Abstract
BACKGROUND
Parental substance use disorder (SUD) is associated with a range of negative offspring outcomes and psychopathology, but the clustering of these outcomes into subtypes has seldom been examined, nor have the familial and environmental contexts of these subtypes been reported. The present study examines the clustering of offspring lifetime substance use and psychiatric disorders into subtypes and characterizes them in terms of familial and non-familial influences using an offspring-of-twins design.
METHOD
Telephone-administered diagnostic interviews were used to collect data on psychiatric disorders and SUD from 488 twin fathers, 420 biological mothers and 831 offspring. Latent class analysis (LCA) was used to derive subtypes of lifetime comorbidity in offspring. Familial risk and environmental variables associated with each subtype (i.e. parenting, childhood physical or sexual abuse, perceived sibling and peer substance use) were identified using multinomial logistic regression.
RESULTS
Four classes identified by LCA were characterized as 1) unaffected, 2) alcohol abuse/dependence, 3) alcohol abuse/dependence comorbid with anxiety and depression, and 4) alcohol, cannabis abuse/dependence and nicotine dependence comorbid with conduct disorder. Inconsistent parenting, childhood physical/sexual abuse, and perceived sibling and peer substance use were significantly associated with profiles of offspring comorbidity after adjusting for familial vulnerability. Some associations were specific (i.e. perceived peer alcohol use to the AUD class), while others were general (peer smoking to all 3 comorbidity classes).
CONCLUSIONS
We observed distinct subtypes of psychiatric and SUD comorbidity in adolescents and young adults. Subtypes of offspring psychopathology have varied associations with parental psychopathology, family environment, and sibling and peer behaviors.
Keywords: substance use disorder, anxiety, depression, twin, comorbid
1. INTRODUCTION
Existing studies of risk for psychopathology in the offspring of parents with substance use disorders (SUD) have largely focused on individual disorders (Hartman et al., 2006; Jacob et al., 2003; Xian et al., 2010; Scherrer et al., 2012, 2008; Marmorstein et al., 2009). While this line of research has identified a wide range of risk factors for specific disorders, we are not aware of previous examinations of the clustering of disorders into subtypes of comorbidity and the familial and environmental characteristics of those subtypes.
Several studies have used latent class analysis (LCA) to characterize the co-occurrence of psychiatric disorders (Kessler et al., 2005). Results from LCA of DSM-IV disorders in adults from the National Comorbidity Survey Replication (NCS-R) suggested there were classes of pure externalizing disorders, pure internalizing disorders and comorbid internalizing and externalizing disorders (Kessler et al., 2005). Subsequent analysis of the NCS and NCS-R data identified classes that could similarly be distinguished by the clustering of internalizing disorders, externalizing disorders, and by the comorbidity of internalizing and externalizing disorders (Vaidyanathan et al., 2011). Overall, the evidence from these and additional reports from other cohorts (Sullivan, 1998; Olino et al., 2012; Todorov et al., 2006, Dawson et al., 2010) support several comorbidity subtypes that typically encompass unaffected, internalizing, externalizing, and highly comorbid patterns of SUD and psychiatric disorders.
Parental SUD is associated with increased risk for offspring SUD, externalizing, and internalizing disorders (Dinwiddie and Reich, 1991, Sher, 1991, Chassin et al., 1999; Morgan et al., 2010). It may also confer increased vulnerability for an array of comorbidities which cross externalizing and internalizing domains, and which are characterized by different risk factors and environmental contexts. While offspring studies are designed to examine familial vulnerability to psychopathology, they have not, to our knowledge, investigated other risk factors putatively associated with parental SUDs, such as parenting behaviors and perceived sibling substance use and peer influences, which could be associated with subtypes of offspring comorbidity.
Parenting behavior, sibling and peer influences have been shown to be associated with greater risk of adolescent and young adult alcohol (Barnow et al., 2002) and drug abuse/dependence, both alone (Scherrer et al., 2008; Duncan et al., 1996) and comorbid with depression (Martin et al., 2004), anxiety (Lindhout et al., 2009) and conduct disorder (Webster-Stratton and Hammond, 1999). However, the existing literature has not demonstrated that these parenting and peer influences are significantly associated with comorbidity after accounting for familial vulnerability. In addition, the magnitude of familial contributions, parenting and peer influences may vary by patterns of comorbidity. For example, these influences may differ in their association with alcohol abuse/dependence that is comorbid with depression as compared to marijuana abuse/dependence comorbid with conduct disorder.
