Abstract
The complexity of structure and functions of the Temporomandibular Joint (TMJ) make the diagnosis of its diseases/disorders difficult. Remarkable progress made in the field of imaging of this joint led us to compare four imaging modalities viz. plain radiographs, CT scan, MRI and ultrasound. We found that MRI was most specific and sensitive for interpretation of soft tissue and inflammatory conditions in the joint, whereas CT examination produced excellent image for osseous morphology and pathology. Plain X-rays are useful for destructive bony changes and sonography is a good in aid in diagnosing disc derangement and is very economical.
Keywords: CAT scan, MRI, plain radiography, TMJ, ultrasonography
INTRODUCTION
The remarkable progress and increasing sophistication in the imaging of the Temporomandibular Joint (TMJ) seems to have added to the confusion among practitioners as to when and what imaging should be used, if at all. Further all imaging techniques are not equally effective for many conditions in which the TMJ is involved.
Obtaining an image by itself means little unless effective, standardized interpretation is available. It is with the intention to compare the transpharyngeal view X-ray, CT scans, MRI and ultrasound with the Clinical Diagnostic Criteria (CDC)[1] and to possibly lay down interpretation of these that this study was undertaken.
Review of literature
TMJ disorders are a heterogeneous collection of signs and symptoms that can be generally characterized by the presence of pain, TMJ noise and limitation of jaw motion. They have largely been classified into structural/organic (ankylosis, trauma, infection, neoplasia or arthritis) and functional (pain, joint noise or limitation of joint movement) and various diseases that affect the TMJ including congenital and developmental malformations of the mandible and / or cranial bones and acquired disorders.[2]
The National Center for Devices and Radiological Health of the Food and Drug Administration (USA), in 1979, recommended that the imaging examination must be capable of providing the desired information regarding patient's internal anatomy or physiology, and the radiographic information sought, even if negative or normal, is expected to be significantly useful in the medical management of the patient.
The efficacy of any imaging examination rests not just with its technical adequacy but also with its diagnostic accuracy, as a complex interaction exists between the image and the person interpreting it.[3] Additionally, increasing sophistication of imaging technique does not guarantee better management of the patient.[4]
Rudisch et al,[5] evaluated the CDC for TMJ disorders against the MRI diagnosis of TMJ internal derangement and osteoarthritis in a patient group, and it was observed that the classification system of the CDC for TMJ disorders are not sufficiently reliable for determining TMJ internal derangement and osteoarthritis; further that a clinical diagnosis of internal derangement type 3 may need to be supplemented by evidence from an MRI to determine functional disc condyle relationship. However, in a long-term study of patients (55 TMJs), with history of osteoarthrosis and internal derangement, it was observed that 30 years after initial diagnosis there were few clinical signs of osteoarthritis and internal derangement although MRI findings were extensive.[6]
In a comparison of MR images of 28 patients with those of respective arthrograms, it was found that the anatomic configuration of the meniscus as seen with MR correlated directly with normal variations of the anterior recess seen with arthography.[7]
The description of the use of CAT in the evaluation of the meniscus of the TMJ was made in 1983. Computerized reconstruction was used extensively and compared with other radio modalities.[8]
High-contrast sensitivity of MRI to tissue differences and the absence of ionizing radiation are the reasons why MRI has replaced CT for imaging soft tissue. Since high-resolution anatomical detail is a feature for TMJ imaging, surface coil imaging is essential for adequate investigation.[9]
Since each TMJ is significantly affected by the contralateral joint, it has been advocated to simultaneously image TMJ bilaterally, which allows the assessment of side to side differences in a range of motions and joint structure at the identical points of mouth opening for either side.[10] MRI may assist the clinician in determining whether primary or delayed treatment is indicated in cases of trauma to the TMJ. The saggital and coronal MRI of TMJ articulation are complimentary, and this might be important for a full assessment of joint dysfunction.[11] Using high-field strength surface coil MRI to illustrate specific changes associated with disc derangement, trauma and previous surgery, other information obtained includes the presence of soft tissue ingrowths, fibrosis and joint effusions.[12] In patients with inflammatory arthritides, MRI has been shown to demonstrate disc destruction. Gadolinium used as a contrast agent, pannus formation can be detected with active rheumatoid or other inflammatory arthritis.
