Abstract
Objective
Four types of antipsychotic-induced movement disorders: tardive dyskinesia (TD), parkinsonism, akathisia and tardive dystonia, subtypes of TD (orofacial and limb truncal dyskinesia), subtypes of parkinsonism (rest tremor, rigidity, and bradykinesia), as well as a principal-factor of the movement disorders and their subtypes, were examined for association with variation in 7 candidate genes (GRIN2B, GRIN2A, HSPG2, DRD3, DRD4, HTR2C, and NQO1).
Methods
Naturalistic study of 168 white long-stay patients with chronic mental illness requiring long-term antipsychotic treatment, examined by the same rater at least two times over a 4-year period, with a mean follow-up time of 1.1 years, with validated scales for TD, parkinsonism, akathisia, and tardive dystonia. The authors genotyped 45 tag SNPs in 7 candidate genes, associated with movement disorders or schizophrenia in previous studies. Genotype and allele frequency comparisons were performed with multiple regression methods for continuous movement disorders.
Results
Various tag SNPs reached nominal significance; TD with rs1345423, rs7192557, rs1650420, as well as rs11644461; orofacial dyskinesia with rs7192557, rs1650420, as well as rs4911871; limb truncal dyskinesia with rs1345423, rs7192557, rs1650420, as well as rs11866328; bradykinesia with rs2192970; akathisia with rs324035; and the principal-factor with rs10772715. After controlling for multiple testing, no significant results remained.
Conclusions
The findings suggest that selected tag SNPs are not associated with a susceptibility to movement disorders. However, as the sample size was small and previous studies show inconsistent results, definite conclusions cannot be made. Replication is needed in larger study samples, preferably in longitudinal studies which take the fluctuating course of movement disorders and gene-environment interactions into account.
Introduction
Soon after the introduction of antipsychotic medication in 1952, movement disorders emerged as a complication of treatment. To date, they remain a major concern in antipsychotic treatment. Of the different movement disorders, tardive dyskinesia (TD) is the most extensively investigated. TD and other movement disorders are associated with social stigmatization, physical disabilities and poorer quality of life. In addition, they play a role in non-compliance and, therefore, risk of psychotic relapse [1]–[3].
A central problem in the management of movement disorders is the lack of clear genetic and non-genetic risk factors that would allow for early identification and prevention. It would be helpful if movement disorders could be predicted from a minimal number of genetic susceptibility loci in candidate genes in combination with demographic, clinical or pharmacological data. In order to identify individuals at risk, pharmacogenetic studies of genetic factors that contribute to interpersonal differences in susceptibility for medication-related adverse effects are needed [4]. Family studies suggest an important genetic component to the risk for movement disorders [4]–[9]. A recent meta-analysis on the prevalence of dyskinesia and parkinsonism reported spontaneous dyskinesia and parkinsonism in antipsychotic naïve patients with schizophrenia, and a higher prevalence of dyskinesia and parkinsonism in healthy family members of patients with schizophrenia, compared to matched controls [10].
Antipsychotic-induced movement disorders [11], [12] can be classified as acute or tardive. Acute syndromes appear within hours/days or weeks after starting antipsychotics or increasing the dosage (or cessation of anticholinergics). Examples of these are parkinsonism and akathisia. Tardive syndromes develop after months or years of treatment with antipsychotics, examples being TD and tardive dystonia. Initially, the term ‘tardive’ (delayed) was introduced to emphasize the late-onset types of movement disorders occurring during antipsychotic use. Yet the definition of tardive disorders in the current study emphasizes their persistence, which is clinically more important than their late-onset [12], [13]. Given that combinations of acute and chronic movement disorders occur in patients undergoing long-term treatment with antipsychotics, prediction models should include both syndromes, i.e., the four major types of movement disorders (TD, parkinsonism, akathisia and tardive dystonia). It is noteworthy that movement disorders may fulfill the criteria for classifying a trait as a spectrum condition of a disorder, in this case schizophrenia: heritability, familial link, co-segregation, and biological and clinical plausibility [14]. Spectrum conditions refer to mild psychopathology of little clinical significance among relatives without the full disorder. The advantage for research of spectrum conditions in contrast to a full disorder is that they may have fewer risk factors and therefore a less complex chain of mechanisms (pathways) leading to their onset, which could make research easier to perform. (Pharmaco) genetic studies may help elucidate these common pathways in the development of both spectrum conditions and the full disorder. It is possible to hypothesize that specific subtypes of movement disorders are more suitable for genetic analysis than a general movement disorder syndrome, as subtypes may better reflect the underlying biological heterogeneity in complex syndromes.
The phenotypes under study were TD, parkinsonism, akathisia, and tardive dystonia, subtypes of TD (orofacial and limb truncal dyskinesia), subtypes of parkinsonism (rest tremor, rigidity, and bradykinesia), as well as a principal-factor of the movement disorders and their subtypes.
The 7 candidate genes were GRIN2B, GRIN2A, HSPG2, DRD3, DRD4, HTR2C, and NQO1 (Text S1). The choice of these genes was hypothesis-driven, under the common disease/common variant (CDCV) hypothesis, which proposes that common diseases may be caused by common genetic variants [15]–[18].
The aim of the current study was to determine the association between movement disorders and variations in these 7 candidate genes.
The prospective design of the current study extends hitherto cross-sectional work in the pharmacogenetic field of antipsychotic-induced movement disorders. Indeed, prospective assessment of fluctuating (repeated) movement disorders measures the phenotype more specifically and that increases the validity of the associations between movement disorders and risk factors.
Methods
Ethics Statement
The protocol was approved by the standing Institutional Review Board, ‘Medisch-ethische Toetsingscommissie Instellingen Geestelijke Gezondheidszorg’ (Review Board for Human Research in Psychiatry), the Netherlands [protocol number 377].
Written informed consent was obtained from each patient, hence, consent obtained from the next of kin was not necessary and not recommended by the Review Board for Human Research in Psychiatry.
Subjects
A 4-year prospective naturalistic study (July 2003– May 2007) was conducted with 209 patients with chronic mental illness in order to determine the genetic risk factors of the four major types of movement disorders (TD, parkinsonism, akathisia, and tardive dystonia), subtypes of TD and parkinsonism, as well as a principal-factor of the movement disorders and their subtypes. To this end, a cohort was drawn from a general psychiatric hospital (GGZ Centraal, Amersfoort, the Netherlands). Full details of the study design and movement disorders have been published previously [19] (Bakker and colleagues, submitted). The cohort was representative of the population of patients with the most severe chronic mental illness requiring long-stay care, given that the hospital serves an epidemiological catchment area, is the only institute providing this type of care in this area, and patients were selected from a comprehensive list of all inpatients.
Of the patients assessed at baseline (N = 207) 93.7% (n = 194) had at least one follow-up and 59.4% (n = 123) had two follow-up assessments. Loss to follow-up was due to patients who were difficult to trace after leaving hospital, died or refused assessment after inclusion.
Assessment
Patients were examined by a trained psychiatrist (PRB), using a standard protocol, described by van Harten and colleagues [20]. In addition, subtypes of movement disorders were assessed using (i) the Abnormal Involuntary Movement Scale (AIMS) [21], [22] with items 1–4 for orofacial and items 5–7 for limb truncal dyskinesia, (ii) the Unified Parkinson Disease Rating Scale (UPDRS) [23] with item c3–c4 for ‘rest tremor’ (rest tremor, and action/postural tremor of hands); item c5 for rigidity; and items c1, c2, c6–c12, and c14 for bradykinesia. This approach has been described previously by 3 members of our research team (AAH, JvO and PNvH) [24]–[26].
