Abstract
Cutaneous malignant melanoma of the breast can be divided into two categories: primary and metastatic lesions. Cutaneous malignant melanoma of the breast is a rare tumor, accounting for less than 5% of all malignant melanomas. Clinical features and diagnostic methods of primary cutaneous malignant melanoma of the breast are similar to those arising from other cutaneous areas. Treatment of choice is wide local excision with adequate resection margin according to tumor thickness. Sentinel lymph node biopsy should be performed because the presence of lymph node metastasis is the most important prognostic factor. There have been only limited reports involving primary cutaneous malignant melanoma of the breast. Thus, we report a case of primary cutaneous malignant melanoma in a 59-year-old woman with a review of the recent literature.
Keywords: Breast neoplasms, Melanoma, Sentinel lymph node biopsy
INTRODUCTION
Malignant melanoma rarely affects the breast, accounting for less than 5% of all malignant melanomas [1,2]. Malignant melanoma of the breast has various manifestations: primary cutaneous melanoma, primary glandular melanoma, metastatic melanoma, and in-transit metastases to the breast [1]. Differential diagnosis of these manifestations is very important in deciding on treatment strategies.
Primary cutaneous malignant melanoma of the breast shows similar clinical features to melanomas arising from other cutaneous areas. It follows different metastatic patterns than do primary carcinomas of the breast and require a different therapeutic approach [3]. Wide local excision with sentinel lymph node (SLN) biopsy is the most important therapeutic modality in preventing local recurrence. Mastectomy offers no advantage over wide local excision of the primary lesion. Malignant melanoma is an immunogenic tumor and adjuvant immunotherapy is indicated in high risk patients [4]. Common metastatic sites are brain, lung, liver and overall prognosis is very poor in metastasis [5].
Herein, we report a case of primary cutaneous malignant melanoma of the breast in a 59-year-old woman and discuss the clinicopathologic features and treatments in correlation to the literature data.
CASE REPORT
A 59-year-old woman was admitted with a black pigmented skin lesion in the right breast. She mentioned that the lesion had appeared at birth but grew rapidly and bled recently. She had no past history of malignancy and no family history of breast carcinoma. The lesion was 2.0 × 1.5 cm in size and located on the periareolar skin in the upper inner quadrant of the right breast which is not associated any breast mass (Fig. 1). The axillary lymph node was not palpated and there was no nipple discharge or retraction.
Fig. 1.

A 59-year-old woman with a 2.0 × 1.5 cm sized and an ulcerative pigmented skin lesion in the right breast.
She underwent incisional biopsy a week earlier at a local breast clinic and was diagnosed with malignant melanoma. The specimen was an ulcerative, pigmented lesion, measuring 1.0 × 0.6 cm in size and 0.25 cm in thickness (pT3b). The depth of invasion according to Clark's classification was level IV.
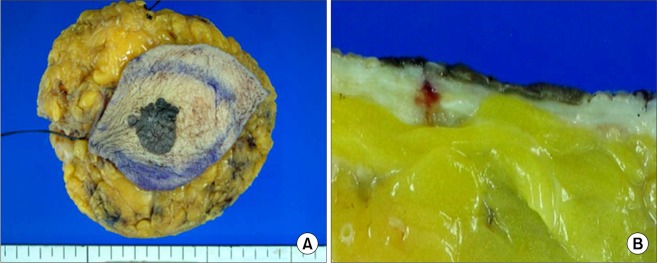
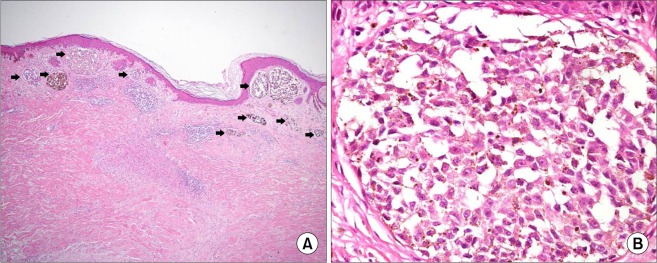
She was examined for evidence of metastatic malignant melanoma. Careful examination of the other skin and mucous membranes revealed no areas suggestive of a malignant melanoma. Mammography (MMG) revealed a dense breast. Breast ultrasonography (US) and magnetic resonance imaging showed normal findings. Brain computed tomography (CT) and positron emission tomography-CT showed no evidence of metastasis. She underwent wide local excision of the lesion, including removal of normal appearing skin and underlying subcutaneous tissue to provide a safety margin; and subsequent sentinel lymph node biopsy (SLNBx) using the technetium (Tc)-99m phytate was performed. Grossly, the specimen revealed a sharply defined, black pigmented lesion, measuring 1.9 × 1.6 cm in size including normal skin 2 cm apart from the tumor margin and subcutaneous tissue (Fig. 2A). The cut surface revealed a superficial pigmented lesion without ulceration (Fig. 2B). The specimen was fixed in 10% neutral-buffered formalin. Paraffin embedded tissue sections were prepared and stained with hematoxylin and eosin. Microscopic findings showed intraepidermal tumor cells and nests that were laterally spreading in a pagetoid manner and tumor nests invaded the superficial dermis 0.12 cm in thickness (pT2a) (Fig. 3A). Tumor cells often had large nuclei and nucleoli and abundant cytoplasm with brown-black pigments (Fig. 3B). The resection margins were free of tumor cells and there was no regional lymph node metastasis (pN0). The final pathologic stage considering incisional biopsy report was IIB (T3bN0M0) according to the 7th edition of the American Joint Committee on Cancer classification [6]. Additional chemotherapy and radiotherapy were not performed. Three years after surgery, the patient is alive and shows no signs of local recurrence or distant metastasis.
