Abstract
The induction of ischemic tolerance by preconditioning provides a platform to elucidate endogenous mechanisms of stroke protection. In these studies, we characterize the relationship between hypoxia-inducible factor (HIF), sphingosine kinase 2 (SphK2), and CCL2 in models of hypoxic or pharmacological preconditioning-induced ischemic tolerance. A genetics-based approach using SphK2- and CCL2-null mice showed both SphK2 and CCL2 to be necessary for the induction of ischemic tolerance following preconditioning with hypoxia, the hypoxia-mimetic cobalt chloride, or the sphingosine-1-phosphate (S1P) agonist FTY720. A pharmacologic approach confirmed the necessity of HIF signaling for all three preconditioning stimuli, and showed the SphK/S1P pathway to transduce tolerance via the S1P1 receptor. Additionally, our data suggest significant cross-talk between HIF and SphK2-produced S1P signaling, which together act to upregulate CCL2 expression. Overall, HIF, SphK, S1P, and CCL2 participate in a signaling cascade to induce the gene expression responsible for the stroke-tolerant phenotype established by hypoxic and FTY720 preconditioning. The identification of these common molecular mediators involved in signaling the genomic response to multiple preconditioning stimuli provides several targets for therapeutic manipulation.
Keywords: bioactive lipids, sphingosine-1-phosphate, neuroprotection, chemokines
Introduction
The brain possesses endogenous mechanisms capable of defending itself against ischemic damage. These innate survival pathways can be activated by a paradigm known as preconditioning, whereby exposure to noninjurious stressors trigger changes in gene and protein expression that lead to an ‘ischemia-tolerant’ phenotype. Experimentally, the preconditioning model represents an elegant tool for increasing our understanding of the pathways and mechanisms of endogenous neuroprotection. Hypoxic preconditioning (HPC) is a well-established approach for inducing tolerance to focal and global cerebral ischemia in both neonates and adults. Moreover, HPC not only protects the brain and other tissues from ischemic insults, it also increases resistance to other types of injury as well. Thus, protective mechanisms induced by HPC may provide therapeutic targets for disease intervention beyond just stroke.
The HPC stimulus is typically considered to be propagated by the accumulation/activation of the transcription factor hypoxia-inducible factor (HIF), which binds to hypoxia-responsive elements (HREs) in the promoters of genes. In normoxic conditions, proline residues on the alpha subunits of HIF are continuously hydroxylated by an oxygen-dependent prolyl hydroxylase, and then ubiquitinated by pVHL, which labels it for ongoing rapid degradation by the proteosome. However, inhibition of the HIF prolyl hydroxylase under hypoxic conditions, or by metal chelating “HIF mimetics” like cobalt chloride, stabilize HIF and, in turn, promote the transcription of dozens of genes, the protein products of which enhance cell survival in severely hypoxic or ischemic conditions. Prominent HIF-regulated cytoprotective pathways include vascular endothelial growth factor (VEGF), erythropoietin, and glucose metabolism (Aragones et al. 2009, Correia & Moreira 2010, Semenza 2009).
One molecule that accumulating evidence suggests is regulated by HIF is sphingosine kinase (SphK) (Anelli et al. 2008, Ralph et al. 2004, Schnitzer et al. 2009, Schwalm et al. 2008). Recently, in an adult mouse model of focal stroke, we identified the sphingosine kinase 2 (SphK2) isoform as a necessary mediator of HPC-induced tolerance, in part because of its early upregulation after HPC (Wacker et al. 2009). SphK2 is one of two SphK isoforms that catalyze the phosphorylation of sphingosine to form sphingosine 1-phosphate (S1P), a potent signaling lipid. S1P can then act intracellularly, or extracellularly via autocrine or paracrine activation of five S1P receptors (S1P1-5), to regulate a diverse set of cellular metabolic processes. Each S1P receptor induces unique signaling effects, and thus the cell- and tissue-dependent expression of S1P receptors typically determines the effect S1P will exhibit. Using SphK2-null mice, we have demonstrated that SphK2/S1P signaling is critical to inducing ischemic tolerance in response to HPC (Wacker et al. 2012), a finding recently corroborated by others (Yung et al. 2011). We also recently demonstrated that FTY720, an S1P receptor agonist that is phosphorylated by SphK2, serves as an effective preconditioning stimulus (Wacker et al. 2009), further underscoring a role for S1P signaling in stroke tolerance. However, the intermediate mediators of S1P signaling, the S1P receptor involved, and the regulation of additional cellular processes by S1P related to preconditioning-induced ischemic tolerance, remain to be elucidated.
We recently identified the chemokine CCL2 (also known as monocyte chemoattractant protein-1 [MCP-1]) as essential to the establishment of ischemic tolerance by HPC (Stowe et al. 2012). It was already known that CCL2 can be produced by central nervous system (CNS) astrocytes, microglia, endothelial cells, and neurons, as well as by immune cells; it is best known for its role in inflammatory cell recruitment. However, we found CCL2 mRNA and protein were rapidly upregulated in mouse cortex following HPC, and immunohistochemistry localized this expression to neurons. The primary CCL2 receptor, CCR2, is found on most CNS cell types. CCL2/CCR2 signaling induces angiogenesis in the vasculature (Niu et al. 2008, Stamatovic et al. 2006) and protects against ischemia in the myocardium (Martire et al. 2003). The promoter region for CCL2 contains several binding sites for HIF, which is believed to account for the increased CCL2 expression in response to either hypoxia- or chemically-induced HIF stabilization (Mojsilovic-Petrovic et al. 2007). Furthermore, while studies of cultured endothelium and mast cells suggest CCL2 expression is upregulated by S1P (Chen et al. 2004, Oskeritzian et al. 2008), whether this same signaling pathway is operative in brain, particularly in the context of cerebral ischemic tolerance, is unknown. However, the necessity for both CCL2 and SphK2 in our model of HPC-induced ischemic tolerance (Yung et al. 2011, Wacker et al. 2012, Stowe et al. 2012) led us to hypothesize that HIF, SIP, and CCL2 are part of a signal transduction cascade responsible for the observed neurovascular protection.
Thus, we undertook the present experiments to characterize the functional interrelationships between HIF, SphK2, and CCL2 in models of preconditioning-induced ischemic tolerance. We hypothesized that following HPC, HIF accumulation causes a downstream increase in SphK2 expression, and the S1P so formed acts through the S1P1 receptor to increase CCL2 expression, culminating in the establishment of an ischemia-tolerant phenotype. We also explored this pathway in the setting of pharmacologic preconditioning with cobalt and FTY720, and determined causality and the signaling sequence with both a genetic (SphK2 and CCL2 knockout mice) and pharmacologic (inhibitors of HIF, SphK2, and S1P1) approach. We found that SphK2 and CCL2 signaling is required downstream of hypoxic, cobalt, or FTY720 preconditioning for the induction of stroke tolerance. Additionally, our data suggest cross-talk between HIF and SphK2-generated S1P. Our identification of key mediators participating in the induction of the gene expression changes promoting endogenous neurovascular protection provides several molecular targets for therapeutic preconditioning.
