Abstract
Remarkably little is known about patterns of emergence of specific symptoms in the early course of nonaffective psychotic disorders. Some 159 well-characterized first-episode psychosis patients were categorized into those with: (1) delusions only (n=29, 18.2%); (2) delusions that emerged at least one month before hallucinations (n=31, 19.5%); (3) hallucinations that began at least one month before delusions (n=26, 16.4%); and (4) delusions and hallucinations that emerged concomitantly, within the same month (n=73, 45.9%). These four groups were compared across a number of clinical features, including duration of untreated psychosis, symptom severity, insight, and functioning, while controlling for potential confounders. Patients with delusions and hallucinations emerging within the same month had a shorter duration of untreated psychosis than those in whom one psychotic symptom emerged greater than one month before the other. The delusions-only group had significantly less severe positive, negative, and general psychopathology symptom scores, as well as better social and occupational functioning. Replication and further elucidation of specific patterns of symptom emergence would deepen the field’s understanding of early-course phenomenology, and may inform efforts to improve upon nosology, prognostication, and treatment selection.
Keywords: Delusions, First-episode psychosis, Hallucinations, Insight, Positive symptoms
1. Introduction
The study of first-episode psychosis represents a burgeoning area of research that has not only enhanced our understanding of the early course of schizophrenia and related psychotic disorders, but has also uncovered myriad new questions. One such unresolved issue pertains to the onset and evolution of two key symptoms, delusions and hallucinations. There is a dearth of literature examining patterns of emergence of these symptoms and how varying patterns of onset relate to other clinical features.
Although the mechanism for the formation of delusions is not completely understood, there are two primary hypotheses, the basic reasoning deficit hypothesis and the anomalous experience hypothesis (Maher, 2006). The former, and perhaps less popular, theorizes that delusions arise from a basic deficit in reasoning and illogical thinking. This explanation has been criticized by some because if illogical thinking is enough to cause delusions, there would presumably be more delusional thinking than is seemingly apparent in the general population (Maher, 2006). However, recent epidemiologic research reveals relatively prevalent delusion-like experiences in the general population (Kelleher and Cannon, 2011; van Os et al., 2009), thereby not necessarily ruling out the reasoning deficit hypothesis. On the other hand, the anomalous experience hypothesis implicates hallucinations as an antecedent of delusions, attributing the rise of delusions to an attempt to explain anomalous perceptual experiences. In line with this theory, hallucinations clearly emerge in some first-episode patients before delusions. This pattern of emergence is also observed in non-clinical settings. In a study of adolescents in Maastricht, The Netherlands, persistence of self-reported auditory hallucinations at age 13/14 and again at 15/16 was significantly predictive of delusional ideation at the second time point (De Loore et al., 2011). Smeets and colleagues (2010) found that, in a cohort of German adolescents followed longitudinally, specific types of delusional ideation were more common among those with any form of hallucination; for example, delusional ideas about one’s thoughts being taken away or having messages directed at oneself were more than six times more likely among adolescents endorsing hallucinations. While these theories of delusion formation and the relation between perceptual anomalies and subsequent delusions are informative, there is remarkably little literature investigating the scenario in which hallucination onset occurs after delusion onset.
Understanding patterns of emergence of delusions and hallucinations in psychotic disorders may have relevance to nosology, prognosis, and treatment, just as patterns of symptom emergence in other disease states is important. For example, although memory impairment is a common symptom characteristic of both frontotemporal dementia and Alzheimer’s disease, it develops earlier in the course of Alzheimer’s dementia (Barber et al., 1995). As such, the timing of onset of key symptoms may be important in clarifying the diagnosis between various dementias. Regarding psychosis, although this analysis was primarily exploratory in nature, the clinical implications of characterizing onset of hallucinations and onset of delusions may be relevant with regard to diagnosis, classification, and ultimately treatment of psychotic disorders. In an earlier study involving a subset of the patients in the present analysis (Compton et al., 2011b), the “dose” (i.e., frequency and severity) of initial, untreated hallucinations and “dose” of initial, untreated delusions added substantively, though differentially, to the prediction of early-course symptomatology and functioning, above and beyond the effect of duration of untreated psychosis (DUP).
Exploring differences across psychotic illnesses based on symptom manifestation, Evensen and coworkers (2011) identified two subgroups of “monopositively symptomatic” first-episode psychosis patients with either hallucinations only (n=16) or delusions only (n=106) and examined clinical characteristics among the groups. The much smaller hallucinations-only group was younger and less educated, and had a longer DUP and better insight. Perhaps most interestingly, the hallucinations-only group scored higher on measures of suicidality compared to the delusions-only group, suggesting that the poorer insight in the patients with only delusions was somewhat protective. Though not the focus, that study also made mention of a dual symptom group (n=179), in which patients demonstrated poorer Global Assessment of Functioning (GAF) scores and greater symptom burden as indicated by the Positive and Negative Syndrome Scale (PANSS).
