Abstract
Pediatric obesity is more prevalent in rural areas, yet rural families may not have access to pediatric obesity treatment programs. Use of new technologies, particularly telemedicine, has proven effective in other behavioral fields, such as psychiatry. This paper reviews the literature on the use of telemedicine in pediatric obesity treatment, and describes one tertiary-care pediatric obesity telemedicine program. We performed a systematic review of the literature from 1990–2011 using the following criteria: pediatric age group, overweight or obesity care or treatment, and use of telemedicine technology. Of 2873 abstracts identified, four studies met all inclusion criteria; all were published after 2008. The limited evidence suggests that telemedicine to be a promising approach to pediatric weight management, particularly for rural families with limited access to treatments. We also provide important lessons learned from one pediatric obesity treatment clinic offering services to rural families via telemedicine. Few studies have examined the use of telemedicine for pediatric obesity treatment, but the available data favor this method for treating rural patients. There are several unique key factors influencing successful delivery of a pediatric obesity telemedicine treatment program. This review identifies a potential avenue for expanded treatment, and highlights the need for further investigation.
Keywords: Obesity, pediatrics, telemedicine, treatment, telehealth
INTRODUCTION
Pediatric obesity affects 17% of children between the ages of 2 and 19(1), and the short(2) and long-term(3, 4) ramifications of this epidemic necessitate effective treatments. In 2007, expert recommendations were published for the assessment, prevention, and treatment of pediatric obesity(5–8); they recommend a staged approach beginning with Prevention Plus (Stage 1) in primary care offices, with a focus on core weight-related behaviors and timely follow-up. Treatment intensity increases with each stage of formal weight management, and higher stages may require unique resources in order to optimally address the severity of each child’s condition. More intense stages of treatment may rely on dietitians and comprehensive weight management teams comprised of multidisciplinary health care providers. Children most in need of treatment may ultimately be referred to tertiary care programs, typically located within pediatric medical centers, where they have access to experienced obesity clinicians, well-established treatment protocols, and if necessary, pharmacologic treatments and bariatric surgery.
Unfortunately, resources for higher levels of care are not commonly available, particularly in rural areas or cities lacking large pediatric health care programs. Advanced stages of treatment require frequent and routine visits: Stage 3 (comprehensive multidisciplinary intervention) is characterized by weekly visits for 2–3 months, then monthly follow-ups; Stage 4 (tertiary-care intervention) operates by protocol, though it is likely to be longer in duration given the nature of such interventions. Frequent visits can be difficult for families that must travel longer distances to treatment facilities. For example, for a family to attend a daytime visit at a clinic located 60 miles away may require interruption of half of their normal daily routine, causing significant time lost from work for the parent and school for the child. Attending an evening program may be equally difficult due to parent work schedules, children’s homework, and dinner and bedtime routines. Because of issues such as these and despite a dire need for treatment, children and families who live further from treatment programs are therefore hindered from participating in potentially life-improving therapies(5–7). Given that obesity affects rural and underserved populations disproportionately(8, 9), more must be done to ensure that children who need treatment are able to receive it, regardless of where they live. As many aspects of pediatric obesity treatment, such as education, counseling, and behavioral therapy, do not require hands-on contact or regular physical exams, technological advancements through telemedicine provide an innovative outlet for reducing health disparities in rural populations and improving access to this type of care.
Research in the field of pediatric mental health provides us with substantial evidence for the use of telemedicine. Pediatric telepsychiatry and telepsychology programs have been employed for nearly two decades, and various studies support their use as effective treatment modalities. In Ontario, Canada, telepsychiatry was found to contribute significantly to the clinical evaluation and treatment of pediatric patients(10). Satisfaction surveys among practitioners in New South Wales, Australia after ten years of telepsychiatry experience demonstrated overall acceptability of telemedicine approaches(11); and interviews with patients and families in the American mid- and north-west revealed that some children preferred such methods of consultation over face-to-face interactions(12). Another telepsychiatry program in the Pacific Northwest was evaluated by patient and provider questionnaires to be feasible and acceptable; however, sustainability was a significant challenge based on low levels of reimbursement(13). A recent review of nine telemedicine studies in pediatric psychology(14) concluded that telepsychiatry services are feasible, cost effective, and satisfying to patients and families, and noted that outcomes may be similar to more traditional encounters. This notion is supported by Nelson, et al, who compared cognitive-behavioral treatment of childhood depression in telemedicine and face-to-face interactions, finding that both methods were equally satisfactory for the patients and families(15). Further, both groups demonstrated similar remission rates of depression (82% overall); and surprisingly, the telepsychiatry group reported a more rapid decline in depressive symptoms compared to the face-to-face group. This difference was postulated to be the result of the novelty of the treatment modality. Overall, experiences in telepsychiatry and telepsychology demonstrate the feasibility and effectiveness of using telemedicine for behavioral interventions, which is highly pertinent to the field of pediatric obesity research given the behavioral nature of treatment approaches.
