parenting behaviour. Due to the small sample size of this pilot study a long term multisite clinical trial is necessary to confirm these first findings. It is a great challenge to organize parent trainings for families often driving long distances to the specialized diabetes centres. To realize an adequate sample size, the program should be offered and evaluated in different settings, e.g. weekend meeting, specific short interventions or internet based sessions. Homogeneous age groups could help to reduce the required time for group sessions. In addition to parents’ self-reports as outcome parameters, observational data on their behaviour should be included.
Heike Saßmann is the Guarantor of this work and, as such, had full access to all of the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis.
Competing interests
The author(s) declare that they have no competing interests.
Authors’ contributions
H.S., K.L., M.dH. wrote the manuscript, H.S. and M.dH. analysed the data, H.S., M.dH., K.L. and T.D. contributed to data collection and/or commented on the paper. All authors read and approved the final manuscript.
Pre-publication history
The pre-publication history for this paper can be accessed here:
Contributor Information
Heike Saßmann, Email: sassmann.heike@mh-hannover.de.
Mira de Hair, Email: Mira.Hair@stud.mh-hannover.de.
Thomas Danne, Email: danne@hka.de.
Karin Lange, Email: lange.karin@mh-hannover.de.
Acknowledgements
The German Diabetes Association (DDG) is gratefully acknowledged for their support (‘Menarini-Award’). Parts of this publication have been presented in 2011 at the annual meeting of the German Diabetes Association (DDG).
References
- Danne T, von Schütz W, Lange K, Nestoris C, Datz N, Kordonouri O. Current practice of insulin therapy in children and adolescents – the hannover recipe. Pediatr Diabetes. 2006;7:25–31. doi: 10.1111/j.1399-543X.2006.00166.x. [DOI] [PubMed] [Google Scholar]
- Holterhus PM, Beyer P, Bürger-Büsing J, Danne T, Etspüler J, Heidtmann B, Holl RW, Karges B, Kiess W, Knerr I, Kordonouri O, Lange K, Lepler R, Marg W, Näke A, Neu A, Petersen M, Podeswik A, Stachow R, von Sengbusch S, Wagner V, Ziegler R. Diagnostik, Therapie und Verlaufskontrolle des Diabetes mellitus im Kindes- und Jugendalter. [Diagnosis, therapy and management of diabetes mellitus in children and adolescents. Kirchheim: Mainz; 2009. [Google Scholar]
- Silverstein J, Klingensmith G, Copeland K, Plotnick L, Kaufman F, Laffel L, Deeb L, Grey M, Anderson B, Holzmeister LA, Clark N. American Diabetes Association. Care of children and adolescents with type 1 diabetes: a statement of the American Diabetes Association (ADA statement) Diabetes Care. 2005;28:186–212. doi: 10.2337/diacare.28.1.186. [DOI] [PubMed] [Google Scholar]
- National Institute for Clinical Excellence (NICE) Clinical guideline 15: Type 1 Diabetes: diagnosis and management of type 1 diabetes in children, young people and adults. 2004.
- Bangstad H-J Danne T Deeb LC Jarosz-Chobot P Urakami T Hanas R ISPAD Clinical Practice Consensus Guidelines 2009, Insulin treatment in children and adolescents with diabetes Pediatr Diabetes 20091082–99.19754621 [Google Scholar]
- Lange K, Saßmann H, von Schütz W, Kordonouri O, Danne T. Prerequisites for age-appropriate education in type 1 diabetes: a model programme for paediatric diabetes education in Germany. Pediatr Diabetes. 2007;8:63–71. doi: 10.1111/j.1399-5448.2007.00277.x. [DOI] [PubMed] [Google Scholar]
- Swift PGF. Diabetes education in children and adolescents. ISPAD clinical practice consensus guidelines 2009 compendium. Pediatr Diabetes. 2009;10(Suppl. 12):51–57. doi: 10.1111/j.1399-5448.2009.00577.x. [DOI] [PubMed] [Google Scholar]
- Hürter P, Jastram H-U, Regling B, Toeller M, Lange K, Weber B, Burger W, Haller R. Diabetes bei Kindern: ein Behandlungs- und Schulungsprogramm. [Diabetes in children: a structured programme for care and education] 3. Kirchheim: Mainz; 2005. [Google Scholar]
