Abstract
The frequency of overweight and obesity among North American Indian children and youth exceeds that of other ethnic groups in the United States. This observation is based on studies using body mass index as the primary measure of overweight and obesity. In the mid-20th century, there were regional differences among North American Indian groups in sub-adults’ size and shape and only a few Southwestern groups were characterized by high rates of overweight and obesity. In most populations, the high prevalence of overweight and obesity developed in the last decades of the 20th century. Childhood obesity may begin early in life as many studies report higher birth weights and greater weight-for-height in the preschool years. Contributing factors include higher maternal weights, a nutritional transition from locally caught or raised foods to store bought items, psychosocial stress associated with threats to cultural identity and national sovereignty, and exposure to obesogenic pollutants, all associated to some degree with poverty. Obesity is part of the profile of poor health among Native Americans in the US and Canada, and contributes to woefully high rates of diabetes, cardiovascular disease, and early mortality. Interventions that are culturally appropriate are needed to reduce weights at all points in the lifespan.
INTRODUCTION
As high as the rates of overweight and obesity are in the non-Native US population, the rates are even higher among Native Americans (Centers for Disease Control and Prevention, 2004, 2011; Indian Health Service, 1998, 2002; Ogden et al., 2002, 2003; Story et al., 1999, 2003). In communities surveyed by the Racial and Ethnic Approaches to Community Health (REACH) 2010 Risk Factor Survey, more than one-third of US Native American men and women are obese whereas approximately one-fifth of adults were obese on the national level.
Even before the national trend in pediatric obesity was clear, many findings indicated that Native American children were stockier than other US children, placing them in higher weight percentiles than height percentiles of the US reference values. Although this stockiness varies with age and to some degree with region, the prevalence of overweight and obesity is now widespread in Native American youth (Caballero et al., 2003; Eisenmann et al., 2000; Hanley et al., 2000; Story et al., 1999, 2003; Zephier et al., 2006). The basis for this conclusion is the data on weight-for-height, usually described as BMI (body mass index, defined as weight in kilograms/height in meters squared). Data on skinfold thickness and other indicators of body composition are very sparse and insufficient to describe characteristic patterns of Native American children and youth as a population. A few studies provide information on the contribution of adipose tissue components to the pattern of overweight and obesity evident from the more prevalent BMI data. Nevertheless, the Native American population of North America is extremely diverse, occupying a wide range of climates, ecological zones, and varying in degree of acculturation or integration with mainstream US and Canadian society. Generalizations about this diverse population are provided with caution.
This review and analysis has organized information by age group to employ a life course approach to the development of overweight and obesity, and by year when the children were measured to provide some sense of secular change. We further organize the information on school age youth by ecological area because growth patterns of North American Native American children and youth have varied significantly among ecological zones (Schell et al., 2006). In general, we emphasize studies of larger samples and of peoples who have been studied several times (Fig. 1).
Fig. 1.

Areas where studies referenced in the text were conducted.
We employ the BMI cutoffs employed by the Centers for Disease Control and Prevention (CDC) to distinguish between conditions of overweight and obesity in children, but adopt the more commonly used labels. Overweight is defined as having a weight-for-height equal to, or greater than the 85th percentile but less than the 95th percentile of National Center for Health Statistics (NCHS) reference population. Obese is defined as a weight-for-height greater than or equal to the 95th percentile of the NCHS reference population (Flegal et al., 2004; Ogden et al., 2003). Some studies report measures of overweight and obesity differently and we identify those departures from the standard definitions when necessary.
Our concentration is on North American Indian populations. Because of the fluid terminology used in studies of American Indians over the past century, some terminological clarification is required. Several terms are used in studies that include American Indians. The most common are Native Americans, Aboriginals, First Nations Peoples, and indigenous peoples. These four terms can include Aleut and Inuit (formerly known as Eskimo) peoples, the Canadian Metis people as well as American Indians. The term American Indian is narrower and does not include Aleut, Inuit or Metis. As much as possible we seek to distinguish results that pertain to Native Americans (Indians, Metis, Aleut, Inuit) from those pertaining specifically to American Indians, but in order to be as accurate as the authors of the reports we cite, we have to use the terms used by those authors. Thus, descriptions of Native Americans could refer to American Indians and the other groups, but description of American Indians does not include the other groups. When the term Native American is used, we try as much as possible to indicate which groups in addition to American Indians are included.
BIRTH SIZE
While the path to obesity begins before birth, the earliest physical measurements of that path are made at birth. Data on weight at birth of American Indians come from numerous studies and demonstrate much variation. An early and very comprehensive report used data from births between July 1964 and June 1969 recorded by the US Public Health Service and obtained from the Health Records Branch of the Division of Indian Health. Mean birth weights were presented by tribe within nine linguistic groups using data from 37,435 infants (the frequencies of LBW (low birth weight, a birth weight less than 2,500 g) or HBW (high birth weight, a birth weight of 4,000 g or more) were not reported) (Adams and Niswander, 1973). Overall, means were substantially greater than those of non-Native comparison groups. The range of American Indian means across tribes was 3.19 through 3.60 kg for boys and 3.09 to 3.48 kg for girls. Since this comprehensive report was published more than 50 years ago, other studies have reported distributions that are similar to those of White Americans while others support the conclusion that American Indian and Alaskan Native birth weight distribution are shifted higher with higher rates of HBW and fewer or similar rates of LBW (Table 1) (Armstrong et al., 1998; Dyck and Tan, 1995; Indian Health Service, 1997; Luo et al., 2004; Martin et al., 2011; Munroe et al., 1984; Thomson, 1990; Vanlandingham et al., 1988; Ventura et al., 1998). A striking example is the Canadian Cree. Of more than 2,000 births between 1994 and 2000, the rate of LBW was 2.4% while the rate of HBW was 36.5% (Willows et al., 2011). Overall, births to American Indians vary over time, by region and by degree of rural isolation.
TABLE 1.
Birth size of American Indians
| Tribal name or location | n | When measured | LBW% | HBW% |
|---|---|---|---|---|
| Northern Saskatchewan predominantly First Nationsa | 10,709 | 1975–1988 | 16.3 | |
| Native Americans from six states (Alaska, Arizona, Montana, New Mexico, North Dakota, South Dakota)b | 15,559 | 1980 | 5.7 | 9.9 |
| British Columbia First Nationsc | 4723 | 1982–1986 | 5.8 | 15.9 |
| James Bay Creed | 2718 | 1985–1995 | 2.3 | 36.1 |
| Creee | 2127 | Jan 1994 to Dec 2000 | 2.4 | 36.5 |
| United States (American Indian or Alaska Native)f | 100,016 | 1994–1996 | 6.7 | 12.7 |
| United States (American Indian only)g | 37,880 | 1996 | 6.5 | 12.3 |
| United States (American Indian or Alaska Native)h | 48,665 | 2009 | 7.3 | 9.7 |
| Comparision: US Whitesh | 3,173,293 | 2009 | 7.1 | 8.5 |
Size at birth among northern tribes tends to be larger than that of non-Native comparison groups (Adams and Niswander, 1967; Caulfield et al., 1998; Moffatt, 1984), and lower birth weights are associated with tribes living in the Southwest: Apache and Navajo, Uto-Aztecans, Zuni, and Tanoan and Keresan (Adams and Niswander, 1968; Adams et al., 1970). The exceptions to this generalization are the Pima, Papago and Mohave who are southwestern and had large mean birth weights (Adams et al., 1970).
More recent reports indicate that the north/south dichotomy may no longer be so clear. Among Saskatchewan American Indian births in the early 1980s, the LBW rate was 6.5 per 1,000 among the American Indian sample, somewhat higher than the rate of 5.2 per 1,000 for the rest of the provincial population (Edouard et al., 1991). In upstate NY, American Indian births recorded from 1980 to 1986, followed a distribution similar to that of upstate white births despite the presence in the American Indian mothers of several important risk factors for poor prenatal growth (Buck et al., 1992). Among a selected sample of southwestern area Mescalero Apache children, only 0.3% were LBW.
More recent analyses demonstrate the role of confounding factors on the wide distribution of American Indian births. After adjusting birth weight for such factors, the rate of LBW appears lower among US American Indian and Alaskan Native births occurring between 1985 and 1997 (Baldwin et al., 2009). Similarly, in a small sample of Canadian Indian births, there was a greater rate of LBW before adjustment for confounders but after adjustment the distribution was more contracted and those rates did not differ (Wenman et al., 2004).
In 1990, birth weights greater than 4,000 g were present in 12.9% of births to US American Indian mothers compared with 10.9% of births to other mothers in the US (National Center for Health Statistics, 1993). Among live births reported between 1994 and 1996, only 6.7% were of LBW; HBW births are relatively more frequent: 12.7% of reported live births were of high birth weight as compared to 10.3% of all races in the US (Indian Health Service, 1997). In 2009, 9.6% of births to American Indians or Alaskan Natives were high birth weight (Martin et al., 2011) (It is possible that the inclusion of Alaskan Natives affects the comparability of the more recent figures with earlier ones on American Indians alone). American Indian births in the US (1995–2001) displayed a wider distribution than those of non-Hispanic whites with significantly higher rates of LBW (5.8 vs. 4.9%) and preterm delivery (11.0 vs. 8.3%) (Alexander et al., 2008). Residence may play a role. Ages and educational attainments of US American Indian mothers vary by region (Alexander et al., 2008). American Indian births in rural, isolated areas of Canada were less likely to be pre-term or LBW compared to urban American Indian births (Luo et al., 2010). American Indian births in counties with a reservation demonstrated lower rates of VLBW (very low birth weight, a birth weight less than 1500g) compared to American Indian births in counties without a reservation suggesting that reporting bias by locale plays a role in the rates (Heck et al., 1999), or that risk factors for poor outcomes are more severe in non-reservation counties. Overall, US Native Americans display higher rates of several risk factors for poor birth outcomes including young maternal age (Martin et al., 2011; Ventura et al., 1998).
In summary, distributions of American Indian births are quite variable, with many displaying high rates of LBW and, or HBW. Adjustment for risk factors may contract the distributions. The risk factors themselves, low maternal age, smoking, late onset of prenatal care, high maternal BMI, diabetes, and others, are themselves often seen as risk factors for poor outcomes including childhood overweight and obesity (Adams et al., 2005). This suggests that the life-course towards obesity in American Indian children is begun in the prenatal period. The tendency for American Indian mothers to have large babies may signal the presence of obesogenic influences operating during gestation and signal a trajectory towards later overweight and obesity.
PRESCHOOL CHILDREN
Studies in the 1960s illustrated two major health issues affecting American Indian preschool children: dietary deficiencies leading to growth retardation and significant underweight (Owen et al., 1969; Reisinger et al., 1972; Story et al., 1998; Van Duzen et al., 1969), with growth rates reported to be well below the national reference at the time. Findings from data obtained in the 1960s showed that an American Indian preschool child, on average, had lower weight-for-height than the average US child of the same age and sex (Table 2). In a small survey of Navajo preschoolers, approximately one-third had reported weights that did not exceed the third percentile, and among Apache preschoolers in Arizona, a large proportion of the children had heights and weights below the 10th percentile (40 and 18%, respectively). Fortunately, through improved health care and increased food availability beginning in the 1970s, problems of underweight and growth retardation have diminished noticeably for the majority of American Indian preschool children.
TABLE 2.