On comparing CAT and MRI images of 15 fresh TMJ autopsy specimens with cryosection in a blinded fashion, no statistically significant difference between these procedures in detecting bony abnormalities or disc position was found.[13] However, a side by side image analysis demonstrated that MRI depicted the soft tissue anatomy of the joint with greater detail. Further, CAT images could not assess the configuration of the disc and the borderlines between the disc and its attachment, which MRIs did. Single Photon Emission Computed Tomography (SPECT) is particularly sensitive for inflammatory disorders and arthritides but is not specific for these conditions. It is not useful for determining deviation in the form of joint disc displacement, dislocation or ankylosis.[8]
Accuracy for diagnosis of internal derangement, disc displacement with reduction and disc displacement without reduction based on prospective interpretation of high-resolution sonograms was 95%, 92% and 90%, respectively. High-resolution sonography allowed greatly improved diagnostic efficacy because of a more defined tissue differentiation and enhanced near-field clarity.[14] Furthermore, the advantage of dynamic high-resolution sonography in investigating the disc condyle relationship during repeated motion at the respective open-mouth positions probably made these structures more clearly distinguishable.[10]
MATERIALS AND METHODS
This study comprised 10 patients of TMJ disorders who visited the outpatient department of Oral and Maxillofacial Surgery of Gandhi Memorial and Associated Hospitals, CSM Medical University (Erstwhile KGMC), Lucknow. Diagnosis was made on the basis of history, clinical examination and investigations (Routine and Specific).
Routine TMJ X-rays (Transpharyngeal view), CT scan of TMJ in saggital plane in soft tissue mode, MRI (1.5 Tesla) and high-resolution ultrasonography (using 10 MHZ probe) were obtained.
Ultrasound was included later in the study because it has shown encouraging results in other studies;[14] moreover it is much cheaper than MRI, hence more feasible.
The transpharyngeal view radiograph provides a saggital view of the medial pole of the condyle. In our study, these radiographs were taken at standard angulations employing standard technique.
Saggital section CT scans were obtained as per Manzione's et al. (1984) technique.[15] These were obtained by a GE 8800 CT/T machine with scout view and saggital reconstruction capabilities. The blink mode, a computer function that highlights a particular tissue density, was also used. Selection of desired density at random enabled the differentiation between subtle shades of grey that might not be appreciated visually. Scans were obtained in mouth open and mouth closed positions and each section was 2 mm apart. The upper and lower levels of the scan were determined on the lateral scout view, making certain that each condylar head was scanned. About 12–15 sections were obtained for each patient.
MRIs of the TMJ were performed on a 1.5 Tesla MR system of the GE company. Fast scan were used to obtain scout images to determine the image location v/s anatomic part having a scan time of 52 sec. Following detection of the optimal image plane, slow scan were obtained at a higher resolution of the specific anatomic part. Slow scan had a scan time of 256 sec. The initial images were obtained with a saggital plane of focus approximately 1.5 cm deep to the skin surface anterior to the tragus of the ear.
Ultrasonography was performed using a 10-MHz linear array transducer on an HDI 5000 scanner using standardized protocol to obtain cross sections intersecting the anterior–superior joint compartment in a saggital to frontal plane. Optimal visualization was obtained by tilting the transducer. On the sonograms, the disc is visualized as a homogenized hypo to isoechoic band lying adjacent to the inferior relation (overlying the mandible condyle).
Clinical diagnosis was made using CDC.[1] The signs and symptoms noted were as follows: Pain in pre-auricular region (Unilateral/Bilateral), Clicking/Crepitus/Grating Sounds, Deviated/Deflected Jaw Movement, Maximal Mouth Opening (in mm) besides any other symptom.
Imaging assessment was done on the basis of bony changes (Pseudocyst, Osteophyte and Flattening of condylar head), soft tissue changes (Disc Position, Adhesions, Fluid or Inflammatory Changes and Degenerated Disc). The above were clinically co-related and the radiation dose noted.
RESULTS
Internal derangement (ID) type II was most common as per CDC classification of patients at 40% followed by internal derangement type III 30%. Internal derangement type I, Degenerative Joint Disease (DJD) type I and DJD type II was 10%.