As movement disorders likely share genetic liability, a genetic association between the combined movement disorders and candidate genes is also required. To determine the association between the combined movement disorders and variation in 7 candidate genes, a principal-factor of the four major types of movement disorders and subtypes of TD and parkinsonism was calculated with the FACTOR procedure in the STATA statistical program [27].
Based on the literature published between 1976 and July 2012, we selected 7 candidate genes (Tables 1 and S1, and Text S1) that are involved in the dopaminergic and serotonergic systems, and protection of neurotoxicity, and we included the gene coding for heparan sulfate proteoglycan 2, all which have been implicated in the development of movement disorders.
Table 1. Selected 45 tag SNPs for multilevel regression of continuous movement disorders.
| Gene | Tag SNP | Chromosome Position | Alleles Public | ReferencesSNPs/Genes | TDa | PKa | AKa | TDta | PFa | |||||
| Major/Minor | Demonstratedassociations | Beta | p-value | Beta | p-value | Beta | p-value | Beta | p-value | Beta | p-value | |||
| GRIN2B | chr12∶13,714,410–14,133,022 | |||||||||||||
| rs1805481 | chr12∶13,763,205–13,763,705 | AC | −0.03 | 0.6062 | 0.05 | 0.3529 | −0.04 | 0.5621 | −0.02 | 0.2882 | 0.08 | 0.4914 | ||
| rs7313149 | chr12∶13,828,037–13,828,537 | TC | 0.02 | 0.7816 | 0.03 | 0.5460 | −0.01 | 0.8739 | 0.00 | 0.9931 | 0.02 | 0.8586 | ||
| rs2192970 | chr12∶13,836,063–13,836,563 | CT | −0.12 | 0.1007 | −0.07 | 0.2263 | 0.04 | 0.6385 | 0.00 | 0.7915 | −0.14 | 0.2406 | ||
| rs2300242 | chr12∶13,840,047–13,840,547 | TA | 0.01 | 0.9097 | 0.05 | 0.3792 | 0.01 | 0.9256 | −0.01 | 0.4171 | 0.12 | 0.2904 | ||
| rs10845838 | chr12∶13,894,146–13,894,646 | GA | 0.06 | 0.4429 | −0.01 | 0.8834 | −0.11 | 0.1218 | −0.02 | 0.1964 | 0.08 | 0.4910 | ||
| rs12300851 | chr12∶13,968,155–13,968,655 | TC | – | – | – | – | – | – | – | – | – | – | ||
| rs220599 | chr12∶13,975,048–13,975,548 | GA | −0.02 | 0.7367 | 0.04 | 0.4773 | −0.01 | 0.8670 | −0.01 | 0.4562 | 0.07 | 0.5170 | ||
| rs10772715 | chr12∶14,037,753–14,038,253 | GA | −0.10 | 0.1086 | −0.07 | 0.1479 | −0.02 | 0.7624 | −0.01 | 0.3444 | −0.20 | 0.0362 | ||
| rs12827536 | chr12∶14,095,907–14,096,407 | CT | −0.04 | 0.4927 | 0.02 | 0.6875 | −0.02 | 0.7378 | −0.01 | 0.4348 | −0.04 | 0.7222 | ||
| GRIN2A | chr16∶9,847,265–10,276,263 | |||||||||||||
| rs11866328 | chr16∶9,862,306–9,862,806 | GT | 0.12 | 0.0512 | −0.02 | 0.7185 | 0.04 | 0.4868 | 0.02 | 0.2581 | −0.02 | 0.8312 | ||
| rs11646587 | chr16∶9,873,069–9,873,569 | GA | −0.03 | 0.6401 | −0.06 | 0.3363 | 0.02 | 0.7751 | −0.02 | 0.2945 | −0.11 | 0.3275 | ||
| rs7196095 | chr16∶9,885,582–9,886,082 | TC | 0.02 | 0.7279 | −0.02 | 0.7082 | 0.09 | 0.1678 | −0.01 | 0.6353 | −0.03 | 0.8048 | ||
| rs8049651 | chr16∶9,943,416–9,943,916 | CT | 0.05 | 0.4769 | 0.02 | 0.7706 | 0.01 | 0.9313 | −0.00 | 0.8313 | 0.08 | 0.4938 | ||
| rs9989388 | chr16∶9,965,889–9,966,389 | CT | −0.03 | 0.6765 | 0.08 | 0.2289 | 0.02 | 0.7748 | −0.00 | 0.7958 | 0.14 | 0.2764 | ||
| rs9921541 | chr16∶9,991,512–9,992,012 | GT | −0.04 | 0.6482 | 0.03 | 0.6181 | 0.01 | 0.8932 | −0.01 | 0.4727 | 0.07 | 0.5684 | ||
| rs4782039 | chr16∶10,006,717–10,007,217 | TC | −0.01 | 0.8343 | 0.01 | 0.9205 | 0.04 | 0.6066 | 0.00 | 0.8070 | 0.10 | 0.3853 | ||
| rs7190619 | chr16∶10,078,874–10,079,374 | GA | −0.01 | 0.9154 | 0.01 | 0.9256 | −0.10 | 0.2778 | 0.02 | 0.3586 | −0.08 | 0.5903 | ||
| rs9788936 | chr16∶10,105,210–10,105,710 | TC | 0.05 | 0.5014 | −0.03 | 0.6344 | 0.04 | 0.6484 | 0.01 | 0.7426 | 0.01 | 0.9558 | ||
| rs8057394 | chr16∶10,115,238–10,115,738 | GC | 0.14 | 0.0525 | 0.04 | 0.4506 | 0.00 | 0.9916 | 0.01 | 0.3378 | 0.07 | 0.5246 | ||
| rs11644461 | chr16∶10,120,640–10,121,140 | TC | −0.13 | 0.0385 | −0.02 | 0.6424 | 0.08 | 0.2276 | −0.02 | 0.2136 | −0.11 | 0.2730 | ||
| rs7192557 | chr16∶10,123,219–10,123,719 | GA | 0.22 | 0.0159 | 0.08 | 0.2742 | 0.11 | 0.2443 | 0.00 | 0.9604 | 0.20 | 0.1877 | ||
| rs7206256 | chr16∶10,196,673–10,197,173 | AG | 0.02 | 0.7845 | 0.02 | 0.7595 | −0.00 | 0.9896 | 0.02 | 0.0919 | 0.00 | 0.9922 | ||
| rs1345423 | chr16∶10,247,814–10,248,314 | TG | −0.13 | 0.0421 | 0.01 | 0.8026 | 0.06 | 0.3536 | −0.02 | 0.1442 | −0.04 | 0.6942 | ||
| rs1650420 | chr16∶10,268,080–10,268,580 | GA | 0.16 | 0.0193 | −0.04 | 0.4499 | −0.07 | 0.2912 | 0.02 | 0.1066 | 0.05 | 0.6514 | ||
| HSPG2 | chr1∶22,148,737–22,263,750 | |||||||||||||
| rs2270697 | chr1∶22,167,738–22,168,238 | GT | 0.01 | 0.9194 | −0.05 | 0.4670 | −0.01 | 0.8797 | 0.01 | 0.5993 | −0.14 | 0.2999 | ||
| rs2445142 | chr1∶22,225,493–22,225,993 | GC | [28]–[30] | −0.05 | 0.4292 | 0.08 | 0.1685 | 0.06 | 0.4036 | 0.01 | 0.6816 | 0.19 | 0.0998 | |
| rs6698486 | chr1∶22,243,773–22,244,273 | CT | −0.10 | 0.2250 | 0.12 | 0.0760 | −0.02 | 0.8130 | −0.00 | 0.8494 | 0.25 | 0.0625 | ||
| DRD3 | chr3∶113,847,557–113,897,899 | [25], [31]–[38] | ||||||||||||
| rs9817063 | chr3∶113,846,858–113,847,358 | TC | −0.02 | 0.8083 | −0.04 | 0.4632 | −0.04 | 0.5922 | 0.02 | 0.2359 | −0.01 | 0.9440 | ||