Selected studies describing the prevalence of at risk for overweight and overweight among Native American youth
| Population | Age (years) | Year | Percentage > 85th percentile
|
Percentage > 95th percentile
|
||||
|---|---|---|---|---|---|---|---|---|
| Total | Males | Females | Total | Males | Females | |||
| Preschool children | ||||||||
| CDC PedNSS data (Broussard et al., 1991)a | <5 | 1988 | – | – | – | 11.2 | – | – |
| Mescalero Apache, NM (Gallaher et al., 1991)a | 1–5 | 1988 | – | – | – | 19.5 | – | – |
| Mescalero Apache, NM (Hauck et al., 1992)a | 1–5 | 1988 | – | – | – | 17.9 | – | – |
| Southwest tribe, AZ (Freedman et al., 1992)a | 1–4 | 1990 | – | – | – | 12.0 | – | – |
| Sandy Lake Oji-Cree (Hanley et al., 2000)b | 2–5 | 1994 | – | 34.6 | 45.2 | – | – | – |
| CDC 1999 PedNSS data (CDC, 2001)c | 2–5 | 1999 | 29.3 | 13.7 | ||||
| Pima Indians, Gila River AZ (Lindsay et al., 2002)c | 1–48 mo | 1990–2000 | – | – | – | – | – | – |
| American Indians, WI (Adams et al., 2005)c | 3 | 1997–2001 | 18.7 | 22.2 | ||||
| Okalohoma City Indian Clinic (Stern et al., 2007)c | 2–5 | 1995–2000 | – | 41.5 | 33.3 | – | – | – |
| Nationally representative sample/early childhood longitudinal studyc | 4 | 2005 | – | – | – | 31.2 | 37.0 | 25.8 |
| CDC 2008 PedNSS data (Polhamus, 2009)c | 2–5 | 20.4 | 20.2 | |||||
| CDC 2010 PedNSS data (CDC, 2011)c | 2–5 | 20.1 | 21.1 | |||||
| First Nations and Inuit youth, Canada (MacMillan et al., 2010)c | 0–5 | 1996–1997 | 3.4 | |||||
| Pine Ridge Reservation, SD (Hearst et al., 2011)c | 3–5 | 1998–2002 | 48.9 | – | – | 21.3 | – | – |
| School-age children | ||||||||
| Survey of 3 Native American communities in AZ, ND, and NE (Broussard et al., 1991)c | 6–17 | 1989 | – | 24.5 | 25.0 | – | – | – |
| Devils Lake Sioux, ND (Broussard et al., 1991)d | 9–13 | 1989 | – | 32.1 | 30.6 | – | 3.6 | 6.1 |
| Navajo (Sugarman et al., 1990)d,e | 5–17 | 1989 | – | – | – | – | 12.5 | 11.2 |
| Navajo (Gilbert et al, 1992)d | 14–18 | 1989 | – | 25.0 | 33.0 | – | – | – |
| Midwestern Native American (Gruber et al., 1995)b | 14–19 | 1989 | – | 27.0 | 17.8 | – | 11.3 | 5.1 |
| National survey (Jackson, 1993)d | 5–18 | 1990 | 39.3 | – | – | – | – | – |
| Winnebago and Omaha, NE (Broussard et al., 1991)d | 7–17 | 1990 | – | 32.7 | 34.4 | – | 16.4 | 13.4 |
| Southwest tribe in Arizona (Broussard et al., 1991)d | 14–17 | 1990 | – | 74.6 | 78.3 | – | 44.1 | 51.8 |
| Navajo (Freedman et al., 1997)d | 12–19 | 1991 | – | 35.0 | 40.0 | – | – | – |
| Pueblo Indian (Davis et al., 1993)d | 9–13 | 1991 | 40.4 | – | – | – | – | – |
| Navajo (Davis et al., 1993)d | 9–13 | 1991 | 29.1 | – | – | – | – | – |
| Winnebago and Omaha, NE (Stuart et al., 1994)d | 3–19 | 1992 | 27.0 | – | – | – | – | – |
| Cree (Bernard et al., 1995)f,g | 9–14 | 1992 | 38.0 | – | – | 17.0 | 9.0 | 24.0 |
| Aberdeen area survey (Zephier et al, 1999)d | 5–17 | 1995 | – | 39.1 | 38.0 | – | 22.0 | 18.0 |
| Sandy Lake Oji-Cree (Hanley et al., 2000)b | 2–19 | 1994 | – | 27.7 | 33.7 | – | – | – |
| Sandy Lake Oji-Cree (Hanley et al., 2000)b | 6–9 | 1994 | – | 30.0 | 30.3 | – | – | – |
| Sandy Lake Oji-Cree (Hanley et al., 2000)b | 10–14 | 1994 | – | 23.5 | 32.1 | – | – | – |
| Sandy Lake Oji-Cree (Hanley et al., 2000)b | 15–19 | 1994 | – | 18.6 | 26.6 | – | – | – |
| Navajo (Eisenmann, 2000)h | 6–12 | 1996 | – | 41.0 | 41.1 | – | 15.2 | 21.1 |
| Navajo (Eisenmann, 2000)h | 6–9 | 1996 | – | 39.5 | 44.3 | – | 14.8 | 22.8 |
| Navajo (Eisenmann, 2000)h | 10–12 | 1996 | – | 43.6 | 36.6 | – | 16.0 | 18.7 |
| Ojibwa–Cree, Manitoba (Young et al., 2000)c | 4–19 | 1995–1997 | 60.0 | 64.0 | 34.0 | 40.0 | ||
| 7 Native American Communities (Caballero et al., 2003)d | 7–8 | 1997 | 48.9 | 46.4 | 51.5 | 28.6 | 26.8 | 30.5 |
| White Mountain Apache (Caballero et al., 2003)d | 7–8 | 1997 | – | 44.1 | 44.8 | – | 29.6 | 24.8 |
| San Carlos Apache (Caballero et al., 2003)d | 7–8 | 1997 | – | 43.2 | 55.3 | – | 22.5 | 26.6 |
| Sicangu Lakota (Caballero et al., 2003)d | 7–8 | 1997 | – | 51.4 | 52.3 | – | 29.2 | 27.7 |
| Oglala Lakota (Caballero et al., 2003)d | 7–8 | 1997 | – | 49.7 | 53.6 | – | 24.5 | 35.5 |
| Navajo (Caballero et al., 2003)d | 7–8 | 1997 | – | 38.8 | 42.1 | – | 20.5 | 23.4 |
| Gila River, Pima-Maricopa (Caballero et al., 2003)d | 7–8 | 1997 | – | 50.0 | 74.4 | – | 27.3 | 53.5 |
| Tohono O-odham (Caballero et al., 2003)d | 7–8 | 1997 | – | 66.7 | 73.6 | – | 49.4 | 50.0 |
| Hopi (Eisenmann et al., 2003)i | 6–12 | No date | 23.0 | 22.7 | 23.6 | 24.0 | 22.6 | 24.0 |
| Anishinaabe (Gray et al., 2003)c | 5–18 | No date | 63.0 | |||||
| Akwesasne Mohawk (Gallo et al., 2005)c | 10–16 | 1997 | 26.3 | 26.9 | 25.7 | 33.0 | 40.0 | 25.7 |
| Canadian Aboriginals-off reserve (Shields, 2005)c | 2–17 | 2004 | 21.0 | 20.0 | ||||
| Aberdeen area survey (Zephier et al, 2006)d | 5 | 2002–2003 | 47.4 | 40.5 | 24.2 | 24.1 | ||
| Aberdeen area survey (Zephier et al, 2006)d | 5–17 | 2002–2003 | 48.1 | 46.3 | 29.4 | 26.1 | ||
| James Bay Cree, Quebec (Willows et al., 2007)c | 5 | 2002 | 27.5 | 37.4 | 40.5 | 34.2 | ||
| Pima and Tohono O’odham, Gila River, AZ (Franks et al., 2007)c | 5–9 | No date | 22.0 | 37.0 | ||||
| Pima and Tohono O’odham, Gila River, AZ (Franks et al., 2007)c | 10–14 | No date | 26.0 | 43.0 | ||||
| Pima and Tohono O’odham, Gila River, AZ (Franks et al., 2007)c | 15–19 | No date | 32.0 | 44.0 | ||||
| Pima and Tohono O’odham, Gila River, AZ (Franks et al., 2007)c | 5–19 | No date | 28.0 | 39.0 | ||||
| Okalohoma City Indian Clinic (Stern et al., 2007)c | 6–12 | 1995–2000 | 61.1 | 38.4 | ||||
| First Nation, Metis, Inuit (Katzmarzyk, 2008) | 2–17 | 2004 | 13.4 | 18.3 | 17.8 | 21.4 | ||
| St. Paul, MN/Project EAT (DeLong et al., 2008)c | 12–18 | 1998–1999 | 40.6 | 43.3 | 38.9 | |||
| Northern Plains (Jollie-Trottier et al., 2008) | 8–12 | 2003–2004 | 19.7 | 32.8 | ||||
| Navajo youth (Dabelea et al., 2009)c | <20 | 2001–2005 | 25.0j | 67.7k | ||||
| Northern Arapaho and Eastern Shosone (Smith et al., 2009)c | 8–14 | 2005–2007 | 62 | 56.6 | ||||
| Aboriginal, Saskatchewan (Anderson et al., 2010)i | 8–17 | 2005–2006 | 47.8l | 50.0l | ||||
| American Indians (Singh et al., 2010)c | 10–17 | 2003 | 41.7 | 20.1 | ||||
| American Indians (Singh et al., 2010)c | 10–17 | 2007 | 38.2 | 22.9 | ||||
| First Nations & Inuit youth, Canada (MacMillan et al., 2010)c | 6–11 | 1996–1997 | 5.9 | |||||
| First Nations & Inuit youth, Canada (MacMillan et al., 2010)c | 12–19 | 1996–1997 | 10.1 | |||||
| Indigenous Canadians-off reserve (Khalil et al., 2010)c | 2–17 | 2004 | 21.0 | 20.0 | ||||
| James Bay Cree (Khalil et al., 2010) | 9–13 | 2005–2007 | 13.2 | 19.3 | ||||
| James Bay Cree (Khalil et al., 2010) | 14–18 | 2005–2007 | 54.4 | 38.6 | ||||
| California (Madsen et al., 2010) | 8–17 | 2001–2008 | 33.5 | 32.8 | 17.8 | 15.1 | ||
| Pine Ridge Reservation, SD (Hearst et al., 2011)c | 6–8 | 1998–2002 | 44.3 | 22.5 | ||||
| Pine Ridge Reservation, SD (Hearst et al., 2011)c | 9–11 | 1998–2002 | 45.8 | 24.5 | ||||
| Pine Ridge Reservation, SD (Hearst et al., 2011)c | 12–14 | 1998–2002 | 48.4 | 28.9 | ||||
| Pine Ridge Reservation, SD (Hearst et al., 2011)c | 15–19 | 1998–2002 | 40.0 | 22.7 | ||||
| Pine Ridge Reservation, SD (Hearst et al., 2011)c | 3–19 | 1998–2002 | 45.9 | 45.8 | 26.2 | 22.3 | ||
Weight-for-height > 95th percentile NCHS reference population (obese).
NHANES III reference population (age- and sex-specific BMI).
CDC 2000 reference population (age- and sex-specific BMI).
NHANES II reference population (age- and sex-specific BMI).