We made use of detailed onset data collected from a relatively large sample of well-characterized first-episode psychosis patients, categorizing them into those with delusions only, those with delusions that began at least one month before the onset of hallucinations, those with an onset of hallucinations at least one month before the emergence of delusions, or those in whom delusions and hallucinations emerged within the same month. These four groups were compared in terms of the following eight dependent variables: DUP; positive, negative, and general psychopathology symptom severity; insight (both patient-rated and researcher-assessed); and global and social/occupational functioning. Because they could influence these dependent variables, gender, family history, and alcohol/cannabis use disorders were examined as potential covariates. The dependent variables were selected as particularly important ones given DUP, symptom severity, insight, and functioning influence treatment response, adherence to treatment, and long-term outcome. By evaluating these variables, we hoped to begin to address whether meaningful clinical differences exist across first-episode psychosis patients based on patterns of emergence of delusions and hallucinations in the early, pre-treatment course.
2. Methods
2.1. Setting and Sample
This analysis was performed using a combined dataset (n=200) that included cross-sectional demographic and symptom-related data collected during six years as part of two research studies on first-episode nonaffective psychosis. While the two projects had different aims—one focused on predictors of treatment delay and DUP (Compton et al., 2008; Compton et al., 2009a; Compton et al., 2009c; Compton et al., 2011a; Compton et al., 2011b), and the other is an ongoing study of the impact of premorbid cannabis use on the early course of psychotic disorders (Compton and Ramsay, 2009; Compton et al., 2009b)—they had identical eligibility criteria, as well as recruitment and data collection procedures. Of the 200 inpatients included in the combined dataset, 41 were excluded from this analysis, as detailed below (see Data Analyses), resulting in a final sample of n=159.
Participants were recruited from an urban, public-sector, university-affiliated hospital (133, 69.2%), the psychiatric emergency room of the same hospital (4, 2.5%), and a public-sector psychiatric crisis center in a neighboring suburban county (22, 13.8%). Individuals who were aged 18–40 years, spoke English, and were admitted for a previously untreated, nonaffective psychotic disorder were eligible. Those with prior outpatient treatment for psychosis lasting >3 months, or prior hospitalization for psychosis more than three months before the index hospitalization, were considered to have had prior treatment for psychosis and were therefore ineligible. Other exclusion criteria included known or suspected mental retardation, a Mini-Mental State Examination (Folstein et al., 1975; Cockrell and Folstein, 1988) score of <24, or a significant medical condition that could compromise ability to participate. Additionally, 13 patients were ineligible to participate secondary to inability to provide written informed consent.
2.2. General Procedures and Measures
Most participants were interviewed during their hospital stay, which typically lasted between 4 and 14 days (mean: 9.3±5.4, median: 8, mode: 8). Referred patients were invited to participate in the study after they were stabilized and had sufficient time to acclimate to the inpatient treatment setting. A detailed research assessment, lasting 3–4 hours for the first study and 6–7 hours for the second, was begun between hospital day 3 and 10 (mean: 7.1±8.7, median: 6, mode: 6). Assessments were divided over two, and when necessary, three days. Both studies included an extensive clinical interview by a trained research assessor to determine the date of onset of delusions, the date of onset of hallucinations, and recent symptom severity and functional status, as described below.
Diagnoses of psychotic disorders and substance use disorders were made using the Structured Clinical Interview for DSM-IV Axis I Disorders (SCID; First et al., 1998) during hospitalization, based on the clinical interview, a chart review, and informants’ reports when available. Regarding the latter, with the research participant’s permission, one or more family members or close friends were invited to participate in a collateral interview (to gather their accounts of the onset of symptoms, DUP, and family history), which was conducted separately. At least one informant was available for 90 (56.6%) participants. Family history of psychotic disorders (among first-degree relatives) was gathered using structured questioning of patients, as well as family members when available. Participants were categorized into having alcohol abuse or dependence, and cannabis abuse or dependence, based on the substance use disorders modules of the SCID (First et al., 1998).
Patients and their respective informants were evaluated using the semi-structured Symptom Onset in Schizophrenia (SOS) inventory (Perkins et al., 2000). Then, dates of onset of delusions and hallucinations, and thus DUP, were derived using a consensus-based, best-estimate approach relying on all available information. Standardized methods were used to resolve ambiguities in obtaining exact dates for the onset of psychotic symptoms, including cross-referencing with milestones and memorable events. From these dates, DUP (weeks from onset of either hallucinations or delusions, or both, to first hospital admission) was derived. Given the expected highly positively skewed distribution of DUP, a transformed DUP variable—log10(DUP+1)— was used in these analyses, as is commonly done in research on this duration measure.
Current and past-month symptom severity was assessed with the PANSS (Kay et al., 1987), which was rated by clinically trained research staff using data gathered from a chart review and an in-depth, semi-structured interview. To assess inter-rater reliability of the PANSS subscale scores, intraclass correlation coefficients (ICCs) were calculated using a two-way mixed (judges fixed) effects analysis of variance (ANOVA) model in which three assessors were the fixed effect while twelve target ratings were the random effect (Shrout and Fleiss, 1979). ICCs were: 0.92 (95% confidence interval (CI): 0.85, 0.96) for the positive subscale, 0.92 (95% CI: 0.86, 0.96) for the negative subscale, and 0.67 (95% CI: 0.42, 0.82) for the general psychopathology subscale. In addition to the three traditional scales of the PANSS, excitement (Lindenmayer et al., 2004) and disorganization (Perlstein et al., 2001) domains were examined, the former including the excitement, hostility, uncooperativeness, and impulse control items, and the latter comprised of the conceptual disorganization, mannerisms and posturing, difficulty in abstract thinking, and poor attention items.