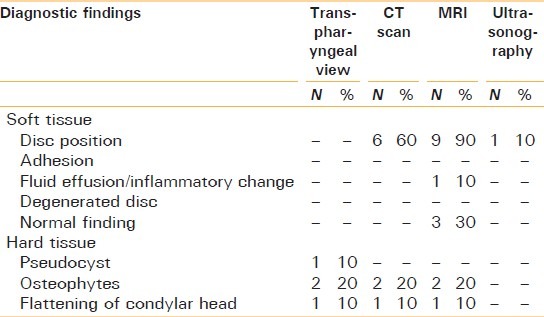
Pseudocyst was found in one patient, osteophytes were interpreted in two patients and flattening of condylar head was seen in one radiograph. The disc position was seen in 6 CT scans. In other scans it could not be determined. Osteophytes were present in 20% patients. Flattening of condylar head were present in 10% patients. By MRJ, disc position was determined in 90% patients. Fluid effusion was seen in 10% patients. Normal findings were seen in 30% patients. Adhesions and degenerated disc were not detected.
Pseudocyst was not appreciated in any patient by MRI. Osteophytes and flattening were present in 20% patients in MRI. Disk position was determined in MRI in 90% patients followed by CT in 60% patients then in ultrasound 10% and could not be appreciated in transpharyngeal view. Fluid effusions were seen in MRI, in one patient. Degenerated disc and adhesion was not interpreted in any patient. Pseudocyst was observed in transpharyngeal view in 10% patients, while it was not detected CT/MRI in the same patient. Osteophytes were detected transpharyngeal view, CT and MRI in 20% patients. In ultrasonography, osteophytes could not be assessed. Flattening of condylar head was observed in transpharyngeal view, CT and MRI in 10% patients while was absent in ultrasound findings.
CT scan was most sensitive diagnostic technique after MRI. Its sensitivity was 83.33% followed by ultrasound 33.33% and transpharyngeal view's sensitivity 0% for soft tissues interpretation. The difference in sensitivity and specificity differed significantly in different techniques (P = 0).
Transpharyngeal view and CT scan were the most sensitive techniques in interpretation of hard tissue against MRI. Their sensitivity was 100% followed by ultrasound (0% for hard tissue interpretation).
The difference in diagnostic interpretation in different techniques was not statistically significant. In soft tissue assessment, sensitivity of transpharyngeal view against MRI was found to be 0% and specificity was 100%. In hard tissue interpretation, sensitivity of transpharyngeal view was found to be 100% and specificity 87.5% against MRI. Interpreting the hard tissue, sensitivity of CT scan against MRI was found to be 100% while specificity was 87.5%. In soft tissue interpretation of three cases, sensitivity of ultrasound against MRI was found to be 33.33% whereas specificity of ultrasonography was 100%. Ultrasonography could not detect any hard tissue, thus its sensitivity to hard tissue was 0% and specificity was 100%.
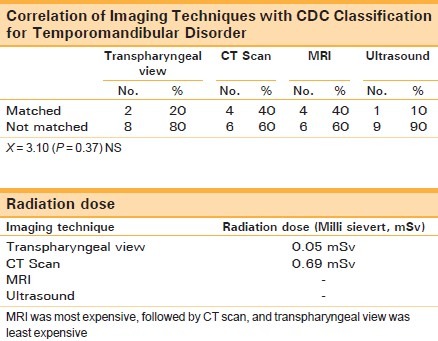
Correlation matched maximum in CT scan and MRI (40%), followed by transpharyngeal view (30%) and minimum in ultrasound (10%) but was statistically non-significant [Tables 1–3].
Table 1.
Demographic, clinical and radiological fi ndings (n = 10)
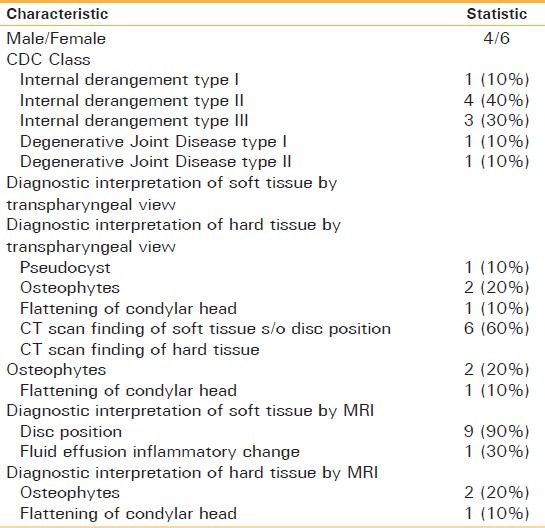
Table 3.
