Abstract
Objective
To demonstrate a refined cost-estimation method that converts detailed charges for inpatient stays into costs at the department level to enable analyses that can unravel the sources of rapid growth in inpatient costs.
Data Sources
Healthcare Cost and Utilization Project State Inpatient Databases and Medicare Cost Reports for all community, nonrehabilitation hospitals in nine states that reported detailed charges in 2001 and 2006 (n = 10,280,416 discharges).
Study Design
We examined the cost per discharge across all discharges and five subgroups (medical, surgical, congestive heart failure, septicemia, and osteoarthritis).
Data Collection/Extraction Methods
We created cost-to-charge ratios (CCRs) for 13 cost-center or department-level buckets using the Medicare Cost Reports. We mapped service-code-level charges to a CCR with an internally developed crosswalk to estimate costs at the service-code level.
Principal Findings
Supplies and devices were leading contributors (24.2 percent) to the increase in mean cost per discharge across all discharges. Intensive care unit and room and board (semiprivate) charges also substantially contributed (17.6 percent and 11.3 percent, respectively). Imaging and other advanced technological services were not major contributors (4.9 percent).
Conclusions
Payers and policy makers may want to explore hospital stay costs that are rapidly rising to better understand their increases and effectiveness.
Background
Hospital inpatient care, among all settings of care, accounts for the largest proportion of health care spending in the United States (Hartman et al. 2009). The cost of inpatient care increased at an average of 4.4 percent per year between 1997 and 2008, while general inflation was declining (Friedman, Wong, and Steiner 2006; Stranges, Kowlessar, and Elixhauser 2011; U.S. Council of Economic Advisors 2011). Change in the intensity of services—reflected in cost per stay—is the largest component (71 percent) of growth in aggregate inpatient costs (Stranges, Kowlessar, and Elixhauser 2011). An additional 24 percent is accounted for by growth in the population.
Some potential factors in rising inpatient costs have been examined. For example, the cost of inpatient stays grew faster than average for septicemia and osteoarthritis discharges (Stranges, Kowlessar, and Elixhauser 2011). More specifically, the increased use of advanced technological services, such as diagnostic radiology and coronary angioplasties, is often cited as one of the most important drivers of hospital costs and a major contributor to increased spending (Fuchs 1999; Goetghebeur, Forrest, and Hay 2003; Hay 2003; Shactman et al. 2003). Many advances in medical technology have supplemented rather than supplanted existing technologies, resulting in greater overall cost and utilization. For example, the rising number of angioplasties between 1987 and 1995 did not result in fewer coronary bypass procedures, despite a concurrent decline in the incidence of heart disease (Fuchs 1999). The development of more sophisticated imaging procedures, such as computed tomography (CT) scans and magnetic resonance imaging (MRI), likewise may have increased the use of radiological services (Shactman et al. 2003).
Identifying the inpatient services with the most rapidly growing costs may indicate where payers and policy makers need to focus greater attention as they attempt to limit health care inflation. A previous analysis found that hospital costs between 2000 and 2002 grew fastest for diagnostic imaging (36 percent), operating rooms (32 percent), intensive and critical care units (27 percent), and medical supplies (26 percent) (Solucient 2004). The study also found that the costs associated with prescription drugs increased more slowly than other hospital services. Of the seven inpatient service categories examined, only room and board and laboratory costs increased less rapidly than pharmacy expenses.
Developing a clear picture of cost growth is hampered by the available data and resulting variety of approaches used to estimate the cost of hospital resources that are consumed in providing patient care. Some studies have used hospital charges, which represent the amount that was billed to the patient, as a proxy for cost (Schwartz, Young, and Siegrist 1995; Taira et al. 2003); this method is typically an overestimation (Schwartz, Young, and Siegrist 1995).
Other studies have estimated cost using the hospital-level cost-to-charge ratio (CCR), which represents the ratio of operating expenses to gross patient revenues (i.e., before discounts) at the hospital level. Costs can be estimated by multiplying this ratio by charges (Cutler and Huckman 2003). However, hospital-level CCRs may produce measurement error because they do not capture the heterogeneity in CCRs across hospital departments (Song and Friedman 2008). As hospitals frequently subsidize nursing services by including higher markups for procedure-based and other ancillary services, the aggregation of CCRs across departments may distort cost estimates by under- or over-estimating costs for specific departments and specific diagnosis-related groups (Dalton 2007). For example, the national average CCR in 2007 was 0.19 for radiology and 0.56 for routine beds. Applying a single hospital-level CCR may bias estimates for certain services.
An even more robust method to estimate costs may be to use department-level CCRs with detailed charges, or the amount that was billed for a specific hospital service (e.g., laboratory, pharmacy) (Schwartz, Young, and Siegrist 1995; Riley 2009). For example, a previous study that compared different methods found that hospital-level CCRs and hospital total charges provided a poorer basis for estimating costs than department-level CCRs (Schwartz, Young, and Siegrist 1995). Improved accuracy of cost estimates is obtained when CCRs are applied to detailed charges at the department level rather than at the hospital level (Riley 2009). Department-level CCRs provide greater specificity because they capture the variation in low-margin and high-margin services within a hospital.
We demonstrate a new application of a classification method developed by Dalton (2007), which we use for estimating hospital-specific costs of inpatient services when detailed charges and standardized Centers for Medicare & Medicaid Services (CMS) accounting data for developing department-level CCRs are available. After applying the newly developed approach, we assess the contribution of various inpatient service components to growth in the overall cost per discharge for all discharges and for five subgroups of discharges (medical, surgical, congestive heart failure, septicemia, and osteoarthritis).