Insight was measured using the 8-item Birchwood Insight Scale (BIS; Birchwood et al., 1994), in addition to the lack of judgment and insight item of the PANSS (Keshavan et al., 2004; Sevy et al., 2004). Higher BIS scores indicate greater insight. The internal consistency coefficient for the BIS was α=0.82 in the overall sample of 200, as well as in the subset of 159 patients involved in this analysis. Scores on the PANSS lack of judgment and insight item range 1–7, with lower scores indicating greater insight.
Global functioning was measured using the GAF scale (Hilsenroth et al., 2000) and the Social and Occupational Functioning Assessment Scale (SOFAS; Goldman et al., 1992), both of which rely on a 100-point continuum divided into 10-point intervals with descriptive anchors.
2.3. Data Analyses
Four mutually exclusive groups were derived from the 159 first-episode patients with available data on the onsets of delusions and hallucinations: (1) those with delusions only (n=29, 18.2%, DEL-ONLY); (2) patients with delusions that began at least one month before the onset of hallucinations (n=31, 19.5%, DEL-HALL); (3) individuals with an onset of hallucinations at least one month before the emergence of delusions (n=26, 16.4%, HALL-DEL); and (4) those in whom delusions and hallucinations emerged concomitantly, within the same month (n=73, 45.9%, DEL+HALL). A one-month cut-point was selected given the difficulty in retrospectively rating the dates of onset of delusions and hallucinations; a cut-point less than this (e.g., one week) was unlikely to provide as accurate classifications. Thirty-seven were excluded due to insufficient data to derive a consensus-based best estimate of the date of onset of delusions or the date of onset of hallucinations. Four patients with only hallucinations were excluded because that sample size was deemed too small to provide reliable statistical estimates.
Comparisons across the four groups in eight continuous dependent variables were made using ANOVAs, and significant F test statistic values were followed by post-hoc tests using the Fisher’s least significant difference procedure for multiple comparisons. For associations in which a potential confounder (from among four examined: gender, family history, alcohol use disorders, and cannabis use disorders) was identified, univariate ANOVAs were followed by multiple linear regressions that accounted for the effect of the third variable. All tests were two-tailed with a criterion for significance set at p<0.05. SPSS 17.0 was used for all analyses.
3. Results
3.1. Sociodemographic Characteristics of the Study Sample
As shown in Table 1, the mean age and years of educational attainment of the study sample were 23.9±5.1 years and 11.7±2.4 years, respectively. The majority of participants were male (119, 74.8%), African American (143, 89.9%), single and never married (144, 90.6%), living with family members prior to hospitalization (103, 64.8%), and unemployed (103, 64.8%). Among the 159 patients, SCID-based psychotic disorder diagnoses were as follows: schizophrenia, paranoid type (77, 48.4%); schizophreniform disorder (27, 17.0%); psychotic disorder not otherwise specified (18, 11.3%); schizoaffective disorder, depressive type (9, 5.7%); schizophrenia, disorganized type (6, 3.8%); schizophrenia, undifferentiated type (6, 3.8%); brief psychotic disorder (6, 3.8%); schizoaffective disorder, bipolar type (5, 3.1%); delusional disorder (3, 1.9%); and schizophrenia, residual type (2, 1.3%). Of note, the three participants with delusional disorder were all within the DEL-ONLY group, though that group included 26 others with diverse primary psychotic disorders.
Table 1.
Sociodemographic Characteristics of the Study Sample (n=159)
| Age at hospitalization, years | 23.9±5.1 |
| Educational attainment, years | 11.7±2.4 |
| Gender, male | 119 (74.8%) |
| Race, African American | 143 (89.9%) |
| Relationship status Single and never married Married or living with a partner Separated, divorced, or widowed |
144 (90.6%) 6 (3.8%) 9 (5.7%) |
| Who the patient lived with during the month prior to hospitalization Parents, siblings, or other family members Alone Friends or roommate Boyfriend, girlfriend, spouse, or partner Homeless Other |
103 (64.8%) 18 (11.3%) 9 (5.7%) 9 (5.7%) 10 (6.3%) 10 (6.3%) |
| Employment status prior to hospitalization, unemployed | 103 (64.8%) |
3.2. Potential Confounders: Gender, Family History, and Alcohol and Cannabis Use Disorders
The four groups did not differ significantly in terms of gender. The proportion of participants with a positive family history of psychosis in a first-degree relative differed significantly across groups; specifically, those in the DEL+HALL group had a lower likelihood (5.9%) of a family history of psychosis than patients in the other three groups (χ2=9.20, df=3, p=0.03). The proportion of participants with a current alcohol use disorder varied across the groups, with those in the DEL-HALL group having a higher rate of alcohol abuse or dependence (43.3%) compared to participants in the other three groups (χ2=9.91, df=3, p=0.02). The proportion of participants with current cannabis abuse or dependence did not differ across the four groups.
