Summary
Background and objectives
In adults, increased carotid intima-media thickness (cIMT) as assessed by ultrasonography is a valid predictor of cardiovascular events. Children with CKD are known to be at increased cardiovascular risk. This study sought to identify cardiovascular risk factors associated with increased cIMT in children with CKD.
Design, setting, participants, & measurements
This was a cross-sectional analysis of cIMT obtained after 12 months of follow-up of 101 children aged 2–18 years with mild to moderate CKD (median GFR 42.9 ml/min per 1.73 m2) in the Chronic Kidney Disease in Children cohort study enrolled between April 2005 and September 2009 and 97 healthy pediatric controls between January 2003 and December 2008. An average of six standardized B-mode ultrasound measurements constituted the overall cIMT measurement.
Results
The median cIMT was 0.43 mm (interquartile range, 0.38–0.48) compared with 0.41 mm in healthy controls (P=0.03 for difference). After multivariable adjustment, the median cIMT was 0.02 mm (95% confidence interval [CI], 0.01–0.05) larger than that of the healthy controls. In a multivariable linear regression analysis, dyslipidemia and hypertension were associated with 0.05 mm (95% CI, 0.01–0.08) and 0.04 mm (95% CI, 0.003–0.08) greater mean cIMT, respectively. Body mass index, CKD etiology, GFR, birth weight, pubertal status, calcium, phosphorus, sex, and race were not associated with cIMT.
Conclusions
cIMT is significantly elevated among children with CKD, as is the prevalence of other cardiovascular risk factors. Of these risk factors, hypertension and dyslipidemia are significantly associated with increased cIMT.
Introduction
Atherosclerosis, characterized by fatty streaks and fibrous plaques on the intimal surface of large and medium-sized arteries, is a well established cause of cardiovascular events in adults (1,2). Many studies in adults and children have shown atherosclerosis to be associated with multiple cardiovascular risk factors (3–7), and have linked atherosclerosis with myocardial infarction, stroke, and sudden cardiac death. The atherosclerotic disease process often begins in childhood (5,8) and it is associated with traditional cardiovascular risk factors such as hypertension, obesity, and dyslipidemia in the pediatric population. Children with CKD manifest many, if not all, of these risk factors. In addition, children with CKD manifest many nontraditional cardiovascular risk factors such as altered mineral metabolism, which places them at even greater risk for cardiovascular disease (CVD). Medial deposition of calcium and phosphorus and the resulting increase in vascular stiffness and BP further contribute to the high prevalence of both hypertension and left ventricular hypertrophy in these children (9). These children are therefore at significant risk for experiencing a cardiovascular event by early adulthood (10); in fact, CVD is the leading cause of death in young adults with childhood-onset ESRD (11,12). Risk identification and reduction is therefore of paramount importance among this group of children.
In adults, assessment of atherosclerosis via carotid B-mode ultrasound imaging is a useful adjunct in quantifying cardiovascular risk (13). This imaging determines the carotid intima-media thickness (cIMT). Increased cIMT is a valid predictor of cardiovascular events in adults (2,14) and as such, measurement of cIMT is currently recommended by the American Heart Association for risk stratification in adults whose cardiovascular risk is not clear or is intermediate (15).
Despite these advancements in cardiovascular risk assessment among adults, the evaluation of cIMT is not part of the recommended screening of children at increased cardiovascular risk (16) in part due to lack of clear evidence linking cIMT to atherosclerosis. However, there is a growing body of literature demonstrating increased cIMT in children with CKD (17,18). In addition, among children, increased cIMT is associated with hypertension, obesity, diabetes, and metabolic syndrome and is affected by interventions to decrease cardiovascular risk such as statin therapy, diet, and exercise (15). In this study, we sought to identify the traditional and nontraditional cardiovascular risk factors associated with increased cIMT in children with mild to moderate CKD by utilizing data acquired from participants of the Chronic Kidney Disease in Children (CKiD) study.
Materials and Methods
Study Population
From April 2005 through September 2009, 586 children with mild to moderate CKD were enrolled in the CKiD study, a multicenter, prospective cohort study conducted at 48 pediatric nephrology centers across North America. Five centers participated in the cIMT substudy and the 133 CKiD participants enrolled at any of these centers were eligible for this study. The study design and conduct for the CKiD study were approved by an external advisory committee appointed by the National Institutes of Health and by the internal review boards for each participating center. Each participating family provided informed consent according to local requirements.
Details of the CKiD study design have been previously published (19). Briefly, eligible children were aged 1–16 years, and had a Schwartz-estimated GFR between 30 and 90 ml/min per 1.73 m2 (20,21). B-mode ultrasound measurement of cIMT to assess risk for CVD is conducted every other year, concurrent with collection of other clinical variables and performance of a measured GFR determined by the plasma disappearance of iohexol.
cIMT Measurements
Standardized protocol imaging to measure cIMT was conducted at each of the five participating clinical sites. The measurements obtained at the 12-month follow-up visit were used in this analysis because this was the first visit in which cIMT was measured. To achieve standardization and uniformity of carotid artery images, qualifying recordings from all local sites were sent for measurements to the Cardiovascular Core Imaging Research Laboratory (Cincinnati, OH), where they were certified. In addition, cIMT measurements from 97 healthy pediatric controls, recruited from families of Cincinnati Children’s Hospital personnel, were obtained at the Imaging Laboratory in Cincinnati between January 2003 and December 2008. These images were obtained by the same vascular sonographer who obtained the cIMT images for CKiD at the Cincinnati site, utilizing the same equipment, software, and technique as for the CKiD study.