Methods
Data Sources for Cost Estimates
We obtained hospital data from the Agency for Healthcare Research and Quality (AHRQ) Healthcare Cost and Utilization Project (HCUP) State Inpatient Databases (SID). The HCUP SID contains all-payer information for inpatient stays that currently account for 97 percent of discharges in U.S. community hospitals (Agency for Healthcare Research and Quality 2009). We extracted 2001 and 2006 data for all community, nonrehabilitation hospitals in the nine states that provided four-digit service codes (categories of inpatient services) consistent with the National Uniform Billing Committee's (NUBC) data element specifications for revenue codes (referred to in this article as service codes). We selected these years because they produced the largest number of states with detailed charge data available in both years. The nine states (Kentucky, Maine, Minnesota, Nebraska, New York, Tennessee, Texas, Washington, and West Virginia) represent 22 percent of all discharges from U.S. community, nonrehabilitation hospitals in 2001 and 2006 combined. The number of hospitals included by state and data year can be found in online Appendix SA2.
Study Population
We identified both surgical and medical discharges. We labeled discharges as surgical if they included a major operating procedure. The condition-specific discharges were identified by their principal diagnosis using the Clinical Classification Software (CCS) developed by AHRQ, which groups ICD-9-CM diagnosis codes into clinically meaningfully categories (Elixhauser et al. 1998). We excluded maternal and newborn discharges (major diagnostic categories 14 and 15). Before applying exclusions, the analytic file consisted of 17,311,242 discharges across both years and all nine states.
Service Codes and Charges
We included detailed (service code-level) charges for codes from 011X (room and board) through 095X (other therapeutic services). If the absolute value of the detailed charge for certain advanced technological services (e.g., therapeutic radiology, nuclear medicine, operating room) was less than $10, we assumed this represented a reporting error. In these cases, the charges for the service code were set to missing and a new total charge was calculated; missing charges were also coded as missing.
We included discharges for analysis as long as there was a detailed charge for at least one service code; discharges with only missing values and/or zero value revenue codes were also removed. In addition, based on the definition of outlier values for total charges in HCUP source data, the total charge for included discharges was restricted to between $25 and $1,000,000. Furthermore, we excluded as invalid discharges where the sum of the detailed charges differed from the total charge by at least 2 percent of the total charge for the discharge or by $400 (approximately 2 percent of the average total charge). We removed discharges with reserved service codes according to NUBC because they do not have universal labels that are applicable to all hospitals across the nine states. Finally, we included only discharges that had both department-level and inpatient hospital-level CCRs.
A total of 7,030,826 discharges (40.6 percent of the total analytic file) were excluded for reasons described. The largest share of discharges removed from the analytic file (49 percent) were maternal or newborn cases, which represent a qualitatively different type of discharge and service use compared to other hospital discharges. In addition, a sizeable proportion of discharges that were removed (37 percent) were in hospitals that did not have both an all-payer inpatient CCR and department-level CCR, which may signal data quality issues at those facilities. Our final analysis was conducted on 10,280,416 discharges across both data years.
Estimating Costs
We created year-specific CCRs for 13 cost-center or department-level buckets using a previously described method that was developed for a different purpose (Dalton 2007). The data consisted of all-payer inpatient and outpatient cost and charges reported in Medicare Cost Reports for 34 standard cost centers (e.g., room and board, operating room, radiology, pharmacy) and 56 nonstandard cost centers (e.g., neonatal intensive care unit, MRI, biopsy). Each standard and nonstandard cost center was first mapped to a Medicare Provider and Analysis Review (MedPAR) group based on Dalton (2007). MedPAR aggregates related UB-04 service codes into 28 groups that represent common hospital service centers, such as intensive care unit (ICU), operating room, and physical therapy. We then mapped the MedPAR group to one of 13 cost-center buckets that represented hospital service lines with similar markups.
We used all hospitals with Medicare Cost Reports in either year, regardless of whether a hospital had a cost report available for both years. Within each hospital, we created a CCR for a cost-center bucket by dividing the sum of total costs from the relevant cost centers by the sum of inpatient and outpatient charges for the same cost centers from the Medicare Cost Reports. If a hospital was missing a CCR for one of the 13 buckets, we used in its place one of 3 “backup” cost-center buckets (room and board, operating room, and other ancillary) representing a higher aggregation of the cost centers, as suggested by Koepke (written communication, April 2011). To address potential outliers, we capped nonmissing CCR values for each of the 13 cost-center buckets and 3 backup buckets at a maximum of the 97.5 percentile and a minimum of the 2.5 percentile for the distribution of hospital-level values.
We then obtained cost estimates by applying department-level CCRs to detailed charges. This involved mapping each service code to one of the department-level cost-center buckets through a crosswalk. To develop the crosswalk, we used the method of Dalton (2007) and the MedPAR data dictionary to first associate each of the service codes to the respective MedPAR variable with the same description and then to one of the 13 cost-center buckets. We multiplied each detailed charge by the department-level CCR for the relevant cost-center bucket to calculate a corresponding detailed (service code-level) cost. For example, because we mapped the service code for room and board (semiprivate) 01X to the “routine” cost-center bucket, we multiplied detailed charges for this service by the “routine” department-level CCR to obtain the service code-level cost. We then calculated the total cost for the discharge as the sum of the detailed costs.