Materials and Methods
Mice
Adult, male mice, 10–15 wks old, were used in all studies. Wildtype C57BL/6 (Jackson Laboratories, SphK2 knockout, and CCL2 knockout mice were used for the genetic knockout experiments in Figure 1. SphK2−/− mice, congenically backcrossed to C57BL/6 mice for at least 7 generations, were provided by Dr. Richard Proia (NIH). CCL2−/−/Cx3CR1+/GFP mice on a C57BL/6 background were used for the CCL2-null studies, courtesy of Dr. Keiko Hirose (Washington University). SW-ND4 mice (Harlan) were used for the HIF, SphK, and S1P1 inhibition experiments shown in Figures 2 and 3. All animals were housed on a 12-hour light/dark cycle with water and food ad libitum. Efforts were made with respect to experimental design to reduce the number of mice used and to minimize stress to the animals. All experimental protocols were approved by the Institutional Animal Care and Use Committee (IACUC) at Washington University and conformed to the National Institutes of Health guidelines for the care and use of animals in research and the ARRIVE guidelines. Surgical procedures were performed using sterile/aseptic techniques and experimental conditions were intermixed to prevent batch effects from affecting a single experimental condition; all analyses were blinded.
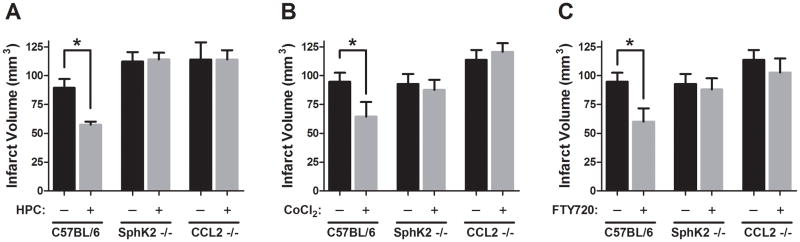
Figure 1. The requirement for SphK2 and CCL2 for preconditioning for ischemic tolerance by hypoxia, cobalt, and the sphingosine analog FTY720.
(A) Previously published data showed that hypoxic preconditioning (HPC) reduces infarct volume 24 h after transient middle cerebral artery occlusion (tMCAO) in wildtype (C57Bl/6) mice, and the loss of such protection in SphK2 knockout (data from (Wacker et al. 2012)) and CCL2 knockout mice (data from (Stowe et al. 2012)). (B) Cobalt (CoCl2) preconditioning reduces infarct volume 24 h after tMCAO in wildtype (C57Bl/6) mice, but this protection is not achieved in SphK2 knockout or CCL2 knockout mice. (C) FTY720 preconditioning also reduces infarct volume 24 h after tMCAO in wildtype (C57Bl/6) mice, but as with hypoxia and cobalt, tolerance is not realized in SphK2 knockout or CCL2 knockout mice. Data represent mean±SEM. N=5–13 per group. (*) P<0.05 between groups.
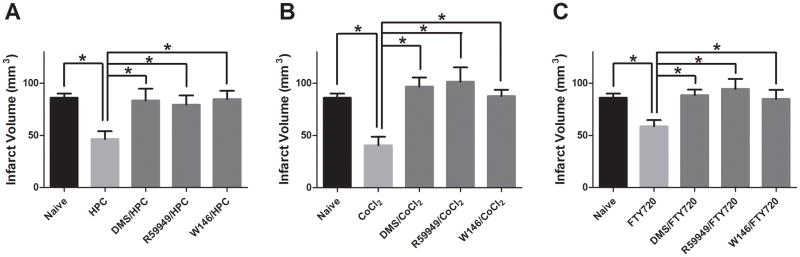
Figure 2. The requirement for SphK-, HIF-, and S1P1-based signaling in preconditioning by hypoxia, cobalt, and FTY720.
(A) Hypoxic preconditioning (HPC) reduces infarct volume 24 h after transient middle cerebral artery occlusion (tMCAO) in naive mice, but this protection is blocked by the inhibition of HIF (R59949), SphK (DMS), or S1P1 (W146) just prior to HPC. Similarly, both cobalt (CoCl2) preconditioning (B) and FTY720 preconditioning (C) reduce infarct volume 24 h after tMCAO in naive mice, but this protection is also blocked when HIF (R59949), SphK (DMS), or S1P1 (W146) are inhibited prior to preconditioning. Data represent mean±SEM. N=4–18 per group. (*) P<0.05 between groups.
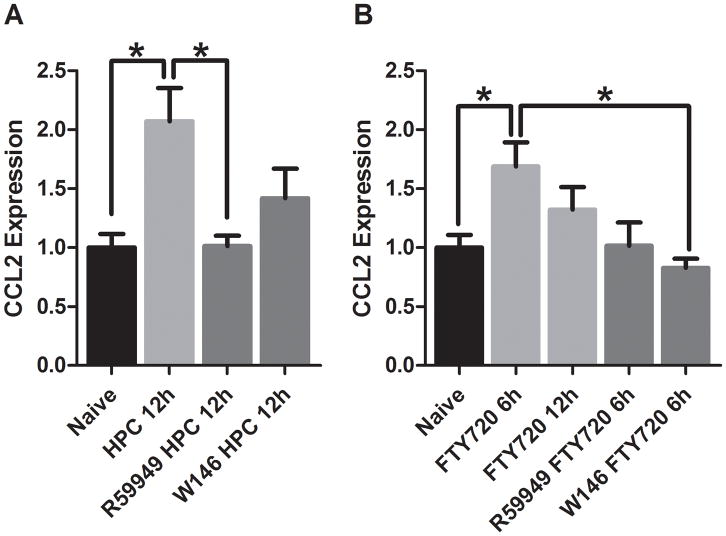
Figure 3. HIF- and S1P1-based regulation of CCL2 expression in response to preconditioning by hypoxia and FTY720.
(A) HPC increases CCL2 protein expression when measured 12 h after the cessation of HPC, but this increase is attenuated if both HIF isoforms are inhibited during HPC by R59949 or if the S1P1 receptor is antagonized during HPC by W146. (B) FTY720 increases CCL2 protein expression 6 h after FTY720 administration, but this increase is abrogated by inhibition of HIF prior to FTY720 administration with R59949, or antagonism of S1P1 prior to FTY720 administration with W146. Data represent mean±SEM. N=4–8 per group. (*) P<0.05 between groups.
Hypoxic and Pharmacologic Preconditioning
Mice were subjected to HPC (normobaric 8% oxygen for 4 h) in modified home cages with water and food ad libitum (Wacker et al. 2009, Wacker et al. 2012, Stowe et al. 2012). Ambient oxygen concentration was confirmed through monitoring cage outflow air with an oxygen analyzer (Vascular Technology). Pharmacological preconditioning was induced by injection of the HIF stabilizer cobalt chloride (CoCl2; 60 mg/kg, i.p.; Sigma) or the SphK2-specific substrate FTY720 (2-amino-2-[2-(4-octylphenyl)ethyl]-1,3-propanediol hydrochloride) (1.0 mg/kg, i.p.; Cayman Chemical). Naïve/control animals were not preconditioned with hypoxia, cobalt, or FTY720. All preconditioning treatments preceded focal ischemia by 48 h.
Pharmacological Inhibition of HIF, SphK, and S1P1
R59949 (60 μg/kg in 0.1 % DMSO, i.v.; Sigma), which inhibits HIF accumulation (Temes et al. 2005), and dimethylsphingosine (DMS, 0.33 mg/kg, i.v.; Cayman Chemical), which nonselectively inhibits both SphK isoforms, were administered by retro-orbital injection 30 min prior to preconditioning. The S1P1-specific competitive antagonist W146 (1.0 mg/kg in 0.1 % DMSO, i.p.; Cayman Chemical) was given 1 h prior to preconditioning.
