Abstract
Purpose
Bladder pain syndrome/interstitial cystitis is a poorly understood condition that can cause serious disability. We provide the first population based symptom prevalence estimate to our knowledge among United States adult females.
Materials and Methods
We developed and validated 2 case definitions to identify bladder pain syndrome/interstitial cystitis symptoms. Beginning in August 2007 we telephoned United States households, seeking adult women with bladder symptoms or a bladder pain syndrome/interstitial cystitis diagnosis. Second stage screening identified those subjects who met case definition criteria. Each completed a 60-minute interview on the severity and impact of bladder symptoms, health care seeking and demographics. Data collection ended in April 2009. Using population and nonresponse weights we calculated prevalence estimates based on definitions spanning a range of sensitivity and specificity. We used United States Census counts to estimate the number of affected women in 2006. The random sample included 146,231 households, of which 131,691 included an adult female. Of these households 32,474 reported an adult female with bladder symptoms or diagnosis, of which 12,752 completed the questionnaire.
Results
Based on the high sensitivity definition 6.53% (95% CI 6.28, 6.79) of women met symptom criteria. Based on the high specificity definition 2.70% (95% CI 2.53, 2.86) of women met the criteria. These percentages translated into 3.3 to 7.9 million United States women 18 years old or older with bladder pain syndrome/interstitial cystitis symptoms. Symptom severity and impact were comparable to those of adult women with established diagnoses. However, only 9.7% of the women reported being assigned a bladder pain syndrome/interstitial cystitis diagnosis.
Conclusions
Bladder pain syndrome/interstitial cystitis symptoms are widespread among United States women and associated with considerable disability. These results suggest bladder pain syndrome/interstitial cystitis may be underdiagnosed.
Keywords: cystitis, interstitial, cross-sectional studies, prevalence, urinary bladder
Bladder pain syndrome/interstitial cystitis is a chronic condition characterized by symptoms of pain perceived to emanate from the bladder, associated with urinary urgency/frequency in the absence of other identified etiologies for the symptoms. Some patients may deny the presence of pain but report bladder pressure or discomfort.1 Most studies show a female-to-male preponderance of 5:1 or greater. Symptoms typically fluctuate in severity but rarely resolve completely.2 Many theories exist to explain the etiology of the condition, but experimental studies have not yielded reproducible find-ings and treatments are frequently ineffective.3 Cystoscopic findings are nonspecific and no objective signs or tests exist to confirm the diagnosis. Therefore, BPS/IC is a clinical diagnosis based on patient reported symptoms.
Previous attempts to estimate BPS/IC prevalence have used medical records from existing convenience samples, questionnaires mailed to convenience samples of patients, medical records abstraction, area probability sampling in a limited geographic area and small general population mail surveys. Un-weighted estimates based on symptom questionnaires mailed to cohorts of women have ranged from 0.45% to 11.20%.4 – 6 Weighted estimates from a personal interview survey about symptoms based on an area probability sample in the Boston area ranged from 0.83% to 2.72%, depending on case definitions.7 Population based studies conducted to estimate the prevalence of BPS/IC have been limited to specific geographic regions or to subpopulations.7,8 Furthermore, the sensitivity and specificity of the case definitions used to define BPS/IC in these studies were not assessed.
MATERIALS AND METHODS
Measures and Validation
No standard case definition for BPS/IC exists for epidemiological studies. As part of the RICE study we developed a case definition for BPS/IC with known sensitivity and specificity, and compared this definition with others that have been used in BPS/IC epidemiological studies. We reviewed the literature and conducted a structured expert panel to arrive at a BPS/IC case definition.1 We developed a questionnaire to assess the presence of BPS/IC symptoms using this case definition and administered the questionnaire to 599 adult women with BPS/IC or other conditions characterized by pelvic symptoms (overactive bladder, endometriosis, vulvodynia). The sensitivity and specificity of the case definition were calculated using physician assigned diagnoses as the reference standard.9
No single epidemiological definition demonstrated high sensitivity and high specificity. Therefore, 2 RICE BPS/IC definitions were developed (see Appendix). One demonstrated high sensitivity (81%) for identifying cases diagnosed with BPS/IC, and low specificity (54%) for distinguishing cases that did not have BPS/IC from those with other bladder and pelvic pain conditions, while the other definition demonstrated the converse (48% sensitivity, 83% specificity). These values were comparable or superior to those of other epidemiological definitions used in BPS/IC prevalence studies.9
APPENDIX.