For the service-code-to-cost-center crosswalk, we made certain deviations from Dalton (2007) or the MedPAR data dictionary, usually because the service code was not included in one of these sources. Less often, we deviated from the procedure when the service code was considered miscategorized (e.g., 074X electroencephalography [EEG] was classified under laboratory in the MedPAR data dictionary, but we mapped it to cardiology, including EEG).
The aggregation of cost centers into cost-center buckets and the crosswalk of service codes to cost-center buckets are included in online Appendices SA3 and SA4, respectively.
Data Analyses
To describe the volume of spending and growth in spending, we estimated the sum of costs and the mean cost per discharge for both data years across all hospitals and states. We also calculated the dollar amount and percentage of change in the mean cost per discharge between 2001 and 2006. Furthermore, we calculated the portion of the dollar amount change in mean cost per discharge that was contributed by each service code. Finally, for additional context, we calculated the 2006 median cost per discharge (online Appendix SA5) as well as the proportion of discharges in each year that use the top 10 service codes (online Appendix SA6). The gross domestic product (GDP) deflator was used to adjust the 2001 costs to 2006 dollars.
To focus on the detailed services that contributed the most to spending growth, we conducted a two-sample t-test to compare the mean cost at the three-digit service-code level within each discharge type across years. This identified the three-digit service codes that did not significantly change over time and were not further analyzed. We also removed from further analysis three-digit service codes for which the mean cost was zero in both years and the service code represented less than 0.01 percent of the total cost per discharge.
To compare the differences in the service components that contributed the most to spending increases for different types of discharges, we conducted our analyses on six sets of discharges: all discharges, medical discharges, surgical discharges, and discharges for congestive heart failure (CHF), septicemia, and osteoarthritis. The latter three conditions were selected to reduce the heterogeneity among cases. The selected conditions also represented common diagnoses that have rapidly increasing overall costs (Wier, Henke, and Friedman 2010; Stranges, Kowlessar, and Elixhauser 2011). Using all discharges as the referent group, we calculated ratios at the service-code level to compare the change in mean cost per discharge between 2001 and 2006 for the different subsets of discharges.
As a sensitivity analysis, we ran the output for private insurance only to explore potential differences in coding completeness for public payers under prospective payment; however, the results did not substantially change and we report the results for all payers. We also performed a sensitivity analysis to include only hospitals that reported in both data years; this also did not substantially change the results (online Appendix SA7). We performed the analyses with SAS version 9.2 (SAS Institute Inc, Cary, NC, USA).
Results
Cost Growth Components for All Discharges
Between 2001 and 2006, the total cost for hospital inpatient services increased by $18.5 billion (52.0 percent) in inflation-adjusted dollars, for an average annual compounded rate of 8.7 percent. By comparison, the mean cost per discharge for hospital inpatient services increased by $1,938 (25.4 percent) overall during the 5-year period. The difference between the change in the total cost and the mean cost per discharge is accounted for by the increase in discharges, which contributed somewhat less than half (41.1 percent) of the increase in total cost for hospital inpatient services.
Supplies and devices (defined by the NUBC as supply items required for patient care) accounted for 24.2 percent ($469) of the change in mean cost per discharge for all discharges, and ICU accounted for an additional 17.6 percent (see Table 1). The top 10 service codes for all discharges (based on dollar change between 2001 and 2006) together accounted for 91.0 percent of the 2001–2006 change in mean cost per discharge. The largest increase in the share of discharges with at least one of the service codes was observed for CT scan, cardiology, and ICU (online Appendix D).
Table 1.
Hospital Inpatient Services Contributing the Most to the Change in Mean Cost per Discharge, 2001–2006*
| Service Codes with Largest Dollar Change in Mean Cost for All Discharges | All Discharges | Medical Discharges | Surgical Discharges | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Percentage of Discharges with at Least One of the Revenue Codes in 2006 | 2006 Mean Cost | Change in Mean Dollars | Percentage of the Total Change in Mean Dollars | Percentage of Discharges with at Least One of the Revenue Codes in 2006 | 2006 Mean Cost | Change in Mean Dollars | Percentage of the Total Change in Mean Dollars | Percentage of Discharges with at Least One of the Revenue Codes in 2006 | 2006 Mean Cost | Change in Mean Dollars | Percentage of the Total Change in Mean Dollars | |
| 027X—Supplies and devices | 75.1% | $1,332 | $469 | 24.2% | 66.3% | $305 | $16 | 1.7% | 95.4% | $3,698 | $1,494 | 36.2% |
| 020X—ICU | 19.7% | $984 | $341 | 17.6% | 18.1% | $759 | $226 | 23.4% | 23.5% | $1,502 | $601 | 14.6% |
| 012X—Room and board, semi-private | 54.7% | $1,841 | $220 | 11.3% | 55.5% | $1,894 | $198 | 20.5% | 52.9% | $1,718 | $270 | 6.6% |
| 036X—OR services | 33.4% | $729 | $166 | 8.6% | 10.6% | $86 | $23 | 2.4% | 86.0% | $2,210 | $483 | 11.7% |
| 025X—Pharmacy (including 063X) | 95.4% | $851 | $150 | 7.7% | 94.5% | $685 | $118 | 12.2% | 97.6% | $1,235 | $219 | 5.3% |
| 011X—Room and board private (one bed) | 28.6% | $795 | $141 | 7.3% | 26.5% | $741 | $125 | 13.0% | 33.4% | $920 | $174 | 4.2% |
| 021X—Coronary care | 8.2% | $327 | $97 | 5.0% | 7.8% | $279 | $64 | 6.6% | 9.4% | $436 | $173 | 4.2% |
| 030X—Laboratory | 95.9% | $494 | $70 | 3.6% | 96.7% | $461 | $49 | 5.1% | 94.1% | $568 | $117 | 2.8% |
| 035X—CT scan | 32.6% | $183 | $63 | 3.3% | 36.7% | $188 | $60 | 6.2% | 23.2% | $171 | $72 | 1.7% |
| 048X—Cardiology | 23.1% | $238 | $47 | 2.4% | 23.2% | $134 | $19 | 1.9% | 23.0% | $478 | $112 | 2.7% |
| All other service codes | $1,796 | $174 | 9.0% | $1,635 | $67 | 7.0% | $2,232 | $407 | 9.9% | |||
| Total | $9,569 | $1,938 | 100% | $7,166 | $967 | 100% | $15,168 | $4,122 | 100% | |||
2001 costs have been inflation-adjusted to 2006 dollars.