To determine whether family history or the presence of an alcohol use disorder was significantly associated with any of the eight dependent variables of interest (and could thus be potential confounders in subsequent analyses), we ran a series of independent samples t-tests. The presence of a family history was associated with log10(DUP+1), such that 27 patients with a family history had a longer DUP than the 146 patients without a family history (t=2.52, df=171, p=0.013). The presence of an alcohol use disorder was associated with GAF and SOFAS scores, such that 53 patients with this comorbidity had a lower GAF score (t=2.40, df=187, p=0.017) and a lower SOFAS score (t=2.54, df=186, p=0.012) than the 136 patients without an alcohol use disorder.
3.3. Association between Group Status and Duration of Untreated Psychosis
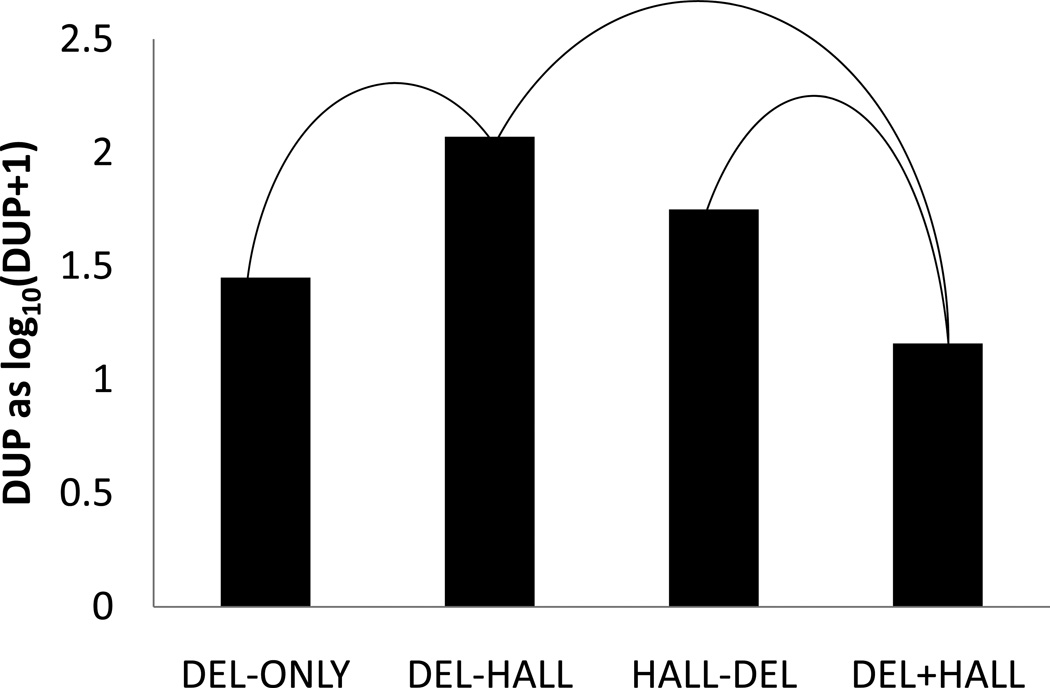
DUP, analyzed as mean of log10(DUP+1), differed significantly across groups (F=14.36; df=3, 153; p<0.001). Post-hoc tests revealed that patients in the DEL+HALL had a shorter DUP than those in HALL-DEL and DEL-HALL groups (Figure 1). Interestingly, patients in the DEL-ONLY group had a shorter DUP than those in the DEL-HALL group. To facilitate interpretation, median DUP values across the four groups were: DEL-ONLY, 12 weeks; DEL-HALL, 94 weeks; HALL-DEL, 43 weeks; and DEL+HALL, 11 weeks.
Figure 1. Mean DUP as log10(DUP+1) across the Four Groups, with Statistically Significant (p<0.05) Differences Indicated.
Median DUP values across the four groups were: 12 weeks, 94 weeks, 43 weeks, and 11 weeks, respectively.
Because family history was also associated with log10(DUP+1), and could thus be a confounder given its association with the main independent variable of interest, we conducted a multiple linear regression (recoding the 4-level factor into three dummy variables). In this model (F=11.21; df=4, 139; p<0.001), those in the DEL-HALL group had a significantly longer DUP than those not in this group (β=0.277, t=2.81, p=0.006), and those in the DEL+HALL group had a significantly shorter DUP than those not in this group (β =−0.233, t=−2.16, p=0.03), while controlling for the effect of family history (β=0.104, t=1.36, p=0.176).