Weight-for-age ≥ 95th percentile NCHS reference population.
NHANES I 90th percentile used to define overweight.
BMI ≥ 95% NHANES I reference population.
NHANES I reference population (age- and sex-specific BMI).
International reference proposed by the IOTF (Cole et al., 2000).
Diagnosed with Type I diabetes.
Diagnosed with Type II diabetes.
Overweight/obesity at post-peak height velocity.
Conversely, a rapid increase in overweight and obesity emerged some 20 years ago as a major public health concern among young children of Native American communities. Findings from the CDC Pediatric Nutrition Surveillance System for Native Americans in 1987 show high rates of obesity (11.2%) among all Native American children 0–4 years of age participating in public health programs with nearly 15% of the 1-year-olds determined to be obese (Broussard et al., 1991). Among Mescalero Apache preschool children measured in 1987 or 1988, nearly 20% were overweight (Gallaher et al., 1991). Similarly, a study of Navajo children less than 2 years of age reported mean BMI that were from 9.1 to 24.4 percentiles above the NCHS/CDC age-specific means (Peck et al., 1987).
Studies of American Indian children conducted since 2000 demonstrate that the average American Indian preschooler is clearly at greater risk for overweight and obesity compared to other preschoolers in the US (Anderson and Whitaker, 2009; Hanley et al., 2000; Harvey-Berino and Rourke, 2003; Hearst et al., 2011; Story et al., 2003; Willows et al., 2007). Prevalence of obesity among American Indian preschoolers (31.2%) was found to be significantly higher when compared to other racial/ethnic groups, especially non-Hispanic White or Asian children (12.8%) (Anderson and Whitaker, 2009). Of the 252 3-year-old American Indian children examined in Wisconsin 22.2% were classified as obese and 19% as overweight (Adams et al., 2005). Forty-nine percent of American Indian children between 3 and 5 years of age living on reserves in South Dakota were reported to be overweight, and 21.3% obese (Hearst et al., 2011). In the Sandy Lake Oji-Cree Native Canadian community, the percent of pre-school children with a BMI ≥ 85th percentile was 34.6% in boys (n = 78) and 45.2% in girls (n = 62), significantly higher in comparison to the corresponding age and sex category of National Health and Nutrition Examination Study III (NHANES III) population (Hanley et al., 2000). Additionally, very early rapid weight gain may be an early signal of developing obesity. A longitudinal study of Pima preschoolers showed that the most marked weight gain in comparison to US reference values occurred in the first 6 months of life and then between 2 and 11 years there was a steady increase in excessive weight gain (Lindsay et al., 2002). Thus, when compared to other children in the US, some American Indian children gain weight at a higher rate before 2 years of age (Lindsay et al., 2002; Salbe et al., 2002b).
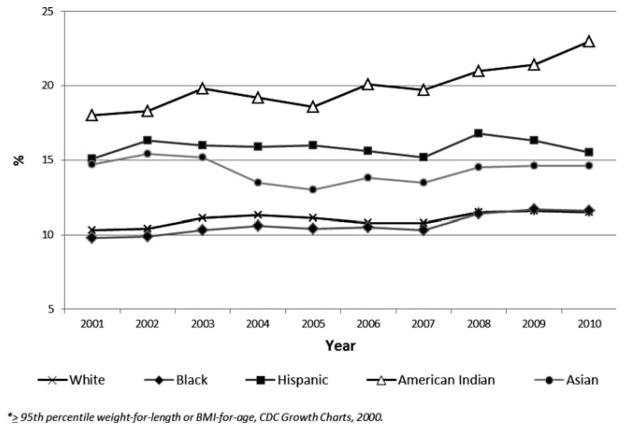
Figure 2 indicates that preschoolers measured earlier had lower frequencies of overweight and obesity than those measured more recently. The trend over the last 20 years does not portend an end to the epidemic among American Indians. Whereas obesity rates of 2- to 5-year-old preschool children have remained relatively stable since the early 2000s among all other racial and ethnic groups, Native Americans have experienced a 30% increase in the prevalence of obesity between 2001 and 2011 (Fig. 2) (Polhamus et al., 2009).
Fig. 2.
Prevalence of obesity trends among 2- to 5-year olds, by race/ethnicity.
Conclusions from many studies conducted in the last 20 years indicate that overweight and obesity begins at the youngest ages among American Indian children. Health care providers should begin obesity prevention at the earliest age possible, and should examine the economic, social, and cultural context of overweight and obesity within the Native American populations (Flegal, 1999; Young, 1996).
SCHOOL-AGED CHILDREN
A review of research on growth and development of North American Native Americans covering the 20th century concluded that Native American school-aged children and youth are in general stockier than their non-Native age and sex peers, as judged by their weights and heights relative to US population reference values (Schell et al., 2006). Furthermore, relying more on studies conducted in the mid-20th century before the epidemic of overweight gained momentum, certain regularities were apparent. Papago children and youth were among the stockiest of all North American Indians. Among males, groups living in the northern areas (the Nootka, Chilcotin, Mohawk, and Alaskan Athabascans) were next, followed by Plains area peoples (the Sioux, Gros Ventres, and Assiniboine). Lighter weights were found among the southwestern groups (excepting the Papago and Pima), the Navajo and the Apache who displayed the lowest weights-for-height of all. The same ordering existed among females (Schell et al., 2006).
Since the mid-20th century, rates of overweight and obesity among school-aged Native American children have risen dramatically, raising the question whether the regional differences in size seen earlier have lessened as the obesity epidemic has spread. Findings from studies conducted in the 21st century show an even greater excess of overweight and obesity among Native American youth relative to the general US population (Hearst et al., 2011; Jollie-Trottier et al., 2009; Khalil et al., 2010; MacMillan et al., 2010; Madsen et al., 2010; Shields, 2005; Zephier et al., 2006). Several large surveys in the 1980s and 1990s reported the high prevalence of overweight and obesity among Native American school children (Broussard et al., 1991, 1995; Jackson, 1993; Story et al., 1999; Zephier et al., 1999), summarizing the higher relative fatness than their non-Native peers. The first large survey (n = 9,000) seeking to characterize all Native American youth between the ages of 5 and 18 years was conducted in 1990, and reported that Native American youth had significantly higher BMIs, for every age and sex, when compared to NHANES II data and Hispanic Health and Nutrition Examination Survey-ME (HHANES-Mexican American subsample of) data (39.3 and 28.6%, respectively) (Jackson, 1993). A compilation of results from studies reporting the frequency of BMI in the overweight and obese ranges (Table 2) shows how common these two conditions are among Native American children and youth. Further, the rates appear to have increased noticeably over the past 20 years although differences in age ranges, origin of the sample, and reporting technique hinder comparison.
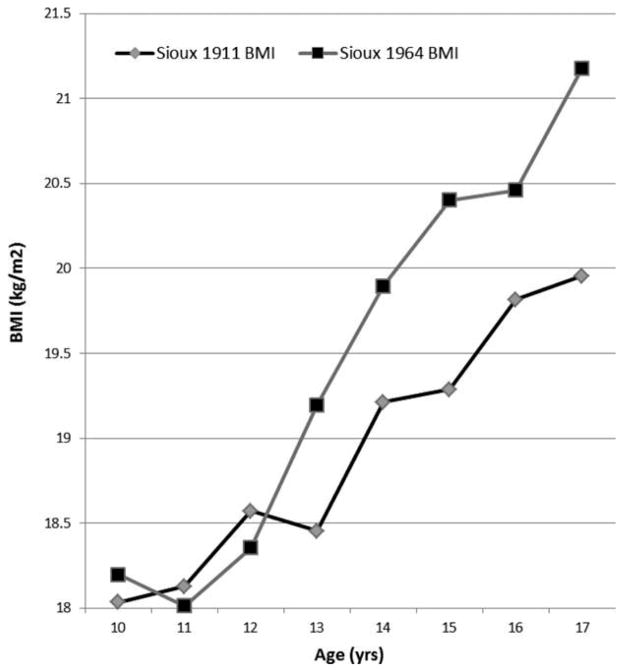
AMERICAN PLAINS
American Indians of the Plains states are among the most storied and studied groups. One of the earliest investigations to measure weight was of the Sioux in 1911 (Wissler, 1911) (Children of known European/Indian parentage were reported separately). These weight data may be compared to Sioux children measured by Ship (1964). Over this 50+ year period heights increased only 3.5 cm on average while weights increased by 3.54 kg on average. BMI increased accordingly. There was little change in the pre-adolescent period but a substantial increase in adolescence (Fig. 3).
Fig. 3.
Changes in BMI among US Sioux from 1911 to 1964.
Recent, well-designed studies show a continuation of this trend of increasing weight. A large study, conducted in 1995–1996, measured over 12,000 Aberdeen area children 5 to 17 years of age from 16 different tribes (includes tribes in North Dakota, South Dakota, Nebraska, and Iowa) reported that the prevalence for overweight was 2.5 times higher relative to gender and age specific national data from NHANES II (Zephier et al., 1999). Obesity prevalence in this cohort was nearly three times that of the reference population among females, and approximately five times the expected prevalence among males at 16 and 17 years of age. Additionally, a subsequent project followed children from the same Aberdeen area (n = 12,000) in 2002–2003 was conducted to evaluate any changes in the prevalence of overweight and obesity among school-aged children. By the age of 5 years 24% of the children were obese, and 44% overweight, exceeding at nearly every age the prevalence among US children of the same age and sex (Zephier et al., 2006). The prevalence of overweight and obesity was increased by 4.5 and 4.3% in the 7 years between studies.
A study of over 4,000 American Indian children attending school on a South Dakota reservation reported that nearly 46% of all children 3- to 19-year old were overweight, and over 24% obese, with the highest prevalence for overweight and obesity between the ages of 12–14 years (48.4 and 28.9%, respectively) (Hearst et al., 2011). These extensive surveys indicate clearly a marked increase in the prevalence of overweight and obesity over a fairly short period.
Anthropometric measurements and rates of obesity were examined among a sample of Cherokee youth (13–16 years) in the early 1980s (Story et al., 1986). The prevalence of obesity was based on triceps skinfold thicknesses. According to the criterion set forth by Seltzer and Mayer, obesity among the Cherokee youth was high: overall, 38% of the Cherokee youth were obese (51% boys; 25% girls) (Story et al., 1986).
Thirty-three percent of Northern Plains children (8–12 years) were found to be obese and 20% overweight (Jollie-Trottier et al., 2009). A retrospective study conducted within a small group (n = 100) of urban Oklahoma City American Indian children (2–12 years) concluded that by the age of 12 years, 60% of the children were overweight or obese, and males demonstrated an earlier onset of excess weight compared to females (Stern et al., 2007). Wind River Indian Reservation children in 3rd to 8th grade were measured in order to examine changes in measurements of BMI during school vacation time. The reported findings established that the combined rates of overweight and obesity (62% for boys, and nearly 60% for girls) substantially exceeded national estimates (Smith et al., 2009).
Urbanization is another factor that may influence weight-for-height among Great Plains American Indian youth. Self-identified Ojibway adolescents from an urban/metropolitan area of Minnesota were measured as part of Project EAT, and measurements were compared to those of the Caucasian children in the study. Significantly higher rates of overweight and obesity were found among the American Indian teenagers: 43% of the boys were overweight and 23% obese and the prevalence for overweight and obesity among the girls was 39 and 21%, respectively (DeLong et al., 2008). Among urban Anishinaabe children (Minneapolis, MN) between the ages of 5–18 years, 63% were either overweight or obese using BMI cutoffs set forth by the CDC (Gray and Smith, 2003).
