Abstract
Background
Callers to 2-1-1 have greater need for and less er use of cancer control services than other Americans. Integrating cancer risk assessment and referrals to preventive services into 2-1-1 systems is both feasible and acceptable to callers.
Purpose
To determine whether callers will act on these referrals.
Methods
In a randomized trial, 2-1-1 callers (n=1,200) received standard service and those with at least one cancer risk factor or need for screening were assigned to receive verbal referrals only, verbal referrals + a tailored reminder mailed to their home, or verbal referrals + a telephone health coach/navigator. All data were collected from June 2010 to March 2012 and analyzed in March and April 2012.
Results
At 1-month follow-up, callers in the navigator condition were more likely to report having contacted a cancer control referral than those receiving tailored reminders or verbal referrals only (34% vs 24% vs 18%, respectively; n=772; p<0.0001). Compared to verbal referrals only, navigators were particularly effective in getting 2-1-1 callers to contact providers for mammograms (OR=2.10, 95% CI=1.04, 4.22), Paps (OR=2.98, 95% CI=1.18, 7.54) and smoking cessation (OR=2.07, 95% CI=1.14, 3.74).
Conclusions
Given the extensive reach of 2-1-1s and the elevated risk profile of their callers, even modest response rates could have meaningful impact on population health if proactive health referrals were implemented nationally.
Background
Recent studies have demonstrated that: (1) 2-1-1 callers have substantial needs for cancer prevention and screening services; (2) these needs can be quickly identified through brief assessments administered after standard 2-1-1 service; and (3) callers are accepting of referrals to cancer control services when offered, and feel that it is appropriate for 2-1-1 systems to proactively assess callers’ health needs.1–3 What is not yet known is whether callers act on these health referrals. The current paper reports findings from the first major follow-up study to track use of health referrals in a 2-1-1 population.
As documented3–7 in this supplement to the American Journal of Preventive Medicine and elsewhere, callers to 2-1-1 helplines generally have lower levels of income, higher rates of unemployment, are less likely to have health insurance and are disproportionately racial or ethnic minorities relative to the overall population in their communities. Because these same attributes are strongly associated with cancer disparities,4,8 several studies have examined the cancer risk profile of 2-1-1 callers. Surveys assessing cancer risk behaviors, screening, and human papillomavirus (HPV) vaccination among 2-1-1 callers in Missouri, North Carolina, Texas and Washington have shown that callers have substantially greater risks than the general populations in their respective states and in the U.S. as a whole.1,2 More than two thirds (69%) of 2-1-1 callers in these studies needed at least one of six cancer control services (smoking cessation; screening for breast, cervical or colorectal cancer; HPV vaccination for themselves or a girl in their household; smokefree home policy), 39% needed at least two of these, and 16% needed three or more.
The current study tested the effects of three types of cancer control referrals delivered to 2-1-1 callers: verbal referrals by telephone, printed tailored reminders mailed to callers’ homes, and telephone-based navigation services from a lay health coach. Verbal referrals are standard practice for 2-1-1s, while tailored print and navigation interventions have been shown to enhance a range of cancer-related outcomes in studies among low-income and racially and ethnically diverse populations.
Navigation interventions are designed to serve disadvantaged populations that are not well connected to systems of cancer screening or care.9–11 Navigators connect individuals with resources and services, help overcome barriers to using those services, make and coordinate appointments, provide or arrange transportation, accompany individuals to appointments, translate medical terminology into plain language, bridge language and cultural differences between providers and patients, provide informational and emotional support, and follow-up to track outcomes.9–14 Compared to usual care, navigator interventions can increase breast, cervical and colorectal cancer screening in underserved, minority and non–English speaking populations,15–19 and improve follow-up of abnormal mammograms.10,20 Multicomponent interventions that include navigation as a central strategy have also increased colorectal and cervical cancer screening in minority populations.21,22
Similarly, printed small media interventions that are tailored to individual characteristics have been effective in addressing a range of health behaviors, including cancer risk factors and screening, in low-income and minority populations23–25 and other potentially vulnerable groups such as food-pantry clients, older adults and cancer survivors.26–28 This type of intervention is also recommended by the Guide to Community Preventive Services based on strong evidence for effectiveness in increasing cancer screening.29,30
The objective of this study was to determine the relative effectiveness of these interventions in encouraging 2-1-1 callers to respond to cancer control referrals within 1 month of receiving them. It compares the rate of response by level of intervention intensity (i.e., study group); easily identifiable participant characteristics (e.g., gender, health insurance status); and interactions between the two. The study’s findings will increase our understanding of 2-1-1’s potential to help address cancer disparities and inform planning efforts for more-efficient delivery of health referrals through 2-1-1- systems.
Methods
Study Setting and Trial Design
Participants in the study were callers to United Way 2-1-1 Missouri. This system serves 99 of 114 counties in Missouri, nine counties in southern Illinois, and received 166,000 calls in 2011. The study was a four-arm randomized intervention trial with assessments at pre-intervention (baseline) and 1-month follow-up. This paper reports findings from the three study groups that received the referral interventions. The IRB at Washington University in St. Louis approved this study.
Study Sample and Recruitment
A random sample of 2-1-1 callers was offered the chance to participate in the project by completing a brief cancer risk assessment after receiving standard service. Those who consented, completed the assessment, and had at least one cancer control need were invited to participate in a longitudinal study that included completing a baseline assessment while still on the phone and telephone follow-up interviews 1 and 4 months later. On 4 days per week, callers enrolled in the study were randomly assigned, by call, to one of three intervention groups: verbal referral only, verbal referral + tailoring, or verbal referral + health coach/navigation. On a fifth day, all callers were enrolled into a control group; this was necessary because these participants were interviewed using a different script that did not include providing referrals.