3.4 Association between Group Status and PANSS Subscale Scores
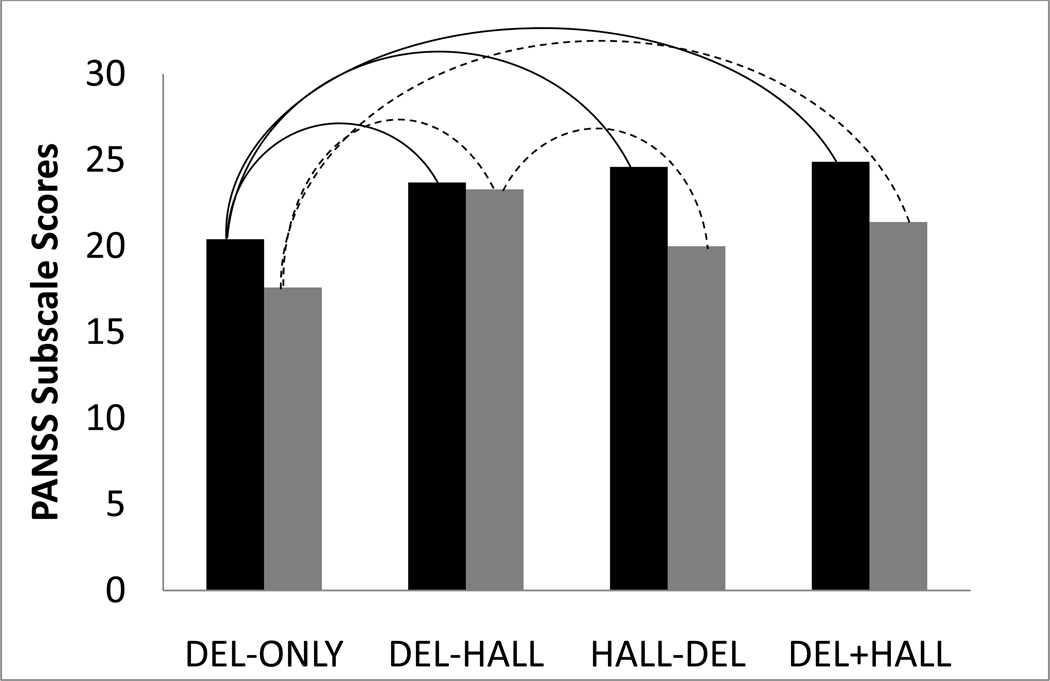
All of the PANSS subscale scores differed significantly across groups (all F-values were significant at p<0.005). As shown in Table 2, patients in the DEL-ONLY group had lower severity scores in all five subscales compared to those in DEL-HALL and DEL+HALL groups. The DEL-ONLY patients also had a lower severity of positive symptoms and disorganization than the HALL-DEL patients. Interestingly, the HALL-DEL group had lower severity of negative symptoms relative to the DEL-HALL group and a lower severity of excitement symptoms compared to the DEL+HALL group. Positive and negative symptom severity is shown graphically in Figure 2. In terms of the single delusions item within the PANSS positive subscale, significant differences were observed across the four groups (F=2.80; df=3, 155; p=0.04); patients in the HALL-DEL group had a greater severity of delusions (5.2±1.2) compared to those in DEL-ONLY (4.6±1.1) and DEL-HALL (4.4±1.1) groups.
Table 2.
PANSS Subscale Scores (Mean±SD) across the Four Groups, n=159
|
A DEL-ONLY n=29 |
B DEL-HALL n=31 |
C HALL-DEL n=26 |
D DEL+HALL n=73 |
Significant Differences |
|
|---|---|---|---|---|---|
| Positive | 20.4±4.0 | 23.7±4.8 | 24.6±4.9 | 24.9±4.5 | A<B,C,D |
| Negative | 17.6±6.3 | 23.3±5.4 | 20.0±5.2 | 21.4±6.7 | A<B,D C<B |
| General Psychopathology | 38.1±9.0 | 44.7±6.5 | 41.6±8.5 | 45.1±8.0 | A<B,D |
| Excitement | 8.4±3.2 | 10.1±2.7 | 9.1±2.8 | 10.6±3.1 | A<B,D C<D |
| Disorganization | 7.7±2.5 | 11.4±3.0 | 10.3±3.3 | 11.2±3.7 | A<B,C,D |
Figure 2. PANSS Positive (Black) and Negative (Gray) Subscale Scores across the Four Groups, with Statistically Significant (p<0.05) Differences Indicated.
3.5. Association between Group Status and Insight
Insight, as assessed by the total score of the self-report BIS, did not differ significantly across groups. Furthermore, the researcher-rated PANSS lack of judgment and insight item score did not differ.
3.6. Association between Group Status and Global and Social/Occupational Functioning
Although GAF scale scores did not differ significantly, SOFAS scores did (F=3.80; df=3, 150; p=0.012), such that patients in the DEL-ONLY group had a higher SOFAS score (median, 45.0) than those in each of the other three groups (medians of 35.0 for DEL-HALL, 37.0 for HALL-DEL, and 36.0 for DEL+HALL).
Because presence of alcohol abuse or dependence was also associated with SOFAS score, and could thus be a confounder given its association with the main independent variable of interest, we conducted a multiple linear regression (again recoding the 4-level factor into three dummy variables). In this model (F=3.94; df=4, 145; p=0.005), those in the DEL-ONLY group had significantly higher SOFAS scores than those not in this group, even while controlling for the effect of the presence of alcohol abuse or dependence (β=−0.156, t=−1.91, p=0.058).
4. Discussion
Several interesting findings emerged from this exploratory analysis that made use of detailed data on the onset not just of psychosis as a syndrome, but of delusions and hallucinations separately. First, among these hospitalized patients with first-episode psychosis, the prevalence of having hallucinations only was very low. Second, the pattern of emergence of delusions and hallucinations is predictive of DUP, which has not been shown previously, such that those with delusions and hallucinations emerging concurrently within the same month have a shorter period of treatment delay than those in which one psychotic symptom emerged greater than one month before the other. Third, PANSS symptom domain scores and social/occupational functioning score differed significantly across groups, with the DEL-ONLY group consistently having lesser severity of symptomatology and impairment. Fourth, despite differences in symptom profiles, insight—both based on self-report and measured objectively by the clinical researcher—did not differ across the four groups. Each of these findings will be discussed briefly in turn.