CT, computed tomography; ICU, intensive care unit; OR, operating room.
Cost Growth Components for Medical versus Surgical Discharges
In comparison to all discharges, the top 10 service codes (based on all discharges) accounted for 93.0 percent and 90.1 percent of the change in mean cost per discharge for medical discharges and surgical discharges, respectively.
Over the study period, the contribution of supplies and devices to the change in mean cost per discharge was especially large among surgical discharges in both dollar amounts and percentages, increasing $1,494 and accounting for 36.2 percent of the total change in mean discharge cost (see Table 1). We also examined the results for the individual four-digit service codes under the main supplies and devices category. Other implants (service code 0278) contributed to a substantial portion of the change in the mean cost per discharge for all discharges ($372) and surgical discharges ($1,197). These are described by NUBC as implants other than prosthetic/orthotic devices, pacemaker, and intraocular lenses; the service code includes stents, artificial joints, shunts, grafts, pins, plates, screws, anchors, and radioactive seeds.
Similarly, although the change in mean cost per discharge for operating room (OR) services across all discharges was $166 (accounting for 8.6 percent of the change in mean cost), OR services contributed to a larger portion (11.7 percent) of the change in mean cost per surgical discharge ($483). Medical discharges had only a $23 (2.4 percent) increase in mean cost per discharge for OR services; we did not expect to find any service charges for OR services for medical discharges.1
The cost of room and board (semiprivate) was consistently a major contributor to the change in mean cost per discharge, particularly for all discharges and medical discharges where it accounted for 11.3 percent and 20.5 percent of the change. The three service components of medical discharges of inpatient ICU, room and board (private), and pharmacy costs also contributed disproportionately to the change in mean cost per discharge, accounting for 23.4 percent ($226), 13.0 percent ($125), and 12.2 percent ($118) of medical discharges, respectively. By comparison, these same service code categories played a smaller role in cost growth for surgical discharges and all discharges.
Imaging and other advanced technological diagnostic services generally did not rank in the top 10 service codes with the largest proportion of the change in mean cost. As shown in Table 2, these service codes only contributed 4.9 percent of the total change in mean cost. However, among these types of services, magnetic resonance technology consistently had the largest growth in mean cost per discharge: 59.4 percent increase for all discharges, 49.9 percent increase for medical discharges, and 111.1 percent increase for surgical discharges. Compared with the other advanced technological diagnostic services, CT scans had the largest dollar change in the mean cost per discharge, ranging between $60 and $72 for the three discharge categories.
Table 2.
Change in the Mean Cost per Discharge for Imaging and Other Advanced Technological Diagnostic Services, 2001–2006*
| Service Codes | All Discharges | Medical Discharges | Surgical Discharges | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Percentage of Discharges with at Least One of the Revenue Codes in 2006 | Percentage Change in Mean Dollars | Change in Mean Dollars | Percentage of the Total Change in Mean Dollars | Percentage of Discharges with at Least One of the Revenue Codes in 2006 | Percentage Change in Mean Dollars | Change in Mean Dollars | Percentage of the Total Change in Mean Dollars | Percentage of Discharges with at Least One of the Revenue Codes in 2006 | Percentage Change in Mean Dollars | Change in Mean Dollars | Percentage of the Total Change in Mean Dollars | |
| 0320×Radiology-diagnostic | 72.1% | 4.1% | $5 | 0.2% | 73.5% | −6.1% | −$6 | −0.6% | 68.8% | 17.5% | $27 | 0.7% |
| 0340×Nuclear medicine | 7.1% | 3.1% | $1 | 0.0% | 7.8% | −1.1% | $0 | 0.0% | 5.4% | 25.7% | $4 | 0.1% |
| 0350×CT scan | 32.6% | 52.9% | $63 | 3.3% | 36.7% | 46.6% | $60 | 6.2% | 23.2% | 72.2% | $72 | 1.7% |
| 0400×Imaging Services | 12.7% | 19.0% | $3 | 0.1% | 13.4% | 16.7% | $2 | 0.3% | 11.2% | 25.9% | $3 | 0.1% |
| 0610×Magnetic resonance technology (MRT) | 7.0% | 59.4% | $19 | 1.0% | 8.0% | 49.9% | $20 | 2.0% | 4.6% | 111.1% | $19 | 0.5% |
| 0730×EKG|ECG | 56.0% | 2.2% | $1 | 0.1% | 57.1% | 0.1% | $0 | 0.0% | 53.3% | 7.1% | $3 | 0.1% |
| 0740×EEG | 3.1% | 42.0% | $3 | 0.2% | 3.5% | 42.4% | $3 | 0.4% | 1.9% | 41.2% | $2 | 0.1% |
2001 costs have been inflation-adjusted to 2006 dollars.
