Abstract
Background
As the population ages and critical care advances, a growing number of survivors of critical illness will be at risk for intensive care unit (ICU)–acquired weakness. Bed rest, which is common in the ICU, causes adverse effects, including muscle weakness. Consequently, patients need ICU-based interventions focused on the muscular system. Although emerging evidence supports the benefits of early rehabilitation during mechanical ventilation, additional therapies may be beneficial. Neuromuscular electrical stimulation (NMES), which can provide some muscular activity even very early during critical illness, is a promising modality for patients in the ICU.
Objective
The objectives of this article are to discuss the implications of bed rest for patients with critical illness, summarize recent studies of early rehabilitation and NMES in the ICU, and describe a protocol for a randomized, phase II pilot study of NMES in patients receiving mechanical ventilation.
Design
The study was a randomized, sham-controlled, concealed, phase II pilot study with caregivers and outcome assessors blinded to the treatment allocation.
Setting
The study setting will be a medical ICU.
Participants
The study participants will be patients who are receiving mechanical ventilation for 1 day or more, who are expected to stay in the ICU for an additional 2 days or more, and who meet no exclusion criteria.
Intervention
The intervention will be NMES (versus a sham [control] intervention) applied to the quadriceps, tibialis anterior, and gastrocnemius muscles for 60 minutes per day.
Measurements
Lower-extremity muscle strength at hospital discharge will be the primary outcome measure.
Limitations
Muscle strength is a surrogate measure, not a patient-centered outcome. The assessments will not include laboratory, genetic, or histological measures aimed at a mechanistic understanding of NMES. The optimal duration or dose of NMES is unclear.
Conclusions
If NMES is beneficial, the results of the study will help advance research aimed at reducing the burden of muscular weakness and physical disability in survivors of critical illness.
Each year, millions of patients are admitted to an intensive care unit (ICU) worldwide.1 Because of medical advances, more patients are surviving critical illness.2,3 In the United States, admission of patients for mechanical ventilation accounts for 12% of all hospital costs, or $27.0 billion annually.4 Moreover, the number of patients requiring prolonged (>4 days) mechanical ventilation in the ICU is increasing at 5.1% per year, outpacing the 1.2% annual growth in hospitalizations.5 Because of aging baby boomers, the need for mechanical ventilation by the year 2026 is projected to be 80% greater than that in the year 2000.6
Critical care survival comes at important costs to patients in terms of impaired physical function and quality of life and to society in terms of ongoing health care utilization and lost productivity.7,8 In a landmark prospective observational study of survivors of acute respiratory distress syndrome, 51% and 23% had not returned to work at 1 and 5 years, respectively.9,10 Survivors' mean self-reported quality-of-life scores on the Medical Outcomes Study 36-Item Short-Form Health Survey (SF-36) Physical Component Summary remained below age- and sex-matched population norms throughout the 5-year follow-up,10 representing poorer self-perception of physical health status. In addition, as a performance-based measure of physical function, survivors' 6-minute walk test results at 1 and 5 years were 66% and 76% of predicted results, respectively,9 despite normal or nearly normal pulmonary function.10
Muscle weakness acquired in the ICU contributes to impaired physical function9,10 and is a common and major long-term complication in patients with critical illness. Intensive care unit–acquired weakness is a specific term describing diffuse, symmetrical, generalized muscle weakness that develops after the onset of critical illness without other identifiable causes.11 A systematic review of 24 studies of 1,424 patients with sepsis, multiorgan failure, or prolonged mechanical ventilation demonstrated that 57% had electrophysiological evidence of neuromuscular abnormalities (critical illness neuromyopathy) and muscle weakness.12 Intensive care unit–acquired weakness and critical illness neuromyopathy are associated with increased mortality, length of stay, duration of mechanical ventilation, and hospital costs and can persist for up to 4 years after ICU discharge.13–18 These neuromuscular issues represent important rehabilitation opportunities to help survivors of critical illness improve their functional status and return to their prior roles in society.
Emerging evidence is demonstrating that early rehabilitation in the ICU improves short-term patient outcomes.19,20 However, not all patients in the ICU can participate in physical activity because of sedation, impaired cognition, or insufficient physiological reserve.19 One potential rehabilitation intervention for such patients is neuromuscular electrical stimulation (NMES), which is nonvolitional and can be administered without causing cardiopulmonary instability while a patient remains in bed.21,22
In 2011, the World Health Organization defined rehabilitation as “a set of measures that assist individuals who experience, or are likely to experience, disability to achieve and maintain optimal functioning in interaction with their environments.”23(p93) Furthermore, the World Health Organization clarified the time frame of rehabilitation as follows: “Typically rehabilitation occurs for a specific period of time…and can be needed from the acute or initial phase immediately following recognition of a health condition….”23(p93) This definition of rehabilitation is particularly relevant for patients with critical illness because of their high likelihood of experiencing disability and because it clarifies that “rehabilitation” can begin when critical illness is first recognized.
The objectives of this article are to discuss the implications of bed rest for patients with critical illness, summarize recent key studies of early rehabilitation and NMES in patients receiving mechanical ventilation, and describe a protocol for a blinded, randomized, sham-controlled, phase II trial of NMES in patients receiving mechanical ventilation in an ICU.
Implications of Bed Rest for Patients With Critical Illness—An Urgent Need for Attention to the Muscular System
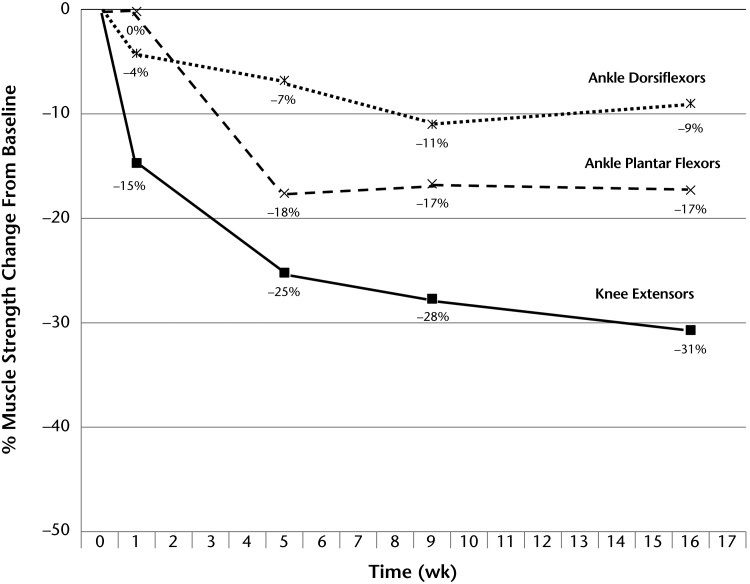
Common clinical practice for patients with critical illness includes bed rest and deep sedation24 to potentially assist with the delivery of interventions for organ failure (eg, mechanical ventilation, vasopressors, and hemodialysis); relatively less attention is directed to the muscular system.25,26 Research on bed rest in volunteers who were healthy demonstrated important deleterious effects on muscles, especially in the lower extremity, with the most rapid rate of loss of strength occurring over the first week.27 After 1 week of bed rest in people who were healthy, muscle volumes in the calf and thigh, measured by magnetic resonance imaging, decreased by 2% and 3% from the baseline, respectively28; by the follow-up at 17 weeks, the total decreases were 30% and 16% to 18%, respectively.27 Overall lean body mass decreased 4% after 17 weeks, with a 12% decrease in the lower extremity.27 Lower-extremity muscle strength, measured by isokinetic dynamometry, decreased in the ankle dorsiflexor, ankle plantar-flexor, and knee extensor muscles by 9%, 17%, and 30%, respectively, after 16 weeks of bed rest; half of the loss of strength in the ankle dorsiflexor and knee extensor muscles occurred during the first week of bed rest (Fig. 1).27
Figure 1.
Changes in lower-extremity muscle strength over time with bed rest in people who were healthy.27
Complications of bed rest in patients with critical illness include systemic inflammation, atelectasis, metabolic and microvascular dysfunction, joint contractures, skin ulcers, and muscle weakness.29 During bed rest, patients do not receive the beneficial effects of exercise, which reduces systemic inflammation through the release of cytokines (eg, interleukin 6).30 In patients with critical illness and on bed rest, there is important physiological evidence of muscle changes that precede clinical recognition.31,32 The loss of lean body mass in patients with critical illness is approximately 1% per day, or 7% per week, in studies with a duration of 3 weeks.33,34 Electromyographic findings of muscle dysfunction can occur within a few days; evidence of structural changes (eg, mildly disturbed muscle fiber structure) can be demonstrated by muscle biopsy at 2 weeks.35 In patients with critical illness, who frequently are on bed rest, strategies for addressing the muscular system early may be important for counteracting these muscular impairments.