Assignment of days was random, and the same information specialists conducted interviews on intervention and control days. Because callers recruited on control days did not receive referrals, they were not asked at 1-month follow-up about calling referrals. Therefore, this paper reports findings for participants in the three intervention groups only.
All participants were recruited during the first 90 weeks of the study, from June, 2010 to March, 2012. During this time period, a subgroup of 2-1-1 information specialists that were trained to administer the research protocol received 13,280 calls. Of these, 7996 callers (60%) were eligible for the risk assessment (aged ≥18 years, living in Missouri, English-speaking, calling with a service request for themselves, willing to provide address and phone number, not currently in extreme crisis). Nearly all of these (95%; n=7620) were offered the opportunity to take the risk assessment; most accepted (76%; n=5766), two thirds provided informed consent (67%; n=3837), and nearly all of these (97%; n=3719) completed the risk assessment. Of those completing the risk assessment, 82% (n=3043) had at least one cancer risk factor or cancer control need.
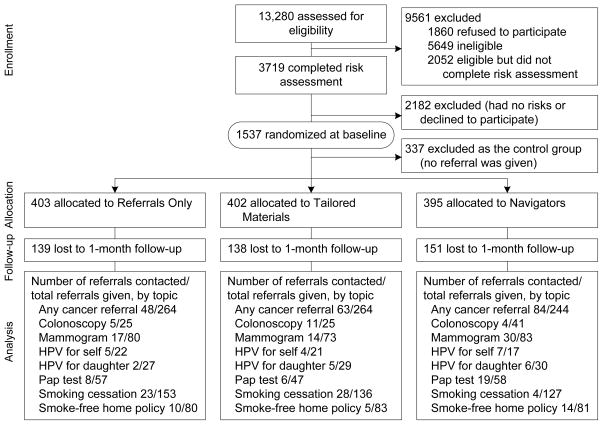
After removing those recruited on a control day (n=491), the remaining 2552 participants were offered cancer control referrals for their specific needs and most accepted (71%; n=1806), making them eligible for the follow-up study. Of these, 75% (n=1347) accepted the offer to participate in the follow-up study and nearly all provided informed consent (91%; n=1227) and completed the baseline assessment (98%; n=1200). They constitute the final baseline sample for this study (Figure 1). Sample size for the study was determined based on reported prevalence of cancer risks and screening needs among 2-1-1 callers and effect sizes of similar interventions in past research.
Figure 1.
Flow diagram
Random Assignment
Randomization was based on nonrecurring lists of participant ID numbers that were equally distributed across study groups in blocks of 42 and administered by the project’s data manager 1 working day after baseline interviews were conducted. This yielded samples equivalent in size: referral only (n=403; 34% of baseline sample); referral + tailoring (n=402; 33%); and referral + navigation (n=395; 33%).
Interventions
The study tested the effects of verbal referrals with and without tailored print reminders or a health coach/navigator.
Verbal referral
Callers’ responses to the cancer risk assessment were entered into a database where a computer algorithm identified and prioritized any cancer control needs and instantly fed this information to the 2-1-1 information specialist who then delivered a scripted referral to the caller. Each referral consisted of three parts: (1) risk assessment feedback (e.g., You said you’ve never had a mammogram); (2) recommended action and importance (e.g., Once you turn 40, getting a mammogram every 1 to 2 years is the best way to fight breast cancer. Mammograms can find breast cancer when it’s easier to treat and cure.); and (3) offer of referral to a free or low-cost service (e.g., There’s a good chance you can get a free mammogram through a program called Show Me Healthy Women. Would you like the phone number for that program?).
For each referral that was accepted, the information specialist input the caller’s ZIP code into 2-1-1’s resource database to identify the closest service provider to the caller’s residence. The information specialist then verbally shared the provider’s phone number and/or address and information about its hours of operation and documentation that may be required to obtain services. Limiting cancer control referrals to three per caller followed standard 2-1-1 procedure. If a caller had four or more needs, the prioritization algorithm was: colonoscopy first, followed by mammography, HPV vaccine for self or girl in home, Pap, smoking cessation, and smokefree home policy. This algorithm was driven by the goal of maximizing statistical power for need-specific analyses, and thus was based on the expected proportion of the sample (from lowest to highest) that would need the referral and not on public health importance or strength of evidence for the recommended cancer control measure.
Tailored reminder
Within 1 working day of receiving the verbal referral, participants randomly assigned to this group were also mailed a printed tailored referral reminder. It was a four-page full-color booklet mailed in a full-color 8.5″ × 11″ envelope, both branded with the project logo. Its contents, photos and referral information were tailored based on each caller’s age, gender, race/ethnicity, presence of children in the home, reason for calling 2-1-1 and responses to the cancer risk assessment.
The tailored materials included: (1) a short personal story from an age, race, and gender-matched peer who had the same problem that led the participant to call 2-1-1 and had used the cancer control referral to which the participant has been referred (i.e., modeling31); (2) action details providing a clear and simple summary of information the caller would need to access the cancer control referral(s) they received; and (3) motivation and preparation information describing why the cancer control service was important and suggesting questions to ask when calling the referral. All content adhered to health literacy and health communication best practices, and was written at a Flesch-Kincaid Grade Level of 4. The tailored personal story applied to each caller’s highest-priority cancer control need based on the prioritization algorithm described above; the other tailored information was provided for up to three needs.
Navigator/health coach
Navigators (called “coaches” to participants) explained each needed cancer control service and why it was important, answered callers’ questions, learned what might keep them from acting on the referral, and addressed these barriers through a variety of strategies including arranging transportation, making appointments and providing reminders to the caller. Participants assigned to this condition received their first call from a navigator within 1 working day of completing the baseline assessment and receiving the verbal referral. The initial call introduced the navigator, explained the navigation relationship and sought to establish rapport. Navigators were allowed to call up to 25 times to reach a participant, and on average it took 6.2 attempts.