This review identifies and summarizes existing literature on the use of telemedicine in pediatric obesity treatment, and details how one tertiary-care center has successfully adapted telemedicine to better reach rural areas and expand treatment to underserved populations. For the purposes of this review, telemedicine will be defined as the use of telemonitors at distant sites to allow teleconferencing between providers and patients who are separated geographically. Other modes of electronic communication, including accessing of websites, email or texting, will not be included in this discussion. This definition is consistent with the use of this term in other disciplines, such as psychiatry(15).
REVIEW METHODS
Data Sources and Search Strategy
We conducted a systematic review of Medline (PubMed), PsychINFO, and CINAHL for English-language studies investigating the use of telemedicine in pediatric weight management programs. Search terms included: pediatrics, pediatric obesity, pediatric overweight, childhood obesity, childhood overweight, weight management, obesity treatment, nutrition, and physical activity. Each of these terms was cross-searched with the terms: telemedicine, telehealth, and telecommunications. We also reviewed studies referenced in the original papers and those by authors known in the field. All studies published between 1990 and 2011 were considered.
Study Selection
All studies had to meet these a priori criteria: pediatric age group (below 18 years of age); overweight and obesity care or treatment; and use of telemedicine technology in the research methodology. Though there are inherent differences between prevention and treatment studies, we broadened our search to include both, as there is a dearth of literature on this topic and our goal was to identify studies focusing on the use of telemedicine for addressing weight-related behavioral outcomes. Therefore, we also considered studies of overweight and obesity prevention, as well as reviews and commentaries of such approaches. Studies exclusively related to internet-, text messaging-, and telephone-based interventions with no mention of telemedicine were excluded, as they are beyond the scope of this review. Three investigators (GMC, MBI, JAS) independently screened titles and abstracts of studies identified by the searches. Full articles were obtained if they appeared to meet inclusion criteria or if the titles and abstracts provided insufficient information to determine inclusion. Full-text articles were then reviewed to determine final inclusion in analysis. Disagreement among reviewers was resolved by consensus.
RESULTS
Telemedicine and Pediatric Obesity Treatment
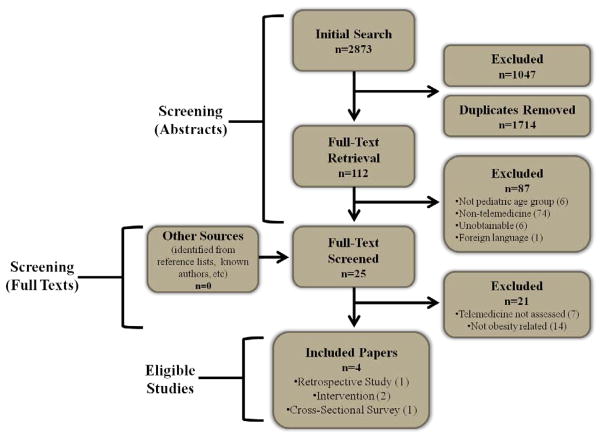
Our search yielded 2873 abstracts, of which 112 studies potentially met inclusion criteria by initial review (Figure 1). Twenty five were included for further full-text review. Of these, four studies met inclusion criteria and were ultimately included; all were published after 2008 (Table 1).
Figure 1.
Literature review search results.
Table 1.