During the imaging, participants were supine, with their neck hyperextended and turned 30–45 degrees contralaterally to the probe. The bilateral mid common carotid artery was imaged in transverse and longitudinal planes using a 5- to 12-MHz linear array transducer, and measured for two-dimensional diameter at peak systole and end diastole. The intima-media thickness of the bilateral distal common carotid artery was measured along the far wall using the point-to-point method. Three measurements were obtained on each side by a single, registered vascular sonographer, and these six values were then averaged, yielding the overall cIMT measurement. Measurements obtained in this manner are reproducible in children, with a coefficient of variation ranging from 8.4% to 11.6% (22).
Primary Exposures
The exposures examined were obtained from the 12-month follow-up visit concurrent with the cIMT measure, unless otherwise stated, and included the following: (1) hypertension, indicated by the average systolic or diastolic age-, sex-, and height-specific BP index ≥1 (BP index is the measured systolic or diastolic BP divided by the 95th age-, sex-, and height-specific percentile BP (16) and a value ≥1 is consistent with hypertension), or the participant reported hypertension and/or antihypertensive medication use at baseline or the 12-month follow-up visit; (2) age- and sex-specific body mass index (BMI) z score (23); (3) dyslipidemia, defined as high density lipoprotein (HDL) cholesterol <40 mg/dl, non-HDL cholesterol >160 mg/dl, or triglycerides >130 mg/dl (24); (4) glomerular CKD diagnosis; (5) iohexol-based GFR, although an estimated GFR (25) was used in place of missing iohexol-based GFR in 5% of participants; (6) birth weight (≥2500 g versus <2500 g); (7) pubertal status, indicated by Tanner stage II–V versus prepubertal status, indicated by Tanner stage I (26); (8) height in meters; (9) serum total calcium in milligrams per deciliter (average of baseline and 12-month follow-up measurements); and (10) serum phosphorus in milligrams per deciliter (average of baseline and 12-month follow-up measurements). The following demographic variables were also included: age, sex, and race (nonwhite versus white). Data from the baseline visit were used in place of missing data at the 12-month follow-up study visit for at least one exposure in 14% of the study participants.
In addition, we conducted several secondary analyses to further examine the association of dyslipidemia and hypertension with cIMT by separating both variables into their composite parts.
Statistical Analyses
The median and interquartile range (IQR) were used to summarize the central location and variability of all continuous variables. Percentages were used to summarize categorical variables. Quantile regression models (27) were used to compare the differences in the 50th, 75th, 90th, and 95th percentiles of the cIMT distribution in our subset of CKiD participants to those of healthy controls with and without adjustment for age, sex, and race. Because the distribution of cIMT measurements did not deviate significantly from a normal distribution, we used multivariable linear regression to quantify the association between cIMT and both the primary exposures and demographic variables. A two-sided P value <0.05 was considered statistically significant. Statistical analyses were conducted using SAS 9.2 software (SAS Institute, Cary, NC).
Results
Of the 133 potential CKiD participants, 108 (81%) had completed the 12-month visit with a valid cIMT measurement available. Our final study population was composed of 101 (94%) study participants for whom data were available on all exposures of interest.
Table 1 shows the characteristics of our study population and the 366 CKiD participants who did not participate in the cIMT substudy. Our study population was slightly more male (70% versus 58%), white (79% versus 66%), more dyslipidemic (55% versus 43%), and had a longer median duration of CKD (8.9 versus 7.1 years) than the rest of the CKiD cohort without cIMT measurements. The median age of the substudy participants was 12.4 years, and the majority of participants had a nonglomerular cause of CKD (85%), were hypertensive (76%), and were dyslipidemic (55%); none were diabetic. The median GFR was 42.9 ml/min per 1.73 m2 (IQR, 28.9–54.0). As shown in Table 2, compared with our study population, the controls were less likely to be male (55% versus 70%; P=0.02), less likely to be overweight/obese (7% versus 26%; P=0.001), and had lower systolic BP (104 mmHg versus 109 mmHg; P=0.01) and BP index (0.87 versus 0.90; P=0.01) and lower diastolic BP (59 mmHg versus 64 mmHg; P<0.001) and BP index (0.76 versus 0.80; P=0.001).
Table 1.
Descriptive statistics at the 12-month follow-up visita of the 101 children in the cIMT substudy included in analyses and the remaining 366 children in the CKiD cohort
| Characteristic | cIMT Substudy Cohortb (n=101) | CKiD Cohort without cIMT (n=366) | P Value |
|---|---|---|---|
| Age (yr) | 12.4 (8.5–15.3) | 11.7 (8.2–15.9) | 0.60 |
| Male sex | 71 (70) | 211 (58) | 0.02 |
| White race | 80 (79) | 243 (66) | 0.01 |
| Height (m) | 1.48 (1.24–1.63) | 1.43 (1.23–1.60) | 0.15 |
| Tanner stage II–V | 59 (58) | 176 (48) | 0.07 |
| Birth weight ≥2500 g | 82 (81) | 297 (81) | 0.90 |
| Duration of CKD (yr) | 8.9 (5.0, 12.4) | 7.1 (4.0–10.7) | 0.01 |
| Nonglomerular CKD etiology | 86 (85) | 284 (78) | 0.10 |
| GFR (ml/min per 1.73 m2) | 42.9 (28.9–54.0) | 44.6 (33.7–58.2) | 0.07 |
| BMI z score | 0.09 (−0.55 to 1.08) | 0.38 (−0.38 to 1.08) | 0.20 |
| BMI ≥85th percentile | 26 (26) | 95 (26) | 0.90 |
| Dyslipidemiac | 56 (55) | 159 (43) | 0.03 |
| HDL cholesterol <40 mg/dl | 28 (28) | 67 (18) | 0.04 |
| HDL cholesterol (mg/dl) | 45 (39–53) | 48 (41–57) | 0.06 |
| Non-HDL cholesterol >160 mg/dl | 18 (18) | 56 (15) | 0.50 |
| Non-HDL cholesterol (mg/dl) | 128 (109–151) | 125 (106–146) | 0.30 |
| Triglycerides >130 mg/dl | 41 (41) | 117 (32) | 0.10 |
| Triglycerides (mg/dl) | 119 (86–162) | 102 (73–141) | 0.01 |
| Hypertensiond | 77 (76) | 274 (75) | 0.80 |
| Systolic BP (mmHg)e | 109 (102–114) | 106 (99–112) | 0.02 |
| Systolic BP indexf | 0.90 (0.84–0.94) | 0.88 (0.83–0.93) | 0.09 |
| Diastolic BP (mmHg)e | 64 (58–69) | 66 (60–72) | 0.03 |
| Diastolic BP indexf | 0.80 (0.74–0.87) | 0.84 (0.76–0.93) | 0.001 |
| Taking antihypertensive medicationg | 71 (70) | 248 (68) | 0.60 |
| Calciume, mg/dl | 9.7 (9.5–9.9) | 9.6 (9.4–9.9) | 0.70 |
| Phosphoruse, mg/dl | 4.8 (4.2–5.1) | 4.6 (4.2–5.0) | 0.10 |
Data are median (interquartile range) or n (%). cIMT, carotid intima-media thickness; CKiD, Chronic Kidney Disease in Children study; BMI, body mass index.