Once a participant was reached, a flyer was immediately mailed to him or her containing the name, picture and contact information for their navigator. The navigator re-contacted the participant soon after to ensure receipt of the flyer and follow up on any issues resulting from their initial conversation. These telephone interactions continued for up to 4 months with the number and frequency of calls determined by participants’ needs, interest, and willingness. Either person (i.e., navigator or participant) could initiate a call.
Navigators were two African-American women similar in age to the average 2-1-1 caller. Both had outstanding interpersonal and communication skills and experience working directly with diverse populations on health-related outcomes. They received training in evidence-based cancer control, cultural competency, identifying barriers, problem-solving techniques, basic counseling concepts and approaches, and resource mapping and documentation; they completed many rehearsal and role-play exercises.
During the first 2 months of the study, navigators received individualized supervision and feedback every week from two licensed clinicians (psychologist and social worker). Feedback included critiques of audio-recorded navigation sessions, discussion of challenging cases, review of participant flow, identification of new resources and solving problems related to process improvement. After 2 months, navigators received clinical oversight from supervisors.
Follow-up
At 1 and 4 months post-enrollment, research staff called all participants to complete follow-up surveys. Interviewers were not 2-1-1 staff (i.e., not involved in making verbal referrals) and were blind to study condition. Mailed postcard reminders were sent to all participants 1 week prior to their follow-up survey eligibility date, and follow-up calls were placed at times participants indicated at baseline would be most convenient for them. A toll-free project hotline was established for participants to inform the project team if their phone number had changed.
Participants who could not be reached (e.g., due to non-working phone numbers) were sent a letter encouraging them to call the toll-free number. Participants who completed the follow-up received a thank you letter and $10 gift card to WalMart or a local grocery store. At 1-month follow-up, 64% of participants (n=772) were reached by telephone and completed an interview.
Measures
The outcomes of primary interest in the study were participants recalling and contacting the cancer control referral(s) they received. Both were measured in phone interviews conducted by the research team at 1-month follow-up. At baseline, 2-1-1 information specialists gathered caller characteristics including demographics, reasons for calling 2-1-1 and cancer control needs; these were used to describe the sample and as potential moderators in outcome analyses.
Recall
Participants were first asked if they remembered receiving health referrals during their 2-1-1 call (yes/no/not sure). Those indicating no or not sure were prompted: The referrals would have been about things you can do to help improve your health, prevent disease, or find disease early. Do you remember getting any referrals like this?” (yes/no). In analyses, participants that responded yes to prompted or unprompted recall are treated as remembering the cancer control referrals.
Contacting referrals
Participants who remembered receiving a referral were asked if they had contacted any health referral(s) they received (yes/no/don’t remember). Those responding yes were then asked questions about the specific referrals they received: You got a referral to [cancer control referral] for [cancer control need]. Did you try to contact that referral? (yes/no/don’t remember).
Demographics
Age, gender, race/ethnicity (white/black or African-American/Asian/Native Hawaiian or other Pacific Islander/American Indian or Alaska Native/Hispanic or Latino/other); years of education (≤kindergarten/Grades 1–8/9–11/12 or General Educational Development test/1–3 years of college/≥4 years of college); annual household income (<$5,000/$5,000–$9,999/$10,000–$14,999/$15,000–$19,999/$20,000–$24,999/$25,000–$34,999/$35,000–$49,999/≥$50,000); health insurance status (private/Medicare/Medicaid/State Children’s Health Insurance Program (SCHIP) or Children’s Health Insurance Program (CHIP)/military health care/other government program/uninsured) and children aged ≤18 years living in the home (yes/no) were gathered from all participants. For race/ethnicity and health insurance, participants could indicate more than one answer.
Reason for calling 2-1-1
For every call received, 2-1-1 records service requests, or “reasons for calling”. Because there are well over 100 service request types, these were coded into seven mutually exclusive categories (bills/employment/home and family/health/housing/other). Up to three service requests were coded for each participant.
Cancer risk assessment
Items from the 2008 Behavioral Risk Factor Surveillance System were used to assess 2-1-1 callers’ needs for mammography (two items); Pap (two items); colonoscopy (two items); HPV vaccination for self (one item); and daughter (one item); smoking (two items); and smokefree home rules (one item). These six topics were chosen because they are both recommended in cancer prevention and control guidelines and are available free or at low cost to disadvantaged populations through programs available in most states. Cancer control referrals were offered to women aged ≥40 years who had no mammogram in the past year; women aged ≥18 years who had no Pap with the last 2 years; those aged ≥50 years who had no colonoscopy in the past 10 years; women aged 18–26 years and those with a girl aged 9–17 years living in their home who had not received the HPV vaccination; current smokers; and those without a total ban on smoking in their household. (Recommendations for Paps changed during the study period. In the first 4 months of recruitment, women aged 18–26 years were offered referrals if they had not a Pap in the past year).
Accepted cancer control referral
When information specialists offered each needed cancer control referral, they recorded whether participants accepted the referral (yes/no).
Analyses
A conditional chi-square test was used to examine the association between study group type and calling the referral services, stratified by demographic variables and health insurance status. Then simple logistic regression was used to estimate ORs and 95% CIs for the effects of study group on calling the referral services. Next, a multiple logistic regression was used to estimate the OR for study group, controlling for the potential confounding effects of demographic variables and health insurance status. Last, a chi-square test and simple logistic regression were used to examine the association between study group and calling each specific health referral.
To test whether study group effects were modified by demographic and health insurance variables, a separate test was conducted on a logistic regression model that included interaction terms between study group and these variables. A significant test result for any interaction terms would indicate a moderation effect of these variables on the relationship between study group and calling the referral service. In all analyses, participants who did not remember receiving health referral (and therefore were not asked about contacting the referrals) were counted as not contacting any referral (i.e., intent to treat).
