Abstract
Objectives
Despite lithium’s clinical efficacy in treating mania in bipolar disorder (BD), studies evaluating early improvement and subsequent treatment response are sparse. This study investigated whether early improvement (within one week) to lithium monotherapy predicted later response and remission in individuals with BD mania.
Methods
BD-I patients (n=46) experiencing a manic episode received lithium monotherapy for four weeks (initial dose: 600 mg/d, adjusted to therapeutic levels); individuals experiencing a mixed episode, rapid cyclers, previous non-responders to lithium, and those with current drug abuse/dependence were excluded. Symptoms were rated using the Young Mania Rating Scale (YMRS) at baseline and at Days 7, 14, 21, and 28.
Results
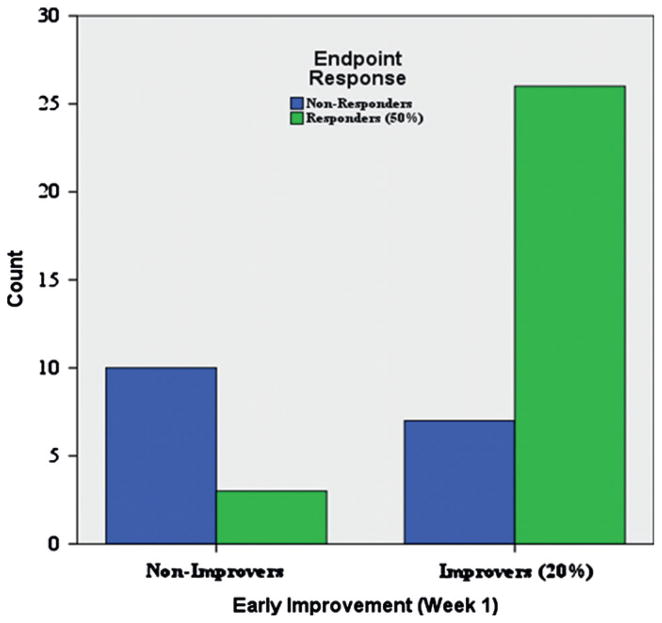
Thirty-three percent of the total sample responded to lithium within the first week of treatment, defined as a ≥50% decrease from baseline YMRS scores; 63% responded by study endpoint. In addition, 39% of the total sample showed early improvement (at least 20% decrease in YMRS scores) after one week of treatment. In this group, 79% responded to lithium by study endpoint. Among those showing less than 20% improvement at Week 1, only 23% responded to lithium by study endpoint.
Limitations
History of episodes sequence was not assessed.
Conclusions
Early improvement in response to lithium monotherapy in subjects with BD mania predicted later response and remission. Most patients who did not show early improvement in response to lithium during the first week of treatment showed no response after one month. The findings provide a valuable clinical tool for early identification of those patients most likely to benefit from lithium in clinical practice.
Keywords: Lithium, Mania, Bipolar disorder, Early response, Treatment, Mood stabilizer
Introduction
In the treatment of bipolar disorder (BD), lithium continues to be the gold standard (American Psychiatric Association, 2002; Suppes et al., 2005; Yatham et al., 2009). It has a long history of safe and effective clinical use in the treatment of both the acute manic phase of the illness as well as maintenance therapy for BD. Clinical evidence regarding predictors of initial treatment response-as opposed to maintenance treatment with lithium-is relatively sparse (Goodnick, 1996); indeed, most of the factors that have been described are associated with non-response to lithium. It is beyond the scope of this paper to review these disparate predictors of response and non-response; the interested reader is referred to recent reviews on the subject (Grof, 2010; Kessing et al., 2011).
