Abstract
Objective
Child mental health treatment and services research yield more immediate public health benefit when they focus on outcomes of relevance to a broader group of stakeholders. We reviewed all experimental studies of child and adolescent treatment and service effectiveness published in the last 15 years (1996–2011) and compared the distribution and types of outcome domains to a prior review that focused on studies from the prior 15 years (1980–1995).
Method
Studies were included if they focused on children from birth to 18 years of age with specific or general psychiatric conditions, employed randomized designs, and examined intervention effects with a six-month or longer post-treatment assessment in treatment studies or a six-month or longer post-baseline assessment for services studies. Two hundred (n=200) studies met criteria. Reported outcome measures were coded into conceptual categories drawn from the 1980–1995 review.
Results
There was a five-fold increase in the total number of studies (38 versus 200) across the two 15-year time periods, with the largest increase in the number of studies that focused on consumer-oriented outcomes (from 8 to 47 studies, an almost 6-fold increase); two new domains, parent symptoms and health-related outcomes were identified. The majority of studies (95+%) continued to focus on symptoms and diagnoses as an outcome. Impact ratings were higher among studies examining four or more outcomes versus one to two outcomes in all categories with the exception of Posttraumatic Stress Disorder.
Conclusions
Given major shifts in healthcare policy affecting mental health services, the emergence of health and parent-related outcomes as well as greater attention to consumer perspectives parallels emerging priorities in healthcare and can enhance the relevance of child outcome studies for implementation in the real world.
Keywords: child, adolescent, outcomes, treatment, services
The raison d’être for developing effective pediatric mental health treatments and services is to improve children’s mental health outcomes. Yet critical questions about outcomes still elude scrutiny: What constitutes an outcome? How are outcomes conceptualized and assessed? How consistent are outcome domains over time as the evidence base develops? What is the relevance or fit of outcomes to new policy and practice contexts? As the science base on pediatric clinical interventions expands, answers to these questions are needed to provide strategic direction to policy-makers, practitioners, and researchers. This becomes even more important as public demands to move effective interventions out of academia and into the real world increase.
In the first of two papers published in 1996, two authors suggested a conceptual typology, symptoms/diagnoses, functioning, consumer perspectives, environments, and systems (SFCES), as an organizing framework for understanding the emerging knowledge base about child and adolescent mental health outcomes.1 SFCES included the outcome domains of symptoms and diagnoses; functioning and impairment across settings; consumer-oriented perspectives about their experience, (e.g., beliefs, expectations and attitudes of the youth or caregiver); interpersonal and environmental contextual factors (e.g. parenting practices, school climate); and service-related outcomes (e.g., costs, service use, placements, trajectories).
The second of the two original reports included a review of 15 years of treatment and service studies (1980–1995), and categorized the kinds of outcomes represented in those experimental studies according to the typology.2 The impetus for those papers was concern about the narrow focus of pediatric intervention research on a small and limited set of outcomes—largely symptom reduction only—and the likelihood that such a narrow focus might thwart or at least constrain adoption of effective interventions in real world settings.
The present paper is an update of the original review. This review encompasses all experimental and rigorous pediatric treatment and service studies published between 1996 and 2011. Thus both reviews cover a 15-year span. Our primary goal with the current review is to examine changes in the distribution and types of outcomes reflected in these more recent studies and compare these to the original review. Specifically our purpose is to (a) assess whether the distribution of outcomes has changed since the 1990–1995 review; (b) determine whether new outcome types are reflected in the more recent literature; and (c) examine whether studies that include a broader range of outcomes (4 or more) have higher impact ratings than studies with a narrower range (1–2). This last goal is based on a premise that studies encompassing a broader range of outcomes may be more widely read and relevant to the concerns of multiple stakeholders (including consumers and policy makers), thus potentially addressing two impediments to implementation of new practices—lack of awareness and lack of practical applicability.
To provide a context, we first briefly summarize important policy and financing developments in child and adolescent treatment and services since 1996 that may have shaped the focus of the current review. We then explain why a typology of outcomes may be even more useful today than in the past given the current scientific and policy context, which is shaped increasingly by healthcare reform that requires attention to quality indicators and to implementation of effective interventions in healthcare systems.
Policy and Funding Initiatives
A series of Surgeon General’s Reports between 1999 and 2002 including the National Children’s Action Plan,3 followed by the President’s New Freedom Commission Report,4 all highlighted the gap between the growing knowledge base on efficacious and effective interventions and their absence in real world practices. Similar themes from the standpoint of healthcare were encapsulated in a series of Institute of Medicine (IOM) reports published between 1998–2011 on the quality chasm in healthcare. A second theme was the lack of integration of mental health and substance abuse services into health services.5 All of these documents were unanimous in their identification of these two issues—the science to practice gap and the asymmetrical and non-integrative structure of healthcare—as major barriers to improving the outcomes for adults and children with psychiatric conditions.
To support the need for expansion of the scientific knowledge base, the National Institute of Mental Health (NIMH) between 2001 and 2008 published a series of reports focused on bridging the science and service gap.6 These were followed by targeted program announcements and funding from the National Institutes of Health (NIH) and foundations to improve the installation of effective treatments and services in broader systems.7
The reports from NIMH, IOM, and the Surgeon General pointed to disparities in access to services for youth and families, particularly the gap between need for mental health services and receipt. Some positive trends suggest that an increase in access has occurred, moving from the mid-1980s (3%) to 1999 (10%) to 2008 (13%).8–9 This increase in access is suggestive of greater availability of services and perhaps more acceptability among families to seek them—i.e., less stigma. The quality of the services received, however, is uneven at best.10–11
Financing of mental health services has been largely fueled by federally-supported community mental health system of care grants,12 which are now shifting away from communities and towards states.13 The State Children’s Insurance Program for uninsured youth and Medicaid waivers to states covers intensive community-based services, including family support.8 Managed care entities initially covered families with private insurance and now increasingly are managing Medicaid services in a growing number of states.12 Twenty-five years in the making, the Wellstone and Domenici Mental Health Parity Act was passed in 2008. In 2010, the Affordable Health Care for America Act was signed into law. A major objective of it is to enforce the Mental Health Parity and Addiction Equity Act. Both of these pieces of legislation were enacted to offer affordable mental health care, ensure parity in coverage for behavioral health and physical illnesses, and facilitate the co-location of mental health services in health care settings. Another important development is reimbursement for evidence-based treatment by states, private insurers, and the Centers for Medicaid and Medicare Services.8
Undergirding the financing of services has been a solid set of values and principles derived from the system of care movement that began in the mid-1980s.14 An important offshoot of this movement has been a focus on family-directed (e.g., consumer-oriented) services.15 This focus is fortunately scaffolded by the existence of family advocacy organizations now operative in all 50 states.16–18 The increased attention to consumer perspectives, along with mental health parity and more regionalized structures for financing and regulating healthcare19 have created a new context to support consumer activation in healthcare decisions. This is important for both ethical and fiscal reasons: consumer involvement may in some instances prevent the use of unnecessary and costly medical or psychiatric services.5,20–21
Growth in Pediatric Intervention Research
Significant growth in the number of pediatric clinical trials on efficacious and effective treatments began around 1991 when NIMH issued a “National Plan for Research on Child and Adolescent Mental Disorders.” This plan helped to shape the clinical treatment and services research agenda with its emphasis on outcome studies. Accompanied by a general increase in NIH funding, this plan led to a tripling of NIMH funding for children’s treatment and services research between 1991 and 2001.3 Importantly this emphasis on strengthening the evidence base on clinical interventions was designed to address the significant gap between the knowledge base on effective interventions for adults with psychiatric issues vs. children.22 The resulting increase in funding for pediatric mental health treatment and services research led to several major multi-site clinical trials—the first of their kind in child mental health. These included the Multimodal Treatment of Attention-Deficit/Hyperactivity Disorder (ADHD),23–24 the Preschool ADHD trial (PATS),25 followed by the Treatment for Adolescents with Depression Study,26 the Child/Adolescent Anxiety Multimodal Study,27 and Treatment-Resistant Depression.28 All of these studies were notable in advancing knowledge about the comparative effectiveness of medication, psychosocial, or other forms of treatments and services for children and adolescents.
Growth in the number of pediatric treatment and service studies continued until recently, when funding cuts at NIH across the board led to a leveling off of treatment studies.29 Yet there has been a spurt of studies over the past decade fueled by political attention and funding support for science directed at children’s mental health. This body of scientific work has strengthened the evidence for the effectiveness and in some cases cost-effectiveness of clinical interventions for common childhood disorders (i.e., disruptive disorders including ADHD, depression, and anxiety)30–31 and for intensive home- or community-based interventions which are not diagnosis-specific (e.g., Brief Strategic Family Therapy, Functional Family Therapy, Multisystemic Therapy, Multidimensional Treatment Foster Care).32–34
Growth in Implementation of Evidence-based Treatments and Services
Since 2006, more than a dozen states,35 healthcare entities (Kaiser, Value Options) and foundations (William T. Grant, Robert Wood Johnson, Annie E. Casey) are focusing policies and new funding initiatives towards improving implementation of evidence-based treatments and services in larger systems.36–39 However, significant implementation challenges exist,11,40–42 because of insufficient attention to the natural contexts within which the tested interventions will be embedded. Notably, researchers rely on sets of outcomes to establish intervention impact, but these may be irrelevant or tangential to the outcomes of interest to those responsible for implementing these interventions in the real world.11,41–43 The lack of fit between the range and types of outcomes assessed by treatment researchers and the outcome expectancies and accountability standards of those responsible for installing the intervention (i.e., agency directors, state policy leaders) can lead to misunderstandings, wasted efforts, inefficiencies, and implementation failures. Thus, failure to specify and measure a range of outcomes that will be important for the intended end-users can impede implementation of effective interventions.
We undertook the present review with specific attention to the types of outcome domains and their distribution in experimental studies of child and adolescent clinical treatments and services. We were interested in whether the types of outcome domains have changed since 1996, when a spurt of funding for a national plan, and renewed policy emphasis sparked growth in treatment and services research. Our assumption is that a comprehensive typology of outcomes can support more successful implementation by providing “truth in advertising,” providing a blueprint by which researchers and adopter constituents can be fully informed about the range of outcomes associated with specific interventions and thereby attend to an intervention’s fit within different contexts.
Method
A comprehensive search of studies of outcomes associated with 1) medication, psychosocial, or combined treatments for specific disorders, and 2) services for general emotional or behavioral problems was conducted. The methodological approach we undertook was identical to our previous review. To locate studies, three of the authors (Hoagwood, Jensen, and Acri) developed a list of search terms within four categories: symptoms/diagnosis, which included both specific terms to capture treatment studies (e.g. anxiety, manic) and more general mental health keywords to locate service studies (e.g. emotion* or disturb*); treatment (e.g. psychotherapy), experimental design (e.g. randomized controlled trial), and follow-up period (e.g. follow-up). Search terms were then shortened to their base word (e.g. manic instead of manic depression), and an asterisk was added to each word to capture all derivatives of that particular term (e.g. treat* to capture both treatment and treated).
Next, search terms within each of the categories were linked with “or,” and larger categories were linked with “and” to capture studies that included at least one search term from all of the categories (e.g., studies of treatments for anxiety with a follow-up assessment point that used an experimental research design). The search was executed using the PsycINFO and Medline (OVID SP) databases through a university library system. Database search limits included year (1996–2011), children and adolescents 0–18 years of age, and type of article (e.g. randomized controlled trial, meta-analysis, controlled clinical trial).
Inclusion and Exclusion Criteria
Treatment and service studies were included if they met the following criteria: (a) published between 1996 and December 2011; (b) used a randomized experimental design; (c) analyses focused on main treatment or services effects; (d) targeted children between 0–18 years of age (studies that included both adolescents and young adults were included if the mean age of the sample was < 18 years of age); and (e) targeted specific psychiatric disorders as described by the Diagnostic and Statistical Manual of Mental Disorders44 or general mental health conditions (e.g., severe emotional/behavioral problems). Finally, consistent with the original 1990–1995 review, included studies were required to have a six-month or longer post-treatment follow-up assessment for treatment studies, or a six-month or longer post-baseline data point for service studies.
Studies of primary or universal prevention interventions were excluded. Additionally, interventions for substance abuse were included only if both substance abuse and mental health functioning and symptoms were the focus of the intervention.
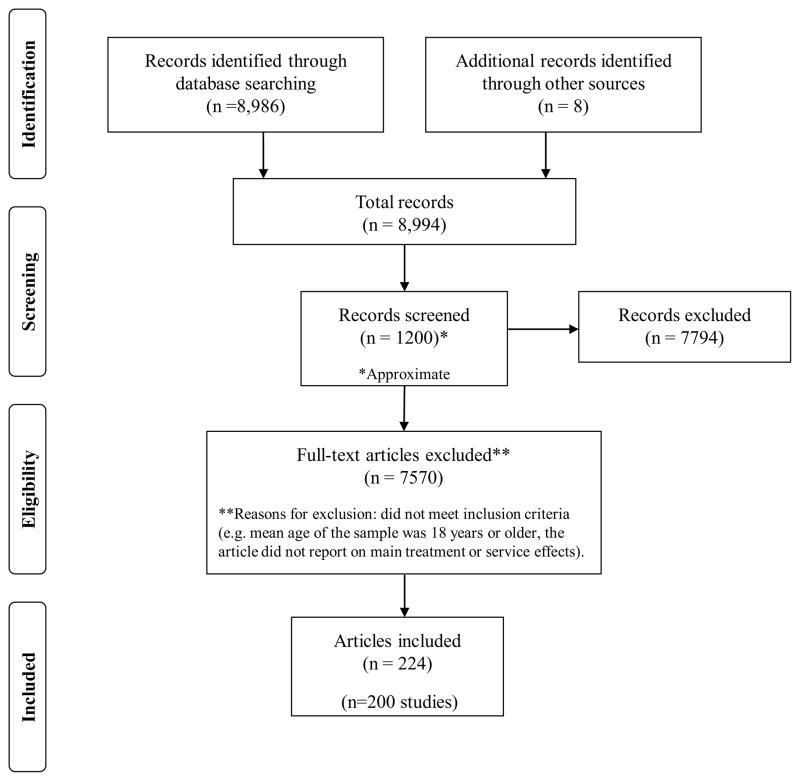
Based on the criteria outlined above, we reviewed approximately 1,200 treatment and service studies. Of these, 200 original studies and 224 total articles met criteria and are included in this review.24,45–267 See Figure 1 for a depiction of our search history, based upon the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA).268 The number of articles exceeds the number of studies because in some cases several articles were published from one study. For a PRISMA checklist, see Table S1, available online.
Figure 1.
Search history and results.
Coding and Analysis
Consistent with the original review, treatment and service studies were grouped separately, and treatment studies were further categorized by symptom or diagnosis, co-morbid conditions, or other. Outcome types were coded applying the original SFCES model: 1) symptoms and diagnoses, 2) functioning/impairment, 3) consumer-oriented perspectives, 4) interpersonal–environmental contexts, and 5) services/systems. Two additional constructs were identified in this review: 6) parent symptoms and 7) health. See Table 1 for a definition of each construct.
Table 1.