Early Rehabilitation in the Critical Care Setting
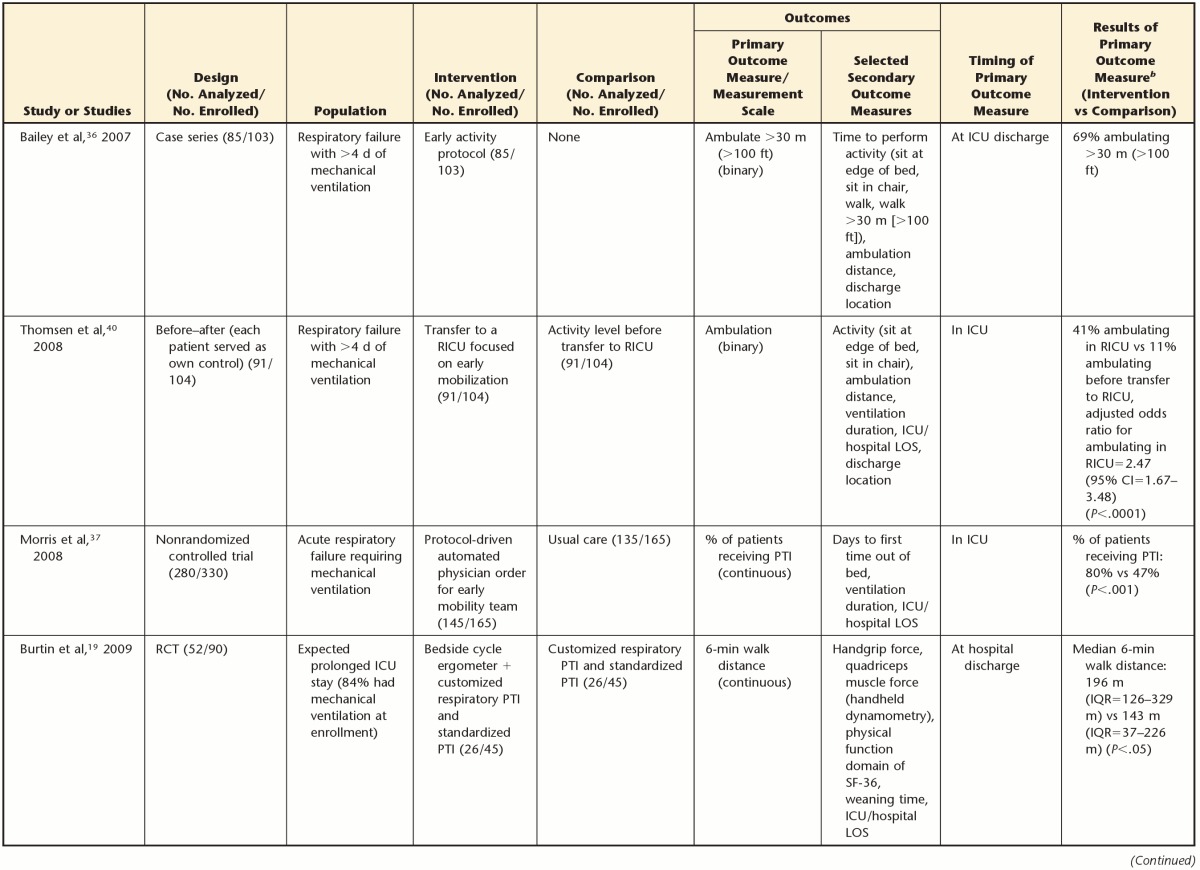
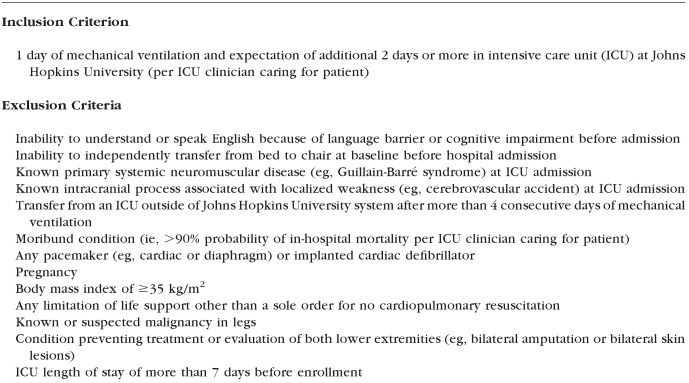
Clinical research evaluating the feasibility, safety, and efficacy of early rehabilitation in patients receiving mechanical ventilation in the ICU presents exciting opportunities for rehabilitation clinicians and researchers. Key features of 6 recent studies in this area are shown in Table 1. Four unique nonrandomized studies36–41 conducted in medical37–39,41 and respiratory36,40 ICUs evaluated various approaches for delivering early rehabilitation. A large case series in a respiratory ICU illustrated that with early rehabilitation, 69% of 85 survivors of critical illness could ambulate more than 30 m (100 ft) by ICU discharge.36 In a separate study, the odds ratio for ambulation was 2.5 (95% confidence interval=1.7–3.5) after transfer of patients requiring mechanical ventilation from a traditional ICU to a respiratory ICU, where early mobility was a priority.40
Table 1.
Early Rehabilitation Studiesa
ICU=intensive care unit, RICU=respiratory intensive care unit, LOS=length of stay, CI=confidence interval, PTI=physical therapy interventions, RCT=randomized controlled trial, SF-36=Medical Outcomes Study 36-Item Short-Form Health Survey questionnaire, IQR=interquartile range, OTI=occupational therapy interventions, QI=quality improvement.
In a nonrandomized controlled trial in a medical ICU setting, 80% of 145 patients received early physical therapist management in the ICU through a protocol-driven, automatic physician order for a multidisciplinary early mobility team (including a physical therapist, nurse, and nursing assistant), whereas 47% of the patients received usual care (P<.001).37 A before-after quality improvement project showed that across all admissions to a medical ICU during this project (n=314) versus the prior year (n=262), interdisciplinary implementation of early rehabilitation was associated with approximately 2- to 4-fold increases in the numbers of physical therapist and occupational therapist consultations and treatments (P≤.04) and an approximately 5-fold increase in the average number of treatments per patient day.38,39 Moreover, in 57 patients receiving mechanical ventilation during this project, rehabilitation treatments during the quality improvement period more often achieved a functional mobility level of sitting or greater than did those during the control period (78% versus 56%) (P=.03).
Two randomized controlled trials (RCTs) of early rehabilitation strategies in patients receiving mechanical ventilation in an ICU provided the most rigorous efficacy evidence to date.19,20 First, in a study of 90 patients, those randomized to use a bedside cycle ergometer as well as to receive standard physical therapist management were able to walk significantly further in the 6-minute walk test at hospital discharge than those receiving standard physical therapist management alone (P<.05).19 Second, in a study of 104 patients, more patients randomized to receive early physical therapist and occupational therapist management while mechanically ventilated at 2 participating medical ICUs achieved functional independence at hospital discharge (as assessed by therapists blinded to treatment allocation) than those randomized to receive standard care (P=.02).20
The strengths of these early rehabilitation studies included the authors' reporting of prospective evaluations,19,20,36–40,42 randomization,19,20 and blinded outcome assessments.20 However, these 6 unique studies measured different primary outcomes, limiting our ability to pool results across studies. Moreover, not all patients with critical illness can actively participate in early rehabilitation because of several factors, including sedation and cognitive impairment.41,43–46 Additional ways to offer such patients some form of physical activity are needed. Neuromuscular electrical stimulation is a promising modality for addressing this gap.
