Abstract
Purpose
One of the major drawbacks of peritoneal dialysis (PD) is catheter migration and dysfunction. Preventing catheter migration is one of the main concerns. We compared laparoscopic internal fixation method with open surgical method for catheter migration rates.
Methods
From January 2008 to August 2009, PD catheters were inserted by laparoscopic fixation (LF) method in 22 patients and by open surgery (OS) in 32 patients. Clinical data were reviewed retrospectively. The frequency of migration, peritonitis, and other complications were compared. Catheter and patient survival rates were also compared.
Results
The mean age and sex ratio were not different between groups. Mean follow-up duration was 29.1 months in LF group and 26.1 months in OS group. More patients in LF group (27.3%) had history of laparotomy than in OS group (3.1%) (P = 0.01). The mean operation time was significantly longer in LF group (101.6 ± 30.4 minutes) than in OS group (72.4 ± 26.03 minutes) (P = 0.00). The cumulative incidence of catheter migration was 65.6% in OS group and 13.6% in LF group (P = 0.00). Migration-free catheter survival was higher in LF group (P = 0.001). There were no differences in complication rates between groups. Overall catheter survival was similar (P = 0.93). Patient survival rate at 2 years was not different (P = 0.13).
Conclusion
Laparoscopic internal fixation of continuous ambulatory peritoneal dialysis catheter significantly reduces migration rates without any addition of complications. Also, laparoscopic technique did not incur patient morbidity or mortality despite the requirement for general endotracheal anesthesia and longer operation time. Therefore, internal fixation can be afforded safely in patients with previous abdominal surgery as either a salvage or preventive measure in patients with repeated catheter migration.
Keywords: CAPD, Catheter, Laparoscopy, Fixation, Migration
INTRODUCTION
Continuous ambulatory peritoneal dialysis (CAPD) has been performed in patients with end-stage renal disease [1,2]. The advantages of CAPD are low cost, technical simplicity, improved patient mobility and independence, better control of hypertension, and fewer dietary restrictions [3,4]. A successful PD program is quite dependent on the proper placement and maintenance of the dialysis catheter [5]. The traditional and common method for placement of PD catheter is open surgical method through a mini-laparotomy incision using a malleable stylet [6]. Other insertion techniques include peritoneoscopic or laparoscopic guidance with different incisions and numbers of ports [7-9]. In recent years, laparoscopic surgery has found a wider use in peritoneal catheter placement with various techniques. Wright et al. [7] prospectively compared laparoscopic and open placement of dialysis catheter and found no difference in complication rates, catheter survival, pain scores, or length of stay. However, several authors have found a benefit to laparoscopic guidance, although consensus statements have not favored a specific technique [6,10]. Potential complications related to PD catheter include dysfunction frequently due to migration, leak, exit site or peritoneal infection, and intraabdominal injury or bleeding. Among them, catheter migration is one of the most frustrating complications resulting in dialysis failure and catheter removal. One of the most common procedures for migrated catheter salvage is laparoscopic procedure [11]. We hypothesized that the laparoscopic internal fixation of PD catheter to anterior abdominal wall may decrease catheter complications caused by catheter migration.
METHODS
From January 2008 to August 2009, PD catheters were inserted in 54 patients with end-stage renal disease. It was our principle to adopt open surgery as a primary method. Open surgical method was used in 32 patients under local anesthesia. Laparoscopic internal fixation method was used in 22 patients under general anesthesia. Laparoscopic technique was preferentially used for patients requiring catheter salvage, previous abdominal surgery and willingness to undergo laparoscopic surgery. Laparoscopic surgery was done under general anesthesia. All procedures were undertaken by one surgeon. Informed consents were obtained before any surgical procedures. Kidney-ureter-bladder (KUB) was checked daily after operation during the index admission, then monthly for a subsequent 6 months. Thereafter, KUB was checked every two or three months depending on the patient's visit. KUB was checked whenever catheter dysfunction was identified. Catheter migration was determined by abdominal radiography as deviation of the catheter tip outside the pelvic cavity. Peritonitis was defined as dialysate count of >100 cells/mm3 with >50% being polymorphonuclear leukocytes. The frequency of migration, peritonitis, and other catheter related complications were compared between the two groups. Migration-free and overall catheter survivals were compared. Patient survival rate at 2 years was also compared. Clinical data were collected retrospectively including patients' demographics, complications, and catheter outcomes.
Description of surgical procedures
Double cuffed coiled catheter was used in all patients. Exit site was created at the left lateral abdominal skin by transverse incision. Upward convex subcutaneous tunnel was created to bury the catheter up to the exit site. Dialysis usually was instituted 2 weeks after operation.