Results
Participants
Baseline data indicate that most participants were women (86%); either African-American (60%) or white (29%); and reported annual household incomes < $15,000 (68%; Figure 1). About half (53%) had minor children (aged <18 years) living in the home. Participants’ average age was 42.8 years, one in four (27%) reported having less than a high school education, and nearly half (45%) were currently out of work. Many participants (41%) had no health insurance, and half (49%) rated their health as “fair” or “poor.” There were no differences among the three study groups on any of these participant characteristics.
Reasons for Calling 2-1-1
Immediately prior to their enrollment in the study, most participants had called 2-1-1 seeking help with bills (77%) and/or home and family needs (42%). Calls for assistance with employment (9%), health (8%) and housing (6%) made up a smaller proportion of calls (Table 1). Reasons for calling did not differ by study group.
Table 1.
Participant characteristics
| % | |
|---|---|
| Mean age, years (SD) | 43.1 (12.9) |
| Gender (n=1200) | |
| Female | 85.7 |
| Race/ethnicity (n=1,190) | |
| African-American | 59.9 |
| White | 28.8 |
| More than one race | 7.5 |
| Hispanic or Latino | 2.6 |
| Other | 1.2 |
| Income, $ (n=1158) | |
| <15,000 | 68.0 |
| 15,000–24,999 | 21.8 |
| 25,000–34,999 | 6.3 |
| ≥35,000 | 4.0 |
| Education (n=1200) | |
| Less than high school | 27.1 |
| High school or GED | 33.0 |
| Some college | 33.4 |
| ≥4 years of college | 6.5 |
| Marital status (n=1118) | |
| Never married | 42.0 |
| Divorced/separated | 34.4 |
| Married or unmarried couple | 23.6 |
| Employment (n=1058) | |
| Employed | 24.4 |
| Out of work <1 year | 25.1 |
| Out of work ≥1 year | 19.6 |
| Unable to work | 30.9 |
| Service request from 2-1-1 (n) | |
| Bills (926) | 77.2 |
| Home and family (501) | 41.8 |
| Employment (110) | 9.2 |
| Health (96) | 8.0 |
| Housing (71) | 5.9 |
| Other (124) | 10.3 |
| Child aged <18 years living in home (n=639) | 53.3 |
| Health insurance (n=1157) | |
| None | 41.1 |
| Public (Medicare or Medicaid) | 35.7 |
| Private | 9.2 |
| More than one type | 14.0 |
| Self-rated general health (n=1197) | |
| Poor | 17.5 |
| Fair | 31.8 |
| Good | 29.1 |
| Very good | 15.5 |
| Excellent | 6.1 |
| Needed cancer control (n) | |
| Colonoscopy (422) | 51.9 |
| Mammogram (597) | 69.7 |
| HPV for self (135) | 78.5 |
| HPV for girl aged <18 years (287) | 63.8 |
| Pap (1028) | 27.5 |
| Smoking cessation (1200) | 62.4 |
| Smokefree home policy (1200) | 55.8 |
Note: “Don’t know” and “Refused” responses excluded from analysis
GED, General Educational Development test; HPV, human papilloma virus
Cancer Risks and Needs
At baseline, many participants reported smoking cigarettes every day (41%) or some days (22%). Among those eligible for cancer screening based on age and gender, 70% had not had a mammogram in the past year, 52% had not had a colonoscopy in the last 10 years, and 28% had not had a Pap in the past 2 years. Half (56%) had no rule banning smoking in their home; most age-eligible women had not received the HPV vaccination (79%); nor had age-eligible girls living in their home (64%). These cancer risks and needs (Table 1) did not vary significantly by study group.
Recall
At 1-month follow-up, participants in the navigator condition were most likely to remember receiving a cancer control referral (84%), followed by those in the tailored reminder (75%) and verbal referral (65%) groups (n=772; p<0.0001). Compared to verbal referrals, tailored reminders increased the odds of recall by 65% (OR=1.65, 95% CI=1.12, 2.39) and having a navigator more than doubled the odds of recall (OR=2.73, 95% CI=1.79, 4.16). The navigator intervention also increased the odds of recall relative to tailored reminders (OR=1.67, 95% CI=1.07, 2.59).
Contacted Any Referral
Also at 1-month follow-up, one third (34%) of 2-1-1 callers who received the navigator intervention reported contacting one of the cancer control referrals they received, compared to 24% of those receiving tailored reminders and 18% of those receiving verbal referrals only (p< 0.0001). Participants in the navigator condition were more than twice as likely to report contacting a referral than those in the verbal referral condition and 67% more likely compared to the tailored reminder group. Tailored reminders were not more effective than verbal referrals (Table 2).
Table 2.
