Abstract
Human follicular fluid, considered sterile, is aspirated as part of an in vitro fertilization (IVF) cycle. However, it is easily contaminated by the trans-vaginal collection route and little information exists in its potential to support the growth of microorganisms. The objectives of this study were to determine whether human follicular fluid can support bacterial growth over time, whether the steroid hormones estradiol and progesterone (present at high levels within follicular fluid) contribute to the in vitro growth of bacterial species, and whether species isolated from follicular fluid form biofilms. We found that bacteria in follicular fluid could persist for at least 28 weeks in vitro and that the steroid hormones stimulated the growth of some bacterial species, specifically Lactobacillus spp., Bifidobacterium spp. Streptococcus spp. and E. coli. Several species, Lactobacillus spp., Propionibacterium spp., and Streptococcus spp., formed biofilms when incubated in native follicular fluids in vitro (18/24, 75%). We conclude that bacteria aspirated along with follicular fluid during IVF cycles demonstrate a persistent pattern of growth. This discovery is important since it can offer a new avenue for investigation in infertile couples.
Introduction
Follicular fluid, which surrounds the oocyte during in vivo folliculogenesis, is a hypocoagulable, semi-viscous fluid comprising proteins, inorganic compounds, carbohydrates, mucopolysaccharides, lipids, gonadotrophins, steroid hormones, immunoglobulins, cytokines, complement components and growth factors [1], [2]. Previous studies have shown that whilst human follicular fluid has antimicrobial properties, it is still capable of supporting microbial growth in vitro [3], [4]. Cottell et al. [5] first reported the presence of bacteria within follicular fluid that had been collected at the time of trans-vaginal oocyte retrieval. In addition, in our recent study, we isolated numerous microorganisms from follicular fluid. The microorganisms were present as asymptomatic colonizers or as contaminants that were introduced into the follicular fluid at the time of trans-vaginal oocyte retrieval [6]. The collected follicular fluids did not appear cloudy/turbid, despite the presence of a mixed microflora, in contrast to acute microbial infections of other body fluids such as urine. In their native environment, the majority of bacteria exist as complex surface-attached communities [7]. This observation prompted our current study to investigate follicular fluid as a medium to support the growth of microorganisms. Since the follicular fluids collected from women undergoing IVF cycles contain high levels of estradiol and progesterone as a result of the IVF stimulation process, we hypothesised that these steroid hormones may affect the growth of microorganisms. We also hypothesised that microorganisms present in human follicular fluids could persist over time and form biofilms in the ovarian follicular fluid.
Methods
1.1 Participants
From September 2007 to November 2008, couples commencing fully stimulated IVF cycles at Wesley-Monash IVF in Brisbane, Australia were invited to enrol in this study. Thirty-six follicular fluid specimens were randomly selected for testing and included equal numbers of clear and blood-stained fluids.
1.2 Ethics Statement
Ethical approval was obtained from the review boards of Uniting Care Health, Human Research Ethics Committee and Queensland University of Technology Human Ethics Committee. All patients provided informed written consent for their follicular fluids to be used in this study.
1.3 Trans-vaginal Oocyte Retrieval
Follicular fluid was collected by the IVF clinicians at the time of oocyte retrieval as previously described [6]. The IVF unit used a ‘boost’ protocol for controlled ovarian hyper-stimulation. For each study participant, the follicular fluid from the largest most accessible follicle in either the left or the right ovary was aspirated first. Follicular fluid was aspirated directly into sterile test tubes in the operating theatre. The follicular fluid specimens were aseptically transferred to a sterile culture dish to determine if there was an oocyte present. Following removal of the oocyte, the IVF scientists transferred the remaining follicular fluid to a sterile 15 mL Falcon tube for storage at −80°C. There was significant variability in the volume of follicular fluid collected from each follicle (range <1 mL–∼12 mL). Therefore, only the follicular fluid samples with a volume of greater than 5 mL were able to be tested using all assays.
1.4 Colony Identification and 16 S Ribosomal RNA (rRNA) PCR and Sequencing
Isolation and identification of microbial species from the 36 human follicular fluid specimens were performed as previously described [6]. Briefly, calibrated 1 µL inoculating loops were used to inoculate a range of microbiological culture media, which were incubated under 5% CO2 or anaerobically at 37°C for the isolation and identification of microorganisms.
DNA extraction was performed on 1 mL aliquots of each follicular fluid specimen, and then the extracted DNA used as a template for 16 S rRNA PCR. The preparation of PCR products for sequencing was performed as per the Australian Genome Research Facility instructions for the preparation of purified DNA (AGRF, St. Lucia, QLD). AGRF sequenced each purified PCR product using a Big Dye 3 sequencing technology (BDT) labelling sequencing platform. The sequence, obtained in a FASTA format was entered into the Basic Local Alignment Search Tool (BLAST, NCBI) for identification of clinical isolates.
1.5 Hormonal Effect on Bacterial Growth in Follicular Fluid
Twelve frozen follicular fluid aliquots were thawed, and 1 µl of each cultured on a range of solid agar plates and in thioglycollate broth containing estradiol and progesterone (Sigma Aldrich, Castle Hill, NSW), at concentrations of 375 µg/L and 800 µg/L respectively (the median concentrations reported in the follicular fluid collected from hyperstimulated women undergoing trans-vaginal oocyte retrieval) [8], [9]. Hormones were added to the culture media because these would be present in the native follicular fluids and would degrade over time in culture. Hormones were used only in combination, rather than individually, as both are present at high concentrations in the follicular fluids of women undergoing IVF treatment and trans-vaginal oocyte retrieval. Follicular fluid specimens were also cultured on the same media without the addition of hormones as controls. Agar plates were incubated either aerobically or anaerobically at 37°C. After seven days of incubation at 37°C, positive thioglycollate broths were vortexed and a sterile 1 µL calibrated loop used to subculture broth onto horse blood agar (Oxoid, Adelaide, SA) for quantification and identification of the bacteria present [6].
1.6 Long-term Follicular Fluid Culture
From 24 follicular fluid specimens 1 mL of follicular fluid was aliquoted aseptically into 1.7 mL microcentrifuge tubes and incubated at 37°C aerobically. These 24 specimens were vortexed and subcultured daily: 1 µL of the follicular fluid was subcultured, onto horse blood agar and anaerobic blood agar plates (Oxoid) and incubated aerobically and anaerobically at 37°C. After (24 hours) incubation, the number of colonies on the horse blood agar were counted and expressed as the number of colony forming units (CFU)/mL of follicular fluid.
