Abstract
Adult intussusception is a rare entity. Most adult intussusceptions require surgical intervention because they have a high rate of pathologic leading point. Mandatory laparotomy and en bloc resection is recommended in colonic intussusceptions due to the possibility of malignancy. We report herein 3 cases of adult colonic intussusceptions. The intussusceptions were located in the sigmoid and rectum, which were managed by laparoscopic colectomy. Case 1 was managed by laparoscopic anterior resection and diverting ileostomy combined with perineal reduction. Perineal approach facilitated laparoscopic reduction. In case 2, intraoperative colonoscopy was performed to determine the distal resection margin. Intraoperative colonoscopy showed edematous bowel mucosa as well as leading point after reduction of intussusceptions. Case 3 showed asymptomatic transient rectorectal colonic intussusceptions.
Keywords: Adult, Intussusception, Colon, Laparoscopy
INTRODUCTION
Intussusception rarely occurs in adults, comprising 0.003 to 0.02% of all hospital admissions [1]. Colonic intussusceptions are less common than small bowel intussusceptions and are mostly caused by malignant neoplasms [1,2]. In children, intussusceptions is treated by pneumatic or hydrostatic reduction in 80% of all patients. However, there are pathologic leading points in 90% of all adult intussusceptions and surgical resection is required for adult cases [3]. Laparoscopic surgery requires smaller incisions than open surgery and postoperative pain is less severe than in open surgery. In addition, laparoscopic colectomy for curable cancers is not inferior to open surgery in terms of long-term oncologic endpoints [4]. Here we describe laparoscopic anterior resection in 2 patients with sigmoidorectal intussusceptions and 1 patient with a rectorectal intussusceptions.
CASE REPORTS
Case 1
A 49-year-old woman was admitted to Hallym University Sacred Heart Hospital with a chief complaint of intermittent rectal bleeding and abdominal discomfort for 2 days. Digital rectal examination revealed a mass in the rectum about 7 cm proximal to the anal verge. Simple abdominal X-rays showed no abnormal bowel gas pattern. In laboratory tests, her neutrophil percentage was mildly elevated to 80.4% and her carcinoembryonic antigen level was slightly increased to 5.34 ng/mL. Flexible sigmoidoscopy revealed an irregular mass at the prolapsed mucosal head of the rectum (Fig. 1). Abdominal computed tomography (CT) demonstrated a sigmoidorectal intussusception, probably due to a sigmoid colon cancer (Fig. 2). There was no evidence of distant metastasis or peritoneal seeding.
Fig. 1.
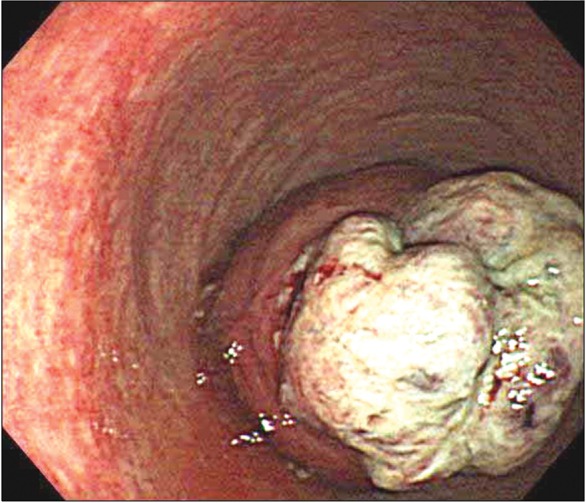
Flexible sigmoidoscopy showed the mass lesion 7 cm from the anal verge and the partial downward displacement of involved bowel.
Fig. 2.
Computed tomography scans showed bowel-within-bowel mesenteric fat and vessel appearance (arrow) with wall thickening representing tumor (arrowhead).