Transient Focal Cerebral Ischemia
Mice were subjected to transient middle cerebral artery occlusion (tMCAO) as described previously (Miller et al. 2001, Stowe et al. 2011, Wacker et al. 2009, Wacker et al. 2012, Stowe et al. 2012). Briefly, under 2% halothane anesthesia, the left middle cerebral artery (MCA) was exposed by incision of the temporal muscle and baseline blood flow in the cortical MCA territory was measured by laser Doppler flowmetry (LDF; TSI, Inc.) The left common carotid artery was exposed via a ventral midline incision on the neck, and a silicon-coated, 6.0-gauge, nylon suture, 12 mm in length, was advanced 9.0–10.5 mm to transiently block the origin of the MCA. Body temperature was maintained throughout the surgical procedure by a thermoregulated heating pad, and animals were placed in a 34 oC incubator during ischemia. After either 45 min (C57Bl/6, SphK−/−, and CCL2−/− mice) or 1 h (SW-ND4 mice), animals were re-anesthetized, and the suture was withdrawn to reestablish cerebral perfusion. Mice were then recovered from anesthesia for 30 min in a 34 °C incubator until fully ambulatory. Cortical blood flow was again determined at the onset of ischemia and at the end of ischemia to confirm blockage of MCA flow, as well as immediately following and 24 h after suture withdrawal to confirm reperfusion. Mice retaining greater than 15% of baseline perfusion during ischemia, and mice that did not reach at least 50% of baseline flow at 5 min of reperfusion, or 70% of baseline flow at 24 h of reperfusion, were excluded. In addition, animals showing evidence of intracerebral bleeding or subarachnoid hemorrhage upon brain extraction were excluded from the study.
Quantification of Infarction Volume
These endpoints were measured as described in our previous publications (Wacker et al. 2012), but only infarct volume data are provided in this study. In brief, at 24 h of reperfusion following tMCAO, neurological deficits were assessed, and then the mice were killed by cervical dislocation, their brains removed, and 1-mm thick coronal sections obtained from a matrix were exposed to a 1% solution (in PBS) of 2,3,5-triphenyl tetrazolium chloride to delineate infarct and noninfarcted brain regions. Edema-corrected infarct volumes were quantified using Sigma Scan Pro 4.
CCL2 Immunoblotting
Animals were sacrificed 6–12 h following preconditioning. Whole cell cortical homogenates lysed in RIPA buffer were immunoblotted using standard protocols. 85 μg of protein/well was loaded and gels were incubated overnight in primary antibody solution (1:1000, CCL2 [Abcam]). IRDye secondary antibody (1:10,000; LI-COR) was imaged and quantified using the LI-COR Odyssey Infrared Imaging System.
Statistical Analyses
Comparisons were done with SigmaStat using 2-way ANOVA for Figure 1 and 1-way ANOVA for Figure 2 and 3. Statistical comparisons between groups were done with the Holm-Sidak method for multiple pair-wise comparisons with p<0.05 accepted as significant.
Results
In experiments from our laboratory that were previously published, we identified both SphK2 (Wacker et al. 2012) and CCL2 (Stowe et al. 2012) as necessary participants in HPC-induced ischemic tolerance (Figure 1A). As partial confirmation of these findings, and to distinguish between the HIF-dependent and HIF-independent effects of HPC with respect to SphK2 and CCL2 signaling, we assessed whether tolerance induced by the hypoxia-mimetic cobalt chloride also required SphK2 and CCL2. Cobalt induces the accumulation of HIF by blocking the VHL degradation of HIF through either inactivating HIF prolyl hydroxylases (chelates Fe in catalytic site) (Epstein et al. 2001), or direct binding of HIF (Yuan et al. 2001, Yuan et al. 2003). As with HPC, the reduction in infarct volume resulting from cobalt preconditioning was prevented in both SphK2- and CCL2-null mice (Figure 1B), implying HIF is upstream of SphK2 and CCL2. Then, given our previous findings that SphK2 protein expression and activity increased 2–4 h after HPC (Wacker et al. 2009), while CCL2 mRNA and protein expression increased 12–24 h after hypoxia (Stowe et al. 2012), we sought to determine whether CCL2 was downstream of SphK2 signaling. To do this, we preconditioned mice using FTY720, a SphK2-specific sphingosine analog that, after becoming phosphorylated by SphK2, acts as an S1P analog by binding to and activating S1P1, S1P3, S1P4, and S1P5 (but not S1P2) receptors (Brinkmann et al. 2002, Mandala et al. 2002). As mentioned earlier, we previously demonstrated that FTY720 was efficacious as a preconditioning drug in our model of transient focal stroke (Wacker et al. 2009). As predicted, in SphK2-null mice, without the enzyme to phosphorylate FTY720, FTY720 preconditioning was completely ineffective in inducing tolerance (Figure 1C). Moreover, FTY720 preconditioning also was impotent as a preconditioning stimulus in CCL2 knockout mice, indicating that CCL2 elaboration is downstream of S1P signaling in the establishment of an ischemia-tolerant phenotype in response to FTY720 preconditioning.
To further elucidate the signaling sequence responsible for the induction of ischemic tolerance following preconditioning with these same three agents, we used pharmacological inhibitors of HIF, SphK, and S1P1. Neither the PBS nor DMSO vehicles used for solubilizing the inhibitors affected preconditioning with any of the stimuli (data not shown). As shown in Figure 2A, when preconditioning with hypoxia, the typical (~45%) reduction in infarct volume (tolerance) is blocked by the administration of R59949, an inhibitor of both the HIF-1 and HIF-2 isoforms, prior to HPC. R59949 functions by activating the HIF prolyl hydroxylases causing VHL degradation of both HIF isoforms (Temes et al. 2005). The protection induced by HPC is also abrogated if the activity of both SphK isoforms is inhibited by dimethylsphingosine (DMS) given prior to HPC. Finally, HPC-induced tolerance is blocked by the administration of W146, a competitive antagonist of the S1P1 receptor. Collectively, these findings indicate that HPC acts through HIF and SphK, ultimately leading to an S1P-induced activation of the S1P1 receptor, in the induction of ischemic tolerance. The ischemic tolerance induced by preconditioning with cobalt, as reflected by a 49% decrease in infarct volume, is also blocked by R59949, DMS, or W146 administered prior to cobalt (Figure 2B). These findings demonstrate that cobalt preconditioning requires HIF1 and/or HIF2, and the SphK-mediated production of S1P, which then, by activating the S1P1 receptor, induces the changes in gene expression required for establishing the ischemia-tolerant phenotype.
As shown in Figure 2C, preconditioning with the SphK2-specific S1P analog FTY720 resulted in a 33% decrease in infarct volume, consistent with our previous results (Wacker et al. 2009). FTY720-induced tolerance was blocked by DMS, confirming that phosphorylation of FTY720 by SphK2 is necessary for this effect. The efficacy of FTY720 preconditioning was lost in R59949-treated mice, indicating that enhanced HIF-1 and/or HIF-2 expression is a necessary step in preconditioning signaling by FTY720, just as it is with hypoxia and cobalt. Finally, that W146 also blocked FTY720-induced protection indicates that it is the binding of phosphorylated FTY720 to the S1P1 receptor that mediates the epigenetic response.