Studies of Telemedicine and Pediatric Obesity
| Author | Site | Study Population | Design & Objectives | Intervention | Outcome Measures | Results | Conclusions |
|---|---|---|---|---|---|---|---|
| Davis (16) | 2 urban and 2 rural schools in Kansas | N = 17 mother-child dyads mean age 9.9yrs (5th grade) Mean BMI %ile: 95% 59% female 47% Caucasian 47% African-American 6% Hispanic Maternal Mean BMI: 32.0 |
Random assignment of families to telemedicine or physician visit Assess the feasibility of conducting family-based pediatric obesity group treatment via telemedicine within a school setting |
Telemedicine intervention: Four 1-hr group sessions over 8 weeks Led by PhD psychologist via telemedicine and school nurse on site Physician Intervention: Single visit to PCP who was given a list of suggested topics to cover |
Feasibility (number of sessions interrupted due to equipment) Parent Satisfaction (survey and attendance) 24hour diet and physical activity recalls Height, weight, BMI |
Feasibility: no technical problems Satisfaction: parents “very satisfied” and attended all sessions Non-significant increase in daily calories; no change in fat calories, fruit/veggie servings, or sugary drinks Non-significant increase in physical activity and decrease in sedentary activity No change in BMI percentile for either group |
Intervention was highly feasible and well received Parents preferred the reduced travel to school location No positive clinical results observed |
| Irby (17) | Brenner FIT Clinic, a tertiary-care weight management program within a children’s hospital; rural remote clinics throughout NW North Carolina (TeleFIT) | Brenner FIT(n=259): Mean age 12.1±3.47 58.7% female 52% Caucasian 41% African American 7% Hispanic Mean BMI 37.1±8.87 Mean BMI z-score 2.584±0.495 TeleFIT (n=35): Mean age 11.2±3.49 60% female 77% Caucasian 20% African American 3% Hispanic Mean BMI 35.6±9.3 Mean BMI z-score 2.6374±0.6299 |
Database review Assess the impact of implementing telemedicine sites in rural areas on patient enrollment, attrition and clinical outcomes |
Brenner FIT: Families attended in-clinic treatment visits 1–2 times per month, face-to-face with multidisciplinary treatment team. TeleFIT: Rural patients attended treatment visits via telemonitor at rural clinical sites 1–2 times per month for real-time “face-to-face” connection with Brenner FIT treatment team at the main clinic location. |
Change in rural patient (>60 miles from clinic) enrollment and outcomes (attrition, BMI z-score) Measured pre- and post-4 months of treatment |
100% attrition in rural families prior to TeleFIT; 30% attrition after implementation of TeleFIT No significant differences at baseline or among those who decreased BMI z-score (64% TeleFIT, 69% Brenner FIT), magnitude of BMI z-score decrease (−0.03, −0.09), or attrition (30%, 32%) at 4 months |
TeleFIT is feasible for reducing rate of attrition among rural families, with comparable outcomes in BMI z-score when compared to patients in traditional clinic program |
| Mulgrew (18) | UC Davis multidisciplinary weight management clinic and rural remote clinics throughout California | N = 54 parents completed questionnaires 25 met inclusion Face-to-Face Group: Mean age 8.1yrs 60% female mean visits 1.9 Telemedicine Group: mean age 6.3yrs 80% female mean visits 1.6 |
Pilot study; cross- sectional survey Assess whether a difference exists in quality of care between face-to-face and telemedicine treatments, measured by parent satisfaction |
Face-to-face Group: Patient and family met with RD and pediatrician specializing in weight management Telemedicine Group: Patient and family met with RD and pediatrician specializing in weight management via telemonitor, with rural healthcare provider present at remote site |
Parent Satisfaction (adapted from 2 previously validated surveys) | Overall parent and provider satisfaction was not statistically significantly different between groups Telemedicine parents were less satisfied with provider’s ability to explain things understandably No differences in scheduling, treatment instructions, or parent’s comfort |
Telemedicine is as effective as face-to-face care for providing patient-centered care Parents are highly satisfied with this approach |
| Shaikh (19) | University affiliated Children’s Hospital at UC Davis 18 rural clinics |
N = 139 children ≤ 18 years old 99 met inclusion 62 with >1 visit mean age 10 ± 3.9 yrs (range, 1–17yo) 63% female mean # visits 2.6 ± 2.0 (range, 1–11) |
Retrospective review of patient medical records Assess whether consultations via telemedicine can improve quality of care, specifically the effect on diagnostic and management decisions and clinical outcomes |
One-on-one patient evaluations by weight management specialist or endocrinologist by telemedicine, with rural health care provider present at remote site | Change in diagnoses, diagnostic evaluations, or treatment Improvement in diet, activity, or weight status (if >1 visit) |
Changes to diagnoses: 77.8% (adding diagnoses) changes to evaluation: 79.8% (sleep studies, psych measures, labs) changes to treatment: 86.9% (parental education, behavior modification, subspecialist referrals, meds) Improvements in diet (80.6%), activity level (69.4%), slowing of weight gain or weight maintenance (21.0%), weight loss (22.6%) |