Contacting any cancer control referral at 1-month follow, by study group, demographic variables, and health insurance status
| Verbal referral (%) | Tailored reminder (%) | Navigator (%) | χ2 p-value (%) | Tailored reminder vs verbal referral OR (95% CI) | Navigator vs verbal referral OR (95% CI) | Navigator vs tailored reminder OR (95% CI) | |
|---|---|---|---|---|---|---|---|
| Contacted any referral (n=772) | 18.2 | 23.9 | 34.4 | 0.0001 | 1.41 (0.93,2.15) | 2.36 (1.57,3.56) | 1.67 (1.14,2.47) |
| Gender | |||||||
| Female (n=669) | 18.7 | 24.7 | 35.9 | 0.0002 | 1.42 (0.91,2.23) | 2.43 (1.57,3.75) | 1.71 (1.13,2.58) |
| Male (n=103) | 14.7 | 18.9 | 25.0 | 0.5696 | 1.35 (0.39,4.75) | 1.93 (0.56,6.69) | 1.43 (0.45,4.50) |
| Race | |||||||
| African-American (n=466) | 20.1 | 27.0 | 31.7 | 0.0691 | 1.47 (0.88,2.46) | 1.84 (1.09,3.10) | 1.25 (0.76,2.06) |
| White (n=220) | 15.7 | 15.8 | 29.7 | 0.0524 | 1.01 (0.41,2.45) | 2.27 (1.01,5.12) | 2.26 (1.02,4.99) |
| Income, $ | |||||||
| <10,000 (n=360) | 17.1 | 33.0 | 33.6 | 0.0041 | 2.40 (1.32,4.38) | 2.46 (1.35,4.48) | 1.03 (0.59,1.78) |
| ≥10,000 (n=386) | 18.9 | 17.6 | 36.1 | 0.0006 | 0.92 (0.49,1.72) | 2.42 (1.35,4.36) | 2.64 (1.50,4.66) |
| Employment | |||||||
| Not employed (n=636) | 19.4 | 23.5 | 36.0 | 0.0003 | 1.27 (0.80,2.01) | 2.33 (1.50,3.62) | 1.83 (1.20,2.80) |
| Employed (n=136) | 12.5 | 25.5 | 26.8 | 0.1769 | 2.40 (0.82,7.05) | 2.57 (0.86,7.71) | 1.07 (0.41,2.77) |
| Education | |||||||
| ≤High school (n=465) | 19.9 | 22.7 | 34.2 | 0.0091 | 1.18 (0.69,2.03) | 2.10 (1.26,3.49) | 1.78 (1.07,2.96) |
| >High school (n=307) | 15.3 | 25.4 | 37.7 | 0.0078 | 1.89 (0.94,3.78) | 2.95 (1.47,5.89) | 1.56 (0.86,2.83) |
| Health insurance | |||||||
| Yes (n=482) | 16.2 | 19.4 | 29.7 | 0.0093 | 1.25 (0.71,2.20) | 2.19 (1.28,3.74) | 1.76 (1.04,2.96) |
| No (n=289) | 21.7 | 31.1 | 42.7 | 0.0085 | 1.63 (0.86,3.09) | 2.70 (1.42,5.12) | 1.65 (0.91,2.99) |
In logistic regression analyses controlling for demographic variables and health insurance status, the navigator intervention was still much more effective than verbal referrals (OR=2.51, 95% CI=1.63, 3.86), but the difference between tailored reminders and verbal referrals slipped to marginal significance (OR=1.54, 95% CI=0.99, 2.39). Of the control variables, being uninsured, African-American, or the member of another other nonwhite racial/ethnic group increased the odds that a participant contacted a cancer control referral (Table 3). However, there were no interaction effects between study group and any demographic or health insurance variable on participants’ likelihood of contacting referrals (data not shown).
Table 3.
Logistic regression for contacting any cancer control referral at 1-month follow-up by study group
| OR (95% CI)a | |
|---|---|
| Study group | |
| Navigator | 2.51 (1.63,3.86) |
| Tailored reminder | 1.54 (0.99,2.39) |
| Verbal referral | 1.0 |
| Uninsured | 1.88 (1.32,2.68) |
| Unemployed | 1.39 (0.86,2.25) |
| Female | 1.54 (0.90,2.64) |
| Race/ethnicity | |
| African-American | 1.52 (1.01,2.29) |
| Other | 2.27 (1.23,4.17) |
| White | 1.0 |
| Education < High school | 0.99 (0.70,1.41) |
| Income < $10,000 | 1.14 (0.80,1.62) |
Note: Regression analysis was controlled for demographics and health insurance.
ORs (95% CIs) are adjusted by the listed demographic variables.
In descriptive subgroup analyses, the likelihood of contacting cancer control referrals was highest among those with no health insurance who received the navigator intervention (43%) and lowest among those who were employed and received verbal referrals only (13%). Stratified analyses showed that the navigation intervention was consistently twice as effective as verbal referrals across demographic and health insurance strata. Navigators were more effective than tailored reminders in some strata, but not others: for example, whites (but not blacks); those with higher relative incomes (but not lower income); and those with insurance (but not the uninsured). Tailored reminders were more effective than verbal referrals only among the lowest-income strata (Table 2).
Contacted Specific Cancer Control Referrals
The navigator intervention was more effective than verbal referrals in getting participants to contact referrals for mammograms, Paps, and smoking cessation (Table 4). Navigators were more effective than tailored reminders in getting participants to contact referrals for mammograms, Paps, and smokefree home policies, but less effective for colonoscopy. Tailored referrals were no more effective than verbal referral for any individual cancer control referral, and there were no study group differences for HPV vaccination for young women or girls.
Table 4.
Contacting specific cancer control referrals at 1-month follow-up, by study group
| Verbal referrals (%) | Tailored reminders (%) | Navigators (%) | χ2-value (%) | Tailored reminder vs Verbal referral | Navigator vs Verbal referral OR (95% CI) | Navigator vs Tailored reminder OR (95% CI) | |
|---|---|---|---|---|---|---|---|
|
|
|||||||
| Called given referrals, by type | |||||||
| Colorectal (n=91) | 20.0 | 44.0 | 9.8 | 0.0048 | 3.14 (0.89,11.06) | 0.43 (0.10,1.79) | 0.14 (0.04,0.51) |
| Mammogram (n=236) | 21.3 | 19.2 | 36.1 | 0.0278 | 0.88 (0.40,1.94) | 2.10 (1.04,4.22) | 2.39 (1.14,4.97) |
| HPV for self (n=60) | 22.7 | 19.1 | 41.2 | 0.2687 | 0.80 (0.18,3.50) | 2.38 (0.59,9.54) | 2.98 (0.69,12.76) |
| HPV for daughter (n=86) | 7.4 | 17.2 | 20.0 | 0.3848 | 2.60 (0.46,14.73) | 3.13 (0.57,17.3) | 1.20 (0.32,4.47) |
| Pap (n=162) | 14.0 | 12.8 | 32.8 | 0.0138 | 0.90 (0.29,2.79) | 2.98 (1.18,7.54) | 3.33 (1.20,9.21) |
| Smoking cessation (n=416) | 15.0 | 20.6 | 26.8 | 0.0527 | 1.47 (0.80,2.69) | 2.07 (1.14,3.74) | 1.41 (0.80,2.50) |
| Smokefree home (n=244) | 12.5 | 6.0 | 17.3 | 0.0818 | 0.45 (0.15,1.38) | 1.46 (0.61,3.52) | 3.26 (1.12,9.52) |
Note: Bold indicates significance.