1.7 Biofilm Assay
From the same 24 follicular fluid specimens 300 µL was added to a sterile 13 mm coverslip in a well of a 24-well microtiter plate for the biofilm assay. Triplicate microtiter plates (technical replicates) were prepared and subsequently incubated in aerobic and anaerobic conditions at 37°C. Two coverslips were stained as described below, and the bacteria from the third coverslip were inoculated onto media as described in Methods 1.9. The follicular fluid specimens were incubated within the microtiter plates and left undisturbed for ten days, to mimic the average period of development of follicular fluid within a maturing ovarian follicle [10]. Upon removal, coverslips were gently rinsed with PBS to remove any unbound cells. The coverslips were subsequently placed onto microscope slides and processed using a method adopted from Allison and Sutherland [11]. Briefly, the coverslips were covered with 10 mM cetyl pyridinium chloride and air-dried before heat fixation. The biofilms then were stained for 15 minutes with a 2∶1 mixture of saturated Congo red (Sigma Aldrich) solution and 10% Tween 20 (Sigma Aldrich). Slides were then rinsed, counterstained with 10% Ziehl carbol fuchsin, rinsed again and dried at 37°C. The prepared coverslips were viewed by light and confocal microscopy.
Biofilms were viewed by light microscopy using an Olympus BX41 light microscope (Olympus, Tokyo, Japan), and images captured with a MicroPublisher 3.3 RTV camera (Adept Electronic Service, Warriewood, NSW) and QCapture Pro software (QImaging, Surrey, BC). Biofilms were examined under total magnifications of ×100 and ×400.
Images of the biofilms also were acquired by a TCS SP5 confocal laser scanning microscope (Leica Microsystems, Germany) equipped with a Leica HCX PL APO CS ×10 objective, and a Leica HCX PL APO CS × 63 oil immersion objective (NA 1.4). To visualise the Congo red and carbol fuschin signal, the excitation wavelength was set at 561 nm, and the fluorescence emission was detected between 567–668 nm. A series of z stack images were acquired through a volume of 60 µm and the images analysed using LAS AF (Leica Microsystems).
Biofilm maturity was graded based on the presence of key characteristic and structural features described previously by Simmons et al. [12]. Biofilms were classified as grade I–planktonic cells (isolated free floating cells, not adherent to the slide) and cells adherent to the conditioning film; grade II–microcolonies and groups of cells (most likely planktonic) attached to each other; grade III–extending/growing microcolonies (towers) with extracellular matrix fibrils, creating interconnections between the microcolonies, thus giving a cobweb appearance; and grade IV–towers with subterranean channels and amorphous extracellular material, giving a honeycomb appearance between the microcolonies.
1.8 Biofilm Assay – Scanning Electron Microscopy (SEM)
SEM was used to visualise biofilm production for four of the follicular fluid specimens and two ATCC controls (Lactobacillus gasseri and Bacteroides fragilis). 300 µL of each of the follicular fluid specimens or ATCC overnight broth cultures was added to a single sterile 13 mm coverslip in each well of a 24-well microtiter plate. Plates were performed in dulplicate so that one set was grown for 5 days, and the other 10 days. Glass coverslips were fixed in 3% glutaraldehyde in 0.1 M sodium cacodylate buffer, pH 7.4 for 24 hours at 4°C. After primary fixation, the coverslips were washed three times for 10 minutes in 0.1 M cacodylate buffer and post fixed for one hour in either 1% Osmium tetroxide or 1% Osmium tetroxide with 0.15% ruthenium red. Post-fixation, coverslips were twice washed in water and dehydrated in an ascending ethanol series (50, 70, 90, and 100% (twice)) before drying with 100% hexamethyldisilazane (HMDS) (Sigma Aldrich). Specimens were mounted on aluminium stubs with adhesive carbon tape and then sputter coated with 10 mm of gold (Leica SCD005 sputter coater). Examination of samples was performed using a FEI Quanta 3D Focused Ion Beam SEM, operating at 10 kv.
1.9 Biofilm Culture
The third coverslip (from Methods 1.7) was rinsed with sterile PBS; a sterile swab was used to remove the biofilm from the coverslip surface. This bacterial suspension was made in thioglycollate broth; a 1 µL calibrated inoculating loop was used to subculture the biofilm onto horse blood agar and anaerobic blood agar plates (Oxoid). Plates were incubated aerobically at 37°C for 24–48 hours and at 37°C for up to 7 days. Isolated bacterial species were identified as previously described [6].
Results
Follicular Fluid Culture and Bacterial Colony Identification
Bacteria were cultured from each of the 24 follicular fluid specimens tested. A single bacterial species was isolated from 15/24 (63%) of the specimens, of which 7/15 (47%) contained Lactobacillus species. Propionibacterium spp. (n = 5), Peptostreptococcus spp. (n = 2), or Salmonella enterica (n = 1) were isolated in the remaining specimens. Two bacterial species were isolated from 6/24 (25%) specimens, and five of these (83%) contained Lactobacillus spp. Only 3/24 (12%) follicular fluid specimens contained three bacterial species and Lactobacillus spp. was isolated from each of these specimens. Lactobacillus spp. and Propionibacterium spp. were the most prevalent isolates detected in follicular fluid, isolated from 51% and 14% specimens respectively (Table 1). Only 13/24 follicular fluid samples were of a sufficient volume for the complete analyses.
Table 1. Bacterial genera isolated and identified from cultures of follicular fluid.
| Genus and species | Follicular fluid culture n = 24 | Percentage of total n = 35 isolates3 | Biofilm culture n = 18 | Percentage of total n = 23 isolates3 |
| Lactobacillus gasseri 1 | 9 | 27% | 9 | 40% |
| L. crispatus 1 | 7 | 20% | 7 | 30% |
| L. jensenii 1 | 2 | 5% | 1 | 5% |
| CoNS2 | 3 | 9% | 0 | 0% |
| Propionibacterium spp. | 5 | 14% | ||
| Peptostreptococcus spp. | 2 | 5% | 0 | 0% |
| B. longum | 2 | 5% | 1 | 5% |
| S. agalactiae | 1 | 3% | 1 | 5% |
| S. anginosus | 1 | 3% | 1 | 5% |
| Micrococcus spp. | 1 | 3% | 1 | 5% |
| Salmonella enterica | 1 | 3% | 1 | 5% |
| Escherichia coli | 1 | 3% | 0 | 0% |
| Total number of isolates | 35 | 23 |
Lactobacillus spp. were the most prevalent bacteria in follicular fluid 18/35 (51%);
CoNS coagulase negative staphylococci;
Some follicular fluids contained more than one bacterial species, giving the total number of isolates as greater than the number of follicular fluids tested.