| rs2134655 | chr3∶113,857,951–113,858,451 | GA | 0.02 | 0.7265 | −0.05 | 0.4003 | 0.11 | 0.1409 | 0.03 | 0.0664 | 0.02 | 0.8868 | ||
| rs963468 | chr3∶113,862,637–113,863,137 | GA | −0.04 | 0.5906 | 0.03 | 0.5874 | 0.08 | 0.2021 | −0.01 | 0.5302 | −0.03 | 0.8098 | ||
| rs324035 | chr3∶113,868,604–113,869,104 | CA | 0.00 | 0.9949 | 0.01 | 0.9005 | −0.20 | 0.0392 | −0.00 | 0.9592 | 0.12 | 0.4326 | ||
| rs3773678 | chr3∶113,869,828–113,870,328 | CT | −0.06 | 0.5968 | 0.05 | 0.5761 | −0.21 | 0.0805 | 0.03 | 0.2130 | 0.18 | 0.3661 | ||
| rs167771 | chr3∶113,876,025–113,876,525 | AG | −0.06 | 0.5606 | 0.06 | 0.4746 | −0.19 | 0.0512 | 0.00 | 0.9197 | 0.19 | 0.2265 | ||
| rs11721264 | chr3∶113,879,154–113,879,654 | GA | 0.05 | 0.4688 | −0.01 | 0.8877 | −0.08 | 0.1930 | −0.01 | 0.5338 | −0.08 | 0.4382 | ||
| rs167770 | chr3∶113,879,312–113,879,812 | AG | [39] | 0.05 | 0.3807 | 0.00 | 0.9367 | −0.07 | 0.2411 | −0.01 | 0.4278 | −0.07 | 0.4798 | |
| rs7633291 | chr3∶113,886,818–113,887,318 | TG | [39] | 0.05 | 0.4719 | 0.00 | 0.9958 | −0.05 | 0.5264 | −0.02 | 0.1561 | −0.08 | 0.4902 | |
| rs1800828 | chr3∶113,891,299–113,891,799 | GC | 0.01 | 0.8492 | 0.02 | 0.7948 | −0.09 | 0.2275 | −0.02 | 0.1701 | 0.02 | 0.8882 | ||
| DRD4 | chr11∶637,305–640,705 | [40], [41] | ||||||||||||
| rs3758653 | chr11∶636,149–636,649 | TC | [42] | −0.02 | 0.7043 | −0.02 | 0.6344 | −0.01 | 0.8712 | 0.00 | 0.6300 | −0.08 | 0.2617 | |
| HTR2C | chrX:113,818,551–114,144,624 | [25], [33], [35], [43]–[46] | ||||||||||||
| rs569959 | chrX:113,820,110–113,820,610 | AG | 0.01 | 0.8501 | 0.06 | 0.1606 | −0.01 | 0.8138 | −0.00 | 0.7311 | 0.11 | 0.1994 | ||
| rs17326429 | chrX:113,826,117–113,826,617 | GA | −0.07 | 0.3678 | 0.06 | 0.3194 | −0.03 | 0.6436 | −0.00 | 0.7743 | 0.14 | 0.2247 | ||
| rs12858300 | chrX:113,897,163–113,897,663 | GC | −0.03 | 0.6927 | −0.10 | 0.1548 | 0.03 | 0.7543 | −0.01 | 0.6958 | −0.15 | 0.2892 | ||
| rs4911871 | chrX:113,996,890–113,997,390 | AG | −0.12 | 0.0634 | 0.02 | 0.7622 | −0.06 | 0.3938 | −0.01 | 0.6267 | 0.12 | 0.2648 | ||
| rs5946189 | chrX:114,071,970–114,072,470 | TC | 0.03 | 0.5470 | 0.04 | 0.4574 | −0.01 | 0.9251 | 0.02 | 0.0565 | 0.06 | 0.5314 | ||
| rs1801412 | chrX:114,142,454–114,142,954 | TG | −0.14 | 0.3456 | −0.15 | 0.2627 | −0.00 | 0.9991 | −0.00 | 0.9149 | −0.34 | 0.1571 | ||
| NQO1 | chr16∶69,743,304–69,760,533 | |||||||||||||
| rs1800566 | chr16∶69,744,895–69,745,395 | CT | [47] | −0.14 | 0.1126 | 0.01 | 0.8486 | 0.02 | 0.7939 | 0.02 | 0.3708 | −0.11 | 0.4720 |
Sources: UCSC (GRCh37/hg19), NCBI, SNPedia, Genecards, CHIP Bioinformatics Tools.
TD = tardive dyskinesia, PK = parkinsonism, AK = akathisia, TDt = tardive dystonia and PF = principal-factor.
In addition, variables possibly affecting risk were extracted from patients’ case notes (Text S1).
Gene and Tag SNP Selection, DNA Extraction, Genotyping
Two 10 ml EDTA tubes of peripheral blood were drawn from participants, and genomic DNA was extracted from leucocytes by Autopure LS method (Qiangen) according to the manufacturer’s protocols.
The tag SNPs were selected using a web-based tool freely available on the internet (SNPinfo Web Server; http://www.niehs.nih.gov/snpinfo) [48] (Text S1).
Statistical Analyses
Hardy weinberg equilibrium
Only SNPs were included in the analyses that were not significantly outside Hardy-Weinberg Equilibrium (HWE) (p>0.05) in (i) the complete control sample (for a dichotomous trait) or (ii) the complete study sample (for a continuous trait). For the six SNPs in the X-chromosomal HTR2C gene, departure from HWE was not calculated.
Departure from the HWE was calculated with the GENASS and GENHW procedures in the STATA statistical program [27] for (i) the dichotomously defined persistent forms of movement disorders separately in both patients (with one movement disorder) and controls (without that movement disorder). Case definition of a persistent movement disorder was based on 2 consecutive assessments over a period of minimally 3 months, and required that individuals met case definition criteria at two consecutive assessments (hereafter: persistent movement disorder), meeting the requirements of Schooler and Kane’s criteria for persistent movement disorder [49], and (ii) the combined group of patients and controls, as continuous measures cannot be separated in both patients and controls.
Association tests for single tag SNPs
Only continuous movement disorder outcomes were used, given that continuous measures better handle the variability of movement disorders and generate more statistical power than cut off points [50], [51]. Genotype and allele frequency comparisons were performed with multiple regression methods for continuous movement disorders, using the Armitage trend test, with the major allele (from our dataset of 168 selected white patients) as reference. The Armitage trend test assumes an additive effect by both alleles on the trait of interest, i.e. the mean effect on the trait by the heterozygous genotype (Major-Minor) is halfway the effects of the two homozygotes. (Major-Major and Minor-Minor).
