Abstract
Generalized anxiety disorder (GAD) and major depressive disorder (MDD) frequently co-occur, yet the reasons for their comorbidity remain poorly understood. In the present experiment, we tested whether a tendency to engage in negative, repetitive thinking constitutes a common risk process for the two disorders. A mixed sample of adults with comorbid GAD-MDD (n = 50), GAD only (n = 35), MDD only (n = 34), or no lifetime psychopathology (n = 35) was administered noncontingent failure and success feedback on consecutive performance tasks. Perseverative thought (PT), measured by negative thought intrusions during a baseline period of focused breathing, emerged as a powerful prospective predictor of responses to this experimental challenge. Participants reporting more frequent negative thought intrusions at baseline, irrespective of thought content or diagnostic status, exhibited a stronger negative response to failure that persisted even after subsequent success. Higher PT over the course of the experiment was associated with later behavioral avoidance, with negative affect and other traits closely linked to anxiety and depression, and with the presence and severity of GAD and MDD. These findings provide evidence for a broadly-defined PT trait that is shared by GAD and MDD and contributes to adverse outcomes in these disorders.
Keywords: Perseveration, Worry, Rumination, Generalized Anxiety Disorder, Major Depression, Comorbidity
A sizable literature has shown that anxiety and mood disorders co-occur at levels far greater than chance (Brown, Campbell, Lehman, Grisham, & Mancill, 2001; Kessler et al., 1996). While the extent of comorbidity is well-established, the mechanisms underlying comorbidity are poorly understood. Prior attempts to explain comorbidity have focused on the shared influence of broad temperament dimensions such as negative affect or neuroticism (Brown, Chorpita, & Barlow, 1998; Goldberg, Krueger, Andrews, & Hobbs, 2009; Mineka, Watson, & Clark, 1998) but have stopped short of describing how broad dimensions increase risk for emotional disorders. Specifying behaviorally measurable processes through which risk is manifested is essential for understanding, treating, and ultimately preventing comorbidity and its associated disability. In recent years, a growing research base has drawn attention to functional processes that cut across disorders and may contribute to comorbidity (Harvey, Watkins, Mansell, & Shafran, 2004; Sanislow et al., 2010). Studying such processes directly—in samples that encompass multiple, relevant disorders—has been advocated for identifying improved phenotypes that map onto neural systems and intervention targets more readily than traditional disorders (Sanislow et al., 2010). Treating these common processes—rather than individual disorders—has also been advocated for increasing treatment flexibility and transportability (McHugh, Murray, & Barlow, 2009) and for enhancing clinical outcomes, especially among persons with comorbid psychopathology (Barlow, Allen, & Choate, 2004; Fairburn et al., 2009).
A promising place to begin the search for common processes is the relationship between generalized anxiety disorder (GAD) and major depressive disorder (MDD). GAD and MDD share perhaps the strongest association of all emotional disorders (Kessler, 1997; Watson, 2005), with upwards of 60% of those with GAD developing MDD in their lifetime (Kessler et al., 2008; Moffitt et al., 2007). GAD and MDD also share virtually all of their genetic risk (Kendler, 1996; Kendler, Gardner, Gatz, & Pederson, 2007; Kendler, Neale, Kessler, & Heath, 1992; Roy, Neale, Pedersen, & Mathé, 1995), suggesting that what is inherited is not the syndromes themselves, but common processes or traits that increase risk for both syndromes. What might these common processes be? One candidate is negative, repetitive thinking. Worry, the defining feature of GAD (American Psychiatric Association, 1994), involves a negative, relatively uncontrollable chain of thoughts concerning future events whose outcome is uncertain (Borkovec, Robinson, Pruzinsky, & DePree, 1983). Rumination, a vulnerability factor and associated feature of depression (Nolen-Hoeksema, Wisco, & Lyubomirsky, 2008; Wisco & Nolen-Hoeksema, 2008), similarly involves a negative, repetitive, passive style of thinking, partly about present symptoms (Nolen-Hoeksema, 1991) or concerns (Martin & Tesser, 1996) but mainly about the past (Thomsen, 2006), especially past loss or failure (Nolen-Hoeksema et al., 2008; Papageorgiou, 2006).
Although worry and rumination are hypothesized to differ in several ways (Nolen-Hoeksema et al., 2008), they appear to share many more similarities than differences (McLaughlin, Borkovec, & Sibrava, 2007; Segerstrom, Tsao, Alden, & Craske, 2000; Watkins, Moulds, & Mackintosh, 2005). Both are abstract, primarily verbal-linguistic, and negatively self-focused—all features which have been shown to perpetuate negative thought and affect (Holmes & Mathews, 2010; Mor & Winquist, 2002; Stokes & Hirsch, 2010). Both involve difficulty extricating attention from negative material, as evident in patterns of neural activation (Hoehn-Saric, Lee, McLeod, & Wong, 2005; Johnson, Nolen-Hoeksema, Mitchell, & Levin, 2009) and in subjective experiences of negative thoughts as “stuck,” persistent, and hard to control (Morrow & Nolen-Hoeksema, 1990; Ruscio & Borkovec, 2004). Finally, both reflect passive, unproductive fixation on largely unsolvable problems in ways that hamper effective coping (Borkovec, Ray, & Stöber, 1998; Nolen-Hoeksema et al., 2008), with similar negative consequences for mood, cognition, interpersonal function, and physical health (Watkins, 2008; Wisco & Nolen-Hoeksema, 2008).
Similarities like these have led to suggestions that worry and rumination represent the same core process of perseverative thought (PT) applied to different content in GAD and MDD (Harvey et al., 2004; McEvoy, Mahoney, & Moulds, 2010). The defining feature of the process is thought to be a tendency to engage in negative thinking in a repetitive, dyscontrolled manner, irrespective of the specific content or temporal focus of the thoughts (Ehring & Watkins, 2008). Evidence for a fundamentally similar thought process in GAD and MDD would have direct implications for treatment. It would draw clinical attention to commonalities across a wide array of thoughts that might efficiently be addressed by a core set of interventions. It would raise the possibility that established interventions for one disorder and thought type could profitably be transferred to the other. It would suggest that treating PT in the context of one disorder may help address or even prevent the onset of the second, comorbid disorder. Given the frequent co-occurrence of GAD and MDD, a modifiable process that cuts across these disorders may constitute an especially profitable target for treatment. However, while parallel findings for worry and rumination provide indirect support for such a process, large gaps in the literature have left important questions unanswered about PT and its role in GAD and MDD.
First, with few exceptions, worry and rumination have been studied in separate literatures using measures specific to each construct (e.g., Hayes, Hirsch, & Mathews, 2008; Nolen-Hoeksema, Morrow, & Fredrickson, 1993). This has challenged efforts to compare the core process of PT across disorders. Second, worry and rumination have typically been assessed using global self-report questionnaires (e.g., Meyer, Miller, Metzger, & Borkovec, 1990; Nolen-Hoeksema, & Morrow, 1991) rather than measures that track the experience of PT in particular situational contexts. Assessing PT in real time, as it unfolds in interaction with the environment, may illuminate pathways through which PT influences symptoms. Third, despite particular interest in the role played by rumination and worry in emotional disorders, investigations of PT have been carried out mainly with healthy or analogue samples (e.g., Moulds, Kandris, Starr, & Wong, 2007; Oathes, Siegle, & Ray, 2011). There is a need for research characterizing broadly-defined PT in GAD and MDD, both in comorbid and pure cases. Finally, most studies have assessed worry or rumination concurrently with outcomes (e.g., Fresco, Frankel, Mennin, Turk, & Heimberg, 2002; Muris, Roelofs, Rassin, Franken, & Mayer, 2005). This has made it difficult to evaluate PT as a potential risk factor rather than merely an epiphenomenon, correlate, or consequence of emotional distress. The case for PT as a risk mechanism would be strengthened if PT can be shown to predict subsequent adverse outcomes, especially following stress. The case would further be enhanced by demonstrating substantial incremental validity of PT over GAD and MDD diagnoses in predicting relevant outcomes.