Use of NMES for Patients With Critical Illness
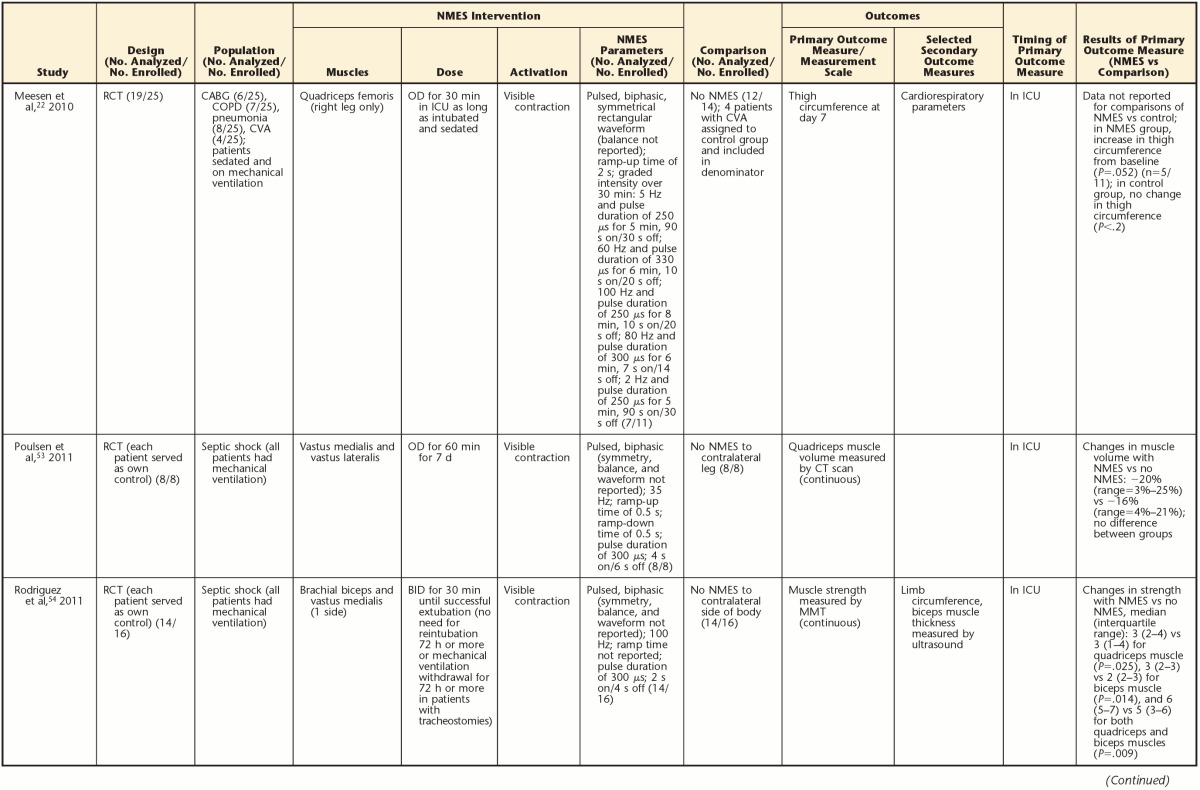
Neuromuscular electrical stimulation is used commonly in outpatient and inpatient rehabilitation settings to preserve or improve muscle mass, strength, and function. Its potential is most promising for immobilized, impaired muscles.21,47 An early study of 1 hour of daily NMES titrated to visible contraction in volunteers who were healthy and immobilized demonstrated preserved leg muscle mass.48 Six unique ICU trials22,49–55 in patients with acute respiratory failure22,49–52,55 and sepsis53,54 and a trial in patients receiving chronic mechanical ventilation56 demonstrated mixed, but promising, results for the potential efficacy of NMES in patients receiving mechanical ventilation in the ICU. Table 2 summarizes key features of these NMES studies.
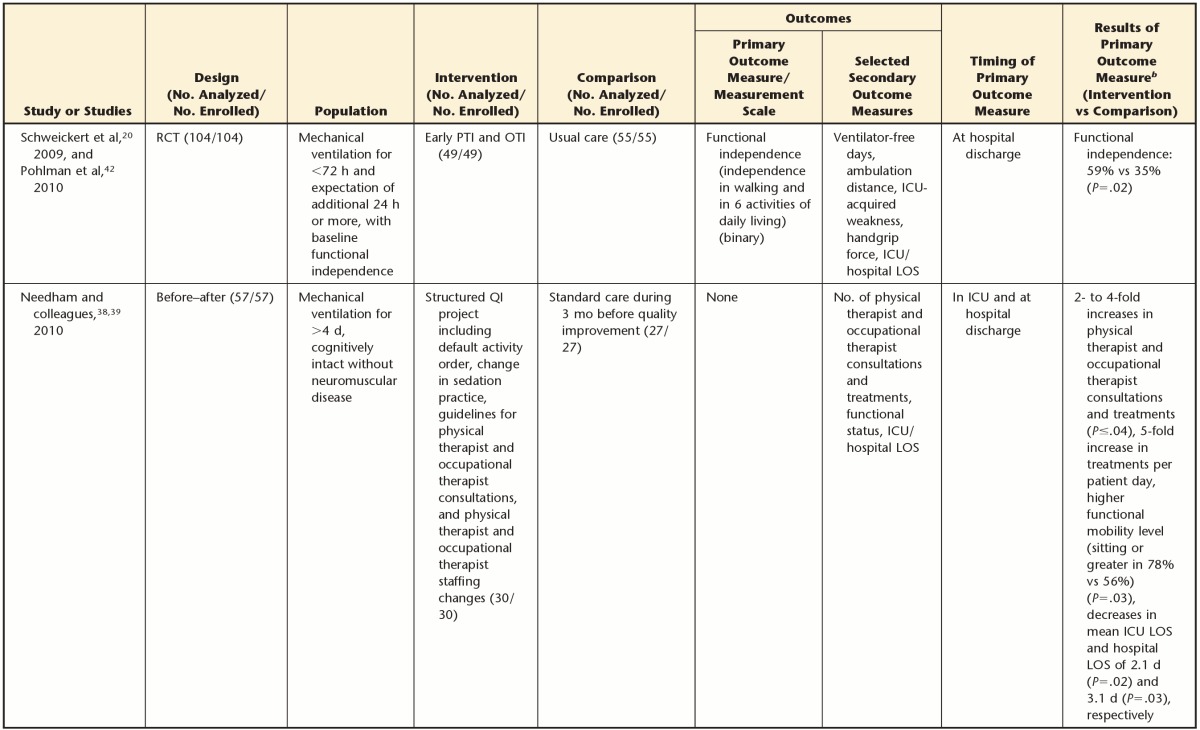
Table 2.
Studies of Neuromuscular Electrical Stimulation (NMES) in People Receiving Mechanical Ventilationa
RCT=randomized controlled trial, ICU=intensive care unit, BID=twice daily, 3-MH=3-methylhistidine, COPD=chronic obstructive pulmonary disease, ALM=active limb mobilization, MMT=manual muscle testing, OD=once daily, LOS=length of stay, CABG=coronary artery bypass graft, CVA=cerebrovascular accident, CT=computed tomography, MIP=maximum inspiratory pressure, MV=mechanical ventilation.
b Because a primary outcome measure was not specified in the study of Bouletreau et al,49 the results shown were from secondary outcome measures.
c ALM also was used.
Neuromuscular electrical stimulation improved muscle strength and physical function in an RCT of patients who had chronic obstructive pulmonary disease, were bed bound, and were receiving chronic ventilation.56 Patients randomized to receive NMES and active limb mobilization had better strength scores (P=.02) and were able to transfer from bed to chair earlier (P=.001) than those receiving active limb mobilization alone.56 In patients with acute respiratory failure, lower-extremity NMES attenuated decreases in quadriceps muscle cross-sectional area55 and thigh circumference22 and reduced muscle catabolism.49 Some evidence of distal effects of lower-extremity NMES on thenar microcirculation also was seen; the hypothesized mechanisms were the local production of cytokines at the site of NMES stimulation and the systemic circulation of these cytokines to increase systemic microcirculation.51 However, in a heterogeneous group of patients receiving short-term (ICU stay of <7 days) and long-term (ICU stay of >14 days) mechanical ventilation, researchers identified no effect of NMES on quadriceps muscle layer thickness in an analysis of all patients combined,52 but the subgroup of patients receiving long-term ventilation and NMES treatment had a significant increase in quadriceps muscle layer thickness compared with patients receiving sham treatment (P=.013). Finally, in an RCT evaluating NMES versus standard care with nonblinded outcome assessments in 52 patients, those randomized to receive NMES had a lower incidence of ICU-acquired weakness at awakening (13%) than those receiving standard care (39%) (P=.04).55
In 2 small studies of patients with sepsis, the effects of NMES were varied, with researchers studying different doses and outcome measures.53,54 In an RCT of 8 patients with sepsis and receiving mechanical ventilation, patients received 7 days of NMES applied to the quadriceps muscle starting within 72 hours of the diagnosis of sepsis. Each patient randomly received NMES on one leg and no NMES on the contralateral leg. After 7 days, there was no difference in the rate of decrease in quadriceps muscle volume measured by computed tomography between the NMES and control groups (P=.12).53 Conversely, in an RCT of 16 patients with sepsis and receiving mechanical ventilation, NMES was randomly assigned to one side of the body for treating both the quadriceps and the biceps muscles. At awakening, both the quadriceps and the biceps muscles randomized to the NMES group had increased strength compared with muscles randomized to the control group (for quadriceps muscle, P=.025; for biceps muscle, P=.014), as assessed by physical therapists blinded to randomization.54
The NMES studies included heterogeneous NMES settings, doses (ie, duration of NMES therapy), target muscles, and outcomes, precluding quantitative pooling of study results. None of these studies assessed the effects of NMES beyond the time of awakening in the ICU or measured patient-centered outcomes such as activity (execution of tasks or actions, such as functional outcomes) or participation (involvement in a life situation, such as return to societal role).57 Thus, there is a need for further, rigorous study of NMES for patients receiving mechanical ventilation in an ICU, with the ultimate goal of determining the efficacy of NMES in a long-term evaluation of patient-centered outcomes. To help evaluate the potential efficacy of NMES, we planned a phase II study with follow-up at hospital discharge.