Briefly, lithium appears to be the mood stabilizer of choice in individuals whose illness is categorized as “classic” mania encompassing euphoric mood (Grof, 2010), in those with a family history of BD (Coryell et al., 2000), and in patients with little psychiatric comorbidity. In contrast, lithium appears to be relatively ineffective in certain subtypes of BD such as mixed states (Dilsaver et al., 1993; McElroy et al., 1992) or dysphoric mania, rapid-cycling, a high prevalence of depressive symptomatology (Cohen et al., 1989; Swann et al., 1997), and mania secondary to organic illness (Himmelhoch and Garfinkel, 1986; Keller et al., 1986; Secunda et al., 1985). In addition, patients with a history of substance abuse are less likely to respond to lithium (Goldberg et al., 1999; Maj, 2003).
Considerable research has been conducted in recent years exploring predictors of treatment response in major depressive disorder (MDD). Studies exploring early improvement (defined as less than two weeks of treatment) as predictors of long-term response and remission to a variety of antidepressants are serving to reshape thinking in psychiatry regarding the speed with which antidepressant response manifests (Nagayama et al., 1991; Katz et al., 1996; Stassen et al., 1996, 1999; Szegedi et al., 2009, Tohen et al., 2010). Notably, those studies support the notion that, for some patients with MDD, early onset of improvement in depressive symptoms may correlate with better short- and long-term outcome. From a public health perspective, such research is particularly important because the ability to rapidly identify individuals who are not likely to respond to initial drug treatment would reduce patient exposure to ineffective medications, thereby allowing the early switch to other, potentially more effective agents (Kemp et al., 2011a,b), and reducing treatment costs (Szegedi et al., 2009).
With regard to BD, few data exist regarding how early improvement in response to lithium influences subsequent response and remission. Here, we report findings from a post-hoc analysis of data from the lithium/placebo arm of a randomized, double-blind, placebo-controlled trial in BD-I (current manic episode) (Machado-Vieira et al., 2008). The aim of this analysis was to determine whether early response (less than one week) to lithium in patients with BD mania predicted later response and remission.
Patients and methods
Sample
Patients (n=46; 29F/17M; 18 to 65 years old) had a diagnosis of BD-I and were currently experiencing a manic episode with or without psychotic features, as assessed by the Structured Clinical Interview for Axis I DSM-IV-TR Disorders, Research Version, Patient Version (First et al., 1996). All subjects were evaluated between September 2003 and September 2006 at the Bipolar Disorder Research Center—Espirita Hospital of Porto Alegre. Subjects were required to have a baseline score ≥22 on the Young Mania Rating Scale (YMRS) (Young et al., 1978). All subjects were in good physical health as determined by medical history, physical examination, and laboratory test results. Patients had been medication-free for at least four weeks before admission. Exclusion criteria included rapid cycling, mixed episodes, previous history of refractoriness to lithium, current comorbid substance abuse or dependence, and current Axis I psychiatric disorder other than BD. The local institutional review board approved the study. All subjects provided written informed consent.
Study design
Before receiving four weeks of lithium monotherapy for acute mania, patients underwent a two- to seven-day screening period. All patients were started on lithium 600 mg/d; after one week, the dose was increased to 900 mg/d. Thereafter, a flexible dose was used in response to plasma lithium levels (maintained at 0.6–1.2 mmol/L). Concomitant use of diazepam (maximum 20 mg/d) for severe agitation was allowed during the four-week study except for a twelve hour period before rating scales were administered. No antipsychotics were allowed during the study.
Efficacy measures
Subjects were rated at baseline and at Days 7, 14, 21, and 28. The YMRS was the primary outcome measure, and the secondary outcome measure was the Clinical Global Impressions-Severity of Illness (CGI-S) scale. The primary efficacy variable was reduction in YMRS total score from baseline to study endpoint (Day 28). Raters were psychiatrists who displayed an inter-rater reliability of 0.90 for the YMRS.
Three measures of response to lithium were defined. (1) Early improvement: improvement of at least 20% from baseline YMRS score after one week of treatment; (2) Response: 50% improvement from baseline at any time point; and (3) Remission, which was defined two ways: YMRS score ≤12 for the liberal definition, and ≤7 for the more stringent definition.