Laparoscopic internal fixation method
While two ports were usually used, an additional 3rd port was inserted for catheter salvage procedures as required. A 10-mm longitudinal incision was made at just below the umbilicus. A 12-mm port was placed through this incision. Then, pneumoperitoneum was created by carbon dioxide insufflation, and a 30 degree laparoscope was introduced into the abdominal cavity through the 12-mm port. A left lower quadrant incision was made at the predetermined site that was selected by measuring with the external length of the catheter, which was used as catheter exit site. A 5-mm port was placed in this incision under visual guidance by laparoscope. After the 5-mm port was inserted, the whole peritoneal cavity was inspected. Then, the laparoscope was transferred through the 5-mm port. A double-cuffed, curled PD catheter on a malleable metal stylet was introduced through the 12-mm port under visual guidance. Malleable stylet guidance enabled saving another port or made it easier to place the catheter tip into the pouch of Douglas. Another 2-mm suprapubic stab incision was made for internal fixation of the catheter. The 2-0 nylon was inserted with a needle passer through the stab incision and the needle passer was pulled out to leave the nylon freely in the abdominal cavity (Fig. 1). Then the needle passer was reinserted through a different point within the incision to grasp and pull out the 2-0 nylon around the catheter and stylet (Fig. 2). The distance between the anchor site and the catheter tip was the range of free motion. An atraumatic forceps was introduced through the 5-mm port to grasp the catheter tip and the camera was inserted through 10-mm port beside the catheter. While the catheter tip was located at the pelvic cavity and maintained under camera guidance, the pneumoperitoneum was deflated. Loose tying of the nylon at the end of the operation simply completed the fixation maneuver to the anterior abdominal wall (Fig. 3). The peritoneal cuff was anchored to a preloaded polypropylene suture at the umbilical port site. The subcutaneous tunnel was created from 12-mm port site to 5-mm port site using a Faller stylet.
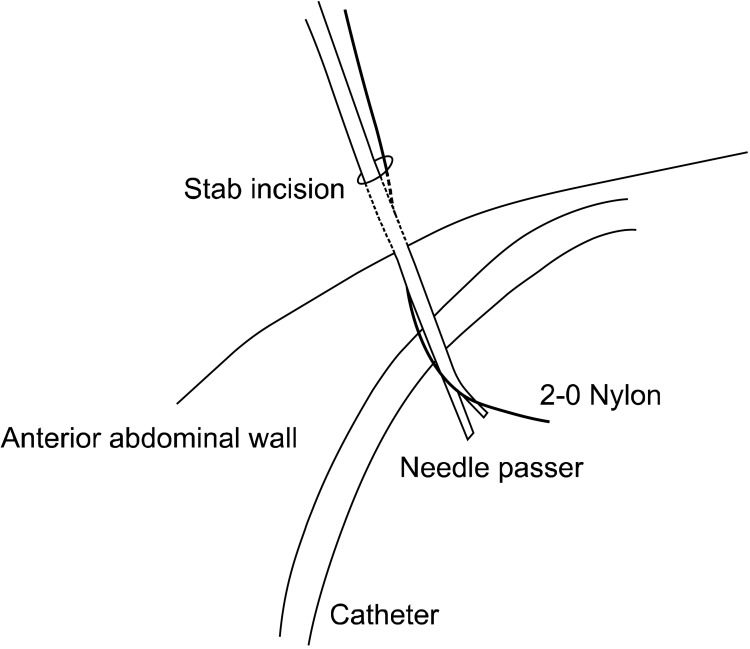
Fig. 1.
Introduction of fixation thread. A tiny stab incision is made at just above the pubic bone. The appropriate point can be determined by pressing the abdominal wall under laparoscopic inspection. The needleless 2-0 nylon suture was inserted with a needle passer into peritoneal space under laparoscopic inspection at just above the pubic bone. Care should be taken not to injure the bladder. The needle passer is pulled out after releasing the suture freely in the peritoneal space.
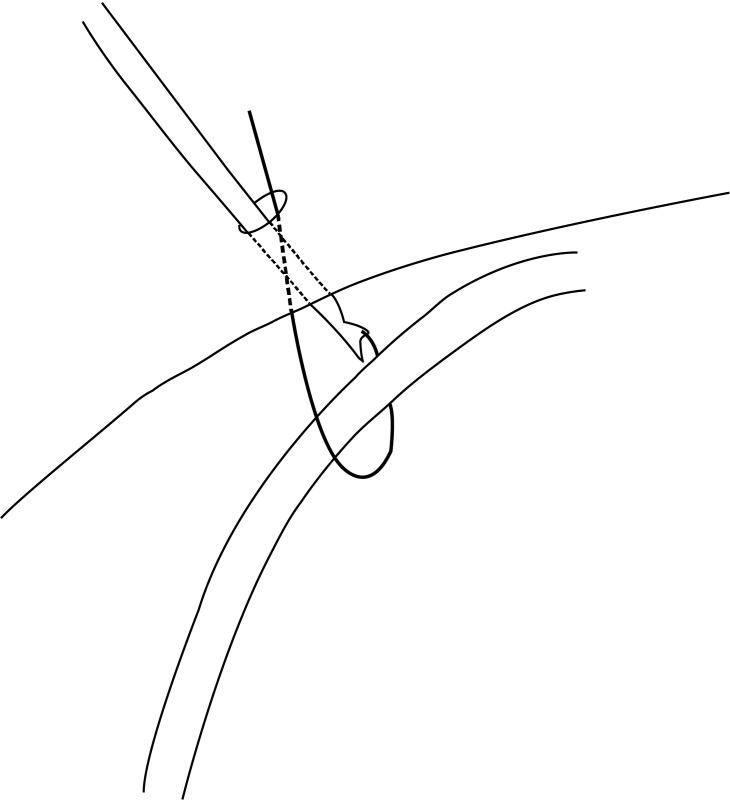
Fig. 2.