Fig. 2.
Gross finding (A) and cut surface (B) of the right breast lesion after wide local excision.
Fig. 3.
Microscopic findings of the right breast lesion. (A) Low power view reveals many tumor cell nests located in superficial dermis just beneath the epidermis (arrows). Tumor cell nests are arranged in laterally spreading pattern and some of them are brown-black pigmented (H&E, ×40). (B) High power view reveals tumor cells with large nuclei, prominent nucleoli and abundant cytoplasm with brown-black pigments (H&E, ×400).
DISCUSSION
The incidence of malignant melanoma has risen sharply over the last decade and can occur anywhere on the body. It occurs most commonly on the extremities in females and on the trunk in males [6]. Malignant melanoma of the breast is classified into primary melanoma of the breast skin or gland, and metastatic melanoma to the breast from an extramammary site [4]. Cutaneous malignant melanoma of the breast is a rare tumor, accounting for less than 5% of all malignant melanomas and primary cutaneous malignant melanoma of the breast is particularly rare [7]. Kurul et al. [1] reported that cutaneous malignant melanoma showed different manifestations in the breast not only at initial presentation but also during the follow-up periods of each patient. To date, several cases of primary cutaneous malignant melanoma of the breast have been reported in the west but have not yet been reported in Korea.
The etiology of primary cutaneous malignant melanoma is not fully understood. Exposure to solar ultraviolet radiation is the major environmental risk factor and the presence of host factors including skin pigmentation, sensitivity to the sun and large numbers of nevus are strongly associated [8]. Bono et al. [9] reported cutaneous malignant melanoma prefers the upper inner quadrant of the breast and this finding is consistent with an etiologic role for sun exposure. In the present case, the lesion was also located in the upper inner quadrant of the right breast.
In comparison to primary cutaneous malignant melanomas arising from other areas, neither the symptoms nor the physical findings of primary cutaneous malignant melanoma of the breast present any characteristic pattern [1,7]. However, in cutaneous malignant melanoma of the breast, MMG and/or US should be obtained to reveal the breast lesion that is considered a metastatic lesion. In our case, all radiologic examinations of the breast showed normal findings. Occasionally, pigmented Paget's disease of the breast might mimic malignant melanoma [10]. If malignant melanoma occurs in the nipple-areolar area, phagocytosis of melanin by Paget's cells can distinguish the malignant melanoma from Paget's disease of the breast.
In our case, the patient underwent incisional biopsy at a local breast clinic. However, incisional biopsy should never be performed to establish the diagnosis of cutaneous malignant melanoma because it would be confusing in determining the pathologic stage. Therefore, if a suspicious lesion is found, excisional biopsy should be performed. For an accurate diagnosis of primary cutaneous malignant melanoma, a comprehensive physical examination should be performed to find the evidence of malignant melanoma at other locations. Also, any history of previous removal of pigmented lesions must be investigated and reviewed if present.
The management of primary cutaneous malignant melanoma of the breast requires special consideration in view of the rarity of the disease and the intricate anatomy of the breast. Surgery is the main therapeutic option and wide local excision with a margin containing normal appearing skin and underlying subcutaneous tissue is the standard of treatment. Adequate excision margin is considered a 1 to 2 cm clearance according to tumor thickness; 1 cm clearance is adequate for lesions <1 mm thickness and 2 cm for >2 mm thickness [2]. In our case, a 2 cm excision margin was adequate according to the 1.2 mm thickness. Mastectomy does not improve the survival rate obtained by breast conserving surgery [2,3]. Because regional lymph node metastasis is the most important prognostic factor, all patients with malignant melanoma of the breast should undergo SLNBx. It is rare for it to spread systemic metastasis without first passing through the SLN. Papachristou et al. [3] reported that lesions located below 3 cm from clavicle metastasized to the axillary lymph nodes regardless of gender or location and lesions located above 3 cm, assessment on the cervical region has been recommended. The incidence of lymph node metastases ranges from 6% for patients with 1 mm cutaneous malignant melanomas to 35% in patients with 4 mm [2]. A positive SLN is associated with Clark level IV depth, tumor regression and ulceration, young age, higher mitotic rate, male and axial location [2].