We planned for a laparoscopic resection because her abdomen was not distended. The patient took 2 L of polyethylene glycol (PEG) solution for bowel preparation the day before operation. Although the simple abdomen X-rays did not show any bowel obstruction, the patient could not defecate anything after taking PEG. On laparoscopic exploration, we identified a distended bowel containing PEG and a sigmoidorectal intussusception. The sigmoid colon telescoped into the lumen of the rectum and the mesentery of the sigmoid colon was trapped between the involved bowels. It was difficult to establish a dissection plane of the mesentery. In order to continue laparoscopic surgery, reduction of the sigmoid was needed. The operator pulled out the proximal bowel using a laparoscopic bowel grasper and the assistant push up the invaginated distal end from the anus with a lubricated sponge-on-the-stick. We monitored this process by laparoscopy. The intussuscepted segment was partially restored and the sigmoid mesentery could finally be identified. It seemed that there was no bowel necrosis or perforation. The inferior mesenteric vessels were divided and ligated using hemolock clips. A 5-cm suprapubic vertical midline incision was made for specimen extraction. After the resection of the proximal segment, we found out stool impaction within the end of the proximal segment. It is thought that the stool impaction caused bowel obstruction and failure of bowel preparation with PEG solution. We performed laparoscopic anterior resection and diverting ileostomy because of the incomplete bowl preparation. After two months, the ileostomy was taken down without any complication. The pathologic finding was a 6 × 4 × 4-cm mucinous adenocarcinoma with moderate differentiation. Invasion depth was pericolic adipose tissue and there were no lymphatic or vascular emboli. The regional lymph nodes were negative for cancer cells. Six years have elapsed after the first operation, and the patient shows neither regional recurrence nor distant metastasis.
Case 2
A 41-years-old woman visited our institute. Her chief complaints were diarrhea and intermittent hematochezia. Simple abdominal X-rays showed a nonspecific bowel gas pattern. On physical examination, the patient showed periumbilical tenderness. Laboratory tests showed no abnormal findings. For the evaluation of tenderness, we first performed abdomino-pelvic CT. CT scans demonstrated that a sigmoidorectal intussusception and a intraluminal enhancing polypoid mass at the distal portion of the sigmoid colon (Fig. 3). The CT scans did not reveal any ischemic sites and obstruction. We performed a flexible sigmoidoscopy after enema through the anus. Sigmoidoscopy showed a polypoid mass with nodular mucosa in the rectum 10 cm from the anal verge, as well as a partial downward displacement of the proximal bowel (Fig. 4). Sigmoidoscopic forceps biopsy was carried out from the mass. During air inflation of sigmoidoscope, the intussusception was partially restored. After the eventually conducted sigmoidoscopy, the patient's abdominal discomfort was improved. Preoperative bowel preparation was performed using PEG solution. Laparoscopic anterior resection was then performed. During the laparoscopy, we could not find the intussusception site or the tumor lesion because there were no serosa deformities. We were thus forced to carry out intraoperative colonoscopy in order to find the tumor location. Intraoperative colonoscopy revealed that a 5-cm polypoid mass located 17 cm from the anal verge as well as an approximately 5-cm segmented mucosal edema and congestion (Fig. 5). This lesion was thought to be a telescoped lesion. We marked distal resection margin using laparoscopic clipping with the help of the colonoscopic light (Fig. 6). Although the sigmoid colon was distended immediately after intraoperative colonoscopy, decompression was completed using a rectal tube. We completed the laparoscopic anterior resection successfully. Histopathological examination revealed a 6 × 4.5-cm villotubular adenoma with focal high-grade dysplasia. The patient recovered uneventfully and was then discharged without any complications.
Fig. 3.
Computed tomography scans demonstrated enlargement of the colorectal wall and fat within the intussusceptum, and air within the intussuscipiens.
Fig. 4.
Flexible sigmoidoscopy showed invaginated bowel with polypoid mass lesion about 10 cm from anal verge.