Regression analyses
The regression analyses were conducted with movement disorder measures at a single assessment (hereafter: fluctuating movement disorder). The reason for this was that movement disorders constantly fluctuate over time, so that inclusion in the regression of their repeated single-occasion measures allowed for calculation of associations between one movement disorder with the other over time. As the study design comprised repeated measures nested in the same patient, clustering of observations in individuals needed to be corrected for. Therefore, multilevel random regression was used with the measurement occasion (baseline and two follow-ups) at level 1, and subjects at level 2, with the XTREG MLE routine of the STATA statistical program [27]. Associations with explanatory variables were expressed as beta coefficients representing the change of continuous movement disorder outcome with 1 unit change of the exposure variable.
Using the dataset of 168 selected white patients, associations with predictors were adjusted for a priori, movement-disorder specific covariates as follows (Bakker and colleagues, submitted) age was adjusted for in the model of TD and its subtypes; age and total antipsychotic use was adjusted for in the model of parkinsonism and its subtypes, and no covariates were introduced in the models of akathisia, tardive dystonia and the principal-factor.
Power calculations were performed using the Quanto program version 1.2.4 (http://hydra.usc.edu/gxe).
Correction for multiple testing
In order to correct for multiple testing of single SNP tests, the Simes modification of the Bonferroni multiple-testing procedure was performed to control the False Discovery Rate (FDR) [52]. Bonferroni correction is too conservative if tests are not independent of each other; in this case FDR represents a less conservative alternative. We used the MULTPROC procedure in the STATA statistical program [27] for FDR calculation, and then the SMILEPLOT procedure calling MULTPROC to build a smile plot. A smile plot summarizes a set of multiple analyses, similarly as a Cochrane forest plot summarizes a meta-analysis, and separates by reference line rejected and non-rejected p-values (on a reverse log scale against the corresponding parameter estimates).
Defined daily dose
Antipsychotic doses were converted to defined daily dose (DDD), for which we refer to our previous publication [19]. Anticholinergic medication was modeled as a dichotomous variable (yes/no).
Results
Sample Characteristics
Over the period of observation (mean = 1.1 years, SD = 0.64), of the 209 patients included at baseline, 207 participated in the study. One patient developed a brain tumor, another patient died after inclusion. All patients had a history of cumulative antipsychotic intake of minimally 1 year. Attrition rate was low at 9.8% over a 4-year period.
Of the 207 patients, with chronic psychiatric illness requiring long-term admission, 199 participated in the genetic study. To prevent ethnic stratification resulting in spurious associations owing to differences in allele frequencies and risk of movement disorders, only white patients, representing the most prevalent group (168 = 84.4%), were included in the analysis. At baseline, mean age expressed in years was 48.8 (SD 12.4); men 48.6 (SD 12.5) and women 49.1 (SD 12.2). Age at first admission, expressed in years, was 25.1 (SD 8.8); men 23.7 (SD 7.8) and women 27.1 (SD 9.7). The total duration of admission, expressed in years, was 23.4 (SD 12.9), men 24.4 (SD 12.5) and women 22.0 (SD 13.4). Diagnoses according to DSM-IV Axis I as defined above were: schizophrenia 112 (66.7%), psychosis 9 (5.4%), affective disorder 27 (16.1%), other Axis I diagnosis 11 (6.6%) and no Axis I diagnosis 9 (5.4%).
Association Analyses with Tag SNPs
The following SNPs were excluded from analysis, due to deviation from HWE: all movement disorders – rs6698486, rs11721264, rs167770, rs3758653 and rs1800566, as well as controls, TD – rs10845838, rs7206256 and rs7633291; orofacial dyskinesia – rs10845838 and rs2445142; limb truncal dyskinesia – rs7633291; parkinsonism, rest tremor and bradykinesia – rs2445142. In addition, rs12300851 was removed as it contained only A alleles.
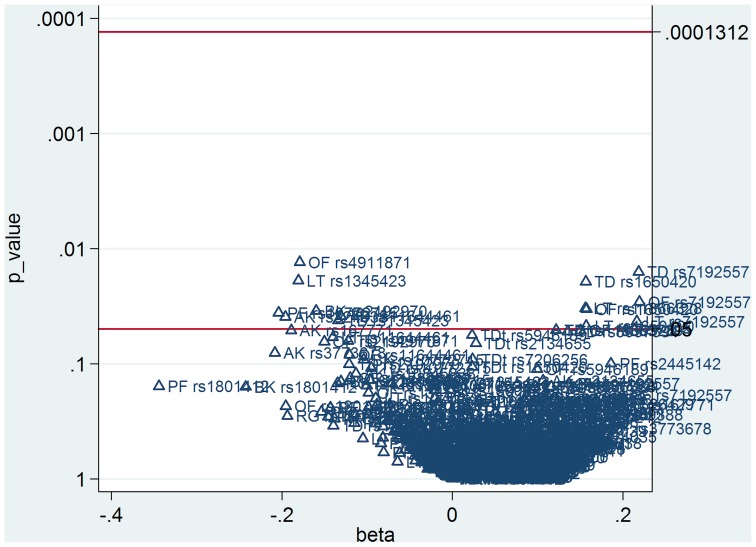
The (multilevel) regression yielded significant coefficients, after adjustment for age, between TD and rs1345423 (B = −0.13, p = 0.0421), rs7192557 (B = 0.22, p = 0.0159), rs1650420 (B = 0.16, p = 0.0193), as well as rs11644461 (B = −0.13, p = 0.0385); between orofacial dyskinesia and rs7192557 (B = 0.22, p = 0.0291), rs1650420 (B = 0.16, p = 0.0336), as well as rs4911871 (B = −0.18, p = 0.0131); between limb truncal dyskinesia and rs1345423 (B = −0.18, p = 0.0190), rs7192557 (B = 0.22, p = 0.0430), rs1650420 (B = 0.16, p = 0.0471), as well as rs11866328 (B = 0.16, p = 0.0330). After adjustment for age and total DDD equivalents, associations were apparent between bradykinesia and rs2192970 (B = −0.16, p = 0.0349). Without adjustment, associations were apparent between akathisia and rs324035 (B = −0.20, p = 0.0392), as well as the principal-factor and rs10772715 (B = −0.20, p = 0.0362). After Simes correction for multiple testing of the above mentioned analyses, the number of rejected p-values was zero, with a corrected overall critical p-value of 0.00013 (Figure 1).
Figure 1. Smile plot summarizing set of multiple analyses after Simes correction for multiple testing of tag SNPs without HWE deviation.
Corresponding p-values (on a reverse log scale against the corresponding parameter estimates). TD = tardive dyskinesia, OF = orofacial dyskinesia, LT = limb truncal dyskinesia, PK = parkinsonism, RT = rest tremor, RG = rigidity, BK = bradykinesia, AK = akathisia,TDt = tardive dystonia.
Power calculations showed that our sample was insufficiently powered (0.05) to identify the betas from our regressions, which were between −0.34 and 0.25.
Discussion
In a population with chronic mental illness, various tag SNPs in 7 candidate genes (GRIN2B, GRIN2A, HSPG2, DRD3, DRD4, HTR2C, and NQO1) reached nominally significant (p≤0.05) associations with drug-induced movement disorders. However, after controlling for multiple testing, our findings suggest that these tag SNPs are not associated with a susceptibility to movement disorders.
Another reason for the inconclusive findings could be explained by the fact that in a naturalistic setting it is possible to evaluate the overall impact of pharmacogenetic signals in the presence of a host of real-life variables that can override pharmacogenetic variation. The fact we did not observe a significant association may also attest to the possibility that each gene makes a small contribution that is often diluted or overridden by environmental and clinical variations.