While our aforementioned genetic and pharmacologic interventions indicated that CCL2 signaling occurs downstream of HIF activation/stabilization, these experiments did not confirm whether S1P receptor activation is needed for HPC- and FTY720-preconditioning–induced CCL2 expression. Thus, we first measured expression changes in cortical CCL2 protein levels in naïve and HPC-treated mice. As seen previously (Stowe et al. 2012), CCL2 protein expression was significantly upregulated 12 h following HPC. Treating animals with R59949 to inhibit HIF accumulation during HPC significantly blocked the HPC-induced increase in CCL2 protein (Figure 3A). In addition, administering W146 prior to HPC to prevent S1P signaling through the S1P1 receptor also abrogated the elevation in CCL2 protein expression induced by HPC (Figure 3A). These results, in parallel with those shown in Figure 1A and 2A, indicate that the HPC-induced increase in CCL2 expression is HIF-dependent. Moreover, they demonstrate that the activation of the S1P1 receptor is required for the elevated CCL2 expression occurring in response to HPC.
We then repeated these CCL2 protein expression measurements following preconditioning with FTY720 (Figure 3B). CCL2 protein expression increased significantly in response to FTY720, with the highest expression observed at 6 h following FTY720 injection. Administration of R59949 prior to FTY720 preconditioning prevented this increase, as did W146 dosing prior to FTY720 preconditioning. These results demonstrate that, even when initiating the preconditioning induction pathway at the stage of S1P signaling, the activation of HIF by FTY720 is required for CCL2 elaboration, as is the FTY720-induced activation of the S1P1 receptor; in turn, such findings reveal a significant degree of cross-talk or positive feedback between S1P and one or both HIF isoforms that defines this signaling cascade.
Discussion
The mechanisms by which preconditioning signals the gene expression required for ischemic tolerance remain to be fully elucidated. Using genetic and pharmacologic approaches, results from the present study indicate that SphK2 signaling and CCL2 production are both required for inducing the genomic reprogramming responsible for endogenous ischemic tolerance in response to HPC, as well as in response to cobalt preconditioning and preconditioning with the sphingosine analog FTY720. The involvement of CCL2 protein was also confirmed by measuring elevated levels of this cytokine following HPC and FTY720 preconditioning. Furthermore, we demonstrated that HIF is a required part of the signaling cascade induced by these preconditioning stimuli, as is activation of the S1P1 receptor. Cross-talk or feed-forward interactions between S1P and HIF aid in the upregulation of CCL2 and is necessary for successful preconditioning. Together, our findings implicate HIF, SphK, S1P1, and CCL2 in the induction of ischemic tolerance by hypoxia, as well as by FTY720.
Previously published findings on the interaction of HIF and SphK (or S1P) are varied and seemingly conflicting, but likely due, in large part, to the cells/tissues examined, as well as which SphK and HIF isoforms were under investigation (Schnitzer et al. 2009, Ralph et al. 2004, Ader et al. 2008, Ader et al. 2009, Anelli et al. 2008, Cho et al. 2011, Cuvillier & Ader 2011, Pchejetski et al. 2011, Schwalm et al. 2008). With respect to SphK being under the control of the transcriptional and metabolic regulator HIF, it was reported that SphK1 mRNA was upregulated (identified as part of a larger microarray study) in hypoxia-stressed neurons overexpressing HIF-2α (Ralph et al. 2004). A HIF-2α–mediated upregulation of SphK1 was later corroborated in U87MG glioma cells in response to hypoxia or chemical stabilization of HIF (Anelli et al. 2008). Moreover, in the human endothelial cell line EA.hy926, upregulation of SphK1, but not SphK2, gene transcription by both HIF-1α and HIF-2α was demonstrated following hypoxia (Schwalm et al. 2008). Finally, a role for HIF in regulating the hypoxia-induced expression of SphK2 was advanced in studies of A549 lung cancer cells (Schnitzer et al. 2009). HIF regulation of SphK1 and SphK2 is not unexpected, as both isoforms contain HREs in their respective promoter regions. Collectively, these studies suggest that, while HIF-mediated upregulation of SphK is common in many cell types, the isoform dependence of both appears to be cell- and tissue-specific. Our present results indicate that, in the mouse cortex, the expression and/or activity of SphK2 is upregulated secondary to the stabilization of HIF levels by hypoxia or cobalt. Because the HIF inhibitor that we used, R59949, is nonspecific (Temes et al. 2005), our findings do not allow for the identification of the specific HIF isoform that regulates SphK2. However, given the well-established rapid increase in HIF-1α that occurs in response to hypoxia (within minutes) (Jewell et al. 2001), and our previous finding that SphK2 is upregulated within 2–4 h of HPC (Wacker et al. 2009), the HIF-1α isoform is implicated in this signaling cascade.
Surprisingly, inhibition of HIF blocked FTY720-induced tolerance, suggesting HIF is downstream of S1P-related signaling. Several recent studies on the interaction of HIF and SphK in a variety of cell/tissues suggest bi-directional cross talk between these molecules, with SphK signaling also facilitating HIF stabilization and thus HIF-induced changes in gene expression. In particular, evidence indicates that SphK1 regulates HIF-1α expression and activity in several tumor cell lines (PC-3 prostate cancer cells, A549 lung cancer cells, SUM-159PT breast adenocarcinoma cells, and U87 glioblastoma cells) secondary to stabilizing the HIF-1α isoform under hypoxic conditions (Ader et al. 2008). Consistent with such a finding, melatonin suppresses HIF-1α accumulation by inhibiting SphK1 activity in PC3 cells (Cho et al. 2011), and LPS induces a Toll-like receptor 4–mediated accumulation of HIF-1α secondary to SphK1 upregulation in macrophages (Pchejetski et al. 2011). However, given that S1P induces HIF-1α in vascular endothelial and smooth muscle cells (Michaud et al. 2009), and that S1P is produced by both SphK isoforms, promotion of HIF stabilization may not be unique to the SphK1 isoform. Indeed, recent reports show elevations in cerebral HIF-1α protein in response to isoflurane preconditioning were not observed in SphK2-null mice (Yung et al. 2011), demonstrating a SphK2-specific upregulation of HIF. Likewise, our results support a SphK2-specific signaling pathway in mouse brain. Thus, taken together, the prevailing evidence for bi-directional signaling between HIF and SphK-derived S1P is consistent with our current genetic and pharmacologic results indicating that SphK2 activity appears to be both downstream of HIF (with cobalt preconditioning being ineffective in SphK2-null or DMS-treated mice) and upstream of HIF (with preconditioning initiated at the stage of S1P signaling with FTY720 being ineffective when HIF is inhibited). This perplexing finding may be explained by the existence of a positive feedback loop from S1P to HIF that functions either to further increase the expression of both molecules, or to extend the time frame over which the increased expression of both molecules persists; such an interaction may represent one of many positive feedback loops regulating HIF activity (Prabhakar & Semenza 2012). Alternatively, this finding could represent paracrine signaling wherein HIF-induced S1P released from one cell-type acts on neighboring cells to increase their expression of HIF. From our findings, we contend that cross-talk between HIF and S1P is integral to the gene expression changes induced by HPC.