To begin addressing these gaps, we investigated broadly-defined PT in a mixed sample of GAD and MDD cases and healthy controls. We chose this sample based on recommendations for studying transdiagnostic mechanisms (Sanislow et al., 2010) which call for sampling across clinical conditions in which the mechanism is implicated and for treating the mechanism—rather than diagnostic groupings—as the independent variable of interest. Including cases as well as controls, and comorbid as well as pure cases, enabled us to examine the predictive value of PT beyond the presence of one or both disorders with which it is most closely associated. PT was assessed “on-line” using thought sampling within the context of a focused breathing task. Baseline levels of naturally-occurring PT were used to predict responses to a subsequent emotional challenge. Associations of PT with clinical, course, and temperament measures were examined to further describe this putative risk mechanism in relation to anxiety and depression and to other risk dimensions (e.g., behavioral inhibition, intolerance of uncertainty) previously linked with these conditions. Consistent with a view of PT as a risk mechanism (e.g., Nolen-Hoeksema, 1991), we hypothesized that, regardless of diagnostic status, persons with elevated baseline PT would respond more negatively to a personal experience of failure and would continue to display more negative affect, cognition, and behavior even after an ensuing experience of success. Consistent with a view of PT as a shared mechanism for GAD and MDD (e.g., Ehring & Watkins, 2008), we hypothesized that PT would be elevated in both GAD and MDD relative to controls, associated with the severity and persistence of both disorders, and related to other vulnerability traits previously implicated in these disorders.
Methods
Participants
Participants were 154 adults recruited from the Philadelphia community (n = 119) and from the student body of a private northeastern university (n = 35). Participants were recruited through electronic and print media and, in the case of student participants, through a website maintained by the psychology department. They were assigned to one of four mutually exclusive groups based on current, primary (most severe) diagnosis: (1) comorbid GAD-MDD (n = 50) met criteria for both GAD and MDD; (2) GAD only (n = 35) met criteria for GAD, but not MDD; (3) MDD only (n = 34) met criteria for MDD, but not GAD; and (4) healthy controls (n = 35) had no past or current psychopathology. Persons with a primary diagnosis other than GAD or MDD, current substance abuse or dependence, active psychosis, or active suicidal intent were excluded from the study.
The final sample was 60% female and ranged in age from 18 to 80 years (M = 31.51, SD = 12.62). Most participants were never married (73%) and relatively well-educated (87% completed at least some college). Racial/ethnic composition was 66% Caucasian, 17% African-American, 11% Asian or Pacific Islander, 3% Hispanic, and 3% other ethnicity. Race, sex, and marital status did not differ significantly by diagnostic group, although controls were younger and less educated on average than clinical participants, especially those diagnosed with MDD (Table 1).
Table 1.
Demographic Characteristics of the Sample by Diagnostic Group
| Comorbid GAD-MDD (n = 50) |
GAD only (n = 35) |
MDD only (n = 34) |
Healthy controls (n = 35) |
|
|---|---|---|---|---|
| Age: M (SD)* | 34.16 (13.11) | 29.09 (10.40) | 36.03 (13.62) | 25.74 (10.46) |
| % Female | 66.0 | 57.1 | 61.8 | 51.4 |
| % Caucasian | 62.0 | 82.9 | 61.8 | 57.1 |
| Marital Status | ||||
| Never married | 68.0 | 77.1 | 69.7 | 82.4 |
| Married or cohabiting | 20.0 | 22.9 | 12.1 | 5.9 |
| Previously married | 12.0 | 0.0 | 18.2 | 11.8 |
| Education* | ||||
| High school or lower | 22.0 | 5.7 | 18.2 | 2.9 |
| Some college | 20.0 | 42.9 | 33.3 | 68.6 |
| College degree or higher | 58.0 | 51.4 | 48.5 | 28.6 |
Note. GAD = generalized anxiety disorder; MDD = major depressive disorder. Values represent percentages unless otherwise noted.
p < .05.
Measures
Clinical Measures
Participants were administered the Anxiety Disorders Interview Schedule for DSM-IV–Lifetime Version (ADIS-IV-L; Brown, DiNardo, & Barlow, 1994), a semi-structured clinical interview designed to assess current and lifetime episodes of anxiety, mood, and substance-related disorders. In addition to yielding DSM-IV diagnoses and establishing diagnostic primacy, the ADIS-IV-L provides detailed information about symptom severity and clinical course and yields an overall clinical severity rating (0–8) for each disorder. The interview is used widely (Brown & Barlow, 2001) and has high reliability and validity (Grisham, Brown, & Campbell, 2004). Participants also were administered the 17-item Hamilton Rating Scale for Depression (HAM-D; Hamilton, 1960) and the 14-item Hamilton Anxiety Rating Scale (HAM-A; Hamilton, 1959). These clinician-administered scales are commonly used to assess depression and anxiety severity and have good psychometric properties (López-Pina, Sánchez-Meca, & Rosa-Alcázar, 2009; Shear et al., 2001). Clinical measures were administered by interviewers with Master’s or Bachelor’s degrees in psychology who received extensive training in these measures and achieved a high level of interrater agreement with the experienced supervising licensed psychologist. Each case was reviewed at team meetings and final diagnostic decisions and clinical severity ratings were determined by consensus.
Experimental Measures
PT was assessed via thought sampling during a focused breathing task (FBT; Borkovec, Robinson, et al., 1983; Ruscio & Borkovec, 2004) completed at baseline, post-failure, and post-success. During each five-minute FBT, participants were signaled four times at varying intervals 30 to 120 seconds apart to prevent anticipation of when signals would occur. At each signal, participants completed a separate rating sheet containing the single question, “What were you doing when the beeper went off?” Participants circled whether, at the time of the signal, they were (a) completely focused on their breathing, (b) distracted by thoughts, or (c) other. Participants choosing an “other” response were asked to write a brief elaboration; “song stuck in head” and “slight headache approaching” were typical elaborations provided by participants. Participants who were distracted by thoughts were asked to circle whether these thoughts were (1) positive, (2) negative, or (3) neutral. The FBT provided an opportunity to freely worry or ruminate and so served as a behavioral measure of naturally-occurring PT (Borkovec, Robinson, et al., 1983; Hirsch, Hayes, & Mathews, 2009; McLaughlin et al., 2007; Ruscio & Borkovec, 2004).
Affective responses to failure and success were assessed using the Positive and Negative Affect Schedule–Expanded Form (PANAS-X; Watson & Clark, 1994). The PANAS-X assesses two broad, independent dimensions of emotional experience, negative affect (NA) and positive affect (PA), as well as several correlated yet distinct lower-order affective states (Watson & Tellegen, 1985). We used a 33-item version of the PANAS-X restricted to the subscales most relevant to our experiment, including the primary outcome of NA, plus PA and the lower-order scales of Fear, Guilt, Sadness, and Serenity. The PANAS-X was administered with state instructions (e.g., “Right now, to what extent do you feel happy?”) to capture immediate fluctuations in mood evoked by the emotional challenge.
Cognitive responses to failure and success were assessed by two questionnaires developed for this study. The Breathing Task Questionnaire probed thoughts experienced during the immediately preceding FBT. Using separate Likert-type scales, participants rated the frequency, intensity, and uncontrollability of negative intrusive thoughts and the anxious and depressed content of these thoughts. The Reactions Questionnaire assessed cognitive reactions to the emotional challenge persisting beyond the FBT. Using a scale from 1 (not at all) to 6 (extremely), participants rated the extent to which their thoughts “right now” were reflected by each of 10 statements. The statements assessed thoughts in five areas: perseveration about the experimental task (e.g., “Wishing I had done better on the word problem”); perseveration about oneself (e.g., “Thinking about my shortcomings, failings, and faults”); positive thoughts about the task (e.g., “Enjoying the feeling of having done well”); positive thoughts about oneself (e.g., “Feeling confident about my problem-solving abilities”); and perseveration about one’s problem-solving ability, assessed by different statements post-failure (e.g., “worrying about performing poorly on the next word problem”) and post-success (e.g., “worrying about my ability to do well on problem solving in the future”).