HPV, human papillomavirus
Discussion
This study provides the first estimates of the extent to which 2-1-1 callers will respond to proactive cancer control referrals when integrated into standard 2-1-1 service. With verbal referrals alone, 18% of callers reported contacting a cancer control referral they received. Callers who also received tailored reminders mailed to their homes were 1.5 times more likely to contact a referral (24%), and those who received access to a telephone navigator/health coach were 2.5 times more likely to contact a referral (34%).
Given the very high prevalence of cancer control needs among 2-1-1 callers, even these relatively modest response levels could have a meaningful impact on population health. For example, a study of 2-1-1 callers in Missouri, North Carolina, Texas, and Washington found a combined 29% smoking prevalence.2 Given that 2-1-1 systems in the U.S. receive over 16 million calls per year, helping connect 15%–27% of 2-1-1 smokers to their state tobacco quitline, as achieved in this study, would likely yield many thousands of new and successful quit attempts.
When judging the level of response to these cancer control referrals, it is important to remember the context in which they were delivered. The overwhelming majority of these callers had sought out 2-1-1 not for health information or services, but because they needed help paying their bills, feeding their families, or finding housing or jobs. As others have observed, people living in poverty often have such overwhelming needs in other areas of life that disease prevention is perceived as irrelevant, or at best, secondary to these priorities.28,29 Studies support this, showing that in disadvantaged populations, meeting basic human needs is perceived as more important than obtaining health and preventive services.30–33 Seen in this light, strategies that succeed in getting one in five to one in three callers with acute unmet basic needs to contact cancer control service providers seem promising and worth applying more broadly.
The navigator intervention tested in this study was particularly effective. Navigators had at least some contact with nearly all participants (88% successfully reached) assigned to this group, and on average had about three interactions (2.85) per participant reached. 2-1-1 callers assigned to this condition were more likely than other callers to remember receiving the cancer control referrals and to report having contacted the referrals they received. These findings add to the growing body of evidence for the effectiveness of navigation interventions, and break new ground in three ways.
First, the geographic coverage of navigation services provided in the study is unique. Navigators served a statewide population of 2-1-1 callers, not one constrained to a particular health clinic or system. Second, the scope of navigation services in the study was broader than usual, including not just clinical services such as screening breast, cervical and colorectal cancers, but also lifestyle behaviors (smoking), vaccination (HPV) and home environment (smokefree policies). Third, the study used a boundary-crossing approach. Navigation services were not imbedded in a healthcare system, but rather in a social service system reaching large numbers of economically disadvantaged and uninsured Americans, many of whom might not reliably be reached by interventions that are only available through healthcare providers.
The navigation intervention was especially effective in getting 2-1-1 callers to contact referrals for mammograms, Paps, and help quitting smoking. Of women assigned to the navigator condition, 36% of those who needed a mammogram reported contacting the referral they received for this service, 33% of those who needed a Pap contacted the recommended provider, and 27% of smokers contacted the tobacco quitline – all of which were significantly higher response levels than the verbal referral condition. The patterns for HPV vaccination for young women and girls are similar, although the smaller sample sizes for these outcomes likely preclude significance.
However, in contrast to these findings and other recent studies,13 navigation was notably less successful in getting callers to contact referrals for colorectal cancer screening. There are at least two possible explanations for this. First, compared to the other cancer control services of interest in the study, there were notably fewer providers of free or low-cost colonoscopies in Missouri to which 2-1-1 callers could be referred. Second, it seems possible that discussing the procedural details of getting a colonoscopy might dissuade some callers from seeking this service. This level of information was not conveyed in the verbal referrals or tailored reminders, but would be discussed by a navigator. If future research found support for either or both of these explanations, navigation interventions could be adapted accordingly. In this study, it may be possible to use content analysis of navigator–participant interactions to further explore this question.
The main limitation of the study is that the current findings stop short of behavior change. Contacting a referral is not the same as obtaining a needed screening, getting vaccinated or quitting smoking. In the case of mammography, for example, a woman calling the referral service might be deemed ineligible for free or reduced-cost screening, and even if eligible would still need to make and keep an appointment, and perhaps find transportation and/or child care on the day of her scheduled visit. Each point in this process represents another possible threat to successful completion of screening. These behavioral outcomes will be measured at the final follow-up to this study and reported as soon as they are available.
A second limitation is that the study did not include an economic analysis. Navigators were more effective than tailored reminders or verbal referrals delivered by existing 2-1-1 staff, but likely cost more as well. For example, tailored reminders can have substantial up-front development costs, but minimal costs for ongoing implementation. In contrast, navigator costs generally do not diminish over time. The two interventions were equally time-consuming to develop, but the tailored reminders were less staff-intensive to deliver. If navigators are found to enhance behavioral outcomes, it will be critically important to understand how the relative costs and benefits of delivering this type of intervention stack up against less-intensive approaches.
Finally, the response level at 1-month follow-up (64%) was low. The life circumstances of this study population pose many challenges for longitudinal human subjects research. Although the retention rate was similar to that found in research among other 2-1-1 samples,1 future studies should explore innovative ways to maintain ongoing contact with 2-1-1 callers. Although the initial sample of 2-1-1 callers was randomly selected, only those with current cancer risks or screening needs were eligible for participation in the study. Generalization of findings to other 2-1-1 populations should acknowledge this.