Telemedicine weight management services can result in changes to care plans and outcomes, perhaps replacing “outreach clinics” |
Davis et al conducted a school-based telemedicine intervention with mother-child dyads to evaluate the feasibility of and satisfaction with the intervention, as well as clinical outcomes such as diet or activity behaviors and weight changes (16). The authors found no change in patient behaviors or weight as the result of intervention; however, parent reports did indicate that the telemedicine approach was very well received, and parents were particularly pleased with the benefits of only having to travel to the child’s school for treatment visits. Irby et al compared patient enrollment, attrition and clinical outcomes from a tertiary care pediatric obesity clinic before and after institution of a telemedicine program (17). After telemedicine implementation, enrollment of families from rural areas increased and the rate of attrition in this population declined. Upon evaluating outcomes in patients seen face-to-face and those seen via telemedicine, no significant differences were found between groups, suggesting that telemedicine may yield comparable benefits to in-person treatments. In a cross sectional survey, Mulgrew et al evaluated parents’ satisfaction with a telemedicine treatment program (18), and found that parents were as satisfied with its ability to deliver patient-centered care as they were with face-to-face approaches. However, parents were not as satisfied with the clinicians’ ability to explain things understandably through this modality. The authors concluded that in this setting, telemedicine is effective for providing patient-centered care. Shaikh et al conducted a retrospective study of 18 rural pediatric clinics to assess evaluation and management decisions in obesity telemedicine programs (19). As a result of telemedicine intervention, changes were frequently made to treatment plans, and there were modest improvements in patient behaviors. However, outcomes for telemedicine patients were not compared to those of patients seen face-to-face. Based on these results, the authors concluded that telemedicine clinics have the potential to replace “outreach” clinics in the future.
DISCUSSION
This is the first systematic review of the use of telemedicine technology in the treatment of pediatric obesity. While only a few studies exist on this topic and they are limited in scope, sample size, and outcomes, they show promise for this field and potential avenues for further study. This initial evidence indicates that telemedicine may be a reasonable mode for reaching geographically isolated families, with possible efficacy for addressing pediatric obesity. One study demonstracted that pediatric obesity treatment via telemedicine appears to be as effective as face-to-face interventions (19). Practitioners have shown interest in this type of care delivery, which appears to improve the quality of patient assessment (19, 20). Importantly, families are both satisfied with this innovative approach and are accepting of the use of telemonitors in treatment. As attrition from weight management programs is a significant problem (21), a positive patient experience is an important component of treatment and is deserving of attention. While these studies are all small and preliminary, the findings indicate potential for eliminating significant barriers to treatment as they relate to rural families and/or those who live at a distance from comprehensive treatment programs. This review highlights the preliminary work in this area, thereby identifying a potential outlet for future clinical work and investigation.
Our findings do not, however, demonstrate efficacy for the use of telemedicine in all populations and settings. In Stage 3 treatment programs, where group settings are more common, telemedicine may not be the most adequate approach for delivering treatment. Due to limitations of the size, cost, and capabilities of telemonitor systems, delivering care in group settings may present more technical challenges, and the group support aspect of such treatments may be lost as a result of less personal interaction. In any setting where telemedicine is used, there is potential for technological issues, particularly in locations with limited bandwidth to support internet connectivity and data transfer between telemonitor systems.
Many other practical issues must also still be examined: Which aspects of behavioral treatment, such as Motivational Interviewing (22), must be modified for telemedicine? What is the optimal mode for disseminating clinical materials via telemedicine, such as educational handouts, food records, and other tangible resources that are otherwise easily delivered during face-to-face treatment visits? Are there aspects of treatment that are more sensitive to face-to-face approaches, or are all treatment components (activity counseling, behavior modification, nutrition education, medical assessment) equally amenable to telemedicine?