Capturing fixation thread around the catheter. The needle passer was inserted through a different point at a different angle to grasp the 2-0 nylon around the catheter. Loosely tying the thread completes the fixation. The knot is buried at the subcutaneous layer.
Fig. 3.
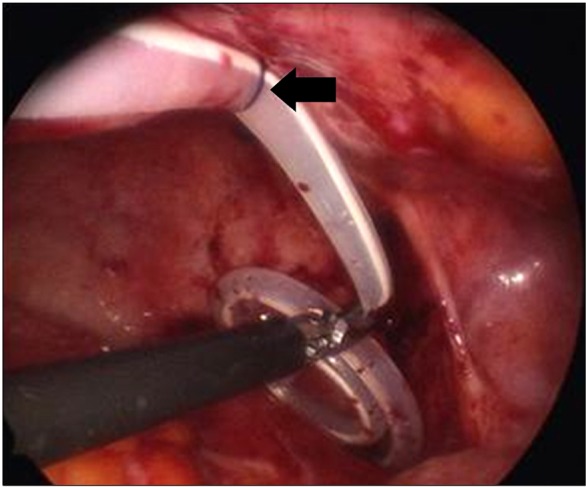
Internal view of the fixed catheter. The catheter is anchored to the anterior abdominal wall by a single thread of non-absorbable suture material (arrow).
Open surgical placement of the PD catheter
Left rectus muscle splitting method was used in open surgery (OS) group under local anesthesia. The anterior rectus fascia was opened longitudinally, and the muscle was split up to the posterior fascia. A small opening was made in the posterior fascia and peritoneum. A purse-string suture with 2-0 polypropylene including peritoneum and Linear Alba was made. Using a stylet for guidance, the two-cuffed, curled catheter was introduced and directed to the pelvis. Free flow of saline into and out of the peritoneal cavity was checked and pelvic X-ray was taken to confirm the position of the catheter tip. Thereafter, the purse-string suture was tightened and tied. The free end of the purse-string suture was secured with the peritoneal cuff at two points. The catheter was brought through a subcutaneous tunnel to the previously chosen exit site.
Statistical analysis
SPSS ver. 16.0 (SPSS Inc., Chicago, IL, USA) was used for analysis. The independent sample t-test was used for continuous variables and they were expressed by mean ± standard deviation. The chi-square test was used for discrete variables. Kaplan-Meier analysis was used for survival analysis. All results were considered significant at a P-value less than 0.05.
RESULTS
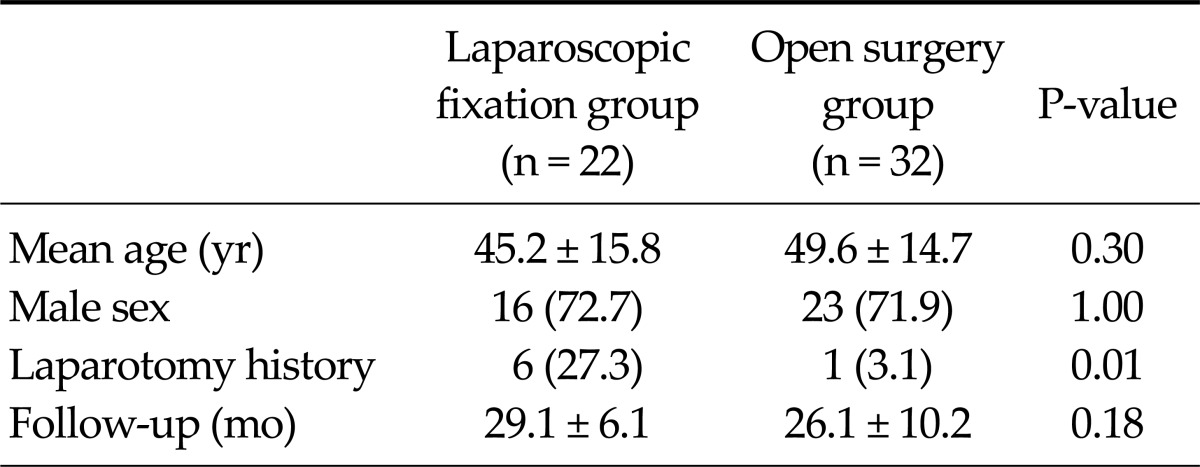
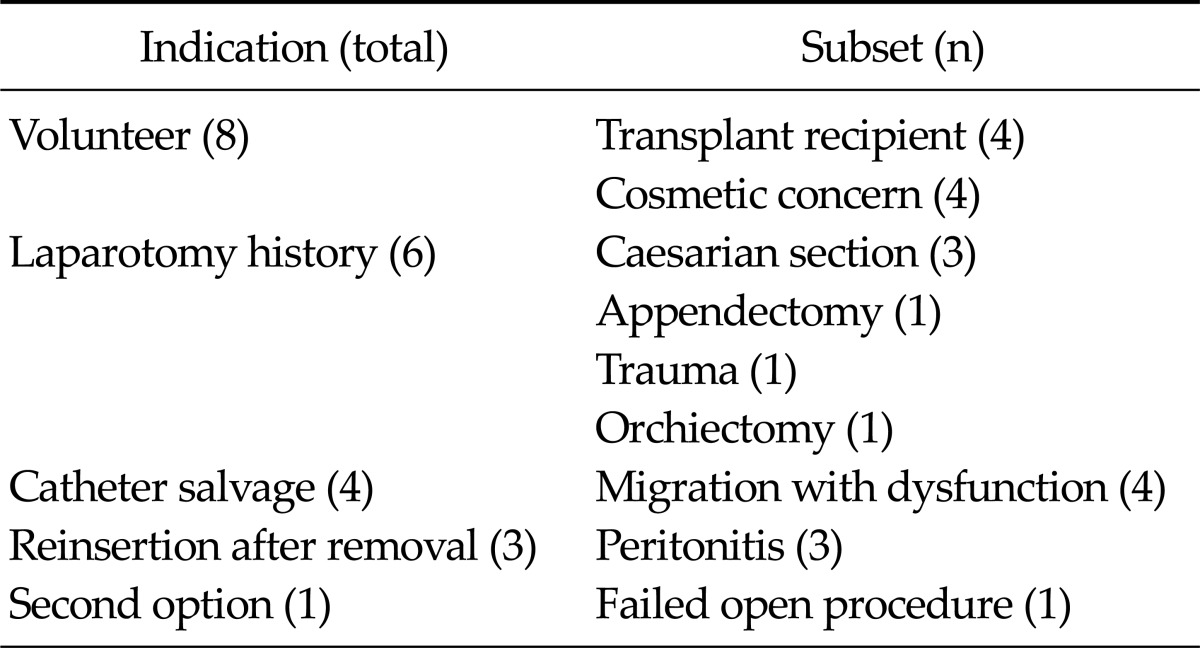
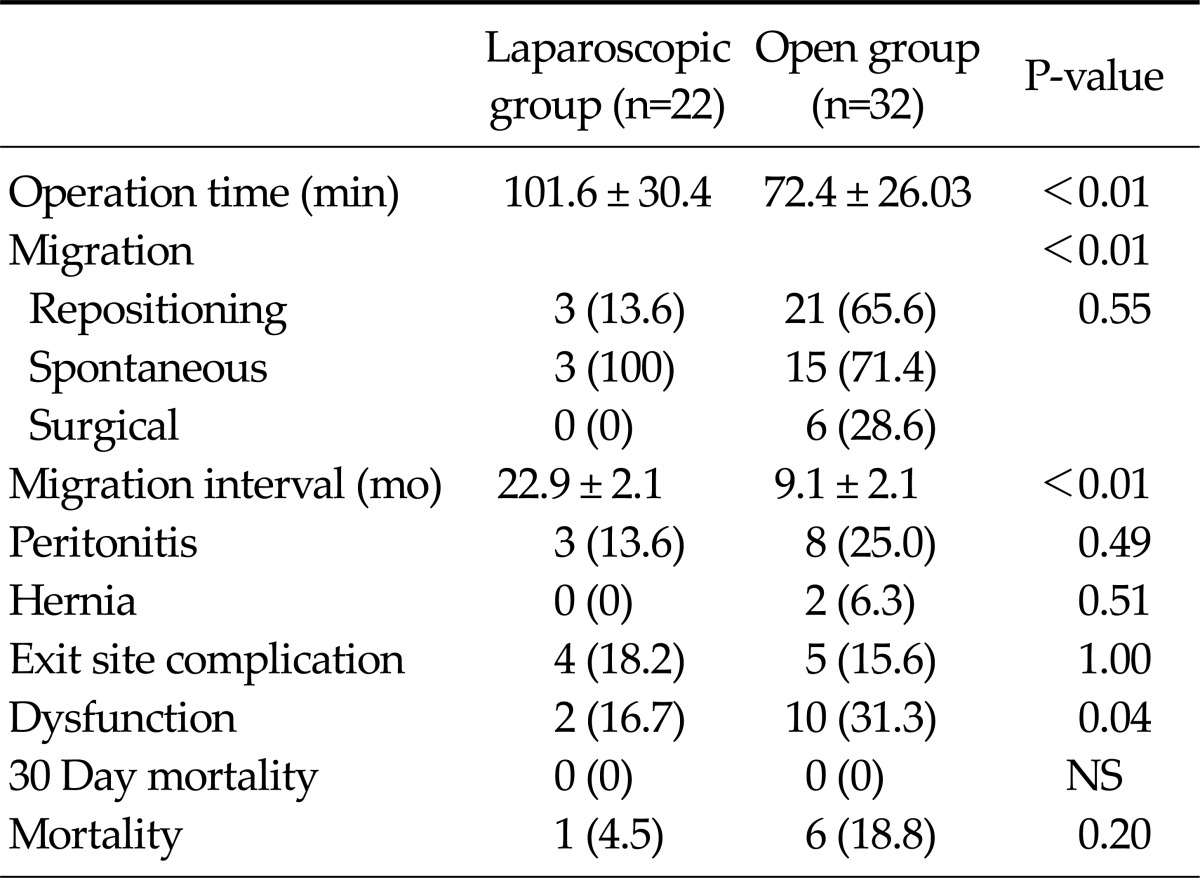
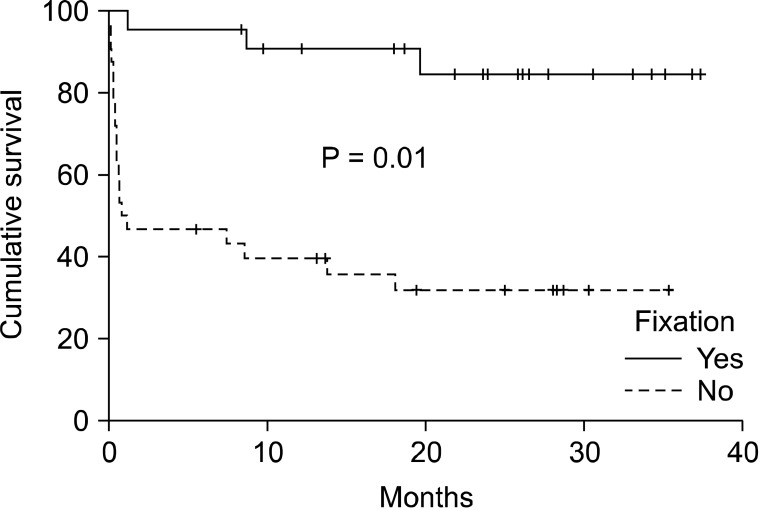