Used baseline data if data were missing at 12-month follow-up visit.
Cincinnati Children’s Hospital and Medical Center (Cincinnati, OH; n=26), University of Texas (Houston, TX; n=26), British Columbia Children’s Hospital (Vancouver, BC; n=24), Children’s Mercy Hospital (Kansas City, MO; n=19), and Nationwide Children’s Hospital (Columbus, OH; n=13).
HDL cholesterol <40 mg/dl, non-HDL cholesterol ≥160 mg/dl, or triglycerides ≥130 mg/dl.
Defined as having an average systolic or diastolic BP from the baseline and 12-month follow-up visits ≥95th age-, sex-, and height-specific percentile, or if the participant reported hypertension at baseline or the 12-month follow-up visit, or if the participant reported using antihypertensive medication at baseline or at the 12-month follow-up visit.
Average of values from baseline and 12-month follow-up.
Measured systolic or diastolic BP/95th age-, sex-, and height-specific percentile BP; a value ≥1 is elevated. The average index from the baseline and 12-month follow-up is reported.
Used antihypertensive medication at the baseline or 12-month follow-up visit.
Table 2.
Descriptive statistics of the 97 healthy controls compared with 101 CKiD cIMT substudy participants
| Characteristic | Healthy Controls (n=97) | cIMT Substudy Cohort (n=101) | P Valuea |
|---|---|---|---|
| Age (yr) | 10.1 (7.9–13.7) | 12.4 (8.5–15.3) | 0.08 |
| Male sex | 53 (55) | 71 (70) | 0.02 |
| White race | 71 (73) | 80 (79) | 0.30 |
| Weight (kg) | 34.6 (25.7–50.0) | 42.9 (26.4–57.8) | 0.20 |
| Height (m) | 1.41 (1.27–1.59) | 1.48 (1.24–1.63) | 0.50 |
| BMI (kg/m2) | 17.3 (16.1–20.2) | 18.9 (16.2–22.7) | 0.10 |
| Overweight/obese (BMI ≥85th percentile) | 7 (7) | 26 (26) | 0.001 |
| Systolic BP (mmHg) | 104 (98–113) | 109 (102–114) | 0.01 |
| Diastolic BP (mmHg) | 59 (55–64) | 64 (58, 69) | <0.001 |
| Systolic BP indexb | 0.87 (0.82–0.91) | 0.90 (0.84–0.94) | 0.01 |
| Diastolic BP indexb | 0.76 (0.7–0.81) | 0.80 (0.74–0.87) | 0.001 |
Data are median (interquartile range) or n (%). CKiD, Chronic Kidney Disease in Children study; cIMT, carotid intima-media thickness; BMI, body mass index.
P value from Wilcoxon rank sum test when medians were compared, and P value from Pearson χ2 when percentages were compared.
Measured systolic or diastolic BP/95th age-, sex-, and height-specific percentile BP; a value ≥1 is elevated.
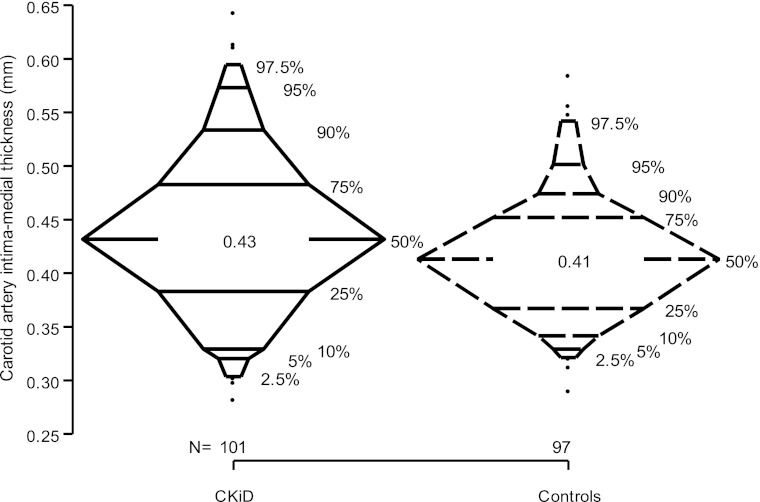
The median cIMT of our study population was 0.43 mm, significantly higher (P=0.03) than the median cIMT of 0.41 mm in the healthy controls (Figure 1). The two distributions were similar up to the 25th percentile; however, in addition to the median cIMT being greater in the CKiD group than in the normal controls, the 75th percentile (0.48 versus 0.45), 90th percentile (0.53 versus 0.48), and 95th percentile (0.57 versus 0.51) were also larger in the CKiD participants. These significant differences persisted after adjusting for differences in age, sex, and race.