Behavioral responses to the experimental challenge were assessed through observation of social behavior on the premise that participants who were more affected by the stressor would be more likely to self-isolate in its aftermath (cf. Brewin, MacCarthy, & Furnham, 1989). Immediately after the experiment, while the experimenter ostensibly prepared a new room for administering questionnaires, participants were given the choice of waiting alone or with another participant who was also taking a break. Their choice was recorded as a dichotomous measure of social avoidance vs. affiliation.
Trait Measures
Several measures of individual differences were examined as correlates of behaviorally-assessed PT. Trait levels of PT were assessed using the Penn State Worry Questionnaire (Meyer et al., 1990), a measure of worry; the Brooding subscale (Treynor, Gonzalez, & Nolen-Hoeksema, 2003) of the Ruminative Responses Scale (Nolen-Hoeksema & Morrow, 1991), a measure of maladaptive depressive rumination; and the Rumination subscale of the Rumination-Reflection Questionnaire (Trapnell & Campbell, 1999), a measure of general rumination. Additional questionnaires assessed the temperament dimension of NA and closely related traits hypothesized to be associated with PT. Trait NA was assessed by the Neuroticism subscale of the Eysenck Personality Questionnaire–Revised (Eysenck, Eysenck, & Barrett, 1985) and by the NA subscale of the original PANAS (Watson, Clark, & Tellegen, 1988) administered with trait instructions. Trait anxiety was assessed by the State-Trait Anxiety Inventory–Trait form (STAI-T; Spielberger, Gorsuch, & Lushene, 1983). Behavioral inhibition, a trait reflecting high sensitivity to impending punishment, was assessed by the Behavioral Inhibition Scale of the BIS/BAS (Carver & White, 1994). Harm avoidance, the tendency to inhibit behavior in response to aversive stimuli, was assessed by the Harm Avoidance scale of the Temperament and Character Inventory (Cloninger, Przybeck, Svrakic, & Wetzel, 1994). Intolerance of uncertainty, the tendency to react negatively to uncertain situations and events, was assessed by the Intolerance of Uncertainty Scale (Freeston, Rhéaume, Letarte, Dugas, & Ladouceur, 1994). All questionnaires are established measures with good psychometric properties.
Procedure
The study took place over two laboratory visits, with each participant run individually through the procedure. Clinical measures were administered during the first visit. Eligible participants returned for a second visit to complete the experiment. The experiment began with a baseline PANAS-X, followed by the FBT. Participants were instructed to close their eyes and focus all of their attention on their breathing. They were informed that they would be signaled periodically by a beeper during the breathing task and that, when signaled, they were to turn over the top rating sheet in front of them and indicate what they were doing at the time of the signal. After setting aside the rating sheet, participants were instructed to return their full attention to their breathing.
Next, participants were informed that they would be completing two word problems. Both problems were anagrams in which participants were given five minutes to generate as many words as possible using the letters from a specified word. Participants were told that these word problems would be used to estimate their verbal ability, an important component of intellectual functioning, relative to their peer group (Philadelphia residents or university students). In actuality, all participants received identical noncontingent failure feedback (39th percentile compared to peers) after the first word problem and success feedback (82nd percentile compared to peers) after the second word problem. To enhance believability, participants’ forms were scored in front of them and participants were presented with an individualized graph showing their score at the reported percentile. On manipulation check measures, participants rated both failure and success feedback as highly believable (means of 5.76 and 5.81, respectively, on a 1–7 scale) and reported far greater satisfaction with their performance following success than failure feedback, t(151) = 21.34, p < .001. Failure feedback was followed by declines in PA, t(152) = −8.78, p < .001, and increases in NA, t(152) = 2.10, p = .037, relative to the baseline assessment, whereas success feedback was followed by increases in PA, t(152) = 5.67, p < .001, and declines in NA, t(152) = −9.30, p < .001, relative to the post-failure assessment.
After failure feedback and again after success feedback, participants completed the FBT, Breathing Task Questionnaire, PANAS-X, and Reactions Questionnaire. Immediately after the experiment, social avoidance or affiliation behavior was recorded. Participants took a short break before completing the trait measures and undergoing debriefing.
Results
Characteristics of the PT Dimension
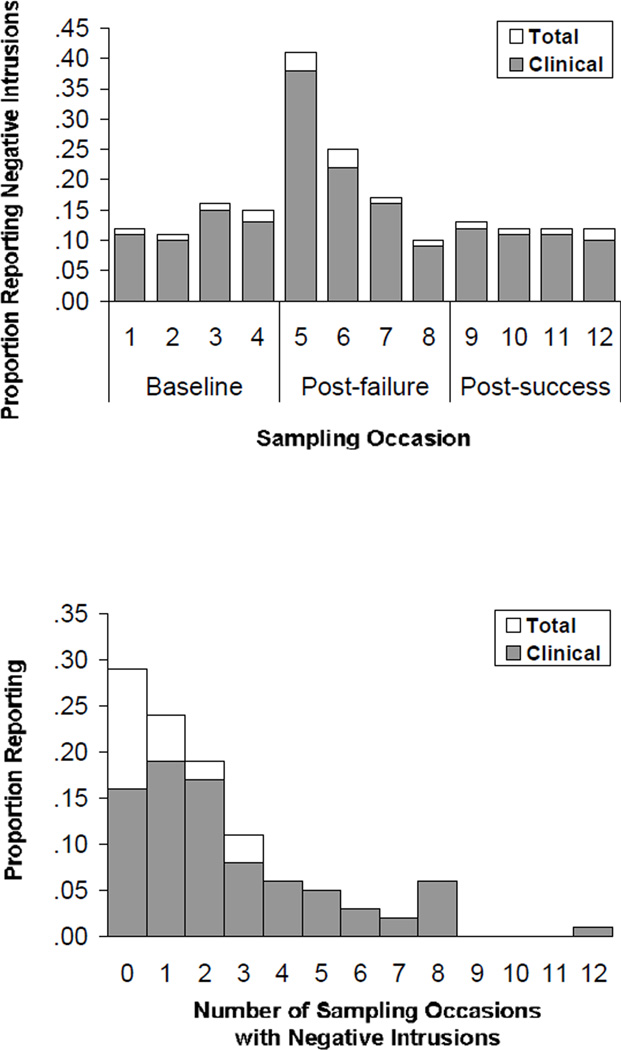
Negative thought intrusions reported during the baseline, post-failure, and post-success periods (Figure 1, top panel) were moderately to highly correlated (r = .38–.52) and together formed a reliable scale (Cronbach’s α = .71). Consequently, a single PT dimension was formed by summing the number of sampling occasions, out of 12, at which negative intrusions were reported across the experiment (Figure 1, bottom panel). This dimension was positively skewed: More than one-quarter of participants reported no negative intrusions, and of the remainder, most reported intrusions on one (24%) or two (19%) occasions. A non-negligible subsample, however, reported substantial PT, with 18% reporting negative intrusions on one-third or more and 6% reporting intrusions on one-half or more of sampling occasions. While negative intrusions were reported by all four groups, PT (transformed using a square root transformation to reduce skew) was higher for the three clinical groups than for controls, F(3, 150) = 7.36, p < .001, with no significant differences among comorbid GAD-MDD, GAD only, and MDD only cases.
Figure 1.
Proportion of the total sample and the clinical (GAD- or MDD-diagnosed) subsample reporting negative thought intrusions during the focused breathing task. The top panel displays the proportion reporting negative intrusions at each sampling occasion during the three experimental periods. The bottom panel displays the proportion with each score on the total perseverative thought dimension, calculated by summing the number of sampling occasions at which a negative intrusion was reported.