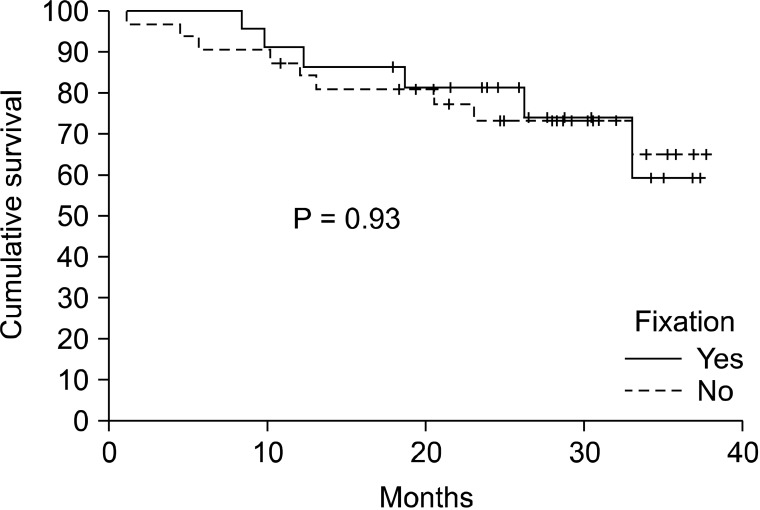
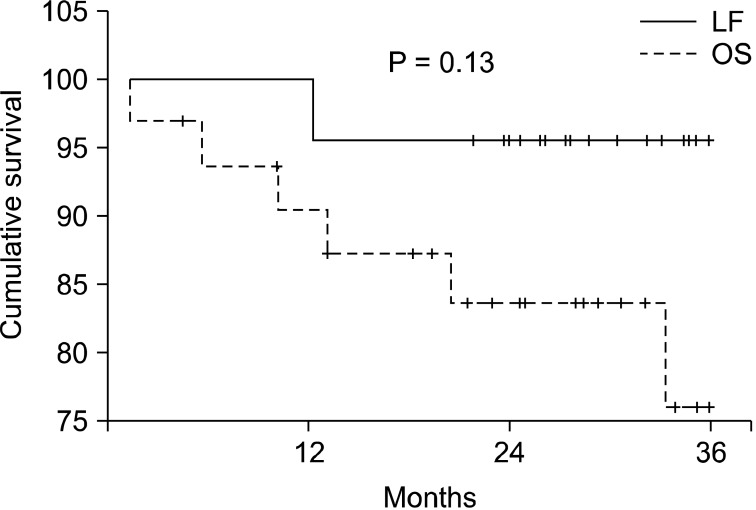
The mean age was 45.2 ± 15.8 years (range, 19 to 69 years) in laparoscopic fixation (LF) group and 49.6 ± 14.7 years (range, 23 to 73 years) in OS group, respectively (P = 0.30). The sex ratio was similar between groups (P = 1.0). The mean follow-up duration was 29.1 ± 6.1 months in LF group and was 26.1 ± 10.2 months in OS group (P = 0.18). One patient in OS group was lost to follow up. Baseline characteristics other than laparotomy history were comparable between groups. Laparotomy history was higher in LF group (27.3%) than in OS group (3.1%) (P = 0.01) (Table 1). Laparoscopic procedure was used in conditions as follows; voluntary request (n = 8), presence of laparotomy history (n = 6), catheter salvage intention (n = 4), catheter reinsertion after catheter related complications (n = 3), failed open procedure (n = 1) (Table 2). The mean operation time was significantly longer in LF group (101.6 ± 30.4 minutes) than in OS group (72.4 ± 26.03 minutes) (P < 0.01). The cumulative incidence of catheter migration was 13.6% in LF group and 65.6% in OS group (P < 0.01) (Table 3). All migrated catheters repositioned spontaneously in LF group, but surgical correction was required in six patients (28.6%) in OS group (P = 0.55). The mean migration interval was 22.9 ± 2.1 months (range, 1.2 to 37.3 months) in LF group and 9.1 ± 2.1 months (range, 0.01 to 35.3 months) in OS group (P < 0.01). Odds ratio for migration between groups was 12.1 (P = 0.01). Migration-free catheter survival rate was significantly better in LF group than OS group (P = 0.01) (Fig. 4). However, overall catheter survival was not different between groups (P = 0.93) (Fig. 5). Peritonitis occurred in 3 patients (13.6%) in the OS group, and 8 patients (25.0%) in the LF group (P = 0.49). Exit site complication was 18.2% in LF group and 15.6% in OS group (P = 