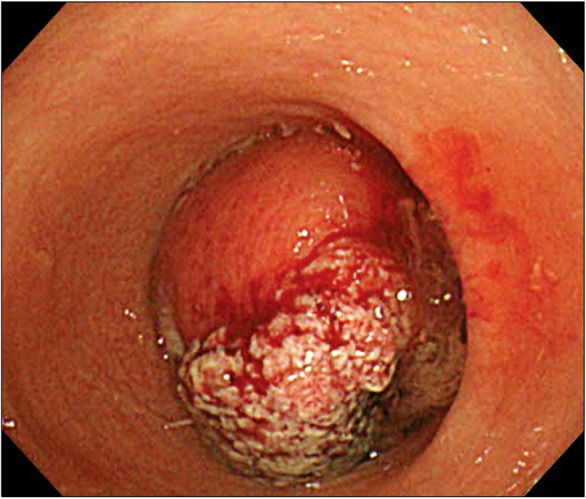
Fig. 5.
Bowel mucosa after reduction of intussusception. Intraoperative colonoscopy showed polypoid mass about 17 cm from anal verge (arrow) and mucosal edema and congestion in intussuscipiens (arrowthead).
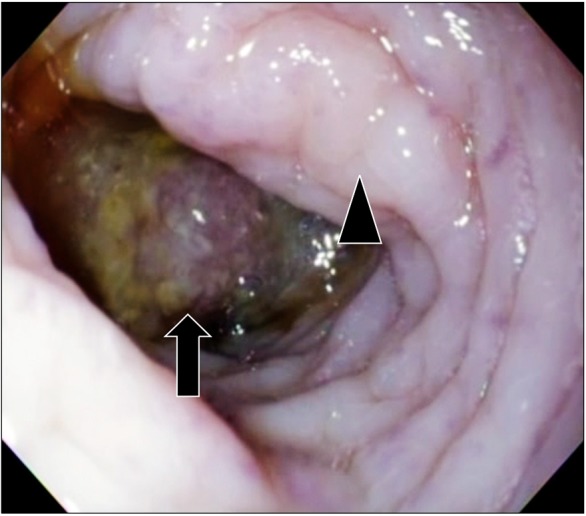
Fig. 6.
Hemolock clip (arrow) and colonoscopic light (arrowhead) at distal portion of mass.
Case 3
A 55-year-old man visited a local clinic for a routine medical checkup. A general practitioner performed a colonoscopy and detected a mass in the rectum. Colonoscopic biopsy was performed and pathology revealed a well-differentiated adenocarcinoma. The patient was referred to our hospital for further evaluation and treatment. At our institute, the patient underwent abdomen-pelvic CT. The CT scans showed rectorectal intussusceptions with irregular enhancing wall thickening at the upper rectum and we could not evaluate perirectal fat invasion due to the intussuscepted state (Fig. 7). Bowel preparation was carefully performed with 4 L of PEG solution the day after CT because the patient had no abdominal symptoms. Bowel preparation and conventional laparoscopic low anterior resection were uneventful. Laparoscopy did not show an intussusception lesion but a distorted serosa in the rectum which was suggestive of cancer. We performed intraoperative colonoscopy to in order to indentify mucosal abnormalities, such as edema or congestion. There were no mucosal abnormalities around the mass. We thought that the intussuseception had been restored by itself and that the lesion might be a transient intussusception. Histopathology revealed a 5 × 4.5-cm well-differentiated adenocarcinoma. The tumor invaded subserosa, and there were lymphatic and vascular emboli. There were no lymph node metastases.
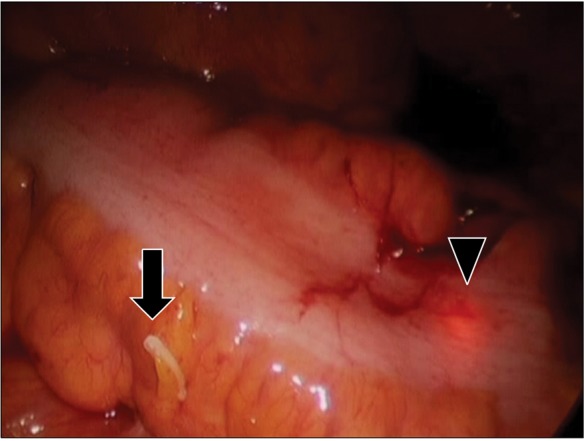
Fig. 7.