Description of Constructs
| Construct | Definition |
|---|---|
| Symptoms and Diagnoses | Symptoms refer to emotions or behaviors a child may exhibit in different settings often leading to a formal psychiatric diagnosis according to the DSM-IV. |
| Parent Symptoms and Diagnoses | Similar to the above, but assigned to the parent or caregiver of the child. |
| Functioning/Impairment | Refers to the capacity to adapt to the demands of home, school, and community. It is a continuous variable that includes competencies, on one end, and impairment on the other. Functioning includes capacities listed in Axis V of DSM-IV. |
| Consumer-oriented Perspectives | Refers to perspectives of parent, caregiver, or youth about quality of life, satisfaction with care, family strain or burden, perceptions and beliefs about treatment, sense of competence, and empowerment, as well as knowledge about psychiatric disorders. |
| Interpersonal and Environmental Contexts | Refers to the broader context that affects children including parenting and the parent/child relationship, parenting styles, family functioning, marital issues, peer-related outcomes, and social-organizational contexts, such as culture and climate. This domain is a counterpoint to functioning as it refers to features of the children’s context that are modifiable. |
| Services/Systems | Refers to the level, type, duration, or change in use of services, restrictiveness, costs, and financing. It can include suspensions, arrests, changes in out of home placements, length of stay, or use of inpatient hospitalization or residential treatment. |
| Health | Refers to physical or biological changes in the child as an outcome of treatment or services, such as height, growth, weight loss, or cortisol levels. Does not include health-related factors that are symptoms of mental health disorders (e.g. weight loss relative to eating disorders). |
Coding proceeded in multiple stages. First, one of the authors (Acri) reviewed each abstract to determine the study’s eligibility based upon the previously-described inclusion and exclusion criteria. Questionable studies (e.g. studies with an unclear follow-up period) were reviewed with two of the other authors (Hoagwood and Jensen) until consensus was met, and decision rules were established.
Then four authors (Acri, Hoagwood, Jensen, Lewandowski) check coded a random selection of 15 articles to categorize each main outcome. Any questionable outcomes were discussed until consensus was reached. One author (Acri) then coded the remaining articles. A kappa statistic was calculated to assess interrater reliability between all four coders. Agreement was 86%, yielding a free-marginal kappa statistic of .84.
We were also interested in whether studies that included a broader range of outcomes had higher impact ratings than studies with a narrower range. Therefore, we examined the number of times articles that examined one or two outcomes vs. four or five outcomes were cited, based upon the Web of Knowledge Platform. Of the 224 articles in our review, 142 examined one or two outcome domains, and 38 studied four or five, yielding a total of 180 articles. However, seven articles from the one to two outcomes group could not be located via Web of Knowledge, leaving a final subsample for the impact analysis of 173 articles (135 examining one to two outcomes, and 38 examining four or five outcomes).
Results
Changes in Number of Studies and Disorder Types
The original review, spanning 15 years from 1980 to 1995, identified 38 treatment or service studies for children and adolescents. By contrast, the present review, spanning the same number of years from 1996 to 2011, identified 200 studies. This represents a 426% or four-fold increase in the total number of studies. The original review identified six primary diagnostic areas as targets for the interventions: 1) behavior problems (conduct disorders, oppositional defiant disorders), 2) attention-deficit hyperactivity disorder, 3) anxiety, 4) depressive, 5) autistic, and 6) eating disorders. Among service studies the categories included therapeutic foster care,269 day treatment,270 and systems of care.271 In the current update, additional diagnostic categories emerged: 1) comorbid conditions (n=12),169,199 including mental health and substance abuse disorders77 and mental health/intellectual functioning;45,125 2) posttraumatic stress disorder and associated symptoms (n=11);82,87,161 3)bipolar disorder (n=1); 177 4) personality disorder (n=1),162 and 5) an “Other” category (n=5) that included Tourette’s Syndrome, tics,264 and risk of self-harm.123 Consistent with the prior review, service studies focused on systems of care65–66 and residential treatment.261 Additionally, a set of studies by Henggeler and colleagues concentrated on the effects of Multisystemic Therapy versus usual care delivered in hospital,133,137 outpatient substance use,130,132 and juvenile justice settings.131 Thus, in comparison to the 1980–1995 review, the current review reveals an expansion of both diagnostic targets and service interventions across settings.
Changes in Outcome Domains
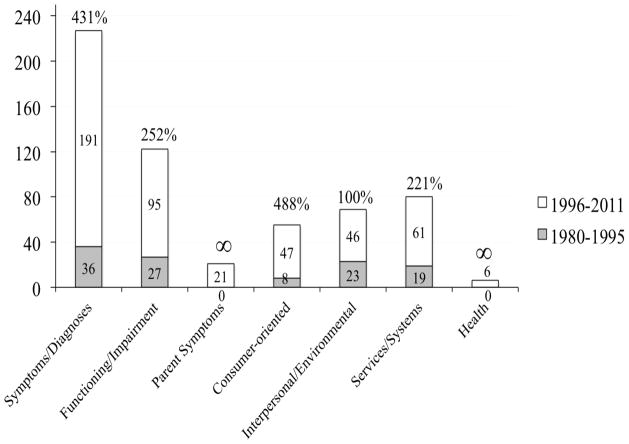
The most common outcome domain assessed across all studies in the current review (as with the original review) was child symptoms and diagnoses accounting for 191 (95.5%) of the total number of studies. This was followed by functioning/impairment (n=95, 47.5%), services and systems (n=61, 30.5%), consumer-oriented perspectives (n=47, 23.5%) and interpersonal-environmental contexts (n=46, 23%). Two new domains emerged: Parent symptoms, specifically related to depression or anxiety (n=21, 10.5%); and health-related outcomes (n=6, 3%) (e.g., height, weight, cortisol levels).
Figure 2 shows the total number of studies in the two reviews (N=238) that targeted all seven domains. The percentage changes in absolute growth of studies across all domains in the two reviews are presented.
Figure 2.
Growth in studies of outcome domains in child psychiatric randomized controlled trials, 1980–2011 (N=238).
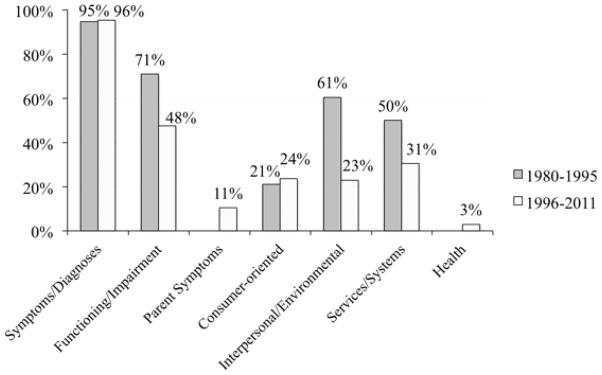
For comparative purposes, Figure 3 graphically presents the proportion of studies from the 1980–1995 and the 1996–2011 reviews that examined each outcome domain, using the total number of studies in each cohort as the denominator. Virtually all studies examined child symptoms/diagnosis outcomes across both reviews, while the relative proportion of studies examining functioning/impairment, interpersonal/environmental, and services/systems domains dropped substantially from the first to the second review. Chi square analysis indicated that these proportional differences in outcome domain distributions were non-random.
Figure 3.
Percent of studies examining 7 outcome domains from 1980–1995 vs. 1996–2011 (N=238).
Impact Factor Ratings
To investigate whether including a broader range of outcomes was associated with higher impact ratings, we examined the impact factors of articles that targeted one or two outcome categories vs. those that targeted four or more. Articles that included one or two outcomes were cited 23.4 times on average; in contrast, articles that studied four or more outcome categories were cited 44.5 times. Impact ratings were higher among studies examining 4 or more outcomes in all categories with the exception of PTSD (only 1 study with 4 or more outcomes) and services (56.45 vs. 44.33). Eating disorders, bipolar, and personality disorders had no studies with 4 or more outcomes. Among the group targeting 4 or more outcomes, ADHD had the highest mean impact rating (M=131.5) followed by autism (M=98.5) and anxiety (M=70.2). Table 2 provides a breakdown of the average number of citations overall, and by diagnosis or services.
Table 2.
Impact Ratings for One/Two vs. Four/Five Outcome Domains
| Category | # of articles (1–2) | Mean times cited (1–2 outcomes) | # of articles (4+) | Mean times cited (4 + outcomes) |
|---|---|---|---|---|
| Attention Deficit Hyperactivity Disorder | 7 | 37.71 | 2 | 131.50 |
| Anxiety | 35 | 30.17 | 5 | 70.20 |
| Autism | 3 | 17.67 | 2 | 98.50 |
| Disruptive Behaviors | 33 | 28.15 | 17 | 37.16 |
| Bipolar | 1 | 0 | 0 | 0 |
| Co-morbid | 6 | 18.50 | 4 | 42.75 |
| Depression | 20 | 41.45 | 2 | 51.50 |
| Eating Disorder | 9 | 16.63 | 0 | 0 |
| Other | 3 | 5.67 | 2 | 53.50 |
| Personality Disorder | 0 | 0 | 0 | 0 |
| Post-Traumatic Stress Disorder | 7 | 28.43 | 1 | 4.0 |
| Service Effectiveness for Emotional/Behavioral Problems | 11 | 56.45 | 3 | 44.33 |
| Total | 135 | 23.40 | 38 | 44.45 |
To look more closely at those articles that included a range of outcomes, we examined those that included four or more. This subgroup of 38 articles is summarized in Table 3. Types of outcomes in this subgroup included child symptoms/diagnoses (100%), followed by consumer-oriented (n=32, 84%) and interpersonal-environmental (n=31, 82%). Functioning/impairment (n=22, 58%), parent symptoms (n=19, 50%) and services/systems (n=16, 42%) were also included but less often. Four (10.5%) targeted health outcomes.
Table 3.
Articles With Four or Five Outcome Domains
| Focus of Study | Symptoms/Diagnoses | Parent Symptoms | Functioning/Impairment | Consumer Perspectives | Interpersonal/Environmental | Services/Systems | Health |
|---|---|---|---|---|---|---|---|
| Attention-Deficit/Hyperactivity Disorder | |||||||
| 1. MTA Cooperative Group (2004a)183 | X | X | X | X | |||
| 2. MTA Cooperative Group (2004b)24 | X | X | X | X | X | ||
| Anxiety | |||||||
| 3. Barrett et al. (2004)57 | X | X | X | X | |||
| 4. Barrett et al. (2005)56 | X | X | X | X | X | ||
| 5. Cobham et al. (1998)86 | X | X | X | X | X | ||
| 6. O’Leary et al. (2009)96 | X | X | X | X | |||
| 7. Silverman et al. (1999)225 | X | X | X | X | |||
| Autism | |||||||
| 8. Kasari et al. (2008)144 | X | X | X | X | |||
| Comorbid | |||||||
| 9. Azrin et al. (2001)50 | X | X | X | X | X | ||
| 10. Bor et al. (2002)69 | X | X | X | X | |||
| 11. Rickards et al. (2009)208 | X | X | X | X | |||
| 12. Roberts et al. (2006)210 | X | X | X | X | |||
| Depression | |||||||
| 13. Clarke et al. (2005)83 | X | X | X | X | X | ||
| 14. Kolko et al. (2000)151 | X | X | X | X | |||
| Disruptive Behaviors | |||||||
| 15. Berkovits et al. (2010)60 | X | X | X | X | |||
| 16. Bradley et al. (2003)71 | X | X | X | X | |||
| 17. Bywater et al. (2009)74 | X | X | X | X | X | ||
| 18. Patterson et al. (2002)202 | X | X | X | X | |||
| 19. Gardner et al. (2006)117 | X | X | X | X | X | ||
| 20. Hutchings et al. (2007)139 | X | X | X | X | |||
| 21. Larsson et al. (2009)156 | X | X | X | X | |||
| 22. Lavigne et al. (2008)158 | X | X | X | X | |||
| 23. Markie-Dadds et al. (2006)171 | X | X | X | X | |||
| 24. Martsch et al. (2005)172 | X | X | X | X | |||
| 25. Nickel et al. (2005)191 | X | X | X | X | |||
| 26. Nickel et al. (2006)192 | X | X | X | X | |||
| 27. Nixon et al. (2004)194 | X | X | X | X | |||
| 28. Sanders et al. (2000a)216 | X | X | X | X | |||
| 29. Sanders et al. (2000b)217 | X | X | X | X | |||
| 30. Sanders et al. (2007)215 | X | X | X | X | |||
| 31. Tucker et al. (1998)243 | X | X | X | X | |||
| 32. Webster-Stratton et al. (1997)254 | X | X | X | X | |||
| Post-Traumatic Stress Disorder | |||||||
| 33. Deblinger et al. (2006)91 | X | X | X | X | X | ||
| Other | |||||||
| 34. Weiss et al. (1999)258 | X | X | X | X | |||
| 35. Weiss et al. (2000)257 | X | X | X | X | |||
| Service Effectiveness for Emotional/Behavioral Problems | |||||||
| 36. Bickman et al. (1997)66 | X | X | X | X | |||
| 37. Bickman et al. (1999)65 | X | X | X | X | X | ||
| 38. Harrington et al. (2000)126 | X | X | X | X | X | ||
Discussion
Our review documents a huge increase in the number of child and adolescent controlled clinical trials since 1996: From 38 total experimental studies of treatments or services between 1980 and 1995 to 200 from 1996 to the present or a 5-fold increase. The growth in knowledge about effective treatments and services for children has been substantial and broad. Thus there now exists a wealth of rigorous research-based knowledge to guide clinicians, payors, policy-makers, and families as they select the type of treatment or service for the most common pediatric problems. Furthermore, through the lens of this classification system, a rational and considered judgment about which treatment or service to provide or to seek (as a family) can be made on the basis of the type of outcome that is sought.
There are several possible reasons for this rapid expansion in pediatric clinical trials. Some of it may have stemmed from growth in pharmaceutical industry trials, subsequent to the pediatric exclusivity option that the Food and Drug Administration (FDA) allowed in 2002. This enabled the industry to retain patent rights on pediatric drug agents for an additional 6 months after going to market, translating into huge potential profits. This rule may account for some of the increase in studies of ADHD and major depressive disorder.
However, most of the studies reflected in the increase are not of medication therapies but rather of psychotherapy or combined trials. Thus the expansion is better understood as a combination of federal leadership and funding initiatives, greater public awareness and demand for research on childhood psychiatric problems, increased availability of diagnostic tools, reduced stigma, support from family advocacy organizations for more research, and the fact that the field was very small to begin with.
The outcome domain showing the largest expansion was consumer-oriented perspectives, from 8 studies in the first review to 47 studies now—almost a 6-fold increase. This expansion also came at a time of increased federal emphasis on patient-centered health care (e.g., the consumer as “true north”272), growth in the mental health family advocacy movement,16 the systems of care movement14,273 and a growing recognition among health care policymakers that health care reform depends in part on consumer ownership.15,19
A surprising and disappointing finding in the review was the decrease in the proportion of studies of services and of studies targeting service-related outcomes. In contrast to the relative expansion of the consumer-oriented domain, studies targeting service system outcomes decreased from 19 of 38 (50%) in the original review to 61 of 200 (31%) in the present review. Furthermore, studies of service effectiveness decreased from 21 studies in the original review to only 12 in the current review, an absolute decrease of 43%.
We can only speculate on the reasons for this. It may be a result of a de-emphasis by granting agencies such as NIMH on service effectiveness studies in favor of basic science studies, and the migration of established services researchers to substance abuse, when the National Institute on Drug Abuse’s (NIDA’s) priorities shifted in the early to mid 2000. The introduction of the dissemination-implementation research agenda within NIH also enabled a number of services researchers to re-engineer their scientific work so that it would be relevant to the new agenda on implementation of effective treatments or service practices, including fidelity, supervision and training.11,22,274
There was also a significant decrease in the proportion of studies targeting interpersonal-environmental contextual outcomes, from 23 out of 38 to 46 out of 200, or 61% to 23%. This too may be a function of the de-emphasis by funding agencies on contextual outcomes, which are more difficult to measure, more difficult to change, and that often require additional resources.