1.00). There were two cases of hernia in OS group (1 inguinal and 1 incisional), but there was no hernia in LF group (P = 0.51). Catheter dysfunction occurred in 2 patients in LF group and ten patients in OS group (P = 0.04). There was no 30-day or in-hospital mortality in both groups. One patient in LF group and six patients in OS group died during follow up (Table 3). Patient survival rate at 2 years was not different between groups (Fig. 6).
Table 1.
Patient demographics
Values are presented as mean ± SD or number (%).
Table 2.
Indication of laparoscopic surgery
Table 3.
Clinical outcomes
Values are presented as mean ± SD or number (%).
NS, not significant.
Fig. 4.
Migration-free catheter survival. Laparoscopic internal fixation showed lower migration-free catheter survival than open method (P = 0.01).
Fig. 5.
Catheter survival. There was no difference in overall catheter survival rate between groups (P = 0.93).
Fig. 6.
Patient survival. There was no difference in overall patient survival at 2 years between groups (P = 0.13). LF, laparoscopic fixation; OS, open surgery.
DISCUSSION
PD is an alternate, affordable, feasible, and readily available form of dialysis. Nevertheless, complications such as outflow obstruction, catheter-related infection, and dialysate leak remain problematic [12]. Ash [13] indicated that successful PD depends more on placement technique than on catheter design. Therefore, appropriate selection of surgical technique and adjunctive procedures to minimize related complications are mandatory. Current available techniques for catheter placement are categorized as follows: 1) percutaneous method, 2) open surgical method, 3) peritoneoscopic method, 4) laparoscopic method [12]. Although percutaneous method seems quick and simple, it carries a risk of visceral injury, particularly in patients with laparotomy history [14,15]. Among various techniques, only laparoscopic method