Computed tomography scans demonstrated irregular enhancing wall thickening at upper rectum with rectorectal intussusception.
DISCUSSION
Intussusceptions in adults are different from those in children in that pathologic leading points are found in 70 to 90% of all adult intussusceptions. En block resection without reduction is recommended for adult intussusceptions because of the possibility of malignancy. If reduction is attempted during operation in patients with malignant tumors, it can lead to intraluminal seeding or venous embolization of malignant cells [1,2]. From an oncologic viewpoint, minimal of manipulation of the tumor cells is appropriate. However, reduction should be considered depending on the location of the intussusception. Azar and Berger [1] have proposed that resection with primary anastomosis can be achieved on right-side intussusceptions in unprepared bowels but the construction of colostomies should be performed on left-side or rectosigmoid lesions. When intussusception involves the lower rectum, operation without reduction requires extensive surgeries, such as abodminoperitoneal excision or very low anterior resection [2]. In contrast, when a sigmoidorectal intussusception is reduced, unnecessary extensive operations sacrificing the anus, such as abdominoperineal excisions, can be avoided [5]. Permanent colostomy affects the quality of life. Though previous studies reported the possibility of intraluminal seeding and venous emboli after reduction of colonic intussusceptions, there is not yet definite evidence to support this possibility because of the scarcity of clinical cases. Our first patient showed no recurrences or distant metastases 6 years after operation. Reduction of sigmoidorectal intussuscpetions that can avoid unnecessary resections and permanent colostomies has clinical implications for the quality of life.
Not all cases of colonic intussusceptions can be reduced. The location of intutssusceptions should be considered in performing reduction. It would be easier to reduce sigmoidorectal or rectorectal intussusceptions than ileo-colic or colo-colic intussusceptions. This may be because pushing an intussusception into the peritoneum can make reduction easier. We found in case 1 that the abdominal approach only allows for pulling the intussusception. The laparoscopic intraabdominal approach carries a high risk of tearing of the colon wall by traction. The simultaneous peritoneal approach allows for easier reduction. There have been several reports on the combined approach for reduction of sigmoidorectal intussusceptions [5,6].
The sigmoidoscopic approach to the intussusceptions site is able to be useful as in case 2. In our case, partial reduction was achieved during air inflation of a sigmoidoscope, and thus patient discomfort was improved. Most patients with intussusceptions have chronic abdominal pain and partial intestinal obstruction [7]. If a patient shows a complete obstruction or ischemic signs, such as fever, rigid abdomen, leukocytosis and nonenhanced bowel wall on contrast CT, sigmoidoscopy should be avoided to prevent bowel perforation. However, when there are no complete obstruction or ischemic signs, flexible sigmoidoscopy may help identify the lesion.
Another problem with reduction is the possibility that the bowel is vital externally but mucosa is necrotized internally [8]. The distal colon of intussusceptions (intussuscipiens) would be too edematous to safely permit primary anastomosis [9]. Intraoperative colonoscopy is useful for identifing the state of bowel mucosa after reduction. We performed intraoperative colonoscopy in order to detect the location of the tumor in case 2. During colonoscopy, mucosal edema and congestion were observed the around the mass caused by intussusception. We marked the resection margin, excluding the congested mucosa, with the help of colonoscopic light. In case 3, we evaluated the mucosal state by intraoperative colonoscopy. It is thought that intra-operative colonoscopy is a useful means of estimating mucosal state and of determining the resection margin.
Complete resection along with lymphatic drainage should be performed due to the possibility of malignancy in all colonic intussusceptions [1]. The validity of laparoscopic oncologic colon surgery has been supported by the results of previous studies [4]. Anatomical knowledge of the mesentery is essential for complete resection along with lymphatic drainage during laparoscopic surgery. In intussusceptions, the proximal bowel is driven distally into the bowel and the mesentery of the involved bowel is trapped. Such anatomic variations make laparoscopic mesenteric dissection more difficult. When of intussusceptions reduction is achieved, the folded mesentery becomes unfolded as in case 1. It is thought that intussusceptions reduction clearly visualizes the mesentery and allows for successful laparoscopic surgery.