RICE BPS/IC case definitions
| High Sensitivity Definition Criteria (sensitivity 81%, specificity 54% for BPS/IC vs endometriosis, vulvodynia and overactive bladder) | High Specificity Definition Criteria (sensitivity 48%, specificity 83% for BPS/IC vs endometrio sis, vulvodynia and overactive bladder) |
|---|---|
| Pain, pressure, or discomfort in the pelvic area and Daytime urinary frequency 10+ or urgency due to pain, pressure, or discomfort, not fear of wetting. |
Pain, pressure, or discomfort in the pelvic area and Daytime urinary frequency 10+ or urgency due to pain, pressure, or discomfort, not fear of wetting and Symptoms did not resolve after treatment with antibiotics and No treatment with hormone injection therapy for endometriosis. |
Exclusion criteria: Bladder cancer, urethral diverticulum, spinal cord injury, stroke, Parkinson’s disease, multiple sclerosis, spina bifida, cyclophosphamide treatment, radiation treatment to pelvic area, tuberculosis affecting the bladder, uterine cancer, ovarian cancer, vaginal cancer, genital herpes, pregnancy.
Because there is little information on the prevalence of BPS/IC by race/ethnicity, we asked participants whether they considered themselves to be of Latino or Hispanic origin, and whether they considered themselves to be white or Caucasian, black or African-American, Native American or Alaskan Native, Asian or Asian American, Pacific Islander, mixed race or something else. Responses were recoded such that women who said they were of Latino or Hispanic origin were classified as Hispanic, and nonHispanic women were classified by their selection into white, black and other.
Sampling and Data
Collection for Population Screening
To estimate the prevalence and identify sufficient cases to describe the characteristics of people with the condition, we needed an inexpensive screening approach. Therefore, for the first stage of population screening we used the Opinion Research Corporation, which conducts twice weekly national probability telephone surveys. Two BPS/IC items were inserted into ORC surveys to screen for households with adult women 18 years old or older who had current symptoms of BPS/IC and/or had previously been diagnosed with BPS/IC. The ORC also provided demographic data about screened households and the sampling/nonresponse weights they developed to project their sample to the population of United States households. Thus, we necessarily assumed that symptoms of pain and urinary urgency and/or frequency were sufficiently severe that any adult member of the household would be aware of them.
There were 2 screening items. 1) Is there a female age 18 years or older in this household who has ever had problems with pain, pressure or discomfort in the bladder area that makes them urinate frequently or feel like they need to urinate frequently? 2) Have you or another woman age 18 years or older currently living in this household ever been told by a doctor that you or they have painful bladder syndrome or interstitial cystitis?
These items were asked of the household member interviewed by the ORC. Female respondents could identify themselves as the person with symptoms or the BPS/IC diagnosis or another woman in the household. Male respondents could only identify a woman in the household with the symptoms. Once an eligible woman in the household was identified, the household member was asked for permission to contact her about the study. If permission was given, the Survey Research Group attempted to contact the eligible woman by telephone for an interview. Nearly all interviews were completed in English while Spanish was available for the few households with a Spanish speaking respondent. Women not speaking English or Spanish were excluded from the study. After the interview respondents were mailed a $50 check. No monetary incentive was provided for completing only the screener. Population screening began in August 2007 and data collection for the baseline survey was completed in April 2009.
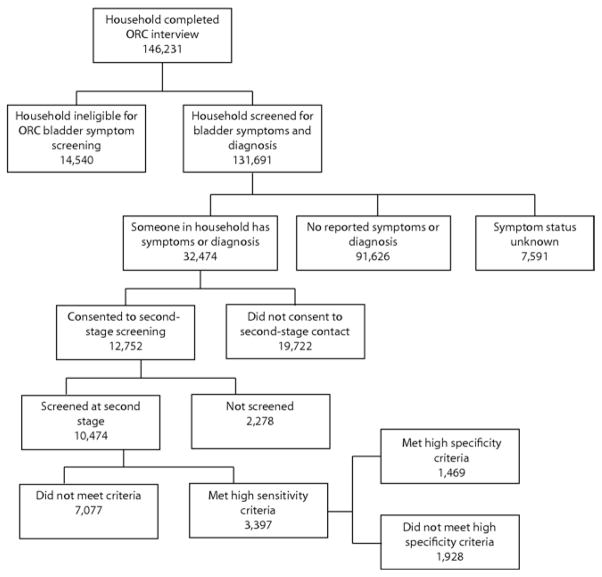
When the identified woman was reached, the interviewer conducted a 5-minute eligibility screening. The screener included an item asking the number of women in the household age 18 years or older with BPS/IC symptoms. If there was more than 1, the woman with the most recent birthday was selected, and administered a series of questions based on inclusion and exclusion criteria for BPS/IC (see Appendix). If she screened positive, she was asked to complete an in-depth 1-hour interview on current and past symptoms related to the condition, medical history, health care seeking and medical treatments, impact on daily life, physical and mental health status, insurance coverage, work status and history, and other demographic information (see figure).