Baseline PT Predicting Subsequent Response to Emotional Challenge
Next, we evaluated PT as a predictor of subsequent response to failure feedback. In these analyses, we focused on PT occurring exclusively during the baseline FBT in order to evaluate naturally-occurring intrusions apart from the effects of the experimental manipulation. At baseline, 60 participants (39%) reported a total of 81 negative intrusions. Number of baseline negative intrusions (0–4) served as the independent variable in separate regression analyses for each outcome, with post-failure and post-success ratings serving as dependent variables. All analyses included as covariates the two demographic variables (age and education) previously shown to differ by diagnostic group. To estimate the predictive power of baseline PT over and above the variance captured by differences in diagnostic status, diagnostic group was also included in the covariate set using contrast coding. Interaction terms representing the products of these contrast codes with baseline PT were entered on the final step of each analysis to test for moderation effects.
Diagnostic group, together with demographics, accounted for 22% of the variance in NA following failure. Entered next into the model, PT explained an additional 20% of the variance in this outcome (Table 2). PT was a strong, nonspecific predictor of negative emotions (11–20%) and a reliable but relatively weaker predictor of positive emotions (3%) post-failure. PT also strongly predicted cognitive responses to failure, beyond large effects of the covariate set. Specifically, PT predicted the intrusion of negative thoughts post-failure (15%) and the subjective frequency and intensity (23%) and uncontrollability (5%) of those thoughts. PT was associated with both anxious (20%) and depressed (16%) thoughts, particularly with thoughts involving rumination about self (16%).
Table 2.
Variance Explained by Baseline Perseverative Thought in Outcome Measures Following Failure and Success Feedback, Over and Above the Effects of Diagnostic Group and Demographics
| Post-failure | Post-success | |||
|---|---|---|---|---|
| Outcome | β | ΔR2 | β | ΔR2 |
| Affect (PANAS-X) | ||||
| Negative affect | .47 | .20*** | .43 | .17*** |
| Fear | .47 | .20*** | .38 | .13*** |
| Guilt | .43 | .17*** | .44 | .18*** |
| Sadness | .35 | .11*** | .32 | .09*** |
| Serenity | −.32 | .10*** | −.26 | .06*** |
| Positive affect | −.17 | .03* | −.23 | .05** |
| Negative thought intrusions (FBT) | .40 | .15*** | .40 | .14*** |
| Cognitions during FBT (BTQ) | ||||
| Frequency and intensity of negative thoughts | .50 | .23*** | .52 | .25*** |
| Uncontrollability of negative thoughts | .23 | .05** | .12 | .01 |
| Anxious thought content | .47 | .20*** | .42 | .16*** |
| Depressed thought content | .42 | .16*** | .53 | .26*** |
| Cognitions after FBT (RQ) | ||||
| Rumination about completed word problem(s) | .20 | .04* | .19 | .03* |
| Rumination about self | .41 | .16*** | .43 | .17*** |
| Positive thoughts about completed word problem(s) | −.03 | .00 | −.20 | .04* |
| Positive thoughts about self | −.13 | .02 | −.16 | .02+ |
| Worry about upcoming word problem | .21 | .04** | —— | —— |
| Worry about future problem-solving performance | —— | —— | .36 | .12*** |
Note. PANAS-X = Positive and Negative Affect Schedule–Expanded Form; FBT = focused breathing task; BTQ = Breathing Task Questionnaire; RQ = Reactions Questionnaire. Values come from individual hierarchical regression analyses in which demographic variables (age, education) and group-related contrast codes were previously entered as covariates. Ns range from 152 to 154 across analyses.
p < .10.
p < .05.
p < .01.
p < .001.
Over and above the effects of group and demographics (21%), PT robustly predicted the persistence of NA after subsequent success feedback (17%). PT was broadly associated with persistently high Fear, Guilt, and Sadness (9–18%) as well as low Serenity (6%) and PA (5%) post-success. Notably, whereas group did not predict negative thought intrusions following the success experience (3%), PT did (14%). Baseline PT predicted more frequent and intense (25%), but not uncontrollable (1%), negative thoughts that were more anxious (16%) and depressed (26%) in content. It was again strongly associated with rumination about self (17%) as well as with worries about the ability to succeed in future problem-solving efforts (12%). Lastly, in a logistic analysis of covariance, PT predicted the decision to wait alone, rather than with another participant, during the waiting period, Wald χ2 (1) = 4.88, p = .027. Across analyses, the effects of PT did not vary systematically by diagnostic status; only 6 out of 33 tests of moderation yielded significant results, with little consistency in the particular interaction terms that were significant and with a relatively small proportion of variance explained by the set of interaction terms in outcomes, mdn R2 = .02, all R2 < .07.1
Correlates of the PT Dimension
The total, transformed PT dimension was moderately to highly correlated with questionnaire measures of trait perseveration (r = .35–.46) as well as with trait NA and other putative temperament risk dimensions for emotional disorders (r = .38–.50; Table 3). Clinically, PT was associated with more severe anxiety and depression in general, and more severe GAD and MDD in particular (r = .33–.36). The associations were larger for current than past psychopathology, with PT largely unrelated to illness course and related to current (r = .31), but not past (r = .02), comorbid disorders. The exception was a finding linking PT to significantly greater recurrence of MDD (r = .18) and marginally greater recurrence of GAD (r = .15) over the lifespan.
Table 3.
Personality and Clinical Correlates of the Total Perseverative Thought Dimension
| Variable | n | r |
|---|---|---|
| Trait perseveration | ||
| Penn State Worry Questionnaire | 154 | .35*** |
| RRS Brooding | 154 | .42*** |
| RRQ Rumination | 154 | .46*** |
| Temperament dimensions | ||
| EPQ-R Neuroticism | 154 | .43*** |
| PANAS Negative Affect | 153 | .42*** |
| Behavioral Inhibition Scale | 154 | .38*** |
| TCI Harm Avoidance | 153 | .39*** |
| State-Trait Anxiety Inventory–Trait | 154 | .49*** |
| Intolerance of Uncertainty Scale | 153 | .50*** |
| Clinical features | ||
| Hamilton Anxiety Rating Scale | 154 | .36*** |
| Hamilton Rating Scale for Depression | 154 | .34*** |
| GAD clinical severity | 154 | .36*** |
| Percent of the day spent worrying | 150 | .40*** |
| Excessiveness of worry (average) | 154 | .28*** |
| Excessiveness of worry (minor matters) | 154 | .25** |
| Uncontrollability of worry (average) | 154 | .35*** |
| Uncontrollability of worry (minor matters) | 153 | .39*** |
| MDD clinical severity | 154 | .33*** |
| Number of current comorbid disordersa | 154 | .31*** |
| Number of lifetime comorbid disordersa | 154 | .02 |
| Illness course | ||
| GAD | ||
| Tendency to worry as a child | 110 | .17+ |
| Age of onset of first episode | 118 | .07 |
| Duration of current episode | 117 | .02 |
| Months in episode over lifetime | 121 | −.04 |
| Number of lifetime episodes | 153 | .15+ |
| MDD | ||
| Age of onset of first episode | 125 | .08 |
| Duration of current episode | 112 | .02 |
| Months in episode over lifetime | 126 | −.04 |
| Number of lifetime episodes | 153 | .18* |
Note. RRS = Ruminative Responses Scale; RRQ = Rumination-Reflection Questionnaire; EPQ-R = Eysenck Personality Questionnaire–Revised; PANAS = Positive and Negative Affect Schedule; TCI = Temperament and Character Inventory; GAD = generalized anxiety disorder; MDD = major depressive disorder.
Excludes GAD and MDD.
p < .10.
p < .05.
p < .01.
p < .001.
Discussion
The present study examined whether a core process of perseverative thinking cuts across GAD and MDD and contributes to risk in these disorders. Among persons with GAD and MDD as well as healthy controls, those experiencing the most frequent negative thought intrusions at baseline, regardless of thought content, exhibited the strongest and most sustained negative response to a subsequent stressor. Negative intrusions were quite consistent across experimental phases, were related to putative vulnerability traits for emotional disorders, and were associated with the presence and severity of GAD and MDD. These findings provide evidence for a broadly-defined PT trait that is shared by GAD and MDD and contributes to adverse outcomes in these disorders.