In previous work from our laboratory, we utilized CCL2-null mice to demonstrate that HPC-induced tolerance to transient focal stroke was CCL2-dependent (Stowe et al. 2012). This result was surprising, given that previous studies had indicated pharmacologic inhibition or genetic knockout of CCL2 protected against stroke, particularly in a permanent ischemia model. In the present study, we confirmed that CCL2-null mice were not protected against transient ischemia when preconditioned with hypoxia, cobalt, or FTY720, and extended these findings to document that HIF activation secondary to preconditioning with either hypoxia or the hypoxia-mimetic cobalt is required for the resultant CCL2 production. Such a dependency is not unexpected, given that CCL2 is also a hypoxia-responsive, HIF-dependent gene (Chao et al. 2010, Marisa et al. 2005, Mojsilovic-Petrovic et al. 2007, Xu et al. 2007). Because FTY720 is not phosphorylated/activated by the SphK1 isoform (Paugh et al. 2003), our additional findings herein that FTY720 also elevated CCL2 expression in a HIF-dependent manner, and that the FTY720 preconditioning-induced reduction in infarct volume was HIF-dependent, underscore the aforementioned bi-directional regulatory link between HIF and SphK2-derived S1P.
Finally, based on our results with the S1P1-specific receptor antagonist W146 (Zhu et al. 2010, Sanna et al. 2006), we also advance the contention that the upregulation in CCL2 expression by S1P, as well as by phosphorylated FTY720, occurs through this bioactive lipid receptor. Studies in peripheral tissues already support an S1P-mediated upregulation of CCL2 (Lin et al. 2006, Oskeritzian et al. 2008, Yopp et al. 2004). In macrophages, this upregulation was reported to be dependent on the S1P3 receptor (Keul et al. 2011), in mast cells, the S1P2 receptor (Oskeritzian et al. 2010), and in peripheral endothelial cells, both the S1P1 and S1P3 receptors (Lin et al. 2007). Although we did not assess the effects of other S1P receptor-specific antagonists, our documentation that W146 completely abrogated ischemic tolerance induced by hypoxia, cobalt, and FTY720, as well as robustly inhibited the upregulation of CCL2 protein by hypoxic and FTY720 preconditioning, would suggest a prominent role for the S1P1 receptor in brain, and may serve to highlight again the unique tissue/cell-dependent regulatory features of S1P signaling. Which cells in brain express this receptor is also not addressed by the present study, or the specific cell types that respond to hypoxia, cobalt, and FTY720 with a HIF-dependent production of S1P. But given our previous immunohistochemical finding that neurons and endothelial cells upregulate CCL2 expression in a time-dependent fashion in response to HPC (Stowe et al. 2012), we would contend that the S1P so formed in response to these preconditioning stimuli acts in an autocrine and/or paracrine manner to generate CCL2. In turn, CCL2 produced in neurons and endothelial cells could signal gene expression changes in these respective cells in an autocrine manner and/or CCL2 released by these cells could, in a paracrine fashion, induce adaptive changes in gene expression in neighboring glial and vascular smooth muscle cells. Given CCL2’s prototypical role as a monocyte chemoattractant, perhaps monocytes also participate in this inter-cellular signaling as well. Clearly, further studies are warranted to elucidate the nature of such CCL2-regulated epigenetic responses.
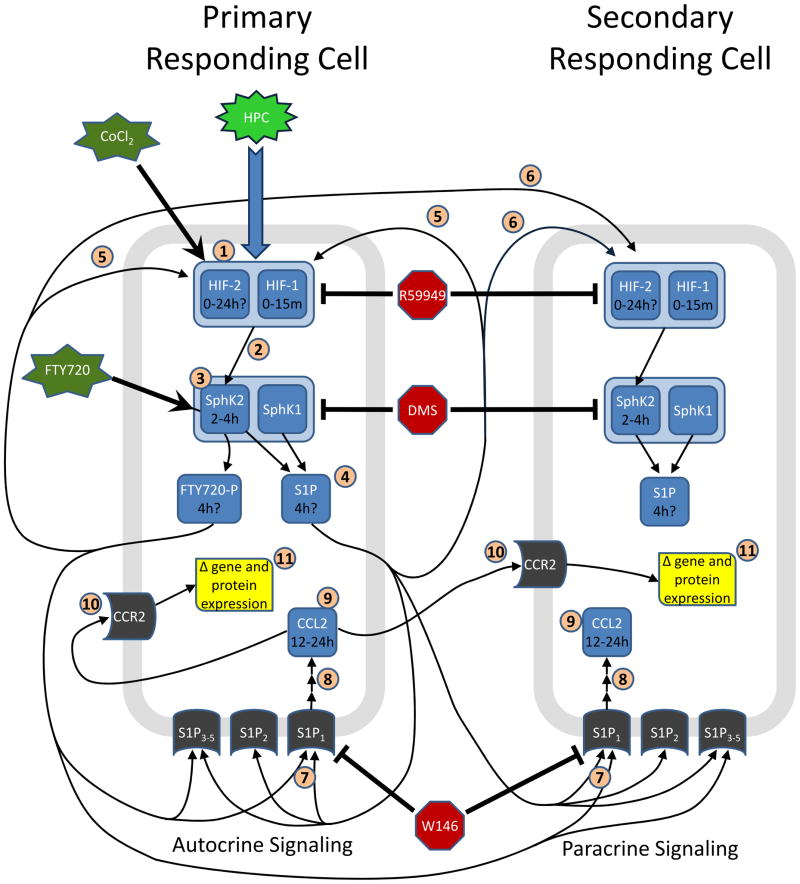
In conclusion, based on the genetic and pharmacologic studies presented herein, we propose a novel signaling cascade for preconditioning-induced cerebral ischemic tolerance (Figure 4). Both hypoxic and cobalt preconditioning stabilize HIF; most likely, it is the HIF-1α, and not the HIF-2α, isoform that is involved initially, given the isoform-specific kinetics for HIF revealed in other studies (Jewell et al. 2001, Stroka et al. 2001, Holmquist-Mengelbier et al. 2006) and the rapid timecourse we reported previously for SphK2 upregulation/activity in response to HPC (Wacker et al. 2009). Then, by a mechanism yet to be defined, HIF-1α facilitates SphK2 protein expression and/or activity leading to an increase in S1P formation. This S1P then acts in an autocrine and/or paracrine fashion through the S1P1 receptor to upregulate CCL2 mRNA and protein expression. While HIF-mediated, survival-promoting changes in gene expression are well-described, at this juncture it remains unclear how CCL2 regulates the genomic reprogramming required for ischemic tolerance. S1P signaling also serves in another yet-to-be-detailed manner to stabilize HIF-1α and/or HIF-2α through autocrine- or paracrine-based cross-talk, further enhancing this signaling cascade. Preconditioning by the sphingosine analog FTY720 transduces this epigenetic response network similarly: After being phosphorylated by SphK2, its activation of the S1P1 receptor also drives the production of CCL2. Additionally, activated FTY720 signaling feeds back to promote HIF-dependent signaling, another step vital to inducing ischemic tolerance. The extent to which this overall signaling cascade is activated by other well-established preconditioning stimuli is presently unclear. Although intentional hypoxic gas breathing is used by some athletes for training purposes, and although FTY720 is clinically approved as a treatment for patients with multiple sclerosis, the continued elucidation of preconditioning signaling pathways as we have done here provides an expanded number of downstream genomic reprogramming effector molecules that one might therapeutically target (Simon et al. 2012) to induce tolerance in humans.