Figure.
Sequence of population screening
Health related quality of life was measured using the SF-36, which assesses domains of physical functioning, role functioning, bodily pain, general health, vitality, social functioning and mental health. SF-36 scales were scored on a standard T-score metric with a mean of 50 and standard deviation of 10 in the general population of United States adult females. Scores were combined into summary physical and mental health measures.10 BPS/IC symptom severity was assessed with the ICSI and ICPI, tandem measures that assess the presence and degree of interstitial cystitis symptoms and their associated bother.11
Development of Weights
Second stage nonresponse weights were created as the inverse of predicted probabilities from a logistic regression model predicting successful screening of households asked to allow contact for secondary screening. This model used as predictors whether the potentially eligible woman had symptoms only, a self-reported diagnosis only or both; general respondent characteristics (gender, age, race/ethnicity, educational attainment, whether head of household, employment and marital status) and household characteristics (total income; home owned by household; and indicators of children younger than age 6, 6 to 11 and 12 to 17 years). Simple imputation of the rare missing predictors was performed with the median assigned for those observations that were missing values for household income. For variables indicating the presence of children, the proportion with those characteristics was assigned.
In preliminary analyses several variables that did not improve model prediction were excluded, such as the number of telephone numbers in the household, census region, household size, an indicator of multiple women in the household having BPS/IC symptoms or diagnosis, and an additional indicator for household income under $25,000 to allow nonlinear effects of low income. The final weight for each of the screened cases was calculated by multiplying the ORC weight by the second stage screening weight, which assumed a value of 1.0 to households with no females with symptoms or diagnoses and to cases without followup interviews. Those households had a final weight consisting of only the ORC component.
Calculation of Prevalence Estimates
The household prevalence estimate was calculated based on the 91,626 households with no females with symptoms or diagnoses and the 10,474 households screened in the second stage screening. The households not asked for contact permission because they did not contain any adult females with bladder symptoms or diagnoses were included in the denominator of the prevalence estimate and assigned a value of zero for the high sensitivity and high specificity definitions, which was a conservative assumption. Symptom status for the 10,474 households screened was derived from the interviews. The household prevalence rate was estimated from the weighted mean (using the weights created) across the 102,100 households. The person-level estimate was calculated by dividing the household-level estimate by 1.25 (the average number of adult females per household in households with at least 1 adult female, calculated from the March 2007 current population survey). Confidence intervals incorporated the design effects of weighting using the linearization approach as implemented by SAS® PROC SURVEYMEANS.
RESULTS
As shown in the figure 146,231 households were interviewed by the ORC and of these 131,691 (90.1%) were eligible for further screening because they reported an adult female in the household. A total of 32,474 households (24.7%) reported an adult female with BPS/IC symptoms or a BPS/IC diagnosis, and of these households 12,752 (39.3%) agreed to further screening. Of the households that agreed to screening 10,474 (82.1%) were successfully screened. Among those screened 3,397 (32.4%) contained at least 1 female who met the high sensitivity definition, of whom 1,469 (14.0%) also met the high specificity definition. A total of 7,077 (67.6%) did not meet the criteria for either definition or were positive on an exclusion criterion (see Appendix).
We estimated symptom prevalence based on the 2 previously validated symptom definitions chosen to bracket the likely range of prevalence calculated using the weighting process described (see Appendix). Based on the high sensitivity (most inclusive) definition, the estimate of prevalence of BPS/IC symptoms among United States adult females was 6.53% (CI 6.28, 6.79). Based on the high specificity definition, the prevalence was estimated to be 2.70% (CI 2.53, 2.86). We project that between 3.3 and 7.9 million women age 18 years or older have pelvic pain and other symptoms, such as urinary urgency or frequency, that are consistent with a possible diagnosis of BPS/IC after applying common exclusion criteria.
Symptom prevalence rates based on the high sensitivity and high specificity definitions varied by race/ethnicity, census region and age (see table). For example, based on the high specificity definition, the prevalence for whites (2.97%) and other race/ethnicity (2.58%) was higher than for blacks (1.91%) and Hispanics (2.03%). Prevalence in the Northeast census region (2.22%) was lower than in the North Central (2.74%), South (2.94%) or West (2.64%) regions. Prevalence increased with age from 2.21% for age 18 to 29 years to a high of 3.41% for age 50 to 59 years and then decreased to 1.70% for age 70 to 75+ years.