Interestingly, within our sample of hospitalized patients with primary psychotic disorders, the early course of psychosis was seldom characterized by having hallucinations in isolation of delusions. This may be explained, in part, by the anomalous experience hypothesis noted above, which suggests that delusions may arise in an attempt to explain hallucinatory experiences (Maher 2006); thus, once an individual at imminent risk of developing a psychotic disorder experiences hallucinations, delusional interpretations of those perceptual abnormalities are likely to follow. However, isolated subclinical hallucinatory experiences are known to exist within the general population (Johns and Van Os, 2001; Ohayon, 2000; Tien, 1991; Van Os et al., 2000; Van Os et al., 2009). What differentiates the phenomenology of non-clinical samples with isolated hallucinations from that of patients with psychotic disorders, who apparently rarely have isolated hallucinations, remains a topic for further research.
Regarding DUP, the simultaneous emergence (within the same month) of both delusions and hallucinations is likely more readily noticeable and alarming to the individual and others around him or her, being perceived as requiring more immediate attention. Those with hallucinations emerging before delusions, and those with delusions occurring before hallucinations, had a longer treatment delay, a finding that may be of interest to programs implementing early detection efforts through, for example, public informational campaigns. That is, early intervention approaches may benefit from increasing awareness about delusions and hallucinations separately since one occurring before the other appears to be associated with treatment delay (relative to both occurring simultaneously). As Evensen and associates (2011) concluded, patients who developed dual symptoms of delusions and hallucinations had an overall poorer GAF and worse symptom burden compared to monopositively symptomatic patients, which may support this interpretation of shorter treatment delays in our DEL+HALL group. However, the DEL-ONLY group (which one might expect to have the longest DUP across our four groups) had a shorter DUP than the DEL-HALL group, a finding that is difficult to explain and requires replication.
PANSS symptom domain scores differed significantly across groups, with the DEL-ONLY group having lesser severity not only of positive symptoms (which is partly just a function of the DEL-ONLY group not having hallucinations, an item within the PANSS-positive subscale), but also negative and general psychopathology symptoms (and excitement and disorganization symptoms), as well as social and occupational functioning. This group of 29 patients, which included only three with delusional disorder, would appear to have a more favorable symptom severity profile, which could imply better prognosis. Larger studies that have a sufficient number of patients with hallucinations only could determine if a similar pattern is observed among those patients with primary psychotic disorders experiencing hallucinations in the absence of delusions. Interestingly, based on our comparison of PANSS delusions item severity across the four groups, when delusions begin after (and perhaps in response to, according to the anomalous experience hypothesis of delusion formation) hallucinations, they appear to be more severe than when they begin before hallucinations or in the absence of hallucinations.
Given the presence of delusions across all four groups, the finding that insight did not differ by group suggests the possibility that insight is inherently related to delusional thought content; the pattern of emergence of hallucinations among those with delusions does not appear to be associated with varying levels of insight. With a larger sample size, it would be interesting to know whether insight is better among first-episode patients with hallucinations in the absence of delusions, especially given that we previously found that although the total “dose” of initial, untreated psychosis (delusions + hallucinations) and the “dose” of initial, untreated delusions were not predictive of insight at first hospitalization, the “dose” of initial, untreated hallucinations was (Compton et al., 2011b).
Significant relationships between group status and two covariates—family history of psychosis and the presence of an alcohol use disorder—are difficult to explain. If replicated, the former finding may have implications in further elucidating differences in psychoses among those with and without a family history, similar to known differences by family history status in, for example, age at onset of psychosis (Esterberg et al., 2010; Esterberg and Compton, 2012).
Several methodological limitations must be considered when interpreting this exploratory analysis. First, we could not include among the comparisons a group with hallucinations only given the very low number of patients belonging to that group. Second, we only examined patterns of emergence of delusions and hallucinations, though it would be of equal interest to consider disorganization and negative symptoms; however, this would be very difficult because retrospective dating of the emergence of such symptoms is remarkably difficult because of their oftentimes subtle and insidious onset. Third, the findings may not be generalizable to dissimilar samples given the specific sociodemographic characteristics of the study sample and the fact that all patients were drawn from hospital settings, indicating a severity of illness necessitating inpatient care. Fourth, related to the previous point, we cannot assess how exclusion of patients related to other eligibility criteria (e.g., 13 patients were ineligible to participate because they could not provide written informed consent) may have affected representativeness of our sample or findings derived from it. Despite the limitations, our results suggest that early psychosis research would benefit from other investigations of the patterns of emergence of positive symptoms.
The sequencing of onset of positive symptoms is a complex and varied process about which remarkably little is definitively known. Further elucidation of specific patterns of symptom emergence would deepen the field’s understanding of early-course phenomenology, and may inform efforts to improve upon nosology, prognostication, and treatment selection. Previous studies have explored varying characteristics between groups of patients with differing psychotic symptoms (Evensen et al., 2011) and perhaps different patterns of symptom emergence represents another approach to understanding these highly heterogeneous disorders.