Expansion of Outcome Domains and Outcome Variables
It is noteworthy that new outcomes of interest have emerged in the past 15 years, specifically parent symptoms and health. Parental symptomatology, long-recognized as a crucial component of child well-being, has been explicitly identified and targeted in more recent studies of children’s mental health. Similarly, health-related medical or biological variables have been the focus of attention, along with mental health symptoms, in a few studies looking at overall health changes. The advent of health-related outcomes is especially propitious given the renewed attention to the interface between primary care and behavioral health.19
Consumer outcomes were assessed in a third of all studies, a huge expansion of interest in this domain. Within the consumer-oriented domain, many new variables and metrics have been identified or more finely partitioned, in part because of input from consumer advocacy groups275 and also because of new findings informed by basic cognitive and affective science about factors contributing to children’s overall well-being. These include (a) perceptions and beliefs about treatment, service engagement, satisfaction with services, parental sense of competence, empowerment (n=46, 33.6%); (b) parental stress or strain (n=20, 14.9%), (c) quality of life (n=4, 2.99%), and (d) knowledge about psychiatric disorders (n=4, 2.99%). The parental experience of raising a child with psychiatric issues raises a host of feelings including grief, loss, and changes in expectations about the child’s and parent’s future. The expansion of studies tapping into consumer experiences also reflects an acknowledgement that parent, youth, and family perspectives are critical to improving the context for service delivery—moving beyond mere symptom or functioning improvement to reflect outcomes of importance to consumers about their overall healthcare experiences. We expect this domain will show increasing research interest, as the knowledge base expands on the complex interplay between clinical symptom/functioning outcomes and parent and youth attitudes, beliefs and expectancies.
Our review tallied the number of studies focusing on specific disorder areas. Surprisingly, studies of ADHD, the most common child psychiatric disorder, had very few studies, possibly because of a perceived saturation of studies about ADHD subsequent to the NIMH multisite Multimodal Treatment of Attention-Deficit/Hyperactivity Disorder (MTA) study.23 However, studies of depression, anxiety, and behavior problems showed large increases, perhaps reflecting increased NIH interest spurred by multi-site trials (Treatment for Adolescents with Depression Study [TADS], Child/Adolescent Anxiety Multimodal Study [CAMS], Treatment of SSRI-resistant Depression in Adolescents [TORDIA], etc.). There were 26 depression studies, up from 3 in 1996, likely reflecting improvements in screening tools, availability of feasible measures of adolescent depression for use in community settings, increased recognition of depression as a common reason for school health referrals,276 and acknowledgement that as with adult depression, it is treatable. Studies examining outcomes of anxiety disorders grew from 3 studies in the original review to 46 studies by 2011. Studies of disruptive behavior problems showed the largest absolute growth, from 6 studies between 1980–1995 to 57 studies between 1996 and 2011. Most of these studies used behavior checklists to identify non-diagnosis specific behavior problems.
Range of Outcome Domains
Even though a larger proportion of studies in the current review include outcome categories beyond symptoms and functioning, it is still the case that the majority of studies only examine these two domains. This suggests that our understanding of outcomes is still largely driven by mental health clinicians’ perspectives and needs. Our understanding of other perspectives—policymakers, parents, children (as patients), and others in the environment (teachers, peers) remain rudimentary. So if, as the IOM suggests, healthcare is to be “owned” by the patient/consumer, one would expect that the ultimate aim of healthcare outcomes should be shaped by attention to family and youth perspectives.
Although the addition of new outcome domains may increase the relevance of research findings to consumers and families, new domains raise new problems: how are the domains correlated (if at all), and which domains are most important, when, and why? How should clinicians, healthcare policy makers, and tax-payers grapple with the complex decisions about resources, particularly when treatments yield improvements in one key outcome domain but not in another? Thorough review of these challenges is beyond the scope of this paper, but this type of problem is familiar to clinicians and researchers accustomed to conducting multi-method/multi-trait/multi-informant assessments of children. When the child’s symptoms and impairment are the key outcome domains, different viewpoints about the child’s problems can usually be reconciled. But with the addition of whole new outcome domains (e.g., clinician-defined vs. consumer-defined vs. policy-maker/payer-defined) the stakes may become much higher, with potentially misaligned, contradictory, or even competing outcomes. Unless clinicians, families, policy-makers and researchers acknowledge, measure, study, and seek to understand these new domains together—and develop fully participatory processes for conducting these studies—the yield from the expansion of outcomes will devolve into ambiguity and lost opportunity to make children’s lives better.
New approaches to measurement development promote a more personalized, participatory, and consumer-driven approach. Weisz et al.42 developed and tested a “Top Problems” using a simple metric which taps into the top problems that parents and youth see as the most important to them. Following a diagnostic interview, both children and parents list the problems that are the most concerning to them, and then provide a severity rating (e.g. how much of a problem is it). Then they create a list of their top three problems based on the ranking. The majority of problems identified by caregivers and children matched items on the Child Behavior Checklist and Youth Self Report, suggesting that this client-directed approach is clinically sound.42
Although we attempted to replicate our previous methodology by using the same databases, keywords, and coding, we acknowledge the possibility that the two approaches were not completely identical. It is possible that our current review was more comprehensive, as the three co-authors (Jensen, Hoagwood and Acri) created a thorough list of terms that were modified and rerun several times to ensure we were capturing relevant articles. Further, given that we wanted to replicate the original review, we excluded various additional databases, including the Education Resources Information Center and Web of Knowledge that may have yielded additional studies.
In addition, we recognize that the findings in Table 2 that describe linkages between research papers’ citation counts and the number of outcome domains may confound the relationship between range of outcomes and impact ratings with other factors. We cannot know whether the relationship is cause–effect (unlikely) or is simply a correlation due to some third variable (e.g., study size, funding). Nevertheless it is striking that only 38 of the 200 studies examined 4 or more outcomes, and yet these studies had almost twice the number of citations on average as studies reporting only 1 or 2 outcomes.
For future studies, we cautiously suggest that our field’s next 15 years of child mental health outcome research may benefit by more deliberate examination of the range of outcomes of interest to additional stakeholder groups—not just clinicians and researchers, but also healthcare planners and policy-makers, parent and family advocates, economists, community leaders, teachers, general healthcare providers, etc. To address this broader array of outcomes, researchers will need to obtain input from additional stakeholders to build expanded assessment domains into study design. Furthermore, given various stakeholder perspectives that need to be aligned for an evidence-based practice to be implemented (i.e., trained and willing clinicians, payors, and motivated consumers), inclusion of a broader array of outcome domains may become a sine qua non for evidence-based practice dissemination.
Over the last 15 years our understanding of treatments and services that improve children’s outcomes has become much more elaborated, sophisticated, and nuanced. Our review suggests that improving the quality of services and service systems to support and treat children and families requires a broader public health approach than can be provided by sole reliance on assessment of symptoms, diagnoses, and functioning. More comprehensive outcome assessments are especially critical given new healthcare accountability reforms and pressures on service providers and payors to focus on outcomes and to be held accountable for achieving them. These pressures in turn put additional demands on researchers to develop and test interventions that will not only improve symptoms and functioning but that are cost-effective (service/systems domain), palatable to families (consumer domain), affect the contexts for children so are likely to be sustained (interpersonal–environmental), and affect not only mental health but general health (health domain) as well.
Because some outcomes are likely to be more personally meaningful for parents and families, attention to these kinds of outcomes may help to construct a more ethical science. Parents’ hopes for their children generally extend well beyond mere symptom improvement. Similarly, from a public health and dissemination standpoint, if costs of services are not associated with other outcomes of relevance to consumers and to providers, the services will not be used. Consequently promoting inclusion of policy-relevant, parent and youth-focused, and contextual outcomes are likely to make research findings more responsive to healthcare system changes as well as reinforce an ethical foundation.
Unfortunately, our review indicates persistent unevenness in the types of outcomes targeted by clinical and services researchers, with a continuing skew towards symptoms and functioning only. In addition, little attention has been paid to disorders with potentially life-long disabilities, such as bipolar disorder, comorbidities, and PTSD. The 43% decrease in service effectiveness studies is especially problematic, given the increased need for practical findings that can improve the efficiency and quality of services and the unprecedented rapidity with which healthcare plans and states are revamping their systems to integrate behavioral health.19
While inclusion of consumer-relevant outcomes is growing in acceptance, most studies still tend to neglect outcome domains other than symptoms and functioning, even though inclusion of a wider range of outcomes incites more attention by more diverse groups of stakeholders, including payors, policy-makers, purchasers, and the consumer advocacy community. Until researchers more comprehensively examine the impact of interventions across a broader array of outcomes, the results of such studies will remain tangential.
We suggest that to craft an ethical, relevant, and usable science base, a broader group of stakeholders should work more assiduously together to ensure that the endpoints and outcomes of interest—implementing effective interventions in the real world to reach the greatest number of children in need— shape the selection of outcomes of key studies, especially those that are tax-payer funded. In this way the self-correcting lens of science can be focused on maximizing the utilitarian principle of the greatest good for the greatest number and ensure public health impact for the broadest population of children and families.
Supplementary Material
Clinical Guidance.
Research on outcomes associated with child mental health treatments and services has identified 7 domains. These include symptoms and diagnoses; parent symptoms; functioning; consumer-oriented perspectives; interpersonal and environmental contexts; services and systems; and health. In some cases it may be valuable to select treatments and services that target a broad group of outcome domains to maximize impact.
Consumer-oriented outcomes are a rapidly growing area of study. These types of outcomes are particularly relevant to healthcare policy changes.
Acknowledgments
This research has been supported by the National Institute of Mental Health (NIMH) grant P30 MH090322-01.
Footnotes
Supplemental material cited in this article is available online.
Clinical guidance is available at the end of this article. The authors thank Jennifer Ball of New York University for her contribution to this manuscript.
Disclosure: Dr. Jensen has received honoraria for invited lectures and keynote presentations from Shire, Inc., and Janssen-Cilag, Ltd., as well as charitable donations from Shire, Inc. He is also a part owner and shareholder of CATCH Services, Inc. Drs. Hoagwood, Acri, Olin, and Lewandowski, and Ms. Herman report no biomedical financial interests or potential conflicts of interest.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Contributor Information
Dr. Kimberly Eaton Hoagwood, The New York University School of Medicine
Dr. Peter S. Jensen, The REsource for Advancing Children’s Health (REACH) Institute
Dr. Mary C. Acri, The New York University School of Medicine
Dr. S. Serene Olin, The New York University School of Medicine
Dr. R. Eric Lewandowski, The New York University School of Medicine
Ms. Rachel J. Herman, The New York State Psychiatric Institute
References
- 1.Hoagwood K, Jensen PS, Petti T, Burns BJ. Outcomes of mental health care for children and adolescents: I. A comprehensive conceptual model. J Am Acad Child Adolesc Psychiatry. 1996;36(8):1055–1063. doi: 10.1097/00004583-199608000-00017. [DOI] [PubMed] [Google Scholar]
- 2.Jensen PS, Hoagwood K, Petti T. Outcomes of mental health care for children and adolescents: II. Literature review and application of a comprehensive model. J Am Acad Child Adolesc Psychiatry. 1996;35(8):1064–1077. doi: 10.1097/00004583-199608000-00018. [DOI] [PubMed] [Google Scholar]
- 3.USPHS. Report of the Surgeon General’s Conference on Children’s Mental Health: A National Action Agenda. Rockville, MD: U.S. Department of Health and Human Services Administration, Center for Mental Health Services, National Institutes of Health, National Institute of Mental Health; 2000. [PubMed] [Google Scholar]
- 4.President’s New Freedom Commission on Mental Health. Achieving the Promise: Transforming Mental Health Care in America (DHHS Publication No. SMA-03-3832) Rockville, MD: U.S. Department of Health and Human Services; 2003. [Google Scholar]
- 5.Institute of Medicine. Improving the Quality of Health Care for Mental and Substance-Use Conditions. Washington, DC: National Academies Press; 2005. [PubMed] [Google Scholar]
- 6.National Institute of Mental Health. Treatment research in mental illness; Improving the nation’s public mental health care through NIMH funded interventions research. [Accessed March 21, 2012.];Report of the national advisory mental health council’s workgroup on clinical trials. http://www.nimh.nih.gov/about/advisory-boards-and-groups/namhc/index.shtml. Published 2005.
- 7.National Institute of Mental Health. The road ahead: partnerships to transform services. [Accessed March 21, 2012.];A report by the advisory mental health council’s services research and epidemiology workshop. http://www.nimh.nih.gov/about/advisory-boards-and-groups/namhc/index.shtml. Published 2006.
- 8.Burns BJ. Realizing the dream. Adm Policy Ment Health. 2010;37(1):145–148. doi: 10.1007/s10488-010-0267-2. [DOI] [PubMed] [Google Scholar]
- 9.Wang PS, Demler O, Olfson M, Pincus HA, Wells KB, Kessler RC. Changing profiles of service sectors used for mental health care in the U.S. Am J Psychiatry. 2006;163(7):1187–1198. doi: 10.1176/appi.ajp.163.7.1187. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Bickman L. Death of treatment as usual: an excellent first step on a long road. Clin Psychol. 2002;9(2):195–199. [Google Scholar]
- 11.Bickman L, Hoagwood KE. Introduction to special issue. Adm Policy Ment Health. 2010;37(1–2):4–6. doi: 10.1007/s10488-010-0289-9. [DOI] [PubMed] [Google Scholar]
- 12.Cooper JL, Aratani Y, Knitzer J, et al. Unclaimed Children Revisited: The Status of Children’s Mental Health Policy in the United States. New York, NY: National Center for Children in Poverty, Mailman School of Public Health, Columbia University; 2008. [Google Scholar]
- 13.Substance Abuse and Mental Health Services. [Accessed May 14, 2012.];Administration Implementation cooperative agreements for expansion of the comprehensive community mental health services for children and their families program: system of care expansion implementation cooperative agreements. http://www.samhsa.gov/grants/2012/sm_12_003.aspx.
- 14.Stroul B, Friedman RM. A System of Care for Children and Youth with Severe Emotional Disturbances. Washington, DC: Georgetown University Child Development Center, CASSP Technical Assistance Center; 1986. [Google Scholar]
- 15.Flynn LM. Family perspectives on evidence-based practice. Child Adolesc Psychiatr Clin N Am. 2005;14(2):217–224. doi: 10.1016/j.chc.2004.04.003. [DOI] [PubMed] [Google Scholar]
- 16.Hoagwood KE, Green E, Kelleher K, et al. Family advocacy, support and education in children’s mental health: results of a national survey. Adm Policy Ment Health. 2008;35(1–2):73–83. doi: 10.1007/s10488-007-0149-4. [DOI] [PubMed] [Google Scholar]
- 17.National Alliance on Mental Illness. [Accessed March 22, 2012.];About NAMI. http://www.nami.org/template.cfm?section=About_NAMI.
- 18.National Federation of Families for Children’s Mental Health. [Accessed March 22, 2012.];PSP certification. http://ffcmh.org/who-we-are/chapters-state-organizations.