Figure 4. Proposed signaling cascade for preconditioning by hypoxia, cobalt, and FTY720.
“Working hypothesis” schematic showing the proposed signaling pathways and molecules involved in the ischemic tolerance achieved by the different preconditioning stimuli tested in this study (green), as well as the pharmacologic manipulations used (red) to elucidate this cascade. Both primary and secondary responding cells are shown to highlight the potential autocrine and paracrine actions of S1P, FTY720-P, and CCL2. Estimated time periods over which the expression of some of the primary mediators in the signaling cascade changes are also shown. Evidence for the inclusion of each numbered molecule or numbered interaction in this signaling pathway is derived from the present study, or others, as follows: [1] Extensive literature supports an increase in HIF expression in response to hypoxia or CoCl2 treatment (Bergeron et al. 2000, Yuan et al. 2003, Yuan et al. 2001, Semenza 2009, Jewell et al. 2001, Semenza 2001, Lahiri et al. 2006). [2] Wacker et al. (2009) showed that HPC leads to a microvascular SphK2 increase 2–4 h later, and that inhibition of this increased activity blocks HPC-induced protection. [3] HPC-, CoCl2-, and FTY720-induced protection is blocked in SphK2-null mice (Figure 1). [4] Inhibition of SphK2 activity blocks preconditioning (Figures 1 and 2), so presumably S1P or FTY720-P formation is required for this process. The timing of increased microvascular SphK2 activity shown in Wacker et al. (2009) suggests S1P increases around 4 h after HPC. [5] FTY720 preconditioning is blocked by HIF inhibition (Figure 2C), indicating it acts on HIF either via an autocrine feedback loop, or [6] via paracrine signaling on another cell. [7] Competitive antagonism of S1P1 with W146 blocked preconditioning-based protection by HPC, CoCl2, and FTY720 (Figure 2). [8] Increased CCL2 expression following HPC or FTY720 treatment did not occur when the S1P1 receptor was antagonized with W146 (Figure 3). [9] CCL2-null mice exhibited larger baseline infarcts than naïve mice following tMCAO (Figure 1). Stowe et al. (2012) showed increases in CCL2 expression 12–24 h following HPC, primarily in neurons. [10] CCR2 is the predominant receptor for CCL2, so the involvement of this receptor in CCL2-mediated preconditioning is presumed. However, paradoxically, CCR2-null mice have reduced baseline infarcts relative to naïve mice (Dimitrijevic et al. 2007); this latter effect may be due to the activity of a different CCR2 ligand, or maybe CCL2-mediated protection functions via a receptor other than CCR2. [11] Synthesis of new proteins secondary to changes in gene expression is known to be required for establishing the preconditioning-induced, ischemia-tolerant phenotype (Gidday 2006, Sharp et al. 2004).
Acknowledgments
This study was supported by NIH NHLBI F32 grant HL101202 (BKW), NIH NHLBI R01 HL79278 (JMG), NIH P01 NS32636 (JMG), the Spastic Paralysis Research Foundation of the Illinois–Eastern Iowa District of Kiwanis International, and an NIH Neuroscience Blueprint Core Grant P30 NS057105 to Washington University. The authors thank Dr. Ann Stowe for technical contributions and discussion regarding CCL2 signaling in ischemic tolerance.
Abbreviations
- HIF
hypoxia inducible factor
- CCL2
chemokine (C-C motif) ligand 2
- S1P
sphingosine 1-phosphate
- FTY720
2-amino-2-[2-(4-octylphenyl)ethyl]-1,3-propanediol hydrochloride
- HPC
hypoxic preconditioning
- HRE
hypoxia response element
- pVHL
von Hippel–Lindau protein
- VEGF
vascular endothelial growth factor
- SphK
sphingosine kinase
- CCR2
chemokine (C-C motif) receptor 2
- CNS
central nervous system
- LDF
laser Doppler flowmetry
- CoCl2
cobalt chloride
- DMSO
dimethyl sulfoxide
- PBS
phosphate buffered saline
- D M S
N, N-dimethylsphingosine
- W146
3-amino-4-(3-hexylphenylamino)-4-oxobutyl phosphonic acid
- R59949
3-[2-[4-(bis(4-Fluorophenyl)methylene)-1-piperidinyl]ethyl]-2,3-dihydro-2-thioxo-4(1H)-quinazolinone
- RIPA
radioimmunoprecipitation assay
- tMCAO
transient middle cerebral artery occlusion
- mRNA
messenger ribonucleic acid
Footnotes
The authors have no conflicts of interest to disclose.
References
- Ader I, Brizuela L, Bouquerel P, Malavaud B, Cuvillier O. Sphingosine kinase 1: a new modulator of hypoxia inducible factor 1alpha during hypoxia in human cancer cells. Cancer Res. 2008;68:8635–8642. doi: 10.1158/0008-5472.CAN-08-0917. [DOI] [PubMed] [Google Scholar]
- Ader I, Malavaud B, Cuvillier O. When the sphingosine kinase 1/sphingosine 1-phosphate pathway meets hypoxia signaling: new targets for cancer therapy. Cancer Res. 2009;69:3723–3726. doi: 10.1158/0008-5472.CAN-09-0389. [DOI] [PubMed] [Google Scholar]
- Anelli V, Gault CR, Cheng AB, Obeid LM. Sphingosine kinase 1 is up-regulated during hypoxia in U87MG glioma cells. Role of hypoxia-inducible factors 1 and 2. J Biol Chem. 2008;283:3365–3375. doi: 10.1074/jbc.M708241200. [DOI] [PubMed] [Google Scholar]
- Aragones J, Fraisl P, Baes M, Carmeliet P. Oxygen sensors at the crossroad of metabolism. Cell Metab. 2009;9:11–22. doi: 10.1016/j.cmet.2008.10.001. [DOI] [PubMed] [Google Scholar]
- Bergeron M, Gidday JM, Yu AY, Semenza GL, Ferriero DM, Sharp FR. Role of hypoxia-inducible factor-1 in hypoxia-induced ischemic tolerance in neonatal rat brain. Ann Neurol. 2000;48:285–296. [PubMed] [Google Scholar]
- Brinkmann V, Davis MD, Heise CE, et al. The immune modulator FTY720 targets sphingosine 1-phosphate receptors. J Biol Chem. 2002;277:21453–21457. doi: 10.1074/jbc.C200176200. [DOI] [PubMed] [Google Scholar]
- Chao J, Donham P, van Rooijen N, Wood JG, Gonzalez NC. Monocyte chemoattractant protein-1 released from alveolar macrophages mediates the systemic inflammation of acute alveolar hypoxia. Am J Respir Cell Mol Biol. 2010;45:53–61. doi: 10.1165/rcmb.2010-0264OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chen XL, Grey JY, Thomas S, Qiu FH, Medford RM, Wasserman MA, Kunsch C. Sphingosine kinase-1 mediates TNF-alpha-induced MCP-1 gene expression in endothelial cells: upregulation by oscillatory flow. Am J Physiol Heart Circ Physiol. 2004;287:H1452–1458. doi: 10.1152/ajpheart.01101.2003. [DOI] [PubMed] [Google Scholar]