Figure 1.
Box-percentile plots illustrating the distribution of cIMT measurements in 101 Children of the CKiD and in 97 healthy controls. The numerical values of the 50th percentile are shown. The 2.5th, 5th, 10th, 25th, 75th, 90th, 95th, and 97.5th percentiles of the distribution are denoted. cIMT values <2.5th percentile or >97.5th percentile are denoted by closed circles. cIMT, carotid artery intima-medial thickness; CKiD, Chronic Kidney Disease in Children study.
Table 3 shows the results of univariate and multivariable linear regression analyses quantifying the association of each primary exposure with cIMT. After adjustment, dyslipidemia and hypertension were associated with a 0.05 mm (95% CI, 0.01–0.08) and 0.04 mm (95% CI, 0.003–0.08) greater mean cIMT, respectively. Each additional 10 cm in height was associated with an average of 0.03 mm (95% CI, 0.003–0.05) greater cIMT. No other exposures were significantly associated with cIMT.
Table 3.
Correlates of cIMT in 101 children of the CKiD cohort study
| Characteristic | Mean Difference in cIMT, mm (95% CI) | |
|---|---|---|
| Unadjusted | Adjusted | |
| Age (per 5-yr increase) | 0.003 (−0.02 to 0.02) | −0.06 (−0.13 to 0.004) |
| Male sex (versus female) | −0.01 (−0.04 to 0.02) | −0.03 (−0.06 to 0.01) |
| Nonwhite race (versus white) | −0.001 (−0.04 to 0.04) | −0.002 (−0.04 to 0.04) |
| Height (per 0.1-m increase) | 0.002 (−0.004 to 0.01) | 0.03 (0.003–0.05) |
| Tanner stage II–V (versus stage I) | 0.000 (−0.03 to 0.03) | −0.02 (−0.08 to 0.03) |
| Birth weight ≥2500 g (versus <2500 g) | 0.01 (−0.03 to 0.05) | 0.02 (−0.03 to 0.06) |
| Glomerular CKD etiology (versus nonglomerular) | 0.004 (−0.04 to 0.05) | −0.02 (−0.07 to 0.03) |
| GFR (per 10 ml/min per 1.73 m2 decrease) | 0.003 (−0.01 to 0.01) | −0.002 (−0.01 to 0.01) |
| BMI z score | −0.001 (−0.01 to 0.01) | −0.01 (−0.02 to 0.003) |
| Dyslipidemiaa | 0.04 (0.01–0.07) | 0.05 (0.01–0.08) |
| Hypertensionb | 0.03 (−0.003 to 0.07) | 0.04 (0.003–0.08) |
| Calcium (per 1-mg/dl increase) | −0.004 (−0.03 to 0.02) | −0.004 (−0.04 to 0.03) |
| Phosphorus (per 1-mg/dl increase) | −0.01 (−0.03 to 0.01) | −0.01 (−0.04 to 0.01) |
Data are median (interquartile range) or n (%). cIMT, carotid intima-media thickness; CKiD, Chronic Kidney Disease in Children study; CI, confidence interval; BMI, body mass index.
HDL cholesterol <40 mg/dl, non-HDL cholesterol >160 mg/dl, or triglycerides >130 mg/dl.
Average systolic or diastolic BP from the baseline and 12-month follow-up visits ≥95th age-, sex-, height-specific percentile, or if the participant reported hypertension at baseline or the 1-month follow-up visit, or if the participant reported using antihypertensive medication at baseline or at the 12-month follow-up visit.
Secondary analyses revealed hypertriglyceridemia to be the sole lipid component significantly associated with cIMT (Table 4). In addition, regardless of whether a child had a systolic or diastolic BP in the hypertensive range, taking an antihypertensive medication was associated with an increased cIMT. Analyses also showed increasing diastolic BP to remain associated with cIMT, regardless of antihypertensive use or degree of systolic BP elevation (Table 5).
Table 4.
Univariate and multivariable relationships of components of dyslipidemia and cIMT
| Characteristic | Mean Difference in cIMT, mm (95% CI) | |
|---|---|---|
| Unadjusted | Adjusted | |
| HDL cholesterol <40 mg/dl | 0.03 (−0.004 to 0.06) | 0.03 (−0.02 to 0.07) |
| Non-HDL cholesterol >160 mg/dl | −0.01 (−0.05 to 0.03) | −0.01 (−0.06 to 0.03) |
| Triglycerides >130 mg/dl | 0.03 (−0.002 to 0.06) | 0.04 (0.01–0.08) |
All variables in Table 3, except dyslipidemia, are included in the adjusted model shown here. cIMT, carotid intima-media thickness; CI, confidence interval.
Table 5.
Univariate and multivariable relationships of components of hypertension variable and cIMT
| Characteristic | Mean Difference in cIMT, mm (95% CI) | |
|---|---|---|
| Unadjusted | Adjusted (Full Model) | |
| Average systolic BP indexa | 0.16 (−0.03 to 0.36) | 0.20 (−0.04 to 0.45) |
| Average diastolic BP indexa | 0.21 (0.07–0.36) | 0.16 (0.002–0.32) |
| Taking antihypertensive medication (yes/no) | 0.04 (0.01–0.07) | 0.04 (0.01–0.08) |
All variables in Table 3, except hypertension, are included in the adjusted model shown here. cIMT, carotid intima-media thickness; CI, confidence interval.
Measured systolic or diastolic BP/95th age-, sex-, and height-specific percentile BP; a value ≥1 is elevated. The average index from the baseline and 12-month follow-up is used.