- 19.Kelleher K. Organizational capacity to deliver effective treatments for children and adolescents. Adm Policy Ment Health. 2010;37(1–2):89–94. doi: 10.1007/s10488-010-0284-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Alegria M, Polo A, Gao S, et al. Evaluation of a patient activation and empowerment intervention in mental health care. Med Care. 2008;46(3):247–256. doi: 10.1097/MLR.0b013e318158af52. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Cortes DE, Mulvaney-Day N, Fortuna L, Reinfeld S, Alergria M. Patient provider communication: understanding the role of patient activation for Latinos in mental health treatment. Health Educ Behav. 2008;36(1):138–154. doi: 10.1177/1090198108314618. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Jensen PS, Weersing R, Hoagwood KE, Goldman E. What is the evidence for evidence-based treatments? A hard look at our soft underbelly. Ment Health Serv Res. 2005;7(1):53–74. doi: 10.1007/s11020-005-1965-3. [DOI] [PubMed] [Google Scholar]
- 23.MTA Cooperative Group. A 14-month randomized clinical trial of treatment strategies for attention-deficit/hyperactivity disorder: the Multimodal Treatment Study of Children with Attention-Deficit Hyperactivity Disorder (MTA Study) Arch Gen Psychiatry. 1999;56:1073–1086. doi: 10.1001/archpsyc.56.12.1073. [DOI] [PubMed] [Google Scholar]
- 24.MTA Cooperative Group. National Institute of Mental Health Multimodal Treatment Study of ADHD follow-up: 24-month outcomes of treatment strategies for attention-deficit/hyperactivity disorder. Pediatrics. 2004;113:754–761. doi: 10.1542/peds.113.4.754. [DOI] [PubMed] [Google Scholar]
- 25.Greenhill L, Kollins S, Abikoff H, et al. Efficacy and safety of immediate-release methylphenidate treatment for preschoolers with ADHD. J Am Acad Child Adolesc Psychiatry. 2006;45(11):1284–1293. doi: 10.1097/01.chi.0000235077.32661.61. [DOI] [PubMed] [Google Scholar]
- 26.Treatment for Adolescents with Depression Study (TADS) Team. Fluoxetine, cognitive-behavioral therapy, and their combination for adolescents with depression: treatment for Adolescents With Depression Study (TADS) randomized controlled trial. JAMA. 2004;292(7):807–820. doi: 10.1001/jama.292.7.807. [DOI] [PubMed] [Google Scholar]
- 27.Compton SN, Walkup JT, Albano AM, et al. Child/Adolescent Anxiety Multimodal Study (CAMS): rationale, design, and methods. Child Adolesc Psychiatry Ment Health. 2010;4:1–15. doi: 10.1186/1753-2000-4-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Brent D, Emslie G, Clarke G, et al. Switching to another SSRI or to venlafaxine with or without cognitive behavioral therapy for adolescents with SSRI-resistant depression: the TORDIA randomized control trial. JAMA. 2008;299(8):901–913. doi: 10.1001/jama.299.8.901. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Cook-Deegan R. Boosting health services research. Science. 2011;333:1384–1385. doi: 10.1126/science.1208201. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Foster EM, Jensen PS, Schlander M, et al. Treatment for ADHD: is more complex treatment cost-effective for more complex cases? Health Serv Res. 2007;42(11):165–182. doi: 10.1111/j.1475-6773.2006.00599.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Jensen PS, Garcia J, Glied S, et al. Cost-effectiveness of ADHD treatments: findings from the MTA Study. Am J Psychiatry. 2005;162:1628–1636. doi: 10.1176/appi.ajp.162.9.1628. [DOI] [PubMed] [Google Scholar]
- 32.Burns BJ, Hoagwood K, Mrazek P. Effective treatment for mental disorders in children and adolescents. Clin Child Fam Psych. 1999;2(4):199–254. doi: 10.1023/a:1021826216025. [DOI] [PubMed] [Google Scholar]
- 33.Burns BJ, Hoagwood K, editors. Community Treatment for Youth: Evidence-Based Interventions for Youth with Severe Emotional and Behavioral Disorders. New York, NY: Oxford University Press; 2002. [Google Scholar]
- 34.Burns BJ, Hoagwood K, editors. Preface. Evidence-based practice part I: a research update. Child Adolesc Psychiatr Clin N Am. 2004;13(4):11–13. [Google Scholar]
- 35.Bruns EJ, Hoagwood KE, Rivard JC, Wotring J, Marsenich L, Carter B. State implementation of evidence-based practice for youths, Part II: recommendations for research and policy. J Am Acad Child Adolesc Psychiatry. 2008;47(5):499–504. doi: 10.1097/CHI.0b013e3181684557. [DOI] [PubMed] [Google Scholar]
- 36.Aarons GA, Sawitzky AC. Organizational culture and climate and mental health provider attitudes toward evidence-based practice. Psychol Serv. 2006;3(1):61–72. doi: 10.1037/1541-1559.3.1.61. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Chambers JA, Power KG, Durham RC. Parental styles and long-term outcome following treatment for anxiety disorders. Clin Psychol Psychother. 2004;11(3):187–198. [Google Scholar]
- 38.Drake RE, Torrey WC, McHugo GJ. Strategies for implementing evidence-based practices in routine mental health settings. Evid Based Ment Health. 2003;6:6–7. doi: 10.1136/ebmh.6.1.6. [DOI] [PubMed] [Google Scholar]
- 39.Glisson C, Landsverk J, Schoenwald S, et al. Assessing the organizational social context (OSC) of mental health services: implications for research and practice. Adm Policy Ment Health. 2008;35(1–2):98–113. doi: 10.1007/s10488-007-0148-5. [DOI] [PubMed] [Google Scholar]
- 40.Atkins MS, Hoagwood KE, Kutash K, Seidman E. Toward the integration of education and mental health in schools. Adm Policy Ment Health. 2010;37(1–2):40–47. doi: 10.1007/s10488-010-0299-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Chorpita BF, Daleiden EL. Mapping evidence-based treatments for children and adolescents: application of the distillation and matching model to 615 treatments from 322 randomized trials. J Consult Clin Psychol. 2009;77(3):566–579. doi: 10.1037/a0014565. [DOI] [PubMed] [Google Scholar]
- 42.Weisz JR, Chorpita BF, Frye A, et al. Youth top problems: using idiographic, consumer-guided assessment to identify treatment needs and track change during psychotherapy. J Consult Clin Psychol. 2011;79(3):369–380. doi: 10.1037/a0023307. [DOI] [PubMed] [Google Scholar]
- 43.Schoenwald SK, Hoagwood K. Effectiveness, transportability, and dissemination of interventions: what matters when? Psychiatr Serv. 2001;52(9):1190–1197. doi: 10.1176/appi.ps.52.9.1190. [DOI] [PubMed] [Google Scholar]
- 44.American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders. 4. Washington, DC: American Psychiatric Association; 2000. text rev. [Google Scholar]
- 45.Aman MG, Armstrong S, Buican B, Sillick T. Four-year follow-up of children with low intelligence and ADHD: a replication. Res Dev Disabil. 2002;23(2):119–134. doi: 10.1016/s0891-4222(02)00090-2. [DOI] [PubMed] [Google Scholar]
- 46.Aman MG, Pejeau C, Osborne P, Rojahn J, Handen B. Four-year follow-up of children with low intelligence and ADHD. Res Dev Disabil. 1996;17(6):417–432. doi: 10.1016/s0891-4222(96)00023-6. [DOI] [PubMed] [Google Scholar]
- 47.Asarnow JR, Jaycox LH, Tang L, et al. Long-term benefits of short-term quality improvement interventions for depressed youths in primary care. Am J Psychiatry. 2009;166(9):1002–1010. doi: 10.1176/appi.ajp.2009.08121909. [DOI] [PubMed] [Google Scholar]
- 48.Asbahr FR, Castillo AR, Ito LM, Latorre M, Moreira MN, Lotufo-Neto F. Group cognitive-behavioral therapy versus Sertraline for the treatment of children and adolescents with obsessive-compulsive disorder. J Am Acad Child Adolesc Psychiatry. 2005;44(11):1128–1136. doi: 10.1097/01.chi.0000177324.40005.6f. [DOI] [PubMed] [Google Scholar]
- 49.Augimeri LK, Farrington DP, Koegl CJ, Day DM. The SNAP Under 12 Outreach Project: effects of a community based program for children with conduct problems. J Child Fam Stud. 2007;16(6):799–807. [Google Scholar]
- 50.Azrin NH, Donohue B, Teichner GA, Crum T, Howell J, DeCato LA. A controlled evaluation and description of individual-cognitive problem solving and family-behavior therapies in dually-diagnosed conduct-disordered and substance-dependent youth. J Child Adolesc Subst Abuse. 2001;11(1):1–43. [Google Scholar]
- 51.Balle M, Tortella-Feliu M. Efficacy of a brief school-based program for selective prevention of childhood anxiety. Anxiety Stress Coping. 2010;23(1):71–85. doi: 10.1080/10615800802590652. [DOI] [PubMed] [Google Scholar]
- 52.Barker ED, Vitaro F, Lacourse E, Fontaine NMG, Carbonneau R, Tremblay RE. Testing the developmental distinctiveness of male proactive and reactive aggression with a nested longitudinal experimental intervention. Aggress Behav. 2010;36(2):127–140. doi: 10.1002/ab.20337. [DOI] [PubMed] [Google Scholar]
- 53.Barrera M, Biglan A, Taylor TK, et al. Early elementary school intervention to reduce conduct problems: a randomized trial with Hispanic and non-Hispanic children. Prev Sci. 2002;3(2):83–94. doi: 10.1023/a:1015443932331. [DOI] [PubMed] [Google Scholar]
- 54.Barrett PM. Evaluation of cognitive-behavioral group treatments for childhood anxiety disorders. J Clin Child Adolesc Psychol. 1998;27(4):459–468. doi: 10.1207/s15374424jccp2704_10. [DOI] [PubMed] [Google Scholar]
- 55.Barrett PM, Dadds MR, Rapee RM. Family treatment of childhood anxiety: A controlled trial. J Consult Clin Psychol. 1996;64(2):333–342. doi: 10.1037//0022-006x.64.2.333. [DOI] [PubMed] [Google Scholar]
- 56.Barrett P, Farrell L, Dadds M, Boulter N. Cognitive-behavioral family treatment of childhood obsessive-compulsive disorder: long-term follow-up and predictors of outcome. J Am Acad Child Adolesc Psychiatry. 2005;44(10):1005–1014. doi: 10.1097/01.chi.0000172555.26349.94. [DOI] [PubMed] [Google Scholar]
- 57.Barrett P, Healy-Farrell L, March JS. Cognitive-behavioral family treatment of childhood obsessive-compulsive disorder: a controlled trial. J Am Acad Child Adolesc Psychiatry. 2004;43(1):46–62. doi: 10.1097/00004583-200401000-00014. [DOI] [PubMed] [Google Scholar]
- 58.Barrington J, Prior M, Richardson M, Allen K. Effectiveness of CBT versus standard treatment for childhood anxiety disorders in a community clinic setting. Behav Change. 2005;22(1):29–43. [Google Scholar]
- 59.Beidel DC, Turner SM, Morris TL. Behavioral treatment of childhood social phobia. J Consult Clin Psychol. 2000;68(6):1072–1080. [PubMed] [Google Scholar]
- 60.Berkovits MD, O’Brien KA, Carter CG, Eyberg SM. Early identification and intervention for behavior problems in primary care: a comparison of two abbreviated versions of parent-child interaction therapy. Behav Ther. 2010;41(3):375–387. doi: 10.1016/j.beth.2009.11.002. [DOI] [PubMed] [Google Scholar]
- 61.Bernat DH, August GJ, Hektner JM, Bloomquist ML. The Early Risers preventive intervention: testing for six-year outcomes and mediational processes. J Abnorm Child Psychol. 2007;35(4):605–617. doi: 10.1007/s10802-007-9116-5. [DOI] [PubMed] [Google Scholar]
- 62.Bernstein GA, Bernat DH, Victor AM, Layne AE. School-based interventions for anxious children: 3-, 6-, and 12-month follow-ups. J Am Acad Child Adolesc Psychiatry. 2008;47(9):1039–1047. doi: 10.1097/CHI.ob013e31817eecco. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Bernstein GA, Hektner JM, Borchardt CM, McMillan MH. Treatment of school refusal: one-year follow-up. J Am Acad Child Adolesc Psychiatry. 2001;40(2):206–213. doi: 10.1097/00004583-200102000-00015. [DOI] [PubMed] [Google Scholar]
- 64.Bettison S. The long-term effects of auditory training on children with autism. J Autism Dev Disord. 1996;26(3):361–374. doi: 10.1007/BF02172480. [DOI] [PubMed] [Google Scholar]
- 65.Bickman L, Noser K, Summerfelt WT. Long-term effects of a system of care on children and adolescents. J Behav Health Serv Res. 1999;26(2):185–202. doi: 10.1007/BF02287490. [DOI] [PubMed] [Google Scholar]
- 66.Bickman L, Summerfelt WT, Noser K. Comparative outcomes of emotionally disturbed children and adolescents in a system of services and usual care. Psychiatr Serv. 1997;48(12):1543–1548. doi: 10.1176/ps.48.12.1543. [DOI] [PubMed] [Google Scholar]
- 67.Birmaher B, Brent DA, Kolko D, et al. Clinical outcome after short-term psychotherapy for adolescents with major depressive disorder. Arch Gen Psychiatry. 2000;57(1):29–36. doi: 10.1001/archpsyc.57.1.29. [DOI] [PubMed] [Google Scholar]
- 68.Boisjoli R, Vitaro F, Lacourse E, Barker ED, Tremblay RE. Impact and clinical significance of a preventive intervention for disruptive boys: 15-year follow-up. Br J Psychiatry. 2007;191:415–419. doi: 10.1192/bjp.bp.106.030007. [DOI] [PubMed] [Google Scholar]
- 69.Bor W, Sanders MR, Markie-Dadds C. The effects of the Triple P-Positive Parenting Program on preschool children with co-occurring disruptive behavior and attentional/hyperactive difficulties. J Abnorm Child Psychol. 2002;30(6):571–587. doi: 10.1023/a:1020807613155. [DOI] [PubMed] [Google Scholar]
- 70.Borduin CM, Mann BJ, Cone LT, et al. Multisystemic treatment of serious juvenile offenders: long-term prevention of criminality and violence. J Consult Clin Psychol. 1995;63(4):569–578. doi: 10.1037//0022-006x.63.4.569. [DOI] [PubMed] [Google Scholar]
- 71.Bradley SJ, Jadaa DA, Brody J, et al. Brief psychoeducational parenting program: an evaluation and 1-year follow-up. J Am Acad Child Adolesc Psychiatry. 2003;42(10):1171–1178. doi: 10.1097/00004583-200310000-00007. [DOI] [PubMed] [Google Scholar]
- 72.Butler S, Baruch G, Hickey N, Fonagy P. A randomized controlled trial of multisystemic therapy and a statutory therapeutic intervention for young offenders. J Am Acad Child Adolesc Psychiatry. 2011;50(12):1220–1235. doi: 10.1016/j.jaac.2011.09.017. [DOI] [PubMed] [Google Scholar]
- 73.Byford S, Barrett B, Roberts C, et al. Economic evaluation of a randomised controlled trial for anorexia nervosa in adolescents. Br J Psychiatry. 2007;191:436–440. doi: 10.1192/bjp.bp.107.036806. [DOI] [PubMed] [Google Scholar]