Hormonal Modulators of Bacterial Growth in Solid Media and Broths
When follicular fluid was cultured on solid agar media and incubated under appropriate atmospheric conditions, with or without hormone supplements, there were no differences in the number of isolated CFUs/mL (103–>106). However, differences were observed in the growth patterns of bacteria cultured in thioglycollate broth (with and without hormones) for 5/12 follicular fluid specimens tested (Table 2). Lactobacillus spp. were recovered from 7/12 (58%) thioglycollate broths. For one specimen (see Table 2, No. 12), Lactobacillus crispatus and L. gasseri were cultured from the hormone-supplemented thioglycollate media, but only L. crispatus was recovered from the hormone-free media. However, for the remaining Lactobacillus containing specimens, there were slight differences in the CFUs/mL of the Lactobacillus spp. isolated in the presence or absence of hormones. Bifidobacterium spp. was detected in two follicular fluid specimens, and where the supplemental hormones supported the growth of the Bifidobacterium spp., this bacterium did not grow in the absence of hormones. In contrast, the supplemental hormones inhibited the growth of E. coli and S. agalactiae, but growth was observed within the thioglycollate broth, without the addition of exogenous steroid hormones (see Table 2).
Table 2. Bacterial growth in hormone supplemented thioglycollate broth.
| Specimen | Species identified | CFU/mL Hormone supplemented media2 | CFU/mL Hormone-free media2 |
| 1 | Bifidobacterium spp. | 104 | No growth |
| 2 | Bifidobacterium spp. | 104 | No growth |
| 3 | E. coli | No growth | <103 |
| 4 | L. crispatus | 106 | 104 |
| 5 | L. crispatus, L. gasseri | <103 * | <103 |
| 6 | L. crispatus, L. gasseri | 104 | L. crispatus only <103 |
| 7 | L. gasseri | 106 | 106 |
| 8 | L. gasseri | 106 | 104 |
| 9 | L. gasseri | 106 | 106 |
| 10 | L. jensenii | 104 | 104 |
| 11 | No growth1 | ||
| 12 | S. agalactiae | No growth | <103 |
Culture negative, however positive by 16 S rRNA PCR assay,
Thioglycollate broths,
<103 represents growth in thioglycollate broth but not on solid agar subculture plates.
Long-term Follicular Fluid in vitro Culture
All follicular fluid specimens cultured in vitro demonstrated increasing numbers of CFUs/mL at each subculture until eight days post-incubation (<103–>106), after which the number of cultivable bacteria reached a plateau and the numbers for these bacteria remained constant for the remaining 27 weeks (103–106). Furthermore, after 5–8 days incubation, only a single bacterial species in pure culture could be isolated from all follicular fluid specimens. With the exception of S. enterica, all of the bacterial species isolated after eight days were Gram-positive (Lactobacillus spp., Bifidobacterium spp. and Staphylococcus spp.). Viable Gram-positive bacteria could be recovered from these follicular fluids, which were incubated in vitro for 28 weeks.
Biofilm Assay
The 24 follicular fluid specimens were tested to determine their ability to form biofilms on glass coverslips in wells of a 24-well plate. Biofilms formed in vitro after incubation at 37°C for 18/24 (75%) of follicular fluids. Of these biofilms, 14 were monomicrobial and four were polymicrobial as determined by the number of different colony types identified by traditional microbiological culture. The bacterial species L. gasseri, L. crispatus, Bifidobacterium longum, S. agalactiae, S. anginosus and S. entericus, if initially present in follicular fluid, were always recovered from the biofilm well sub-cultures after 10 days of in vitro culture. Other bacterial