enables not only internal fixation but also other adjunctive procedures enhancing catheter longevity or catheter salvage [16,17]. With the aid of laparoscopy, one can rescue a malfunctioning catheter, place a new catheter, or simultaneously perform other laparoscopic procedures [18-20]. Currently, the ideal method for inserting PD catheter remains debatable. Some reports favor laparoscopic technique [18,21,22], others do not [23,24]. A recent prospective randomized study reported that laparoscopic group had lower migration rates [12]. But, they indicated that laparoscopic technique had longer operative time than open surgery [12]. In our study, we found that more operative time is required for laparoscopic technique because of adjunctive procedures. Despite a longer operation time, we couldn't find additional morbidities attributable to elongated procedure time. The PD catheter may undergo spontaneous migration within the abdominal cavity, reducing dialysate flux. These problems may occur immediately or several months after the insertion [25,26]. Several studies have demonstrated that securing of the catheter tip in the pelvis reduces the incidence of catheter obstruction. Catheter fixation is easily accomplished by a laparoscopic approach using techniques which vary from suturing to stapling the suture loop to the pelvic peritoneum [5]. Comert et al. [27] reported a laparoscopic technique for the placement of PD catheter through a preperitoneal tunnel and found advantages of this method including accurate placement, preperitoneal fixation, and immediate use of the catheter for routine PD. Since internal fixation reduces free motion range of the catheter, the migration rate might be lower and the possibility of spontaneous return might be higher. As expected, migration rate was lower and all the migrated catheters returned spontaneously to the desired position in LF group in our study.