Whether residing in an urban or rural environment, these studies indicate that a higher percentage of American Indian children from the Great Plains area of the US are overweight or obese when compared to non-Native children. In fact, these prevalence rates are continuing to increase as demonstrated by the larger surveys.
CANADIAN PLAINS AND WOODLANDS
Several studies in the past 10 years have indicated increasing temporal trends in obesity and overweight among First Nation and Aboriginal children and youth of Canada (Hanley et al., 2000; Katzmarzyk, 2002, 2007; Khalil et al., 2010; Tremblay et al., 2002; Young, 2007; Young et al., 2000). In a sample of over nearly 1,800 children (1st Nation, Metis, Inuit, and non-Aboriginals) between the ages of 2 and 17 years, the prevalence of obesity was substantially higher among Aboriginal children (15.8%) than non-Aboriginals (8%) (Katzmarzyk, 2007). A project assessing the physical and emotional well-being of on-reserve Aboriginal youth, combined data from nine surveys conducted in 1996–1997, and reported that over 6% of children aged 6–11 years and 10% of those 12 years and up were overweight (MacMillan et al., 2010). Among 6- to 9-year-old Sandy Lake Oji-Cree children of central Canada, prevalence of overweight was generally similar between boys and girls (30%), yet significantly higher when compared to the NHANES III reference population (Hanley et al., 2000). The prevalence of overweight remains consistently higher among Oji-Cree girls in comparison to their male peers between the ages of 10–14 (32 vs. 24%) and 15–19 years (27 vs. 19%) (Hanley et al., 2000). Further north in Manitoba, nearly two-thirds of Ojibwa-Cree school children (4–19 years) of the St. Theresa Point First Nation measured between 1996 and 1998 were found to have BMIs exceeding the 85th percentile; of those exceeding the 85th percentile 64% of females and 60% of males were obese (Young et al., 2000).
A smaller study (n = 416) assessing measures of overall body fatness in 8- to 17-year old Aboriginal youth found that Aboriginal girls and boys had more total body fat (5.4 and 7.6%, respectively), and higher trunk fatness (6 and 8.3%, respectively) than non-Aboriginal youth of the same age (Anderson et al., 2010). On average, Aboriginal girls had a greater prevalence of overweight/obesity pre-, during, and post-peak height velocity than their non-Aboriginal peers (47.4 vs. 20.8%; 25.6 vs. 19.5%; and 50 vs. 26.2%, respectively).
In the 1990s, a study of Cree school children (4th to 9th grade) in the Sandy Lake Oji-Cree community defined overweight as a BMI ≥ 90th percentile of an undefined reference population, and found that 38% of the participants were considered overweight (Bernard et al., 1995). Thirty-five percent of Cree children of Northern Quebec were reported obese by the Cree Board of Health and Social Services (Ngnie Teta, 2002). More recently, a study of James Bay Cree school-aged children reported that 54% of 9- to 13-year olds were obese, and the obesity prevalence reached nearly 39% of 14- to 18-year olds (Khalil et al., 2010).
Living in a more urban environment does not appear to alter these high rates of overweight and obesity. Among urban Mohawk children of Kahnawake near Montreal, the prevalence of overweight of school-aged youth reached 29.5% in boys, and 32.8% in girls (Willows, 2005).
Clearly, Canadian American Indian children are experiencing the alarming rise in overweight and obesity similar to that among other Native Americans and North Americans generally. Young Aboriginals are experiencing an obesity rate over twice that of the Canadian national average (Shields, 2005).
SOUTHWEST
Of all American Indian groups, those in the southwest have been studied most often allowing comparison over time of the rates of overweight and obesity (Table 2). Evidence for a high prevalence of overweight and obesity among many American Indian groups in this region is substantial. Further, there is substantial evidence that this is a long developing phenomenon. In one of the best controlled studies of secular trend, Miller measured young Apache men in 1967 whose fathers had been measured in 1940 (Miller, 1970). The sons averaged 5.9 kg more than their fathers though the sons were only 1.3 cm taller. Since the 1960s, there have been further substantial increases in the weights of youth from the US southwest.
Findings from studies in the 1980s among older Navajo adolescents (14 to 18 years of age), demonstrated that 33% of the girls and 25% of the boys were found to be overweight using NHANES II reference values (Gilbert et al., 1992). Consistent with other earlier reports of Navajo growth status (Gilbert et al., 1992; Sugarman et al., 1990), results of the Navajo Health and Nutrition Survey found that the prevalence of overweight (at or above the 85th percentile of NHANES II reference population) among 12-to 19-year-old Navajo adolescents was 35% in boys and 40% in girls (Freedman et al., 1997). Results from this study show a median BMI that is ~2 kg/m2 higher when compared to the US reference population of the same age and sex.
In a study from 1997–2000, of over 1,700 7- and 8-year olds from two Apache and Lakota communities, a Navajo, a Tohono O’odham and a Gila River (Pima-Maricopa) community, nearly 50% of the children were above the 85th percentile for BMI-for-age (based on NHANES II), and ~29% were above the 95th percentile; the percentage of children with a BMI above the 95th percentile fluctuated between 23% (Navajo) to 54% (Pima-Maricopa) in girls and 21% (Navajo) to 49% (Tohono O’odham) in boys (Caballero et al., 2003).
Among Navajo children, 5–17 years of age, BMIs have increased substantially between 1955 and 1989. Mean heights among Navajo children increased 6.1% in boys and 4.4% in girls whereas weights increased 28.8% among boys and 18.7% among girls across all age groups (Sugarman et al., 1990). By 1989, BMIs of Navajo boys exceeded those of the general US population (using reference values from NHANES I) at all ages by ~1 unit, and girls’ BMIs exceeded the NHANES I values increasingly from 1 unit at age 8 to nearly 4 at age 17 years (Sugarman et al., 1990). A more recent study reported that Navajo youth under 20 years of age with Type II diabetes had a higher prevalence of obesity (67.7 vs. 12.5%) than those with Type I diabetes (Dabelea et al., 2009).
These results were consistent with recent findings of the Navajo Health and Nutrition Survey (Eisenmann et al., 2000) that examined children between the ages of 6 and 12 years over a similar period (1955–1997). Approximately 41% of the Navajo youth had a BMI ≥85th percentile of the NHANES I reference population. While there was only a small difference in the prevalence of overweight and obesity among Navajo boys, the younger girls (between 6 and 9 years) had a higher prevalence of overweight and obesity than the older girls (44 vs. 37%) (Eisenmann et al., 2000). Furthermore, the authors note a secular increase in BMI between the years 1989 and 1997 that was equal or greater than the increase between 1955 and 1989. Between 1955 and 1997, BMI had increased ~0.5 units per decade in younger children and 1.0 unit per decade in older children (Eisenmann et al., 2000).
Using the more recently developed international reference to classify overweight and obesity standards proposed by the IOTF (International Obesity Task Force) (Cole et al., 2000), ~24% of Hopi children measured in 1996 and 1997, 6–12 years of age, are overweight and an additional 24% are obese with age-specific mean BMIs tracking the 85th percentile (Eisenmann et al., 2003). Comparisons of data on Pima children from the turn of the century to a recent cohort indicate that Pima children at 5 and 10 years of age are now 6 kg heavier at comparable heights (Salbe et al., 2002a,b).
NORTHEAST: THE MOHAWK
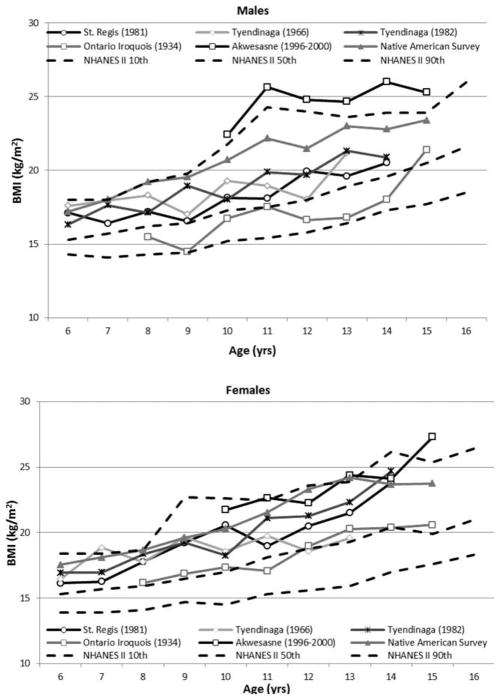
One of the most studied American Indian groups is the Mohawk. They are one of the nations of the Haudenosaunee Confederacy (sometimes referred to as the Iroquois League of Nations). There are several Mohawk or Kahniakenhaka communities: Kahnawá:ke, Kanehsatake, Ohsweken, Tyendinaga, Wahta, Kana’tsiohare:ke, Ganienkeh, and Akwesasne. Population size estimates of each community vary. Mohawk children have been studied several times over a period dating back to 1934 (Helmuth, 1983b) and these studies provide an opportunity to examine within a single population the changes in size and obesity during the period when the obesity epidemic developed.
The most recent information comes from a study of Akwesasne Mohawk youth (10–16 years of age) measured between 1996 and 2000 (Gallo et al., 2005). Mean heights closely approximate the 50th percentile of NCHS reference values at each age. However, mean weights of boys and girls at every age are significantly greater than the NCHS 50th percentile (Fig. 4a, b). Age specific BMI means of boys and girls exceed the 50th percentile of the CDC reference population consistently. Nearly 60% of the youth met or exceed the 85th percentile; the frequency of overweight is 26%: the frequency of obesity is 33% (Gallo et al., 2005).
Fig. 4.
(a, b) BMI of Haudenosaunee males measured between 1934 and 2000 with NHANES II 10th, 50th, and 90th percentiles. Citations are found in the text.
Over the 65-year period covered by the studies, the change in weights among males is extraordinary (Fig. 4a). The earliest study (n = 49) included Mohawk youth, as well some youth from other Haudenosaunee groups, the Seneca and Cayuga (Helmuth, 1983a). Ten-year old Haudenosaunee boys measured in 1934 weighed 28.5 kg while same-aged Akwesasne boys measured between 1996 and 2000 weighed 45.5 kg. The 17 kg difference is similar across the entire 10–16 age range. Heights increased also though not to the same degree.
As the sample measured in 1934 includes some non-Mohawk youth, a comparison of the two Akwesasne Mohawk samples may be more exact and informative. Eight- to fourteen-year old boys measured between 1996 and 2000 are from 11 to 19 kg heavier than their Mohawk age-peers measured in 1981 (Helmuth, 1983a). The average difference across the age range is 15.4 kg. In contrast, there was virtually no change in heights over those same 14 years. BMIs increased by 5.5 units on average. Although the studies were performed by different investigators and one could question the role of differences in measurement methods between studies, the measurement of weight is subject to very little inter-observer error. Also, clothing weight is not an issue as the most recent study measured youth in standard, lightweight clothes.
DISCUSSION
The extremely high prevalence of overweight and obesity among the Mohawk and nearly every other American Indian group studied recently and described here is hardly the result of changes in measurement methods, or definitions of overweight or obesity. It is powerfully real and affects the lives of all American Indians either directly or through friends and family. The very high rates of disability, productivity losses, and premature death that seem terribly characteristic of American Indian communities can be traced to this epidemic.