Statistics
Pearson correlations were used to examine the relationship between potential predictors and outcomes on a continuous scale, and chi-square tests were used for categorical measures. The primary analysis was the association between early response and response at study endpoint. Categorical response relationships were examined to give a more clinical view of this relationship. No multiple comparisons correction was applied to these tests. However, Bonferroni correction was used for additional predictors. All tests were evaluated for significance at p<.05, two-tailed.
Results
Prevalence of improvement
Thirty-three percent of patients (15/46) responded to lithium-that is, they had an at least 50% improvement from YMRS baseline score-within the first week of treatment. Another 39% (18/46) showed early improvement, as assessed by an at least 20% reduction in YMRS scores in the first week. With regard to remission, 22% (10/46) of the patients met the more liberally defined remission criteria by the end of Week 1, and 8% (4/46) achieved remission when the stricter remission criteria were used. The average proportion of improvement from baseline was 37% (SD=25.3).
By study endpoint, 63% (29/46) of the sample had a response to lithium of at least 50%, and another 17% (8/46) improved at least 20% compared to baseline. Furthermore, 52% (25/46) of the patients met the more liberally defined remission criteria by study endpoint, and 39% (18/46) achieved remission when the stricter remission criteria were used. The average proportion of improvement from baseline was 57.4% (SD=36.4).
Relationship between early response and endpoint response
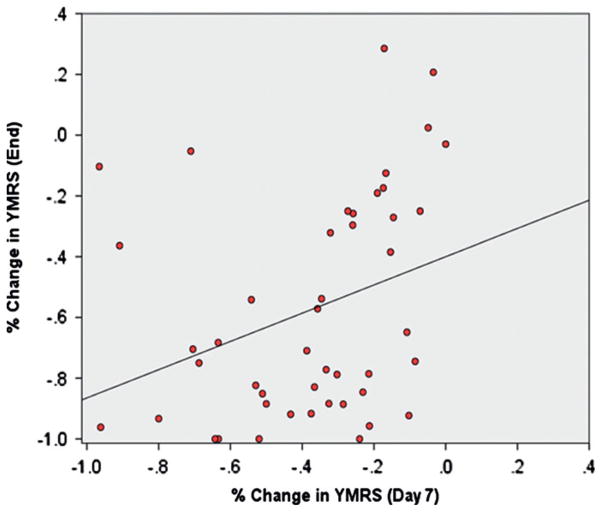
A Pearson correlation between the proportion of change at Week 1 and at endpoint was significant (r=.32, p=.03). This suggests a moderate positive relationship between early improvement and later response.
Chi-square tests were used to further examine whether a minimum 20% improvement after one week was related to response or remission at study endpoint. Using 50% improvement at endpoint (response criteria) as the outcome, it was found a significant relationship between early and later outcome (χ2=12.42, p=.0004; OR=12.38, sensitivity=.89, specificity=.59, positive predictive value=.79, negative predictive value=.77). Of those patients showing early improvement at Week 1, 79% (26/33) had a 50% or better response by study endpoint. In contrast, for those who had not improved by the end of Week 1, only 23% (3/13) had a response at study endpoint. Similar results were obtained when remission at study endpoint was used as the criterion, regardless of whether the liberal (χ2=11.09, p=.0009; OR=12.65) or stricter definition (χ2=7.52, p=.006; OR=12.75) was applied. These results are consistent with the previous correlation indicating that early improvement is positively associated with later response.
Predictors of early improvement
Several potential predictors of early response (by Week 1) to lithium were examined. These included baseline YMRS, individual YMRS items, sex, age, age at first episode, duration of illness, psychosis, number of previous psychiatric hospitalizations, number of suicide attempts, number of mood and manic episodes, serum lithium levels, and serum uric acid levels. No significant predictors were identified after correcting for multiple comparisons.
Predictors of endpoint response
Pearson correlations were used to examine the same variables as potential predictors of endpoint response. Again, no significant predictors were identified after correcting for multiple comparisons.