Despite these questions, telemedicine is a promising means to reach areas in need of clinical pediatric obesity services. Further research will address these important aspects of telemedicine treatment, though it may take a significant amount of time before experimental evidence can be translated into practice settings. Clinical case reports and experience from established programs can inform future treatment approaches by providing practical considerations, suggestions for addressing barriers, and implications for improved participation and adherence. As demonstrated in our review, we have previously reported our own efforts to better treat rural children and families struggling with obesity within our referral area(17). Using a telemonitor placed within a satellite clinic, enrollment of rural families into treatment increased by three-fold within one year and showed a decrease in rates of attrition. Outcomes in families participating in our telemedicine program are comparable to families seen face-to-face in clinic. Here we share practical aspects of our telemedicine program and provide lessons learned from the process of program development.
BRENNER FIT
Brenner FIT (Families In Training) is a tertiary-care pediatric weight management program located within Brenner Children’s Hospital, a part of Wake Forest Baptist Medical Center. The multidisciplinary team is comprised of a pediatrician, family counselor, dietitian, physical therapist, exercise specialist, and social worker. Brenner FIT accepts patients ages 2–18 with obesity (BMI ≥ 95th percentile for age and gender) and a diagnosis of one or more weight-related comorbidities (hypertension, type 2 diabetes, hyperlipidemia, hypertriglyceridemia, sleep apnea, fatty liver, musculoskeletal complications, Polycystic ovary syndrome), and are referred by their primary care or subspecialty physician. More in-depth descriptions of Brenner FIT, including our treatment approach, have been published elsewhere(21–24).
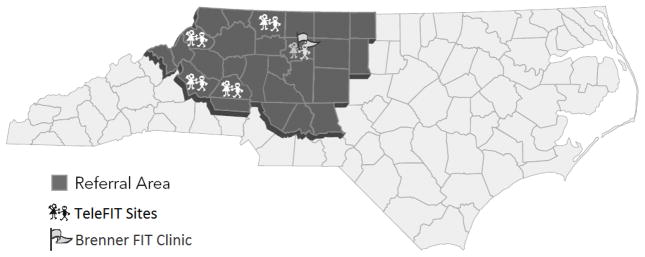
TELEFIT
As described previously(17), Brenner FIT and Brenner Children’s Hospital provides services primarily to a 19 county region in Northwest North Carolina (NWNC). Due to this broad catchment area, including both urban and rural communities, many patients seeking treatment must travel up to 90 miles to attend treatment visits. To address the burden of distance, Brenner FIT established a clinical outreach program (TeleFIT) offering pediatric obesity treatment via telemedicine within four pediatric offices in rural NWNC (Figure 1). Children and their families referred to Brenner FIT who live 45 or more miles from clinic are eligible for TeleFIT. While most treatment visits are conducted via telemonitor, initial intake visits and medical review visits (held once every four months), are held at the Brenner FIT clinic. Follow up visits are conducted by a Brenner FIT dietitian and family counselor every two to four weeks via telemonitor at the TeleFIT location nearest to the family’s residence. Over the one-year period, TeleFIT families must only travel to the Brenner FIT clinic four times; traditional participation in Brenner FIT requires 16 visits to clinic.
Lessons Learned
Telemedicine approaches may not be suitable for all families
In accordance with patient-centered care(23), families referred from rural areas are given the option to participate in TeleFIT or to travel to attend all visits at the Brenner FIT clinic. While some families prefer face-to-face visits, the Brenner FIT team assesses the appropriateness of telemedicine for all families who express interest in TeleFIT at their intake visit. For children with significant mental or physical health issues, in-person visits may be more appropriate for addressing specific treatment concerns, particularly if the child also requires subspecialty care (i.e. pulmonology, cardiology). Additionally, some families not making progress in behavior change via telemedicine may have greater success attending in-person visits. This approach could be attempted if a family is not having success in telemedicine treatment.