Several results presented here suggest that PT functions as a common mechanism for anxiety and depression. PT predicted anxious as well as depressed affect and cognitions following emotional challenge and shared similar associations with clinically-rated anxiety and depression severity. These findings are in line with a handful of studies showing that worry is heightened in depression (Starcevic, 1995), rumination is heightened in anxiety (Harrington & Blankenship, 2002), and both forms of PT increase anxious and depressed affect (Andrews & Borkovec, 1988; McLaughlin et al., 2007). Such studies have been rare, however, in a literature in which worry is investigated almost exclusively in relation to anxiety, and rumination in relation to depression. Contrary to this conventional division, we found the core process of intrusive negative thought to be a nonspecific predictor of negative emotional experience, consistent with its proposed contribution to both anxiety and mood disorders and hence to their comorbidity. Perhaps most striking was the considerable predictive power of this process even after accounting for the effects of GAD and MDD, despite strong associations of these disorders with PT and with the outcomes examined here. Collectively, these findings argue for studying PT across anxiety and mood disorders and for including PT along with clinical syndromes in efforts to predict and explain emotional disturbance.
These conclusions echo calls for an increased focus on functional processes that span traditional mental disorder categories (Harvey et al., 2004; Insel & Cuthbert, 2009). The complexity and heterogeneity of traditional syndromes—and the consequent challenges of mapping these syndromes onto brain systems, molecules, cells, and genes—has led to the pursuit of narrower dimensions of functioning that are disrupted in psychopathology. Several initial dimensions that have been proposed for emotional disorders (Sanislow et al., 2010), including fear and reward processes, do not capture features linking GAD with MDD; other dimensions, such as NA, are themselves so complex that they may have limited value for identifying neural and genetic underpinnings of affective disturbance. Our data support PT as a promising functional mechanism for emotional disorders with relevance for GAD and MDD. Indeed, robust associations of PT with trait NA in our sample, together with prior research showing that worry and rumination mediate the association of NA with anxiety and depression (Muris et al., 2005), imply that PT may be one process through which NA increases risk for emotional disorders. Although future experimental manipulation of PT is required to establish a causal influence, our findings suggest two pathways through which PT may influence symptoms: first, through heightened negative response to failure, perhaps resulting from negative self-focused thoughts; and secondarily, through attenuated positive response to success. Additional research is needed to isolate other pathways through which PT has its effects and to probe still more basic processes (e.g., attention, cognitive flexibility, cognitive control) whose disruption underlies experiences of PT and whose normalization could help prevent or treat emotional disturbance.
An important question to be addressed by future research is whether PT constitutes an etiological factor, maintaining factor, or severity marker for GAD and MDD. Our investigation of currently-ill individuals, while speaking to the clinical significance of PT, precludes a clear answer to this question. Studies showing that worry and rumination are relatively stable over time (Just & Alloy, 1997; Meyer et al., 1990) even in the absence of acute disorder episodes (McMurrich & Johnson, 2008; Roberts, Gilboa, & Gotlib, 1998) suggest that PT is not merely a marker of current illness severity, although stronger associations with current than lifetime psychopathology reported here suggest that the strength of PT may vary somewhat with symptoms. An important next step is to determine whether PT predicts the first onset of GAD and MDD and is a plausible etiological factor or intermediate phenotype (Insel & Cuthbert, 2009) for these disorders, or whether PT is better understood as maintaining GAD and MDD once they have developed, perhaps in part by increasing sensitivity to stress.
While the etiological influence of PT remains to be determined, the discovery that PT robustly predicts response to stress in GAD and MDD speaks to a possible role of PT in maintaining these disorders. This possibility raises a number of intriguing clinical implications. Together with emerging evidence that rumination, as well as worry, is elevated in GAD (Seitchik, Raposa, Weisbrot, & Ruscio, 2007), our findings challenge the primary focus on worry in cognitive-behavioral therapy for GAD and suggest that outcomes may be improved by extending the focus to rumination. Our findings likewise hint at the potential value of PT-focused interventions as adjuncts to MDD treatments, which historically have paid less attention to thought process than to thought content and which do not, as a rule, target perseverative thinking (cf. Beck, Rush, Shaw, & Emery, 1979). Such interventions might draw on strategies that have been shown to decrease worry (e.g., stimulus-control interventions, present-moment focus; Borkovec, Wilkinson, Folensbee, & Lerman, 1983; Brosschot & Van Der Doef, 2006) as well as those that have been used to target rumination (e.g., functional analysis, directed imagery; Jacobson, Martell, & Dimidjian, 2001; Watkins et al., 2007). Broadening patient (and therapist) recognition of repetitive, “stuck” thinking—whether directed toward future threat, present distress, or past loss—may enhance early detection of PT in its myriad forms and facilitate its replacement with more adaptive responses. Additionally, as GAD so often presents with comorbid MDD, interventions targeting a functional process shared by these disorders are likely to enhance treatment efficiency. Such interventions are in line with calls for treatments that take relevant comorbidity into consideration (Ruscio & Holohan, 2006) and that address transdiagnostic mechanisms which contribute to varied psychopathological outcomes (Harvey et al., 2004).
Several limitations temper the strength of conclusions that may be drawn from this study. First, in order to maximize statistical power, all participants underwent an identical emotional challenge involving negative, followed by positive, performance feedback. Although changes in satisfaction, cognition, and emotion coincided with the timing of failure and success feedback, the absence of a no-challenge control condition prevents us from attributing these outcomes with certainty to the feedback received. Second, for ethical and pragmatic reasons, the emotional challenge employed here was relatively minor. While participants regarded the feedback as believable and responded differently to the failure and success experiences, generalizability to more severe stressors remains to be established. Third, in order to provide a detailed characterization of the nature and correlates of PT, we examined PT in relation to a large number of experimental and clinical measures. The consistency of findings across these measures increases confidence in the results. Nevertheless, replication in new samples and extension to new measures are needed to corroborate the promising initial findings reported here.
Fourth, the thought sampling method used by the FBT—while correlated with relevant questionnaires, sensitive to situational context, and predictive of important outcomes—is doubtlessly an imperfect measure of PT. The internal, private nature of PT challenges efforts to assess its occurrence objectively, apart from its subjective experience and immediate impact. Its assessment is further complicated by a lack of consensus over how long thoughts must persist, or how repetitive thoughts must be (at the level of phrases, topics, or themes), to be considered perseverative. We chose to operationalize PT on the basis of negative content and uncontrollability, as these are two features of the process for which there is emerging consensus (cf. Ehring & Watkins, 2008). To minimize interference with the process, we assessed PT using brief, relatively infrequent thought sampling. This approach enhanced ecological validity, but likely missed some negative thoughts. It also did not distinguish isolated negative intrusions from the persistent sequence of interconnected thoughts more typically associated with PT. These limitations are tempered somewhat by robust correlations of the PT dimension with trait measures of perseveration as well as with varied outcomes of clinical interest. Nevertheless, other thought sampling approaches, including more frequent sampling or more detailed assessment of thought content (cf. Hirsch et al., 2009), may yield a more refined measure of PT with even greater predictive validity.
Aside from refinement of the FBT, there is room for the development of improved behavioral and neurobiological measures of PT, including measures of specific aspects of PT that are important for emotional disorders (e.g., termination capacity; Paulesu et al., 2010). One promising measurement approach, given the inherently persistent nature of PT, is to assess the process repeatedly in daily life over longer intervals than are possible in the laboratory. Researchers have begun to use ecological momentary assessment of this sort to study worry (Szabo & Lovibond, 2002; Verkuil, Brosschot, & Thayer, 2007) and rumination (Moberly & Watkins, 2008) and might profitably extend this work to broadly-defined PT. An advantage of this approach is that it would allow PT to be studied in response to ongoing as well as acute events and in relation to mediating variables that cannot be manipulated experimentally. Resulting discoveries about PT, and about the mechanisms through which it influences anxiety and depression, have the potential to yield more powerful interventions for GAD, MDD, and their disabling and costly comorbidity.