species, including CoNS, Peptostreptococcus spp. and E. coli, were only cultured from the original follicular fluid specimens. In 16/24 (66%) of the follicular fluids tested, the primary culture demonstrated polymicrobial colonisation, but only a single species was detected after 10 days of incubation within each well of the microtiter plate. In addition, if only a single species was detected in the primary follicular fluid culture, the same single species was always detected in the microtiter well culture. The facultative anaerobic species, Staphylococcus spp., Streptococcus spp. and Lactobacillus spp., were isolated following incubation under both aerobic and anaerobic conditions. In contrast, the strict anaerobes Bifidobacterium spp., and Peptostreptococcus spp. were isolated only when the follicular fluid specimens were incubated anaerobically.
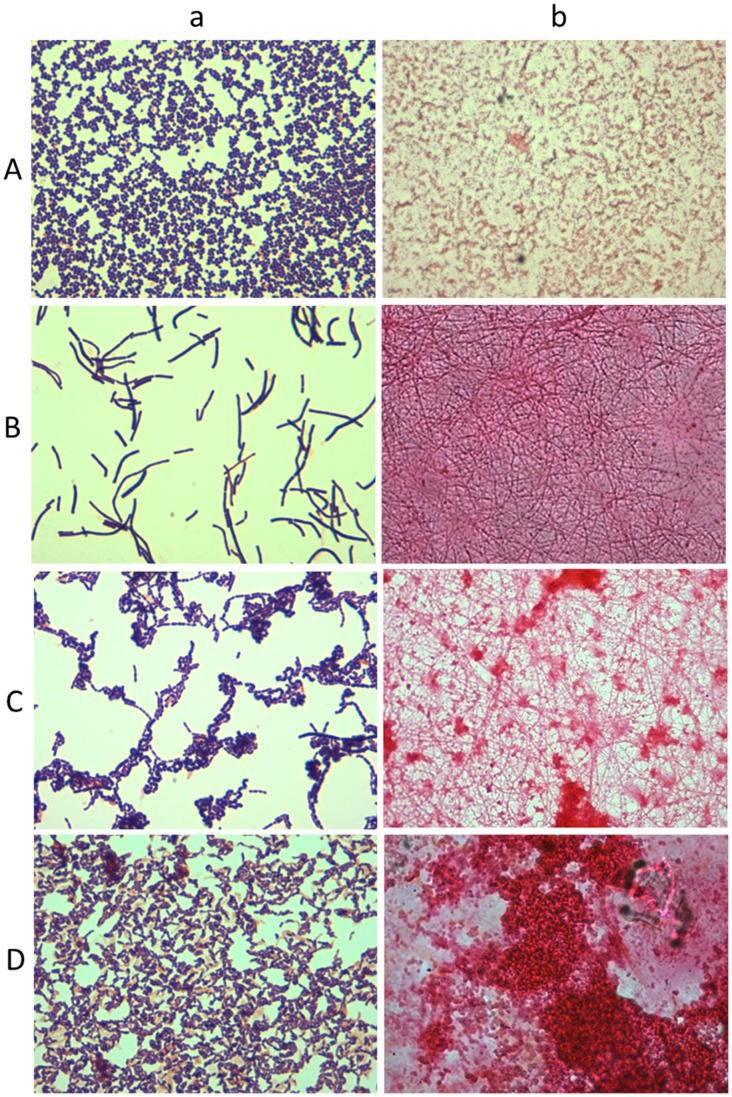
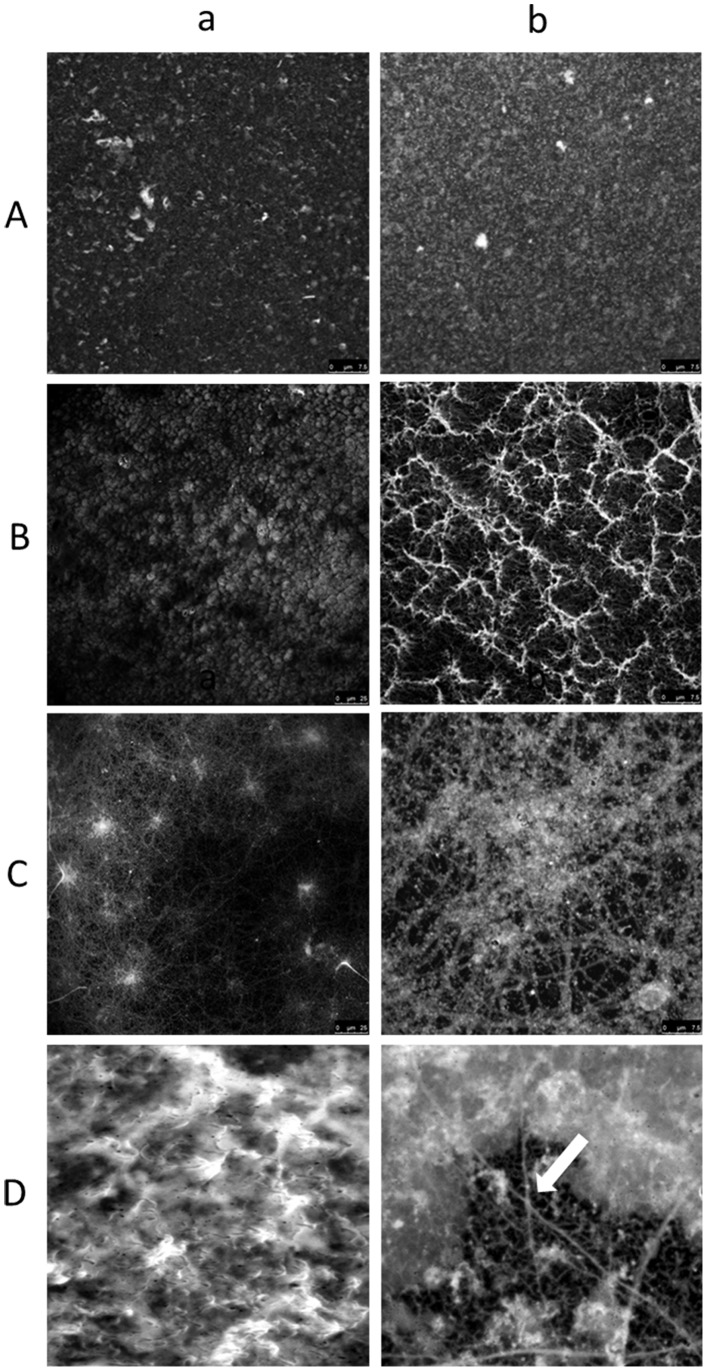
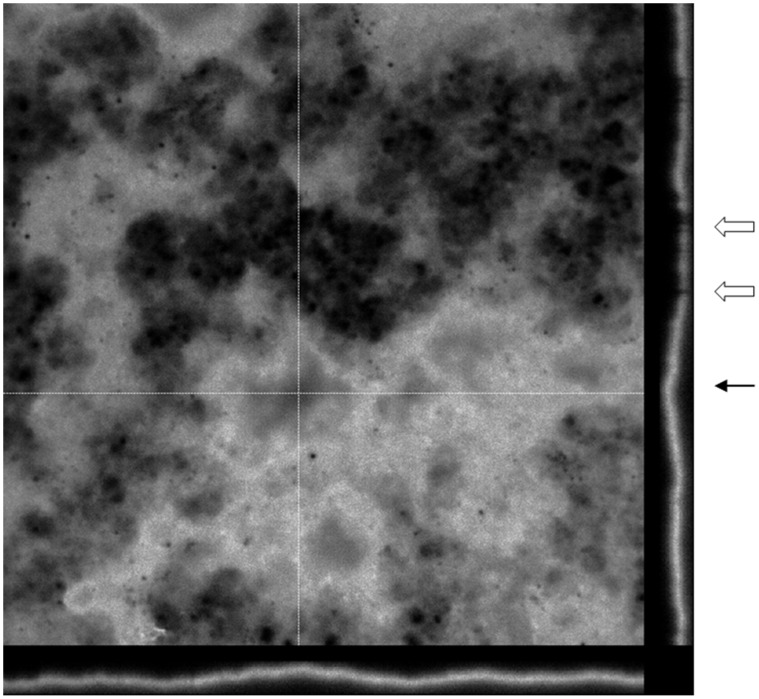
For six biofilms slides, there was no evidence of biofilm formation or planktonic cell adhesion. Instead, the Congo red stain revealed the presence of a polysaccharide-containing conditioning film. The images shown in Figure 1 are representative of the different types of Lactobacillus spp. biofilms observed for follicular fluids incubated both under aerobic and anaerobic atmospheric conditions. Variations in the architecture of mature biofilms was observed, ranging from flat homogenous cell layers through to cell clusters, microcolonies and towers with channelling and significant quantities of amorphous extracellular material between the more complex heterogeneous structures (Figure 1 B–D). The simplest biofilm architecture visualised by light microscopy was seen for follicular fluid cultures that were incubated aerobically. The grade II biofilm presented in Figure 1A (b) demonstrated few microcolonies (which proliferate at fixed positions [13], [14], and some of these extended to form towers (outward growing masses of bacterial cells). Initial microcolonies were formed by cells growing outwards into towers, with the highest points of elevation appearing white in greyscale using confocal microscopy, as shown in Figure 2A (a) and (b). A grade III biofilm was characterised by fibril formation, as observed by light microscopy, following anaerobic incubation (Figure 1B (b)); with a carpet-pile appearance as observed with confocal microscopy with some microcolonies extending to form towers, as shown in Figure 2B (a). The polymeric extracellular matrix appeared to be more abundant in microcolonies (Figure 1C (b)). When magnified (×4 zoom, confocal microscopy), crater-like formations were visible (Figure 2B (b)). In the grade IV biofilm grown under anaerobic conditions, complex networks were observed between the microcolonies and towers and these had a cobwebbed appearance, as shown in Figure 2C (a) and (b). Grade IV biofilms were also visualised using light microscopy (Figure 1D (b)) and an amorphous polymeric extracellular matrix was observed surrounding the interconnecting microcolonies, towers and cells. In these biofilms, continuous layers of cells covered the coverslip, with clusters forming prominences. These biofilms had a honeycomb appearance, as shown in Figure 2D (a) and (b) and could be visualised using three dimensional and orthogonal confocal images. This image (Figure 3) demonstrated the presence of channels within the biofilms and hollow areas under the towers. All observed biofilms showed an uneven spatial distribution, which is consistent with the previously described characteristic of in vitro biofilms [15].
