Abstract
Forehead defects often present myriad challenges for the reconstructive surgeon. Many options exist for forehead reconstruction, from primary closure to free flaps. To optimally match colour, contour and texture, the best approach replaces ‘like with like’. When primary closure is not possible due to size limitations, and colour or depth is not suitable for grafts, then locoregional flaps become the mainstay of repair. The authors present three cases in which a dual-plane modified A to T flap is used to reconstruct central and lateral forehead defects up to 8 cm in size with excellent aesthetic results. This technique applies principles of the periglabellar flap, with modifications designed to encompass larger defects as well as defects of the lateral forehead.
Keywords: A to T, Forehead reconstruction, Large forehead defect
Abstract
Les anomalies du front comportent de multiples défis pour le plasticien. Il existe de nombreuses possibilités pour reconstruire le front, de la fermeture primaire aux lambeaux libres. Pour optimiser l’agencement de couleur, de contour et de texture, la meilleure démarche consiste à utiliser des structures similaires. Lorsqu’il est impossible de procéder à une fermeture primaire en raison des dimensions, et que la couleur ou la profondeur ne se prêtent pas à une greffe, les lambeaux locorégionaux deviennent le pilier de la reconstruction. Les auteurs présentent trois cas dans lesquels un lambeau en A modifié en lambeau en T en deux plans est utilisé pour reconstruire les anomalies centrales et latérales du front d’une dimension pouvant atteindre 8 cm et ainsi obtenir d’excellents résultats esthétiques. Cette technique met en application les principes du lambeau périglabellaire, et les modifications sont conçues pour englober des anomalies plus importantes et les anomalies de la partie latérale du front.
Forehead reconstruction is often challenging due to the aesthetic prominence of the area and difficulties in matching skin colour, contour and texture. Additionally, the forehead is typically a ‘donor’ site for facial reconstruction and lacks the abundance of matching adjacent tissue. Tumours (most commonly sun-related skin cancers) as well as trauma, congenital lesions and burns, make forehead reconstruction a common plastic surgical challenge. The size and location of the defect dictates the most appropriate approach, with the simplest usually being the most successful (1). However, larger defects require more complex techniques.
The reconstructive ladder for forehead wounds is reviewed to determine the best approach for each specific patient. Defects may be repaired using any of the following: healing by secondary intention, primary closure, skin grafting, local flaps, tissue expansion, regional flaps and free flaps. The optimal approach is often the simplest and strives to replace tissue with like tissue. With larger defects, the surrounding tissue must be recruited in a tension-free fashion to optimize the scar and terminal blood flow. We present an advancement flap for the repair of central and lateral forehead defects up to 8 cm in size that applies principles of the periglabellar flap as previously described by Birgfeld and Chang (2).
TECHNIQUE
The flap is designed with careful consideration of the final location of resulting scars to best camouflage within natural relaxed lines of tension, hair or brow lines. For central defects, horizontal superior limbs, with the length approximately equal to the diameter of the lesion, are designed to lie within the natural transverse forehead crease formed by the frontalis muscle. Two inferior vertical limbs, with widths equal to the radius of the lesion, are then marked to lie within creases formed by the corrugator muscles (Figure 1). Lateral defects are approached by placing the horizontal limbs inferiorly following the brow, which serves to conceal the eventual scar. The vertical limb extends cephalad toward the hairline and can extend back into the hairline or chased transversely at its apex depending on the patient’s hairline.
Figure 1).

The edges are freshened and horizontal and vertical triangles are designed to lie within creases of the frontalis and corrugator muscles, respectively
In all cases, care is taken to preserve the supratrochlear vessels and the frontal branch of the facial nerve. A dual-plane dissection carried out both superficial and deep to the galea is essential to both the functional and aesthetic appearance of the wound (Figure 2). The superficial plane dissection occurs just superficial to the frontalis muscle and deep to the subcutaneous tissue. The deep plane dissection occurs in the loose areolar tissue deep to the galea in all directions to recruit tissue. Lateral defect closure can be assisted by extending the vertical limb into the hairline to allow additional dissection across the horizon of the forehead.
Figure 2).
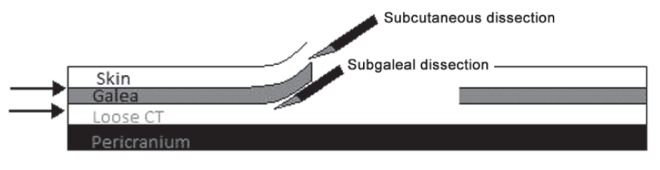
Dual-plane dissection, in subcutaneous and subgaleal planes, enables optimal en-bloc tissue advancement for closure of larger wounds plus tension-free and everted skin edges. CT Connective tissue
After completion of the posterior dissection, the galea is scored perpendicular to the long axis to improve tissue recruitment (Figure 3). Electrocautery is used to create short rents in the posterior galea; blunt separation to the intervening tissue is then performed to minimize injury to more superficial nerves and vessels. After extensive mobilization, advancement of the galea effectively offloads tension on the more superficial layers of the skin to improve cosmetic appearance. The anterior plane dissection facilitates eversion of the skin edges to improve scar quality.
Figure 3).