Diagnostic efficacy of different techniques against MRI
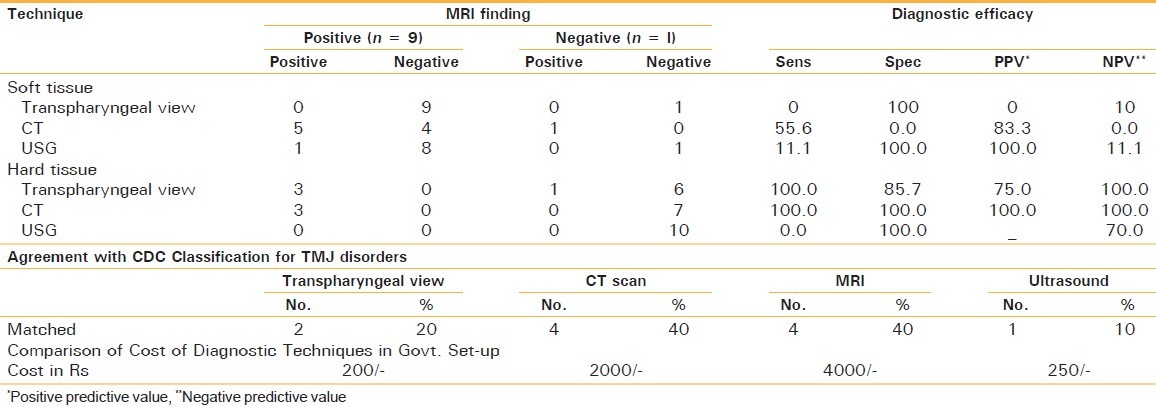
Table 2.
Comparison of different diagnostic techniques
DISCUSSION
Our understanding and interest in the diagnosis and management of patients with various types of TMJ disorders has increased as research has identified structural abnormalities and disease mechanisms associated with some of these disorders. Along with these discoveries, there has also been remarkable progress in the imaging of the TMJ.
The aim of present study was to evaluate the efficacy of transpharyngeal view, X-ray, CT scan and MRI in diagnosing the multitude of TMJ disorders. Ultrasound was not included at the start of our study, but it was included later on as it has shown attractive results.
In our study group of 10 patients, 2 patients were diagnosed as having DJD and rest of the patients were diagnosed as having internal derangement (disc displacement with reduction or without reduction). The patients with DJD were of older age group (above 35 years of age). DJD is the most common disease affecting the TMJ. Radiographic evidence of DJD occurs in 20%.
Internal derangements of the TMJ have been noted in 40–50% of the general population. However, only a fraction of these individuals require interventional treatment. In our study of 10 cases, we diagnosed 8 patients (80%) having internal derangement, based on the CDC.[1] Transpharyngeal view X-ray was of no value in interpreting soft tissue as plain radiographs are unable to depict soft tissue images. In hard tissue interpretation, pseudocyst was diagnosed in one patient in the glenoid fossa, in the same patient flattening of condylar head and osteophytes were found anteriorly. CT scan and MRI interpreted the same findings in the patient. On the other hand, pseudocyst detected in transpharyngeal view of one patient could not be detected by other imaging techniques. This may be explained due to the fact that CT or MRI sections were made 2 mm apart; the portion of condyle having pseudocyst may not be visualized by CT or MRI.
In our study there was no statistically significant difference in efficacy of transpharyngeal view, CT scan or MRI in interpreting hard tissue. Ultrasound was of no value in interpreting hard tissue. MRI was found to be superior to CT scan or transpharyngeal view, in diagnosing DJD.[3] This difference may be due to the fact that our study group was very small. Moreover, MRI shows early subchondral erosion or disc degeneration, more clearly than by other techniques, which are indicative of early osteoarthritis or DJD.