Figure 1. Light micrographs of Gram stains and biofilm slides.
A–D (a)) Light microscopy image at ×1000 total magnification of Gram stained bacterial S. agalactiae and Lactobacillus spp. colonies cultured from biofilms. (A–D (b)) Light microscopy image at × 1000 total magnification of Congo red stained S. agalactiae and Lactobacillus spp. biofilms grown for 10 days on glass coverslips.
Figure 2. Laser scanning confocal microscopy images of biofilms.
(A–D (a)) Laser scanning confocal microscopy image of various grades of biofilms at × 630 total magnification. Scale bars represent 25 µM (A–D (a) Laser scanning confocal microscopy images of various grades of biofilms at × 630 total magnifications plus × 4 zoom. Scale bars represent 7.5 µM (C (b)) Image of cobwebbing. (D (b)) Image of the honeycombed region. The arrow points to the cavities in the honeycombs. Grade II biofilms presented in Figure 2 A (a and b) demonstrated few microcolonies, some of which extended to form towers. A grade III biofilm was characterised by a carpet-pile appearance with some microcolonies extending to form towers (Figure 2B (a)). Grade IV biofilms had a honeycomb appearance where the continuous layers of cells covered the coverslip with clusters forming prominences (Figure 2D (a) and (b)).
Figure 3. Representative orthogonal view of a 10-day-old biofilm incubated under anaerobic conditions.
Laser scanning confocal microscopy image of a mature Grade IV biofilm at × 630 total magnifications plus × 4 zoom. The orthogonal view allows the representation of the 3D biofilm to be presented in 2D. The cross hairs indicate the area of the biofilm presented in 2D along the borders of the image. Depicted below and to the right of the main image are the yz and xz planes respectively. In this biofilm, there are channels between the microcolonies appearing in ‘gaps’ in the 2D structure and indicated by the white arrows. The hollow interconnecting areas under the towers are indicated by the black arrow.
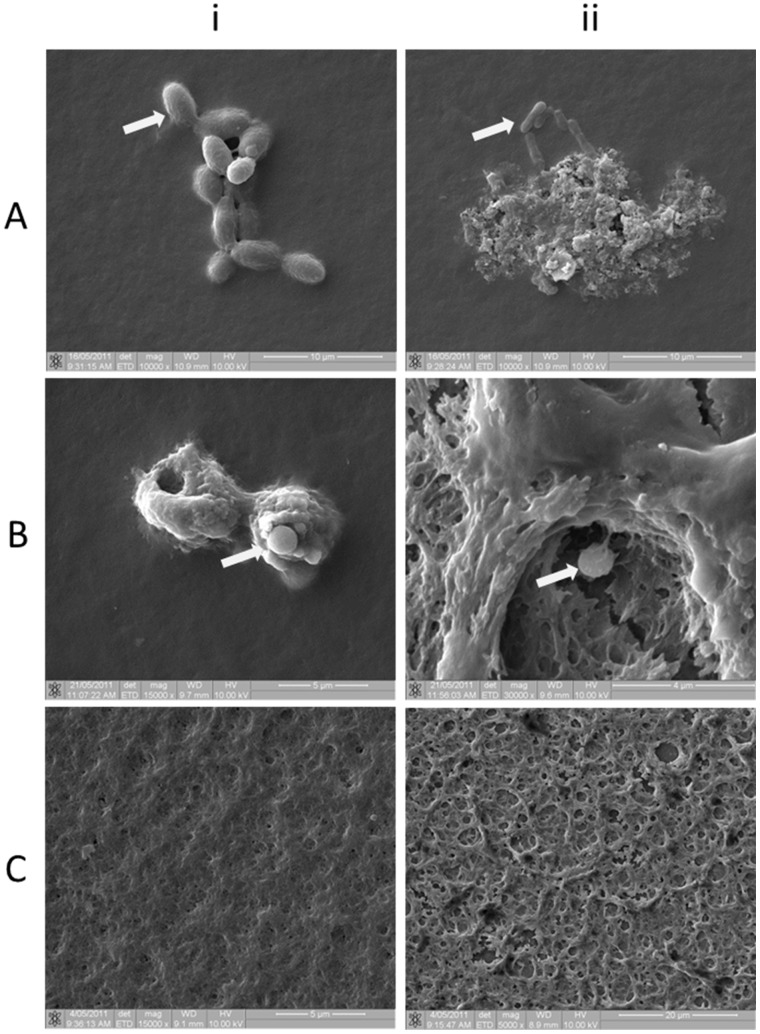
Biofilm Assay – Scanning Electron Microscopy
Scanning electron microscopy (SEM) was used to visualize the surface topography of biofilms grown in vitro on glass coverslips for 5 days or 10 days. SEM revealed the presence of bacterial cell aggregates covered by a thin layer of glycocalyx (Figure 4A (i)), as well as microcolonies (Figure 4A (ii)). The surface topography, with a crater-like appearance was similar to that seen in images obtained using confocal microscopy (Figure 2B). The preservation of the glycocalyx was enhanced when the post-fixative OsO4 (Figure 4C (i)) was combined with ruthenium red (Figure 4C (ii)). The use of the ruthenium red enhanced the stabilization and visualization of the highly charged anionic mucopolysaccharides forming the extracellular glycocalyx. Evidence of biofilm maturity, extensive extracellular polysaccharide and microcolonies was apparent in both five and ten day-old biofilms.
Figure 4. Scanning electron micrographs of 10-day-old biofilms.
Individual bacilli, identified as Lactobacillus spp. (day 5) (arrows) are covered by a light glycocalyx (4A (i)) and a control ATCC strain Bacteroides spp. (day 5) by a more mature biofilm (4A (ii)) both captured at × 10000 magnification. Figures 4B (i (day 5) and ii (day 10)) represent osmium fixed biofilms containing coccoid bacteria identified as Streptococcus spp. (by culture) (arrows) at × 15000 and × 30000 magnification. Glycocalyx is not well preserved using traditional aldehyde fixatives followed by OsO4 post-fixation. Figure 4C (i) (day 10) was fixed using OsO4, which stabilises lipids and figure 4C (ii) (day 10) was fixed using an aldehyde fixative followed by OsO4 plus ruthenium red to enhance the preservation of the anionic polysaccharides in the glycocalyx.