Method
We designed a randomized phase II study to determine the appropriateness and feasibility of a future phase III RCT to evaluate the efficacy of early NMES for improving patient-centered outcomes in patients receiving mechanical ventilation in the ICU. Because of the tremendous costs of multicenter phase III RCTs,58 randomized pilot trials play an important role in the development and evaluation of research ideas before phase III trials are conducted (eg, National Institutes of Health R34 grants and Canadian Institutes of Health Research RCT competition). Pilot RCTs inform the design and conduct of larger RCTs by assessing feasibility, examining eligibility criteria, and/or assessing potential mechanisms of an intervention.59 In our randomized phase II study, we will examine the feasibility of implementing our research protocol, assess the appropriateness of our eligibility criteria, and determine the effects of NMES on strength (a measure of body structure and function, in accordance with the International Classification of Functioning, Disability and Health,57 and a potential surrogate outcome for patient-centered outcomes, such as activity or function). Here we described our pilot trial protocol, in accordance with Consolidated Standards of Reporting Trials (CONSORT) standards.60
Our hypothesis is that 60 minutes of daily NMES (versus a sham [control] intervention) applied to 3 bilateral lower-extremity muscle groups will increase lower-extremity muscle strength at hospital discharge in patients receiving mechanical ventilation in the ICU.
Design Overview
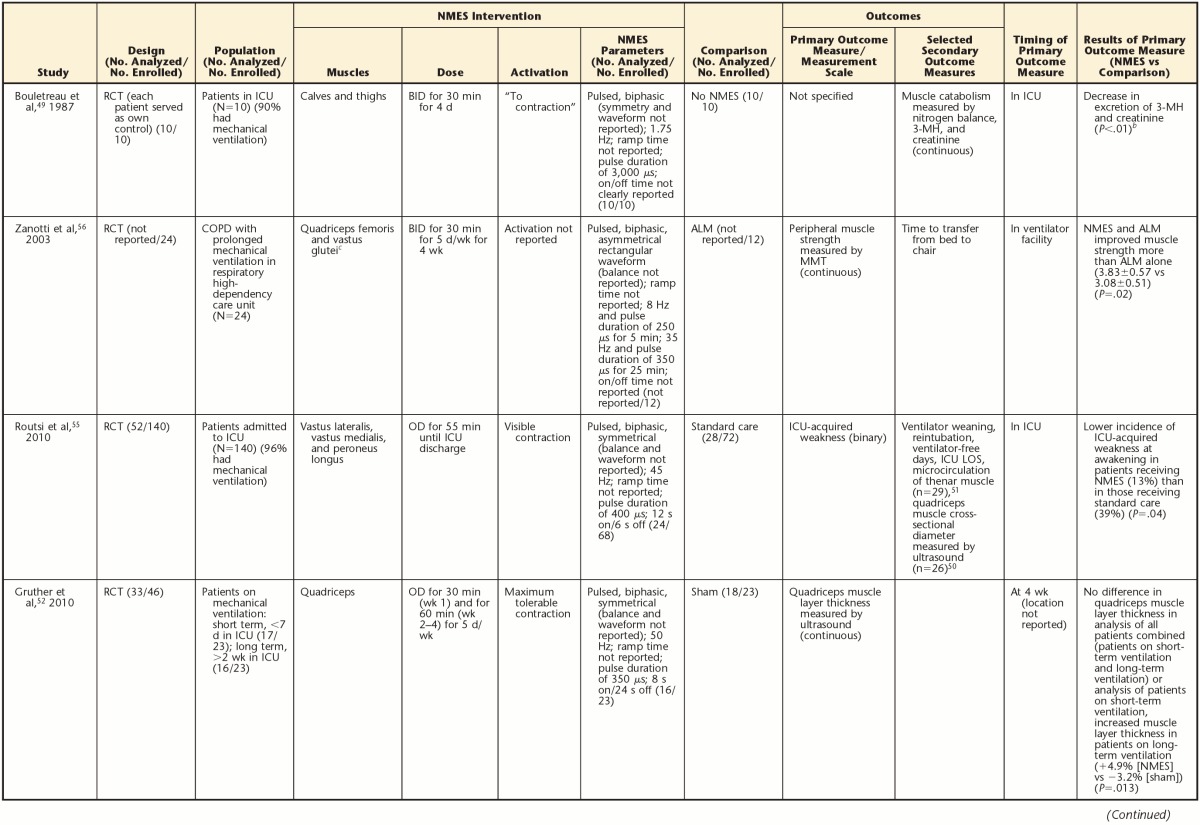
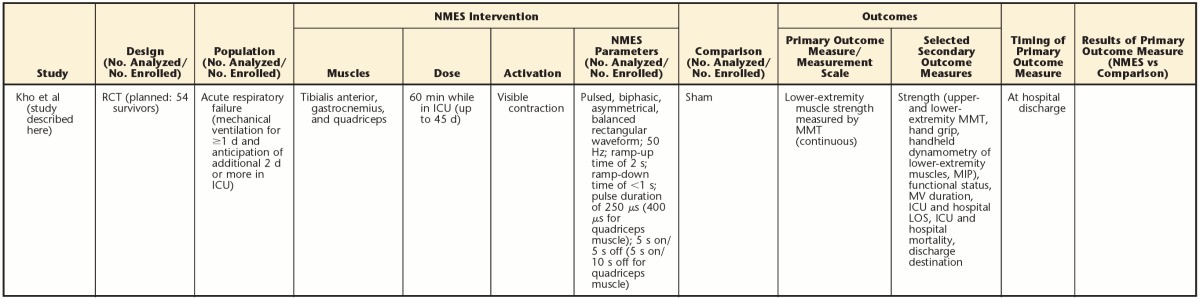
Figure 2 shows our trial schema. The study will be a single-blind, sham-controlled, randomized trial.
Figure 2.
Trial schema: timing of trial enrollment, trial interventions (neuromuscular electrical stimulation [NMES] versus sham), and outcome assessments. See the text and Table 3 for detailed descriptions of primary and secondary outcome measures. ICU=intensive care unit, MV=mechanical ventilation, PT=physical therapy.
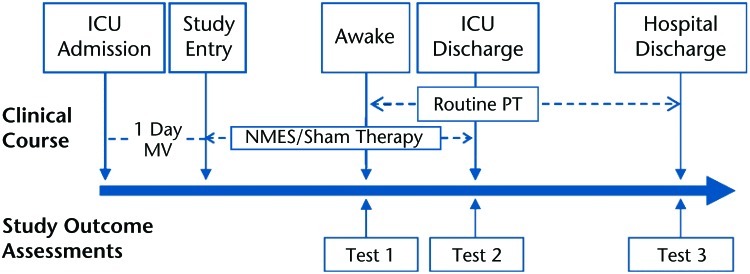
Setting and Participants
The setting will be an ICU at Johns Hopkins University. The participants will be adults (>18 years of age) receiving mechanical ventilation for 1 day and expected to require an additional 2 days or more in the ICU. Appendix 1 outlines the trial eligibility criteria.
Randomization and Interventions
Because mechanical ventilation is a requirement for eligibility, the participants frequently will be delirious and incapable of consent.61,62 In such cases, we will obtain consent from surrogates making decisions for eligible patients. As the participants recover, they will be evaluated for the capacity to provide consent to continue in the study. After consent is obtained, we will randomize the participants in a 1:1 ratio to 60 minutes of daily NMES versus a sham intervention for the duration of their ICU stay (up to a maximum of 28 days of intervention), which corresponds to the time period during which bed rest is most likely. We will use sequentially numbered, opaque, sealed envelopes to maintain randomization allocation concealment in accordance with existing standards63; thus, those obtaining consent will be unaware of the allocation assignment at the time of consent.
NMES.