To address these gaps in the literature, the current study aims to: 1) identify subtypes of comorbidity among alcohol and marijuana abuse/dependence, nicotine dependence, conduct disorder, anxiety disorder and major depressive disorder in adolescents and young adults using latent class analysis, 2) determine if the familial vulnerability associated with parental SUD and internalizing disorders is associated with subtypes of comorbidity, and 3) identify parenting behaviors, early family environmental factors, and perceived sibling and peer influences that are associated with subtypes of comorbidity after accounting for familial vulnerability in an offspring-of-twins design.
2. METHODS
2.1 Sample
Subjects for the current study were offspring of male twins from the Vietnam Era Twin Registry (VETR; Eisen et al., 1987, Henderson et al., 1990). The VETR comprises male-male twin pairs identified from military discharge files, each of whom served in the military during the Vietnam Era (1965–1975). Twin zygosity, monozygotic (MZ) or dizygotic (DZ), was determined using questionnaires and blood group typing (Eisen et al., 1989). Twin pairs from the VETR were selected for participation in a subsequent offspring-of-twins (OOT) study designed to examine the intergenerational transmission of illicit drug dependence based on differing levels of genetic and environmental risk to offspring. Twins (i.e., biological fathers of the subjects in the OOT study) completed a 1987 health survey (Henderson et al., 1990) in which the birth dates of offspring were reported and a 1992 telephone administration of the Diagnostic Interview Schedule (DIS-III-R; Robins, 1989) in which DSM-III-R alcohol abuse and dependence, drug abuse and dependence and psychiatric disorders were assessed (Tsuang et al., 1996, 1998). Beginning in 2002, twins were recruited into the OOT study based on 3 selection criteria: (i) both members of the twin pair completed the 1987 mailed questionnaire and the 1992 telephone interview, (ii) at least one member of the twin pair had a child born between 1973 and 1987, and (iii) at least one member of the twin pair met criteria for DSM-III-R lifetime illicit drug dependence based on data from the 1992 structured interview. Twin pairs were identified as concordant or discordant for lifetime history of illicit drug dependence. Control twin pairs with no history of drug dependence were also identified.
Latent (unmeasured) levels of familial and environmental risk to offspring were assigned to one of four categories based on each twin pair’s (father and uncle of offspring) lifetime drug dependence status and zygosity (MZ or DZ). The highest risk category (Group 1) comprised offspring of MZ or DZ fathers who had a history of drug dependence, regardless of co-twin status for drug dependence, or who had a history of alcohol dependence, if the co-twin had a history of drug dependence. This was termed the high-genetic, high-environmental (HG-HE) risk group, since offspring were at elevated genetic risk by virtue of having a father with SUD and also at elevated environmental risk by virtue of experiencing a high risk rearing environment via their affected parent (Hartman et al., 2006, Hussong et al., 2008, Jacob et al., 2003, Thompson et al., 2008). Groups 2 and 3 were offspring of MZ (Group 2) and DZ (Group 3) twins, in which 100% (MZ) and 50% (DZ) of genes are shared between the twin fathers. Offspring in Group 2 had fathers who did not themselves meet criteria for lifetime drug dependence but had an affected identical co-twin; thus, these offspring were at low environmental risk because they did not grow up with a father with SUD, but at high genetic risk because their fathers, though unaffected, had an affected identical twin (HG-LE). Group 3 included offspring with an unaffected father whose DZ cotwin was affected; thus they were at low environmental risk but medium genetic risk (MG-LE). The lowest risk group (Group 4) comprised a random sample of offspring of male twin pairs (both MZ and DZ) in which neither had a lifetime history of drug dependence.
Details on response rates of twins, biological mothers and offspring invited to participate are available from previous studies (Duncan et al., 2008; Scherrer et al., 2008). In brief, 80% (excluding twins who were too ill or untraceable) of the twin fathers participated, 71% of the mothers were interviewed from 2002–2003, and fathers gave consent to contact 950 offspring of whom 839 (88%) were interviewed initially from 2003–2004. Response rates did not significantly (chi-square=3.34; p=0.34) differ by genetic and environmental risk group. We observed 81.5% of HG-HE twins, 76.3% of HG-LE twins, 78.5% of MG-LE twins and 75.8% of LG-LE twins responded. As well, no differences in response rate among offspring were observed. Of those contacted for interview, 86.6% of HG-HE offspring completed interviews, 94.0% of HG-LE, 90.3% of MG-LE and 88.9% of LG-LE offspring (chi-square=7.53, p=0.44).