Discussion
Follicular fluids collected at the time of trans-vaginal oocyte retrieval were found to harbour bacteria and continued to support the bacterial growth in vitro. These results demonstrate that bacterial species that colonise follicular fluid, or gain access to the follicular fluid at the time of oocyte retrieval, may be a relevant focus of infertility investigations in couples with idiopathic infertility or repeated adverse IVF treatment outcomes.
Our study demonstrated that in vitro, elevated levels of estradiol and progesterone in thioglycollate broth media enhanced the growth of the high numbers of CFUs of Lactobacillus spp., which were originally present within follicular fluid specimens. This is consistent with Lactobacillus spp. growth in the lower genital tract. At puberty, as estrogen levels increase, the vaginal pH drops and Lactobacillus spp. dominate the vaginal microflora [16]. After menopause, the vaginal microflora reverts to the pre-menarchal state and the Lactobacillus spp. decline [17]. However, if post-menopausal women receive estrogen replacement therapy, the vaginal pH decreases and the concentration of Lactobacillus spp. increases [18]. The effect of endogenous steroid hormones on lactobacilli has previously been monitored in IVF patients. Jakobsson and Forsum [19] reported that during IVF treatment, with increasing estrogen levels, three major vaginal lactobacilli (L. crispatus, L. gasseri or L. jensenii) were predominant. These results are consistent with the findings reported in this paper, as these species were the only lactobacilli isolated from follicular fluid (collected prior to ovulation when estradiol levels were highest), although Bifidobacterium spp. was also isolated from the hormone-supplemented media. Both genera can metabolise carbohydrates from glycogen degradation in response to elevated estradiol levels, making the female genital tract a niche environment, enhancing the ability of the lactobacilli to persist and protect the genital tract epithelium from opportunistic infection [20]. Bifidobacterium spp., whilst traditionally accepted as members of the normal regional flora of the gastrointestinal tract, have more recently been detected in the vaginal flora of healthy women [20], [21], [22].
During an IVF treatment cycle, hormones including follicle stimulating hormone and human chorionic gonadotropin are administered to trigger the simultaneous maturation of multiple ovarian follicles. This results in the production of elevated levels of estradiol and progesterone within the follicular fluids collected from women undergoing trans-vaginal oocyte retrieval for IVF at levels approximately eight and three times higher, respectively, than those of women with normal cycles [8], [9]. The ovarian granulosa cells are the dominant source of these steroid hormones. Granulosa cells may be aspirated with the follicular fluid and the oocyte at the time of trans-vaginal oocyte retrieval, however once removed from the ovary, the granulosa cells are no longer under pituitary control and so rapidly proceed to undergo apoptosis [23], [24], and do not continue to produce the steroid hormones in vitro as they do in vivo [25]. Thus, over time in culture without the addition of exogenous hormones, the impact of steroid hormone levels on microbial growth would not be observed.
Studies have demonstrated that the hormone concentration within maturing follicles is significantly higher than that found in the systemic circulation, as it is governed by the hyaluronan composed cumulus-oocyte complex [2]. In the current study, hyaluronidase-producing species (Propionibacterium spp., Streptococcus spp. and E. coli) were isolated from follicular fluid. The hyaluronidase virulence factor of these species could lead to poor quality cumulus cells via enzymatic hyaluronan degradation, decreased steroid hormone synthesis and ultimately to detrimental effects of these more pathogenic bacteria within the follicle. Our findings indicate that high concentrations of steroid hormones within ovarian follicular fluid can influence bacterial growth in a species-dependent manner.
We demonstrated that follicular fluid supported the survival of viable bacteria for a period of at least 28 weeks. This growth occurred without the addition of supplemental nutrients or the removal of metabolic waste products; such processes that would occur in vivo and may facilitate continual microbial colonisation of the follicular fluid. Gurgan et al. [4] found that filter-sterilised and centrifuged follicular fluid was inhibitory to the Gram-positive bacteria S. aureus, S. agalactiae and L. monocytogenes, as these species did not survive in vitro for longer than four days. However, Gurgan et al. [4] did demonstrate that follicular fluid supported the growth of a range of Gram-negative species and the yeast Candida albicans for up to 15 days post-inoculation. These results are inconsistent with those reported here, where predominantly Gram-positive species survived, most likely as a result of the composition of the follicular fluid, which may have been significantly altered by the filtration and centrifugation prior to inoculation. To the best of our knowledge, our study is the first continuous follicular fluid culture experiment lasting 28 weeks, indicating that follicular fluid is an excellent growth medium for microorganisms.
Many of the bacteria that we detected within follicular fluid have previously been shown to form biofilms in vitro when cultured on vaginal epithelial cells [26], in vivo on the surface of intrauterine devices [27] and in amniotic fluid sludge aspirated from women diagnosed with intrauterine infection [28]. However, despite the range and load of bacteria isolated from follicular fluid, this fluid did not have a turbid appearance, which may suggest that bacteria within the follicle were present predominantly in biofilms, rather than as planktonic bacteria. Thus, the process of trans-vaginal oocyte retrieval may result in puncture and collection of the follicle wall biofilm within the lumen of the aspiration needle, and the subsequent transfer of biofilm components, including bacteria into the follicular fluid at the time of egg retrieval.
The majority of mature biofilms in the present study revealed only a single cultivable species after 10 days, even when two different species of lactobacilli were initially isolated from the follicular fluid prior to in vitro incubation. This may be due to competition amongst the lactobacilli themselves, or because of alterations in adhesion. It has been reported that some bacterial species can co-colonise the surface of urogenital tract cells already colonised by lactobacilli; however, after lactobacilli are established, they can cause other species of bacterial cells to detach from the epithelium, which may offer a defence mechanism by preventing attachment of pathogens to the epithelium [29], [30]. In polymicrobial biofilms, early colonising species often promote the establishment of other species [31], [32]; however, whilst the initial interactions may be synergistic, once the biofilm is established, competition between species can result in the dominance of a single species [33]. Quorum sensing, the process by which microorganisms communicate within a population, establishes the overall population size of each representative microbial species and initiates alterations in gene expression. In addition to quorum sensing, microbial growth within the biofilm is also modulated by these metabolic cues [34]. Species production of lactic acid, succinic acid and isobutyric acid has been reported to enhance both the synergistic and competitive interactions between different microbial species within a biofilm. Acid production resulting in a pH shift, often causes a reduction in the microbial diversity, as many species are acid intolerant [35]. We hypothesise that the predominance of monomicrobial in vitro biofilms reported in this study might therefore be due to the lactic acid and H2O2 production by Lactobacillus spp.