- Lange K, Burger W, Holl R, Hürter P, Saßmann H, von Schütz W, Danne T. Diabetes bei Jugendlichen: ein Behandlungs- und Schulungsprogramm. [Diabetes in adolescence: a structured programme for care and education] 2. Kirchheim: Mainz; 2009. [Google Scholar]
- Hürter P, von Schütz W, Lange K. Kinder und Jugendliche mit Diabetes. [Children and adolescents with diabetes] Springer Verlag: Heidelberg; 2012. [Google Scholar]
- Lange K, Kleine T, Danne T. on behalf of the AG Diabetesschulung für Eltern. Initial education for parents of children with diabetes: effort and outcomes in children and parents. Dtsch Med Wochenschr. 2011;136:1106–1110. doi: 10.1055/s-0031-1280518. [DOI] [PubMed] [Google Scholar]
- Lange K, Kinderling S, Hürter P. Eine multizentrische Studie zur Prozess- und Ergebnisqualität eines strukturierten Schulungsprogramms [A multi-centre study for evaluating a structured education program] Diab Stoffw. 2001;10:59–65. [Google Scholar]
- Lange K, Burger W, Haller R, Heinze E, Holl R, Hürter P, Schmidt H, Weber B. Diabetes in adolescents: a programme for patient education. Patient Educ Couns. 1994;23:S120. [Google Scholar]
- Lange K, Hürter P. Effekte einer strukturierten Diabetesschulung für Jugendliche auf Stoffwechsel, Wissen, Wohlbefinden und Selbständigkeit – Ergebnisse einer multizentrischen Studie. [Effectivity of a structured diabetes education for adolescents on metabolic control, knowledge, well-being and self-management – results of a multi-centre study] Diab Stoffw. 1998;7:S62. [Google Scholar]
- Cameron FJ, Skinner TC, de Beaufort CE, Hoey H, Swift PG, Aanstoot H, Aman J, Martul P, Chiarelli F, Daneman D, Danne T, Dorchy H, Kaprio EA, Kaufman F, Kocova M, Mortensen HB, Njølstad PR, Phillip M, Robertson KJ, Schoenle EJ, Urakami T, Vanelli M, Ackermann RW, Skovlund SE. Hvidoere Study Group on Childhood Diabetes. Are family factors universally related to metabolic outcomes in adolescents with type 1 diabetes? Diabet Med. 2008;25:463–468. doi: 10.1111/j.1464-5491.2008.02399.x. [DOI] [PubMed] [Google Scholar]
- Wysocki T, Iannotti R, Weissberg-Benchel J, Hood K, Laffel L, Anderson BJ, Chen R. Family Management of Childhood Diabetes Steering Committee. Diabetes problem solving by youths with type 1 diabetes and their caregivers: measurement, validation and longitudinal associations with glycemic control. J Pediatr Psychol. 2008;33(8):875–884. doi: 10.1093/jpepsy/jsn024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Delamater AM, Jacobson AM, Anderson B, Cox D, Fisher L, Lustman P, Rubin R, Wysocki T. Psychosocial Therapies Working Group. Psychosocial therapies in diabetes. Report of the Psychosocial Therapies Working Group. Diabetes Care. 2001;24:1286–1292. doi: 10.2337/diacare.24.7.1286. [DOI] [PubMed] [Google Scholar]
- Laffel LMB, Connell A, Vangsness L, Goebel-Fabbri A, Mansfield A, Anderson BJ. General quality of life in youth with type 1 diabetes. Diabetes Care. 2003;26(11):3067–3073. doi: 10.2337/diacare.26.11.3067. [DOI] [PubMed] [Google Scholar]
- Jacobson AM, Hauser ST, Lavori P, Willett JB, Cole CF, Wolfsdorf JI, Dumont RH, Wertlieb D. Family environment and glycemic control: a four-year prospective study of children and adolescents with insulin-dependent diabetes mellitus. Psychosom Med. 1994;56:401–409. doi: 10.1097/00006842-199409000-00004. [DOI] [PubMed] [Google Scholar]
- Lange K, Danne T, Kordonouri O, Berndt V, Müller B, Schwarz H-P, Hesse V, Busse-Widmann P. Diabetesmanifestation im Kindesalter: Alltagsbelastungen und berufliche Entwicklung der Eltern [Diabetes onset in childhood: burden and professional consequences for parents] Dtsch Med Wochenschr. 2004;129:1130–1134. doi: 10.1055/s-2004-824861. [DOI] [PubMed] [Google Scholar]