Limitations
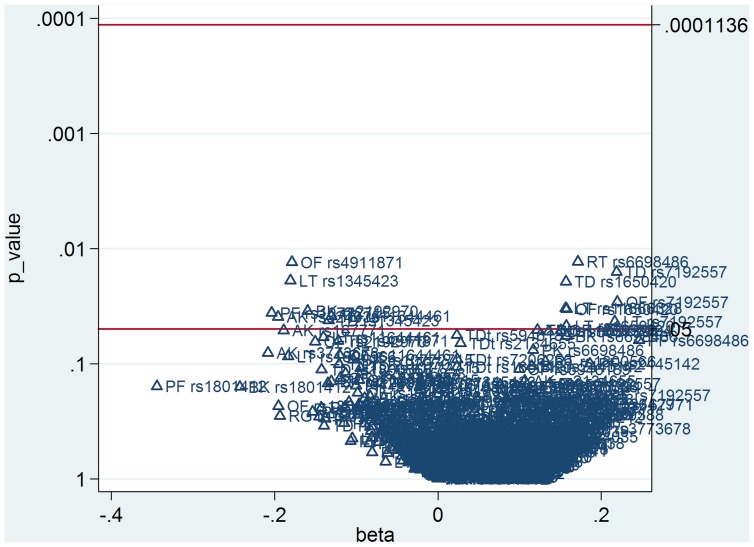
This study had limitations, for which we refer to our previous publications [19], [53] (Bakker and colleagues, submitted) as well point to additional limitations. First, some authors may argue that the SNPs with HWE deviation should not be excluded from the analyses, as SNPs in HWE could in reality be also out of HWE owing to lack of power. Therefore, we performed a post-hoc analysis with all SNPs, i.e., also those deviating from HWE, which resulted in one extra nominal significant result, which also did not survive Simes correction for multiple testing (Figure 2). Second, the choice to genotype tag SNPs in the candidate genes, and not only the specific SNPs that were previously associated with movement disorders, increased the multiple testing burden. However, tag SNPs are a relatively small set of common polymorphisms [54] in the candidate genes providing maximum information; therefore, they may reveal new (unknown) SNPs in linkage disequilibrium related to movement disorders. Third, the inclusion of patients with various psychiatric illnesses, not only schizophrenia, may result in spurious associations.
Figure 2. Smile plot summarizing set of multiple analyses after Simes correction for multiple testing of all tag SNPs.
Corresponding p-values (on a reverse log scale against the corresponding parameter estimates). TD = tardive dyskinesia, OF = orofacial dyskinesia, LT = limb truncal dyskinesia, PK = parkinsonism, RT = rest tremor, RG = rigidity, BK = bradykinesia, AK = akathisia,TDt = tardive dystonia.
Strengths
We refer to our previous publications [19], [53] (Bakker and colleagues, submitted). The importance of repeated measures should be noted, as case definition of repeated measures, rather than a single cross-sectional measure, for continuous movement disorders better reflects the continuously fluctuating nature in time of both acute and chronic movement disorders, and therefore may represent a more suitable standard in future research. To the best of our knowledge only few papers in the literature address this issue.
As the sample size of the current study is small and previous studies show inconsistent results, definite conclusions cannot be made. Yet the question is how to interpret these results. In our opinion, the findings of weak genetic signals need to be replicated in larger study samples, preferably in longitudinal studies which take the fluctuating course of movement disorders and gene-environment interactions into account [55], [56].
Even though the current study is inconclusive, the importance of negative findings should not be underestimated as they can inform future meta-analysis, which otherwise might be biased by excess significance bias occasioned by selection of positive studies for publication. The pioneering meta-analyses of Lerer and colleagues [31], [57] showed that with meta-analysis, synthesis of association studies for TD can be accomplished; it was shown that small effects may point to the involvement of other genes in the development of TD. In recent years, genome-wide association studies (GWASs) revealed several SNPs related to movement disorders including tardive dyskinesia [29], [30], [58], [59] and parkinsonism [60], [61]. We further refer to our previous publication [53].
All in all, it seems legitimate to conclude that future research projects into antipsychotic-induced movement disorders may take advantage of a new perspective on common pathways of movement disorders. Directed acyclic graphs (DAGs, also known as “causal diagrams” or “causal pathways”) allow pathways to be visualized by analytical graphs and conceptualize the relationships between all of the important variables (e.g., schizophrenia, movement disorder, antipsychotics, genes, etc.) as a precise theoretical model. DAGs depict explicitly, in an easy and flexible way, confounding effects (“backdoor paths”) and collider effects (two causal pathways). The latter is important as adjusting for colliders creates confounding [62] (p161) [63] (p183). Rothman’s sufficient-component cause model (or sufficient-cause model) permits the postulation of different sufficient causes comprising a collection of collaborating risk factors (also known as “causal components”) “sufficient to produce the disease in the individual” [63] (p8). This model can also identify proximal (biological markers of risk), intermediate, and distal sufficient causes, hence describing a chain of causality [62] (p379).
The sufficient-component cause model shows that risk factors in complex diseases plausibly interact non-additively, since these risk factors may be neither necessary nor sufficient to produce disease, and frequently co-participate in similar pathways [63] (p81) [64], [65]. Although in psychiatry there is great interest in these interactions (gene-environment, environment-environment and gene-gene), concerns are being raised about the correct underlying interaction model (additive versus multiplicative), as are doubts about the recent interpretation of pathogenesis increasingly identified in a growing number of interaction studies [66].
New research designs to help understand gene-environment causality are in progress. For example, contrary to between-subject cross-sectional designs, longitudinal within-subject (longitudinal and multilevel) designs with repeated assessments [67] are being implemented. They have the advantage of being free of between-subject confounding [68], may reveal the dynamics of behavior (movements), and therefore elucidate gene-environment causality. Of importance are the so called momentary assessment tools [69], examples being the Experience Sampling Method (ESM) by Csikszentmihalyi and Larson [70] and ‘PsyMate’ by Myin-Germeys [71].
In addition, future research may be served by data-intensive science that concentrates on sharing and integrating selected data sets [72]. As rightly stated by Chalise and colleagues [73], new sets of integrative genomic approach, i.e., the collection of different types of genomic data, do more justice to the complexity of drug-related phenotypes, than most of the existing “naïve one-at-a-time analysis approach” which overlooks this complexity. Important initiatives are (i) the EUropean network of national schizophrenia networks studying Gene-Environment Interactions (EU-GEI, www.eu-gei.eu) and (ii) the Network of Investigator Networks sponsored by the global Human Genome Epidemiology Network (HuGENet, www.cdc.gov/genomics/hugenet) [74]. An important issue concerns the identification of significant SNPs in the genome, e.g. from genome-wide association studies (GWASs) [75].
In conclusion, the findings suggest that selected tag SNPs are not associated with a susceptibility to movement disorders. However, replication is needed in larger study samples, preferably in longitudinal studies which take the fluctuating course of movement disorders and gene-environment interactions into account. The use of intermediate phenotypes, for example, laboratory based phenotypes [76], or more accurate measures of movement disorders, for example instrument measurement of lingual force variability as proposed by Koning and colleagues [77], which may represent a powerful alternative since instrument measurement detects subclinical movement disorders and is highly reliable. Moreover, (pharmaco) genetic studies may help elucidate common pathways in the development of movement disorders. Future research on movement disorders may be served by the inclusion of all four movement disorders, as performed in the current study, since they may represent pleiotropic effects from (partly) shared genetic factors [78].