Acknowledgments
Acknowledgment of Funding Support:
This research was supported by grants K23 MH067589 and R01 MH081011 to the first author from the National Institute of Mental Health (NIMH).
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- Barber R, Snowden JS, Craufurd D. Frontotemporal dementia and Alzheimer's disease: Retrospective differentiation using information from informants. Journal of Neurology, Neurosurgery, and Psychiatry. 1995;59:61–70. doi: 10.1136/jnnp.59.1.61. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Birchwood M, Smith J, Drury V, Healy J, Macmillan F, Slade M. A self-report Insight Scale for psychosis: Reliability, validity and sensitivity to change. Acta Psychiatrica Scandanavica. 1994;89:62–67. doi: 10.1111/j.1600-0447.1994.tb01487.x. [DOI] [PubMed] [Google Scholar]
- Cockrell JR, Folstein MF. Mini-Mental State Examination (MMSE) Psychopharmacology Bulletin. 1988;24:689–692. [PubMed] [Google Scholar]
- Compton MT, Chien VH, Leiner AS, Goulding SM, Weiss PS. Mode of onset of psychosis and family involvement in help-seeking as determinants of duration of untreated psychosis. Social Psychiatry and Psychiatric Epidemiology. 2008;43:975–982. doi: 10.1007/s00127-008-0397-y. [DOI] [PubMed] [Google Scholar]
- Compton MT, Gordon TL, Goulding SM, Esterberg ML, Carter T, Leiner AS, Weiss PS, Druss BG, Walker EF, Kaslow NJ. Patient-level predictors and clinical correlates of duration of untreated psychosis among hospitalized first-episode patients. Journal of Clinical Psychiatry. 2011a;72:225–232. doi: 10.4088/JCP.09m05704yel. [DOI] [PubMed] [Google Scholar]
- Compton MT, Gordon TL, Weiss PS, Walker EF. The “doses” of initial, untreated hallucinations and delusions: A proof-of-concept study of enhanced predictors of first-episode symptomatology and functioning relative to duration of untreated psychosis. Journal of Clinical Psychiatry. 2011b;72:1487–1493. doi: 10.4088/JCP.09m05841yel. [DOI] [PubMed] [Google Scholar]
- Compton MT, Goulding SM, Gordon TL, Weiss PS, Kaslow NJ. Family-level predictors and correlates of the duration of untreated psychosis in African American first-episode patients. Schizophrenia Research. 2009a;115:338–345. doi: 10.1016/j.schres.2009.09.029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Compton MT, Kelley ME, Ramsay CE, Pringle M, Goulding SM, Esterberg ML, Stewart T, Walker EF. Association of pre-onset cannabis, alcohol, and tobacco use with the age at onset of prodrome and age at onset of psychosis in first-episode patients. American Journal of Psychiatry. 2009b;166:1251–1257. doi: 10.1176/appi.ajp.2009.09030311. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Compton MT, Ramsay CE. The impact of pre-onset cannabis use on age at onset of prodromal and psychotic symptoms. Primary Psychiatry. 2009;16:35–43. [Google Scholar]
- Compton MT, Ramsay CE, Shim RS, Goulding SM, Gordon TL, Weiss PS, Druss B. Health services determinants of the duration of untreated psychosis among African-American first-episode patients. Psychiatric Services. 2009c;60:1489–1494. doi: 10.1176/ps.2009.60.11.1489. [DOI] [PMC free article] [PubMed] [Google Scholar]
- De Loore E, Gunther N, Drukker M, Feron F, Sabbe B, Deboutte D, van Os J, Myin-Germeys I. Persistence and outcome of auditory hallucinations in adolescence: A longitudinal general population study of 1800 individuals. Schizophrenia Research. 2011;127:252–256. doi: 10.1016/j.schres.2011.01.015. [DOI] [PubMed] [Google Scholar]
- Esterberg ML, Compton MT. Family history of psychosis and its association with age at onset, symptoms, and durations of untreated illness and psychosis in first-episode psychosis patients. Psychiatry Research. 2012 doi: 10.1016/j.psychres.2012.03.001. (in press). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Esterberg ML, Trotman HD, Holtzman C, Compton MT, Walker EF. The impact of a family history of psychosis on age-at-onset and positive and negative symptoms of schizophrenia: A meta-analysis. Schizophrenia Research. 2010;120:121–130. doi: 10.1016/j.schres.2010.01.011. [DOI] [PubMed] [Google Scholar]
- Evensen J, Røssberg JI, Haahr U, ten Velden Hegelstad W, Joa I, Johannessen JO, Langeveld H, Larsen TK, Melle I, Opjordsmoen S, Rund BR, Simonsen E, Sundet K, Vaglum P, Friis S, McGlashan T. Contrasting monosymptomatic patients with hallucinations and delusions in first-episode psychosis patients: A five-year longitudinal follow-up study. Psychopathology. 2011;44:90–97. doi: 10.1159/000319789. [DOI] [PMC free article] [PubMed] [Google Scholar]