Table.
Estimated prevalence rates
| High Sensitivity Definition Prevalence (95% CI) | High Specificity Definition Prevalence (95% CI) | |
|---|---|---|
| Overall | 0.065 (0.063, 0.068) | 0.027 (0.025, 0.029) |
| Race: | ||
| White | 0.067 (0.065, 0.070) | 0.030 (0.028, 0.032) |
| Black | 0.058 (0.050, 0.065) | 0.019 (0.015, 0.023) |
| Hispanic | 0.065 (0.055, 0.075) | 0.020 (0.015, 0.026) |
| Other | 0.065 (0.054, 0.076) | 0.026 (0.019, 0.033) |
| Refused/no response | 0.033 (0.021, 0.046) | 0.021 (0.011, 0.032) |
| Census region: | ||
| Northeast | 0.056 (0.051, 0.062) | 0.022 (0.019, 0.026) |
| North Central | 0.063 (0.058, 0.069) | 0.027 (0.024, 0.031) |
| South | 0.072 (0.068, 0.077) | 0.029 (0.027, 0.032) |
| West | 0.063 (0.057, 0.069) | 0.026 (0.023, 0.030) |
| Age: | ||
| 18–29 | 0.057 (0.050, 0.064) | 0.022 (0.018, 0.026) |
| 30–39 | 0.067 (0.060, 0.075) | 0.026 (0.021, 0.030) |
| 40–49 | 0.075 (0.069, 0.080) | 0.032 (0.028, 0.036) |
| 50–59 | 0.074 (0.069, 0.079) | 0.034 (0.031, 0.038) |
| 60–69 | 0.068 (0.063, 0.074) | 0.028 (0.025, 0.032) |
| 70–75+ | 0.048 (0.042, 0.053) | 0.017 (0.014, 0.020) |
We found that women who met high specificity criteria had a mean SF-36 physical functioning score of 39.3 and a mean SF-36 mental health score of 44.8. Women who met the high sensitivity criteria but not the high specificity criteria had a mean physical functioning score of 42.1 and a mean mental health score of 45.3 (SE 0.3 to 0.4 for all). A score of 40 is 1 standard deviation below the age adjusted mean for adult United States females and indicates considerable loss of functioning in this population.
Women who met the high specificity criteria had a mean ICSI score of 11.5 and a mean ICPI score of 14.2, while those who met the high sensitivity criteria but not the high specificity criteria had a mean ICSI score of 10.1 and a mean ICPI score of 12.5 (SE 0.1 for all). Scores of 12 or greater on these scales are considered indicative of severe BPS/IC symptoms.4,12
Based on interviews, among the women who met the high specificity definition for current symptoms (1,469), 87.1% had consulted a physician about their symptoms and the mean number of physicians seen was 3.5, but only 40.4% had seen a urologist. While 45.8% reported having received a specific diagnosis, only 9.9% had a diagnosis of BPS/IC. Other frequently reported diagnoses were infection and pelvic prolapse.
DISCUSSION
Our prevalence estimates are comparable to previously published population prevalence estimates for BPS/IC obtained in a variety of ways using different criteria for identifying cases.4,6,7,12 They indicate that symptoms of BPS/IC are fairly widespread among adult women and are associated with considerable disability in terms of self-reported physical and mental health functioning, and the presence of bladder symptoms. The severity of symptoms reported by the women in this community based sample is comparable to that of women selected from urology practices for clinical studies of BPS/IC, which frequently require an ICSI score of 12 or higher, indicating significant experience of symptoms.
While we did not observe significant differences by race/ethnicity using the high sensitivity definition, we did observe that, using the high specificity definition, the prevalence for white females was significantly higher than for black or Hispanic females, although we have no explanation for this finding. Prevalence rates in the South census region were significantly higher than rates in the Northeast. Prevalence by age increased from age 18 to 59 years, which would be expected for a condition that does not resolve through treatment, and decreased in older age groups, possibly through death of the least healthy women in the population.