- 74.Bywater T, Hutchings J, Daley D, et al. Long-term effectiveness of a parenting intervention for children at risk of developing conduct disorder. Br J Psychiatry. 2009;195:318–324. doi: 10.1192/bjp.bp.108.056531. [DOI] [PubMed] [Google Scholar]
- 75.Carpentier MY, Silovsky JF, Chaffin M. Randomized trial of treatment for children with sexual behavior problems: ten-year follow-up. J Consult Clin Psychol. 2006;74(3):482–488. doi: 10.1037/0022-006X.74.3.482. [DOI] [PubMed] [Google Scholar]
- 76.Cartwright-Hatton S, McNally D, Field AP, et al. A new parenting-based group intervention for young anxious children: results of a randomized controlled trial. J Am Acad Child Adolesc Psychiatry. 2011;50(3):242–251. doi: 10.1016/j.jaac.2010.12.015. [DOI] [PubMed] [Google Scholar]
- 77.Castellanos N, Conrod P. Brief interventions targeting personality risk factors for adolescent substance misuse reduce depression, panic and risk-taking behaviours. J Ment Health. 2006;15(6):645–658. [Google Scholar]
- 78.Catani C, Kohiladevy M, Ruf M, Schauer E, Elbert T, Neuner F. Treating children traumatized by war and Tsunami: a comparison between exposure therapy and meditation-relaxation in North-East Sri Lanka. BMC Psychiatry. 2009;9:22–32. doi: 10.1186/1471-244X-9-22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Chadwick O, Momcilovic N, Rossiter R, Stumbles E, Taylor E. A randomized trial of brief individual versus group parent training for behaviour problems in children with severe learning disabilities. Behav Cogn Psychother. 2001;29:151–167. [Google Scholar]
- 80.Charach A, Ickowicz A, Schachar R. Stimulant treatment over five years: adherence, effectiveness, and adverse effects. J Am Acad Child Adolesc Psychiatry. 2004;43(5):559–567. doi: 10.1097/00004583-200405000-00009. [DOI] [PubMed] [Google Scholar]
- 81.Chemtob CM, Nakashima J, Carlson JG. Brief treatment for elementary school children with disaster-related posttraumatic stress disorder: a field study. J Clin Psychol. 2002;58(1):99–112. doi: 10.1002/jclp.1131. [DOI] [PubMed] [Google Scholar]
- 82.Chemtob CM, Nakashima JP, Hamada RS. Psychosocial intervention for postdisaster trauma symptoms in elementary school children: a controlled community field study. Arch Pediatr Adolesc Med. 2002;156:211–216. doi: 10.1001/archpedi.156.3.211. [DOI] [PubMed] [Google Scholar]
- 83.Clarke G, Debar L, Lynch F, et al. A randomized effectiveness trial of brief cognitive-behavioral therapy for depressed adolescents receiving antidepressant medication. J Am Acad Child Adolesc Psychiatry. 2005;44(9):888–898. [PubMed] [Google Scholar]
- 84.Clarke GN, Hornbrook M, Lynch F, et al. Group cognitive-behavioral treatment for depressed adolescent offspring of depressed parents in a health maintenance organization. J Am Acad Child Adolesc Psychiatry. 2002;41(3):305–313. doi: 10.1097/00004583-200203000-00010. [DOI] [PubMed] [Google Scholar]
- 85.Clarke GN, Rohde P, Lewinsohn PM, Hops H, Seeley JR. Cognitive-behavioral treatment of adolescent depression: efficacy of acute group treatment and booster sessions. J Am Acad Child Adolesc Psychiatry. 1999;38(3):272–279. doi: 10.1097/00004583-199903000-00014. [DOI] [PubMed] [Google Scholar]
- 86.Cobham VE, Dadds MR, Spence SH. The role of parental anxiety in the treatment of childhood anxiety. J Consult Clin Psychol. 1998;66(6):893–905. doi: 10.1037//0022-006x.66.6.893. [DOI] [PubMed] [Google Scholar]
- 87.Cohen JA, Mannarino AP, Knudsen K. Treating sexually abused children: 1 year follow-up of a randomized controlled trial. Child Abuse Negl. 2005;29:135–145. doi: 10.1016/j.chiabu.2004.12.005. [DOI] [PubMed] [Google Scholar]
- 88.Connell A, Bullock BM, Dishion TJ, Shaw D, Wilson M, Gardner F. Family intervention effects on co-occurring early childhood behavioral and emotional problems: a latent transition analysis approach. J Abnorm Child Psychol. 2008;36:1211–1225. doi: 10.1007/s10802-008-9244-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Dadds MR, Holland DE, Laurens KR, Mullins M, Barrett PM, Spence SH. Early intervention and prevention of anxiety disorders in children: results at 2-year follow-up. J Consult Clin Psychol. 1999;67(1):145–150. doi: 10.1037//0022-006x.67.1.145. [DOI] [PubMed] [Google Scholar]
- 90.Dadds MR, Spence SH, Holland DE, Barrett PM, Laurens KR. Prevention and early intervention for anxiety disorders: a controlled trial. J Consult Clin Psychol. 1997;65(4):627–635. doi: 10.1037//0022-006x.65.4.627. [DOI] [PubMed] [Google Scholar]
- 91.Deblinger E, Mannarino AP, Cohen JA, Steer RA. A follow-up study of a multisite, randomized, controlled trial for children with sexual abuse-related PTSD symptoms. J Am Acad Child Adolesc Psychiatry. 2006;45(12):1474–1484. doi: 10.1097/01.chi.0000240839.56114.bb. [DOI] [PubMed] [Google Scholar]
- 92.Deblinger E, Steer RA, Lippmann J. Two-year follow-up study of cognitive behavioral therapy for sexually abused children suffering post-traumatic stress symptoms. Child Abuse Negl. 1999;23(12):1371–1378. doi: 10.1016/s0145-2134(99)00091-5. [DOI] [PubMed] [Google Scholar]
- 93.De Cuyper S, Timbremont B, Braet C, De Backer V, Wullaert T. Treating depressive symptoms in schoolchildren: a pilot study. Eur Child Adolesc Psychiatry. 2004;13:105–114. doi: 10.1007/s00787-004-0366-2. [DOI] [PubMed] [Google Scholar]
- 94.De Groot J, Cobham V, Leong J, McDermott B. Individual versus group family-focused cognitive-behaviour therapy for childhood anxiety: pilot randomized controlled trial. Aust N Z J Psychiatry. 2007;41:990–997. doi: 10.1080/00048670701689436. [DOI] [PubMed] [Google Scholar]
- 95.Dembo R, Seeberger W, Shemwell M, et al. Psychosocial functioning among juvenile offenders 12 months after family empowerment intervention. J Offender Rehabil. 2000;32(1):1–56. [Google Scholar]
- 96.Dembo R, Wareham J, Poythress NG, Cook B, Schmeidler J. The impact of arbitration intervention services on youth recidivism: one-year follow-up. J Offender Rehabil. 2006;43(4):95–131. [Google Scholar]
- 97.DeRosier ME, Marcus SR. Building friendships and combating bullying: effectiveness of S.S.GRIN at one-year follow-up. J Clin Child Adolesc Psychol. 2005;34(1):140–150. doi: 10.1207/s15374424jccp3401_13. [DOI] [PubMed] [Google Scholar]
- 98.Devlin MJ, Goldfein JA, Petkova E, Liu L, Walsh BT. Cognitive behavioral therapy and Fluoxetine for binge eating disorder: two-year follow-up. Obesity. 2007;15(7):1702–1709. doi: 10.1038/oby.2007.203. [DOI] [PubMed] [Google Scholar]
- 99.Diamond GS, Reis B, Diamond GM, Siqueland L, Isaacs L. Attachment-based family therapy for depressed adolescents: a treatment development study. J Am Acad Child Adolesc Psychiatry. 2002;41(10):1190–1196. doi: 10.1097/00004583-200210000-00008. [DOI] [PubMed] [Google Scholar]
- 100.Dishion TJ, Andrews DW. Preventing escalation in problem behaviors with high-risk young adolescents: immediate and 1-year outcomes. J Consult Clin Psychol. 1995;63(4):538–548. doi: 10.1037//0022-006x.63.4.538. [DOI] [PubMed] [Google Scholar]
- 101.Dobson KS, Hopkins JA, Fata L, Scherrer M, Allan LC. The prevention of depression and anxiety in a sample of high-risk adolescents: a randomized controlled trial. Canadian Journal of School Psychology. 2010;25(4):291–310. [Google Scholar]
- 102.Dorn LD, Kolko DJ, Shenk CE, Susman EJ, Bukstein O. Influence of treatment for disruptive behavior disorders on adrenal and gonadal hormones in youth. J Clin Child Adolesc Psychol. 2011;40(4):562–571. doi: 10.1080/15374416.2011.581614. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.Doyle AC, McLean C, Washington BN, Hoste RR, le Grange D. Are single-parent families different from two-parent families in the treatment of adolescent bulimia nervosa using family-based treatment? Int J Eat Disord. 2009;42(2):153–157. doi: 10.1002/eat.20584. [DOI] [PubMed] [Google Scholar]
- 104.Drugli MB, Larsson B. Children aged 4–8 years treated with parent training and child therapy because of conduct problems: generalisation effects to day-care and school settings. Eur Child Adolesc Psychiatry. 2006;15:392–399. doi: 10.1007/s00787-006-0546-3. [DOI] [PubMed] [Google Scholar]
- 105.Drugli MB, Larsson B, Clifford G. Changes in social competence in young children treated because of conduct problems as viewed by multiple informants. Eur Child Adolesc Psychiatry. 2007;16:370–378. doi: 10.1007/s00787-007-0609-0. [DOI] [PubMed] [Google Scholar]
- 106.Du Y, Jiang W, Vance A. Longer term effect of randomized, controlled group cognitive behavioural therapy for Internet addition in adolescent students in Shanghai. Aust N Z J Psychiatry. 2010;44:129–134. doi: 10.3109/00048670903282725. [DOI] [PubMed] [Google Scholar]
- 107.Efron D, Jarman FC, Barker MJ. Medium-term outcomes are comparable with short-term outcomes in children with attention deficit hyperactivity disorder treated with stimulant medication. J Paediatr Child Health. 2000;36:457–461. doi: 10.1046/j.1440-1754.2000.00555.x. [DOI] [PubMed] [Google Scholar]
- 108.Eisler I, Simic M, Russell GFM, Dare C. A randomised controlled treatment trial of two forms of family therapy in adolescent anorexia nervosa: a five-year follow-up. J Child Psychol Psychiatry. 2007;48(6):552–560. doi: 10.1111/j.1469-7610.2007.01726.x. [DOI] [PubMed] [Google Scholar]
- 109.Emslie GJ, Rush AJ, Weinberg WA, Kowatch RA, Carmody T, Mayes TL. Fluoxetine in child and adolescent depression: acute and maintenance treatment. Depress Anxiety. 1998;7:32–39. doi: 10.1002/(sici)1520-6394(1998)7:1<32::aid-da4>3.0.co;2-7. [DOI] [PubMed] [Google Scholar]
- 110.Epstein JN, Conners CK, Hervey AS, et al. Assessing medication effects in the MTA study using neuropsychological outcomes. J Child Psychol Psychiatry. 2006;47(5):446–456. doi: 10.1111/j.1469-7610.2005.01469.x. [DOI] [PubMed] [Google Scholar]
- 111.Flannery-Schroeder E, Choudhury MS, Kendall PC. Group and individual cognitive-behavioral treatments for youth with anxiety disorders: 1-year follow-up. Cognit Ther Res. 2005;29(2):253–259. [Google Scholar]
- 112.Flatt N, King N. Brief psycho-social interventions in the treatment of specific childhood phobias: a controlled trial and a 1-year follow-up. Behav Change. 2010;27(3):130–153. [Google Scholar]
- 113.Fristad MA, Verducci JS, Walters K, Young ME. Impact of multifamily psychoeducational psychotherapy in treating children aged 8 to 12 years with mood disorders. Arch Gen Psychiatry. 2009;66(9):1013–1021. doi: 10.1001/archgenpsychiatry.2009.112. [DOI] [PubMed] [Google Scholar]
- 114.Garber J, Clarke GN, Weersing VR, et al. Prevention of depression in at-risk adolescents: a randomized controlled trial. JAMA. 2009;301(21):2215–2224. doi: 10.1001/jama.2009.788. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 115.Garcia-Lopez L, Olivares J, Beidel D, Albano AM, Turner S, Rosa AI. Efficacy of three treatment protocols for adolescents with social anxiety disorder: a 5-year follow-up assessment. J Anxiety Disord. 2006;20:175–191. doi: 10.1016/j.janxdis.2005.01.003. [DOI] [PubMed] [Google Scholar]
- 116.Garcia-Lopez L, Olivares J, Turner SM, Beidel DC, Albano AM, Sanchez-Meca J. Results at long-term among three psychological treatments for adolescents with generalized social phobia (II): clinical significance and effect size. Psicol Conductual. 2002;10(2):371–385. [Google Scholar]
- 117.Gardner F, Burton J, Klimes I. Randomised controlled trial of a parenting intervention in the voluntary sector for reducing child conduct problems: outcomes and mechanisms of change. J Child Psychol Psychiatry. 2006;47(11):1123–1132. doi: 10.1111/j.1469-7610.2006.01668.x. [DOI] [PubMed] [Google Scholar]
- 118.Gilboa-Schechtman E, Foa EB, Shafran N, et al. Prolonged exposure versus dynamic therapy for adolescent PTSD: a pilot randomized controlled trial. J Am Acad Child Adolesc Psychiatry. 2010;49(10):1034–1042. doi: 10.1016/j.jaac.2010.07.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 119.Gillham JE, Hamilton J, Freres DR, Patton K, Gallop R. Preventing depression among early adolescents in the primary care setting: a randomized controlled study of the Penn Resiliency Program. J Abnorm Child Psychol. 2006;34(2):203–219. doi: 10.1007/s10802-005-9014-7. [DOI] [PubMed] [Google Scholar]
- 120.Gillham JE, Reivich KJ, Freres DR, et al. School-based prevention of depression and anxiety symptoms in early adolescence: a pilot of a parent intervention component. School Psychol Quart. 2006;21(3):323–348. [Google Scholar]
- 121.Glisson C, Schoenwald SK, Hemmelgarn A, et al. Randomized trial of MST and ARC in a two-level evidence-based treatment implementation strategy. J Consult Clin Psychol. 2010;78(4):537–550. doi: 10.1037/a0019160. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 122.Gordon MS, Tonge B, Melvin GA. Outcome of adolescent depression: 6 months after treatment. Aust N Z J Psychiatry. 2011;45(3):232–239. doi: 10.3109/00048674.2010.538838. [DOI] [PubMed] [Google Scholar]
- 123.Green JM, Wood AJ, Kerfoot MJ, et al. Group therapy for adolescents with repeated self harm: randomised controlled trial with economic evaluation. BMJ. 2011;342:d682. doi: 10.1136/bmj.d682. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 124.Hagen KA, Ogden T, Bjornebekk G. Treatment outcomes and mediators of parent management training: a one-year follow-up of children with conduct problems. J Clin Child Adolesc Psychol. 2011;40(2):165–178. doi: 10.1080/15374416.2011.546050. [DOI] [PubMed] [Google Scholar]