Highlights.
Perseverative thought (PT) was evaluated as a shared risk process for GAD and MDD.
We defined PT as negative, dyscontrolled thinking, without regard to thought content.
PT prospectively predicted adverse responses to a laboratory stressor.
PT had substantial incremental validity as a predictor over diagnostic status.
PT was associated with the presence and severity of GAD and MDD.
Acknowledgments
This research was supported in part by a University Research Foundation grant from the University of Pennsylvania. We thank Kelly Allred, Brooke Boyarski, Jenna Feldman, Maria Gaudio, Michael Haas, Christina Hadzitheodorou, Julie Helinek, Kendall Hoescht, Jenna Katz, Lindsey Sankin, Rhia Shah, Julie Stein, Kristin Szuhany, Sophie York-Williams, and Jeanette Zhang for their help with recruitment and data collection and Elizabeth S. Coleman for her assistance in preparing the manuscript.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Although PT predicted affective, cognitive, and behavioral outcomes following emotional challenge, it was less clear whether PT predicted changes in these outcomes in reaction to the challenge. Having assessed affect at baseline as well as post-manipulation, we performed sensitivity analyses in which baseline PT was used to predict subsequent affect, controlling for baseline affect as well as diagnostic group, age, and education. After baseline NA, diagnostic group, and demographics captured 66% of the variance in post-failure NA, PT explained a modest but significant portion of the remaining variance, β = .20, F(1, 143) = 13.18, p < .001, predicting heightened Fear, Sadness, and Guilt reactivity and diminished Serenity, all βs ≥ .16, all ps < .007. In contrast, PT no longer predicted post-failure PA after 73% of the variance was captured by the covariate set, β = −.05, F(1, 143) = 1.12, p = .291. In predicting reactions to subsequent success, PT provided a small but significant improvement in prediction of NA over the 61% of variance explained by baseline NA, group, and demographics, β = .17, F(1, 144) = 8.87, p = .003. PT predicted sustained Fear, Sadness, and Guilt reactivity and persistently low Serenity, all βs ≥ .14, all ps < .008. PT also predicted attenuated PA reactivity to success, β = −.11, F(1, 144) = 4.23, p = .041, beyond the covariate set (61%). Diagnostic group moderated the effects of PT for only 1 of the 12 outcomes, mdn R2 = .01, all R2 < .03. In sum, even in very conservative analyses examining emotional reactivity, PT had incremental value as a predictor.
References
- American Psychiatric Association. Diagnostic and statistical manual of mental disorders (4th ed.) Washington, DC: American Psychiatric Association; 1994. [Google Scholar]
- Andrews VH, Borkovec TD. The differential effects of inductions of worry, somatic anxiety, and depression on emotional experience. Journal of Behavior Therapy and Experimental Psychiatry. 1988;19:21–26. doi: 10.1016/0005-7916(88)90006-7. [DOI] [PubMed] [Google Scholar]
- Barlow DH, Allen LB, Choate ML. Toward a unified treatment for emotional disorders. Behavior Therapy. 2004;35:205–230. doi: 10.1016/j.beth.2016.11.005. [DOI] [PubMed] [Google Scholar]
- Beck AT, Rush AJ, Shaw BF, Emery G. Cognitive therapy of depression: A treatment manual. New York, NY: The Guilford Press; 1979. [Google Scholar]
- Borkovec TD, Ray WJ, Stöber J. Worry: A cognitive phenomenon intimately linked to affective, physiological, and interpersonal behavioral processes. Cognitive Therapy and Research. 1998;22:561–576. [Google Scholar]
- Borkovec TD, Robinson E, Pruzinsky T, DePree JA. Preliminary exploration of worry: Some characteristics and processes. Behaviour Research and Therapy. 1983;21:9–16. doi: 10.1016/0005-7967(83)90121-3. [DOI] [PubMed] [Google Scholar]
- Borkovec TD, Wilkinson L, Folensbee R, Lerman C. Stimulus control applications to the treatment of worry. Behaviour Research and Therapy. 1983;21:247–251. doi: 10.1016/0005-7967(83)90206-1. [DOI] [PubMed] [Google Scholar]
- Brewin CR, MacCarthy B, Furnham A. Social support in the face of adversity: The role of cognitive appraisal. Journal of Research in Personality. 1989;23:354–372. [Google Scholar]
- Brosschot JF, Van Der Doef M. Daily worrying and somatic health complaints: Testing the effectiveness of a simple worry reduction intervention. Psychology & Health. 2006;21:19–31. [Google Scholar]
- Brown TA, Barlow DH. Classification of anxiety and mood disorders. In: Barlow DH, editor. Anxiety and its disorders: The nature and treatment of anxiety and panic (2nd ed.) New York, NY: Guilford Press; 2001. pp. 292–327. [Google Scholar]
- Brown TA, Campbell LA, Lehman CL, Grisham JR, Mancill RB. Current and lifetime comorbidity of the DSM-IV anxiety and mood disorders in a large clinical sample. Journal of Abnormal Psychology. 2001;110:585–599. doi: 10.1037//0021-843x.110.4.585. [DOI] [PubMed] [Google Scholar]
- Brown TA, Chorpita BF, Barlow DH. Structural relationships among dimensions of the DSM-IV anxiety and mood disorders and dimensions of negative affect, positive affect, and autonomic arousal. Journal of Abnormal Psychology. 1998;107:179–192. doi: 10.1037//0021-843x.107.2.179. [DOI] [PubMed] [Google Scholar]
- Brown TA, DiNardo PA, Barlow DH. Anxiety Disorders Interview Schedule for DSM-IV. New York, NY: Oxford University Press; 1994. [Google Scholar]
- Carver CS, White TL. Behavioral inhibition, behavioral activation, and affective responses to impending reward and punishment: The BIS/BAS scales. Journal of Personality and Social Psychology. 1994;67:319–333. [Google Scholar]
- Cloninger CR, Przybeck TR, Svrakic DM, Wetzel RD. The Temperament and Character Inventory (TCI): A guide to its development and use. St Louis, MO: Center for Psycho-biology of Personality; 1994. [Google Scholar]
- Ehring T, Watkins ER. Repetitive negative thinking as a transdiagnostic process. International Journal of Cognitive Therapy. 2008;1:192–205. [Google Scholar]
- Eysenck SBG, Eysenck HJ, Barrett P. A revised version of the psychoticism scale. Personality and Individual Differences. 1985;6:21–29. [Google Scholar]
- Fairburn CG, Cooper Z, Doll HA, O’Connor ME, Bohn K, Hawker DM, Palmer RL. Transdiagnostic cognitive-behavioral therapy for patients with eating disorders: A two-site trial with 60-week follow-up. American Journal of Psychiatry. 2009;166:311–319. doi: 10.1176/appi.ajp.2008.08040608. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Freeston MH, Rhéaume J, Letarte H, Dugas MJ, Ladouceur R. Why do people worry? Personality and Individual Differences. 1994;17:791–802. [Google Scholar]
- Fresco DM, Frankel AN, Mennin DS, Turk CL, Heimberg RG. Distinct and overlapping features of rumination and worry: The relationship of cognitive production to negative affective states. Cognitive Therapy and Research. 2002;26:179–188. [Google Scholar]
- Goldberg D, Krueger RF, Andrews G, Hobbs MJ. Emotional disorders: Cluster 4 of the proposed meta-structure for DSM-V and ICD-11. Psychological Medicine. 2009;39:2043–2059. doi: 10.1017/S0033291709990298. [DOI] [PubMed] [Google Scholar]