Supporting Information
Selected 45 tag SNPs for multilevel regression of continuous movement disorders (subtypes).
(DOC)
Supporting information about the 7 candidate genes.
(DOC)
Acknowledgments
The authors are very grateful for Prof. Dr. Anton Loonen (University of Groningen, Groningen, the Netherlands) for generously facilitating the genotyping analyses. The authors are also grateful for the staff of the Genome Analysis Facility of the Genetics Department of the University Medical Center Groningen (UMCG, Groningen, the Netherlands) for their kind technical assistance.
The authors are also grateful for M. Hoornweg-van Beek (MSc), G.V. Boedijn (MSc), M. van Drie (MSc), R. Emons (MSc), A.E. Willems (MSc), I.W. de Groot (MSc), L. Broer
(MSc), Saltro laboratory, hospital and outpatient pharmacies, hospital staff for providing their assistance, and to all patients for participating in this study.
Funding Statement
This work was supported by grant from the Foundation ‘the Open Ankh’, the Netherlands (grant number SG 21.02). The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
References
- 1. Casey DE (2006) Implications of the CATIE trial on treatment: extrapyramidal symptoms. CNS Spectr 11: 25–31. [DOI] [PubMed] [Google Scholar]
- 2. Lambert M, Conus P, Eide P, Mass R, Karow A, et al. (2004) Impact of present and past antipsychotic side effects on attitude toward typical antipsychotic treatment and adherence. Eur Psychiatry 19: 415–422. [DOI] [PubMed] [Google Scholar]
- 3. Robinson DG, Woerner MG, Alvir JM, Bilder RM, Hinrichsen GA, et al. (2002) Predictors of medication discontinuation by patients with first-episode schizophrenia and schizoaffective disorder. Schizophr Res 57: 209–219. [DOI] [PubMed] [Google Scholar]
- 4.Lerer B (2002) Pharmacogenetics of psychotropic drugs. Cambridge, UK: Cambridge University Press.
- 5. Halliday J, Farrington S, Macdonald S, MacEwan T, Sharkey V, et al. (2002) Nithsdale Schizophrenia Surveys 23: movement disorders. 20-year review. Br J Psychiatry 181: 422–7. [DOI] [PubMed] [Google Scholar]
- 6. McCreadie RG, Thara R, Srinivasan TN, Padmavathi R (2003) Spontaneous dyskinesia in first-degree relatives of chronically ill, never-treated people with schizophrenia. Br J Psychiatry 183: 45–49. [DOI] [PubMed] [Google Scholar]
- 7. Muller DJ, Schulze TG, Knapp M, Held T, Krauss H, et al. (2001) Familial occurrence of tardive dyskinesia. Acta Psychiatr Scand 104: 375–379. [DOI] [PubMed] [Google Scholar]
- 8. Fenton WS (2000) Prevalence of spontaneous dyskinesia in schizophrenia. J Clin Psychiatry 61 Suppl 4 10–4. [PubMed] [Google Scholar]
- 9. Lencer R, Eismann G, Kasten M, Kabakci K, Geithe V, et al. (2004) Family history of primary movement disorders as a predictor for neuroleptic-induced extrapyramidal symptoms. Br J Psychiatry 185: 465–471. [DOI] [PubMed] [Google Scholar]
- 10. Koning JP, Tenback DE, van Os J, Aleman A, Kahn RS, et al. (2010) Dyskinesia and parkinsonism in antipsychotic-naive patients with schizophrenia, first-degree relatives and healthy controls: a meta-analysis. Schizophr Bull 36: 723–731. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Owens DGC (1999) A guide to the extrapyramidal side-effects of antipsychotic drugs. New York: Cambridge University Press UK.
- 12.Factor SA, Lang AE, Weiner WJ (2005) Drug induced movement disorders. Malden, Mass: Blackwell Futura.
- 13.Sachdev PS (2005) Neuroleptic-induced movement disorders: an overview. Psychiatr Clin North Am 28: 255–74, x. [DOI] [PubMed]
- 14.Faraone SV, Tsuang MT, and Tsuang BW (1999) Genetic of mental disorders. New York: The Guilford Press.
- 15. Wellcome Trust Case Control Consortium (2007) Genome-wide association study of 14,000 cases of seven common diseases and 3,000 shared controls. Nature 447: 661–678. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Hemminki K, Forsti A, Bermejo JL (2008) The ‘common disease-common variant’ hypothesis and familial risks. PLoS ONE 3: e2504. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Reich DE, Lander ES (2001) On the allelic spectrum of human disease. Trends Genet 17: 502–510. [DOI] [PubMed] [Google Scholar]
- 18. Wang WY, Barratt BJ, Clayton DG, Todd JA (2005) Genome-wide association studies: theoretical and practical concerns. Nat Rev Genet 6: 109–118. [DOI] [PubMed] [Google Scholar]
- 19.Bakker PR, de Groot IW, van Os J, van Harten PN (2011) Long-stay psychiatric patients: a prospective study revealing persistent antipsychotic-induced movement disorder. PLoS ONE 6: e25588. 10.1371/journal.pone.0025588 [doi];PONE-D-11-04652 [pii]. [DOI] [PMC free article] [PubMed]
- 20. van Harten PN, Matroos GE, Hoek HW, Kahn RS (1996) The prevalence of tardive dystonia, tardive dyskinesia, parkinsonism and akathisia The Curacao Extrapyramidal Syndromes Study: I. Schizophr Res. 19: 195–203. [DOI] [PubMed] [Google Scholar]
- 21.Guy W (1975) ECDEU assessment manual for psychopharmacology. In: Washington DC: Department of Health, Education and Welfare. 534–537.
- 22.Guy W (1976) ECDEU assessment manual for psychopharmacology. Rockville, Md: U.S. Dept. of Health, Education, and Welfare, Public Health Service, Alcohol, Drug Abuse, and Mental Health Administration, National Institute of Mental Health, Psychopharmacology Research Branch, Division of Extramural Research Programs.
- 23.Fahn S, Elton R (1987) UPDRS Development Committee. Unified Parkinson’s Disease Rating Scale. In: Fahn S, Marsden CD, Calne DB, Goldstein M, eds. Recent Developments in Parkinson’s Disease. In: Florham Park, NJ: Macmillan. 153–163.
- 24. Al Hadithy AF, Wilffert B, Bruggeman R, Stewart RE, Brouwers JR, et al. (2009) Lack of association between antipsychotic-induced Parkinsonism or its subsymptoms and rs4606 SNP of RGS2 gene in African-Caribbeans and the possible role of the medication: the Curacao extrapyramidal syndromes study X. Hum Psychopharmacol. 24: 123–128. [DOI] [PubMed] [Google Scholar]
- 25. Wilffert B, Al Hadithy AF, Sing VJ, Matroos G, Hoek HW, et al. (2009) The role of dopamine D3, 5-HT2A and 5-HT2C receptor variants as pharmacogenetic determinants in tardive dyskinesia in African-Caribbean patients under chronic antipsychotic treatment: Curacao extrapyramidal syndromes study IX. J Psychopharmacol 23: 652–659. [DOI] [PubMed] [Google Scholar]
- 26. Al Hadithy AF, Wilffert B, Stewart RE, Looman NM, Bruggeman R, et al. (2008) Pharmacogenetics of parkinsonism, rigidity, rest tremor, and bradykinesia in African-Caribbean inpatients: differences in association with dopamine and serotonin receptors. Am J Med Genet B Neuropsychiatr Genet 147B: 890–897. [DOI] [PubMed] [Google Scholar]
- 27.StataCorp.2009. Stata: Release 11. Statistical Software. College Station, TX: StataCorp LP.