Our conclusions regarding overweight and obesity are based on reports of BMI among many American Indian groups over time and space. Problems associated with BMI as an indicator of adiposity have been described and its limitations must be acknowledged (Wells, 2010). Furthermore, as BMI is a function of weight and height, changes in heights may be influential in creating patterns of BMI. Evidence is lacking for positive or negative changes in heights during the rise of the obesity epidemic over the last 2 decades among American Indians suggesting that changes in BMI are largely due to changes in weight.
There are several explanations for the high frequencies of overweight and obesity among American Indians in the past and their increasing prevalence. The most common explanation is the nutrition transition. While the nutrition transition concept is more commonly applied to dietary transitions in less economically developed countries, there is a clear parallel with many American Indian communities where poverty, unemployment, and psychosocial stress are too common. Historical and present-day prejudice, exploitation, and attacks on sovereignty and identity play large roles in the daily lives of tribal members (Cook, 2011).
Many American Indian communities are changing from consumption of traditional, locally grown or caught foods to commodities (Compher, 2006; Kuhnlein et al., 2004; Sharma et al., 2009). Store bought foods are characteristically energy dense but nutritionally weak; fresh fruits and vegetables are rare in local stores mirroring the food deserts of poor urban neighborhoods. Studies of urban American Indians conducted 2–4 decades ago reported higher weight for heights in conjunction with more urban or acculturated diets (Johnston et al., 1978). Similarly, in a study conducted sometime before 1986 (date of data collection not reported), North Carolina Cherokee teenagers, who may have been similar to the urban samples in terms of dietary acculturation, also display far greater weight for height in comparison to NCHS reference values (Story et al., 1986). These earlier studies of more acculturated American Indian groups foreshadowed a trend current in American Indian communities generally as diets high in fat and energy have become common in most American Indian communities (Downs et al., 2009; Ho et al., 2008; Khalil et al., 2010; Lytle et al., 2002; Stroehla et al., 2005).
Obesity and overweight among American Indian children and youth may result from the multigenerational transmission of overweight and obesity. This review found that many studies report higher weights at birth as well as associations between larger maternal weights, larger birth weights, and diabetes risk among offspring (Alexander et al., 2008; Baldwin et al., 2009; Caulfield et al., 1998; Luo et al., 2004; Wenman et al., 2004). Together these findings suggest multigenerational continuity of risk. A review of the physical growth and development of American Indian children and youth concluded that among those measured 25–50 years ago, they were characteristically stocky (Schell et al., 2005). The children measured then have become the parents of the children described in studies of the last decade. Mechanisms for the transmission of overweight and obesity include social inheritance (familial dietary and activity habits) and epigenetic mechanisms.
Finally, there is now considerable evidence that some chemical exposures are associated with overweight and obesity (Elobeid and Allison, 2008; Elobeid et al., 2010; Karmaus et al., 2009; Mendez et al., 2011). Although these studies provide correlative evidence, controlled laboratory experiments prove the concept of causal relationships (Grun and Blumberg, 2009; Grun et al., 2006; Newbold et al., 2007a, b). The mechanism of action may involve alteration of thyroid economy as lower thyroid activity is one cause of positive energy balance that contributes to overweight and obesity. Lower thyroid activity has been found in connection with toxicant exposures, particularly some persistent organic pollutants (Boas et al., 2009; Crofton, 2008; Jugan et al., 2010; Miller et al., 2009; Pearce and Braverman, 2009; Schell et al., 2008, 2009).
More often studied in this regard is the connection between certain toxicant exposures and diabetes, a frequent consequence of overweight and obesity. Studies of human populations have shown clear associations between measures of exposure to specific persistent organic pollutants and diabetes, usually Type II (Lee et al., 2006; Park et al., 2009; Uemura et al., 2009).
Toxicant exposures are too common among Native American groups (Donaldson et al., 2010; Garza, 2001; Harada et al., 2005; Zaferatos, 2006). The “ecological footprint” (Rees, 1992) of industrialized areas includes the distribution of many kinds of wastes to rural areas including the sites of some Native American communities and of minority communities generally. Further, many remote areas have become industrialized. A prime example is the Akwesasne (St. Regis) Mohawk Nation, a community located on the St. Lawrence River and downstream from industries that developed when the St. Lawrence River itself was developed in the 1950s. Some of these industries have contaminated local waterways and the local ecology. The Nation is now downriver from a federal superfund site and two New York State Superfund sites, designations that testify to the contamination of the local waterways.
Like many Native American communities, the Akwesasne Mohawk have depended on local plants and animals for their traditional diet. The consumption of local foods to supply traditional diets can be a healthier approach to food acquisition than use of prepared foods from markets, but the contamination of the community’s local environment has led to contamination of the local food supply, particularly local fish (Fitzgerald et al., 1995, 1998, 2004; Lacetti, 1993; Sloan and Jock, 1990). In fact, consumption of local wildlife is associated with higher levels of persistent polychlorinated biphenyls in young adults (Schell et al., in press). The community finds itself between two negative, obesogenic forces: consumption of local foods containing certain toxicants can lead to overweight and obesity as recent research suggests, yet avoiding such foods and consuming energy dense prepared foods also elevates risk of overweight and obesity. This is the dietary dilemma (Halpern, 2007; Haman et al., 2010) of what is a safe food in the modern world that many Native American groups have faced (Dewailly et al., 1993, 1996; Girard et al., 1996; Harris and Harper, 1997). Now we all do.
CONCLUSION
This review clearly suggests that American Indian youth are affected disproportionately when compared to other US ethnic/racial groups. The high prevalence of overweight and obesity contribute to the poor health of many American Indian groups. To remedy this problem, long-term interventions are necessary. These should be consonant with cultural values, accepted by tribal leaders and supported by community health care providers. New interventions are sorely needed as ones in place have not stemmed the rise in overweight and obesity. Continuing efforts between American Indian health care providers, medical centers, and universities on a long-term basis can make a lasting difference to this epidemic. Interventions at many points in the lifecycle may be helpful as overweight and obesity are multigenerational problems. Thus, interventions among children and youth may promote health in one generation and additionally contribute to the health of the next and future generations. In many American Indian communities, goals and actions are evaluated in terms of their benefits for seven generations in the future. Solving the epidemic of overweight and obesity is essential to safeguard the future of Native Americans, seven generations on and further.
Acknowledgments
Contract grant sponsor: National Institute of Environmental Health Sciences; Contract grant numbers: NIEHS-ESO4913, ES10904; Contract grant sponsor: National Institutes of Health; Contract grant number: 1P20 MD003373; Contract grant sponsor: National Institute on Minority Health and Health Disparities.
We would like to acknowledge and thank the many Native American communities who cooperated with researchers over many decades to describe and understand child growth, its causes and consequences among Native Americans. In particular, we thank Maxine Cole, Alice Tarbell, Agnes Jacobs, Ken Jock, Craig Arquette, and the Akwesasne Mohawk community for their contributions, cooperation, and participation in the research we have done together on this topic. The content is solely the responsibility of the authors and does not represent the official views of the National Institute on Minority Health and Health Disparities or the National Institutes of Health.
LITERATURE CITED
- Adams AK, Harvey HE, Prince RJ. Association of maternal smoking with overweight at age 3 y in American Indian children. Am J Clin Nutr. 2005;82:393–398. doi: 10.1093/ajcn.82.2.393. [DOI] [PubMed] [Google Scholar]
- Adams MS, Brown KS, Iba BY, Niswander JD. Health of Papago Indian children. Public Health Rep. 1970;85:1047–1061. [PMC free article] [PubMed] [Google Scholar]
- Adams MS, Niswander JD. Developemental “noise” and a congenital malformation. Genet Res. 1967;10:313–317. doi: 10.1017/s0016672300011071. [DOI] [PubMed] [Google Scholar]
- Adams MS, Niswander JD. Birth weight of North American Indians. Am J Human Biol. 1968;40:226–234. [PubMed] [Google Scholar]
- Adams MS, Niswander JD. Birth weight of North American Indians: a correction and amplification. Hum Biol. 1973;45:351–357. [PubMed] [Google Scholar]
- Alexander GR, Wingate MS, Boulet S. Pregnancy outcomes of American Indians: contrasts among regions and with other ethnic groups. Matern Child Health J. 2008;12 (Suppl 1):5–11. doi: 10.1007/s10995-007-0295-z. [DOI] [PubMed] [Google Scholar]
- Anderson KD, Baxter-Jones AD, Faulkner RA, Muhajarine N, Henry CJ, Chad KE. Assessment of total and central adiposity in Canadian Aboriginal children and their Caucasian peers. Int J Pediatr Obes. 2010;5:342–350. doi: 10.3109/17477160903473721. [DOI] [PubMed] [Google Scholar]
- Anderson SE, Whitaker RC. Prevalence of obesity among US preschool children in different racial and ethnic groups. Arch Pediatr Adolesc Med. 2009;163:344–348. doi: 10.1001/archpediatrics.2009.18. [DOI] [PubMed] [Google Scholar]