Our patients who were initially diagnosed as having DJD, by CDC, were divided into DJD type I i.e. arthrosis with arthralgia and type II i.e. arthrosis without arthralgia. There was not much difference in their imaging presentation (either by transpharyngeal view, CT scan or MRI), in other words either clinical findings or imaging alone are not sufficient in diagnosing DJD, rather it should be supplemented by laboratory tests (such as for rheumatic factor, etc.), for arriving on definitive diagnosis. In a study of 259 patients, it was found that CT scan was superior than arthrograms in depicting osseous changes.[16] Arthrograms were not within the scope of this study hence not carried out.
Out of 10 patients, disc position could be determined in 6 patients only by CT scan, whereas MRI depicted position of disc in 9 cases. Moreover fluid effusion or inflammatory changes were appreciable in MRI of one patient clinically, who was diagnosed as having internal derangement type III. Adhesion or degenerated disc could not be appreciated in any patient probably because of our small sample size.
In our study, for soft tissue interpretation, MRI was found to be more specific and sensitive than CT. On the other hand, a study has found MRI more specific and equally sensitive to CT scan (15 TMJs) i.e. MRI has shown the configuration of the disc more clearly, thereby causing less false-positive results.[13]
In our study, high-resolution ultrasonography was performed on three patients using 10 MHz probe, but could detect internal derangement in only one patient (33.33%) while MRI detected internal derangement in all the three patients (100%). This finding is in contradiction to that of study of Emshoff et al.,[14] who found internal derangement in 92.3% cases by using ultrasonography. This may be due to the fact that we used 10 MHz probe, whereas Emshoff et al.[14] used 12 MHz probe in sonography. Using ultrasound we could not assess any bony structure clearly.
Transpharyngeal view X-ray correlated in only two cases, which were diagnosed as having DJD as per CDC[1] and were predictable as this view depicted bony structures quite accurately.
Diagnosis made by CT scan and MRI could match only with our four patients’ clinical diagnosis. In the remaining 6 patients, it could not be matched and we had to change our clinical diagnosis. There was no difference in radiographic features of type I or type II internal derangement.
Diagnosis made by transpharyngeal view correlated with clinical diagnosis in 20% cases, by CT scan and MRI, it was 40% whereas diagnosis made by ultrasound correlated with clinical diagnosis only in 10% cases; but this was statistically non-significant (P = 0.37).
Rudisch et al.[5] in their study of 69 patients, who had a clinical diagnosis of unilateral internal derangement type III, compared clinical diagnosis with MRI findings and found that overall diagnostic agreement for internal derangement type III was 78.3%. Most of the disagreement was due to false-positive interpretations of an absence of internal derangement. They concluded that a clinical TMJ-related diagnosis of internal derangement may need to be supplemented by evidence from an MRI to determine the functional disc-condyle relationship [Figures 1–14].
Figure 1.
Closed Mouth Plain Transpharyngeal View X Ray (Left)
Figure 14.
Open Mouth High Resolution Ultra Sonograph (10 MHz Probe) (Right)
Figure 2.

Open Mouth Plain Transpharyngeal View X Ray (Left)
Figure 3.
Closed Mouth Plain Transpharyngeal View X Ray (Right)
Figure 4.
Open Mouth Plain Transpharyngeal View X Ray (Right)
Figure 5.
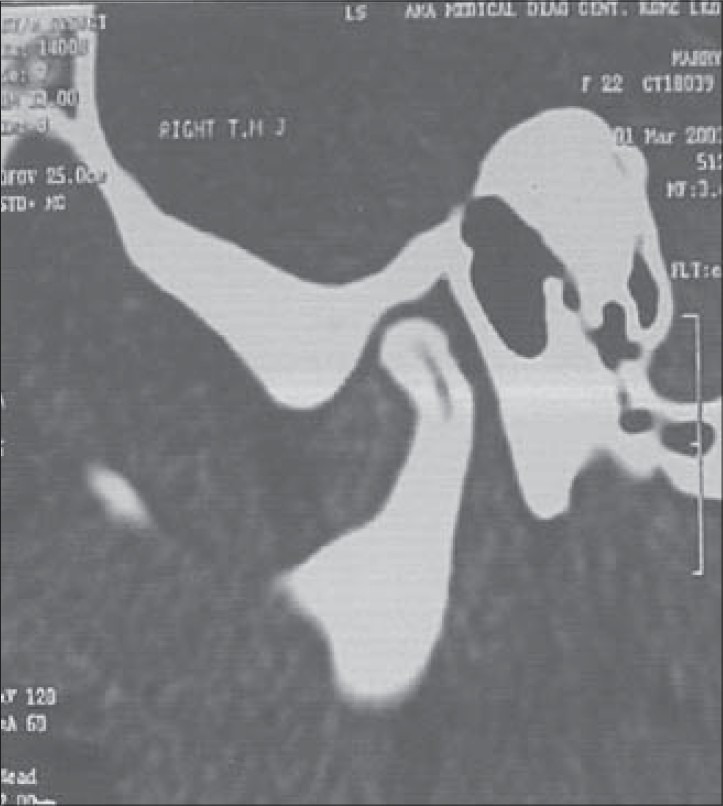
Closed Mouth Saggital Section CT Scan (Right)
Figure 6.