- 28.Greenbaum L, Alkelai A, Zozulinsky P, Kohn Y, Lerer B (2011) Support for association of HSPG2 with tardive dyskinesia in Caucasian populations. Pharmacogenomics J. tpj201132 [pii];10.1038/tpj.2011.32 [doi]. [DOI] [PubMed]
- 29.Syu A, Ishiguro H, Inada T, Horiuchi Y, Tanaka S, et al.. (2010) Association of the HSPG2 gene with neuroleptic-induced tardive dyskinesia. Neuropsychopharmacology 35: 1155–1164. npp2009220 [pii];10.1038/npp.2009.220 [doi]. [DOI] [PMC free article] [PubMed]
- 30. Inada T, Koga M, Ishiguro H, Horiuchi Y, Syu A, et al. (2008) Pathway-based association analysis of genome-wide screening data suggest that genes associated with the gamma-aminobutyric acid receptor signaling pathway are involved in neuroleptic-induced, treatment-resistant tardive dyskinesia. Pharmacogenet Genomics 18: 317–323. [DOI] [PubMed] [Google Scholar]
- 31. Lerer B, Segman RH, Fangerau H, Daly AK, Basile VS, et al. (2002) Pharmacogenetics of tardive dyskinesia: combined analysis of 780 patients supports association with dopamine D3 receptor gene Ser9Gly polymorphism. Neuropsychopharmacology 27: 105–19. [DOI] [PubMed] [Google Scholar]
- 32. Bakker PR, van Harten PN, van Os J (2006) Antipsychotic-induced tardive dyskinesia and the Ser9Gly polymorphism in the DRD3 gene: a meta analysis. Schizophr Res 83: 185–192. [DOI] [PubMed] [Google Scholar]
- 33. Al Hadithy AF, Ivanova SA, Pechlivanoglou P, Semke A, Fedorenko O, et al. (2009) Tardive dyskinesia and DRD3, HTR2A and HTR2C gene polymorphisms in Russian psychiatric inpatients from Siberia. Prog Neuropsychopharmacol Biol Psychiatry 33: 475–481. [DOI] [PubMed] [Google Scholar]
- 34. Eichhammer P, Albus M, Borrmann-Hassenbach M, Schoeler A, Putzhammer A, et al. (2000) Association of dopamine D3-receptor gene variants with neuroleptic induced akathisia in schizophrenic patients: a generalization of Steen’s study on DRD3 and tardive dyskinesia. Am J Med Genet 96: 187–91. [DOI] [PubMed] [Google Scholar]
- 35. Segman RH, Heresco-Levy U, Finkel B, Inbar R, Neeman T, et al. (2000) Association between the serotonin 2C receptor gene and tardive dyskinesia in chronic schizophrenia: additive contribution of 5-HT2Cser and DRD3gly alleles to susceptibility. Psychopharmacology (Berl) 152: 408–413. [DOI] [PubMed] [Google Scholar]
- 36. Segman RH, Heresco-Levy U, Yakir A, Goltser T, Strous R, et al. (2002) Interactive effect of cytochrome P450 17alpha-hydroxylase and dopamine D3 receptor gene polymorphisms on abnormal involuntary movements in chronic schizophrenia. Biol Psychiatry 51: 261–263. [DOI] [PubMed] [Google Scholar]
- 37. Basile VS, Masellis M, Potkin SG, Kennedy JL (2002) Pharmacogenomics in schizophrenia: the quest for individualized therapy. Hum Mol Genet 11: 2517–30. [DOI] [PubMed] [Google Scholar]
- 38. Zhang ZJ, Zhang XB, Hou G, Yao H, Reynolds GP (2003) Interaction between polymorphisms of the dopamine D3 receptor and manganese superoxide dismutase genes in susceptibility to tardive dyskinesia. Psychiatr Genet 13: 187–192. [DOI] [PubMed] [Google Scholar]
- 39. Zai CC, Tiwari AK, De Luca V, Muller DJ, Bulgin N, et al. (2009) Genetic study of BDNF, DRD3, and their interaction in tardive dyskinesia. Eur Neuropsychopharmacol 19: 317–328. [DOI] [PubMed] [Google Scholar]
- 40. Srivastava V, Varma PG, Prasad S, Semwal P, Nimgaonkar VL, et al. (2006) Genetic susceptibility to tardive dyskinesia among schizophrenia subjects: IV. Role of dopaminergic pathway gene polymorphisms. Pharmacogenet Genomics 16: 111–117. [DOI] [PubMed] [Google Scholar]
- 41. Lattuada E, Cavallaro R, Serretti A, Lorenzi C, Smeraldi E (2004) Tardive dyskinesia and DRD2, DRD3, DRD4, 5-HT2A variants in schizophrenia: an association study with repeated assessment. Int J Neuropsychopharmacol 7: 489–493. [DOI] [PubMed] [Google Scholar]
- 42. Zai CC, Tiwari AK, Basile V, De Luca V, Muller DJ, et al. (2009) Association study of tardive dyskinesia and five DRD4 polymorphisms in schizophrenia patients. Pharmacogenomics J 9: 168–174. [DOI] [PubMed] [Google Scholar]
- 43. Zhang ZJ, Zhang XB, Sha WW, Zhang XB, Reynolds GP (2002) Association of a polymorphism in the promoter region of the serotonin 5-HT2C receptor gene with tardive dyskinesia in patients with schizophrenia. Mol Psychiatry 7: 670–671. [DOI] [PubMed] [Google Scholar]
- 44. Segman RH, Lerer B (2002) Age and the relationship of dopamine D3, serotonin 2C and serotonin 2A receptor genes to abnormal involuntary movements in chronic schizophrenia. Mol Psychiatry 7: 137–139. [DOI] [PubMed] [Google Scholar]
- 45. Gunes A, Dahl ML, Spina E, Scordo MG (2008) Further evidence for the association between 5-HT2C receptor gene polymorphisms and extrapyramidal side effects in male schizophrenic patients. Eur J Clin Pharmacol 64: 477–482. [DOI] [PubMed] [Google Scholar]
- 46. Rizos EN, Siafakas N, Katsantoni E, Lazou V, Sakellaropoulos K, et al. (2009) Association of the dopamine D3 receptor Ser9Gly and of the serotonin 2C receptor gene polymorphisms with tardive dyskinesia in Greeks with chronic schizophrenic disorder. Psychiatr Genet 19: 106–107. [DOI] [PubMed] [Google Scholar]
- 47.Pae CU, Yu HS, Kim JJ, Lee CU, Lee SJ, et al.. (2004) Quinone oxidoreductase (NQO1) gene polymorphism (609C/T) may be associated with tardive dyskinesia, but not with the development of schizophrenia. Int J Neuropsychopharmacol 7: 495–500. 10.1017/S1461145704004419 [doi];S1461145704004419 [pii]. [DOI] [PubMed]
- 48.Xu Z, Taylor JA (2009) SNPinfo: integrating GWAS and candidate gene information into functional SNP selection for genetic association studies. Nucleic Acids Res 37: W600-W605. gkp290 [pii];10.1093/nar/gkp290 [doi]. [DOI] [PMC free article] [PubMed]
- 49. Schooler NR, Kane JM (1982) Research diagnoses for tardive dyskinesia. Arch Gen Psychiatry 39: 486–7. [DOI] [PubMed] [Google Scholar]
- 50.Steyerberg EW (2009) Clinical prediction models: a practical approach to development, validation, and updating. New York: Springer.