Studies of biofilms have reported that bacteria can exist in a viable, but non-cultivable state [36]. It is therefore possible that cultures of 10-day biofilms detected only those species that were actively replicating, whereas molecular techniques targeting 16 S rRNA would be able to detect and quantify all species (both viable and non-viable) present within the biofilm. This study did report that one culture-negative follicular fluid sample did not produce any visible growth on the range of solid agar or in the thioglycollate broth; however sequencing of the 16 S rRNA PCR product identified a sequence matching an uncultured bacterial clone, again highlighting the need for molecular based techniques. To gain further understanding of an individual species contribution to a biofilm, quantitative 16 S rRNA PCR assays could be used to test cultures at various time points, in order to establish growth curves for each individual species and compare culture results to PCR assay results to identify early and late species contributing to the biofilm.
An ovarian follicle has all the characteristics necessary to support the development of a microbial biofilm. Bacterial cells that would contribute to the formation of the biofilm have been detected in this work (see Table 1 and Figure 1). On some biofilm slides there is evidence of polysaccharide accumulation (in the absence of bacterial cells), which shows that there are components of follicular fluid (substrate) that could form a conditioning film to allow microbial attachment to the inside wall of the follicle (substratum). Furthermore, the in vitro development of various grades of biofilms in human follicular fluid (Figure 1) is demonstrated. Mature biofilms are characterised by the development of towers and fluid–filled channels [37], [38]. Mature biofilms reportedly exhibit a variety of phenotypes due to the changes in their three-dimensional structure, occurring in response to changes in cell density, osmolarity, temperature, pH and nutrient supply [36]. We showed that even follicular fluids containing the same bacterial species demonstrated different grades of biofilms and different morphology.
On six biofilm slides, no bacteria were observed, only a conditioning film was present. This could be due to the removal of any bacterial cells (by the PBS rinse prior to staining) present in the early stage of biofilm formation prior to permanent attachment to the conditioning film. Alternatively, the follicle may have been colonised by non-biofilm forming bacterial species. Further studies examining the effect of these biofilm bacterial species on each other would therefore, be beneficial to our understanding of the impact of single species and polymicrobial biofilms on reproductive health outcomes.
The findings reported in this paper have shown that (1) the ovarian steroid hormones (estradiol and progesterone) are capable of modulating the in vitro growth of some microbial species; (2) follicular fluid supports the long-term survival of microorganisms; and (3) bacteria isolated from follicular fluid can form biofilms in vitro. Further characterisation of the microorganisms detected in follicular fluid and their metabolites will increase our understanding of the effects of follicular fluid microorganisms on oocyte quality, on IVF fertilisation and pregnancy rates, and on early pregnancy events. Knowledge of the microorganisms present within this anatomical niche may lead to an improved understanding of ovarian resistance to infection and also on IVF outcomes.
Acknowledgments
The authors wish to thank the Wesley Monash IVF Service consulting IVF specialists Doctors John Chenoweth, Stephen Baines, Stephen Cook, Ross Turner and Dana Moisuc who collected the clinical specimens. Our thanks also to the IVF scientists Marta Gutierrez and Pan Ouk who aliquotted follicular fluid samples; the IVF administration co-ordinator Jo-Anne O’ Connor for facilitating site visits to the clinic for data collection and the IVF nurse coordinators Cheryl Morton, Angela Banning, Karen Dever, Kara Carter and Tanya Wallace for enrolling patients in this study and assisting with retrospective collation of IVF outcome data. We also are most grateful to Audrey Partenan, Jann Heynes and April Peteru-Barnard for transferring specimens and storing them at the Wesley Research Institute Tissue Bank.
Funding Statement
This work was supported by a Wesley Research Institute Grant. Laboratory work was performed in the John and Wendy Thorsen Women’s Health Laboratory at the Wesley Research Institute. The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
References
- 1. Edwards RG (1974) Follicular fluid. J Reprod Fertil 37: 189–219. [DOI] [PubMed] [Google Scholar]
- 2. Shimada H, Kasakura S, Shiotani M, Nakamura K, Ikeuchi M, et al. (2001) Hypocoagulable state of human preovulatory ovarian follicular fluid: role of sulfated proteoglycan and tissue factor pathway inhibitor in the fluid. Biol Reprod 64: 1739–1745. [DOI] [PubMed] [Google Scholar]
- 3. Stepanovic S, Djukic S, Veljkovic M, Arsic B, Garalejic E (2003) Antimicrobial activity of human follicular fluids. Gynecol Obstet Investig 56: 173–178. [DOI] [PubMed] [Google Scholar]
- 4. Gurgan T, Urman B, Diker KS, Delilbasi L, Kisnisci HA (1993) Human follicular fluid from pre-ovulatory follicles in patients undergoing in-vitro fertilization inhibits the in-vitro growth of Gram-positive microorganisms. Hum Reprod 8: 508–510. [DOI] [PubMed] [Google Scholar]
- 5. Cottell E, McMorrow J, Lennon B, Fawsy M, Cafferkey M, et al. (1996) Microbial contamination in an in vitro fertilization-embryo transfer system. Fertil Steril 66: 776–780. [DOI] [PubMed] [Google Scholar]
- 6. Pelzer ES, Allan JA, Cunningham K, Mengersen K, Allan JM, et al. (2011) Microbial colonization of follicular fluid: alterations in cytokine expression and adverse assisted reproduction technology outcomes. Hum Reprod 26: 1799–1812. [DOI] [PubMed] [Google Scholar]
- 7. Nijland R, Hall MJ, Burgess JG (2010) Dispersal of biofilms by secreted, matrix degrading, bacterial DNase. PLoS One 5: e15668. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Kushnir MM, Naessen T, Kirilovas D, Chaika A, Nosenko J, et al. (2009) Steroid profiles in ovarian follicular fluid from regularly menstruating women and women after ovarian stimulation. Clin Chem 55: 519–526. [DOI] [PubMed] [Google Scholar]
- 9. Loret de Mola JR GJ, Hecht BR, Babbo CJ, Friedlander MA (1999) Gonadotropins induce higher active renin levels in the follicular fluid of normal and hyperstimulated cycles. Gynecol Endocrinol 13: 155–160. [DOI] [PubMed] [Google Scholar]
- 10.Speroff L, Fritz MA (2005) Clinical Gynecologic Endocrinology and Infertility. Philadelphia: Lippincott Williams & Wilkins.
- 11.Allison DG, Sutherland IW (1984) A staining technique for attached bacteria and its correlation to extracellular carbohydrate production. Journal of Microbiological Methods: 93–99.