Because sex (r=−.30, p=.045) was significantly correlated with response before Bonferroni correction, we performed a hierarchical linear regression to determine whether early improvement and sex independently predicted later response, and whether sex added variance to a predictive model that used only early improvement. Early improvement was entered into the model first, and sex was added in a second block. We found that early improvement explained 10% of the variance in later response when included in the model by itself (p=.03). Early improvement remained a significant predictor after adding sex (p=.04). Though adding sex increased the amount of variance explained by 7%, it was not a significant independent predictor (p=.07).
Discussion
This study examined a group of BD-I patients with classic euphoric mania receiving lithium monotherapy and found that early improvement predicted subsequent response and remission to lithium at four weeks. In contrast, among those subjects who showed no early improvement during the first week of lithium treatment, less than one-fourth responded to lithium after four weeks.
Recent research has explored predictors of treatment response in patients with MDD receiving antidepressants. Several studies in MDD suggest that improvement within the first two weeks is associated with endpoint treatment response (Nagayama et al., 1991; Katz et al., 1996; Stassen et al., 1993, 1996, 1999; Szegedi et al., 2009; Tohen et al., 2010; Nierenberg et al., 1995). In contrast, and despite its long history of safe clinical use in BD, little clinical evidence exists regarding predictors of initial treatment response-as opposed to maintenance treatment with lithium (Goodnick, 1996). Fig. 1 Table 1.
Fig. 1.
Association between early improvement in manic symptoms (decrease ≥20% in total YMRS scores after one week of treatment) and response at endpoint (decrease ≥50%, 28 day).
Table 1.
Demographic and clinical characteristics.
| N | % | |
|---|---|---|
| Gender (female) | 29 | 63 |
| Family history of mood disorder (1st degree relatives) | 24 | 52 |
| Psychosis | 21 | 46 |
| Study completion | 31 | 67 |
| Response (end) | 29 | 63 |
| Remission (end) | ||
| • YMRS <12 | 25 | 54 |
| • YMRS <7 | 18 | 39 |
| Mean | SD | |
| Age | 29.3 | 8.5 |
| Duration of illness (years) | 7.9 | 7.5 |
| All mood episodes | 4.7 | 3.3 |
| Previous manic episodes (lifetime) | 3.1 | 2.5 |
| Hospitalizations | 3.1 | 2.9 |
| Clinical ratings (baseline) | ||
| • YMRS | 33.8 | 1.4 |
| • CGI | 5.1 | 0.2 |
| Lithium (serum) | 0.95 | 0.20 |
Recent work in this area has highlighted agents other than lithium in BD. (Kemp et al., 2011b) pooled data from 10 placebo-controlled trials evaluating four different agents-but not lithium-in the treatment of bipolar depression. That study, which considered early improvement as a reduction of 20% or higher from baseline in Montgomery-Asberg Depression Rating Scale (MADRS) scores, reported that the predictive value of early improvement appeared to be both less consistent and less robust in individuals with bipolar depression than in those with MDD; however, the authors did conclude that the absence of early improvement was a reliable predictor of subsequent non-response (Kemp et al., 2011a,b). A similar study exploring early response in BD mania found that patients who responded to olanzapine and risperidone (≥50% reduction on the YMRS) at Week 1 were likely to remain responders at study endpoint (23). In BD patients with acute manic/mixed episodes who received the antipsychotic ziprasidone, early improvement of psychotic symptoms predicted remission at three weeks (Ketter et al., 2010). Another study of BD subjects experiencing a mixed episode who received olanzapine combined with divalproex reported that improvement on CGI-S measures as early as Day 2 predicted remission at six weeks (Houston et al., 2011) Fig. 2.
Fig. 2.
Association between early improvement in manic symptoms (YMRS after one week of treatment) and decrease in severity at endpoint (total YMRS scores after 28 day).