Mothers not currently married to the biological father and those married to a twin of ethnic minority were less likely to be interviewed (p<0.001). Offspring whose fathers were not currently married to their biological mothers were less likely to be interviewed than those whose fathers were married to their biological mothers (p<0.001). The current study analyzed data from 831 offspring (from 488 fathers) aged 12 to 32 (mean (SD) =22.7 (4.4)) and data from 420 mothers.
2.2 Assessments
Structured diagnostic interviews based on the Semi-Structured Assessment for the Genetics of Alcoholism (SSAGA; Bucholz et al., 1994; Hesselbrock et al., 1999) were administered by telephone with mothers and offspring during 2003–2004. Experienced staff at the Institute for Survey Research at Temple University recruited participants and collected all data. Interviewers were blind to the drug dependence status of the fathers and co-twins. Fathers were interviewed first and provided permission to contact the offspring and the biological mother of the offspring for interviews. All participants (fathers, co-twins, mothers, and offspring) gave verbal consent before participating in the interview. The period of interview, target population (twins, mothers, and child) and primary assessment are shown in Figure 1.
Figure 1.
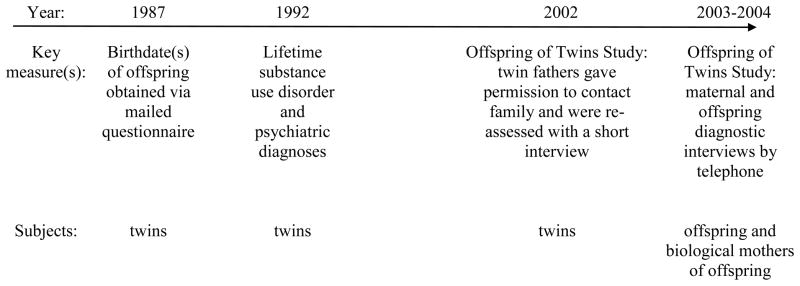
Data collection timeline
The Institutional Review Boards at participating universities and at the Seattle Veteran’s Administration, where the VETR is maintained, approved the study protocols.
2.3. Measures
2.3.1. Offspring substance use and psychiatric disorders
Offspring data obtained from telephone administration of the adapted SSAGA (Bucholz et al., 1994) were used to derive DSM-IV lifetime diagnoses of major depression, conduct disorder, panic disorder, social phobia and generalized anxiety disorder, alcohol abuse or dependence, marijuana abuse or dependence, and nicotine dependence. Due to the low prevalence of specific anxiety disorders, (i.e., panic disorder, generalized anxiety disorder, and social phobia), these disorders were combined into one variable representing anxiety disorders.
2.3.2. Offspring early environment
Measures of parental strictness, rule consistency, and closeness were based on offspring perceptions of these measures using constructs for perceived support in social relationships (Sarason et al., 1991) and from Robins and colleagues’ (Robins et al., 1985) scale for assessing early home environmental correlates of psychopathology. Details about these variables have been previously reported (Scherrer et al., 2008).
2.3.2.1. Offspring history of childhood abuse
Reports of exposure to childhood physical and/or sexual abuse were combined into one variable. Childhood physical abuse was a composite variable derived from the following questions: (1) having often been punched or hit with a belt or stick by either parent when aged 6 to 12, (2) having been physically injured on purpose by any adult when aged 6 to 12, (3) serious physical assault before age 16, (4) physical abuse as a child. Childhood sexual abuse was a composite variable derived from questions about forced intercourse, rape, or sexual molestation before age 16, within or, in most cases, extra-familial.
2.3.4. Parental substance use and substance use disorder
Father’s lifetime history of DSM-III-R diagnoses of alcohol and drug dependence were derived from data collected in the 1992 DIS-III-R interview. Data from the 2003–2004 telephone interviews with mothers were used to derive DSM-IV lifetime history of alcohol and marijuana abuse and dependence. Maternal and paternal history of cigarette-smoking was based on self-report from their respective interviews from 2002–2004.