- 12. Simmons WL, Bolland JR, Daubenspeck JM, Dybvig K (2007) A stochastic mechanism for biofilm formation by Mycoplasma pulmonis . J Bacteriol 189: 1905–1913. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Klausen M, Aaes-Jorgensen A, Molin S, Tolker-Nielsen T (2003) Involvement of bacterial migration in the development of complex multicellular structures in Pseudomonas aeruginosa biofilms. Mol Microbiol 50: 61–68. [DOI] [PubMed] [Google Scholar]
- 14. Klausen M, Heydorn A, Ragas P, Lambertsen L, Aaes-Jorgensen A, et al. (2003) Biofilm formation by Pseudomonas aeruginosa wild type, flagella and type IV pili mutants. Mol Microbiol 48: 1511–1524. [DOI] [PubMed] [Google Scholar]
- 15. Sanchez MC, Llama-Palacios A, Blanc V, Leon R, Herrera D, et al. (2011) Structure, viability and bacterial kinetics of an in vitro biofilm model using six bacteria from the subgingival microbiota. J Periodontal Res 46: 252–260. [DOI] [PubMed] [Google Scholar]
- 16. Brabin L, Roberts SA, Fairbrother E, Mandal D, Higgins SP, et al. (2005) Factors affecting vaginal pH levels among female adolescents attending genitourinary medicine clinics. Sex Transm Infect 81: 483–487. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Brabin L, Fairbrother E, Mandal D, Roberts SA, Higgins SP, et al. (2005) Biological and hormonal markers of chlamydia, human papillomavirus, and bacterial vaginosis among adolescents attending genitourinary medicine clinics. Sex Transm Infect 81: 128–132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Raz R, Stamm WE (1993 ) A controlled trial of intravaginal estriol in postmenopausal women with recurrent urinary tract infections. N Engl J Med 329: 753–756. [DOI] [PubMed] [Google Scholar]
- 19. Jakobsson T, Forsum U (2008) Changes in the predominant human Lactobacillus flora during in vitro fertilisation. Ann Clin Microbiol Antimicrob 7: 14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Swidsinski A, Dorffel Y, Loening-Baucke V, Mendling W, Schilling J, et al. (2010) Dissimilarity in the occurrence of Bifidobacteriaceae in vaginal and perianal microbiota in women with bacterial vaginosis. Anaerobe 16: 478–482. [DOI] [PubMed] [Google Scholar]
- 21. Verhelst R, Verstraelen H, Claeys G, Verschraegen G, Van Simaey L, et al. (2005) Comparison between Gram stain and culture for the characterization of vaginal microflora: definition of a distinct grade that resembles grade I microflora and revised categorization of grade I microflora. BMC Microbiol 5: 61. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Hyman RW, Fukushima M, Diamond L, Kumm J, Giudice LC, et al. (2005) Microbes on the human vaginal epithelium. Proc Natl Acad Sci U S A 102: 7952–7957. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Quirk SM, Cowan RG, Harman RM (2006) The susceptibility of granulosa cells to apoptosis is influenced by oestradiol and the cell cycle. J Endocrinol 189: 441–453. [DOI] [PubMed] [Google Scholar]
- 24. Makrigiannakis A, Coukos G, Blaschuk O, Coutifaris C (2000) Follicular atresia and luteolysis. Evidence of a role for N-cadherin. Ann N Y Acad Sci 900: 46–55. [DOI] [PubMed] [Google Scholar]
- 25. Hill GA, Osteen KG (1989) Follicular fluid steroid content and in vitro steroid secretion by granulosa-lutein cells from individual follicles among different stimulation protocols for in vitro fertilization-embryo transfer. J In vitro Fert Embryo Transf 6: 201–206. [DOI] [PubMed] [Google Scholar]
- 26.Patterson JL, Stull-Lane A, Girerd PH, Jefferson KK (2009) Analysis of adherence, biofilm formation, and cytotoxicity suggest a greater virulence potential of Gardnerella vaginalis relative to other bacterial vaginosis-associated anaerobes. Microbiology. [DOI] [PMC free article] [PubMed]
- 27. Pruthi V, Al-Janabi A, Pereira BJ (2003) Characterization of biofilm formed on intrauterine devices. Indian J Med Microbiol 21: 161–165. [PubMed] [Google Scholar]
- 28.Romero R, Schaudinn C, Kusanovic JP, Gorur A, Gotsch F, et al.. (2008) Detection of a microbial biofilm in intraamniotic infection. Am J Obstet Gynecol 198: 135 e131–135. [DOI] [PMC free article] [PubMed]
- 29. Spurbeck RR, Arvidson CG (2008) Inhibition of Neisseria gonorrhoeae epithelial cell interactions by vaginal Lactobacillus species. Infect Immun 76: 3124–3130. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Vielfort K, Sjolinder H, Roos S, Jonsson H, Aro H (2008) Adherence of clinically isolated lactobacilli to human cervical cells in competition with Neisseria gonorrhoeae . Microbes Infect 10: 1325–1334. [DOI] [PubMed] [Google Scholar]
- 31. Jakubovics NS (2010) Talk of the town: interspecies communication in oral biofilms. Mol Oral Microbiol 25: 4–14. [DOI] [PubMed] [Google Scholar]
- 32. Jakubovics NS, Kolenbrander PE (2010) The road to ruin: the formation of disease-associated oral biofilms. Oral Dis 16: 729–739. [DOI] [PubMed] [Google Scholar]
- 33. Periasamy S, Kolenbrander PE (2009) Mutualistic biofilm communities develop with Porphyromonas gingivalis and initial, early, and late colonizers of enamel. J Bacteriol 191: 6804–6811. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Kreth J, Vu H, Zhang Y, Herzberg MC (2009) Characterization of hydrogen peroxide-induced DNA release by Streptococcus sanguinis and Streptococcus gordonii . J Bacteriol 191: 6281–6291. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Li Y, Ku CY, Xu J, Saxena D, Caufield PW (2005) Survey of oral microbial diversity using PCR-based denaturing gradient gel electrophoresis. J Dent Res 84: 559–564. [DOI] [PubMed] [Google Scholar]
- 36. Fux CA, Costerton JW, Stewart PS, Stoodley P (2005) Survival strategies of infectious biofilms. Trends Microbiol 13: 34–40. [DOI] [PubMed] [Google Scholar]
- 37. Fey PD, Olson ME (2010) Current concepts in biofilm formation of Staphylococcus epidermidis . Future Microbiol 5: 917–933. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Fey PD (2010) Modality of bacterial growth presents unique targets: how do we treat biofilm-mediated infections? Curr Opin Microbiol 13: 610–615. [DOI] [PMC free article] [PubMed] [Google Scholar]