The present findings could provide information on clinical therapeutics, potentially gaining better understanding from early predictors of subsequent manic episode clinical improvement. However, this study has limitations. First, extrapolation of the relationship between early symptom improvement or persistence and subsequent clinical improvement may not necessarily apply to clinical populations that are not under the controlled conditions present in this study. Also, we did not examine whether depressive symptoms (or lack thereof) could predict lithium response. Moreover, the history of mood episodes sequence, which has been proposed as a potential predictor of lithium response (Kukopulos et al., 1980; Grof et al., 1987) was not assessed.
The present study adds an important dimension to this recent literature on early treatment response in BD. We found that improvement in manic symptoms after one week of treatment appears to reliably predict treatment outcome after 28 day of lithium monotherapy. Furthermore, a lack of early improvement predicted subsequent absence of response or remission in this sample. Consistent with past literature on this subject, when potential predictors of early response to lithium were examined-including baseline YMRS, individual YMRS items, sex, age, age at first episode, duration of illness, psychosis, number of previous psychiatric hospitalizations, number of suicide attempts, number of mood and manic episodes, serum lithium levels, and serum uric acid levels-no significant predictors could be identified.
Lithium continues to be the proof of concept agent and widely used worldwide in the treatment of BD. Over the past decade, treatment guidelines for BD have become routinely available. Such guidelines are particularly useful in BD, given the symptomatic and functional complexity of the illness and its chronic course. Here, early improvement in response to lithium mono-therapy in subjects with BD mania predicted later response and remission. Also, most patients who did not show early improvement in response to lithium during the first week of treatment in classic mania showed no response after one month. The present findings may guide clinical decision making process and provides an additional piece of important information that clinicians can use to determine the best possible treatment regimen for their individual patients.
Acknowledgments
Role of funding source
This work was supported by a grant from the Stanley Medical Research Institute, 03T-356 to RMV and the Intramural Research Program of the National Institute of Mental Heath, National Institutes of Health (IRP-NIMH-NIH).
This work was supported by a grant from the Stanley Medical Research Institute, 03T–356 to RMV. We thank also Fapesp (2009/14891–9) and Associação Beneficente Alzira Denise Hertzog da Silva (ABADHS). The authors gratefully acknowledge the staff and patients of the Espirita Hospital of Porto Alegre and Drs Viale, Kapczinski and Hecktheuer.
Footnotes
Trial registration
clinicaltrials.gov Identifier: NCT00560079
Conflict of interest
The authors have no conflict of interest to report.
The authors have no conflict of interest to disclose, financial or otherwise.
References
- American Psychiatric Association. Practice guideline for the treatment of patients with bipolar disorder (revision) The American Journal of Psychiatry. 2002;159 (4 Suppl):1–50. [PubMed] [Google Scholar]
- Cohen S, Khan A, Cox G. Demographic and clinical features predictive of recovery in acute mania. The Journal of Nervous and Mental Disease. 1989;177 (10):638–642. doi: 10.1097/00005053-198910000-00007. [DOI] [PubMed] [Google Scholar]