2.3.5. Parental psychiatric disorder
Lifetime DSM-III-R history of paternal depression, panic disorder, posttraumatic stress disorder, antisocial personality disorder, and conduct disorder were derived from data collected from the 1992 diagnostic interview with the male twins.
Maternal DSM-IV depression and antisocial symptoms were based on data collected from the SSAGA interview. Maternal antisocial symptoms were based on responses to a screen during the interview which queried behavior indicative of consistent irresponsibility (e.g., frequently quitting jobs, failing to pay debts or take care of financial responsibilities), irritability or aggressiveness (i.e., physically attacking anyone, including family members), and disregard for the safety of others (i.e., 4 or more traffic tickets for moving violations), and failure to conform to social norms (i.e., arrests other than for drunk driving or drunken behavior). There was no evidence of an increasing association between latent class and greater number of maternal antisocial behaviors. Therefore maternal antisocial behaviors were modeled as none vs. any symptoms.
2.3.6. Offspring perception of sibling substance use
Offspring reported on substance use of all siblings regardless of sibling participation in the study. Sibling problem drinking was defined by offspring report that their sibling was ever an excessive drinker or that drinking ever caused problems with health, school, family, police or other problems. Sibling illicit drug use was based on offspring report that siblings ever used marijuana, cocaine, stimulants, ecstasy, opiates, hallucinogens, PCP, sedatives, solvents or inhalants, (not counting any if taken as prescribed by a doctor).
2.3.7. Offspring perception of friend substance use
Offspring were asked to report the number of current male/female friends that used alcohol at least once a week, and the number that smoked cigarettes. Friend illicit drug use was based on offspring report that friends ever used marijuana, cocaine, stimulants, ecstasy, opiates, hallucinogens, PCP, sedatives, solvents or inhalants (again, not counting if any were taken as prescribed by a doctor).
2.3.8. Demographics
Offspring gender, age, and ethnicity were based on self-report. Paternal education, marital status, and yearly household income were based on father’s report during the 2002–2003 interviews. Maternal educational level was based on mother’s report.
2.4. Statistical analysis
Latent class analysis using MPLUS (version 5.1; Muthen and Muthen, 2001) was used to examine the clustering of offspring substance abuse or dependence (alcohol and marijuana abuse or dependence and nicotine dependence) and psychiatric disorder (depression, anxiety disorder, conduct disorder). Estimation was performed for 2 through 6 classes.
Bivariate associations between latent class of psychopathology and demographic, early environment, trauma, perceived substance use by sibling and friends, parent substance use, and other psychiatric disorder variables were examined using chi-square tests, controlling for the clustering of family data. Variables with significant bivariate associations (p ≤ .05) were included in a series of 3 multinomial logistic regressions, all adjusted for age, gender and race and constructed according to familial risk, family environmental factors and perceived substance use of friends. Model 1 tested the association between the latent classes and the following familial risk factors: 4-level familial risk variable, maternal marijuana abuse/dependence, paternal smoking, paternal externalizing disorder, maternal depression and sibling alcohol and drug use. Model 2 added the following early environmental factors: father marital status, mother rule consistency, closeness to father and mother and childhood sexual or physical abuse. Model 3 added perceived substance use of friends. Examination of the tetrachoric correlations between covariates indicated no evidence of collinearity in the regression models. Dummy variables representing missing maternal data (for mothers who did not complete an interview) and missing sibling data (for offspring with no siblings) were included in all regressions with maternal or sibling data to adjust for potential non-response bias; in all cases these were non-significant. The Huber White robust variance estimator was used in all regressions to correct for the non-independence of family data. The STATA statistical program was used for all tests (StataCorp, 2009).
3. RESULTS
3.1 Latent Class Analysis
A 4-class solution provided the best fit to the offspring data based on fit statistics from the Akaike Information Criterion (AIC) and the sample-size-adjusted Bayesian Information Criterion (ABIC), which were lower for the 4 class (AIC=4322.21, ABIC=4363.98) than for either the 3 (AIC=4335.47, ABIC=4366.42) or the 5-class solutions (AIC=4325.38, ABIC=4377.98). The most likely class membership probability was used for class assignment. Fifty-three percent of the sample (n=443) was assigned to Class 1, 31% (n=260) was assigned to Class 2, 8% (n=69) to Class 3 and 7% (n=59) to Class 4.