Open Mouth Saggital Section CT Scan (Right)
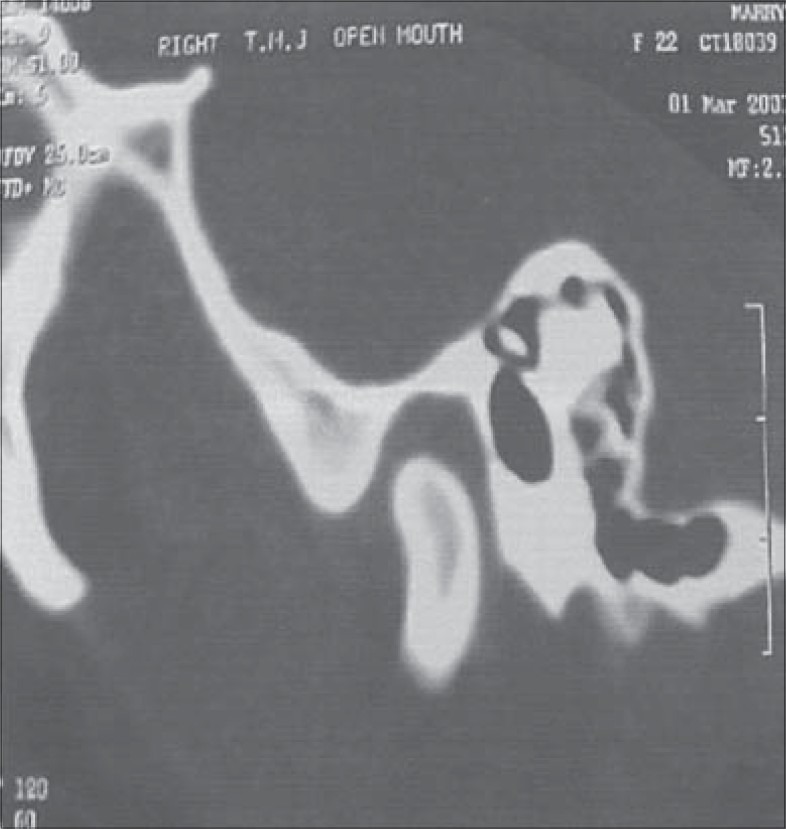
Figure 7.

Closed Mouth Saggital Section CT Scan (Left)
Figure 8.
Open Mouth Saggital Section CT Scan (Left)
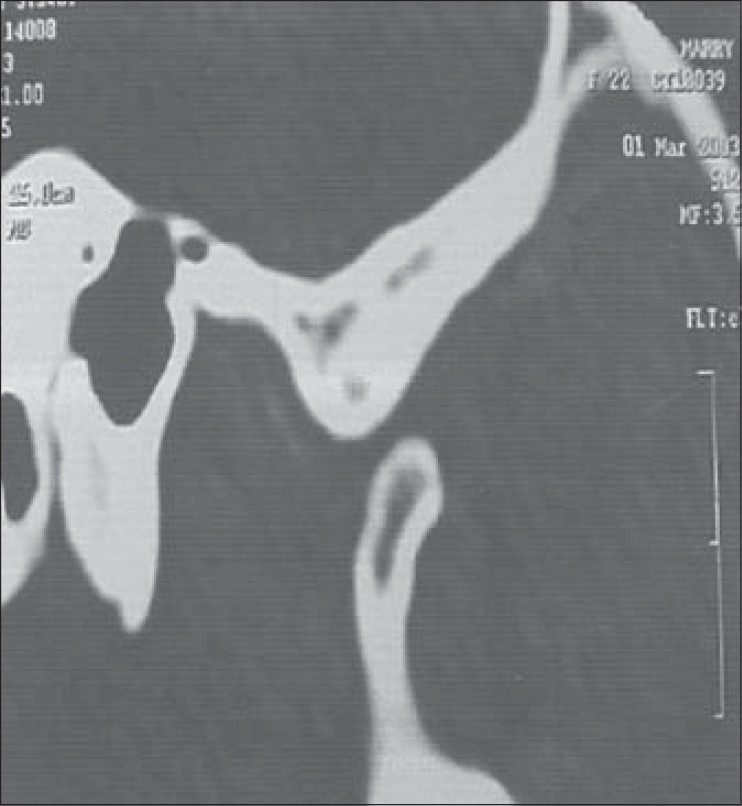
Figure 9.