- Coryell W, et al. Family history and symptom levels during treatment for bipolar I: Affective disorder. Biological Psychiatry. 2000;47:1034–1042. doi: 10.1016/s0006-3223(00)00242-0. [DOI] [PubMed] [Google Scholar]
- Dilsaver SC, et al. The manic syndrome: factors which may predict a patient’s response to lithium, carbamazepine and valproate. Journal of Psychiatry & Neuroscience: JPN. 1993;18 (2):61–66. [PMC free article] [PubMed] [Google Scholar]
- First MB, Spitzer RL, Williams JB. Structured Clinical Interview for DSM-IV Axis I Disorders SCID-I. American Psychiatric Press; Washington, DC: 1996. [Google Scholar]
- Goldberg JF, et al. A history of substance abuse complicates remission from acute mania in bipolar disorder. The Journal of Clinical Psychiatry. 1999;60 (11):733–740. doi: 10.4088/jcp.v60n1103. [DOI] [PubMed] [Google Scholar]
- Goodnick PJ. Predictors of treatment response in mood disorders. American Psychiatric Publishing Inc; 1996. [Google Scholar]
- Grof E, et al. Lithium response and the sequence of episode polarities: preliminary report on a Hamilton sample. Progress in Neuro-Psychopharmacology & Biological Psychiatry. 1987;11 (2–3):199–203. doi: 10.1016/0278-5846(87)90060-1. [DOI] [PubMed] [Google Scholar]
- Grof P. Sixty years of lithium responders. Neuropsychobiology. 2010;62:8–16. doi: 10.1159/000314305. [DOI] [PubMed] [Google Scholar]
- Himmelhoch JM, Garfinkel ME. Sources of lithium resistance in mixed mania. Psychopharmacology Bulletin. 1986;22 (3):613–620. [PubMed] [Google Scholar]
- Houston JP, et al. Early symptom change and prediction of subsequent remission with olanzapine augmentation in divalproex-resistant bipolar mixed episodes. Journal of Psychiatric Research. 2011;45 (2):169–173. doi: 10.1016/j.jpsychires.2010.05.016. [DOI] [PubMed] [Google Scholar]
- Katz MM, Koslow SH, Frazer A. Onset of antidepressant activity: reexamining the structure of depression and multiple actions of drugs. Depression and Anxiety. 1996;4 (6):257–267. doi: 10.1002/(SICI)1520-6394(1996)4:6<257::AID-DA1>3.0.CO;2-9. [DOI] [PubMed] [Google Scholar]
- Keller MB, et al. Differential outcome of pure manic, mixed/cycling, and pure depressive episodes in patients with bipolar illness. JAMA: The Journal of the American Medical Association. 1986;255 (22):3138–3142. [PubMed] [Google Scholar]
- Kemp DE, Johnson E, et al. Clinical utility of early improvement to predict response or remission in acute mania: focus on olanzapine and risperidone. The Journal of Clinical Psychiatry. 2011a doi: 10.4088/JCP.09m05874yel. [DOI] [PubMed] [Google Scholar]
- Kemp DE, Ganocy SJ, et al. Clinical value of early partial symptomatic improvement in the prediction of response and remission during short-term treatment trials in 3369 subjects with bipolar I or II depression. Journal of Affective Disorders. 2011b;130 (1–2):171–179. doi: 10.1016/j.jad.2010.10.026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kessing LV, Hellmund G, Andersen PK. Predictors of excellent response to lithium: results from a nationwide register-based study. International Clinical Psychopharmacology. 2011;26:323–328. doi: 10.1097/YIC.0b013e32834a5cd0. [DOI] [PubMed] [Google Scholar]
- Ketter TA, et al. Rapid antipsychotic response with ziprasidone predicts subsequent acute manic/mixed episode remission. Journal of Psychiatric Research. 2010;44 (1):8–14. doi: 10.1016/j.jpsychires.2009.07.006. [DOI] [PubMed] [Google Scholar]
- Kukopulos A, et al. Course of the manic-depressive cycle and changes caused by treatment. Pharmakopsychiatrie, Neuro-Psychopharmakologie. 1980;13 (4):156–167. doi: 10.1055/s-2007-1019628. [DOI] [PubMed] [Google Scholar]