- Armstrong IE, Robinson EJ, Gray-Donald K. Prevalence of low and high birthweight among the James Bay Cree of Northern Quebec. Can J Public Health. 1998;89:419–420. doi: 10.1007/BF03404087. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Baldwin LM, Grossman DC, Murowchick E, Larson EH, Hollow WB, Sugarman JR, Freeman WL, Hart LG. Trends in perinatal and infant health disparities between rural American Indians and Alaska natives and rural Whites. Am J Public Health. 2009;99:638–646. doi: 10.2105/AJPH.2007.119735. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bernard L, Lavallee C, Gray-Donald K, Delisle H. Overweight in Cree schoolchildren and adolescents associated with diet, low physical activity, and high television viewing. J Am Diet Assoc. 1995;95:800–802. doi: 10.1016/S0002-8223(95)00221-9. [DOI] [PubMed] [Google Scholar]
- Boas M, Main KM, Feldt-Rasmussen U. Environmental chemicals and thyroid function: an update. Curr Opin Endocrinol Diabetes Obes. 2009;16:385–391. doi: 10.1097/MED.0b013e3283305af7. [DOI] [PubMed] [Google Scholar]
- Broussard BA, Johnson A, Himes JH, Story M, Fichtner R, Hauck F, Bachman-Carter K, Hayes J, Frohlich K, Gray N, et al. Prevalence of obesity in American Indians and Alaska Natives. Am J Clin Nutr. 1991;53:1535S–1542S. doi: 10.1093/ajcn/53.6.1535S. [DOI] [PubMed] [Google Scholar]
- Broussard BA, Sugarman JR, Bachman-Carter K, Booth K, Stephenson L, Strauss K, Gohdes D. Toward comprehensive obesity prevention programs in Native American communities. Obes Res. 1995;3 (Suppl 2):289s–297s. doi: 10.1002/j.1550-8528.1995.tb00476.x. [DOI] [PubMed] [Google Scholar]
- Buck GM, Mahoney MC, Michalek AM, Powell EJ, Shelton JA. Comparison of Native American births in upstate New York with other race births, 1980–1986. Public Health Rep. 1992;107:569–575. [PMC free article] [PubMed] [Google Scholar]
- Caballero B, Himes JH, Lohman T, Davis SM, Stevens J, Evans M, Going S, Pablo J. Body composition and overweight prevalence in 1704 schoolchildren from 7 American Indian communities. Am J Clin Nutr. 2003;78:308–312. doi: 10.1093/ajcn/78.2.308. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Caulfield LE, Harris SB, Whalen EA, Sugamori ME. Maternal nutritional status, diabetes and risk of macrosomia among Native Canadian women. Early Hum Dev. 1998;50:293–303. doi: 10.1016/s0378-3782(97)00074-1. [DOI] [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention. Prevalence of overweight among children and adolescents: United States, 1999. 2001. [Google Scholar]
- Centers for Disease Control and Prevention. REACH 2010 Surveillance for Health Status in Minority Communities–United States, 2001–2002. Morbidity Mortality Wkly Rep. 2004;53:1–36. [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention. Obesity trends among U.S. adults between 1985 and 2010. Atlanta, GA: Centers for Disease Control and Prevention; 2011. [Google Scholar]
- Centers for Disease Control and Prevention. Pediatric Data Tables. CDC; 2011. www.cdc.gov/pednss/pednss_tables/html/pednss_national_table18.htm. [Google Scholar]
- Cole TJ, Bellizzi MC, Flegal KM, Dietz WH. Establishing a standard definition for child overweight and obesity worldwide: international survey. Br Med J. 2000;320:1240–1243. doi: 10.1136/bmj.320.7244.1240. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Compher C. The nutrition transition in American Indians. J Transcult Nurs. 2006;17:217–223. doi: 10.1177/1043659606288376. [DOI] [PubMed] [Google Scholar]
- Cook B. The Toxic Effects of Stress on American Indians. Indian Country Today Media Network; 2011. http://indiancountrytodaymedianetwork.com/ict_sbc/the-toxic-effects-of-stress-on-american-indians. [Google Scholar]
- Crofton KM. Thyroid disrupting chemicals: mechanisms and mixtures. Int J Androl. 2008;31:209–223. doi: 10.1111/j.1365-2605.2007.00857.x. [DOI] [PubMed] [Google Scholar]
- Dabelea D, DeGroat J, Sorrelman C, Glass M, Percy CA, Avery C, Hu D, D’Agostino RB, Jr, Beyer J, Imperatore G, et al. Diabetes in Navajo youth: prevalence, incidence, and clinical characteristics: the search for diabetes in youth study. Diabetes Care. 2009;32 (Suppl 2):S141–S147. doi: 10.2337/dc09-S206. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Davis S, Gomez Y, Lambert L, Skipper B. Primary prevention of obesity in American Indian children. Ann N Y Acad Sci. 1993;699:167–180. doi: 10.1111/j.1749-6632.1993.tb18848.x. [DOI] [PubMed] [Google Scholar]
- DeLong AJ, Larson NI, Story M, Neumark-Sztainer D, Weber-Main AM, Ireland M. Factors associated with overweight among urban American Indian adolescents: findings from project EAT. Ethn Dis. 2008;18:317–323. [PubMed] [Google Scholar]
- Dewailly E, Ayotte P, Bruneau S, Laliberte C, Muir DC, Norstrom RJ. Inuit exposure to organochlorines through the aquatic food chain in arctic quebec. Environ Health Perspect. 1993;101:618–620. doi: 10.1289/ehp.93101618. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dewailly E, Ayotte P, Laliberte C, Weber J-P, Gingras S, Nantel AJ. Polychlorinated biphenyl (PCB) and dichlorodiphenyl dichloroethylene (DDE) concentrations in the breast milk of women in Quebec. Am J Public Health. 1996;86:1241–1246. doi: 10.2105/ajph.86.9.1241. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Donaldson SG, Van OJ, Tikhonov C, Feeley M, Armstrong B, Ayotte P, Boucher O, Bowers W, Chan L, Dallaire F, et al. Environmental contaminants and human health in the Canadian Arctic. Sci Total Environ. 2010;408:5165–5234. doi: 10.1016/j.scitotenv.2010.04.059. [DOI] [PubMed] [Google Scholar]
- Downs SM, Arnold A, Marshall D, McCargar LJ, Raine KD, Willows ND. Associations among the food environment, diet quality and weight status in Cree children in Quebec. Public Health Nutr. 2009;12:1504–1511. doi: 10.1017/S1368980008004515. [DOI] [PubMed] [Google Scholar]
- Dyck RF, Tan L. Differences in high birthweight rates between Northern and Southern Saskatchewan: implications for Aboriginal peoples. Chron Dis Can. 1995;16:7. [Google Scholar]
- Edouard L, Gillis D, Habbick B. Pregnancy outcome among native Indians in Saskatchewan. Can Med Assoc J. 1991;144:1623–1625. [PMC free article] [PubMed] [Google Scholar]
- Eisenmann JC, Arnall DA, Kanuho V, McArel H. Growth status and obesity of Hopi children. Am J Human Biol. 2003;15:741–745. doi: 10.1002/ajhb.10211. [DOI] [PubMed] [Google Scholar]
- Eisenmann JC, Katzmarzyk PT, Arnall DA, Kanuho V, Interpreter C, Malina RM. Growth and overweight of Navajo youth: secular changes from 1955 to 1997. Int J Obes Relat Metab Disord. 2000;24:211–218. doi: 10.1038/sj.ijo.0801116. [DOI] [PubMed] [Google Scholar]
- Elobeid MA, Allison DB. Putative environmental-endocrine disruptors and obesity: a review. Curr Opin Endocrinol Diabetes Obes. 2008;15:403–408. doi: 10.1097/MED.0b013e32830ce95c. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Elobeid MA, Padilla MA, Brock DW, Ruden DM, Allison DB. Endocrine disruptors and obesity: an examination of selected persistent organic pollutants in the NHANES 1999–2002 data. Int J Environ Res Public Health. 2010;7:2988–3005. doi: 10.3390/ijerph7072988. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fitzgerald EF, Hwang S-A, Brix KA, Bush B, Cook K, Worswick P. Fish PCB concentrations and consumption patterns among Mohawk women at Akwesasne. J Expo Anal Environ Epidemiol. 1995;5:1–19. [PubMed] [Google Scholar]
- Fitzgerald EF, Hwang S-A, Bush B, Cook K, Worswick P. Fish consumption and breast milk PCB concentrations among Mohawk women at Akwesasne. Am J Epidemiol. 1998;148:164–172. doi: 10.1093/oxfordjournals.aje.a009620. [DOI] [PubMed] [Google Scholar]
- Fitzgerald EF, Hwang S-A, Langguth K, Cayo MR, Yang B-Z, Bush B, Worswick P, Lauzon T. Fish consumption and other environmental exposures and their associations with serum PCB concentrations among Mohawk women at Akwesasne. Environ Res. 2004;94:160–170. doi: 10.1016/s0013-9351(03)00133-6. [DOI] [PubMed] [Google Scholar]
- Flegal KM. The obesity epidemic in children and adults: current evidence and research issues. Med Sci Sports Exerc. 1999;31:S509–S514. doi: 10.1097/00005768-199911001-00004. [DOI] [PubMed] [Google Scholar]
- Flegal KM, Ogden CL, Carroll MD. Prevalence and trends in overweight in Mexican-American adults and children. Nutr Rev. 2004;62:S144–S148. doi: 10.1111/j.1753-4887.2004.tb00085.x. [DOI] [PubMed] [Google Scholar]
- Franks PW, Hanson RL, Knowler WC, Moffett C, Enos G, Infante AM, Krakoff J, Looker HC. Childhood predictors of young-onset type 2 diabetes. Diabetes. 2007;56:2964–2972. doi: 10.2337/db06-1639. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Freedman DS, Byers T, Sell K, Kuester S, Newell E, Lee S. Tracking of serum cholesterol levels in a multiracial sample of preschool children. Pediatrics. 1992;90:80–86. [PubMed] [Google Scholar]
- Freedman DS, Serdula MK, Percy CA, Ballew C, White LL. Obesity, levels of lipids and glucose, and smoking among Navajo adolescents. J Nutr. 1997;127:2120S–2127S. doi: 10.1093/jn/127.10.2120S. [DOI] [PubMed] [Google Scholar]
- Gallaher MM, Hauck FR, Yang-Oshida M, Serdula MK. Obesity among Mescalero preschool children. Association with maternal obesity and birth weight. Am J Dis Child. 1991;145:1262–1265. doi: 10.1001/archpedi.1991.02160110054019. [DOI] [PubMed] [Google Scholar]
- Gallo MV, Schell LM Akwesasne Task Force on the Environment. Height, weight and body mass index among Akwesasne Mohawk youth. Am J Human Biol. 2005;17:269–279. doi: 10.1002/ajhb.20316. [DOI] [PubMed] [Google Scholar]
- Garza D. Alaska Natives assessing the health of their environment. Int J Circumpolar Health. 2001;60:479–486. [PubMed] [Google Scholar]
- Gilbert TJ, Percy CA, Sugarman JR, Benson L, Percy C. Obesity among Navajo adolescents. Relationship to dietary intake and blood pressure. Am J Dis Child. 1992;146:289–295. doi: 10.1001/archpedi.1992.02160150029015. [DOI] [PubMed] [Google Scholar]
- Girard M, Noel F, Dumont C. Varying mercury exposure with varying food source in a James Bay Cree community. Arctic Med Res. 1996;55:69–74. [PubMed] [Google Scholar]
- Gray A, Smith C. Fitness, dietary intake, and body mass index in urban Native American youth. J Am Diet Assoc. 2003;103:1187–1191. doi: 10.1016/s0002-8223(03)00979-9. [DOI] [PubMed] [Google Scholar]
- Gruber E, Anderson MM, Ponton L, DiClemente R. Overweight and obesity in Native-American adolescents: Comparing nonreservation youths with African-American and Caucasian peers. Am J Prev Med. 1995;11:306–310. [PubMed] [Google Scholar]