- Grisham JR, Brown TA, Campbell LA. The Anxiety Disorders Interview Schedule for DSM-IV (ADIS-IV) In: Hilsenroth MJ, Segal DL, editors. Comprehensive handbook of psychological assessment, Vol. 2: Personality assessment. Hoboken, NJ: Wiley Publishing; 2004. pp. 163–177. [Google Scholar]
- Hamilton M. The assessment of anxiety states by rating. British Journal of Medical Psychology. 1959;32:50–55. doi: 10.1111/j.2044-8341.1959.tb00467.x. [DOI] [PubMed] [Google Scholar]
- Hamilton M. A rating scale for depression. Journal of Neurosurgery Psychiatry. 1960;23:56–62. doi: 10.1136/jnnp.23.1.56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Harrington JA, Blankenship V. Ruminative thoughts and their relation to depression and anxiety. Journal of Applied Social Psychology. 2002;32:465–485. [Google Scholar]
- Harvey AG, Watkins E, Mansell W, Shafran R. Cognitive behavioural processes across psychological disorders: A transdiagnostic approach to research and treatment. New York, NY: Oxford University Press; 2004. [Google Scholar]
- Hayes S, Hirsch C, Mathews A. Restriction of working memory capacity during worry. Journal of Abnormal Psychology. 2008;117:712–717. doi: 10.1037/a0012908. [DOI] [PubMed] [Google Scholar]
- Hirsch CR, Hayes S, Mathews A. Looking on the bright side: Accessing benign meanings reduces worry. Journal of Abnormal Psychology. 2009;118:44–54. doi: 10.1037/a0013473. [DOI] [PubMed] [Google Scholar]
- Hoehn-Saric R, Lee JS, McLeod DR, Wong DF. Effect of worry on regional cerebral blood flow in nonanxious subjects. Psychiatry Research: Neuroimaging. 2005;140:259–269. doi: 10.1016/j.pscychresns.2005.05.013. [DOI] [PubMed] [Google Scholar]
- Holmes EA, Mathews A. Mental imagery in emotion and emotional disorders. Clinical Psychology Review. 2010;30:349–362. doi: 10.1016/j.cpr.2010.01.001. [DOI] [PubMed] [Google Scholar]
- Insel T, Cuthbert BN. Endophenotypes: Bridging genomic complexity and disorder heterogeneity. Biological Psychiatry. 2009;66:988–989. doi: 10.1016/j.biopsych.2009.10.008. [DOI] [PubMed] [Google Scholar]
- Jacobson NS, Martell CR, Dimidjian S. Behavioral activation treatment for depression: Returning to contextual roots. Clinical Psychology: Science and Practice. 2001;8:255–270. [Google Scholar]
- Johnson MK, Nolen-Hoeksema S, Mitchell KJ, Levin Y. Medial cortex activity, self-reflection and depression. Social Cognitive and Affective Neuroscience. 2009;4:313–327. doi: 10.1093/scan/nsp022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Just N, Alloy LB. The response styles theory of depression: Tests and an extension of the theory. Journal of Abnormal Psychology. 1997;106:221–229. doi: 10.1037//0021-843x.106.2.221. [DOI] [PubMed] [Google Scholar]
- Kendler KS. Major depression and generalised anxiety disorder: Same genes, (partly) different environments—Revisited. British Journal of Psychiatry. 1996;168:68–75. [PubMed] [Google Scholar]
- Kendler KS, Gardner CO, Gatz M, Pederson NL. The sources of co-morbidity between major depression and generalized anxiety disorder in a Swedish national twin sample. Psychological Medicine. 2007;37:453–462. doi: 10.1017/S0033291706009135. [DOI] [PubMed] [Google Scholar]
- Kendler KS, Neale MC, Kessler RC, Heath AC. Major depression and generalized anxiety disorder: Same genes, (partly) different environments? Archives of General Psychiatry. 1992;49:716–722. doi: 10.1001/archpsyc.1992.01820090044008. [DOI] [PubMed] [Google Scholar]
- Kessler RC. The prevalence of psychiatric comorbidity. In: Wetzler S, Sanderson WC, editors. Treatment strategies for patients with psychiatric comorbidity. New York, NY: Wiley Publishing; 1997. pp. 23–48. [Google Scholar]
- Kessler RC, Gruber M, Hettema JM, Hwang I, Sampson N, Yonkers KA. Co-morbid major depression and generalized anxiety disorders in the National Comorbidity Survey follow-up. In: Goldberg D, Kendler KS, Sirovatka PJ, Regier DA, editors. Diagnostic issues in depression and generalized anxiety disorder: Refining the research agenda for DSM-V. Arlington, VA: American Psychiatric Association; 2008. pp. 139–170. [Google Scholar]
- Kessler RC, Nelson CB, McGonagle KA, Liu J, Swartz M, Blazer DG. Comorbidity of DSM-III-R major depressive disorder in the general population: Results from the US National Comorbidity Survey. British Journal of Psychiatry. 1996;168:17–30. [PubMed] [Google Scholar]
- López-Pina JA, Sánchez-Meca J, Rosa-Alcázar AI. The Hamilton Rating Scale for Depression: A meta-analytic reliability generalization study. International Journal of Clinical and Health Psychology. 2009;9:143–159. [Google Scholar]
- Martin LL, Tesser A. Some ruminative thoughts. In: Wyer RS Jr, editor. Advances in social cognition, Vol. 9: Ruminative thoughts. Hillsdale, NJ: Erlbaum; 1996. pp. 1–47. [Google Scholar]
- McEvoy PM, Mahoney AEJ, Moulds ML. Are worry, rumination, and post-event processing one and the same? Development of the repetitive thinking questionnaire. Journal of Anxiety Disorders. 2010;24:500–519. doi: 10.1016/j.janxdis.2010.03.008. [DOI] [PubMed] [Google Scholar]
- McHugh RK, Murray HW, Barlow DH. Balancing fidelity and adaptation in the dissemination of empirically-supported treatments: The promise of transdiagnostic interventions. Behaviour Research and Therapy. 2009;47:946–953. doi: 10.1016/j.brat.2009.07.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McLaughlin KA, Borkovec TD, Sibrava NJ. The effects of worry and rumination on affect states and cognitive activity. Behavior Therapy. 2007;38:22–38. doi: 10.1016/j.beth.2006.03.003. [DOI] [PubMed] [Google Scholar]
- McMurrich SL, Johnson SL. Dispositional rumination in individuals with a depression history. Cognitive Therapy and Research. 2008;32:542–553. doi: 10.1007/s10608-006-9093-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Meyer TJ, Miller ML, Metzger RL, Borkovec TD. Development and validation of the Penn State Worry Questionnaire. Behaviour Research and Therapy. 1990;28:487–495. doi: 10.1016/0005-7967(90)90135-6. [DOI] [PubMed] [Google Scholar]
- Mineka S, Watson D, Clark LA. Comorbidity of anxiety and unipolar mood disorders. Annual Review of Psychology. 1998;49:377–412. doi: 10.1146/annurev.psych.49.1.377. [DOI] [PubMed] [Google Scholar]
- Moberly NJ, Watkins ER. Ruminative self-focus and negative affect: An experience sampling study. Journal of Abnormal Psychology. 2008;117:314–323. doi: 10.1037/0021-843X.117.2.314. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moffitt TE, Harrington H, Caspi A, Kim-Cohen J, Goldberg D, Gregory AM, Poulton R. Depression and generalized anxiety disorder. Archives of General Psychiatry. 2007;64:651–660. doi: 10.1001/archpsyc.64.6.651. [DOI] [PubMed] [Google Scholar]
- Mor N, Winquist J. Self-focused attention and negative affect: A meta-analysis. Psychological Bulletin. 2002;128:638–662. doi: 10.1037/0033-2909.128.4.638. [DOI] [PubMed] [Google Scholar]
- Morrow J, Nolen-Hoeksema S. Effects of responses to depression on the remediation of depressive affect. Journal of Personality and Social Psychology. 1990;58:519–527. doi: 10.1037//0022-3514.58.3.519. [DOI] [PubMed] [Google Scholar]