Clinicians should demonstrate flexibility in the approach to telemedicine treatment
Flexibility in the use of telemedicine is an important component of treatment for clinicians, particularly in types of visits (in-person versus telemedicine), duration and scheduling of clinic visits, and use of additional clinicians and resources. Though most families meet with the Brenner FIT dietitian and family counselor concurrently via telemonitor, clinicians may occasionally travel to TeleFIT sites to meet with families and facilitate relationship-building, or schedule in-person visits at the Brenner FIT clinic. Families with significant financial, social, and relationship stressors may require more intensive sessions via telemonitor. Telemedicine visits are typically one hour, but may need to be scheduled for longer. To accommodate additional needs, other clinicians and resources may need to be utilized. Typically a dietitian and family counselor work together in each session to address challenges and reduce barriers to change. If other needs arise, resources located within the children’s hospital can be utilized, such as financial assistance, social workers, or clinicians from other clinics (i.e. Cardiology). Often times these other clinicians must be scheduled at future visits, or representatives, such as a nurse in the cardiology clinic, can meet with the family by telemonitor. In our experience, other clinicians and resources are willing to participate readily, but this has only been on a few occasions. This type of flexible collaboration and scheduling allows the clinical team to effectively integrate both nutrition and psychosocial perspectives in each session, without compromising access to additional resources and without requiring additional appointments to be scheduled with multiple care providers.
Positive clinician-family relationships are key in telemedicine treatment
Due to the less-personal feel of the telemedicine approach, there are inherent challenges to building rapport with families. Given the nature of behavioral treatments and the unique issues each family must address during the change process, it is likely that difficult conversations will arise; addressing such concerns via telemonitor is more challenging than with face-to-face interactions. To assist with building rapport and developing trusting relationships with families, the clinical team uses MI, which helps families recognize and overcome potential barriers to treatment. MI also helps to increase the team’s understanding of each family and the specific challenges they face. As the team may not be familiar with resources in the multiple communities served by TeleFIT, this type of communication between clinicians and families also increases clinicians’ understanding of what resources families need and have access to in their specific locations.
An additional challenge to rapport-building is the inherent difficulty in noticing and assessing patients’ emotional reactions via telemonitor, which is greatly influenced by the connection quality between telemonitors. A Metro-E wide area network (WAN) connection, which offers a higher resolution monitor image, allows clinicians to notice more subtle emotional responses. Via commodity network connections, the ability to notice these responses is more challenging due to poor image resolution.
Take advantage of face-to-face visits, opportunities for social interaction, and clinical resources
To foster patient-provider relationships, the treatment team meets with families in person each time they attend a medical review visit with the Brenner FIT physician at the main clinic location. As telemedicine treatment may have a less personal feel, these occasional face-to-face visits give clinicians the opportunity to interact with families without the limitations of the telemonitor. Outside of treatment, TeleFIT families are also encouraged to attend group classes offered by Brenner FIT (i.e., cooking classes, parenting workshops, family fitness opportunities), which expose them to information about behavior change in different, non-clinical settings, as well as to other families participating in treatment. This type of social interaction is useful for reinforcing treatment recommendations delivered by telemedicine and provides families with an encouraging and friendly environment to compliment their treatment. To further facilitate treatment, each family is given a TeleFIT binder with treatment information, teaching handouts, and helpful tools for behavior change. Though each family has their own binder, these additional materials are also available to families at each TeleFIT location and provide visual and tangible teaching aids that clinicians can refer to during each visit.
Partnering with physician practices improves care delivery
Placing telemonitors in rural pediatric practices not only allows families to be treated remotely, but also helps to facilitate communication with a child’s local care providers to create a clinical environment that is supportive of the entire family. Medicaid case managers affiliated with individual practices have provided assistance to the Brenner FIT team, as they are intimately familiar with the families and resources available in the community. Collaborating with pediatric clinics also allows patients to have necessary laboratory work completed at their pediatrician’s office. There are challenges, however, when working remotely with pediatric practices, as facilitating telemedicine treatment requires additional responsibilities on behalf of the administrative and clinical staff at each TeleFIT location. For example, at least one staff member at each practice is needed to coordinate patients’ treatment by bringing families from the waiting area to the telemonitor room or assisting with technical issues. Thus, communication and collaboration between treatment staff and remote practices are essential.
Anticipate technical difficulties and establish protocols to overcome them
Creating a telemedicine program requires frequent collaboration among all clinical and information technology (IT) staff, as telemedicine treatment can be challenging due to the multidisciplinary nature of this approach. Establishing a protocol or a manual of operations for telemedicine treatment is crucial for outlining treatment procedures and trouble-shooting issues that may arise with staff, equipment, and unexpected technology issues. For TeleFIT, liaisons from the treatment team were also designated to facilitate communication between the IT staff at each TeleFIT site and the IT department at the main Brenner FIT location. Connecting to rural communities through TeleFIT requires that IT staff work together to solve technical issues that may arise, which can be complicated by limited financial and personnel resources at each TeleFIT site. Once the efficacy of the telemedicine equipment has been established, using the telemonitors to communicate between sites is relatively simple for both families and providers. However, in the event that technical difficulties prevent connection between the Brenner FIT team and a TeleFIT site at the time of a scheduled visit, the team may have to improvise by conducting treatment visits with families over the telephone. We have done this on several occasions, and having prepared the family to call from the office allows for maximal use of the scheduled meeting time. Therefore, each family is provided with a list of phone numbers and a plan in-case the telemonitor is not working.