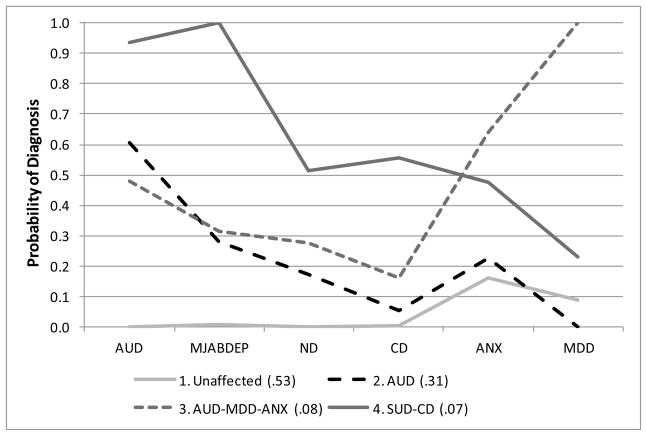
As shown in Figure 2, Class 1 was characterized by near zero probability of all disorders except anxiety and depression, for which probabilities were modest (.16 and .09, respectively). Given this low risk profile, Class 1 was defined as “Unaffected”. In class 2, alcohol abuse and dependence had a high probability (.60), with lower probabilities for marijuana abuse/dependence (.28), nicotine dependence (.17) conduct disorder (.06), and anxiety disorders (.23), and a “0” probability for depression. Thus, Class 2 was defined by its most prominent endorsement as alcohol abuse/dependence (AUD). Class 3 had very high probabilities for anxiety disorders (.64) and major depression (1.0), moderate probability for alcohol abuse/dependence (.48) and lower probabilities for nicotine dependence (.28), cannabis abuse/dependence (.32) and conduct disorder (.16). Class 3 was termed ‘AUD-MDD-ANX’ class. Class 4 had very high probabilities for the substance use disorders: alcohol abuse/dependence (.94), marijuana abuse/dependence (1.0), nicotine dependence (.51) and conduct disorder (.56), but less elevated probability for anxiety and depression (< .5) Class 4 was labeled the SUD-CD class, since poly-substance use disorder and conduct disorder characterized its profile. The intersection of class profiles (i.e., Class 1 with Class 2; Class 2 with Class 3; Class 3 with Class 4) is a visual indication that the classes represent qualitatively distinct patterns of comorbid substance use and psychiatric disorder, rather than gradations of severity.
Figure 2.
Results of latent class analysis of offspring substance use and psychiatric disorder (N=831).
AUD=alcohol abuse or dependence
MJABDEP=marijuana abuse or dependence
ND=nicotine dependence
CD=conduct disorder
ANX=anxiety disorder (social phobia, panic disorder, or generalized anxiety disorder)
MDD=major depressive disorder
Based on patterns of endorsement probabilities, Class 1 (grey line) was defined as ‘Unaffected’, Class 2 (dashed line) was defined as ‘AUD’, Class 3 (dotted line) was defined as ‘AUD-MDD-ANX’ and Class 4 (solid line) was defined as substance use disorder ‘(SUD)-CD’, see text for details.
Numbers in parenthesis are the proportion of offspring in each class
3.2 Sample Characteristics and Bivariate Associations
As shown in Table 1, the mean age of the offspring was 22.7 (SD=4.4), a slight majority (51.5%) was male and 13% was non-Caucasian. There was evidence for an association between father’s 4 group design variable and offspring class assignment, with a disproportionate number of offspring in the SUD-CD class at HG and HE risk.
Table 1.