We will use 3 identical, dual-channel NMES machines (CareStim, Care Rehab Products, McLean, Virginia) to apply therapy bilaterally to 3 muscle groups (quadriceps, tibialis anterior, and gastrocnemius) for 60 minutes daily. We chose these muscles because they are most vulnerable to weakness after bed rest in people who are healthy27 and are easily accessible in people in the supine position. We will use the following NMES settings for all muscles: pulsed-current, biphasic, asymmetrical, balanced rectangular waveform; ramp-up time of 2 seconds; ramp-down time of less than 1 second; and frequency (pulse rate) of 50 Hz. For the quadriceps muscle, we will use a pulse duration of 400 microseconds, an “on” time of 5 seconds, and an “off” time of 10 seconds. For the tibialis anterior and gastrocnemius muscles, we will use a pulse duration of 250 microseconds, an on time of 5 seconds, and an off time of 5 seconds; we derived these settings from outpatient rehabilitation care standards and studies available at the time of our study design.56,64,65 We will apply surface reusable gel electrodes (∼5 × 10 cm [2 × 4 in] oval for quadriceps and gastrocnemius muscles; ∼5 × 5 cm [2 × 2 in] square for tibialis anterior muscle) at standardized electrode placements, modified to avoid interference with heart monitors.66
At the start of each treatment, we will titrate the NMES amplitude to achieve visible contraction of the muscle without causing pain. Pain will be assessed before the NMES/sham session as a baseline evaluation and repeated 5 minutes later using the Behavioral Pain Rating Scale (for sedated patients)67 or numerical rating scale (if awake).68 We chose a longer pulse duration for the quadriceps muscle because of increased muscle bulk, as in earlier studies.56,64,65 Electrical stimulation will occur simultaneously in all muscles, except that stimulation of the tibialis anterior muscle will alternate with stimulation of the gastrocnemius muscle to simulate physiologic contractions and optimize comfort.
Sham intervention.
For the sham intervention, electrodes will be applied and all conditions will be similar to those in the NMES intervention, except that the amplitude will be set to 0 mA so that no muscle stimulation occurs.
Only staff who administer the NMES and sham sessions will know each participant's randomized allocation. All ICU clinical staff providing care (eg, nurses, physicians, and physical therapists) and the research staff performing the outcome assessments will be unaware of the allocation. When administering the sessions, we will draw each participant's bedside curtain while we prepare the NMES machines, and we will cover the participant's legs with a bed sheet so that ICU clinical staff, patients, and family members cannot see the machines or muscle contractions. Although participants will not be informed of their randomized allocation, they may feel the stimulation and contractions with NMES (versus with the sham intervention) and, therefore, may be aware of the allocation. To address this situation, we will instruct the participants not to discuss their perception regarding treatment allocation with outcome assessors or ICU clinical staff. The staff applying NMES will use generic, standardized language to describe each session (eg, calling the intervention a “research session” without reference to NMES or sham). To evaluate blinding, we will ask the participants and outcome assessors to provide their “best guess” regarding treatment allocation (NMES versus sham) at hospital discharge and after each outcome assessment, respectively.
Outcomes and Follow-up
Our primary outcome will be lower-extremity muscle strength at hospital discharge. This outcome (range=0–30) will be the sum of the strength scores (range=0–5) for each of 3 bilateral muscle groups (quadriceps, tibialis anterior, and gastrocnemius) assessed by manual muscle testing.69 We chose the American Spinal Injury Association system to test muscle strength because it is a standardized method for evaluating strength while a person is supine, permitting assessments to be readily standardized and feasible throughout a person's hospital stay, including upon awakening while still critically ill in the ICU.70 Table 3 outlines our secondary outcomes, which include hand grip, maximum inspiratory pressure,71 and assessment of functional status.41 Appendix 2 outlines our feasibility objectives. Outcomes will be evaluated by trained research staff (blinded to treatment allocation) at 3 time points: immediately after the participant is alert and can follow simple commands, at ICU discharge, and at hospital discharge (Fig. 2). If a participant is readmitted to the ICU during the index hospitalization, we will restart NMES or sham treatment (in accordance with the original randomization) and repeat all assessments at awakening and ICU discharge. Participants will receive routine physical therapy interventions during their entire ICU stay and hospital stay.
Table 3.
Secondary Outcomes, Measurement Instruments, and Timing of Assessmentsa
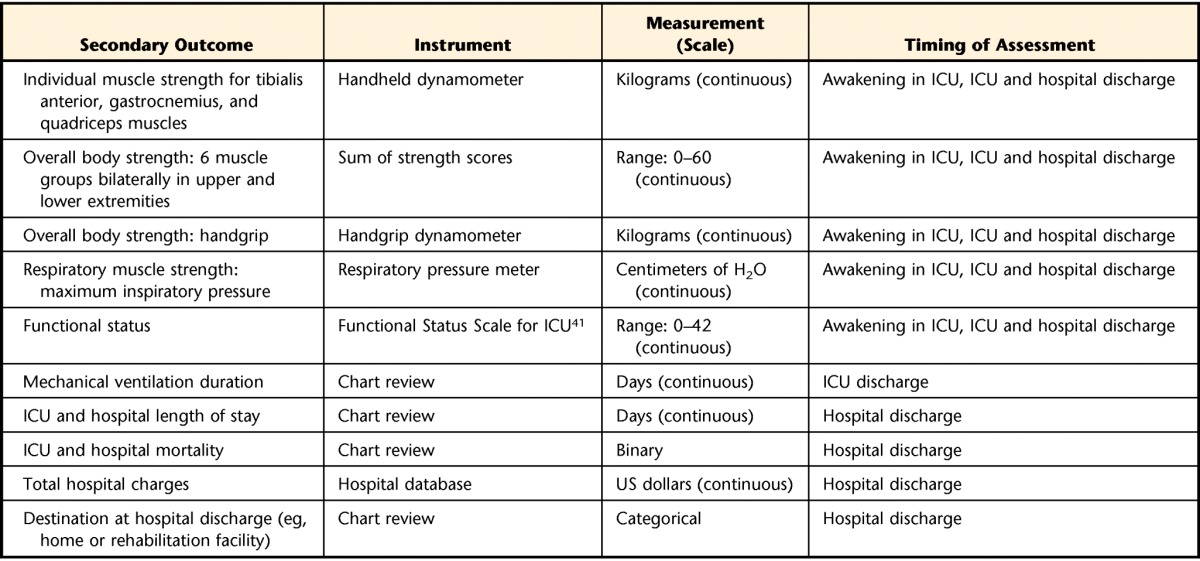
ICU=intensive care unit.
Sample Size and Data Analysis
On the basis of previous analyses of data from similar patients at our study site, we anticipate a control group total muscle strength score of 21.3 (SD=6.8) points out of a maximum of 30 points (3 bilateral muscle groups rated on a scale from 0 [no muscle contraction] to 5 [muscle contraction against a normal amount of resistance]).70 On the basis of strength gains of 24% to 31% in earlier trials of NMES,56,65 we believe that a 25% increase in strength (ie, a 5.3-point increase in the total score) is feasible and clinically important. Therefore, at a power of 80% and an alpha value of 5%, we will need 27 survivors per group (for a total of 54). This sample size is larger than those used in earlier trials of NMES for chronic obstructive pulmonary disease or congestive heart failure (sample sizes of 14–42), which yielded a positive effect of NMES.56,64,65,72,73 Assuming a 34% hospital mortality and an 80% consent rate (based on earlier data from similar patients at our study site), we anticipate needing to identify 103 eligible patients in the ICU to enroll 82 participants to obtain the goal sample size of 54 survivors with complete outcome assessments at hospital discharge. We will use the intention-to-treat principle for all statistical analyses.74 No early stopping will be considered, and no interim analysis will occur in this small pilot trial.
For all continuous variables, we will compare the 2 randomized groups by using the Student t test if the data are normally distributed or the Mann-Whitney U test if the data are not normally distributed. For binary variables, we will use the chi-square test for nonparametric data and the Fisher exact test as needed. If important confounders are unequally distributed between the groups during randomization, we will adjust for important imbalances in confounders by using multiple linear and logistic regression analyses for continuous and binary outcomes, respectively. If one or more of our feasibility objectives are not met, we may revise our protocol to ensure the success of a future phase III trial.59
Role of the Funding Source
Dr Kho receives funding from a Canadian Institutes of Health Research (CIHR) Fellowship Award and Bisby Prize. Dr Fan receives funding from a CIHR Fellowship Award. Blinded outcome assessments are funded through grant UL1 RR 025005 from the National Center for Research Resources, a component of the National Institutes of Health (NIH) and NIH Roadmap for Medical Research. Care Rehab Products (McLean, Virginia) provided CareStim NMES machines for use during the study. The CIHR, the NIH, and Care Rehab Products had no role in the design, conduct, or planned statistical analysis of the study and had no influence on the analysis, interpretation, or decision to submit the study for publication.