CONCLUSION
Pediatric obesity poses a tremendous burden on millions of families in America, many of whom are unable to access effective treatments due to geographic and socio-economic barriers. Use of telemedicine technologies has shown promise for delivering treatments to rural locations in other fields such as psychiatry and psychology, and has done so without compromising patient satisfaction or outcomes. Our review of the use of telemedicine treatment revealed few investigations of this novel approach in pediatric obesity practice; however, even these limited data support telemedicine as a potentially effective mode for delivering treatment.
From our own experience with the TeleFIT program, we recognized several key factors essential to the telemedicine approach in family-based pediatric obesity treatment. First and foremost, though telemedicine may increase access to treatment in rural areas, it is unlikely that this approach will work for all populations. Clinicians must also remain flexible when using this approach, and establish partnerships and protocols to facilitate treatment delivery and prevent technical difficulties. To overcome the less-personalized nature of telemedicine, clinicians should strive to develop relationships with their patients through effective communication techniques, and reinforce treatment recommendations with tangible materials and opportunities for experiential learning and group activity.
Given the current lack of evidence regarding telemedicine treatment in pediatric obesity, more research is warranted. Not only should this approach be tested in relationship to treatment effectiveness and access to quality care, future studies should also focus on reducing technical difficulties, forming partnerships with rural treatment providers, and improving patient satisfaction, as well as discussions with insurance providers regarding reimbursement of services. Larger investigations of the utility of telemedicine in pediatric obesity treatment should continue to evaluate clinical outcomes as well.
Figure 2.
Map of Brenner FIT referral area and TeleFIT sites.
Acknowledgments
Source of support: Dr. Skelton was supported in part through NICHD/NIH Mentored Patient-Oriented Research Career Development Award (K23 HD061597). Kate B. Reynolds Charitable Trust Grant #2009-098, and the Northwest Area Health Education Center.
The authors would like to thank Karen Klein for providing helpful revisions of this manuscript.
Footnotes
Conflict of Interest: The authors have no other financial disclosures to make.
Drs. Cohen and Skelton and Ms. Irby conceptualized the overall review, as well as reviewed the resultant articles and interpretation.
Dr. Cohen and Ms. Irby performed the systematic review of the literature.
Ms. Irby, Boles, and Jordan developed the "lessons learned" and practical applications component of the manuscript.
Drs. Cohen and Skelton and Ms. Irby, Boles and Jordan all participated in the writing of the manuscript, and all approve of the final submitted and published versions.
References
- 1.Ogden CL, Carroll MD, Kit BK, Flegal KM. Prevalence of obesity and trends in body mass index among US children and adolescents, 1999–2010. JAMA. 2012;307:483–490. doi: 10.1001/jama.2012.40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Dietz WH. Health consequences of obesity in youth: childhood predictors of adult disease. Pediatrics. 1998;101:518–525. [PubMed] [Google Scholar]
- 3.Must A, Strauss RS. Risks and consequences of childhood and adolescent obesity. Int J Obes Relat Metab Disord. 1999;23 (Suppl 2):S2–11. doi: 10.1038/sj.ijo.0800852. [DOI] [PubMed] [Google Scholar]
- 4.Franks PW, Hanson RL, Knowler WC, Sievers ML, Bennett PH, Looker HC. Childhood obesity, other cardiovascular risk factors, and premature death. N Engl J Med. 2010;362:485–493. doi: 10.1056/NEJMoa0904130. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Levey LM, Curry JP, Levey S. Rural-urban differences in access to Iowa child health services. J Rural Health. 1988;4:59–72. doi: 10.1111/j.1748-0361.1988.tb00313.x. [DOI] [PubMed] [Google Scholar]