Prevalence of hypothesized class correlates, by variable grouping and comorbidity class
| Total (n=831) | Class 1 Unaffected (n=443) | Class 2 AUD1 (n=260) | Class 3 AUD-MDD-ANX2 (n=69) | Class 4 SUD-CD3 (n=59) | p-value | |
|---|---|---|---|---|---|---|
| Father’s 4-group design | ||||||
| Group 1, HG & HE | 62.2 | 56.9 | 66.1 | 69.6 | 76.3 | .059 |
| Group 2, HG & LE | 8.4 | 8.6 | 9.6 | 4.3 | 6.8 | |
| Group 3, MG & LE | 9.0 | 9.9 | 8.8 | 5.8 | 6.8 | |
| Group 4, LG & LE | 20.3 | 24.6 | 15.4 | 20.3 | 10.2 | |
| Offspring Demographics | ||||||
| Male gender | 51.5 | 45.1 | 61.5 | 39.1 | 69.5 | < .001 |
| Age, M (S.D.) | 22.7 (4.4) | 21.7 (4.8) | 23.8 (3.7) | 23.8 (4.0) | 23.4 (3.6) | < .001 |
| Non-Caucasian | 13.0 | 15.8 | 11.5 | 8.7 | 3.4 | .020 |
| Parental Demographics‡ | ||||||
| Father’s reported yearly household income < 40,000 (2003) | 18.2 | 20.8 | 13.6 | 18.8 | 18.6 | .138 |
| Father’s reported marital status | ||||||
| Married | 63.2 | 69.5 | 57.0 | 53.6 | 54.2 | .002 |
| Separated, divorced, widowed, or never married | 36.8 | 30.5 | 43.0 | 46.4 | 45.8 | |
| Father’s education | ||||||
| High school or less | 32.7 | 35.7 | 31.9 | 24.6 | 23.7 | .143 |
| Greater than high school | 67.3 | 64.3 | 68.1 | 75.4 | 76.3 | |
| Mother’s education | ||||||
| High school or less | 31.9 | 33.1 | 28.4 | 36.4 | 34.0 | .598 |
| Greater than high school | 68.1 | 66.9 | 71.6 | 63.6 | 66.0 | |
| No maternal interview (missing data on mother) | 16.7 | 16.7 | 16.1 | 20.3 | 15.2 | .861 |
| Offspring report on early environment | ||||||
| Father more strict than other fathers | 38.9 | 39.8 | 35.4 | 45.6 | 40.0 | .412 |
| Mother more strict than other mothers | 43.1 | 44.8 | 39.6 | 45.6 | 42.4 | .581 |
| Father inconsistent rules | 17.8 | 15.1 | 19.1 | 22.4 | 27.8 | .064 |
| Mother inconsistent rules | 18.1 | 12.0 | 21.9 | 30.9 | 32.2 | < .001 |
| Offspring relationship with father not very/not at all close | 14.4 | 11.4 | 15.5 | 18.8 | 28.1 | .004 |
| Offspring relationship with mother not very/not at all close | 6.8 | 4.3 | 7.7 | 13.0 | 13.6 | .006 |
| Childhood physical or sexual abuse | 21.5 | 14.2 | 24.2 | 39.1 | 44.1 | < .001 |
| Parent self-report on lifetime substance use | ||||||
| Paternal alcohol abuse or dependence | 66.9 | 63.1 | 70.3 | 72.5 | 74.6 | .113 |
| Maternal alcohol abuse or dependence | 18.9 | 18.2 | 21.6 | 20.0 | 12.0 | .459 |
| Paternal marijuana abuse or dependence | 35.2 | 33.0 | 37.3 | 36.2 | 42.4 | .448 |
| Maternal marijuana abuse or dependence | 7.6 | 6.1 | 9.2 | 4.3 | 15.2 | .049 |
| Father current or former smoker | 70.0 | 64.5 | 75.3 | 76.8 | 78.0 | .008 |
| Mother current or former smoker | 52.3 | 49.9 | 57.3 | 50.9 | 50.0 | .401 |
| Parent self-report on lifetime psychiatric disorder | ||||||
| Paternal Internalizing disorder (MDD, PD, PTSD) | 25.7 | 24.3 | 23.8 | 36.2 | 32.2 | .133 |
| Depression | 15.7 | 14.3 | 14.2 | 24.6 | 22.0 | .097 |
| Panic Disorder | 2.5 | 2.7 | 2.7 | 1.4 | 1.7 | .904 |
| PTSD | 15.3 | 15.1 | 13.9 | 21.7 | 15.5 | .503 |
| Paternal externalizing disorder (CD, ASPD) | 14.4 | 11.6 | 15.0 | 17.4 | 28.8 | .009 |
| Paternal conduct disorder | 14.4 | 11.6 | 15.0 | 17.4 | 28.8 | .009 |
| Paternal ASPD | 6.5 | 4.1 | 6.9 | 8.7 | 20.3 | < .001 |
| Maternal depression | 29.7 | 22.2 | 33.6 | 53.7 | 41.7 | < .001 |
| Maternal ASPD symptoms | 41.6 | 37.1 | 46.8 | 45.4 | 48.0 | .107 |
| Offspring self-report on illicit substance use 6 or more times ‡‡ | 20.0 | 3.8 | 32.6 | 30.3 | 74.6 | < .001 |
| Offspring report on sibling and friend substance use‡‡‡ | ||||||
| Sibling problem drinker | 24.2 | 17.5 | 27.6 | 47.4 | 34.0 | < .001 |
| Sibling drug use | ||||||
| None | 45.1 | 60.5 | 30.4 | 25.4 | 19.2 | |
| Marijuana or other drug only | 28.1 | 26.3 | 32.2 | 27.3 | 23.4 | < .001 |