CT, computed tomography; ECG and EKG, electrocardiography; EEG, electroencephalography.
Cost Growth Components for Specific Conditions
We also examined the service components contributing to the change in the mean cost per discharge for CHF and septicemia (both medical discharges) and osteoarthritis, which was categorized as a subset of surgical discharges because the prevailing reason for hospitalization for this condition is surgical treatment.2 Figures 1 through 3 show the top 10 service codes with the largest mean cost in 2006 for each condition-specific discharge subset. The size of the bar represents the ratio of the change in mean cost per discharge between 2001 and 2006 for the condition-specific discharge subset compared with all discharges.
Figure 1.
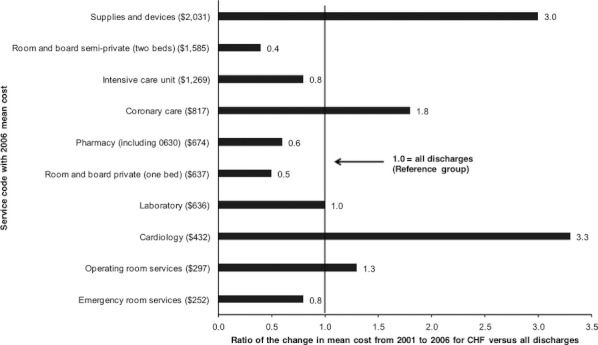
Ratio of the Change in Mean Cost for the Top 10 Service Codes with Statistically Significant Change between 2001 and 2006, Congestive Heart Failure versus All Discharges*Note. *2001 costs have been inflation adjusted to 2006 dollars. CHF, congestive heart failure.
Figure 3.
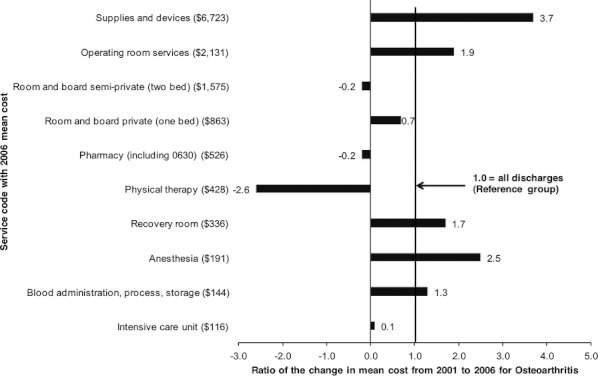
Ratio of the Change in Mean Cost for the Top 10 Service Codes with Statistically Significant Change between 2001 and 2006, Osteoarthritis versus All Discharges*Note. *2001 costs have been inflation adjusted to 2006 dollars.
Among osteoarthritis discharges (Figure 3), the mean cost per discharge ($6,723) in 2006 for top-ranking supplies and devices was 3 times higher than the next most costly service component; in addition, the 2001–2006 increase in the mean cost for supplies and devices among osteoarthritis discharges was 3.7 times higher than among all discharges. Other components for which the change in the mean cost per osteoarthritis discharge was nearly 2 times higher (or more) than all discharges were anesthesia, OR, and recovery-room services.
Among CHF discharges (Figure 1), supplies and devices represented the most costly service component, with a mean cost per discharge of $2,031 in 2006; the 2001–2006 dollar change in the mean cost for supplies and devices per discharge for CHF was 3.0 times higher than that for all discharges. Despite being considered a medical discharge, CHF discharges probably increased because of more frequent use of supplies and devices. For example, cardiac pacemakers and other implants dominated 2006 costs within that service component (data not shown). In addition, the increase in the mean costs for coronary care and cardiology services was 1.8 and 3.3 times higher for CHF than for all discharges.
Among septicemia discharges (Figure 2), ICU ($3,085) and pharmacy ($2,198) were in the top three services by mean cost per discharge in 2006. Furthermore, the 2001–2006 dollar increase in mean cost for ICU and pharmacy per discharge for septicemia was 5.0 to 4.5 times higher than for all discharges. The change in the cost per septicemia discharge versus all discharges was especially dramatic for respiratory services (6.5 times higher), coronary care (4.2 times higher), and laboratory (3.7 times higher). These service-spending patterns may reflect changes in how septicemia has been treated over time or changes in the severity of the patients hospitalized for the condition.
Figure 2.
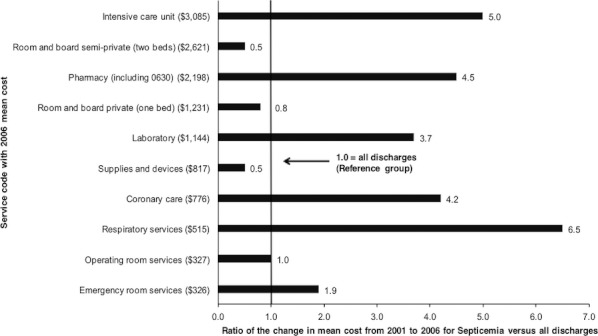
Ratio of the Change in Mean Cost for the Top 10 Service Codes with Statistically Significant Change between 2001 and 2006, Septicemia versus All Discharges*Note. *2001 costs have been inflation adjusted to 2006 dollars.