- First MB, Spitzer RL, Gibbon M, Williams JBW. Structured Clinical Interview for DSM-IV Axis I Disorders. New York: Biometrics Research Department, New York State Psychiatric Institute; 1998. [Google Scholar]
- Folstein MF, Folstein SE, McHugh PR. “Mini-mental state”: A practical method for grading the cognitive state of patients for the clinician. Journal of Psychiatric Research. 1975;12:189–198. doi: 10.1016/0022-3956(75)90026-6. [DOI] [PubMed] [Google Scholar]
- Goldman HH, Skodal AE, Lave TR. Revising Axis V for DSM-IV: A review of measures of social functioning. American Journal of Psychiatry. 1992;149:1148–1156. doi: 10.1176/ajp.149.9.1148. [DOI] [PubMed] [Google Scholar]
- Hilsenroth MJ, Ackerman SJ, Blagys MD, Baumann BD, Baity MR, Smith SR, Price JL, Smith CL, Heindselman TL, Mount MK, Holdwick DJ. Reliability and validity of DSM-IV Axis V. American Journal of Psychiatry. 2000;157:1858–1863. doi: 10.1176/appi.ajp.157.11.1858. [DOI] [PubMed] [Google Scholar]
- Johns LC, Van Os J. The continuity of psychotic experiences in the general population. Clinical Psychology Review. 2001;21:1125–1141. doi: 10.1016/s0272-7358(01)00103-9. [DOI] [PubMed] [Google Scholar]
- Kay SR, Fizbein A, Opler LA. The Positive and Negative Syndrome Scale (PANSS) for schizophrenia. Schizophrenia Bulletin. 1987;13:261–276. doi: 10.1093/schbul/13.2.261. [DOI] [PubMed] [Google Scholar]
- Kelleher I, Cannon M. Psychotic-like experiences in the general population: Characterizing a high-risk group for psychosis. Psychological Medicine. 2011;4:1–6. doi: 10.1017/S0033291710001005. [DOI] [PubMed] [Google Scholar]
- Keshavan MS, Rabinowitz J, DeSmedt G, Harvey PD, Schooler N. Correlates of insight in first episode psychosis. Schizophrenia Research. 2004;70:187–194. doi: 10.1016/j.schres.2003.11.007. [DOI] [PubMed] [Google Scholar]
- Lindenmayer JP, Brown E, Baker RW, Schuh LM, Shao L, Tohen M, Ahmed S, Stauffer VL. An excitement subscale of the Positive and Negative Syndrome Scale. Schizophrenia Research. 2004;68:331–337. doi: 10.1016/S0920-9964(03)00087-2. [DOI] [PubMed] [Google Scholar]
- Maher BA. The relationship between delusions and hallucinations. Current Psychiatry Reports. 2006;8:179–183. doi: 10.1007/s11920-006-0021-3. [DOI] [PubMed] [Google Scholar]
- Ohayon MM. Prevalence of hallucinations and their pathological associations in the general population. Psychiatry Research. 2000;97:153–164. doi: 10.1016/s0165-1781(00)00227-4. [DOI] [PubMed] [Google Scholar]
- Perkins DO, Leserman J, Jarskog LF, Graham K, Kazmer J, Lieberman JA. Characterizing and dating the onset of symptoms in psychotic illness: The Symptom Onset in Schizophrenia (SOS) inventory. Schizophrenia Research. 2000;44:1–10. doi: 10.1016/s0920-9964(99)00161-9. [DOI] [PubMed] [Google Scholar]
- Perlstein WM, Carter CS, Noll DC, Cohen JD. Relation of prefrontal cortex dysfunction to working memory and symptoms in schizophrenia. American Journal of Psychiatry. 2001;158:1105–1113. doi: 10.1176/appi.ajp.158.7.1105. [DOI] [PubMed] [Google Scholar]
- Sevy S, Nathanson K, Visweswaraiah H, Amador X. The relationship between insight and symptoms in schizophrenia. Comprehensive Psychiatry. 2004;45:16–19. doi: 10.1016/j.comppsych.2003.09.002. [DOI] [PubMed] [Google Scholar]
- Shrout PE, Fleiss JL. Intraclass correlations: Uses in assessing rater reliability. Psychological Bulletin. 1979;86:420–428. doi: 10.1037//0033-2909.86.2.420. [DOI] [PubMed] [Google Scholar]
- Smeets F, Lataster T, Dominguez MD, Hommes J, Lieb R, Wittchen HU, van Os J. Evidence that onset of psychosis in the population reflects early hallucinatory experiences that through environmental risks and affective dysregulation become complicated by delusions. Schizophrenia Bulletin. 2010:1–12. doi: 10.1093/schbul/sbq117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tien AY. Distribution of hallucinations in the population. Social Psychiatry and Psychiatric Epidemiology. 1991;26:287–292. doi: 10.1007/BF00789221. [DOI] [PubMed] [Google Scholar]
- Van Os J, Hanssen M, Bijl RV, Ravelli A. Strauss (1969) revisited: A psychosis continuum in the general population? Schizophrenia Research. 2000;45:11–20. doi: 10.1016/s0920-9964(99)00224-8. [DOI] [PubMed] [Google Scholar]
- Van Os J, Linscott RJ, Myin-Germeys I, Delespaul P, Krabbendam L. A systematic review and meta-analysis of the psychosis continuum: evidence for a psychosis proneness-persistence-impairment model of psychotic disorder. Psychological Medicine. 2009;39:179–195. doi: 10.1017/S0033291708003814. [DOI] [PubMed] [Google Scholar]