What limits this study is that it is neither a randomized nor a prospective one. In addition, factors affecting catheter migration were not included in this study. It requires further investigation to compare clinical outcomes between laparoscopic groups with or without internal fixation in well-designed prospective study.
In conclusion, laparoscopic internal fixation of PD catheter significantly reduces migration rates and migration interval without any addition of catheter related complications. Also, laparoscopic internal fixation improved migration-free catheter survival rates. Furthermore, laparoscopic technique incurs no patient morbidity and mortality despite the requirement of general endotracheal anesthesia and longer operation time. Therefore, internal fixation can be afforded safely in patients with previous abdominal surgery as a primary option or as a salvage or preventive measure in patients with repeated catheter migration events.
ACKNOWLEDGEMENTS
This work was financially supported by a grant from Gachon University Gil Medical Center to Jinmo Kang, MD.
Footnotes
This work was presented as oral presentation at the 62nd Annual Congress of the Korean Surgical Society.
No potential conflict of interest relevant to this article was reported.
References
- 1.Bailie GR, Eisele G. Continuous ambulatory peritoneal dialysis: a review of its mechanics, advantages, complications, and areas of controversy. Ann Pharmacother. 1992;26:1409–1420. doi: 10.1177/106002809202601115. [DOI] [PubMed] [Google Scholar]
- 2.Steinberg SM, Cutler SJ, Nolph KD, Novak JW. A comprehensive report on the experience of patients on continuous ambulatory peritoneal dialysis for the treatment of end-stage renal disease. Am J Kidney Dis. 1984;4:233–241. doi: 10.1016/s0272-6386(84)80098-0. [DOI] [PubMed] [Google Scholar]
- 3.Kimmelstiel FM, Miller RE, Molinelli BM, Lorch JA. Laparoscopic management of peritoneal dialysis catheters. Surg Gynecol Obstet. 1993;176:565–570. [PubMed] [Google Scholar]
- 4.Kittur DS, Gazaway PM, Abidin MR. Laparoscopic repositioning of malfunctioning peritoneal dialysis catheters. Surg Laparosc Endosc. 1991;1:179–182. [PubMed] [Google Scholar]
- 5.Soontrapornchai P, Simapatanapong T. Comparison of open and laparoscopic secure placement of peritoneal dialysis catheters. Surg Endosc. 2005;19:137–139. doi: 10.1007/s00464-004-8156-y. [DOI] [PubMed] [Google Scholar]
- 6.Dombros N, Dratwa M, Feriani M, Gokal R, Heimburger O, Krediet R, et al. European best practice guidelines for peritoneal dialysis. 4 Continuous ambulatory peritoneal dialysis delivery systems. Nephrol Dial Transplant. 2005;20(Suppl 9):ix13–ix15. doi: 10.1093/ndt/gfi1118. [DOI] [PubMed] [Google Scholar]
- 7.Wright MJ, Bel'eed K, Johnson BF, Eadington DW, Sellars L, Farr MJ. Randomized prospective comparison of laparoscopic and open peritoneal dialysis catheter insertion. Perit Dial Int. 1999;19:372–375. [PubMed] [Google Scholar]
- 8.Leblanc M, Ouimet D, Pichette V. Dialysate leaks in peritoneal dialysis. Semin Dial. 2001;14:50–54. doi: 10.1046/j.1525-139x.2001.00014.x. [DOI] [PubMed] [Google Scholar]
- 9.Gadallah MF, Pervez A, el-Shahawy MA, Sorrells D, Zibari G, McDonald J, et al. Peritoneoscopic versus surgical placement of peritoneal dialysis catheters: a prospective randomized study on outcome. Am J Kidney Dis. 1999;33:118–122. doi: 10.1016/s0272-6386(99)70266-0. [DOI] [PubMed] [Google Scholar]
- 10.Gokal R, Alexander S, Ash S, Chen TW, Danielson A, Holmes C, et al. Peritoneal catheters and exit-site practices toward optimum peritoneal access: 1998 update. (Official report from the International Society for Peritoneal Dialysis) Perit Dial Int. 1998;18:11–33. [PubMed] [Google Scholar]
- 11.Yilmazlar T, Kirdak T, Bilgin S, Yavuz M, Yurtkuran M. Laparoscopic findings of peritoneal dialysis catheter malfunction and management outcomes. Perit Dial Int. 2006;26:374–379. [PubMed] [Google Scholar]