Case 3 had a transient rectorectal colonic intussusception. Previous reports have shown that most transient intussusceptions occur in the small bowel in adults [9,10]. However, our case was occurred directly related to a cancer. Most intussusceptions in the small bowel are incidentally discovered and do not cause specific symptoms [9,10]. In our case, the intussusception was also incidentally detected by CT and had no specific symptoms. Our case showed the possibility of transient colonic intussusceptions caused by a cancer. It is thought that our uneventful laparoscopic surgery may be due to spontaneous reduction. If an asymptomatic colonic intussusception is incidentally found, the possibility of transient intussusceptions should be considered.
We conclude that sigmoidrectal or rectorectal intussusceptions can be managed by laparoscopic colectomy combined with perineal reduction. Sigmoidoscopy can reduce rectosigmoid intussusceptions without obstruction or bowel necrosis. After reduction, intraoperative colonoscopy is helpful in evaluating mucosal state. Incidental colonic intussusceptions without abdominal symptoms may be transient and may not be emergent.
Footnotes
No potential conflict of interest relevant to this article was reported.
References
- 1.Azar T, Berger DL. Adult intussusception. Ann Surg. 1997;226:134–138. doi: 10.1097/00000658-199708000-00003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Nagorney DM, Sarr MG, McIlrath DC. Surgical management of intussusception in the adult. Ann Surg. 1981;193:230–236. doi: 10.1097/00000658-198102000-00019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Eisen LK, Cunningham JD, Aufses AH., Jr Intussusception in adults: institutional review. J Am Coll Surg. 1999;188:390–395. doi: 10.1016/s1072-7515(98)00331-7. [DOI] [PubMed] [Google Scholar]
- 4.Fleshman J, Sargent DJ, Green E, Anvari M, Stryker SJ, Beart RW, Jr, et al. Laparoscopic colectomy for cancer is not inferior to open surgery based on 5-year data from the COST Study Group trial. Ann Surg. 2007;246:655–662. doi: 10.1097/SLA.0b013e318155a762. [DOI] [PubMed] [Google Scholar]
- 5.Park KJ, Choi HJ, Kim SH, Han SY, Hong SH, Cho JH, et al. Sigmoidorectal intussusception of adenoma of sigmoid colon treated by laparoscopic anterior resection after spongeon-the-stick-assisted manual reduction. World J Gastroenterol. 2006;12:146–149. doi: 10.3748/wjg.v12.i1.146. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Greenley CT, Ahmed B, Friedman L, Deitte L, Awad ZT. Laparoscopic management of sigmoidorectal intussusception. JSLS. 2010;14:137–139. doi: 10.4293/108680810X12674612015184. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Kim KH, Lee IK, Lee YS, Kim DH, Park JK, An CH, et al. Analysis of the Diagnostic Maneuver and Timing of Operation in Adult Intussusception. J Korean Surg Soc. 2007;73:419–423. [Google Scholar]
- 8.Chang CC, Chen YY, Chen YF, Lin CN, Yen HH, Lou HY. Adult intussusception in Asians: clinical presentations, diagnosis, and treatment. J Gastroenterol Hepatol. 2007;22:1767–1771. doi: 10.1111/j.1440-1746.2007.04907.x. [DOI] [PubMed] [Google Scholar]
- 9.Agha FP. Intussusception in adults. AJR Am J Roentgenol. 1986;146:527–531. doi: 10.2214/ajr.146.3.527. [DOI] [PubMed] [Google Scholar]
- 10.Catalano O. Transient small bowel intussusception: CT findings in adults. Br J Radiol. 1997;70:805–808. doi: 10.1259/bjr.70.836.9486044. [DOI] [PubMed] [Google Scholar]