- Grun F, Blumberg B. Endocrine disrupters as obesogens. Mol Cell Endocrinol. 2009;304:19–29. doi: 10.1016/j.mce.2009.02.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grun F, Watanabe H, Zamanian Z, Maeda L, Arima K, Cubacha R, Gardiner DM, Kanno J, Iguchi T, Blumberg B. Endocrine-disrupting organotin compounds are potent inducers of adipogenesis in vertebrates. Mol Endocrinol. 2006;20:2141–2155. doi: 10.1210/me.2005-0367. [DOI] [PubMed] [Google Scholar]
- Halpern P. Obesity and American Indians/Alaskan Natives. Washington, DC: United States Department of Health and Human Services; 2007. p. 169. [Google Scholar]
- Haman F, Fontaine-Bisson B, Batal M, Imbeault P, Blais JM, Robidoux MA. Obesity and type 2 diabetes in Northern Canada’s remote First Nations communities: the dietary dilemma. Int J Obes (Lond) 2010;34 (Suppl 2):S24–S31. doi: 10.1038/ijo.2010.236. [DOI] [PubMed] [Google Scholar]
- Hanley AJ, Harris SB, Gittelsohn J, Wolever TM, Saksvig B, Zinman B. Overweight among children and adolescents in a Native Canadian community: prevalence and associated factors. Am J Clin Nutr. 2000;71:693–700. doi: 10.1093/ajcn/71.3.693. [DOI] [PubMed] [Google Scholar]
- Harada M, Fujino T, Oorui T, Nakachi S, Nou T, Kizaki T, Hitomi Y, Nakano N, Ohno H. Followup study of mercury pollution in indigenous tribe reservations in the Province of Ontario, Canada, 1975–2002. Bull Environ Contam Toxicol. 2005;74:689–697. doi: 10.1007/s00128-005-0638-7. [DOI] [PubMed] [Google Scholar]
- Harris S, Harper B. A Native American exposure scenario. Risk Anal. 1997;17:789–795. doi: 10.1111/j.1539-6924.1997.tb01284.x. [DOI] [PubMed] [Google Scholar]
- Harvey-Berino J, Rourke J. Obesity prevention in preschool Native-American children: a pilot study using home visiting. Obes Res. 2003;11:606–611. doi: 10.1038/oby.2003.87. [DOI] [PubMed] [Google Scholar]
- Hauck FR, Gallaher MM, Yang-Oshida M, Serdula MK. Trends in anthropometric measurements among Mescalero Apache Indian pre-school children. 1968 through 1988. Am J Dis Child. 1992;146:1194–1198. doi: 10.1001/archpedi.1992.02160220080027. [DOI] [PubMed] [Google Scholar]
- Hearst MO, Laska MN, Himes JH, Butterbrodt M, Sinaiko A, Iron Cloud R, Tobacco M, Story M. The co-occurrence of obesity, elevated blood pressure, and acanthosis nigricans among American Indian school children: identifying individual heritage and environment-level correlates. Am J Hum Biol. 2011;23:346–352. doi: 10.1002/ajhb.21140. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Heck K, Schoendorf KC, Parker J. Are very low birthweight births among American Indians and Alaska Natives underregistered? Int J Epidemiol. 1999;28:1096–1101. doi: 10.1093/ije/28.6.1096. [DOI] [PubMed] [Google Scholar]
- Helmuth H. An anthropometric survey of Tyendinaga Mohawk children: secular trends. Can J Anthropol. 1983a;3:131–142. [Google Scholar]
- Helmuth H. Anthropometry and the secular trend in growth of Canadians. Zeitschrift Morphol Anthropol. 1983b;74:75–90. [PubMed] [Google Scholar]
- Ho L, Gittelsohn J, Sharma S, Cao X, Treuth M, Rimal R, Ford E, Harris S. Food-related behavior, physical activity, and dietary intake in First Nations—a population at high risk for diabetes. Ethn Health. 2008;13:335–349. doi: 10.1080/13557850701882936. [DOI] [PubMed] [Google Scholar]
- Indian Health Service. Trends in Indian health, 1996. Rockville, MD: US Department of Health and Human Services; 1997. [Google Scholar]
- Indian Health Service. Regional differences in Indian health, 1997. Rockville, MD: US Department of Health and Human Services; 1998. [Google Scholar]
- Indian Health Service. Trends in Indian health: 1998–1999. Rockville, MD: US Department of Health and Human Services; 2002. [Google Scholar]
- Jackson MY. Height, weight, and body mass index of American Indian schoolchildren, 1990–1991. J Am Diet Assoc. 1993;93:1136–1139. doi: 10.1016/0002-8223(93)91645-7. [DOI] [PubMed] [Google Scholar]
- Johnston FE, McKigney JI, Hopwood S, Smelker J. Physical growth and development of urban Native Americans: A study in urbanization and its implications for nutritional status. Am J Clin Nutr. 1978;31:1017–1027. doi: 10.1093/ajcn/31.6.1017. [DOI] [PubMed] [Google Scholar]
- Jollie-Trottier T, Holm JE, McDonald JD. Correlates of overweight and obesity in American Indian children. J Pediatr Psychol. 2009;34:245–253. doi: 10.1093/jpepsy/jsn047. [DOI] [PubMed] [Google Scholar]
- Jugan ML, Levi Y, Blondeau JP. Endocrine disruptors and thyroid hormone physiology. Biochem Pharmacol. 2010;79:939–947. doi: 10.1016/j.bcp.2009.11.006. [DOI] [PubMed] [Google Scholar]
- Karmaus W, Osuch JR, Eneli I, Mudd LM, Zhang J, Mikucki D, Haan P, Davis S. Maternal levels of dichlorodiphenyl-dichloroethylene (DDE) may increase weight and body mass index in adult female offspring. Occup Environ Med. 2009;66:143–149. doi: 10.1136/oem.2008.041921. [DOI] [PubMed] [Google Scholar]
- Katzmarzyk PT. The Canadian obesity epidemic: an historical perspective. Obes Res. 2002;10:666–674. doi: 10.1038/oby.2002.90. [DOI] [PubMed] [Google Scholar]
- Katzmarzyk PT. Obesity and physical activity among Aboriginal Canadians. Obesity (Silver Spring) 2007;16:184–190. doi: 10.1038/oby.2007.51. [DOI] [PubMed] [Google Scholar]
- Khalil CB, Johnson-Down L, Egeland GM. Emerging obesity and dietary habits among James Bay Cree youth. Public Health Nutr. 2010;13:1829–1837. doi: 10.1017/S1368980010000406. [DOI] [PubMed] [Google Scholar]
- Kuhnlein HV, Receveur O, Soueida R, Egeland GM. Arctic indigenous peoples experience the nutrition transition with changing dietary patterns and obesity. J Nutr. 2004;134:1447–1453. doi: 10.1093/jn/134.6.1447. [DOI] [PubMed] [Google Scholar]
- Lacetti G. General Motors/Central Foundry Division. Albany, NY: NYSDOH; 1993. Public health assessment. [Google Scholar]
- Lee DH, Lee IK, Song K, Steffes M, Toscano W, Baker BA, Jacobs DR., Jr A strong dose-response relation between serum concentrations of persistent organic pollutants and diabetes: results from the National Health and Examination Survey 1999–2002. Diabetes Care. 2006;29:1638–1644. doi: 10.2337/dc06-0543. [DOI] [PubMed] [Google Scholar]
- Lindsay RS, Cook V, Hanson RL, Salbe AD, Tataranni A, Knowler WC. Early excess weight gain of children in the Pima Indian population. Pediatrics. 2002;109:E33. doi: 10.1542/peds.109.2.e33. [DOI] [PubMed] [Google Scholar]
- Luo ZC, Wilkins R, Heaman M, Martens P, Smylie J, Hart L, Simonet F, Wassimi S, Wu Y, Fraser WD. Birth outcomes and infant mortality by the degree of rural isolation among first nations and non-first nations in Manitoba, Canada. J Rural Health. 2010;26:175–181. doi: 10.1111/j.1748-0361.2010.00279.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Luo ZC, Wilkins R, Platt RW, Kramer MS. Risks of adverse pregnancy outcomes among Inuit and North American Indian women in Quebec, 1985–1997. Paediatr Perinat Epidemiol. 2004;18:40–50. doi: 10.1111/j.1365-3016.2003.00529.x. [DOI] [PubMed] [Google Scholar]
- Lytle LA, Dixon LB, Cunningham-Sabo L, Evans M, Gittelsohn J, Hurley J, Snyder P, Stevens J, Weber J, Anliker J, et al. Dietary intakes of Native American children: findings from the pathways feasibility study. J Am Diet Assoc. 2002;102:555–558. doi: 10.1016/s0002-8223(02)90129-x. [DOI] [PubMed] [Google Scholar]
- MacMillan HL, Jamieson E, Walsh C, Boyle M, Crawford A, MacMillan A. The health of Canada’s Aboriginal children: results from the First Nations and Inuit Regional Health Survey. Int J Circumpolar Health. 2010;69:158–167. doi: 10.3402/ijch.v69i2.17439. [DOI] [PubMed] [Google Scholar]
- Madsen KA, Weedn AE, Crawford PB. Disparities in peaks, plateaus, and declines in prevalence of high BMI among adolescents. Pediatrics. 2010;126:434–442. doi: 10.1542/peds.2009-3411. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Martin JA, Hamilton BE, Ventura SJ, Osterman MJ, Kirmeyer S, Mathews TJ, Wilson E. Births: final data for 2009. National vital statistics reports: from the Centers for Disease Control and Prevention, National Center for Health Statistics. Natl Vital Stat Syst. 2011;60:1–104. [PubMed] [Google Scholar]
- Mendez MA, Garcia-Esteban R, Guxens M, Vrijheid M, Kogevinas M, Goni F, Fochs S, Sunyer J. Prenatal organochlorine compound exposure, rapid weight gain, and overweight in infancy. Environ Health Perspect. 2011;119:272–278. doi: 10.1289/ehp.1002169. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Miller MD, Crofton KM, Rice DC, Zoeller RT. Thyroid-disrupting chemicals: interpreting upstream biomarkers of adverse outcomes. Environ Health Perspect. 2009;117:1033–1041. doi: 10.1289/ehp.0800247. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Miller PS. Secular changes among the Western Apache. Am J Phys Anthropol. 1970;33:197–206. doi: 10.1002/ajpa.1330330205. [DOI] [PubMed] [Google Scholar]
- Moffatt MEK. In: Fortuine R, editor. Length, Weight, and Head Circumference in Quebec Cree Children; Circumpolar Health 84: Proceedings of the Sixth International Symposium on Circumpolar Health; Anchorage, Alaska: University of Washington Press; 1985. pp. 170–172. [Google Scholar]
- Munroe M, Shah CP, Badgley R, Bain HW. Birth weight, length, head circumference and bilirubin level in Indian newborns in the Sioux Lookout Zone, Northwestern Ontario. Can Med Assoc J. 1984;131:453–456. [PMC free article] [PubMed] [Google Scholar]
- National Center for Health Statistics. Advance report of final natality statistics, 1990. Hyattsville, MD: US Department of Health and Human Services, Public Health Service, Centers for Disease Control; 1993. [Google Scholar]
- Newbold RR, Padilla-Banks E, Snyder RJ, Jefferson WN. Perinatal exposure to environmental estrogens and the development of obesity. Mol Nutr Food Res. 2007a;51:912–917. doi: 10.1002/mnfr.200600259. [DOI] [PubMed] [Google Scholar]
- Newbold RR, Padilla-Banks E, Snyder RJ, Phillips TM, Jefferson WN. Developmental exposure to endocrine disruptors and the obesity epidemic. Reprod Toxicol. 2007b;23:290–296. doi: 10.1016/j.reprotox.2006.12.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ngnie Teta I. Secular trends in the physical growth of Cree children. Mistissini, QC: Cree Board of Health and Social Services of James Bay; 2002. [Google Scholar]
- Ogden CL, Carroll MD, Flegal KM. Epidemiologic trends in overweight and obesity. Endocrinol Metab Clin North Am. 2003;32:741–760. vii. doi: 10.1016/s0889-8529(03)00074-4. [DOI] [PubMed] [Google Scholar]
- Ogden CL, Flegal KM, Carroll MD, Johnson CL. Prevalence and trends in overweight among US children and adolescents, 1999–2000. J Am Med Assoc. 2002;288:1728–1732. doi: 10.1001/jama.288.14.1728. [DOI] [PubMed] [Google Scholar]