- 6.Saywell RM, Jr, Zollinger TW, Schafer ME, Schmit TM, Ladd JK. Children with special health care needs program: urban/rural comparisons. J Rural Health. 1993;9:314–325. doi: 10.1111/j.1748-0361.1993.tb00527.x. [DOI] [PubMed] [Google Scholar]
- 7.Merwin E, Snyder A, Katz E. Differential access to quality rural healthcare: professional and policy challenges. Fam Community Health. 2006;29:186–194. doi: 10.1097/00003727-200607000-00005. [DOI] [PubMed] [Google Scholar]
- 8.Eberhardt MS, Pamuk ER. The importance of place of residence: examining health in rural and nonrural areas. Am J Public Health. 2004;94:1682–1686. doi: 10.2105/ajph.94.10.1682. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Hartley D. Rural health disparities, population health, and rural culture. Am J Public Health. 2004;94:1675–1678. doi: 10.2105/ajph.94.10.1675. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Boydell KM, Volpe T, Kertes A, Greenberg N. A review of the outcomes of the recommendations made during paediatric telepsychiatry consultations. J Telemed Telecare. 2007;13:277–281. doi: 10.1258/135763307781644889. [DOI] [PubMed] [Google Scholar]
- 11.Starling J, Foley S. From pilot to permanent service: ten years of paediatric telepsychiatry. Journal of Telemedicine and Telecare. 2006;12:80–82. [Google Scholar]
- 12.Sulzbacher S, Vallin T, Waetzig EZ. Telepsychiatry improves paediatric behavioural health care in rural communities. J Telemed Telecare. 2006;12:285–288. doi: 10.1258/135763306778558123. [DOI] [PubMed] [Google Scholar]
- 13.Myers KM, Valentine JM, Melzer SM. Feasibility, acceptability, and sustainability of telepsychiatry for children and adolescents. Psychiatr Serv. 2007;58:1493–1496. doi: 10.1176/ps.2007.58.11.1493. [DOI] [PubMed] [Google Scholar]
- 14.Van Allen J, Davis AM, Lassen S. The use of telemedicine in pediatric psychology: research review and current applications. Child Adolesc Psychiatr Clin N Am. 20:55–66. doi: 10.1016/j.chc.2010.09.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Nelson EL, Citarelli M, Cook D, Shaw P. Reshaping health care delivery for adolescent parents: healthy steps and telemedicine. Telemed J E Health. 2003;9:387–392. doi: 10.1089/153056203772744725. [DOI] [PubMed] [Google Scholar]
- 16.Davis AM, James RL, Boles RE, Goetz JR, Belmont J, Malone B. The use of TeleMedicine in the treatment of paediatric obesity: feasibility and acceptability. Matern Child Nutr. 2011;7:71–79. doi: 10.1111/j.1740-8709.2010.00248.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Irby MB, Boles KA, Jordan C, Skelton JA. TeleFIT: Adapting a Multidisciplinary, Tertiary-Care Pediatric Obesity Clinic to Rural Populations. Telemed J E Health. 2012 doi: 10.1089/tmj.2011.0117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Mulgrew KW, Shaikh U, Nettiksimmons J. Comparison of parent satisfaction with care for childhood obesity delivered face-to-face and by telemedicine. Telemed J E Health. 2011;17:383–387. doi: 10.1089/tmj.2010.0153. [DOI] [PubMed] [Google Scholar]
- 19.Shaikh U, Cole SL, Marcin JP, Nesbitt TS. Clinical management and patient outcomes among children and adolescents receiving telemedicine consultations for obesity. Telemed J E Health. 2008;14:434–440. doi: 10.1089/tmj.2007.0075. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Shaikh U, Nettiksimmons J, Romano P. Pediatric obesity management in rural clinics in California and the role of telehealth in distance education. J Rural Health. 2011;27:263–269. doi: 10.1111/j.1748-0361.2010.00335.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Skelton JA, Beech BM. Attrition in paediatric weight management: a review of the literature and new directions. Obesity Reviews. 2011;12:e273–281. doi: 10.1111/j.1467-789X.2010.00803.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Miller WR, Rollnick S. Motivational Interviewing: Preparing People for Change. Guilford Press; New York, NY: 2002. [Google Scholar]
- 23.Institute of Medicine CoQHCiA. Crossing the Quality Chasm: A New Health System for the 21st Century. National Academy Press; Washington, D.C: 2001. [PubMed] [Google Scholar]