- 125.Handen BL, Janosky J, McAuliffe S. Long-term follow-up of children with mental retardation/borderline intellectual functioning and ADHD. J Abnorm Child Psychol. 1997;25(4):287–295. doi: 10.1023/a:1025760302598. [DOI] [PubMed] [Google Scholar]
- 126.Harrington R, Peters S, Green J, Byford S, Woods J, McGowan R. Randomised comparison of the effectiveness and costs of community and hospital based mental health services for children with behavioural disorders. BMJ. 2000;321(7268):1047–1050. doi: 10.1136/bmj.321.7268.1047. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 127.Hayward C, Varady S, Albano AM, Thienemann M, Henderson L, Schatzberg AF. Cognitive-behavioral group therapy for social phobia in female adolescents: results of a pilot study. J Am Acad Child Adolesc Psychiatry. 2000;39(6):721–726. doi: 10.1097/00004583-200006000-00010. [DOI] [PubMed] [Google Scholar]
- 128.Hazell PL, Martin G, McGill K, et al. Group therapy for repeated deliberate self-harm in adolescents: failure of replication of a randomized trial. J Am Acad Child Adolesc Psychiatry. 2009;48(6):662–670. doi: 10.1097/CHI.0b013e3181aOacec. [DOI] [PubMed] [Google Scholar]
- 129.Heinicke BE, Paxton SJ, McLean SA, Wertheim EH. Internet-delivered targeted group intervention for body dissatisfaction and disordered eating in adolescent girls: a randomized controlled trial. J Abnorm Child Psychol. 2007;35(3):379–391. doi: 10.1007/s10802-006-9097-9. [DOI] [PubMed] [Google Scholar]
- 130.Henggeler SW, Clingempeel WG, Brondino MJ, Pickrel SG. Four-year follow-up of multisystemic therapy with substance-abusing and substance-dependent juvenile offenders. J Am Acad Child Adolesc Psychiatry. 2002;41(7):868–874. doi: 10.1097/00004583-200207000-00021. [DOI] [PubMed] [Google Scholar]
- 131.Henggeler SW, Melton GB, Brondino MJ, Scherer DG, Hanley JH. Multisystemic therapy with violent and chronic juvenile offenders and their families: the role of treatment fidelity in successful dissemination. J Consult Clin Psychol. 1997;65(5):821–833. doi: 10.1037//0022-006x.65.5.821. [DOI] [PubMed] [Google Scholar]
- 132.Henggeler SW, Pickrel SG, Brondino MJ. Multisystemic treatment of substance-abusing and -dependent delinquents: outcomes, treatment fidelity, and transportability. Ment Health Serv Res. 1999;1(3):171–184. doi: 10.1023/a:1022373813261. [DOI] [PubMed] [Google Scholar]
- 133.Henggeler SW, Rowland MD, Halliday-Boykins C, et al. One-year follow-up of multisystemic therapy as an alternative to the hospitalization of youths in psychiatric crisis. J Am Acad Child Adolesc Psychiatry. 2003;42(5):543–551. doi: 10.1097/01.CHI.0000046834.09750.5F. [DOI] [PubMed] [Google Scholar]
- 134.Herrmann DS, McWhirter JJ. Anger and aggression management in young adolescents: an experimental validation of the SCARE program. Educ Treat Children. 2003;26(3):273–302. [Google Scholar]
- 135.Hirshfeld-Becker DR, Masek B, Henin A, et al. Cognitive behavioral therapy for 4- to 7-year-old children with anxiety disorders: a randomized clinical trial. J Consult Clin Psychol. 2010;78(4):498–510. doi: 10.1037/a0019055. [DOI] [PubMed] [Google Scholar]
- 136.Hudson JL, Rapee RM, Deveney C, Schniering CA, Lyneham HJ, Bovopoulos N. Cognitive-behavioral treatment versus an active control for children and adolescents with anxiety disorders: a randomized trial. J Am Acad Child Adolesc Psychiatry. 2009;48(5):533–544. doi: 10.1097/CHI.0b013e31819c2401. [DOI] [PubMed] [Google Scholar]
- 137.Huey SJ, Henggeler SW, Rowland MD, et al. Multisystemic therapy effects on attempted suicide by youths presenting psychiatric emergencies. J Am Acad Child Adolesc Psychiatry. 2004;43(2):183–190. doi: 10.1097/00004583-200402000-00014. [DOI] [PubMed] [Google Scholar]
- 138.Hunt C, Andrews G, Crino R, Erskine A, Sakashita C. Randomized controlled trial of an early intervention programme for adolescent anxiety disorders. Aust N Z J Psychiatry. 2009;43(4):300–304. doi: 10.1080/00048670902721152. [DOI] [PubMed] [Google Scholar]
- 139.Hutchings J, Bywater T, Daley D, et al. Parenting intervention in Sure Start services for children at risk of developing conduct disorder: pragmatic randomised controlled trial. BMJ. 2007;334:678–682. doi: 10.1136/bmj.39126.620799.55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 140.Jensen PS, Arnold LE, Swanson JM, et al. 3-year follow-up of the NIMH MTA study. J Am Acad Child Adolesc Psychiatry. 2007;46(8):989–1002. doi: 10.1097/CHI.0b013e3180686d48. [DOI] [PubMed] [Google Scholar]
- 141.Jones K, Daley D, Hutchings J, Bywater T, Eames C. Efficacy of the incredible years programme as an early intervention for children with conduct problems and ADHD: long-term follow-up. Child Care Health Dev. 2008;34(3):380–390. doi: 10.1111/j.1365-2214.2008.00817.x. [DOI] [PubMed] [Google Scholar]
- 142.Jouriles EN, McDonald R, Rosenfield D, Stephens N, Corbitt-Shindler D, Miller PC. Reducing conduct problems among children exposed to intimate partner violence: a randomized clinical trial examining effects of project support. J Consult Clin Psychol. 2009;77(4):705–717. doi: 10.1037/a0015994. [DOI] [PubMed] [Google Scholar]
- 143.Kasari C, Gulsrud AC, Wong C, Kwon S, Locke J. Randomized controlled caregiver mediated joint engagement intervention for toddlers with autism. J Autism Dev Disord. 2010;40(9):1045–1056. doi: 10.1007/s10803-010-0955-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 144.Kasari C, Paparella T, Freeman S, Jahromi LB. Language outcome in autism: randomized comparison of joint attention and play interventions. J Consult Clin Psychol. 2008;76(1):125–137. doi: 10.1037/0022-006X.76.1.125. [DOI] [PubMed] [Google Scholar]
- 145.Kendall PC, Flannery-Schroeder E, Panichelli-Mindel SM, Southam-Gerow M, Henin A, Warman M. Therapy for youths with anxiety disorders: a second randomized clinical trial. J Consult Clin Psychol. 1997;65(3):366–380. doi: 10.1037//0022-006x.65.3.366. [DOI] [PubMed] [Google Scholar]
- 146.Kendall PC, Hudson JL, Gosch E, Flannery-Schroeder E, Suveg C. Cognitive-behavioral therapy for anxiety disordered youth: a randomized clinical trial evaluating child and family modalities. J Consult Clin Psychol. 2008;76(2):282–297. doi: 10.1037/0022-006X.76.2.282. [DOI] [PubMed] [Google Scholar]
- 147.Kendall PC, Safford S, Flannery-Schroeder E, Webb A. Child anxiety treatment: outcomes in adolescence and impact on substance use and depression at 7.4-year follow-up. J Consult Clin Psychol. 2004;72(2):276–287. doi: 10.1037/0022-006X.72.2.276. [DOI] [PubMed] [Google Scholar]
- 148.Kerfoot M, Harrington R, Harrington V, Rogers J, Verduyn C. A step too far? Randomized trial of cognitive-behaviour therapy delivered by social workers to depressed adolescents. Eur Child Adolesc Psychiatry. 2004;13(2):92–99. doi: 10.1007/s00787-004-0362-6. [DOI] [PubMed] [Google Scholar]
- 149.Kling A, Forster M, Sundell K, Melin L. A randomized controlled effectiveness trial of parent management training with varying degrees of therapist support. Behav Ther. 2010;41(4):530–542. doi: 10.1016/j.beth.2010.02.004. [DOI] [PubMed] [Google Scholar]
- 150.Kolko DJ. Efficacy of cognitive-behavioral treatment and fire safety education for children who set fires: initial and follow-up outcomes. J Child Psychol Psychiatry. 2001;42(3):359–369. [PubMed] [Google Scholar]
- 151.Kolko DJ, Brent DA, Baugher M, Bridge J, Birmaher B. Cognitive and family therapies for adolescent depression: treatment specificity, mediation, and moderation. J Consult Clin Psychol. 2000;68(4):603–614. [PubMed] [Google Scholar]
- 152.Kolko DJ, Dorn LD, Bukstein O, Burke JD. Clinically referred ODD children with or without CD and healthy controls: comparison across contextual domains. J Child Fam Stud. 2008;17(5):714–734. [Google Scholar]
- 153.Kolko DJ, Dorn LD, Bukstein OG, Pardini D, Holden EA, Hart J. Community vs. clinic-based modular treatment of children with early-onset ODD or CA: a clinical trial with 3-year follow-up. J Abnorm Child Psychol. 2009;37(5):591–609. doi: 10.1007/s10802-009-9303-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 154.Lacourse E, Cote S, Nagin DS, Vitaro F, Brendgen M, Tremblay RE. A longitudinal-experimental approach to testing theories of antisocial behavior development. Dev Psychopathol. 2002;14(4):909–924. doi: 10.1017/s0954579402004121. [DOI] [PubMed] [Google Scholar]
- 155.Landa RJ, Holman KC, O’Neill AH, Stuart EA. Intervention targeting development of socially synchronous engagement in toddlers with autism spectrum disorder: a randomized controlled trial. J Child Psychol Psychiatry. 2011;52(1):13–21. doi: 10.1111/j.1469-7610.2010.02288.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 156.Larsson B, Fossum S, Clifford G, Drugli MB, Handegard BH, Morch WT. Treatment of oppositional defiant and conduct problems in young Norwegian children. Eur Child Adolesc Psychiatry. 2009;18(1):42–52. doi: 10.1007/s00787-008-0702-z. [DOI] [PubMed] [Google Scholar]
- 157.Lau W, Chan CK, Li JC, Au TK. Effectiveness of group cognitive-behavioral treatment for childhood anxiety in community clinics. Behav Res Ther. 2010;48(11):1067–1077. doi: 10.1016/j.brat.2010.07.007. [DOI] [PubMed] [Google Scholar]
- 158.Lavigne JV, LeBailly SA, Gouze KR, et al. Treating oppositional defiant disorder in primary care: a comparison of three models. J Pediatr Psychol. 2008;33(5):449–461. doi: 10.1093/jpepsy/jsm074. [DOI] [PubMed] [Google Scholar]
- 159.Le Grange D, Crosby RD, Rathouz PJ, Leventhal BL. A randomized controlled comparison of family-based treatment and supportive psychotherapy for adolescent bulimia nervosa. Arch Gen Psychiatry. 2007;64(9):1049–1056. doi: 10.1001/archpsyc.64.9.1049. [DOI] [PubMed] [Google Scholar]
- 160.Leong J, Cobham VE, de Groot J, McDermott B. Comparing different modes of delivery: a pilot evaluation of a family-focused, cognitive-behavioral intervention for anxiety-disordered children. Eur Child Adolesc Psychiatry. 2009;18(4):231–239. doi: 10.1007/s00787-008-0723-7. [DOI] [PubMed] [Google Scholar]
- 161.Lesmana CBJ, Suryani LK, Jensen GD, Tiliopoulos N. A spiritual-hypnosis assisted treatment of children with PTSD after the 2002 Bali terrorist attack. Am J Clin Hypn. 2009;52(1):23–34. doi: 10.1080/00029157.2009.10401689. [DOI] [PubMed] [Google Scholar]
- 162.Liberman RP, Robertson MJ. A pilot, controlled skills training study of schizotypal high school students. Verhaltenstherapie. 2005;15:176–180. [Google Scholar]
- 163.Lieberman AF, Ippen CG, Van Horn P. Child-parent psychotherapy: 6-month follow-up of a randomized controlled trial. J Am Acad Child Adolesc Psychiatry. 2006;45(8):913–918. doi: 10.1097/01.chi.0000222784.03735.92. [DOI] [PubMed] [Google Scholar]
- 164.Lochman JE, Wells KC. Effectiveness of the coping power program and of classroom intervention with aggressive children: outcomes at a 1-year follow-up. Behav Ther. 2003;34(4):493–515. [Google Scholar]
- 165.Lochman JE, Wells KC. The coping power program for preadolescent aggressive boys and their parents: outcome effects at the 1-year follow-up. J Consult Clin Psychol. 2004;72(4):571–578. doi: 10.1037/0022-006X.72.4.571. [DOI] [PubMed] [Google Scholar]
- 166.Lock J, Agras WS, Bryson S, Kraemer HC. A comparison for short- and long-term family therapy for adolescent anorexia nervosa. J Am Acad Child Adolesc Psychiatry. 2005;44(7):632–639. doi: 10.1097/01.chi.0000161647.82775.0a. [DOI] [PubMed] [Google Scholar]
- 167.Lock J, Couturier J, Agras WS. Comparison of long-term outcomes in adolescents with anorexia nervosa treated with family therapy. J Am Acad Child Adolesc Psychiatry. 2006;45(6):666–672. doi: 10.1097/01.chi.0000215152.61400.ca. [DOI] [PubMed] [Google Scholar]
- 168.Mager W, Milich R, Harris MJ, Howard A. Intervention groups for adolescents with conduct problems: is aggregation harmful or helpful? J Abnorm Child Psychol. 2005;33(3):349–362. doi: 10.1007/s10802-005-3572-6. [DOI] [PubMed] [Google Scholar]
- 169.Manassis K, Wilansky-Traynor P, Farzan N, Kleiman V, Parker K, Sanford M. The feelings club: randomized controlled evaluation of school-based CBT for anxious or depressive symptoms. Depress Anxiety. 2010;27(10):945–952. doi: 10.1002/da.20724. [DOI] [PubMed] [Google Scholar]
- 170.March S, Spence SH, Donovan CL. The efficacy of an internet-based cognitive-behavioral therapy intervention for child anxiety disorders. J Pediatr Psychol. 2009;34(5):474–487. doi: 10.1093/jpepsy/jsn099. [DOI] [PubMed] [Google Scholar]
- 171.Markie-Dadds C, Sanders MR. A controlled evaluation of an enhanced self-directed behavioural family intervention for parents of children with conduct problems in rural and remote areas. Behav Change. 2006;23(1):55–72. [Google Scholar]
- 172.Martsch MD. A comparison of two group interventions for adolescent aggression: high process versus low process. Res Soc Work Pract. 2005;15(1):8–18. [Google Scholar]
- 173.Masia-Warner C, Klein RG, Dent HC, et al. School-based intervention for adolescents with social anxiety disorder: results of a controlled study. J Abnorm Child Psychol. 2005;33(6):707–722. doi: 10.1007/s10802-005-7649-z. [DOI] [PubMed] [Google Scholar]
- 174.Mattejat F, Hirt BR, Wilken J, Schmidt MH, Remschmidt H. Efficacy of inpatient and home treatment in psychiatrically disturbed children and adolescents: follow-up assessment of the results of a controlled treatment study. Eur Child Adolesc Psychiatry. 2001;10(Sup 1):S71–S79. doi: 10.1007/s007870170008. [DOI] [PubMed] [Google Scholar]
- 175.Melvin GA, Tonge BJ, King NJ, Heyne D, Gordon MS, Klimkeit E. A comparison of cognitive-behavioral therapy, Sertraline, and their combination for adolescent depression. J Am Acad Child Adolesc Psychiatry. 2006;45(10):1151–1161. doi: 10.1097/01.chi.0000233157.21925.71. [DOI] [PubMed] [Google Scholar]