Discussion
This national, multicenter, cross-sectional study of children with mild to moderate CKD as assessed by iohexol clearance is the largest study of cIMT in pediatric stage 2–4 CKD to date. It provides further evidence that children with CKD are at increased cardiovascular risk, because the majority of these children were hypertensive and dyslipidemic, and over a quarter of them were either overweight or obese. In addition, children with CKD had significantly greater cIMT compared with healthy controls, even after adjusting for differences in age, sex, and race.
Other investigators have similarly demonstrated that children with varying degrees of kidney dysfunction have higher cIMT than the general population, with dialysis patients having the most extremely elevated measurements (17,18). What makes our results particularly striking is that this finding still holds among children without extreme kidney dysfunction or ESRD compared with normative data obtained in a more racially diverse, representative group of healthy controls.
In adults, cIMT measurement is considered a valid and reliable assessment of atherosclerotic burden (15,28) that can predict coronary atherosclerosis and its clinical sequelae, such as myocardial infarction and stroke (14,28). In fact, the Atherosclerosis Risk in Communities study demonstrated that among adults aged 45–64 years without clinical coronary heart disease at baseline, those with a cIMT ≥1 mm had a significantly increased hazard for development of coronary heart disease (5.07 for women [95% CI, 3.08–8.36] and 1.85 for men [95% CI, 1.28–2.69]) over the next 4–7 years compared with those with a cIMT <1 mm (29).
Although the Study of Heart and Renal Protection showed that simvastatin-ezetimibe reduced cardiovascular events in adults aged >40 years with CKD, subgroup analysis and other independent studies have failed to show the benefit of lipid-lowering therapy specifically among adults with ESRD (30–33). In part, this may be due to the presence of advanced CVD in that population; however, it may be that other processes are playing a greater role in the development of CVD among individuals with more advanced CKD and ESRD. In our study population of 101 children with mild to moderate CKD (none with ESRD), dyslipidemia and hypertension were the only cardiovascular risk factors found to be significantly associated with increased cIMT. Other traditional and nontraditional cardiovascular risk factors, notably BMI, calcium, and phosphorus were not found to be associated with cIMT. The high prevalence of cardiovascular risk factors and greater cIMT in this cohort of children was not unexpected given the increased cardiovascular mortality seen among children with CKD (11,12). Recently published National Heart, Lung, and Blood Institute (NHLBI) consensus guidelines for cardiovascular health and risk reduction in children and adolescents recommend that children with CKD be considered in the highest tier of cardiovascular risk (34) and be managed aggressively to minimize their risk of developing atherosclerosis and subsequent cardiovascular events. These treatment guidelines, endorsed by the American Academy of Pediatrics, modified the 2006 recommendations made by an expert pediatric panel (35) and include targeting BP <90th percentile, BMI <85th percentile, and lipids <75th percentile (LDL cholesterol ≤100 mg/dl, triglycerides <90 mg/dl, non-HDL cholesterol <120 mg/dl). The previous guidelines published in 2006 by the American Heart Association specifically indicate that these guidelines are intended for children with GFR <15 ml/min per 1.73 m2 or ESRD, whereas the 2011 NHLBI guidelines do not make this distinction and only state that the high-risk group should include children with “chronic kidney disease/end stage kidney disease/post-kidney transplant” (10,35). Our data support the need for the inclusion of children with stage 2–4 CKD in these recommendations because they clearly demonstrate an increased risk for accelerated atherosclerosis. Not only were hypertension and dyslipidemia associated with increased cIMT among children with mild to moderate CKD, but the majority of children in this cohort manifested these cardiovascular risk factors and only 12 children had lipid levels within the recommended target range.
Hypertriglyceridemia was the only lipid abnormality associated with cIMT in this study. Although hypertriglyceridemia has been shown to be associated with atherosclerotic lesions in children and young adults (5), LDL is considered by many to be the major lipid risk factor for atherosclerosis. In fact, many studies in children with familial hypercholesterolemia have not only described this association, but have also shown that pharmacological lowering of LDL can effectively decrease cIMT (34,36–38). Interestingly, hypertriglyceridemia was the most highly prevalent lipid abnormality among our cohort. Only nine children had an LDL as elevated as those seen in the studies of children with familial hypercholesterolemia (LDL ≥155 mg/dl) and only four participants (4%) reported using lipid-lowering medication at the same study visit as the cIMT measurement. The dyslipidemic pattern observed in our cohort mirrors the predominant dyslipidemic pattern seen in childhood, a pattern known to be associated with atherosclerosis: significant hypertriglyceridemia, normal/mild increased LDL, and low HDL (34). Although the pathogenesis and characteristics of dyslipidemia in children with CKD are different than that seen among children with familial hypercholesterolemia, the association between dyslipidemia and cIMT among children with CKD and the high burden of this risk factor further underscore the need for vigilant screening for dyslipidemia among children with CKD. Our findings also suggest that there may be other characteristics unique to CKD that influence the effect of dyslipidemia on the vasculature; future studies utilizing longitudinal follow-up data from CKiD will help to better elucidate the contribution of cholesterol on cIMT.
Although we were not surprised to find an association between hypertension and cIMT, the association of antihypertensive medication use and cIMT after adjusting for degree of BP elevation is particularly interesting. This suggests that children who require an antihypertensive to maintain a certain BP target are at increased cardiovascular risk compared with similar children who achieve the same BP without the use of an antihypertensive. Alternatively, if many of the patient’s antihypertensive agents were initiated relatively recently, our data could reflect a delay between a relatively prompt BP normalization and a slower effect on the vasculature.