- 51.Ziegler A and König IR (2006) A statistical approach to genetic epidemiology: concepts and applications. Weinheim: Wiley-VCH.
- 52.Benjamini Y, Bretz F, and Sarkar SK (2004) Recent developments in multiple comparison procedures. Beachwood, Ohio: Institute of Mathematical Statistics.
- 53.Bakker PR, Bakker E, Amin N, van Duijn CM, van Os J, et al.. (2012) Candidate gene-based association study of antipsychotic-induced movement disorders in long-stay psychiatric patients: a prospective study. PLoS ONE 7: e36561. 10.1371/journal.pone.0036561 [doi];PONE-D-12-00737 [pii]. [DOI] [PMC free article] [PubMed]
- 54.Carlson CS, Eberle MA, Rieder MJ, Yi Q, Kruglyak L, et al.. (2004) Selecting a maximally informative set of single-nucleotide polymorphisms for association analyses using linkage disequilibrium. Am J Hum Genet 74: 106–120. S0002-9297(07)61949-1 [pii];10.1086/381000 [doi]. [DOI] [PMC free article] [PubMed]
- 55.Howes OD, Kapur S (2009) The dopamine hypothesis of schizophrenia: version III–the final common pathway. Schizophr Bull 35: 549–562. sbp006 [pii];10.1093/schbul/sbp006 [doi]. [DOI] [PMC free article] [PubMed]
- 56. van Os J, Kenis G, Rutten BP (2010) The environment and schizophrenia. Nature 468: 203–212. [DOI] [PubMed] [Google Scholar]
- 57. Lerer B, Segman RH, Tan EC, Basile VS, Cavallaro R, et al. (2005) Combined analysis of 635 patients confirms an age-related association of the serotonin 2A receptor gene with tardive dyskinesia and specificity for the non-orofacial subtype. Int J Neuropsychopharmacol 8: 411–425. [DOI] [PubMed] [Google Scholar]
- 58.Greenbaum L, Alkelai A, Rigbi A, Kohn Y, Lerer B (2010) Evidence for association of the GLI2 gene with tardive dyskinesia in patients with chronic schizophrenia. Mov Disord 25: 2809–2817. 10.1002/mds.23377 [doi]. [DOI] [PubMed]
- 59.Tanaka S, Syu A, Ishiguro H, Inada T, Horiuchi Y, et al.. (2011) DPP6 as a candidate gene for neuroleptic-induced tardive dyskinesia. Pharmacogenomics J. tpj201136 [pii];10.1038/tpj.2011.36 [doi]. [DOI] [PubMed]
- 60.Alkelai A, Greenbaum L, Rigbi A, Kanyas K, Lerer B (2009) Genome-wide association study of antipsychotic-induced parkinsonism severity among schizophrenia patients. Psychopharmacology Published online. [DOI] [PubMed]
- 61. Aberg K, Adkins DE, Bukszar J, Webb BT, Caroff SN, et al. (2010) Genomewide association study of movement-related adverse antipsychotic effects. Biol Psychiatry 67: 279–282. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Szklo M and Nieto FJ (2007) Epidemiology: beyond the basics. Sudbury, Mass: Jones and Bartlett Publishers.
- 63.Rothman KJ, Greenland S, and Lash TL (2008) Modern epidemiology. Philadelphia: Wolters Kluwer Health/Lippincott Williams & Wilkins.
- 64.Zammit S, Lewis G, Dalman C, Allebeck P (2010) Examining interactions between risk factors for psychosis. Br J Psychiatry 197: 207–211. 197/3/207 [pii];10.1192/bjp.bp.109.070904 [doi]. [DOI] [PubMed]
- 65.Kendler KS, Gardner CO (2010) Interpretation of interactions: guide for the perplexed. Br J Psychiatry 197: 170–171. 197/3/170 [pii];10.1192/bjp.bp.110.081331 [doi]. [DOI] [PubMed]
- 66.Zammit S, Owen MJ, Lewis G (2010) Misconceptions about gene-environment interactions in psychiatry. Evid Based Ment Health 13: 65–68. 13/3/65 [pii];10.1136/ebmh.13.3.65 [doi]. [DOI] [PubMed]
- 67.Rabe-Hesketh S and Skrondal A (2008) Multilevel and longitudinal modelling using stata. College Station, Tex: Stata Press.
- 68. Molenaar PCM, Campbell CG (2009) The New Person-Specific Paradigm in Psychology. Current Directions in Psychological Science 18: 112–117. [Google Scholar]
- 69.Myin-Germeys I, Oorschot M, Collip D, Lataster J, Delespaul P, et al.. (2009) Experience sampling research in psychopathology: opening the black box of daily life. Psychol Med 39: 1533–1547. S0033291708004947 [pii];10.1017/S0033291708004947 [doi]. [DOI] [PubMed]
- 70. Csikszentmihalyi M, Larson R (1987) Validity and reliability of the Experience-Sampling Method. J Nerv Ment Dis 175: 526–536. [DOI] [PubMed] [Google Scholar]
- 71.Myin-Germeys I, Birchwood M, Kwapil T (2011) From environment to therapy in psychosis: a real-world momentary assessment approach. Schizophr Bull 37: 244–247. sbq164 [pii];10.1093/schbul/sbq164 [doi]. [DOI] [PMC free article] [PubMed]
- 72.Smith A, Balazinska M, Baru C, Gomelsky M, McLennan M, et al.. (2011) Biology and data-intensive scientific discovery in the beginning of the 21st century. OMICS 15: 209–212. 10.1089/omi.2011.0006 [doi]. [DOI] [PubMed]
- 73.Chalise P, Batzler A, Abo R, Wang L, Fridley BL (2012) Simultaneous analysis of multiple data types in pharmacogenomic studies using weighted sparse canonical correlation analysis. OMICS 16: 363–373. 10.1089/omi.2011.0126 [doi]. [DOI] [PMC free article] [PubMed]
- 74. Ioannidis JP, Gwinn M, Little J, Higgins JP, Bernstein JL, et al. (2006) A road map for efficient and reliable human genome epidemiology. Nat Genet 38: 3–5. [DOI] [PubMed] [Google Scholar]
- 75.Gunther T, Schmitt AO, Bortfeldt RH, Hinney A, Hebebrand J, et al.. (2011) Where in the genome are significant single nucleotide polymorphisms from genome-wide association studies located? OMICS 15: 507–512. 10.1089/omi.2010.0154 [doi]. [DOI] [PubMed]
- 76. Braff DL, Freedman R, Schork NJ, Gottesman II (2007) Deconstructing schizophrenia: an overview of the use of endophenotypes in order to understand a complex disorder. Schizophr Bull 33: 21–32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77. Koning JP, Tenback DE, Kahn RS, Van Schelven LJ, van Harten PN (2010) Instrument measurement of lingual force variability reflects tardive tongue dyskinesia. J Med Eng Technol 34: 71–77. [DOI] [PubMed] [Google Scholar]
- 78.Koning JP, Vehof J, Burger H, Wilffert B, Al Hadithy A, et al.. (2012) Association of two DRD2 gene polymorphisms with acute and tardive antipsychotic-induced movement disorders in young Caucasian patients. Psychopharmacology (Berl) 219: 727–736. 10.1007/s00213–011–2394–1 [doi]. [DOI] [PubMed]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Selected 45 tag SNPs for multilevel regression of continuous movement disorders (subtypes).
(DOC)
Supporting information about the 7 candidate genes.
(DOC)