- Moulds ML, Kandris E, Starr S, Wong ACM. The relationship between rumination, avoidance and depression in a non-clinical sample. Behaviour Research and Therapy. 2007;45:251–261. doi: 10.1016/j.brat.2006.03.003. [DOI] [PubMed] [Google Scholar]
- Muris P, Roelefs J, Rassin E, Franken I, Mayer B. Mediating effects of rumination and worry on the links between neuroticism, anxiety and depression. Personality and Individual Differences. 2005;39:1105–1111. [Google Scholar]
- Nolen-Hoeksema S. Responses to depression and their effects on the duration of depressive episodes. Journal of Abnormal Psychology. 1991;100:569–582. doi: 10.1037//0021-843x.100.4.569. [DOI] [PubMed] [Google Scholar]
- Nolen-Hoeksema S, Morrow J. A prospective study of depression and posttraumatic stress symptoms after a natural disaster: The 1989 Loma Prieta earthquake. Journal of Personality and Social Psychology. 1991;6:115–121. doi: 10.1037//0022-3514.61.1.115. [DOI] [PubMed] [Google Scholar]
- Nolen-Hoeksema S, Morrow J, Fredrickson BL. Response styles and the duration of episodes of depressed mood. Journal of Abnormal Psychology. 1993;102:20–28. doi: 10.1037//0021-843x.102.1.20. [DOI] [PubMed] [Google Scholar]
- Nolen-Hoeksema S, Wisco BE, Lyubomirsky S. Rethinking rumination. Perspectives on Psychological Science. 2008;3:400–424. doi: 10.1111/j.1745-6924.2008.00088.x. [DOI] [PubMed] [Google Scholar]
- Oathes DJ, Siegle GJ, Ray WJ. Chronic worry and the temporal dynamics of emotional processing. Emotion. 2011;11:101–114. doi: 10.1037/a0021781. [DOI] [PubMed] [Google Scholar]
- Papageorgiou C. Worry and rumination: Styles of persistent negative thinking in anxiety and depression. In: Davey GCL, Wells A, editors. Worry and its psychological disorders: Theory, assessment and treatment. Hoboken, NJ: Wiley Publishing; 2006. pp. 21–40. [Google Scholar]
- Paulesu E, Sambugaro E, Torti T, Danelli L, Ferri F, Scialfa G, Sassaroli S. Neural correlates of worry in generalized anxiety disorder and in normal controls: A functional MRI study. Psychological Medicine. 2010;40:117–124. doi: 10.1017/S0033291709005649. [DOI] [PubMed] [Google Scholar]
- Roberts JE, Gilboa E, Gotlib IH. Ruminative response style and vulnerability to episodes of dysphoria: Gender, neuroticism, and episode duration. Cognitive Therapy and Research. 1998;22:401–423. [Google Scholar]
- Roy M, Neale MC, Pedersen NL, Mathé AA. A twin study of generalized anxiety disorder and major depression. Psychological Medicine. 1995;25:1037–1049. doi: 10.1017/s0033291700037533. [DOI] [PubMed] [Google Scholar]
- Ruscio AM, Borkovec TD. Experience and appraisal of worry among high worriers with and without generalized anxiety disorder. Behaviour Research and Therapy. 2004;42:1469–1482. doi: 10.1016/j.brat.2003.10.007. [DOI] [PubMed] [Google Scholar]
- Ruscio AM, Holohan DR. Applying empirically supported treatments to complex cases: Ethical, empirical, and practical considerations. Clinical Psychology: Science and Practice. 2006;13:146–162. [Google Scholar]
- Sanislow CA, Pine DS, Quinn KJ, Kozak MJ, Garvey MA, Heinssen RK, Cuthbert BN. Developing constructs for psychopathology research: Research domain criteria. Journal of Abnormal Psychology. 2010;119:631–639. doi: 10.1037/a0020909. [DOI] [PubMed] [Google Scholar]
- Segerstrom S, Tsao JC, Alden LE, Craske MG. Worry and rumination: Repetitive thought as a concomitant and predictor of negative mood. Cognitive Therapy and Research. 2000;24:671–688. [Google Scholar]
- Seitchik AE, Raposa E, Weisbrot J, Ruscio AM. Problem-solving beliefs and standards among worriers; Paper presented at the annual meeting of the Association for Behavioral and Cognitive Therapies; Philadelphia, PA. 2007. Nov, [Google Scholar]
- Shear MK, Bilt JV, Rucci P, Endicott J, Lydiard B, Otto MW, Frank DM. Reliability and validity of a structured interview guide for the Hamilton Anxiety Rating Scale (SIGH-A) Depression and Anxiety. 2001;13:166–178. [PubMed] [Google Scholar]
- Spielberger CD, Gorsuch RL, Lushene RE. Manual for the State-Trait Anxiety Inventory. Palo Alto, CA: Consulting Psychologist Press; 1983. [Google Scholar]
- Starcevic V. Pathological worry in major depression: A preliminary report. Behaviour Research and Therapy. 1995;33:55–56. doi: 10.1016/0005-7967(93)e0028-4. [DOI] [PubMed] [Google Scholar]
- Stokes C, Hirsch CR. Engaging in imagery versus verbal processing of worry: Impact on negative intrusions in high worriers. Behaviour Research and Therapy. 2010;48:418–423. doi: 10.1016/j.brat.2009.12.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Szabo M, Lovibond PF. The cognitive content of naturally occurring worry episodes. Cognitive Therapy and Research. 2002;26:167–177. [Google Scholar]
- Thomsen DK. The association between rumination and negative affect: A review. Cognition and Emotion. 2006;20:1216–1235. [Google Scholar]
- Trapnell PD, Campbell JD. Private self-consciousness and the five-factor model of personality: Distinguishing rumination from reflection. Journal of Personality and Social Psychology. 1999;76:284–304. doi: 10.1037//0022-3514.76.2.284. [DOI] [PubMed] [Google Scholar]
- Treynor W, Gonzalez R, Nolen-Hoeksema S. Rumination reconsidered: A psychometric analysis. Cognitive Therapy and Research. 2003;27:247–259. [Google Scholar]
- Verkuil B, Brosschot JF, Thayer JF. Capturing worry in daily life: Are trait questionnaires sufficient? Behaviour Research and Therapy. 2007;45:1835–1844. doi: 10.1016/j.brat.2007.02.004. [DOI] [PubMed] [Google Scholar]
- Watkins E. Constructive and unconstructive repetitive thought. Psychological Bulletin. 2008;134:163–206. doi: 10.1037/0033-2909.134.2.163. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Watkins E, Moulds M, Mackintosh B. Comparisons between rumination and worry in a non-clinical population. Behaviour Research and Therapy. 2005;43:1577–1585. doi: 10.1016/j.brat.2004.11.008. [DOI] [PubMed] [Google Scholar]
- Watkins E, Scott J, Wingrove J, Rimes K, Bathurst N, Steiner H, Malliaris Y. Rumination-focused cognitive behaviour therapy for residual depression: a case series. Behaviour Research and Therapy. 2007;45:2144–2154. doi: 10.1016/j.brat.2006.09.018. [DOI] [PubMed] [Google Scholar]
- Watson D. Rethinking the mood and anxiety disorders: A quantitative hierarchical model for DSM-V. Journal of Abnormal Psychology. 2005;114:522–536. doi: 10.1037/0021-843X.114.4.522. [DOI] [PubMed] [Google Scholar]
- Watson D, Clark LA. Manual for the Postive and Negative Affect Schedule-Expanded Form. The University of Iowa; 1994. . [Google Scholar]
- Watson D, Clark LA, Tellegen A. Development and validation of brief measures of positive and negative affect: The PANAS scales. Journal of Personality and Social Psychology. 1988;54:1063–1070. doi: 10.1037//0022-3514.54.6.1063. [DOI] [PubMed] [Google Scholar]
- Watson D, Tellegen A. Toward a consensual structure of mood. Psychological Bulletin. 1985;98:219–235. doi: 10.1037//0033-2909.98.2.219. [DOI] [PubMed] [Google Scholar]
- Wisco BE, Nolen-Hoeksema S. Ruminative response style. In: Dobson KS, Dozois DJA, editors. Risk factors in depression. San Diego, CA: Academic Press; 2008. pp. 221–236. [Google Scholar]