1.5 Tesla Closed Mouth Saggital Section MRI (Right)
Figure 10.

1.5 Tesla Open Mouth Saggital Section MRI (Right)
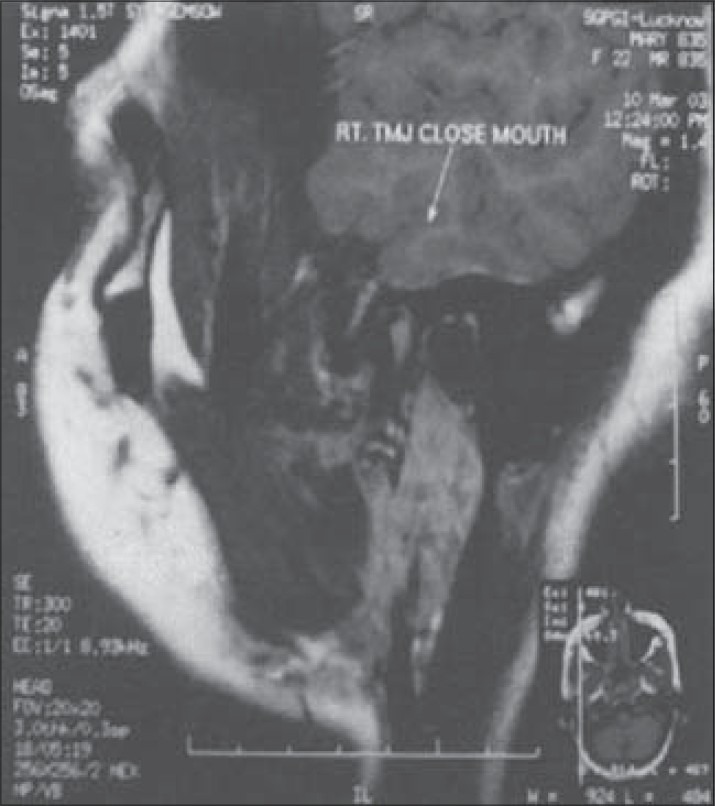
Figure 11.
1.5 Tesla Closed Mouth Saggital Section MRI (Left)
Figure 12.
1.5 Tesla Open Mouth Saggital Section MRI (Left)
Figure 13.