Discussion
Previous studies have suggested that the increased utilization of imaging services, such as CT scans and MRI, may be responsible for driving the growth in hospital costs. We found that, aside from CT scans, imaging and other advanced technological diagnostic services were not among the top service codes accounting for the largest proportion of the total change in mean cost per discharge. However, supplies and devices—types of medical technology—were key components of increased spending on inpatient services. Across most groups of discharges, supplies and devices contributed the largest proportion of the 2001–2006 change in the mean cost per discharge. Medical technologies are well documented in the extant literature to be an important driver of the growth in health care costs (Hay 2003; Chernew et al. 2004; Callahan 2008).
Several known policy and environmental changes with the potential to affect service-level costs of hospital discharges occurred over the study period. Examples are continued shifts in the delivery of care from the inpatient to the outpatient setting, better hospital defining of diagnosis and procedure codes in response to changes in Medicare payment policies, and refined accounting procedures that better delineated hospital costs within certain departments. However, we generally do not expect these changes to be reflected in the results because the costs would still be associated with the same cost-center buckets. An exception is the shift of certain types of care to outpatient settings, which would alter the clinical composition of inpatient hospital discharges.
Our findings of disproportionate contributions of certain inpatient services to the change in the mean cost per discharge suggests that payers and policy makers might consider looking further into specific inpatient services that could be economized as a way to curb utilization and control costs. The current economic environment has further heightened awareness regarding the evidence base for specific medical services. The significant growth in the mean cost per discharge of supplies and devices raises some questions regarding whether their effectiveness should be examined more closely relative to their cost increases. For example, a recent study highlighted that brain stents, which is a new technology, caused more harm than an aggressive regimen of drugs and behavioral counseling for patients with intracranial arterial stenosis (Chimowitz et al. 2011).
The growth of supplies and devices may also reflect new hospital practices that include the adoption of technologies that have higher ancillary costs for procedures. This too raises the question of whether payers have enough evidence for determining if certain procedures or devices are cost-effective. In terms of unit costs, there is recent evidence of substantial variation among hospitals in reported prices paid for selected implantable medical devices, including cardiac devices (U.S. Government Accountability Office 2012). Hospital bargaining power and differing device preferences among physicians are identified as possible factors.
We further explored the finding that room and board (semiprivate) charges were also a large contributor to cost growth for all discharges, medical discharges, and surgical discharges. Varying increases between 2001 and 2006 in the mean length of stay for each of these groups of discharges (3.7 percent, 0.7 percent, and 10.6 percent, respectively) prevent us from ruling out the notion that cost growth could be the result of longer stays, at least among surgical discharges.
The change in the mean cost per discharge for private rooms also increased significantly. The growth in cost of private beds requires further investigation into who is paying for these services and whether it is justified through improved patient outcomes. Additional investigation is needed to better understand whether this cost growth reflects changing patterns in coverage (e.g., favoring greater privacy), clinical needs (e.g., isolation for more infectious disease), disproportionate increases in unit prices, hospital attempts to market to consumer preferences, or other underlying explanations.
Various factors may contribute to the changes in cost growth for the condition-specific discharges as well as discharges overall. For example, the presumed change in patient acuity over time may result in more severe cases in the inpatient setting, although the exact magnitude of this effect is largely uncertain because empirical evidence in the United States is lacking (Jennings 2008). In addition, the purchasing practices of hospitals may play a role. A recent study found that even though group purchasing organizations (GPOs) exist to provide purchasing power to hospitals, medical device manufacturers pay GPOs for the right to sell their products to hospitals—creating a conflict of interest that may result in higher device costs to hospitals (Litan, Singer, and Birkenbach 2011). The growing amount of medical waste from unused disposables may also be a contributor to the increased use of certain supplies and devices (Chen 2010). These possible explanations are merely speculative, however, because we were unable to look at the role of the change in treatment choices in our study.
There are some limitations to our study. First, although cost-accounting systems—which take into consideration the cost of each service or procedure independently—would provide the most precise estimates of cost, this level of detailed information was unavailable. Although relying on detailed charges and department-level CCRs to estimate costs is preferred, the approach still may bias our estimates either upward or downward, depending on the mix of specific services for the discharge(s). For example it is known that hospitals apply lower markups to expensive medical devices, but have higher markups for routine medical supplies (Dalton, Freeman, and Bragg 2008).
Another limitation is that we accepted the service codes as they were reported by the hospitals because we could not assess the accuracy or compliance with the NUBC manual, whose definitions we used to inform our interpretation. The extent to which states or hospitals within states conform to NUBC specifications is unknown. However, a previous study found that service codes are more likely to reflect actual resource utilization than ICD-9-CM procedure codes because they are automatically generated from accounting charge masters and are not at the discretion of medical coders (Dismuke 2005).
We are also unable to differentiate changes in service utilization from changes in service cost in our analysis of the growth per discharge in inpatient costs. However, to further inform this issue, we provided a crude measure of utilization in 2001 and 2006 based on the percentage of discharges with the service codes for the top 10 services.
Furthermore, we focused only on inpatient discharges—yet we could not distinguish between inpatient and outpatient discharges in some data sources. Therefore, in calculating the CCRs for ancillary cost centers (or departments), we assumed the inpatient CCR to be the same as the overall cost-center CCR (for inpatient and outpatient). Lastly, we only included data from nine states.