Discussion
If NMES is successful, then our protocol will be an important contribution to reducing the burden of weakness and physical disability in survivors of critical illness and addressing a significant public health issue. Our study will advance this research agenda by examining the effects of NMES on muscle strength at hospital discharge, but there is still a need for future research examining patient-centered outcomes at hospital discharge and at long-term follow-up. The strengths of our phase II randomized trial include rigorous design (randomized, concealed allocation, with caregivers and outcome assessors blinded to allocation, and intention-to-treat analysis) and measurement of the primary outcome at hospital discharge. We will minimize potential differences between groups during the study by using specific measures to ensure that caregivers are unaware of the allocation (drawing the participant's bedside curtain at the start of the research session and covering the participant's legs with a sheet) to protect against differences in cointerventions (participants in treatment groups receiving care other than the intervention under study).74 We will use blinded outcome assessments to protect against bias.74 By conducting an intention-to-treat analysis, we will analyze all participants in the arm to which they are randomized, regardless of whether they receive the randomly allocated intervention.74 We will collect secondary outcome data based on patient-centered functional assessments (Tab. 3) and will determine the feasibility of implementing and coordinating a complex research protocol during our phase II study (Appendix 2).
Our study has potential limitations. First, our primary outcome measure, muscle strength, is not a patient-centered outcome. However, as this field emerges, some signal of efficacy at the level of body structure and function is needed before larger studies powered on patient-centered outcomes can be pursued. The proposed sample size will detect a difference in lower-extremity muscle strength of 25%, which translates to an average increase in the average score of approximately 1 point (ie, from 3 to 4) for our ordinal measure of strength for each of the 6 lower-extremity muscles examined. There is no research validating the minimal important difference for this measure. Although this 25% difference is substantial, we believe that a smaller difference may translate into little meaningful functional benefit for patients. Moreover, we will be evaluating secondary outcome measures to help determine the functional effect of NMES, as measured with the Functional Status Scale for the ICU.41 This is an important advance because a patient's muscle strength may improve, but this improvement may not be reflected in functional status, which is a more important outcome for patients.
The second limitation is that our assessments will not include laboratory, genetic, or histological measures aimed at a mechanistic understanding of how NMES may affect proposed outcomes. We specifically chose multiple measures of strength and important clinical and functional outcomes to demonstrate clinically relevant effects of NMES on patients. Mechanistic measures (eg, muscle size, protein breakdown, and microcirculation effects) have been evaluated in other studies of NMES in patients with critical illness and support its use.49–51 The third limitation is that the optimal duration or dose of NMES is unclear. However, the duration or dose is based on the positive effect of NMES in earlier trials conducted with various groups of patients, including patients receiving mechanical ventilation.
Our study will advance the paradigm of early rehabilitation in patients with critical illness by providing an intervention, NMES, specifically aimed at the muscular system. There is a gap in current research on the effects of NMES in patients receiving mechanical ventilation because no published NMES studies examined outcomes beyond awakening in the ICU (Tab. 2). Our protocol builds on previous research on NMES in patients with critical illness by ensuring that both caregivers and outcome assessors are unaware of the treatment allocation, measuring outcomes at 2 time points beyond awakening in the ICU, and collecting secondary outcome data on patient-centered outcomes. We carefully designed the trial to minimize bias. Our study will contribute short-term longitudinal data characterizing the physical recovery of patients with critical illness in a hospital setting. As the field of critical care rehabilitation evolves, more research on the measurement properties (eg, reliability and responsiveness) of outcome measures will be needed. Data on patient-centered outcomes measured during our phase II study will contribute to the expansion of outcome measures for patients recovering from critical illness.
We suggest that clinicians working at the bedside cautiously interpret the eventual results of our phase II trial for patient care purposes. As with all pilot trials, the results of our trial will be valuable for informing the potential design and conduct of a larger RCT.59 The purpose of our trial is to determine the effects of NMES on muscle strength, measured by manual muscle testing, a potential surrogate outcome. Surrogate outcomes are valuable if they can be validated to substitute for direct measures of patient-centered outcomes focused on patients' feelings, function, or survival.74 Such validation has not yet occurred for manual muscle testing in survivors of critical illness. In emerging areas of research, validated surrogate outcomes are helpful because they can establish the potential benefit of an intervention with a smaller sample size and shorter duration of follow-up.74 However, proposed surrogate outcomes may not have a relationship to patient-centered outcomes. For example, researchers found no relationship between lumbar range of motion and a measure of disability, the Oswestry Disability Index, in patients with chronic low back pain.75 Thus, there is a need for clinical trial evidence supporting the use of NMES for patient-centered outcomes related to activity and participation.57
In conclusion, as the demand for mechanical ventilation increases with the aging population and as ICU mortality declines, there will be a growing number of survivors at risk of developing ICU-acquired weakness. Consequently, novel therapeutic interventions directed at the muscular system during critical illness are needed. Although the use of NMES is common in outpatient and inpatient rehabilitation settings, its early use to preserve muscle strength or attenuate decreases in muscle strength in the critical care setting is novel. Early interventions directed at the muscular system in patients with critical illness may have an important impact on short- and long-term outcomes. If our phase II trial demonstrates a positive effect of NMES on our primary outcome, muscle strength, then a multicenter randomized trial to evaluate the efficacy of NMES for patient-centered outcomes may be warranted. If our phase II trial demonstrates a negative effect or no effect of NMES on our primary outcome, we must carefully examine our secondary outcomes to interpret the results and the associated hypothesis-generating implications for future study. Additional research examining the optimal frequency, dose, and duration of NMES and evaluating patient-centered outcomes beyond hospital discharge is needed to further advance this field of study.
Appendix 1.
Appendix 1.
Eligibility Criteria
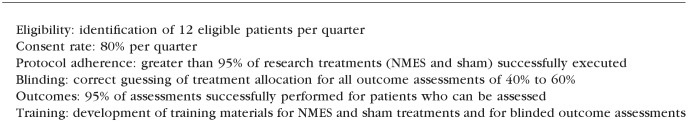
Appendix 2.
Appendix 2.
Feasibility Objectives for Neuromuscular Electrical Stimulation (NMES) Pilot Trial
Footnotes
Dr Kho, Dr Truong, Dr Brower, Dr Palmer, Dr Fan, Dr Zanni, Dr Ciesla, Dr Korupolu, and Dr Needham provided concept/idea/research design. Dr Kho, Dr Truong, and Dr Needham provided writing. Dr Kho, Dr Truong, Dr Zanni, Dr Ciesla, Dr Feldman, and Dr Korupolu provided data collection. Dr Needham provided data analysis. Dr Kho and Dr Truong provided project management. Dr Kho and Dr Truong provided participants, and Dr Kho provided clerical support. All authors provided consultation (including review of manuscript before submission).
The authors are grateful to the following people (in alphabetical order) for their contributions to the development and execution of the phase II study: Gadi Alon, PT, PhD; Jenna Bohrer, PT, DPT; Lora Clawson, MSN, CRNP; David Cornblath, MD; Steven Crandall, PT, DPT; Fern Dickman, BS, MPH; Victor Dinglas, BS; Elizabeth Fuller, BA; Robert Martin; Rasha Nusr, MBBS, MPH; Karen Oakjones-Burgess, RN; Jessica Rossi, PT, DPT; Kristin Sepulveda, BA; Faisal Siddiqi, MD; Cynthia Reilly, PT, DPT; Julie Skrzat, PT, DPT; Rachel Woloszyn, PT, DPT; and Nicole Yare, PT, DPT. The authors are grateful to the following people for assistance in preparing the manuscript: Kareem Fakhoury; Rod Rahimi, MD, PhD; and Ken Johnson, PT.
The study was approved by the Johns Hopkins University Institutional Review Board (NA 000117423).
Dr Kho receives funding from a Canadian Institutes of Health Research (CIHR) Fellowship Award and Bisby Prize. Dr Fan receives funding from a CIHR Fellowship Award. Blinded outcome assessments are funded through grant UL1 RR 025005 from the National Center for Research Resources, a component of the National Institutes of Health (NIH) and NIH Roadmap for Medical Research. Care Rehab Products (McLean, Virginia) provided CareStim NMES machines for use during the study.
ClinicalTrials.gov Identifier: NCT00709124.