- Owen GM, Nelson C, Kram K, Garry P. Nutrition survey of White Mountain Apache preschool children. In: Moore W, Silverberg M, Read M, editors. Nutrition, growth and development of North American Indian children. Washington, DC: Government Printing Office; 1969. [Google Scholar]
- Park HY, Park JS, Sovcikova E, Kocan A, Linderholm L, Bergman A, Trnovec T, Hertz-Picciotto I. Exposure to hydroxylated polychlorinated biphenyls (OH-PCBs) in the prenatal period and subsequent neurodevelopment in Eastern Slovakia. Environ Health Perspect. 2009;117:1600–1606. doi: 10.1289/ehp.0900611. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pearce EN, Braverman LE. Environmental pollutants and the thyroid. Best Pract Res Clin Endocrinol Metab. 2009;23:801–813. doi: 10.1016/j.beem.2009.06.003. [DOI] [PubMed] [Google Scholar]
- Peck RE, Marks JS, Dibley MJ, Lee SL, Trowbridge FL. Birth weight and subsequent growth among Navajo children. Public Health Rep. 1987;102:500–507. [PMC free article] [PubMed] [Google Scholar]
- Polhamus B, Dalenius K, Mackintosh H, Smith B, Grummer-Strawn L. Pediatric nutrition surveillance 2009 report. Atlanta: Centers for Disease Control and Prevention; 2009. [Google Scholar]
- Rees W. Ecological footprints and appropriated carrying capacity: what urban economic leaves out. Environ Urban. 1992;4:121–130. [Google Scholar]
- Reisinger K, Rogers K, Johnson O. Nutrition survey of lower Greasewood, Arizona Navajos. Washington, DC: National Institute of Health; 1972. pp. 72–76. [Google Scholar]
- Salbe AD, Weyer C, Harper I, Lindsay RS, Ravussin E, Tataranni PA. Assessing risk factors for obesity between childhood and adolescence. II. Energy metabolism and physical activity. Pediatrics. 2002a;110:307–314. doi: 10.1542/peds.110.2.307. [DOI] [PubMed] [Google Scholar]
- Salbe AD, Weyer C, Lindsay RS, Ravussin E, Tataranni AP. Assessing risk factors for obesity between childhood and adolescence. I. Birth weight, childhood adiposity, parental obesity, insulin, and leptin. Pediatrics. 2002b;110:299–306. doi: 10.1542/peds.110.2.299. [DOI] [PubMed] [Google Scholar]
- Schell LM, Gallo MV, Cook K. What’s NOT to eat - Food adulteration in the context of human biology. Am J Hum Biol. 2012;24:139–148. doi: 10.1002/ajhb.22202. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schell LM, Gallo MV, Denham M, Ravenscroft J, DeCaprio AP, Carpenter DO. Relationship of thyroid hormone levels to levels of polychlorinated biphenyls, lead, p,p′-DDE, and other toxicants in Akwesasne Mohawk youth. Environ Health Perspect. 2008;116:806–813. doi: 10.1289/ehp.10490. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schell LM, Gallo MV, Johnston FE. Growth and development. In: Ubelaker D, editor. Handbook of North American Indians: environment, origins, and population. Washington, DC: Smithsonian Institution; 2006. pp. 727–739. [Google Scholar]
- Schell LM, Gallo MV, Ravenscroft J, DeCaprio AP. Persistent organic pollutants and anti-thyroid peroxidase levels in Akwesasne Mohawk young adults. Environ Res. 2009;109:86–92. doi: 10.1016/j.envres.2008.08.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schell LM, Ravenscroft J, Cole M, Jacobs A, Newman J Akwesasne Task Force on the Environment. Health disparities and toxicant exposure of Akwesasne Mohawk young adults. Environ Health Perspect. 2005;113:1826–1832. doi: 10.1289/ehp.7914. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sharma S, De Roose E, Cao X, Pokiak A, Gittelsohn J, Corriveau A. Dietary intake in a population undergoing a rapid transition in diet and lifestyle: the Inuvialuit in the Northwest Territories of Arctic Canada. Can J Public Health. 2009;100:442–448. doi: 10.1007/BF03404341. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shields M. Measured obesity: overweight Canadian children and adolescents. Nutrition: findings from the Canadian community health survey. Component of Statistical Canada Catologue. 2005;34 [Google Scholar]
- Ship II. Relationships of dental caries, tooth eruption and growth, based on a study of dicalcium phosphate dietary supplementation in an American Indian boarding school population. Pennsylvania: University of Pennsylvania, School of Medicine; 1964. [Google Scholar]
- Singh GK, Siahpush M, Kogan MD. Rising Social Inequalities in US Childhood Obesity, 2003–2007. Ann Epidemiol. 2010;20:40–52. doi: 10.1016/j.annepidem.2009.09.008. [DOI] [PubMed] [Google Scholar]
- Sloan RJ, Jock K. Chemical contaminants in fish from the St. Lawrence River drainage on lands of the Mohawk nation at Akwesasne and near the General Motors Corporation/Central Foundry Divisioin, Massena, NY Plant. Albany, NY: New York State Department of Environmental Conservation; 1990. [Google Scholar]
- Smith DT, Bartee RT, Dorozynski CM, Carr LJ. Prevalence of overweight and influence of out-of-school seasonal periods on body mass index among American Indian schoolchildren. Prev Chronic Dis. 2009;6:A20. [PMC free article] [PubMed] [Google Scholar]
- Stern NG, Barrett JR, Lawler FH. Childhood obesity onset in an urban American Indian health clinic. J Okla State Med Assoc. 2007;100:462–465. [PubMed] [Google Scholar]
- Story M, Evans M, Fabsitz RR, Clay TE, Holy RB, Broussard B. The epidemic of obesity in American Indian communities and the need for childhood obesity-prevention programs. Am J Clin Nutr. 1999;69:747S–754S. doi: 10.1093/ajcn/69.4.747S. [DOI] [PubMed] [Google Scholar]
- Story M, Stevens J, Himes JH, Stone E, Rock BH, Ethelbah B, Davis S. Obesity in American-Indian children: prevalence, consequences, and prevention. Prev Med. 2003;37:S3–S12. doi: 10.1016/j.ypmed.2003.08.008. [DOI] [PubMed] [Google Scholar]
- Story M, Strauss KF, Zephier E, Broussard BA. Nutritional concerns in American Indian and Alaska Native children: transitions and future directions. J Am Diet Assoc. 1998;98:170–176. doi: 10.1016/S0002-8223(98)00042-X. [DOI] [PubMed] [Google Scholar]
- Story M, Tompkins RA, Bass MA, Wakefield LM. Anthropometric measurements and dietary intakes of Cherokee Indian teenagers in North Carolina. J Am Diet Assoc. 1986;86:1555–1560. [PubMed] [Google Scholar]
- Stroehla BC, Malcoe LH, Velie EM. Dietary sources of nutrients among rural Native American and White children. J Am Diet Assoc. 2005;105:1908–1916. doi: 10.1016/j.jada.2005.09.002. [DOI] [PubMed] [Google Scholar]
- Stuart CA, Smith MM, Gilkison CR, Shaheb S, Stahn RM. Acanthosis Nigricans among Native Americans: an indicator of high diabetes risk. Am J Public Health. 1994;84:1839–1842. doi: 10.2105/ajph.84.11.1839. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sugarman JR, White LL, Gilbert TJ. Evidence for a secular change in obesity, height, and weight among Navajo Indian school children. Am J Clin Nutr. 1990;52:960–966. doi: 10.1093/ajcn/52.6.960. [DOI] [PubMed] [Google Scholar]
- Thomson M. Heavy birthweight in Native Indians of British Columbia. Can J Public Health. 1990;81:443–446. [PubMed] [Google Scholar]
- Tremblay MS, Katzmarzyk PT, Willms JD. Temporal trends in overweight and obesity in Canada, 1981–1996. Int J Obes. 2002;26:543. [PubMed] [Google Scholar]
- Uemura H, Arisawa K, Hiyoshi M, Kitayama A, Takami H, Sawachika F, Dakeshita S, Nii K, Satoh H, Sumiyoshi Y, et al. Prevalence of metabolic syndrome associated with body burden levels of dioxin and related compounds among Japan’s general population. Environ Health Perspect. 2009;117:568–573. doi: 10.1289/ehp.0800012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Van Duzen J, Carter JP, Secondi J, Federspiel C. Protein and calorie malnutrition among preschool Navajo Indian children. Am J Clin Nutr. 1969;22:1362–1370. doi: 10.1093/ajcn/22.10.1362. [DOI] [PubMed] [Google Scholar]
- Vanlandingham MJ, Buehler JW, Hogue CJ, Strauss LT. Birth-weight-specific infant mortality for native Americans compared with whites, six states, 1980. Am J Public Health. 1988;78:499–503. doi: 10.2105/ajph.78.5.499. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ventura SJ, Martin JA, Curtin SC, Mathews TJ. Report of final natality statistics, 1996. Mon Vital Stat Rep. 1998;46:1–99. [PubMed] [Google Scholar]
- Wells JCK. The evolutionary biology of human fatness. Cambridge: Cambridge University Press; 2010. [Google Scholar]
- Wenman WM, Joffres MR, Tataryn IV. A prospective cohort study of pregnancy risk factors and birth outcomes in Aboriginal women. Can Med Assoc J. 2004;171:585–589. doi: 10.1503/cmaj.1031730. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Willows ND. Overweight in First Nations children: prevalence, implications, and solutions. J Aborig Health. 2005;2:76–86. [Google Scholar]
- Willows ND, Johnson MS, Ball GD. Prevalence estimates of overweight and obesity in Cree preschool children in Northern Quebec according to international and US reference criteria. Am J Public Health. 2007;97:311–316. doi: 10.2105/AJPH.2005.073940. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Willows ND, Sanou D, Bell RC. Assessment of Canadian Cree infants’ birth size using the WHO Child Growth Standards. Am J Hum Biol. 2011;23:126–131. doi: 10.1002/ajhb.21115. [DOI] [PubMed] [Google Scholar]
- Wissler C. Measurements of Dakota Indian children. Ann N Y Acad Sci. 1911;20:355–364. [Google Scholar]
- Young TK. Sociocultural and behavioural determinants of obesity among Inuit in the central Canadian Arctic. Soc Sci Med. 1996;43:1665–1671. doi: 10.1016/s0277-9536(96)00075-5. [DOI] [PubMed] [Google Scholar]
- Young TK. Are the circumpolar Inuit becoming obese? Am J Hum Biol. 2007;19:181–189. doi: 10.1002/ajhb.20617. [DOI] [PubMed] [Google Scholar]
- Young TK, Dean HJ, Flett B, Wood-Steiman P. Childhood obesity in a population at high risk for type 2 diabetes. J Pediatr. 2000;136:365–369. doi: 10.1067/mpd.2000.103504. [DOI] [PubMed] [Google Scholar]
- Zaferatos NC. Environmental justice in Indian country: dumpsite remediation on the Swinomish Indian reservation. Environ Manag. 2006;38:896–909. doi: 10.1007/s00267-004-0103-0. [DOI] [PubMed] [Google Scholar]
- Zephier E, Himes JH, Story M. Prevalence of overweight and obesity in American Indian School children and adolescents in the Aberdeen area: a population study. Int J Obes Relat Metab Disord. 1999;23 (Suppl 2):S28–S30. doi: 10.1038/sj.ijo.0800856. [DOI] [PubMed] [Google Scholar]
- Zephier E, Himes JH, Story M, Zhou X. Increasing prevalences of overweight and obesity in Northern Plains American Indian children. Arch Pediatr Adolesc Med. 2006;160:34–39. doi: 10.1001/archpedi.160.1.34. [DOI] [PubMed] [Google Scholar]