Closed Mouth High Resolution Ultra Sonograph (10 MHz Probe) (Right)
CONCLUSIONS
It was observed that no single imaging modality studied can accurately show all changes in the hard and soft tissues of the joint. MRI provides the most accurate information about the soft tissues of the joint, whereas CAT provides the most accurate information about hard tissues changes. The plain transpharyngeal radiograph provides reasonably accurate information regarding hard tissue changes in the joint. Ultrasonography provides information only about soft tissue and is encouraging from the economic point of view. Although the aims of the study included comparing the imaging results with CDC, it was not possible to correlate with any single imaging modality.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared
REFERENCES
- 1.Truelove EL, Sommers EE, LeResche L, Dworkin SF, Von Korff M. Clinical diagnostic criteria for TMD.New classification permits multiple diagnosis. J Am Dent Assoc. 1992;123:47–54. doi: 10.14219/jada.archive.1992.0094. [DOI] [PubMed] [Google Scholar]
- 2.American Academy of Orofacial Pain. Temporomandibular disorders: guidelines for classification, assessment and management. In: Mc Neil C, editor. Carolstream 12. Chicago: Quintessence Pub. Co; 1993. p. 66. [Google Scholar]
- 3.Brooks SL, Brand JW, Gibbs SJ, Hollender L, Lurie AG, Omnell KA, et al. Imaging of the Temporomandibular Joints, Position Paper of the American Academy of Oral and Maxillofacial Radiology. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 1997;93:609–18. doi: 10.1016/s1079-2104(97)90128-1. [DOI] [PubMed] [Google Scholar]
- 4.Fryback DG. The efficacy of diagnostic imaging. Med Decis Making. 1991;11:88–94. doi: 10.1177/0272989X9101100203. [DOI] [PubMed] [Google Scholar]
- 5.Rudisch A, Emshoff R. Validity of clinical diagnostic criteria for temporomandibular disorders. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2001;91:50–5. doi: 10.1067/moe.2001.111129. [DOI] [PubMed] [Google Scholar]
- 6.de Leeuw R, Boering G, van der Kuijl B, Stegenga B. Hard and soft tissue imaging of the temporomandibular joint 30 years after diagnosis of osteoarthrosis and internal derangement. J Oral Maxillofac Surg. 1996;54:1270–80. doi: 10.1016/s0278-2391(96)90480-2. [DOI] [PubMed] [Google Scholar]
- 7.Kaplan PA, Tu HK, Williams SM, Lydiatt DD. The temporomandibular joint: MR and arthrographic correlation. Radiology. 1987;165:177–8. doi: 10.1148/radiology.165.1.3628766. [DOI] [PubMed] [Google Scholar]
- 8.Helms CA, Morrish RB, Jr, Kircos LT, Katzberg RW, Dolwick MF. Computed tomography of the meniscus of the temporomandibular joint: preliminary observations. Radiology. 1982;145:719–22. doi: 10.1148/radiology.145.3.7146402. [DOI] [PubMed] [Google Scholar]
- 9.Cirbus MT, Smilack MS, Beltran J, Simon DC. Magnetic resonance imaging in confirming internal derangement of the temporomandibular joint. J Prosthet Dent. 1987;57:488–94. doi: 10.1016/0022-3913(87)90023-0. [DOI] [PubMed] [Google Scholar]
- 10.Canavan D, Gratt BM. Electronic thermography for the assessment of mild and moderate temporomandibular joint dysfunction. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 1995;79:778–86. doi: 10.1016/s1079-2104(05)80316-6. [DOI] [PubMed] [Google Scholar]
- 11.Shellock FG, Pressman BD. Dual surface coil MR imaging of bilateral temporomandibular joints: improvements in the imaging protocol. AJNR Am J Neuroradiol. 1989;10:595–8. [PMC free article] [PubMed] [Google Scholar]
- 12.Matsuda S, Yoshimura Y, Lin Y. Magnetic resonance imaging assessment of the temporomandibular joint in disc displacement. Int J Oral Maxillofac Surg. 1994;23:266–70. doi: 10.1016/s0901-5027(05)80105-5. [DOI] [PubMed] [Google Scholar]
- 13.Westesson PL, Katzberg RW, Tallents RH, Sanchez-Woodworth RE, Svensson SA. CT and MR of the temporomandibular joint: comparison with autopsy specimens. Am J Roentgenol. 1987;148:1165–71. doi: 10.2214/ajr.148.6.1165. [DOI] [PubMed] [Google Scholar]
- 14.Emshoff R, Jank S, Bertram S, Rudisch A, Bodner G. Disc displacement of the temporomandibular joint: sonography versus sonographic imaging. Am J Roentgenol. 2002;178:1557–62. doi: 10.2214/ajr.178.6.1781557. [DOI] [PubMed] [Google Scholar]
- 15.Manzione JV, Katzberg RW, Brodsky GL, Seltzer SE, Mellins HZ. Internal derangements of the temporomandibular joints: diagnosis by direct saggital computed tomography. Radiology. 1984;150:111–5. doi: 10.1148/radiology.150.1.6689751. [DOI] [PubMed] [Google Scholar]
- 16.Helms CA, Kaplan P. Diagnostic imaging of the temporomandibular joint: reccomendations for use of the various techniques. Am J Roentgenol. 1990;154:319–22. doi: 10.2214/ajr.154.2.2105023. [DOI] [PubMed] [Google Scholar]