References
- 1. Adhikari NK, Rubenfeld GD. Worldwide demand for critical care. Curr Opin Crit Care. 2011;17:620–625 [DOI] [PubMed] [Google Scholar]
- 2. Spragg RG, Bernard GR, Checkley W, et al. Beyond mortality: future clinical research in acute lung injury. Am J Respir Crit Care Med. 2010;181:1121–1127 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Martin GS, Mannino DM, Eaton S, Moss M. The epidemiology of sepsis in the United States from 1979 through 2000. N Engl J Med. 2003;348:1546–1554 [DOI] [PubMed] [Google Scholar]
- 4. Wunsch H, Linde-Zwirble WT, Angus DC, et al. The epidemiology of mechanical ventilation use in the United States. Crit Care Med. 2010;38:1947–1953 [DOI] [PubMed] [Google Scholar]
- 5. Zilberberg MD, de Wit M, Shorr AF. Accuracy of previous estimates for adult prolonged acute mechanical ventilation volume in 2020: update using 2000–2008 data. Crit Care Med. 2012;40:18–20 [DOI] [PubMed] [Google Scholar]
- 6. Needham DM, Bronskill SE, Calinawan JR, et al. Projected incidence of mechanical ventilation in Ontario to 2026: preparing for the aging baby boomers. Crit Care Med. 2005;33:574–579 [DOI] [PubMed] [Google Scholar]
- 7. Cheung AM, Tansey CM, Tomlinson G, et al. Two-year outcomes, health care use, and costs of survivors of acute respiratory distress syndrome. Am J Respir Crit Care Med. 2006;174:538–544 [DOI] [PubMed] [Google Scholar]
- 8. Unroe M, Kahn JM, Carson SS, et al. One-year trajectories of care and resource utilization for recipients of prolonged mechanical ventilation: a cohort study. Ann Intern Med. 2010;153:167–175 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Herridge MS, Cheung AM, Tansey CM, et al. One-year outcomes in survivors of the acute respiratory distress syndrome. N Engl J Med. 2003;348:683–693 [DOI] [PubMed] [Google Scholar]
- 10. Herridge MS, Tansey CM, Matte A, et al. Functional disability 5 years after acute respiratory distress syndrome. N Engl J Med. 2011;364:1293–1304 [DOI] [PubMed] [Google Scholar]
- 11. Stevens RD, Marshall SA, Cornblath DR, et al. A framework for diagnosing and classifying intensive care unit-acquired weakness. Crit Care Med. 2009;37(10 suppl):S299–S308 [DOI] [PubMed] [Google Scholar]
- 12. Stevens RD, Dowdy DW, Michaels RK, et al. Neuromuscular dysfunction acquired in critical illness: a systematic review. Intensive Care Med. 2007;33:1876–1891 [DOI] [PubMed] [Google Scholar]
- 13. Ali NA, O'Brien JM, Jr, Hoffmann SP, et al. Acquired weakness, handgrip strength, and mortality in critically ill patients. Am J Respir Crit Care Med. 2008;178:261–268 [DOI] [PubMed] [Google Scholar]
- 14. De Jonghe B, Bastuji-Garin S, Durand MC, et al. Respiratory weakness is associated with limb weakness and delayed weaning in critical illness. Crit Care Med. 2007;178:261–268 [DOI] [PubMed] [Google Scholar]
- 15. De Jonghe B, Bastuji-Garin S, Sharshar T, et al. Does ICU-acquired paresis lengthen weaning from mechanical ventilation? Intensive Care Med. 2004;30:1117–1121 [DOI] [PubMed] [Google Scholar]
- 16. Garnacho-Montero J, Amaya-Villar R, Garcia-Garmendia JL, et al. Effect of critical illness polyneuropathy on the withdrawal from mechanical ventilation and the length of stay in septic patients. Crit Care Med. 2005;33:349–354 [DOI] [PubMed] [Google Scholar]
- 17. Rudis MI, Guslits BJ, Peterson EL, et al. Economic impact of prolonged motor weakness complicating neuromuscular blockade in the intensive care unit. Crit Care Med. 1996;24:1749–1756 [DOI] [PubMed] [Google Scholar]
- 18. Sharshar T, Bastuji-Garin S, Stevens RD, et al. Presence and severity of intensive care unit-acquired paresis at time of awakening are associated with increased intensive care unit and hospital mortality. Crit Care Med. 2009;37:3047–3053 [DOI] [PubMed] [Google Scholar]
- 19. Burtin C, Clerckx B, Robbeets C, et al. Early exercise in critically ill patients enhances short-term functional recovery. Crit Care Med. 2009;37:2499–2505 [DOI] [PubMed] [Google Scholar]
- 20. Schweickert WD, Pohlman MC, Pohlman AS, et al. Early physical and occupational therapy in mechanically ventilated, critically ill patients: a randomised controlled trial. Lancet. 2009;373:1874–1882 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Maffiuletti NA. Physiological and methodological considerations for the use of neuromuscular electrical stimulation. Eur J Appl Physiol. 2010;110:223–234 [DOI] [PubMed] [Google Scholar]
- 22. Meesen RL, Dendale P, Cuypers K, et al. Neuromuscular electrical stimulation as a possible means to prevent muscle tissue wasting in artificially ventilated and sedated patients in the intensive care unit: a pilot study. Neuromodulation. 2010;13:315–321 [DOI] [PubMed] [Google Scholar]
- 23. World Report on Disability 2011. Geneva, Switzerland: World Health Organization; 2011 [PubMed] [Google Scholar]
- 24. Needham DM. Mobilizing patients in the intensive care unit: improving neuromuscular weakness and physical function. JAMA. 2008;300:1685–1690 [DOI] [PubMed] [Google Scholar]
- 25. Bolton CF, Young GB. Managing the nervous system effects of sepsis. Chest. 2007;131:1273–1274 [DOI] [PubMed] [Google Scholar]
- 26. Petty TL. Suspended life or extending death? Chest. 1998;114:360–361 [DOI] [PubMed] [Google Scholar]
- 27. LeBlanc AD, Schneider VS, Evans HJ, et al. Regional changes in muscle mass following 17 weeks of bed rest. J Appl Physiol. 1992;73:2172–2178 [DOI] [PubMed] [Google Scholar]
- 28. Ferrando AA, Stuart CA, Brunder DG, Hillman GR. Magnetic resonance imaging quantitation of changes in muscle volume during 7 days of strict bed rest. Aviat Space Environ Med. 1995;66:976–981 [PubMed] [Google Scholar]
- 29. Brower RG. Consequences of bed rest. Crit Care Med. 2009;37(10 suppl):S422–S428 [DOI] [PubMed] [Google Scholar]
- 30. Petersen AM, Pedersen BK. The anti-inflammatory effect of exercise. J Appl Physiol. 2005;98:1154–1162 [DOI] [PubMed] [Google Scholar]
- 31. Ferrando AA, Paddon-Jones D, Wolfe RR. Bed rest and myopathies. Curr Opin Clin Nutr Metab Care. 2006;9:410–415 [DOI] [PubMed] [Google Scholar]
- 32. Reid CL, Campbell IT, Little RA. Muscle wasting and energy balance in critical illness. Clin Nutr. 2004;23:273–280 [DOI] [PubMed] [Google Scholar]
- 33. Finn PJ, Plank LD, Clark MA, et al. Progressive cellular dehydration and proteolysis in critically ill patients. Lancet. 1996;347:654–656 [DOI] [PubMed] [Google Scholar]
- 34. Griffiths RD. Muscle mass, survival, and the elderly ICU patient. Nutrition. 1996;12:456–458 [DOI] [PubMed] [Google Scholar]
- 35. Ahlbeck K, Fredriksson K, Rooyackers O, et al. Signs of critical illness polyneuropathy and myopathy can be seen early in the ICU course. Acta Anaesthesiol Scand. 2009;53:717–723 [DOI] [PubMed] [Google Scholar]
- 36. Bailey P, Thomsen GE, Spuhler VJ, et al. Early activity is feasible and safe in respiratory failure patients. Crit Care Med. 2007;35:139–145 [DOI] [PubMed] [Google Scholar]
- 37. Morris PE, Goad A, Thompson C, et al. Early intensive care unit mobility therapy in the treatment of acute respiratory failure. Crit Care Med. 2008;36:2238–2243 [DOI] [PubMed] [Google Scholar]
- 38. Needham DM, Korupolu R. Rehabilitation quality improvement in an intensive care unit setting: implementation of a quality improvement model. Top Stroke Rehabil. 2010;17:271–281 [DOI] [PubMed] [Google Scholar]
- 39. Needham DM, Korupolu R, Zanni JM, et al. Early physical medicine and rehabilitation for patients with acute respiratory failure: a quality improvement project. Arch Phys Med Rehabil. 2010;91:536–542 [DOI] [PubMed] [Google Scholar]