- 12.Jwo SC, Chen KS, Lee CC, Chen HY. Prospective randomized study for comparison of open surgery with laparoscopic-assisted placement of Tenckhoff peritoneal dialysis catheter: a single center experience and literature review. J Surg Res. 2010;159:489–496. doi: 10.1016/j.jss.2008.09.008. [DOI] [PubMed] [Google Scholar]
- 13.Ash SR. Chronic peritoneal dialysis catheters: overview of design, placement, and removal procedures. Semin Dial. 2003;16:323–334. doi: 10.1046/j.1525-139x.2003.16062.x. [DOI] [PubMed] [Google Scholar]
- 14.Simkin EP, Wright FK. Perforating injuries of the bowel complicating peritoneal catheter insertion. Lancet. 1968;1:64–66. doi: 10.1016/s0140-6736(68)90066-4. [DOI] [PubMed] [Google Scholar]
- 15.Devine H, Oreopoulos DG, Izatt S, Mathews R, DeVeber GA. The permanent Tenckhoff catheter for chronic peritoneal dialysis. Can Med Assoc J. 1975;113:219–221. [PMC free article] [PubMed] [Google Scholar]
- 16.Giannattasio M, De Maio P, La Rosa R, Balestrazzi A. Videolaparoscopy: a new alternative for implantation of peritoneal catheters in ESRD patients with previous abdominal surgeries. Perit Dial Int. 1996;16:96–97. [PubMed] [Google Scholar]
- 17.Brandt CP, Franceschi D. Laparoscopic placement of peritoneal dialysis catheters in patients who have undergone prior abdominal operations. J Am Coll Surg. 1994;178:515–516. [PubMed] [Google Scholar]
- 18.Jwo SC, Chen KS, Lin YY. Video-assisted laparoscopic procedures in peritoneal dialysis. Surg Endosc. 2003;17:1666–1670. doi: 10.1007/s00464-003-8106-0. [DOI] [PubMed] [Google Scholar]
- 19.Ogunc G, Tuncer M, Ogunc D, Yardimsever M, Ersoy F. Laparoscopic omental fixation technique versus open surgical placement of peritoneal dialysis catheters. Surg Endosc. 2003;17:1749–1755. doi: 10.1007/s00464-002-8586-3. [DOI] [PubMed] [Google Scholar]
- 20.Carrillo SA, Ghersi MM, Unger SW. Laparoscopic-assisted peritoneal dialysis catheter placement: a microinvasive technique. Surg Endosc. 2007;21:825–829. doi: 10.1007/s00464-006-9148-x. [DOI] [PubMed] [Google Scholar]
- 21.Yun EJ, Meng MV, Brennan TV, McAninch JW, Santucci RA, Rogers SJ. Novel microlaparoscopic technique for peritoneal dialysis catheter placement. Urology. 2003;61:1026–1028. doi: 10.1016/s0090-4295(02)02589-x. [DOI] [PubMed] [Google Scholar]
- 22.Ogunc G. Videolaparoscopy with omentopexy: a new technique to allow placement of a catheter for continuous ambulatory peritoneal dialysis. Surg Today. 2001;31:942–944. doi: 10.1007/s005950170042. [DOI] [PubMed] [Google Scholar]
- 23.Daschner M, Gfrorer S, Zachariou Z, Mehls O, Schaefer F. Laparoscopic Tenckhoff catheter implantation in children. Perit Dial Int. 2002;22:22–26. [PubMed] [Google Scholar]
- 24.Batey CA, Crane JJ, Jenkins MA, Johnston TD, Munch LC. Mini-laparoscopy-assisted placement of Tenckhoff catheters: an improved technique to facilitate peritoneal dialysis. J Endourol. 2002;16:681–684. doi: 10.1089/089277902761403041. [DOI] [PubMed] [Google Scholar]
- 25.Crabtree JH, Fishman A. Laparoscopic omentectomy for peritoneal dialysis catheter flow obstruction: a case report and review of the literature. Surg Laparosc Endosc Percutan Tech. 1999;9:228–233. [PubMed] [Google Scholar]
- 26.Nielsen PK, Hemmingsen C, Friis SU, Ladefoged J, Olgaard K. Comparison of straight and curled Tenckhoff peritoneal dialysis catheters implanted by percutaneous technique: a prospective randomized study. Perit Dial Int. 1995;15:18–21. [PubMed] [Google Scholar]
- 27.Comert M, Borazan A, Kulah E, Ucan BH. A new laparoscopic technique for the placement of a permanent peritoneal dialysis catheter: the preperitoneal tunneling method. Surg Endosc. 2005;19:245–248. doi: 10.1007/s00464-003-9302-7. [DOI] [PubMed] [Google Scholar]