- Machado-Vieira R, et al. A double-blind, randomized, placebo-controlled 4-week study on the efficacy and safety of the purinergic agents allopurinol and dipyridamole adjunctive to lithium in acute bipolar mania. The Journal of Clinical Psychiatry. 2008;69 (8):1237–1245. doi: 10.4088/jcp.v69n0806. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McElroy SL, et al. Clinical and research implications of the diagnosis of dysphoric or mixed mania or hypomania. The American Journal of Psychiatry. 1992;149 (12):1633–1644. doi: 10.1176/ajp.149.12.1633. [DOI] [PubMed] [Google Scholar]
- Maj M. The effect of lithium in bipolar disorder: a review of recent research evidence. Bipolar Disorders. 2003;5 (3):180–188. doi: 10.1034/j.1399-5618.2003.00002.x. [DOI] [PubMed] [Google Scholar]
- Nagayama H, et al. Prediction of efficacy of antidepressant by 1-week test therapy in depression. Journal of Affective Disorders. 1991;23 (4):213–216. doi: 10.1016/0165-0327(91)90102-x. [DOI] [PubMed] [Google Scholar]
- Nierenberg AA, et al. Early nonresponse to fluoxetine as a predictor of poor 8-week outcome. The American Journal of Psychiatry. 1995;152 (10):1500–1503. doi: 10.1176/ajp.152.10.1500. [DOI] [PubMed] [Google Scholar]
- Secunda SK, et al. Mania. Diagnosis, state measurement and prediction of treatment response. Journal of Affective Disorders. 1985;8 (2):113–121. doi: 10.1016/0165-0327(85)90033-3. [DOI] [PubMed] [Google Scholar]
- Stassen HH, Angst J, Delini-Stula A. Delayed onset of action of anti-depressant drugs? Survey of results of Zurich meta-analyses. Pharmacopsychiatry. 1996;29 (3):87–96. doi: 10.1055/s-2007-979551. [DOI] [PubMed] [Google Scholar]
- Stassen HH, Angst J, Delini-Stula A. Fluoxetine versus moclobemide: cross-comparison between the time courses of improvement. Pharmacopsychiatry. 1999;32 (2):56–60. doi: 10.1055/s-2007-979192. [DOI] [PubMed] [Google Scholar]
- Stassen HH, Delini-Stula A, Angst J. Time course of improvement under antidepressant treatment: a survival-analytical approach. European Neuropsychopharmacology: The Journal of the European College of Neuropsychopharmacology. 1993;3 (2):127–135. doi: 10.1016/0924-977x(93)90264-m. [DOI] [PubMed] [Google Scholar]
- Suppes T, et al. The Texas implementation of medication algorithms: update to the algorithms for treatment of bipolar I disorder. The Journal of Clinical Psychiatry. 2005;66 (7):870–886. doi: 10.4088/jcp.v66n0710. [DOI] [PubMed] [Google Scholar]
- Swann AC, Bowden CL, Morris D, Calabrese JR, Petty F, Small J, Dilsaver SC, Davis JM. Depression during mania. Treatment response to lithium or divalproex. Archives of General Psychiatry. 1997;54 (1):37–42. doi: 10.1001/archpsyc.1997.01830130041008. [DOI] [PubMed] [Google Scholar]
- Szegedi A, et al. Early improvement in the first 2 weeks as a predictor of treatment outcome in patients with major depressive disorder: a meta-analysis including 6562 patients. The Journal of Clinical Psychiatry. 2009;70 (3):344–353. doi: 10.4088/jcp.07m03780. [DOI] [PubMed] [Google Scholar]
- Tohen M, et al. Olanzapine/fluoxetine combination in patients with treatment-resistant depression: rapid onset of therapeutic response and its predictive value for subsequent overall response in a pooled analysis of 5 studies. The Journal of Clinical Psychiatry. 2010;71 (4):451–462. doi: 10.4088/JCP.08m04984gre. [DOI] [PubMed] [Google Scholar]
- Yatham LN, et al. Canadian network for mood and anxiety treatments (CANMAT) and international society for bipolar disorders (ISBD) collaborative update of CANMAT guidelines for the management of patients with bipolar disorder: update 2009. Bipolar Disorders. 2009;11 (3):225–255. doi: 10.1111/j.1399-5618.2009.00672.x. [DOI] [PubMed] [Google Scholar]
- Young RC, et al. A rating scale for mania: reliability, validity and sensitivity. The British Journal of Psychiatry: The Journal of Mental Science. 1978;133:429–435. doi: 10.1192/bjp.133.5.429. [DOI] [PubMed] [Google Scholar]