- Cho SY, Lee HJ, Jeong SJ, Lee HJ, Kim HS, Chen CY, Lee EO, Kim SH. Sphingosine kinase 1 pathway is involved in melatonin-induced HIF-1alpha inactivation in hypoxic PC-3 prostate cancer cells. J Pineal Res. 2011;51:87–93. doi: 10.1111/j.1600-079X.2011.00865.x. [DOI] [PubMed] [Google Scholar]
- Correia SC, Moreira PI. Hypoxia-inducible factor 1: a new hope to counteract neurodegeneration? J Neurochem. 2010;112:1–12. doi: 10.1111/j.1471-4159.2009.06443.x. [DOI] [PubMed] [Google Scholar]
- Cuvillier O, Ader I. Hypoxia-inducible factors and sphingosine 1-phosphate signaling. Anticancer Agents Med Chem. 2011;11:854–862. doi: 10.2174/187152011797655050. [DOI] [PubMed] [Google Scholar]
- Dimitrijevic OB, Stamatovic SM, Keep RF, Andjelkovic AV. Absence of the chemokine receptor CCR2 protects against cerebral ischemia/reperfusion injury in mice. Stroke. 2007;38:1345–1353. doi: 10.1161/01.STR.0000259709.16654.8f. [DOI] [PubMed] [Google Scholar]
- Epstein AC, Gleadle JM, McNeill LA, et al. C. elegans EGL-9 and mammalian homologs define a family of dioxygenases that regulate HIF by prolyl hydroxylation. Cell. 2001;107:43–54. doi: 10.1016/s0092-8674(01)00507-4. [DOI] [PubMed] [Google Scholar]
- Gidday JM. Cerebral preconditioning and ischaemic tolerance. Nat Rev Neurosci. 2006;7:437–448. doi: 10.1038/nrn1927. [DOI] [PubMed] [Google Scholar]
- Holmquist-Mengelbier L, Fredlund E, Lofstedt T, et al. Recruitment of HIF-1alpha and HIF-2alpha to common target genes is differentially regulated in neuroblastoma: HIF-2alpha promotes an aggressive phenotype. Cancer Cell. 2006;10:413–423. doi: 10.1016/j.ccr.2006.08.026. [DOI] [PubMed] [Google Scholar]
- Jewell UR, Kvietikova I, Scheid A, Bauer C, Wenger RH, Gassmann M. Induction of HIF-1alpha in response to hypoxia is instantaneous. Faseb J. 2001;15:1312–1314. [PubMed] [Google Scholar]
- Keul P, Lucke S, von Wnuck Lipinski K, Bode C, Graler M, Heusch G, Levkau B. Sphingosine-1-phosphate receptor 3 promotes recruitment of monocyte/macrophages in inflammation and atherosclerosis. Circ Res. 2011;108:314–323. doi: 10.1161/CIRCRESAHA.110.235028. [DOI] [PubMed] [Google Scholar]
- Lahiri S, Roy A, Baby SM, Hoshi T, Semenza GL, Prabhakar NR. Oxygen sensing in the body. Prog Biophys Mol Biol. 2006;91:249–286. doi: 10.1016/j.pbiomolbio.2005.07.001. [DOI] [PubMed] [Google Scholar]
- Lin CI, Chen CN, Chen JH, Lee H. Lysophospholipids increase IL-8 and MCP-1 expressions in human umbilical cord vein endothelial cells through an IL-1-dependent mechanism. J Cell Biochem. 2006;99:1216–1232. doi: 10.1002/jcb.20963. [DOI] [PubMed] [Google Scholar]
- Lin CI, Chen CN, Lin PW, Lee H. Sphingosine 1-phosphate regulates inflammation-related genes in human endothelial cells through S1P1 and S1P3. Biochem Biophys Res Commun. 2007;355:895–901. doi: 10.1016/j.bbrc.2007.02.043. [DOI] [PubMed] [Google Scholar]
- Mandala S, Hajdu R, Bergstrom J, et al. Alteration of lymphocyte trafficking by sphingosine-1-phosphate receptor agonists. Science. 2002;296:346–349. doi: 10.1126/science.1070238. [DOI] [PubMed] [Google Scholar]
- Marisa C, Lucci I, Di Giulio C, Bianchi G, Grilli A, Patruno A, Reale M. MCP-1 and MIP-2 expression and production in BB diabetic rat: effect of chronic hypoxia. Mol Cell Biochem. 2005;276:105–111. doi: 10.1007/s11010-005-3556-4. [DOI] [PubMed] [Google Scholar]
- Martire A, Fernandez B, Buehler A, Strohm C, Schaper J, Zimmermann R, Kolattukudy PE, Schaper W. Cardiac overexpression of monocyte chemoattractant protein-1 in transgenic mice mimics ischemic preconditioning through SAPK/JNK1/2 activation. Cardiovasc Res. 2003;57:523–534. doi: 10.1016/s0008-6363(02)00697-1. [DOI] [PubMed] [Google Scholar]
- Michaud MD, Robitaille GA, Gratton JP, Richard DE. Sphingosine-1-phosphate: a novel nonhypoxic activator of hypoxia-inducible factor-1 in vascular cells. Arterioscler Thromb Vasc Biol. 2009;29:902–908. doi: 10.1161/ATVBAHA.109.185280. [DOI] [PubMed] [Google Scholar]
- Miller BA, Perez RS, Shah AR, Gonzales ER, Park TS, Gidday JM. Cerebral protection by hypoxic preconditioning in a murine model of focal ischemia-reperfusion. Neuroreport. 2001;12:1663–1669. doi: 10.1097/00001756-200106130-00030. [DOI] [PubMed] [Google Scholar]
- Mojsilovic-Petrovic J, Callaghan D, Cui H, Dean C, Stanimirovic DB, Zhang W. Hypoxia-inducible factor-1 (HIF-1) is involved in the regulation of hypoxia-stimulated expression of monocyte chemoattractant protein-1 (MCP-1/CCL2) and MCP-5 (Ccl12) in astrocytes. J Neuroinflammation. 2007;4:12. doi: 10.1186/1742-2094-4-12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Niu J, Azfer A, Zhelyabovska O, Fatma S, Kolattukudy PE. Monocyte chemotactic protein (MCP)-1 promotes angiogenesis via a novel transcription factor, MCP-1-induced protein (MCPIP) J Biol Chem. 2008;283:14542–14551. doi: 10.1074/jbc.M802139200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Oskeritzian CA, Alvarez SE, Hait NC, Price MM, Milstien S, Spiegel S. Distinct roles of sphingosine kinases 1 and 2 in human mast-cell functions. Blood. 2008;111:4193–4200. doi: 10.1182/blood-2007-09-115451. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Oskeritzian CA, Price MM, Hait NC, Kapitonov D, Falanga YT, Morales JK, Ryan JJ, Milstien S, Spiegel S. Essential roles of sphingosine-1-phosphate receptor 2 in human mast cell activation, anaphylaxis, and pulmonary edema. J Exp Med. 2010;207:465–474. doi: 10.1084/jem.20091513. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Paugh SW, Payne SG, Barbour SE, Milstien S, Spiegel S. The immunosuppressant FTY720 is phosphorylated by sphingosine kinase type 2. FEBS Lett. 2003;554:189–193. doi: 10.1016/s0014-5793(03)01168-2. [DOI] [PubMed] [Google Scholar]
- Pchejetski D, Nunes J, Coughlan K, Lall H, Pitson SM, Waxman J, Sumbayev VV. The involvement of sphingosine kinase 1 in LPS-induced Toll-like receptor 4-mediated accumulation of HIF-1alpha protein, activation of ASK1 and production of the pro-inflammatory cytokine IL-6. Immunol Cell Biol. 2011;89:268–274. doi: 10.1038/icb.2010.91. [DOI] [PubMed] [Google Scholar]