In conclusion, the growth in the cost of hospital services is of ongoing concern. Payers and policy makers may want to explore in closer detail the areas of hospital stay costs that are rapidly rising to better understand what is behind the cost increases. Payers might consider negotiating discounts in areas of care that are growing quickly or use contractual tools such as bundled payments to slow cost growth. In addition, certain services could be restricted to cost-effective uses for specific patient populations. Future research that focuses on condition-specific cost trends is needed.
Acknowledgments
Joint Acknowledgment/Disclosure Statement: We would like to acknowledge Minya Sheng for her statistical programming, Robert Houchens for his expert statistical advice, David Koepke for his invaluable insights about service codes, Rosanna Coffey and Mark Smith for reviewing an earlier version of this manuscript, and Linda Lee for editorial assistance. We would also like to acknowledge the following HCUP Partners that made this research possible: the Kentucky Cabinet for Health and Family Services, Maine Health Data Organization, Minnesota Hospital Association, Nebraska Hospital Association, New York State Department of Health, Tennessee Hospital Association, Texas Department of State Health Services, Washington State Department of Health, and West Virginia Health Care Authority.
Disclosures: This study was sponsored by the Agency for Healthcare Research and Quality under contract number HHSA-290-2006-00009-C.
Disclaimers: The views expressed herein are those of the authors. No official endorsement by any agency of the federal or state government is intended or should be inferred.
Notes
All-listed ICD-9-CM procedure codes were used to identify surgical discharges and distinguish them from medical discharges. The top 10 all-listed medical conditions (DXCCS) for discharges that had an OR service code (036X), but were identified as medical discharges, were essential hypertension, fluid and electrolyte disorders, coronary artherosclerosis and other heart disease, substance-related mental disorders, cardiac dysrhythmias, nonhypertensive congestive heart failure, diabetes without complication, chronic obstructive pulmonary disease and bronchiectasis, disorders of lipid metabolism, and deficiency and other anemia. These CCS categories of conditions accounted for nearly a third of medical discharges across both years.
Ninety-seven percent of osteoarthritis discharges in our sample were considered to be surgical, based on the OR major operating procedure indicator variable in the SID. By comparison, only 7 percent of CHF discharges and 10 percent of septicemia discharges were considered surgical.
SUPPORTING INFORMATION
Additional supporting information may be found in the online version of this article:
Appendix SA1: Author Matrix.
Appendix SA2: Number of Hospitals Included by State and Data Year.
Appendix SA3: Mapping of Standard and Nonstandard Cost Centers to Department-Level Buckets.
Appendix SA4: Crosswalk of Service Codes to Cost Center Buckets.
Appendix SA5: Mean Cost per Discharge and Median Cost per Discharge, 2006.
Appendix SA6: Percentage of Discharges That Used the Service Code in 2001 and 2006.
Appendix SA7: Hospital Inpatient Services Contributing the Most to the Change in Mean Cost per Discharge, 2001 to 2006, for Hospitals in Sample for Both Data Years.*
Please note: Wiley-Blackwell is not responsible for the content or functionality of any supporting materials supplied by the authors. Any queries (other than missing material) should be directed to the corresponding author for the article.
References
- Agency for Healthcare Research and Quality. 2009. HCUP Overview [accessed on September 12, 2011]. Available at http://www.hcup-us.ahrq.gov/overview.jsp. [DOI] [PubMed]
- Callahan D. “Health Care Costs and Medical Technology”. In: Crowley M, editor. Birth to Death and Bench to Clinic: The Hastings Center Bioethics Briefing Book for Journalists, Policymakers, and Campaigns. Garrison, NY: The Hastings Center; 2008. pp. 79–82. [Google Scholar]
- Chen I. 2010. “In a World of Throwaways, Making a Dent in Medical Waste” [accessed on June 15, 2012]. Available at http://www.nytimes.com/2010/07/06/health/06waste.html?_r&=1&partner=rss&emc=rss&pagewanted=all.