We expected to replicate results from prior studies that demonstrated a correlation between increased cIMT and markers of abnormal calcium-phosphorus metabolism (18). As such, the lack of an association between total calcium or serum phosphorus and cIMT in our study was not expected; however, it can likely be explained by the largely normal values of calcium and phosphorus and the mild to moderate nature of CKD in this group (39). Only 28% of children had an average serum phosphorus value that was above published Kidney Disease Outcomes Quality Initiative cut-offs for medical therapy (1 of 37 children aged 6–13 years had a phosphorus >5.8 mg/dl and 27 of 49 children had a phosphorus >4.5 mg/dl) (40). In addition, only 44% of children were taking activated vitamin D and only 35% of children reported taking phosphate binders (26 reported calcium carbonate, 7 reported calcium acetate, and 5 reported sevelamer). Lending further credence to this hypothesis is the fact that we were unable to investigate the association of calcium-phosphorus product with cIMT because only five children had an elevated product. It may also be that for abnormal calcium-phosphorus metabolism to have a detrimental effect on the vasculature, there needs to be a prolonged exposure and/or that calcium and phosphorus abnormalities are more important in the development of abnormal cIMT in children with advanced CKD as opposed to in children with mild to moderate CKD. As the CKiD study progresses, we aim to utilize longitudinal data to investigate this relationship further.
Although this study contributes significantly to the existing knowledge of CVD risk among children with CKD, there are several important limitations to keep in mind. Its cross-sectional nature does not allow one to infer causality, and its relatively small sample size may limit the generalizability of the study results to the overall population of children with mild to moderate CKD. Due to the significant differences between the healthy controls and our study population, one cannot rule out the possibility of residual confounding when interpreting the larger cIMT found in the children with CKD. In addition, althoough we were able to study many risk factors not previously studied in this population of children, we were unable to investigate the effect of inflammatory markers or markers of impaired glucose metabolism.
Despite these limitations, the results presented here add to the growing evidence that children with CKD are at significantly increased cardiovascular risk. They also support the practice of vigilant screening and nutritional counseling to avoid or detect dyslipidemia and hypertension, and underscore the need for future studies designed to investigate the effectiveness of targeted dyslipidemia and hypertension treatment on normalizing cIMT and decreasing adverse cardiovascular outcomes among children with CKD.
Disclosures
None.
Supplementary Material
Acknowledgments
We thank the divisions of pediatric cardiology and the echocardiogram technicians at Cincinnati Children’s Hospital and Medical Center (Cincinnati, OH), University of Texas (Houston, TX), British Columbia Children’s Hospital (Vancouver, BC), Children’s Mercy Hospital (Kansas City, MO), and Nationwide Children’s Hospital (Columbus, OH) for their dedication and important contributions to this study, without which this work could not have been done.
The CKiD study is funded by the National Institute of Diabetes and Digestive and Kidney Diseases with additional funding from the Eunice Kennedy Shriver National Institute of Child Health and Human Development and the National Heart, Lung, and Blood Institute (UO1-DK-66143, UO1-DK-66174, U01-DK-082194, and UO1-DK-66116).
Footnotes
Published online ahead of print. Publication date available at www.cjasn.org.
This article contains supplemental material online at http://cjasn.asnjournals.org/lookup/suppl/doi:10.2215/CJN.03130312/-/DCSupplemental.
References
- 1.Labarthe DR: Atherosclerosis. In: Epidemiology and Prevention of Cardiovascular Diseases: A Global Challenge, edited by Colilla J, Gaithersburg, MD, Aspen Publishers, 1998, pp 29–41 [Google Scholar]
- 2.Toth PP: Subclinical atherosclerosis: What it is, what it means and what we can do about it. Int J Clin Pract 62: 1246–1254, 2008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.D’Agostino RB, Sr, Vasan RS, Pencina MJ, Wolf PA, Cobain M, Massaro JM, Kannel WB: General cardiovascular risk profile for use in primary care: The Framingham Heart Study. Circulation 117: 743–753, 2008 [DOI] [PubMed] [Google Scholar]
- 4.Heiss G, Sharrett AR, Barnes R, Chambless LE, Szklo M, Alzola C: Carotid atherosclerosis measured by B-mode ultrasound in populations: Associations with cardiovascular risk factors in the ARIC study. Am J Epidemiol 134: 250–256, 1991 [DOI] [PubMed] [Google Scholar]
- 5.Berenson GS, Srinivasan SR, Bao W, Newman WP, 3rd, Tracy RE, Wattigney WA: Association between multiple cardiovascular risk factors and atherosclerosis in children and young adults. The Bogalusa Heart Study. N Engl J Med 338: 1650–1656, 1998 [DOI] [PubMed] [Google Scholar]