Scoring of the galea perpendicular to the vertical axis, facilitates superficial advancement toward the defect. Short releases with electrocautery and blunt joining of those segments helps prevent damage to superficial nerves
CASE PRESENTATIONS
Three cases of forehead defects ranging from 16 cm2 to 40 cm2 in size are shown in which a dual-plane modified A to T flap resulted in aesthetically satisfactory results. Two cases were a result of Mohs’ defects following cancer removal and one case was the result of neurofibroma excision.
Case 1
A 62-year-old Caucasian man presented with a 6 cm × 6 cm neurofibroma above the left eyebrow (Figure 4). The mass was mobile, had no deep tissue involvement and did not disrupt the frontal nerve. Sufficient forehead laxity and the large tumour size made the patient a good candidate for the modified dual-plane A to T flap. The lesion was excised with 3 mm around all sides down to the frontalis muscle. Advancement flaps were created as previously described. The patient reported satisfactory aesthetic and functional results (Figure 5).
Figure 4).
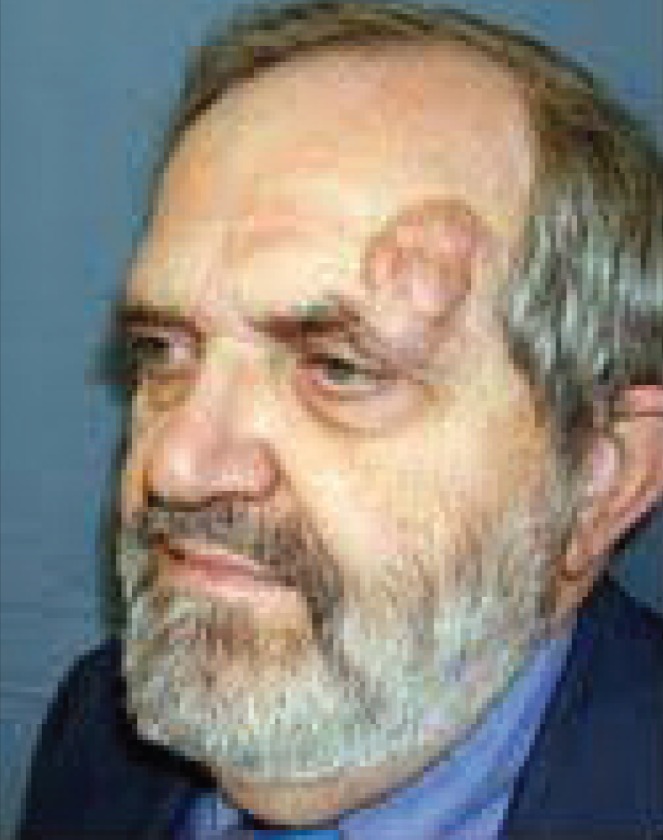
A 62-year-old man presenting with a 6 cm × 6 cm neurofibroma above the left eyebrow
Figure 5).

Result of reconstruction using a modified dual-plane A to T flap
Case 2
A 68-year-old white male cigar smoker presented with a 4.0 cm × 4.0 cm central forehead defect resulting from Mohs surgery (Figure 6). The size and location of the defect, along with the presence of adequate skin laxity, made the patient a good candidate for the modified dual-plane A to T flap. A 1 mm margin was excised around the circular defect to freshen the edges. Advancement flaps were created as shown in Figure 7. At follow-up, the patient reported satisfaction with his results (Figure 8).
Figure 6).

A 68-year-old man with a 4 cm × 4 cm central defect following Mohs surgery
Figure 7).
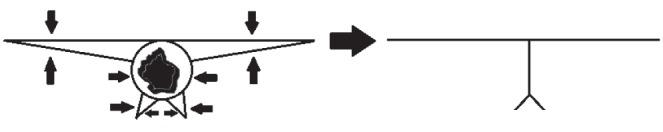
Diagram showing the initial tissue excised to create the A to T flap and the final scar lines
Figure 8).

Result of reconstruction at follow-up
Case 3
A 73-year-old white woman presented with right lateral forehead defect following Mohs surgical removal of melanoma (Figure 9). The lesion measured 8.0 cm × 5.0 cm and the frontal bone was exposed. The right frontal nerve was not intact before reconstruction. The defect was closed using the modified dual-plane A to T flap as shown in Figure 10. Z-plasty of the vertical incision was used to hide the scar within the hairline, and a 7 Fr drain was placed before closure. The resulting suture lines can be seen in Figure 11. Follow-up of the patient revealed excellent cosmetic results (Figure 12).
Figure 9).