Given the findings from this study, the missing link in the causal chain of 2-1-1–based cancer control interventions now shifts one step further downstream. Previous studies showed that 2-1-1 callers have major cancer control needs, but it is feasible for existing staff to assess these needs and make appropriate referrals.1–3 These studies also found that most callers accept cancer control referrals when offered, and believe it is appropriate for 2-1-1 to proactively make such referrals. The current study adds the important next step, showing that about 1 in 5 callers will contact a cancer control referral when receiving a verbal referral from 2-1-1, and as many as one in three will do so when these referrals are supplemented with telephone-based navigation.
The final link is to determine whether receiving and contacting cancer control referrals actually increases cancer prevention and early detection behaviors. If it does, integrating these interventions into 2-1-1 systems across the country should become a priority for dissemination and implementation. Given the expansive reach of 2-1-1 systems and widespread use by disadvantaged populations, this approach could greatly contribute to population-wide efforts to eliminate cancer disparities.
Acknowledgments
This study was supported by funding from the National Cancer Institute (P50-CA095815).
Publication of this article was supported by funding from the National Cancer Institute (NCI) and the Office of Behavioral and Social Science Research (OBSSR) of the NIH.
Footnotes
No financial disclosures were reported by the authors of this paper.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Eddens KS, Kreuter MW, Archer K. Proactive screening for health needs in United Way’s 2-1-1 Information and Referral Service. J Soc Serv Res. 2011;37(2):113–123. doi: 10.1080/01488376.2011.547445. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Purnell JQ, Kreuter MW, Eddens KS, et al. Cancer control needs of 2-1-1 callers in Missouri, North Carolina, Texas and Washington. J Health Care Poor Underserved. 2012;23(2):752–67. doi: 10.1353/hpu.2012.0061. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Savas LS, Fernández ME, Jobe D, Carmack CC. Human papillomavirus vaccination: a 2-1-1 helpline study of minority-parent decision-making. Am J Prev Med. 2012;43(6S):XXX–XXX. doi: 10.1016/j.amepre.2012.09.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Alcaraz KI, Arnold LD, Eddens KS, et al. Exploring 2-1-1 service requests as potential markers for cancer control needs. Am J Prev Med. 2012;43(6S):XXX–XXX. doi: 10.1016/j.amepre.2012.08.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Cortinois AA, Glazier RH, Caidi N, Andrews G, Helbert-Copley M, Jadad AR. Toronto’s 2-1-1 healthcare services for immigrant populatins. Am J Prev Med. 2012;43(6S):XXX–XXX. doi: 10.1016/j.amepre.2012.08.010. [DOI] [PubMed] [Google Scholar]
- 6.Rodgers JT, Purnell JQ. Healthcare navigation service in 2-1-1 San Diego: Guiding individuals to the care they need. Am J Prev Med. 2012;43(6S):XXX–XXX. doi: 10.1016/j.amepre.2012.08.012. [DOI] [PubMed] [Google Scholar]
- 7.Roux AM, Herrera P, Wold CM, Dunkle MC, Glascoe FP, Shattuck PT. Developmental and autism screening through 2-1-1: reaching underserved families. Am J Prev Med. 2012;43(6S):XXX–XXX. doi: 10.1016/j.amepre.2012.08.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Jemal A, Siegel R, Ward E, Murray T, Xu J, Thun M. Cancer statistics, 2007. CA Cancer J Clin. 2007;57(1):43–66. doi: 10.3322/canjclin.57.1.43. [DOI] [PubMed] [Google Scholar]
- 9.Dohan D, Schrag D. Using navigators to improve care of underserved patients: Current practices and approaches. Cancer. 2005 Aug 15;104(4):848–855. doi: 10.1002/cncr.21214. [DOI] [PubMed] [Google Scholar]
- 10.Battaglia T, Roloff K, Posner M, Freund K. Improving follow-up to abnormal breast cancer screening in an urban population: A patient navigation intervention. Cancer. 2007 Jan 15;109(2 Suppl):359–367. doi: 10.1002/cncr.22354. [DOI] [PubMed] [Google Scholar]
- 11.Freeman H. Patient navigation: A community centered approach to reducing cancer mortality. J Cancer EducSpring. 2006;21(1 Suppl):S11–S14. doi: 10.1207/s15430154jce2101s_4. [DOI] [PubMed] [Google Scholar]
- 12.Schwaderer K, Itano J. Bridging the healthcare divide with patient navigation: Development of a research program to address disparities. Clin J Oncol Nurs. 2007 Oct;11(5):633–639. doi: 10.1188/07.CJON.633-639. [DOI] [PubMed] [Google Scholar]
- 13.Freeman H, Chu K. Determinants of cancer disparities: barriers to cancer screening, diagnosis, and treatment. Surg Oncol Clin N Am. 2005 Oct;14(4):655–669. v. doi: 10.1016/j.soc.2005.06.002. [DOI] [PubMed] [Google Scholar]
- 14.Steinberg M, Fremont A, Khan D, et al. Lay patient navigator program implementation for equal access to cancer care and clinical trials: Essential steps and initial challenges. Cancer. 2006;107(11):2669–2677. doi: 10.1002/cncr.22319. [DOI] [PubMed] [Google Scholar]