- Patton S, Dolan LM, Smith LB, Thomas IH, Powers SW. Pediatric parenting stress and its relation to depressive symptoms and fear of hypoglycemia in parents of young children with type 1 diabetes mellitus. J Clin Psychol Med Settings. 2011;18(4):345–352. doi: 10.1007/s10880-011-9256-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Powers SW, Byars KC, Mitchell MJ, Patton SR, Standiford DA, Dolan LM. Parent report of mealtime behaviour and parenting stress in young children with type 1 diabetes and in healthy control subjects. Diabetes Care. 2002;25:313–318. doi: 10.2337/diacare.25.2.313. [DOI] [PubMed] [Google Scholar]
- Lange K, de Beaufort C, Fisher LK, Hoey H, Kocova M, Mortensen HB, Danne T, Neu A, Robert JJ, Kaprio E, Castano L, Schönle EJ, Aman J, Phillip M, Vanelli M, Urakami T, Cameron F, Njolstad PR, Dorchy H, Barrett TG, Aanstoot HJ, Chiarelli F, Robertson KJ, Swift P. Hvidoere Study Group. Prevalence of behaviour difficulties and their predictors in an international cohort of 1090 young children with type 1 diabetes. Pediatr Diabetes. 2011;12(Suppl. 15):20. [Google Scholar]
- Anderson BJ, Ho J, Brackett J, Finkelstein D, Laffel L. Parental involvement in diabetes management tasks: Relationships to blood glucose monitoring adherence and metabolic control in young adolescents with insulin-dependent diabetes mellitus. J Pediatr. 1997;130:257–265. doi: 10.1016/S0022-3476(97)70352-4. [DOI] [PubMed] [Google Scholar]
- Delamater AM Psychological care of children and adolescents with diabetes. ISPAD Clinical Practice Consensus Guidelines 2009 Compendium Pediatr Diabetes 200910Suppl. 12175–184.19754628 [Google Scholar]
- Barlow JH, Coren E, Stewar-Brown S. Meta-analysis of the effectiveness of parenting programmes in improving maternal psychosocial health. Br J Gen Pract. 2002;52:223–233. [PMC free article] [PubMed] [Google Scholar]
- Barlow JH, Ellard DR. Psycho-educational interventions for children with chronic disease, parents and siblings: an overview of the research evidence base. Child Care Health Dev. 2004;30(6):637–645. doi: 10.1111/j.1365-2214.2004.00474.x. [DOI] [PubMed] [Google Scholar]
- Hampson SE, Skinner TC, Hart J, Storey L, Gage H, Foxcroft D, Kimber A, Shaw K, Walker J. Effects of educational and psychosocial interventions for adolescents with diabetes mellitus: a systematic review. Health Technol Assess. 2001;5(10):1–79. doi: 10.3310/hta5100. [DOI] [PubMed] [Google Scholar]
- Méndez F, Beléndez M. Effects of a behavioural intervention on treatment adherence and stress management in adolescents with IDDM. Diabetes Care. 1997;20(9):1370–1375. doi: 10.2337/diacare.20.9.1370. [DOI] [PubMed] [Google Scholar]
- Patton SR, Dolan LM, Mitchell MJ, Byars KC, Standiford D, Powers SW. Mealtime interactions in families of pre-schoolers with type 1 diabetes. Pediatr Diabetes. 2004;5:190–198. doi: 10.1111/j.1399-543X.2004.00058.x. [DOI] [PubMed] [Google Scholar]
- Wysocki T, Harris M, Buckloh LM, Mertlich D, Lochrie AS, Taylor A, Sadler M, Mauras N, White NH. Effects of behavioral family systems therapy for diabetes on adolescents` family relationships, treatment adherence, and metabolic control. J Pediatr Psychol. 2006;31(9):928–938. doi: 10.1093/jpepsy/jsj098. [DOI] [PubMed] [Google Scholar]
- Monaghan M, Hilliard ME, Cogen FR, Streisand R. Supporting parents of very young children with type 1 diabetes: Results from a pilot study. Patient Educ Couns. 2011;82:271–274. doi: 10.1016/j.pec.2010.04.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sullivan-Bolyai S, Bova C, Leung K, Trudeau A, Lee M, Gruppuso P. Social support to empower parents (STEP): an intervention for parents of young children newly diagnosed with type 1 diabetes. Diabetes Educ. 2010;36:88–97. doi: 10.1177/0145721709352384. [DOI] [PubMed] [Google Scholar]
- Heinrichs N, Saßmann H, Hahlweg K, Perrez M. Prävention von Verhaltensauffälligkeiten bei Kindern [Prevention of behavioural problems in children] Psychologische Rundschau. 2002;53:170–183. doi: 10.1026//0033-3042.53.4.170. [DOI] [Google Scholar]