CONCLUSIONS
While most women who met the high specificity criteria consulted multiple physicians for their pelvic pain and urinary symptoms, indicating that they were bothered by these symptoms, less than half of them saw a urologist. Less than half of the women had any diagnosis for their symptoms and only a tenth had a diagnosis of BPS/IC. This may indicate that these symptoms are generally under-addressed in medical practice, and that the condition BPS/IC may be underdiagnosed and under-addressed in treatment. There are 2 key limitations of this study. Determination of the presence of BPS/IC symptoms was based on patient self-reports and not on medical examination. However, BPS/IC is a condition for which there was no medical test or established diagnostic protocol when the study was conducted. In addition, the telephone survey techniques used to screen this large population yielded low response rates. However, recent reviews of the survey methodology literature suggest that among probability samples conducted with a standardized process that adheres to typical survey methodology standards, as in this study, response rates are only weakly associated with nonresponse bias and may not be a strong proxy for survey data quality.13,14
Acknowledgments
Supported by Cooperative Agreement U01DK070234-01 from the National Institute of Diabetes and Digestive and Kidney Disorders. National Institute of Diabetes and Digestive and Kidney Disorders staff participated in study design and analysis. Research protocol approved by the Human Subjects Protection Committee (FWA00003425). The authors vouch for the accuracy and completeness of the reported findings.
Abbreviations and Acronyms
- BPS/IC
bladder pain syndrome/interstitial cystitis
- ICPI
Interstitial Cystitis Problem Index
- ICSI
Interstitial Cystitis Symptom Index
- ORC
Opinion Research Corporation
- RICE
RAND Interstitial Cystitis Epidemiology
- SF-36
Medical Outcomes Study Short Form-36
References
- 1.Bogart LM, Berry SH, Clemens JQ. Symptoms of interstitial cystitis, painful bladder syndrome and similar diseases in women: a systematic review. J Urol. 2007;177:450. doi: 10.1016/j.juro.2006.09.032. [DOI] [PubMed] [Google Scholar]
- 2.Propert KJ, Schaeffer AJ, Brensinger CM, et al. A prospective study of interstitial cystitis: results of longitudinal followup of the interstitial cystitis data base cohort. J Urol. 2000;163:1434. doi: 10.1016/s0022-5347(05)67637-9. [DOI] [PubMed] [Google Scholar]
- 3.Dimitrakov J, Kroenke K, Steers WD, et al. Pharmacologic management of painful bladder syndrome/interstitial cystitis: a systematic review. Arch Intern Med. 2007;167:1922. doi: 10.1001/archinte.167.18.1922. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Leppilahti M, Tammela TL, Huhtala H, et al. Prevalence of symptoms related to interstitial cystitis in women: a population based study in Finland. J Urol. 2002;168:139. [PubMed] [Google Scholar]
- 5.Clemens JQ, Meenan RT, O’Keeffe Rosetti MC, et al. Prevalence of interstitial cystitis symptoms in a managed care population. J Urol. 2005;174:576. doi: 10.1097/01.ju.0000165170.43617.be. [DOI] [PubMed] [Google Scholar]
- 6.Lifford KL, Curhan GC. Prevalence of painful bladder syndrome in older women. Urology. 2009;73:494. doi: 10.1016/j.urology.2008.01.053. [DOI] [PubMed] [Google Scholar]
- 7.Clemens JQ, Link CL, Eggers PW, et al. Prevalence of painful bladder symptoms and effect on quality of life in black, Hispanic and white men and women. J Urol. 2007;177:1390. doi: 10.1016/j.juro.2006.11.084. [DOI] [PubMed] [Google Scholar]
- 8.Curhan GC, Speizer FE, Hunter DJ, et al. Epidemiology of interstitial cystitis: a population based study. J Urol. 1999;161:549. [PubMed] [Google Scholar]
- 9.Berry SH, Bogart LM, Pham C, et al. Development, validation and testing of an epidemiological case definition of interstitial cystitis/painful bladder syndrome. J Urol. 2010;183:1848. doi: 10.1016/j.juro.2009.12.103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Ware JE, Jr, Kosinski M, Gandek B. SF-36 Health Survey: Manual & Interpretation Guide. Lincoln, RI: QualityMetric Inc; 2005. [Google Scholar]
- 11.O’Leary MP, Sant GR, Fowler FJ, Jr, et al. The interstitial cystitis symptom index and problem index. Urology. 1997;49:58. doi: 10.1016/s0090-4295(99)80333-1. [DOI] [PubMed] [Google Scholar]
- 12.Clemens JQ, Meenan RT, Rosetti MC, et al. Prevalence and incidence of interstitial cystitis in a managed care population. J Urol. 2005;173:98. doi: 10.1097/01.ju.0000146114.53828.82. [DOI] [PubMed] [Google Scholar]
- 13.Groves RM. Nonresponse rates and nonresponse bias in household surveys. Public Opin Q. 2006;70:646. [Google Scholar]
- 14.Groves RM, Peytcheva E. The impact of non-response rates on nonresponse bias: a meta-analysis. Public Opin Q. 2008;72:167. [Google Scholar]