- 15.Dietrich A, Tobin J, Cassells A, et al. Telephone care management to improve cancer screening among low-income women: A randomized, controlled trial. Ann Intern Med. 2006;144(8):563–571. doi: 10.7326/0003-4819-144-8-200604180-00006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Fang C, Ma G, Tan Y, Chi N. A multifaceted intervention to increase cervical cancer screening among underserved Korean women. Cancer Epidemiol Biomarkers Prev. 2007;16(6):1298–1302. doi: 10.1158/1055-9965.EPI-07-0091. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Percac-Lima S, Grant RW, Green AR, et al. A culturally tailored navigator program for colorectal cancer screening in a community health center: A randomized, controlled trial. J Gen Intern Med. 2009;24(2):211–217. doi: 10.1007/s11606-008-0864-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Phillips CE, Rothstein JD, Beaver K, Sherman BJ, Freund KM, Battaglia TA. Patient navigation to increase mammography screening among inner-city women. J Gen Intern Med. 2010;26(2):123–129. doi: 10.1007/s11606-010-1527-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Lasser KE, Murillo J, Lisboa S, et al. Colorectal cancer screening among ethnically diverse, low-income patients: a randomized controlled trial. Arch Intern Med. 2011;171(10):906–912. doi: 10.1001/archinternmed.2011.201. [DOI] [PubMed] [Google Scholar]
- 20.Ell K, Vourlekis B, Lee P, Xie B. Patient navigation and case management following an abnormal mammogram: A randomized clinical trial. Prev Med. 2007;44(1):26–33. doi: 10.1016/j.ypmed.2006.08.001. [DOI] [PubMed] [Google Scholar]
- 21.Nash D, Azeez S, Vlahov D, Schori M. Evaluation of an intervention to increase screening colonoscopy in an urban public hospital setting. J Urban Health. 2006;83(2):231–243. doi: 10.1007/s11524-006-9029-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Nguyen T, McPhee S, Bui-Tong N, et al. Community-based participatory research increases cervical cancer screening among Vietnamese-Americans. J Health Care Poor Underserved. 2006;17(2 Suppl):31–54. doi: 10.1353/hpu.2006.0091. [DOI] [PubMed] [Google Scholar]
- 23.Kreuter MW, Caburnay CA, Chen JJ, Donlin MJ. Effectiveness of individually-tailored calendars in promoting childhood immunization in urban public health centers. Am J Public Health. 2004;94(1):122–127. doi: 10.2105/ajph.94.1.122. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Kreuter MW, Skinner CS, Holt CL, et al. Cultural tailoring for mammography and fruit and vegetable intake among low-income African American women in urban public health centers. Prev Med. 2005;41(1):53–62. doi: 10.1016/j.ypmed.2004.10.013. [DOI] [PubMed] [Google Scholar]
- 25.Eddens K, Snider R, Kreuter MW. Screen for Life: Using targeted health messages to increase participation in a state colorectal cancer screening program. Cases in Public Health Commun Market. 2007 Jun;1(6):1–29. [Google Scholar]
- 26.Clarke P, Evans SH, Hovy EH. Indigenous message tailoring increases consumption of fresh vegetables by clients of community pantries. Health Commun. 2011;26(6):571–582. doi: 10.1080/10410236.2011.558337. [DOI] [PubMed] [Google Scholar]
- 27.Demark-Wahnefried W, Clipp EC, Lipkus IM, et al. Main outcomes of the FRESH START trial: A sequentially tailored diet and exercise mailed print intervention among breast and prostate cancer survivors. J Clin Oncol. 2007;25(19):2709–2718. doi: 10.1200/JCO.2007.10.7094. [DOI] [PubMed] [Google Scholar]
- 28.van Stralen MM, de Vries H, Bolman C, Muddle AN, Lechner L. Exploring the efficacy and moderators of two computer-tailored physical activity interventions for older adults: A randomized controlled trial. Ann Behav Med. 2010;39:139–150. doi: 10.1007/s12160-010-9166-8. [DOI] [PubMed] [Google Scholar]
- 29.Baron RC, Rimer BK, Coates RJ, et al. Client-Directed Interventions to Increase Community Access to Breast, Cervical, and Colorectal Cancer Screening: A Systematic Review. Am J Prev Med. 2008;35(1):S56–S66. doi: 10.1016/j.amepre.2008.04.001. [DOI] [PubMed] [Google Scholar]
- 30.Task Force on Community Preventive Services. Recommendations for client- and provider-directed interventions to increase breast, cervical, and colorectal cancer screening. Am J Prev Med. 2008;35(1s):S21–S5. doi: 10.1016/j.amepre.2008.04.004. [DOI] [PubMed] [Google Scholar]
- 31.Bandura A. Self-efficacy: Toward a unifying theory of behavior change. Psychol Rev. 1977;84(2):191–215. doi: 10.1037//0033-295x.84.2.191. [DOI] [PubMed] [Google Scholar]
- 32.Kerner J, Dusenbury L, Mandelblatt J. Poverty and cultural diversity: challenges for health promotion among the medically underserved. Annu Rev Public Health. 1993;14:355–377. doi: 10.1146/annurev.pu.14.050193.002035. [DOI] [PubMed] [Google Scholar]
- 33.Chisholm J, Burbank V. Evolution and inequality. Int J Epidemiol. 2001;30(2):206–211. doi: 10.1093/ije/30.2.206. [DOI] [PubMed] [Google Scholar]
- 34.Diamant A, Hays R, Morales L, et al. Delays and unmet need for health care among adult primary care patients in a restructured urban public health system. Am J Public Health. 2004;94(5):783–789. doi: 10.2105/ajph.94.5.783. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Gelberg L, Browner C, Lejano E, Arangua L. Access to women’s health care: a qualitative study of barriers perceived by homeless women. Women Health. 2004;40(2):87–100. doi: 10.1300/J013v40n02_06. [DOI] [PubMed] [Google Scholar]
- 36.Rosengard C, Chambers D, Tulsky J, Long H, Chesney M. Value on health, health concerns and practices of women who are homeless. Women Health. 2001;34(2):29–44. [Google Scholar]
- 37.Schlossstein E, St Clair P, Connell F. Referral keeping in homeless women. J Community HealthDec. 1991;16(6):279–285. doi: 10.1007/BF01324513. [DOI] [PubMed] [Google Scholar]