- Prabhakar NR, Semenza GL. Adaptive and maladaptive cardiorespiratory responses to continuous and intermittent hypoxia mediated by hypoxia-inducible factors 1 and 2. Physiol Rev. 2012;92:967–1003. doi: 10.1152/physrev.00030.2011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ralph GS, Parham S, Lee SR, et al. Identification of potential stroke targets by lentiviral vector mediated overexpression of HIF-1 alpha and HIF-2 alpha in a primary neuronal model of hypoxia. J Cereb Blood Flow Metab. 2004;24:245–258. doi: 10.1097/01.WCB.0000110532.48786.46. [DOI] [PubMed] [Google Scholar]
- Sanna MG, Wang SK, Gonzalez-Cabrera PJ, et al. Enhancement of capillary leakage and restoration of lymphocyte egress by a chiral S1P1 antagonist in vivo. Nat Chem Biol. 2006;2:434–441. doi: 10.1038/nchembio804. [DOI] [PubMed] [Google Scholar]
- Schnitzer SE, Weigert A, Zhou J, Brune B. Hypoxia enhances sphingosine kinase 2 activity and provokes sphingosine-1-phosphate-mediated chemoresistance in A549 lung cancer cells. Mol Cancer Res. 2009;7:393–401. doi: 10.1158/1541-7786.MCR-08-0156. [DOI] [PubMed] [Google Scholar]
- Schwalm S, Doll F, Romer I, Bubnova S, Pfeilschifter J, Huwiler A. Sphingosine kinase-1 is a hypoxia-regulated gene that stimulates migration of human endothelial cells. Biochem Biophys Res Commun. 2008;368:1020–1025. doi: 10.1016/j.bbrc.2008.01.132. [DOI] [PubMed] [Google Scholar]
- Semenza GL. HIF-1 and mechanisms of hypoxia sensing. Curr Opin Cell Biol. 2001;13:167–171. doi: 10.1016/s0955-0674(00)00194-0. [DOI] [PubMed] [Google Scholar]
- Semenza GL. Regulation of oxygen homeostasis by hypoxia-inducible factor 1. Physiology (Bethesda) 2009;24:97–106. doi: 10.1152/physiol.00045.2008. [DOI] [PubMed] [Google Scholar]
- Sharp FR, Ran R, Lu A, Tang Y, Strauss KI, Glass T, Ardizzone T, Bernaudin M. Hypoxic preconditioning protects against ischemic brain injury. Neurorx. 2004;1:26–35. doi: 10.1602/neurorx.1.1.26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Simon RP, Meller R, Zhou A, Henshall D. Can genes modify stroke outcome and by what mechanisms? Stroke. 2012;43:286–291. doi: 10.1161/STROKEAHA.111.622225. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stamatovic SM, Keep RF, Mostarica-Stojkovic M, Andjelkovic AV. CCL2 regulates angiogenesis via activation of Ets-1 transcription factor. J Immunol. 2006;177:2651–2661. doi: 10.4049/jimmunol.177.4.2651. [DOI] [PubMed] [Google Scholar]
- Stowe AM, Altay T, Freie AB, Gidday JM. Repetitive hypoxia extends endogenous neurovascular protection for stroke. Ann Neurol. 2011;69:975–985. doi: 10.1002/ana.22367. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stowe AM, Wacker BK, Cravens PD, Perfater JL, Li MK, Hu R, Freie AB, Stuve O, Gidday JM. CCL2 upregulation triggers hypoxic preconditioning-induced protection from stroke. J Neuroinflammation. 2012;9:33. doi: 10.1186/1742-2094-9-33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stroka DM, Burkhardt T, Desbaillets I, Wenger RH, Neil DA, Bauer C, Gassmann M, Candinas D. HIF-1 is expressed in normoxic tissue and displays an organ-specific regulation under systemic hypoxia. FASEB J. 2001;15:2445–2453. doi: 10.1096/fj.01-0125com. [DOI] [PubMed] [Google Scholar]
- Temes E, Martin-Puig S, Acosta-Iborra B, Castellanos MC, Feijoo-Cuaresma M, Olmos G, Aragones J, Landazuri MO. Activation of HIF-prolyl hydroxylases by R59949, an inhibitor of the diacylglycerol kinase. J Biol Chem. 2005;280:24238–24244. doi: 10.1074/jbc.M414694200. [DOI] [PubMed] [Google Scholar]
- Wacker BK, Freie AB, Perfater JL, Gidday JM. Junctional protein regulation by sphingosine kinase 2 contributes to blood-brain barrier protection in hypoxic preconditioning-induced cerebral ischemic tolerance. J Cereb Blood Flow Metab. 2012;32:1014–1023. doi: 10.1038/jcbfm.2012.3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wacker BK, Park TS, Gidday JM. Hypoxic preconditioning-induced cerebral ischemic tolerance: role of microvascular sphingosine kinase 2. Stroke. 2009;40:3342–3348. doi: 10.1161/STROKEAHA.109.560714. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Xu Q, Wang S, Jiang X, et al. Hypoxia-induced astrocytes promote the migration of neural progenitor cells via vascular endothelial factor, stem cell factor, stromal-derived factor-1alpha and monocyte chemoattractant protein-1 upregulation in vitro. Clin Exp Pharmacol Physiol. 2007;34:624–631. doi: 10.1111/j.1440-1681.2007.04619.x. [DOI] [PubMed] [Google Scholar]
- Yopp AC, Fu S, Honig SM, Randolph GJ, Ding Y, Krieger NR, Bromberg JS. FTY720-enhanced T cell homing is dependent on CCR2, CCR5, CCR7, and CXCR4: evidence for distinct chemokine compartments. J Immunol. 2004;173:855–865. doi: 10.4049/jimmunol.173.2.855. [DOI] [PubMed] [Google Scholar]
- Yuan Y, Beitner-Johnson D, Millhorn DE. Hypoxia-inducible factor 2alpha binds to cobalt in vitro. Biochem Biophys Res Commun. 2001;288:849–854. doi: 10.1006/bbrc.2001.5835. [DOI] [PubMed] [Google Scholar]
- Yuan Y, Hilliard G, Ferguson T, Millhorn DE. Cobalt inhibits the interaction between hypoxia-inducible factor-alpha and von Hippel-Lindau protein by direct binding to hypoxia-inducible factor-alpha. J Biol Chem. 2003;278:15911–15916. doi: 10.1074/jbc.M300463200. [DOI] [PubMed] [Google Scholar]
- Yung LM, Wei Y, Qin T, Wang Y, Smith CD, Waeber C. Sphingosine kinase 2 mediates cerebral preconditioning and protects the mouse brain against ischemic injury. Stroke. 2011;43:199–204. doi: 10.1161/STROKEAHA.111.626911. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhu D, Wang Y, Singh I, Bell RD, Deane R, Zhong Z, Sagare A, Winkler EA, Zlokovic BV. Protein S controls hypoxic/ischemic blood-brain barrier disruption through the TAM receptor Tyro3 and sphingosine 1-phosphate receptor. Blood. 2010;115:4963–4972. doi: 10.1182/blood-2010-01-262386. [DOI] [PMC free article] [PubMed] [Google Scholar]