- Kuschel A, Heinrichs N, Bertram H, Naumann S, Kessemeier Y, Saßmann H, Hahlweg K. In: Prävention und Gesundheitsförderung Bd. III, Kinder und Jugendliche. Röhrle B, editor. dgvt-Verlag, Tübingen; 2007. Die kurzfristige Effektivität eines Elterntrainings zur universellen Prävention kindlicher Verhaltensstörungen. [Short-term efficacy of a universal parent program to prevent behavioural problems in children; pp. 257–278. [Google Scholar]
- Taylor TK, Biglan A. Behavioral family interventions for improving child-rearing: a review of the literature for clinicians and policy makers. Clin Child Fam Psychol Rev. 1998;1(1):41–60. doi: 10.1023/A:1021848315541. [DOI] [PubMed] [Google Scholar]
- Serketich WJ, Dumas JE. The effectiveness of behavioural parent training to modify antisocial behaviour in children: a meta-analysis. Behav Ther. 1996;27:171–186. doi: 10.1016/S0005-7894(96)80013-X. [DOI] [Google Scholar]
- Sanders MR, Markie-Dadds C, Bor W, Tully LA. The Triple P – Positive Parenting Program: A comparison of enhanced, standard, and self-directed behavioural family intervention for parents of children with early onset conduct problems. J Consult Clin Psychol. 2000;68:624–640. [PubMed] [Google Scholar]
- Arnold DS, O`Leary SG, Wolff LS, Acker MM. The Parenting Scale: a measure of dysfunctional parenting in discipline situations. Psychol Assess. 1993;5(2):137–144. [Google Scholar]
- Miller Y. Erziehung von Kindern im Kindergartenalter: Erziehungsverhalten und Kompetenzüberzeugungen von Eltern und der Zusammenhang zu kindlichen Verhaltensstörungen. [Parenting of preschool children: parenting behaviour and competence beliefs of parents and relation with child behavioural problems] Technical University Braunschweig: PhD thesis; 2001. [Google Scholar]
- Heinrichs N, Hahlweg K, Bertram H, Kuschel A, Naumann S, Harstick S. Die langfristige Wirksamkeit eines Elterntrainings zur universellen Prävention kindlicher Verhaltensstörungen: Ergebnisse aus Sicht der Mütter und Väter. [Long-term efficacy of a universal parent program to prevent behavioural problems in children: from the point of view of mothers and fathers. Z Klin Psychol Psychother. 2006;35(2):82–96. doi: 10.1026/1616-3443.35.2.82. [DOI] [Google Scholar]
- Lovibond SH, Lovibond PF. Manual for the Depression Anxiety Scale. Sydney, NSW: Psychology Foundation of Australia; 1995. [Google Scholar]
- Köppe EC. Glückliche Eltern – Liebe Kinder? Auswirkungen von Partnerschaft und psychischer Symptomatik der Eltern auf das Verhalten ihrer Kinder. [Lucky parents – nice kids? Impact of relationship and psychological symptoms of parents on their children’s behaviour.] Technical University BraunschweigPhD thesis; 2001. [Google Scholar]
- Goodman R. The extended version of the Strengths and Difficulties Questionnaire as a guide to child psychiatric caseness and consequent burden. J Child Psychol Psychiatry. 1999;40:791–801. doi: 10.1111/1469-7610.00494. [DOI] [PubMed] [Google Scholar]
- Woerner W, Becker A, Rothenberger A. Normative data and scale properties of the German parent SDQ. Eur Child Adolesc Psychiatry. 2004;13:3–10. doi: 10.1007/s00787-004-2002-6. [DOI] [PubMed] [Google Scholar]
- Nansel TR, Anderson BJ, Laffel LMB, Simons-Morton BG, Weissberg-Benchell J, Wysocki T, Iannotti RJ, Holmbeck GN, Hood KK, Lochrie AS. A multisite trial of a clinic-integrated intervention for promoting family management of pediatric type 1 diabetes: feasibility and design. Pediatr Diabetes. 2009;10:105–115. doi: 10.1111/j.1399-5448.2008.00448.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lange K, Klotmann S, Saßmann H, Aschemeier B, Wintergerst E, Gerhardsson P, Kordonouri O, Szypanzka A, Danne T. the SWEET group. A pediatric diabetes toolbox for creating centres of reference. Pediatr Diabetes. 2012;13(Suppl 16):49–61. doi: 10.1111/j.1399-5448.2012.00913.x. [DOI] [PubMed] [Google Scholar]