- 6.Wagenknecht L, Wasserman B, Chambless L, Coresh J, Folsom A, Mosley T, Ballantyne C, Sharrett R, Boerwinkle E: Correlates of carotid plaque presence and composition as measured by MRI: The Atherosclerosis Risk in Communities Study. Circ Cardiovasc Imaging 2: 314–322, 2009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Newman WP, 3rd, Freedman DS, Voors AW, Gard PD, Srinivasan SR, Cresanta JL, Williamson GD, Webber LS, Berenson GS: Relation of serum lipoprotein levels and systolic blood pressure to early atherosclerosis. The Bogalusa Heart Study. N Engl J Med 314: 138–144, 1986 [DOI] [PubMed] [Google Scholar]
- 8.McGill HC, Jr, McMahan CA, Zieske AW, Sloop GD, Walcott JV, Troxclair DA, Malcom GT, Tracy RE, Oalmann MC, Strong JP, The Pathobiological Determinants of Atherosclerosis in Youth (PDAY) Research Group : Associations of coronary heart disease risk factors with the intermediate lesion of atherosclerosis in youth. Arterioscler Thromb Vasc Biol 20: 1998–2004, 2000 [DOI] [PubMed] [Google Scholar]
- 9.Mitsnefes MM: Cardiovascular disease in children with chronic kidney disease. J Am Soc Nephrol 23: 578–585, 2012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.American Academy of Pediatrics : Cardiovascular risk reduction in high-risk pediatric populations. Pediatrics 119: 618–621, 2007 [DOI] [PubMed] [Google Scholar]
- 11.Parekh RS, Carroll CE, Wolfe RA, Port FK: Cardiovascular mortality in children and young adults with end-stage kidney disease. J Pediatr 141: 191–197, 2002 [DOI] [PubMed] [Google Scholar]
- 12.Groothoff JW, Gruppen MP, Offringa M, Hutten J, Lilien MR, Van De Kar NJ, Wolff ED, Davin JC, Heymans HS: Mortality and causes of death of end-stage renal disease in children: A Dutch cohort study. Kidney Int 61: 621–629, 2002 [DOI] [PubMed] [Google Scholar]
- 13.Baldassarre D, Amato M, Pustina L, Castelnuovo S, Sanvito S, Gerosa L, Veglia F, Keidar S, Tremoli E, Sirtori CR: Measurement of carotid artery intima-media thickness in dyslipidemic patients increases the power of traditional risk factors to predict cardiovascular events. Atherosclerosis 191: 403–408, 2007 [DOI] [PubMed] [Google Scholar]
- 14.Lorenz MW, Markus HS, Bots ML, Rosvall M, Sitzer M: Prediction of clinical cardiovascular events with carotid intima-media thickness: A systematic review and meta-analysis. Circulation 115: 459–467, 2007 [DOI] [PubMed] [Google Scholar]
- 15.Urbina EM, Williams RV, Alpert BS, Collins RT, Daniels SR, Hayman L, Jacobson M, Mahoney L, Mietus-Snyder M, Rocchini A, Steinberger J, McCrindle B, American Heart Association Atherosclerosis, Hypertension, and Obesity in Youth Committee of the Council on Cardiovascular Disease in the Young : Noninvasive assessment of subclinical atherosclerosis in children and adolescents: Recommendations for standard assessment for clinical research: A scientific statement from the American Heart Association. Hypertension 54: 919–950, 2009 [DOI] [PubMed] [Google Scholar]
- 16.National High Blood Pressure Education Program Working Group on High Blood Pressure in Children and Adolescents : The fourth report on the diagnosis, evaluation, and treatment of high blood pressure in children and adolescents. Pediatrics 114[Suppl 4th Report]: 555–576, 2004 [PubMed] [Google Scholar]
- 17.Litwin M, Wühl E, Jourdan C, Trelewicz J, Niemirska A, Fahr K, Jobs K, Grenda R, Wawer ZT, Rajszys P, Tröger J, Mehls O, Schaefer F: Altered morphologic properties of large arteries in children with chronic renal failure and after renal transplantation. J Am Soc Nephrol 16: 1494–1500, 2005 [DOI] [PubMed] [Google Scholar]
- 18.Mitsnefes MM, Kimball TR, Kartal J, Witt SA, Glascock BJ, Khoury PR, Daniels SR: Cardiac and vascular adaptation in pediatric patients with chronic kidney disease: Role of calcium-phosphorus metabolism. J Am Soc Nephrol 16: 2796–2803, 2005 [DOI] [PubMed] [Google Scholar]
- 19.Furth SL, Cole SR, Moxey-Mims M, Kaskel F, Mak R, Schwartz G, Wong C, Muñoz A, Warady BA: Design and methods of the Chronic Kidney Disease in Children (CKiD) prospective cohort study. Clin J Am Soc Nephrol 1: 1006–1015, 2006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Schwartz GJ, Haycock GB, Edelmann CM, Jr, Spitzer A: A simple estimate of glomerular filtration rate in children derived from body length and plasma creatinine. Pediatrics 58: 259–263, 1976 [PubMed] [Google Scholar]
- 21.Schwartz GJ, Gauthier B: A simple estimate of glomerular filtration rate in adolescent boys. J Pediatr 106: 522–526, 1985 [DOI] [PubMed] [Google Scholar]
- 22.Urbina EM, Kimball TR, McCoy CE, Khoury PR, Daniels SR, Dolan LM: Youth with obesity and obesity-related type 2 diabetes mellitus demonstrate abnormalities in carotid structure and function. Circulation 119: 2913–2919, 2009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Centers for Disease Control and Prevention: Clinical growth charts, 2000. Available at: http://www.cdc.gov/growthcharts/clinical_charts.htm Accessed March 15, 2010
- 24.Saland JM, Ginsberg HN: Lipoprotein metabolism in chronic renal insufficiency. Pediatr Nephrol 22: 1095–1112, 2007 [DOI] [PubMed] [Google Scholar]
- 25.Schwartz GJ, Muñoz A, Schneider MF, Mak RH, Kaskel F, Warady BA, Furth SL: New equations to estimate GFR in children with CKD. J Am Soc Nephrol 20: 629–637, 2009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Johns Hopkins Hospital: Harriet Lane Handbook: A Manual for Pediatric House Officers, 18th Ed., Philadelphia, Mosby Elsevier, 2008 [Google Scholar]
- 27.Koenker R, Hallock K: Quantile regression. J Econ Perspect 15: 143–156, 2001 [Google Scholar]