- 176.Mendenhall AN, Fristad MA, Early TJ. Factors influencing service utilization and mood symptom severity in children with mood disorders: effects of multifamily psychoeducation groups (MFPGs) J Consult Clin Psychol. 2009;77(3):463–473. doi: 10.1037/a0014527. [DOI] [PubMed] [Google Scholar]
- 177.Miklowitz DJ, Axelson DA, Birmaher B, et al. Family-focused treatment for adolescents with bipolar disorder: results of a 2-year randomized trial. Arch Gen Psychiatry. 2008;65(9):1053–1061. doi: 10.1001/archpsyc.65.9.1053. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 178.Miller LD, Laye-Gindhu A, Liu Y, March JS, Thordarson DS, Garland EJ. Evaluation of a preventive intervention for child anxiety in two randomized attention-control school trials. Behav Res Ther. 2011;49(5):315–323. doi: 10.1016/j.brat.2011.02.006. [DOI] [PubMed] [Google Scholar]
- 179.Molina BSG, Flory K, Hinshaw SP, et al. Delinquent behavior and emerging substance use in the MTA at 36 months: prevalence, course, and treatment effects. J Am Acad Child Adolesc Psychiatry. 2007;46(8):1028–1040. doi: 10.1097/chi.0b013e3180686d96. [DOI] [PubMed] [Google Scholar]
- 180.Molina BSG, Hinshaw SP, Swanson JM, et al. The MTA at 8 years: prospective follow-up of children treated for combined-type ADHD in a multisite study. J Am Acad Child Adolesc Psychiatry. 2009;48(5):484–500. doi: 10.1097/CHI.0b013e31819c23d0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 181.Morawska A, Haslam D, Milne D, Sanders MR. Evaluation of a brief parenting discussion group for parents of young children. J Dev Behav Pediatr. 2010;32(2):136–145. doi: 10.1097/DBP.0b013e3181f17a28. [DOI] [PubMed] [Google Scholar]
- 182.Morawska A, Sanders MR. Self-administered behavioral family intervention for parents of toddlers: part I. Efficacy. J Consult Clin Psychol. 2006;74(1):10–19. doi: 10.1037/0022-006X.74.1.10. [DOI] [PubMed] [Google Scholar]
- 183.MTA Cooperative Group. National Institute of Mental Health Multimodal Treatment Study of ADHD follow-up: changes in effectiveness and growth after the end of treatment. Pediatrics. 2004;113:762–769. doi: 10.1542/peds.113.4.762. [DOI] [PubMed] [Google Scholar]
- 184.The Multisite Violence Prevention Project. The Multisite Violence Prevention Project: impact of a universal school-based violence prevention program on social-cognitive outcomes. Prev Sci. 2008;9(4):231–244. doi: 10.1007/s11121-008-0101-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 185.The Multisite Violence Prevention Project. The ecological effects of universal and selective violence prevention programs for middle school students: a randomized trial. J Consult Clin Psychol. 2009;77(3):526–542. doi: 10.1037/a0014395. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 186.Muntz R, Hutchings J, Edwards RT, Hounsome B, O’Ceilleachair A. Economic evaluation of treatments for children with severe behavioural problems. J Ment Health Policy Econ Econ. 2004;7(4):177–189. [PubMed] [Google Scholar]
- 187.Muratori F, Picchi L, Casella C, Tancredi R, Milone A, Patarnello MG. Efficacy of brief dynamic psychotherapy for children with emotional disorders. Psychother Psychosom. 2002;71(1):28–38. doi: 10.1159/000049341. [DOI] [PubMed] [Google Scholar]
- 188.Nauta MH, Scholing A, Emmelkamp PMG, Mideraa RB. Cognitive-behavioural therapy for anxiety disordered children in a clinical setting: does additional cognitive parent training enhance treatment effectiveness? Clin Psychol Psychother. 2001;8(5):330–340. [Google Scholar]
- 189.Nestler J, Goldbeck L. A pilot study of social competence group training for adolescents with borderline intellectual functioning and emotional and behavioural problems (SCT-ABI) J Intell Disabil Res. 2011;55(2):231–241. doi: 10.1111/j.1365–2788.2010.01369.x. [DOI] [PubMed] [Google Scholar]
- 190.Neziroglu F, Yaryura-Tobias JA, Walz J, McKay D. The effect of Fluvoxamine and behavior therapy on children and adolescents with obsessive-compulsive disorder. J Child Adolesc Psychopharmacol. 2000;10(4):295–306. doi: 10.1089/cap.2000.10.295. [DOI] [PubMed] [Google Scholar]
- 191.Nickel MK, Krawczyk J, Nickel C, et al. Anger, interpersonal relationships, and health-related quality of life in bullying boys who are treated with outpatient family therapy: a randomized, prospective, controlled trial with 1 year of follow-up. Pediatrics. 2005;116(2):247–254. doi: 10.1542/peds.2004-2534. [DOI] [PubMed] [Google Scholar]
- 192.Nickel M, Luley J, Krawczyk J, et al. Bullying girls—Changes after brief strategic family therapy: a randomized, prospective, controlled trial with one-year follow-up. Psychother Psychosom. 2006;75(1):47–55. doi: 10.1159/000089226. [DOI] [PubMed] [Google Scholar]
- 193.Nixon RDV. Changes in hyperactivity and temperament in behaviourally disturbed preschoolers after Parent-Child Interaction Therapy (PCIT) Behav Change. 2001;18(3):168–176. [Google Scholar]
- 194.Nixon RDV, Sweeney L, Erickson DB, Touyz SW. Parent-Child Interaction Therapy: a comparison of standard and abbreviated treatments for oppositional defiant preschoolers. J Consult Clin Psychol. 2003;71(2):251–260. doi: 10.1037/0022-006x.71.2.251. [DOI] [PubMed] [Google Scholar]
- 195.Nixon RDV, Sweeney L, Erickson DB, Touyz SW. Parent-Child Interaction Therapy: one- and two-year follow-up of standard and abbreviated treatments for oppositional preschoolers. J Abnorm Child Psychol. 2004;32(3):263–271. doi: 10.1023/b:jacp.0000026140.60558.05. [DOI] [PubMed] [Google Scholar]
- 196.O’Leary EMM, Barrett P, Fjermestad KW. Cognitive-behavioral family treatment for childhood obsessive-compulsive disorder: a 7-year follow-up study. J Anxiety Disord. 2009;23(7):973–978. doi: 10.1016/j.janxdis.2009.06.009. [DOI] [PubMed] [Google Scholar]
- 197.Olivares J, Garcia-Lopez LJ, Beidel DC, Turner SM, Albano AM, Hidalgo MD. Results at long-term among three psychological treatments for adolescents with generalized social phobia (I): Statistical significance. Psicol Conductual. 2002;10(1):147–164. [Google Scholar]
- 198.Olivares-Olivares PJ, Rosa-Alcazar AI, Olivares-Rodriguez J. Does individual attention improve the effect of group treatment of adolescents with social phobia? Int J Clin Health Psychol. 2008;8(2):465–481. [Google Scholar]
- 199.Ollendick TH, Ost LG, Reuterskiold L, Costa N. Comorbidity in youth with specific phobias: impact of comorbidity on treatment outcomes and the impact of treatment on comorbid disorders. Behav Res Ther. 2010;48:827–831. doi: 10.1016/j.brat.2010.05.024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 200.Ollendick TH, Ost LG, Reuterskiold L, et al. One-session treatment of specific phobias in youth: a randomized clinical trial in the United States and Sweden. J Consult Clin Psychol. 2009;77(3):504–516. doi: 10.1037/a0015158. [DOI] [PubMed] [Google Scholar]
- 201.Ost LG, Svensson L, Hellstrom K, Lindwall R. One-session treatment of specific phobias in youths: a randomized clinical trial. J Consult Clin Psychol. 2001;69(5):814–824. [PubMed] [Google Scholar]
- 202.Patterson J, Barlow J, Mockford C, Klimes I, Pyper C, Stewart-Brown S. Improving mental health through parenting programmes: block randomised controlled trial. Arch Dis Child. 2002;87(6):472–477. doi: 10.1136/adc.87.6.472. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 203.Pepler D, Walsh M, Yuile A, et al. Bridging the gender gap: interventions with aggressive girls and their parents. Prev Sci. 2010;11(3):229–238. doi: 10.1007/s11121-009-0167-4. [DOI] [PubMed] [Google Scholar]
- 204.Pincus DB, May JE, Whitton SW, Mattis SG, Barlow DH. Cognitive-behavioral treatment of panic disorder in adolescence. J Clin Child Adolesc Psychol. 2010;39(5):638–649. doi: 10.1080/15374416.2010.501288. [DOI] [PubMed] [Google Scholar]
- 205.Puskar K, Sereika S, Tusaie-Mumford K. Effect of the Teaching Kids to Cope (TKC) program on outcomes of depression and coping among rural adolescents. J Child Adolesc Psychiatr Nurs. 2003;16(2):71–80. doi: 10.1111/j.1744-6171.2003.tb00350.x. [DOI] [PubMed] [Google Scholar]
- 206.Reid MJ, Webster-Stratton C, Hammond M. Follow-up of children who received the Incredible Years intervention for oppositional-defiant disorder: maintenance and prediction of 2-year outcome. Behav Ther. 2003;34(4):471–491. [Google Scholar]
- 207.Renaud J, Brent DA, Baugher M, Birmaher B, Kolko DJ, Bridge J. Rapid response to psychosocial treatment for adolescent depression: a two-year follow-up. J Am Acad Child Adolesc Psychiatry. 1998;37(11):1184–1190. doi: 10.1097/00004583-199811000-00019. [DOI] [PubMed] [Google Scholar]
- 208.Rickards AL, Walstab JE, Wright-Rossi RA, Simpson J, Reddihough DS. One-year follow-up of the outcome of a randomized controlled trial of a home-based intervention programme for children with autism and developmental delay and their families. Child Care Health Dev. 2009;35(5):593–602. doi: 10.1111/j.1365-2214.2009.00953.x. [DOI] [PubMed] [Google Scholar]
- 209.Roberts C, Kane R, Thomson J, Bishop B, Hart B. The prevention of depressive symptoms in rural school children: a randomized controlled trial. J Consult Clin Psychol. 2003;71(3):622–628. doi: 10.1037/0022-006x.71.3.622. [DOI] [PubMed] [Google Scholar]
- 210.Roberts C, Mazzucchelli T, Studman L, Sanders MR. Behavioral family intervention for children with developmental disabilities and behavioral problems. J Clin Child Adolesc Psychol. 2006;35(2):180–193. doi: 10.1207/s15374424jccp3502_2. [DOI] [PubMed] [Google Scholar]
- 211.Robin AL, Siegel PT, Moye AW, Gilroy M, Dennis AB, Sikand A. A controlled comparison of family versus individual therapy for adolescents with anorexia nervosa. J Am Acad Child Adolesc Psychiatry. 1999;38(12):1482–1489. doi: 10.1097/00004583-199912000-00008. [DOI] [PubMed] [Google Scholar]
- 212.Rohde P, Clarke GN, Mace DE, Jorgensen JS, Seeley JR. An efficacy/effectiveness study of cognitive-behavioral treatment for adolescents with comorbid major depression and conduct disorder. J Am Acad Child Adolesc Psychiatry. 2004;43(6):660–668. doi: 10.1097/01.chi.0000121067.29744.41. [DOI] [PubMed] [Google Scholar]
- 213.Rohde P, Seeley JR, Kaufman NK, Clarke GN, Stice E. Predicting time to recovery among depressed adolescents treated in two psychosocial group interventions. J Consult Clin Psychol. 2006;74(1):80–88. doi: 10.1037/0022-006X.74.1.80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 214.Ruf M, Schauer M, Neuner F, Catani C, Schauer E, Elbert T. Narrative exposure therapy for 7- to 16-year-olds: a randomized controlled trial with traumatized refugee children. J Trauma Stress. 2010;23(4):437–445. doi: 10.1002/jts.20548. [DOI] [PubMed] [Google Scholar]
- 215.Sanders MR, Bor W, Morawska A. Maintenance of treatment gains: a comparison of enhanced, standard, and self-directed Triple P-Positive Parenting Program. J Abnorm Child Psychol. 2007;35(6):983–998. doi: 10.1007/s10802-007-9148-x. [DOI] [PubMed] [Google Scholar]
- 216.Sanders MR, Markie-Dadds C, Tully LA, Bor W. The Triple P-Positive Parenting Program: a comparison of enhanced, standard, and self-directed behavioral family intervention for parents of children with early onset conduct problems. J Consult Clin Psychol. 2000;68(4):624–640. [PubMed] [Google Scholar]
- 217.Sanders MR, McFarland M. Treatment of depressed mothers with disruptive children: a controlled evaluation of cognitive behavioral family intervention. Behav Ther. 2000;31(1):89–112. [Google Scholar]
- 218.Schaal S, Elbert T, Neuner F. Narrative exposure therapy versus interpersonal psychotherapy: a pilot randomized controlled trial with Rwandan genocide orphans. Psychother Psychosom. 2009;78(5):298–306. doi: 10.1159/000229768. [DOI] [PubMed] [Google Scholar]
- 219.Schaeffer CM, Borduin CM. Long-term follow-up to a randomized clinical trial of multisystemic therapy with serious and violent juvenile offenders. J Consult Clin Psychol. 2005;73(3):445–453. doi: 10.1037/0022-006X.73.3.445. [DOI] [PubMed] [Google Scholar]
- 220.Scheeringa MS, Weems CF, Cohen JA, Amaya-Jackson L, Guthrie D. Trauma-focused cognitive-behavioral therapy for posttraumatic stress disorder in three- through six year-old children: a randomized clinical trial. J Child Psychol Psychiatry. 2011;52(8):853–860. doi: 10.1111/j.1469-7610.2010.02354.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 221.Schmidt NB, Eggleston AM, Woolaway-Bickel K, Fitzpatrick KK, Vasey MW, Richey JA. Anxiety Sensitivity Amelioration Training (ASAT): a longitudinal primary prevention program targeting cognitive vulnerability. J Anxiety Disord. 2007;21(3):302–319. doi: 10.1016/j.janxdis.2006.06.002. [DOI] [PubMed] [Google Scholar]
- 222.Schmidt U, Lee S, Beecham J, et al. A randomized controlled trial of family therapy and cognitive behavior therapy guided self-care for adolescents with bulimia nervosa and related disorders. Am J Psychiatry. 2007;164(4):591–598. doi: 10.1176/ajp.2007.164.4.591. [DOI] [PubMed] [Google Scholar]
- 223.Sheffield JK, Spence SH, Rapee RM, et al. Evaluation of universal, indicated, and combined cognitive-behavioral approaches to the prevention of depression among adolescents. J Consult Clin Psychol. 2006;74(1):66–79. doi: 10.1037/0022-006X.74.1.66. [DOI] [PubMed] [Google Scholar]
- 224.Shortt AL, Barrett PM, Fox TL. Evaluating the FRIENDS program: a cognitive-behavioral group treatment for anxious children and their parents. J Clin Child Adolesc Psychol. 2001;30(4):525–535. doi: 10.1207/S15374424JCCP3004_09. [DOI] [PubMed] [Google Scholar]