- 40. Thomsen GE, Snow GL, Rodriguez L, Hopkins RO. Patients with respiratory failure increase ambulation after transfer to an intensive care unit where early activity is a priority. Crit Care Med. 2008;36:1119–1124 [DOI] [PubMed] [Google Scholar]
- 41. Zanni JM, Korupolu R, Fan E, et al. Rehabilitation therapy and outcomes in acute respiratory failure: an observational pilot project. J Crit Care. 2010;25:254–262 [DOI] [PubMed] [Google Scholar]
- 42. Pohlman MC, Schweickert WD, Pohlman AS, et al. Feasibility of physical and occupational therapy beginning from initiation of mechanical ventilation. Crit Care Med. 2010;38:2089–2094 [DOI] [PubMed] [Google Scholar]
- 43. Bailey PP, Miller RR, III, Clemmer TP. Culture of early mobility in mechanically ventilated patients. Crit Care Med. 2009;37(10 suppl):S429–S435 [DOI] [PubMed] [Google Scholar]
- 44. Hopkins RO, Spuhler VJ. Strategies for promoting early activity in critically ill mechanically ventilated patients. AACN Adv Crit Care. 2009;20:277–289 [DOI] [PubMed] [Google Scholar]
- 45. Hopkins RO, Spuhler VJ, Thomsen GE. Transforming ICU culture to facilitate early mobility. Crit Care Clin. 2007;23:81–96 [DOI] [PubMed] [Google Scholar]
- 46. Garzon-Serrano J, Ryan C, Waak K, et al. Early mobilization in critically ill patients: patients' mobilization level depends on health care provider's profession. PM R. 2011;3:307–313 [DOI] [PubMed] [Google Scholar]
- 47. Truong AD, Fan E, Brower RG, Needham DM. Bench-to-bedside review: mobilizing patients in the intensive care unit—from pathophysiology to clinical trials. Crit Care. 2009;13:216. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48. Gibson JN, Smith K, Rennie MJ. Prevention of disuse muscle atrophy by means of electrical stimulation: maintenance of protein synthesis. Lancet. 1988;2:767–770 [DOI] [PubMed] [Google Scholar]
- 49. Bouletreau P, Patricot MC, Saudin F, et al. Effects of intermittent electrical stimulations on muscle catabolism in intensive care patients. JPEN J Parenter Enteral Nutr. 1987;11:552–555 [DOI] [PubMed] [Google Scholar]
- 50. Gerovasili V, Stefanidis K, Vitzilaios K, et al. Electrical muscle stimulation preserves the muscle mass of critically ill patients: a randomized study. Crit Care. 2009;13:R161. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51. Gerovasili V, Tripodaki E, Karatzanos E, et al. Short-term systemic effect of electrical muscle stimulation in critically ill patients. Chest. 2009;136:1249–1256 [DOI] [PubMed] [Google Scholar]
- 52. Gruther W, Kainberger F, Fialka-Moser V, et al. Effects of neuromuscular electrical stimulation on muscle layer thickness of knee extensor muscles in intensive care unit patients: a pilot study. J Rehabil Med. 2010;42:593–597 [DOI] [PubMed] [Google Scholar]
- 53. Poulsen JB, Moller K, Jensen CV, et al. Effect of transcutaneous electrical muscle stimulation on muscle volume in patients with septic shock. Crit Care Med. 2011;39:456–461 [DOI] [PubMed] [Google Scholar]
- 54. Rodriguez PO, Setten M, Maskin LP, et al. Muscle weakness in septic patients requiring mechanical ventilation: protective effect of transcutaneous neuromuscular electrical stimulation. J Crit Care. 2011. June 27 [Epub ahead of print] [DOI] [PubMed] [Google Scholar]
- 55. Routsi C, Gerovasili V, Vasileiadis I, et al. Electrical muscle stimulation prevents critical illness polyneuromyopathy: a randomized parallel intervention trial. Crit Care. 2010;14:R74. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56. Zanotti E, Felicetti G, Maini M, Fracchia C. Peripheral muscle strength training in bed-bound patients with COPD receiving mechanical ventilation: effect of electrical stimulation. Chest. 2003;124:292–296 [DOI] [PubMed] [Google Scholar]
- 57. Jette AM. Toward a common language for function, disability, and health. Phys Ther. 2006;86:726–734 [PubMed] [Google Scholar]
- 58. Brower RG, Fessler HE. Another “negative” trial of surfactant: time to bury this idea? Am J Respir Crit Care Med. 2011;183:966–968 [DOI] [PubMed] [Google Scholar]
- 59. Arnold DM, Burns KE, Adhikari NK, et al. The design and interpretation of pilot trials in clinical research in critical care. Crit Care Med. 2009;37(1 suppl):S69–S74 [DOI] [PubMed] [Google Scholar]
- 60. Moher D, Hopewell S, Schulz KF, et al. CONSORT 2010 explanation and elaboration: updated guidelines for reporting parallel group randomised trials. BMJ. 2010;340:c869. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61. Ely EW, Shintani A, Truman B, et al. Delirium as a predictor of mortality in mechanically ventilated patients in the intensive care unit. JAMA. 2004;291:1753–1762 [DOI] [PubMed] [Google Scholar]
- 62. Fan E, Shahid S, Kondreddi VP, et al. Informed consent in the critically ill: a two-step approach incorporating delirium screening. Crit Care Med. 2008;36:94–99 [DOI] [PubMed] [Google Scholar]
- 63. Doig GS, Simpson F. Randomization and allocation concealment: a practical guide for researchers. J Crit Care. 2005;20:187–191 [DOI] [PubMed] [Google Scholar]
- 64. Bourjeily-Habr G, Rochester CL, Palermo F, et al. Randomised controlled trial of transcutaneous electrical muscle stimulation of the lower extremities in patients with chronic obstructive pulmonary disease. Thorax. 2002;57:1045–1049 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65. Vivodtzev I, Pepin JL, Vottero G, et al. Improvement in quadriceps strength and dyspnea in daily tasks after 1 month of electrical stimulation in severely deconditioned and malnourished COPD. Chest. 2006;129:1540–1548 [DOI] [PubMed] [Google Scholar]
- 66. Baker LL, McNeal CL, Newsam DR, et al. Neuro Muscular Electrical Stimulation: A Practical Guide. 4th ed. Downey, CA: Los Amigos Research & Education Institute; 2000 [Google Scholar]
- 67. Gelinas C, Fortier M, Viens C, et al. Pain assessment and management in critically ill intubated patients: a retrospective study. Am J Crit Care. 2004;13:126–135 [PubMed] [Google Scholar]
- 68. Hamill-Ruth RJ, Marohn ML. Evaluation of pain in the critically ill patient. Crit Care Clin. 1999;15:35–54, v–vi [DOI] [PubMed] [Google Scholar]
- 69. American Spinal Injury Association International standards for the classification of spinal cord injury: motor exam guide. Available at: http://www.asia-spinalinjury.org/elearning/Motor_Exam_Guide.pdf. Published June 2008 Accessed March 13, 2012
- 70. Neurological assessment: the motor examination. In: Reference Manual of the International Standards for Neurological Classification of Spinal Cord Injury. Chicago, IL: American Spinal Injury Association; 2003 [Google Scholar]
- 71. Tzanis G, Vasileiadis I, Zervakis D, et al. Maximum inspiratory pressure, a surrogate parameter for the assessment of ICU-acquired weakness. BMC Anesthesiol. 2011;11:14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72. Neder JA, Sword D, Ward SA, et al. Home based neuromuscular electrical stimulation as a new rehabilitative strategy for severely disabled patients with chronic obstructive pulmonary disease (COPD). Thorax. 2002;57:333–337 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73. Quittan M, Wiesinger GF, Sturm B, et al. Improvement of thigh muscles by neuromuscular electrical stimulation in patients with refractory heart failure: a single-blind, randomized, controlled trial. Am J Phys Med Rehabil. 2001;80:206–214 [DOI] [PubMed] [Google Scholar]
- 74. Guyatt GH, Rennie D, Meade MO, Cook DJ.Users' Guides to the Medical Literature: A Manual for Evidence-Based Clinical Practice. 2nd ed. Chicago, IL: AMA Press; 2008 [Google Scholar]
- 75. Nattrass CL, Nitschke JE, Disler PB, et al. Lumbar spine range of motion as a measure of physical and functional impairment: an investigation of validity. Clin Rehabil. 1999;13:211–218 [DOI] [PubMed] [Google Scholar]