- 28.Greenland P, Abrams J, Aurigemma GP, Bond MG, Clark LT, Criqui MH, Crouse JR, 3rd, Friedman L, Fuster V, Herrington DM, Kuller LH, Ridker PM, Roberts WC, Stanford W, Stone N, Swan HJ, Taubert KA, Wexler L: Prevention Conference V: Beyond secondary prevention: Identifying the high-risk patient for primary prevention: Noninvasive tests of atherosclerotic burden: Writing Group III. Circulation 101: E16–E22, 2000 [DOI] [PubMed] [Google Scholar]
- 29.Chambless LE, Heiss G, Folsom AR, Rosamond W, Szklo M, Sharrett AR, Clegg LX: Association of coronary heart disease incidence with carotid arterial wall thickness and major risk factors: The Atherosclerosis Risk in Communities (ARIC) Study, 1987-1993. Am J Epidemiol 146: 483–494, 1997 [DOI] [PubMed] [Google Scholar]
- 30.Baigent C, Landray MJ, Reith C, Emberson J, Wheeler DC, Tomson C, Wanner C, Krane V, Cass A, Craig J, Neal B, Jiang L, Hooi LS, Levin A, Agodoa L, Gaziano M, Kasiske B, Walker R, Massy ZA, Feldt-Rasmussen B, Krairittichai U, Ophascharoensuk V, Fellström B, Holdaas H, Tesar V, Wiecek A, Grobbee D, de Zeeuw D, Grönhagen-Riska C, Dasgupta T, Lewis D, Herrington W, Mafham M, Majoni W, Wallendszus K, Grimm R, Pedersen T, Tobert J, Armitage J, Baxter A, Bray C, Chen Y, Chen Z, Hill M, Knott C, Parish S, Simpson D, Sleight P, Young A, Collins R, SHARP Investigators : The effects of lowering LDL cholesterol with simvastatin plus ezetimibe in patients with chronic kidney disease (Study of Heart and Renal Protection): A randomised placebo-controlled trial. Lancet 377: 2181–2192, 2011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Holdaas H, Holme I, Schmieder RE, Jardine AG, Zannad F, Norby GE, Fellström BC, AURORA study group : Rosuvastatin in diabetic hemodialysis patients. J Am Soc Nephrol 22: 1335–1341, 2011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Wanner C, Krane V, März W, Olschewski M, Mann JF, Ruf G, Ritz E, German Diabetes and Dialysis Study Investigators : Atorvastatin in patients with type 2 diabetes mellitus undergoing hemodialysis. N Engl J Med 353: 238–248, 2005 [DOI] [PubMed] [Google Scholar]
- 33.Holdaas H, Fellström B, Jardine AG, Holme I, Nyberg G, Fauchald P, Grönhagen-Riska C, Madsen S, Neumayer HH, Cole E, Maes B, Ambühl P, Olsson AG, Hartmann A, Solbu DO, Pedersen TR, Assessment of LEscol in Renal Transplantation (ALERT) Study Investigators : Effect of fluvastatin on cardiac outcomes in renal transplant recipients: A multicentre, randomised, placebo-controlled trial. Lancet 361: 2024–2031, 2003 [DOI] [PubMed] [Google Scholar]
- 34.Expert Panel on Integrated Guidelines for Cardiovascular Health and Risk Reduction in Children and Adolescents. National Heart, Lung, and Blood Institute : Expert panel on integrated guidelines for cardiovascular health and risk reduction in children and adolescents: Summary report. Pediatrics 128[Suppl 5]: S213–S256, 2011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Kavey RE, Allada V, Daniels SR, Hayman LL, McCrindle BW, Newburger JW, Parekh RS, Steinberger J, American Heart Association Expert Panel on Population and Prevention Science. American Heart Association Council on Cardiovascular Disease in the Young. American Heart Association Council on Epidemiology and Prevention. American Heart Association Council on Nutrition, Physical Activity and Metabolism. American Heart Association Council on High Blood Pressure Research. American Heart Association Council on Cardiovascular Nursing. American Heart Association Council on the Kidney in Heart Disease. Interdisciplinary Working Group on Quality of Care and Outcomes Research : Cardiovascular risk reduction in high-risk pediatric patients: A scientific statement from the American Heart Association Expert Panel on Population and Prevention Science; the Councils on Cardiovascular Disease in the Young, Epidemiology and Prevention, Nutrition, Physical Activity and Metabolism, High Blood Pressure Research, Cardiovascular Nursing, and the Kidney in Heart Disease; and the Interdisciplinary Working Group on Quality of Care and Outcomes Research: Endorsed by the American Academy of Pediatrics. Circulation 114: 2710–2738, 2006 [DOI] [PubMed] [Google Scholar]
- 36.Wiegman A, Hutten BA, de Groot E, Rodenburg J, Bakker HD, Büller HR, Sijbrands EJ, Kastelein JJ: Efficacy and safety of statin therapy in children with familial hypercholesterolemia: A randomized controlled trial. JAMA 292: 331–337, 2004 [DOI] [PubMed] [Google Scholar]
- 37.Rodenburg J, Vissers MN, Wiegman A, van Trotsenburg AS, van der Graaf A, de Groot E, Wijburg FA, Kastelein JJ, Hutten BA: Statin treatment in children with familial hypercholesterolemia: The younger, the better. Circulation 116: 664–668, 2007 [DOI] [PubMed] [Google Scholar]
- 38.Guardamagna O, Restagno G, Rolfo E, Pederiva C, Martini S, Abello F, Baracco V, Pisciotta L, Pino E, Calandra S, Bertolini S: The type of LDLR gene mutation predicts cardiovascular risk in children with familial hypercholesterolemia. J Pediatr155: 199–204 e2, 2009 [DOI] [PubMed] [Google Scholar]
- 39.Chen NX, O’Neill KD, Duan D, Moe SM: Phosphorus and uremic serum up-regulate osteopontin expression in vascular smooth muscle cells. Kidney Int 62: 1724–1731, 2002 [DOI] [PubMed] [Google Scholar]
- 40.National Kidney Foundation: K/DOQI clinical practice guidelines for bone metabolism and disease in children with chronic kidney disease. Am J Kid Dis 46[Suppl 1]: 1–122, 2005 [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.