- 225.Silverman WK, Kurtines WM, Ginsburg GS, Weems CF, Lumpkin PW, Carmichael DH. Treating anxiety disorders in children with group cognitive-behavioral therapy: a randomized clinical trial. J Consult Clin Psychol. 1999;67(6):995–1003. doi: 10.1037//0022-006x.67.6.995. [DOI] [PubMed] [Google Scholar]
- 226.Silverman WK, Kurtines WM, Jaccard J, Pina AA. Directionality of change in youth anxiety treatment involving parents: an initial examination. J Consult Clin Psychol. 2009;77(3):474–485. doi: 10.1037/a0015761. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 227.Simons M, Schneider S, Herpertz-Dahlmann B. Metacognitive therapy versus exposure and response prevention for pediatric obsessive-compulsive disorder: a case series with randomized allocation. Psychother Psychosom. 2006;75(4):257–264. doi: 10.1159/000092897. [DOI] [PubMed] [Google Scholar]
- 228.Siqueland L, Rynn M, Diamond GS. Cognitive behavioral and attachment based family therapy for anxious adolescents: phase I and II studies. J Anxiety Disord. 2005;19(4):361–381. doi: 10.1016/j.janxdis.2004.04.006. [DOI] [PubMed] [Google Scholar]
- 229.Smith P, Yule W, Perrin S, Tranah T, Dalgleish T, Clark DM. Cognitive-behavioral therapy for PTSD in children and adolescents: a preliminary randomized controlled trial. J Am Acad Child Adolesc Psychiatry. 2007;46(8):1051–1061. doi: 10.1097/CHI.0b013e318067e288. [DOI] [PubMed] [Google Scholar]
- 230.Smith T, Groen AD, Wynn JW. Randomized trial of intensive early intervention for children with pervasive developmental disorder. Am J Ment Retard. 2000;105(4):269–285. doi: 10.1352/0895-8017(2000)105<0269:RTOIEI>2.0.CO;2. [DOI] [PubMed] [Google Scholar]
- 231.So CYC, Leung PWL, Hung S. Treatment effectiveness of combined medication/behavioural treatment with Chinese ADHD children in routine practice. Behav Res Ther. 2008;46(9):983–992. doi: 10.1016/j.brat.2008.06.007. [DOI] [PubMed] [Google Scholar]
- 232.Spence SH, Donovan C, Brechman-Toussaint M. The treatment of childhood social phobia: the effectiveness of a social skills training-based, cognitive-behavioural intervention, with and without parental involvement. J Child Psychol Psychiatry. 2000;41(6):713–726. [PubMed] [Google Scholar]
- 233.Spence SH, Donovan CL, March S, et al. A randomized controlled trial of online versus clinic-based CBT for adolescent anxiety. J Consult Clin Psychol. 2011;79(5):629–642. doi: 10.1037/a0024512. [DOI] [PubMed] [Google Scholar]
- 234.Spence SH, Holmes JM, March S, Lipp OV. The feasibility and outcome of clinic plus internet delivery of cognitive-behavior therapy for childhood anxiety. J Consult Clin Psychol. 2006;74(3):614–621. doi: 10.1037/0022-006X.74.3.614. [DOI] [PubMed] [Google Scholar]
- 235.Stice E, Rohde P, Gau J, Shaw H. An effectiveness trial of a dissonance-based eating disorder prevention program for high-risk adolescent girls. J Consult Clin Psychol. 2009;77(5):825–834. doi: 10.1037/a0016132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 236.Stice E, Rohde P, Seeley JR, Gau JM. Brief cognitive-behavioral depression prevention program for high-risk adolescents outperforms two alternative interventions: a randomized efficacy trial. J Consult Clin Psychol. 2008;76(4):595–606. doi: 10.1037/a0012645. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 237.Stice E, Shaw H, Burton E, Wade E. Dissonance and healthy weight eating disorder prevention programs: a randomized efficacy trial. J Consult Clin Psychol. 2006;74(2):263–275. doi: 10.1037/0022-006X.74.2.263. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 238.Suveg C, Hudson JL, Brewer G, Flannery-Schroeder E, Gosch E, Kendall PC. Cognitive-behavioral therapy for anxiety-disordered youth: secondary outcomes from a randomized clinical trial evaluating child and family modalities. J Anxiety Disord. 2009;23(3):341–349. doi: 10.1016/j.janxdis.2009.01.003. [DOI] [PubMed] [Google Scholar]
- 239.Swanson JM, Elliott GR, Greenhill LL, et al. Effects of stimulant medication on growth rates across 3 years in the MTA follow-up. J Am Acad Child Adolesc Psychiatry. 2007;46(8):1015–1027. doi: 10.1097/chi.0b013e3180686d7e. [DOI] [PubMed] [Google Scholar]
- 240.Timmons-Mitchell J, Bender MB, Kishna MA, Mitchell CC. An independent effectiveness trial of multisystemic therapy with juvenile justice youth. J Clin Child Adolesc Psychol. 2006;35(2):227–236. doi: 10.1207/s15374424jccp3502_6. [DOI] [PubMed] [Google Scholar]
- 241.Treatment for Adolescents with Depression Study (TADS) Team. The Treatment for Adolescents with Depression Study (TADS): outcomes over 1 year of naturalistic follow-up. Am J Psychiatry. 2009;166(10):1141–1149. doi: 10.1176/appi.ajp.2009.08111620. [DOI] [PubMed] [Google Scholar]
- 242.Trowell J, Joffe I, Campbell J, et al. Childhood depression: a place for psychotherapy. Eur Child Adolesc Psychiatry. 2007;16(3):157–167. doi: 10.1007/s00787-006-0584-x. [DOI] [PubMed] [Google Scholar]
- 243.Tucker S, Gross D, Fogg L, Delaney K, Lapporte R. The long-term efficacy of a behavioral parent training intervention for families with 2-year-olds. Res Nurs Health. 1998;21(3):199–210. doi: 10.1002/(sici)1098-240x(199806)21:3<199::aid-nur3>3.0.co;2-c. [DOI] [PubMed] [Google Scholar]
- 244.Turner KMT, Sanders MR. Help when it’s needed first: a controlled evaluation of brief, preventive behavioral family intervention in a primary care setting. Behav Ther. 2006;37(2):131–142. doi: 10.1016/j.beth.2005.05.004. [DOI] [PubMed] [Google Scholar]
- 245.Van de Wiel N, Matthys W, Cohen-Kettenis P, van Engeland H. Application of the Utrecht Coping Power Program and care as usual to children with disruptive behavior disorders in outpatient clinics: a comparative study of cost and course of treatment. Behav Ther. 2003;34(4):421–436. [Google Scholar]
- 246.Van den Hoofdakker BJ, van der Veen-Mulders L, Sytema S, Emmelkamp PMG, Minderaa RB, Nauta MH. Effectiveness of behavioral parent training for children with ADHD in routine clinical practice: a randomized controlled study. J Am Acad Child Adolesc Psychiatry. 2007;46(10):1263–1271. doi: 10.1097/chi.0b013e3181354bc2. [DOI] [PubMed] [Google Scholar]
- 247.Van Manen TG, Prins PJM, Emmelkamp PMG. Reducing aggressive behavior in boys with a social cognitive group treatment: results of a randomized, controlled trial. J Am Acad Child Adolesc Psychiatry. 2004;43(12):1478–1487. doi: 10.1097/01.chi.0000142669.36815.3e. [DOI] [PubMed] [Google Scholar]
- 248.Verduyn C, Barrowclough C, Roberts J, Tarrier N, Harrington R. Maternal depression and child behaviour problems: randomised placebo-controlled trial of a cognitive-behavioural group intervention. Br J Psychiatry. 2003;183:342–348. doi: 10.1192/bjp.183.4.342. [DOI] [PubMed] [Google Scholar]
- 249.Volpe RJ, DuPaul GJ, Jitendra AK, Tresco KE. Consultation-based academic interventions for children with attention-deficit hyperactivity disorder: effects on reading and mathematics outcomes at 1-year follow-up. School Psychol Rev. 2009;38(1):5–13. [Google Scholar]
- 250.Vostanis P, Feehan C, Grattan E, Bickerton W. A randomised controlled out-patient trial of cognitive-behavioural treatment for children and adolescents with depression: 9-month follow-up. J Affect Disord. 1996;40(1–2):105–116. doi: 10.1016/0165-0327(96)00054-7. [DOI] [PubMed] [Google Scholar]
- 251.Wallin U, Kronovall P, Majewski ML. Body awareness therapy in teenage anorexia nervosa: outcome after 2 years. Eur Eat Disord Rev. 2000;8(1):19–30. [Google Scholar]
- 252.Wanders F, Serra M, de Jongh A. EMDR versus CBT for children with self-esteem and behavioral problems: a randomized controlled trial. J EMDR Pract Res. 2008;2(3):180–189. [Google Scholar]
- 253.Warner CM, Fisher PH, Shrout PE, Rathor S, Klein RG. Treating adolescents with social anxiety disorder in school: an attention control trial. J Child Psychol Psychiatry. 2007;48(7):676–686. doi: 10.1111/j.1469-7610.2007.01737.x. [DOI] [PubMed] [Google Scholar]
- 254.Webster-Stratton C, Hammond M. Treating children with early-onset conduct problems: a comparison of child and parent training interventions. J Consult Clin Psychol. 1997;65(1):93–109. doi: 10.1037//0022-006x.65.1.93. [DOI] [PubMed] [Google Scholar]
- 255.Webster-Stratton C, Reid MJ, Hammond M. Social skills and problem-solving training for children with early-onset conduct problems: who benefits? J Child Psychol Psychiatry. 2001;42(7):943–952. doi: 10.1111/1469-7610.00790. [DOI] [PubMed] [Google Scholar]
- 256.Webster-Stratton C, Reid MJ, Hammond M. Treating children with early-onset conduct problems: intervention outcomes for parent, child, and teacher training. J Clin Child Adolesc Psychol. 2004;33(1):105–124. doi: 10.1207/S15374424JCCP3301_11. [DOI] [PubMed] [Google Scholar]
- 257.Weiss B, Catron T, Harris V. A 2-year follow-up of the effectiveness of traditional child psychotherapy. J Consult Clin Psychol. 2000;68(6):1094–1101. doi: 10.1037//0022-006x.68.6.1094. [DOI] [PubMed] [Google Scholar]
- 258.Weiss B, Catron T, Harris V, Phung TM. The effectiveness of traditional child psychotherapy. J Consult Clin Psychol. 1999;67(1):82–94. doi: 10.1037//0022-006x.67.1.82. [DOI] [PubMed] [Google Scholar]
- 259.Weisz JR, Thurber CA, Sweeney L, Proffitt VD, LeGagnoux GL. Brief treatment of mild-to-moderate child depression using primary and secondary control enhancement training. J Consult Clin Psychol. 1997;65(4):703–707. doi: 10.1037//0022-006x.65.4.703. [DOI] [PubMed] [Google Scholar]
- 260.Whittingham K, Sofronoff K, Sheffield J, Sanders MR. Stepping Stones Triple P: an RCT of a parenting program with parents of a child diagnosed with an autism spectrum disorder. J Abnorm Child Psychol. 2009;37(4):469–480. doi: 10.1007/s10802-008-9285-x. [DOI] [PubMed] [Google Scholar]
- 261.Wilmshurst LA. Treatment programs for youth with emotional and behavioral disorders: an outcome study of two alternate approaches. Adm Policy Ment Health. 2002;4(2):85–96. doi: 10.1023/a:1015200200316. [DOI] [PubMed] [Google Scholar]
- 262.Wood A, Harrington R, Moore A. Controlled trial of a brief cognitive-behavioural intervention in adolescent patients with depressive disorders. J Child Psychol Psychiatry. 1996;37(6):737–746. doi: 10.1111/j.1469-7610.1996.tb01466.x. [DOI] [PubMed] [Google Scholar]
- 263.Wood JJ, McLeod BD, Piacentini JC, Sigman M. One-year follow-up of family versus child CBT for anxiety disorders: exploring the roles of child age and parental intrusiveness. Child Psychiatry Hum Dev. 2009;40(2):301–316. doi: 10.1007/s10578-009-0127-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 264.Woods DW, Piacentini JC, Scahill L, et al. Behavior therapy for tics in children: acute and long-term effects on psychiatric and psychosocial functioning. J Child Neurol. 2011;26(7):858–865. doi: 10.1177/0883073810397046. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 265.Young JF, Mufson L, Davies M. Efficacy of Interpersonal Psychotherapy-Adolescent Skills Training: an indicated preventive intervention for depression. J Child Psychol Psychiatry. 2006;47(12):1254–1262. doi: 10.1111/j.1469-7610.2006.01667.x. [DOI] [PubMed] [Google Scholar]
- 266.Young JF, Mufson L, Gallop R. Preventing depression: a randomized trial of interpersonal psychotherapy-adolescent skills training. Depress Anxiety. 2010;27(5):426–433. doi: 10.1002/da.20664. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 267.Zonnevylle-Bender MJS, Matthys W, van de Wiel NMH, Lochman JE. Preventive effects of treatment of disruptive behavior disorder in middle childhood on substance use and delinquent behavior. J Am Acad Child Adolesc Psychiatry. 2007;46(1):33–39. doi: 10.1097/01.chi.0000246051.53297.57. [DOI] [PubMed] [Google Scholar]
- 268.Liberati A, Altman DG, Tetzlaff J, et al. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate health care interventions: explanation and elaboration. BMJ. 2009;339:b2700. doi: 10.1136/bmj.b2700. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 269.Chamberlain P, Reid JB. Using a specialized foster care community treatment model for children and adolescents leaving the state mental hospital. J Community Psychol. 1991;19:266–276. [Google Scholar]
- 270.Grizenko N, Papineau D, Sayegh L. Effectiveness of a multimodal day treatment program for children with disruptive behavior problems. J Am Acad Child Adolesc Psychiatry. 1993;32(1):127–134. doi: 10.1097/00004583-199301000-00019. [DOI] [PubMed] [Google Scholar]
- 271.Bickman L, Guthrie P, Foster EM, et al. Evaluating Managed Mental Health Services: The Fort Bragg Experiment. New York, NY: Plenum Press; 1995. [Google Scholar]
- 272.Institute of Medicine. Crossing the Quality Chasm: A New Health System for the 21st Century. Washington, DC: National Academy Press; 2001. [PubMed] [Google Scholar]
- 273.Stroul BA, Friedman RM. A System of Care for Children and Youth with Severe Emotional Disturbances. Washington, D.C: Georgetown University Child Development Center, CASSP Technical Assistance Center; 1994. Revised. [Google Scholar]
- 274.Jensen PS, Foster M. Closing the research to practice gap in children’s mental health: structures, solutions, and strategies. Adm Policy Ment Health. 2010;37(1):111–119. doi: 10.1007/s10488-010-0286-z. [DOI] [PubMed] [Google Scholar]
- 275.Dixon LB, Lucksted A, Medoff DR, et al. Outcomes of a randomized study of a peer-taught family-to-family education program for mental illness. Psychiatr Serv. 2011;62:591–597. doi: 10.1176/ps.62.6.pss6206_0591. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 276.Teich JL, Robinson G, Weist MD. What kinds of mental health services do public schools in the United States provide? Adv Sch Ment Health Promot. 2008;1(sup 1):13–22. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.