A 73-year-old woman after Mohs surgery for melanoma removal. The defect measured 8 cm × 5 cm, and the frontal nerve was not intact before reconstruction
Figure 10).
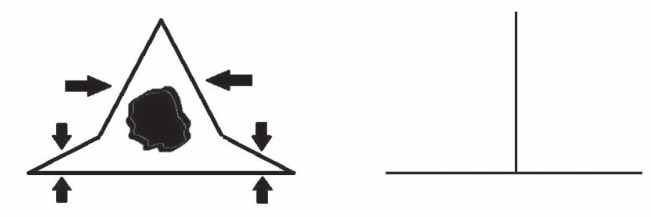
Diagram of the initial tissue excised and the resultant suture lines of the advancement flap
Figure 11).

Resulting suture lines after reconstruction
Figure 12).

Final result using a lateral based dual-plane modified A to T flap
DISCUSSION
The aesthetic significance of the forehead and low availability of loose adjacent donor tissue can present a challenge for plastic surgeons. Primary closure is an ideal solution but is often limited to defects smaller than 3 cm in size (1). When dealing with larger defects, other methods of reconstruction are considered. Skin grafts offer adequate coverage of larger defects; however, colour matching and depth irregularities are less than optimal (2,3). Local flaps provide like tissue for reconstruction, providing optimal skin texture and colour matching, but had previously been limited to smaller defects in this region and suboptimal scarring (4,5). Tissue expansion can be used to achieve aesthetically pleasing results (6) but imparts unsightly appearance in early stages, increases infection risk and requires two stages (1). Free flaps are often recommended for forehead defects exceeding 50 cm2, and may be ideal in cases of trauma, radiation, failed local flaps or when adjacent tissue is compromised (1), with many different flap choices being possible (3,7).
The periglabellar flap is a modified A to T flap previously applied to central forehead defects ranging from 2.1 cm to 5.3 cm in size (2). We have expanded this technique to defects up to 40 cm2 by using extended galea recruitment liberal deep plane dissection and have successfully applied it to lateral defects by using the brow and hair lines to conceal scarring. This technique facilitates the use of local flaps in the reconstruction of large central and lateral defects and provides excellent aesthetic results. Scarring is minimized by dual-plane dissection, which allows the skin to be approximated and everted tension free. Furthermore, the remaining scars are hidden within features already present on the forehead. Older patients with significant laxity are ideal candidates for this technique because adequate creases are already present and brow and hairline positioning can be relatively maintained. Young patients with little laxity may benefit from other methods of reconstruction because this technique may produce inadequate aesthetic results.
The dual-plane modified A to T flap applies principles put forth in the previously described periglabellar flap. These modifications make this flap quite versatile in repairing defects of the central and lateral forehead up to 40 cm2.
Acknowledgments
All patients depicted in this article have provided written permission to reproduce the images herein.
Footnotes
DISCLOSURES: The authors have no financial disclosures or conflicts of interest to declare.
REFERENCES
- 1.Beasley N, Gilbert R, Gullane PJ, Brown DH, Irish JC, Neligan PC. Scalp and forehead reconstruction using free revascularized tissue transfer. Arch Facial Plast Surg. 2004;6:16–20. doi: 10.1001/archfaci.6.1.16. [DOI] [PubMed] [Google Scholar]
- 2.Birgfeld C, Chang B. The periglabellar flap for closure of central forehead defects. J Plast Reconstr Surg. 2007;120:130–3. doi: 10.1097/01.prs.0000263534.37515.51. [DOI] [PubMed] [Google Scholar]
- 3.Kruse-Losler B, Presser D, Meyer U, Schul C, Luger T, Joos U. Reconstruction of large defects on the scalp and forehead as an interdisciplinary challenge: Experience in the management of 39 cases. Eur J Surg Oncol. 2006;32:1006–14. doi: 10.1016/j.ejso.2006.05.001. [DOI] [PubMed] [Google Scholar]
- 4.Guerrerosantos J. Frontalis musculocutaneous island flap for coverage of forehead defect. Plast Reconstr Surg. 2000;105:18–22. doi: 10.1097/00006534-200001000-00003. [DOI] [PubMed] [Google Scholar]
- 5.Rose V, Overstall S, Moloney DM, Powell BW. The H-flap: A useful flap for forehead reconstruction. Br J Plast Surg. 2001;54:705. doi: 10.1054/bjps.2001.3689. [DOI] [PubMed] [Google Scholar]
- 6.Fan J. A new technique of scarless expanded forehead flap for reconstructive surgery. Plast Reconstr Surg. 2000;106:777–85. doi: 10.1097/00006534-200009040-00004. [DOI] [PubMed] [Google Scholar]
- 7.Temple C, Ross D. Scalp and forehead reconstruction. Clin Plastic Surg. 2005;32:377–90. doi: 10.1016/j.cps.2005.02.002. [DOI] [PubMed] [Google Scholar]