Cutaneous malignant melanoma is an immunogenic tumor and high dose interferon alpha has gained approval for adjuvant treatment of malignant melanoma. Interferon has shown to improve relapse-free survival but a definitive benefit in overall survival is debatable [4]. Though radiotherapy decreases the locoregional failure from 30-50% to 10-20%, a survival benefit remains vague because of low radiosensitivity in melanoma cells [4]. In contrast to breast carcinoma, a significance of chemotherapy or hormonal therapy is unclear.
Despite various aggressive systemic treatments, cutaneous malignant melanoma is possibly a life-threatening disease in which regional or distant metastasis may develop. The most common metastatic site is the brain, for which dacarbazine is considered the standard treatment [5]. The important prognostic factors are regional lymph node metastasis, primary tumor thickness, and ulceration [5,6]. During follow-up visits, particular attention should be paid to the importance of breast examination. Not only in visible in-transit metastasis, but also when there is evidence of mild breast skin abnormalities such as a light blue spot, histological confirmation should be performed.
The rarity of cutaneous malignant melanomas of the breast have made them difficult to evaluate. Moreover, distinguishing whether a cutaneous malignant melanoma of the breast is primary or metastatic is important for the treatment strategies and the overall prognosis. Awareness of unusual cutaneous lesions of the breast is necessary to determine the optimal treatment modalities on this rare disease.
Footnotes
No potential conflict of interest relevant to this article was reported.
References
- 1.Kurul S, Tas F, Buyukbabani N, Mudun A, Baykal C, Camlica H. Different manifestations of malignant melanoma in the breast: a report of 12 cases and a review of the literature. Jpn J Clin Oncol. 2005;35:202–206. doi: 10.1093/jjco/hyi068. [DOI] [PubMed] [Google Scholar]
- 2.Alzaraa A, Sharma N. Primary cutaneous melanoma of the breast: a case report. Cases J. 2008;1:212. doi: 10.1186/1757-1626-1-212. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Papachristou DN, Kinne DW, Rosen PP, Ashikari R, Fortner JG. Cutaneous melanoma of the breast. Surgery. 1979;85:322–328. [PubMed] [Google Scholar]
- 4.Biswas A, Goyal S, Jain A, Suri V, Mathur S, Julka PK, et al. Primary amelanotic melanoma of the breast: combating a rare cancer. Breast Cancer. 2010 Oct 27; doi: 10.1007/s12282-010-0231-8. [Epub]. http://dx.doi.org/10.1007/s12282-010-0231-8. [DOI] [PubMed] [Google Scholar]
- 5.Bassi F, Gatti G, Mauri E, Ballardini B, De Pas T, Luini A. Breast metastases from cutaneous malignant melanoma. Breast. 2004;13:533–535. doi: 10.1016/j.breast.2004.02.006. [DOI] [PubMed] [Google Scholar]
- 6.Balch CM, Gershenwald JE, Atkins MB, Buzaid AC, Cascinelli N, Cochran AJ, et al. Melanoma of the skin. In: Edge SB, Byrd DR, Compton CC, Fritz AG, Greene FL, Trotti A, editors. AJCC cancer staging manual. 7th ed. New York: Springer; 2010. pp. 325–344. [Google Scholar]
- 7.Lee YT, Sparks FC, Morton DL. Primary melanoma of skin of the breast region. Ann Surg. 1977;185:17–22. doi: 10.1097/00000658-197701000-00003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.English DR, Armstrong BK, Kricker A, Fleming C. Sunlight and cancer. Cancer Causes Control. 1997;8:271–283. doi: 10.1023/a:1018440801577. [DOI] [PubMed] [Google Scholar]
- 9.Bono A, Baldi M, Maurichi A, Tomatis S. Distribution of melanoma on breast surface suggests its etiology. Int J Cancer. 2003;105:434. doi: 10.1002/ijc.11084. [DOI] [PubMed] [Google Scholar]
- 10.Mitchell S, Lachica R, Randall MB, Beech DJ. Paget's disease of the breast areola mimicking cutaneous melanoma. Breast J. 2006;12:233–236. doi: 10.1111/j.1075-122X.2006.00247.x. [DOI] [PubMed] [Google Scholar]