- Chernew ME, Jacobson PD, Hofer TP, Aaronson KD, Fendrick AM. “Barriers to Constraining Health Care Cost Growth”. Health Affairs. 2004;23(6):122–8. doi: 10.1377/hlthaff.23.6.122. [DOI] [PubMed] [Google Scholar]
- Chimowitz MI, Lynn MJ, Derdeyn CP, Turan TN, Fiorella D, Lane BF, Janis LS, Lutsep HL, Barnwell SL, Waters MF, Hoh BL, Hourihane M, Levy EI, Alexandrov AV, Harrigan MR, Chiu D, Klucznik RP, Clark JM, McDougall CG, Johnson MD, Pride GL, Torbey MT, Zaidat OO, Rumboldt Z, Cloft HJ. “Stenting versus Aggressive Medical Therapy for Intracranial Arterial Stenosis”. New England Journal of Medicine. 2011;365(11):993–1003. doi: 10.1056/NEJMoa1105335. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cutler D, Huckman R. “Technological Development and Medical Productivity: The Diffusion of Angioplasty in New York State”. Journal of Health Economics. 2003;22(2):187–217. doi: 10.1016/S0167-6296(02)00125-X. [DOI] [PubMed] [Google Scholar]
- Dalton K. A Study of Charge Compression in Calculating DRG Relative Weights. Research Triangle Park, NC: RTI International; 2007. [Google Scholar]
- Dalton K, Freeman S, Bragg A. Refining Cost to Charge Ratios for Calculating APC and MS-DRG Relative Payment Rates. Research Triangle Park, NC: RTI International; 2008. [Google Scholar]
- Dismuke CE. “Underreporting of Computed Tomography and Magnetic Resonance Imaging Procedures in Inpatient Claims Data”. Medical Care. 2005;43(7):713–7. doi: 10.1097/01.mlr.0000167175.72130.a7. [DOI] [PubMed] [Google Scholar]
- Elixhauser A, Steiner CA, Whittington C, McCarthy E. Clinical Classifications for Health Policy Research: Hospital Inpatient Statistics. Rockville, MD: Agency for Health Care Policy and Research; 1998. Healthcare Cost and Utilization Project, HCUP Research Note 3. [Google Scholar]
- Friedman BS, Wong HS, Steiner C. “Renewed Growth in Hospital Inpatient Cost Since 1998: Variation across Metropolitan Statistical Areas and Leading Clinical Conditions”. American Journal of Managed Care. 2006;12(3):157–66. [PubMed] [Google Scholar]
- Fuchs VR. “Health Care for the Elderly: How Much? Who Will Pay for It?”. Health Affairs. 1999;18(1):11–21. doi: 10.1377/hlthaff.18.1.11. [DOI] [PubMed] [Google Scholar]
- Goetghebeur M, Forrest S, Hay JW. “Understanding the Underlying Drivers of Inpatient Cost Growth: A Literature Review”. American Journal of Managed Care. 2003;9(Spec No. 1):SP3–12. [PubMed] [Google Scholar]
- Hartman M, Martin A, McDonnell P, Catlin A. “National Health Spending in 2007: Slower Drug Spending Contributes to Lowest Rate of Overall Growth Since 1998”. Health Affairs. 2009;28(1):246–61. doi: 10.1377/hlthaff.28.1.246. [DOI] [PubMed] [Google Scholar]
- Hay JW. “Hospital Cost Drivers: An Evaluation of 1998–2001 State-Level Data”. American Journal of Managed Care. 2003;9(Spec No. 1):SP13–24. [PubMed] [Google Scholar]
- Jennings BM. “Patient Acuity”. In: Hughes RG, editor. Patient Safety and Quality: An Evidence-Based Handbook for Nurses. Rockville, MD: Agency for Healthcare Research and Quality; 2008. pp. 1–8. [PubMed] [Google Scholar]
- Litan RE, Singer HJ, Birkenbach A. “Do Group Purchasing Organizations Achieve the Best Prices for Member Hospitals? An Empirical Analysis of Aftermarket Transactions”. Journal of Contemporary Health Law and Policy. 2011;28(1):23–38. [PubMed] [Google Scholar]
- Riley GF. “Administrative and Claims Records as Sources of Health Care Cost Data”. Medical Care. 2009;47(7 suppl 1):S51–5. doi: 10.1097/MLR.0b013e31819c95aa. [DOI] [PubMed] [Google Scholar]
- Schwartz M, Young DW, Siegrist R. “The Ratio of Costs to Charges: How Good a Basis for Estimating Costs”. Inquiry. 1995;32(4):476–81. [PubMed] [Google Scholar]
- Shactman D, Altman SH, Eilat E, Thorpe KE, Doonan M. “The Outlook for Hospital Spending”. Health Affairs. 2003;22(6):12–26. doi: 10.1377/hlthaff.22.6.12. [DOI] [PubMed] [Google Scholar]
- Solucient. Costs of Inpatient Drugs Rise Less Rapidly Than Other Hospital Services. Evanston, IL: Solucient; 2004. [Google Scholar]
- Song X, Friedman BS. 2008. Calculate Cost Adjustment Factors by APR_DRG and CCS Using Selected States with Detailed Charges [accessed on September 12, 2011]. Available at http://hcup-us.ahrq.gov/reports/methods/2008_04.pdf.
- Stranges E, Kowlessar N, Elixhauser A. 2011. Components of Growth in Hospital Inpatient Costs, 1997–2009. HCUP Statistical Brief #123. Agency for Healthcare Research and Quality [accessed on December 22, 2011]. Available at http://www.hcup-us.ahrq.gov/reports/statbriefs/sb123.jsp.
- Taira D, Seto TB, Siegrist R, Cosgrove R, Berezin R, Cohen DJ. “Comparison of Analytic Approaches for the Economic Evaluation of New Technologies Alongside Multicenter Clinical Trials”. American Heart Journal. 2003;145(3):452–8. doi: 10.1067/mhj.2003.3. [DOI] [PubMed] [Google Scholar]
- U.S. Council of Economic Advisors. Economic Report of the President. Washington, DC: U.S. Government Printing Office; 2011. [Google Scholar]
- U.S. Government Accountability Office. Lack of Price Transparency May Hamper Hospitals' Ability to be Prudent Purchasers of Implantable Medical Devices. Washington, DC: General Accounting Office; 2012. [Google Scholar]
- Wier L, Henke R, Friedman BS. 2010. Diagnostic Groups with Rapidly Increasing Costs, by Payer, 2001–2007. HCUP Statistical Brief #91. Agency for Healthcare Research and Quality [accessed on September 12, 2011]. Available at http://www.hcup-us.ahrq.gov/reports/statbriefs/sb91.pdf.
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