| Marijuana and other drugs | 26.8 | 13.2 | 37.4 | 47.3 | 57.4 | |
| Friends smoke | 55.6 | 39.7 | 71.5 | 68.1 | 89.8 | < .001 |
| Friends drink alcohol at least weekly | 73.6 | 60.8 | 90.7 | 79.7 | 87.9 | < .001 |
| Friend drug use – none | 17.0 | 28.7 | 3.5 | 7.6 | 0 | |
| Marijuana or other drug only | 24.4 | 34.3 | 17.8 | 6.0 | 0 | < .001 |
| Marijuana and other drugs | 58.6 | 37.0 | 78.7 | 86.4 | 100.0 | |
| No full siblings | 15.6 | 14.9 | 16.5 | 17.4 | 15.2 | .918 |
AUD = alcohol abuse/dependence.
AUD-MDD-ANX = alcohol abuse/dependence, major depressive disorder and any anxiety disorder (social phobia, panic disorder, generalized anxiety disorder).
SUD – CD = alcohol abuse/dependence, marijuana abuse/dependence, nicotine dependence and conduct disorder.
prevalence of maternal variables based on 692 offspring (Class 1=369, Class 2=218; Class 3=55, Class 4=50) whose mothers who completed interviews
illicit substance use = use of cocaine, stimulants, ecstasy, opiates, hallucinogens, PCP, sedatives, solvents, inhalants
prevalence of sibling variables based on 701 offspring (Class 1=377, Class 2=217, Class 3=57, Class 4=50) who had biological siblings
Offspring and parental demographic variables associated with class assignment were gender, age and race, and father’s marital status. Offspring with any pattern of comorbidity were more likely to have fathers who were not currently married to the biological mother (separated, divorced, or never married), compared to the unaffected class.
Measures of offspring childhood environment which were more likely to be endorsed by members of the affected classes than the unaffected class were maternal rule inconsistency, lack of a close relationship with parents, and childhood physical or sexual abuse.
Regarding parental substance use, maternal marijuana abuse/dependence was strikingly high in the SUD-CD class (15.2%) relative to the other classes, and paternal (but not maternal) history of smoking was more common in all affected classes as compared to the unaffected class.
Parental psychiatric disorders significantly associated with class assignment were paternal externalizing disorders, which were much more common in the SUD-CD class compared to other classes, and maternal depression, which was most common in the AUD-MDD-ANX class.
All sibling and friend substance use variables were significantly associated with class assignment. Rates of perceived sibling polydrug use (defined as use of marijuana plus other drugs), friend smoking and friend polydrug use were particularly elevated in the SUD-CD class.
3.3 Regression results
Several familial risk factors remained significantly associated with class assignment after adjustment for offspring sociodemographics (Table 2). Sibling polydrug use was associated with membership in all affected classes, and sibling use of only marijuana or another drug with membership in the AUD class, as compared to the unaffected class. Maternal depression was associated with membership in the AUD and AUD-MDD-ANX classes, with evidence of an association with the SUD-CD class. The HG-HE risk group was significantly associated with membership in the AUD class, with evidence of an association with the SUD-CD class as compared to the unaffected class. More specific associations were observed for paternal externalizing disorder, which was associated only with the SUD-CD class, and for reports of sibling alcohol problems, which were associated only with membership in the AUD-MDD-ANX class.
Table 2.
Model 1, multinomial logistic regressions showing associations of class membership1 with familial risk factors (father’s 4-group design variable indicating levels of genetic and environmental risk, paternal and maternal substance use and psychiatric disorders and sibling problem substance use) adjusted for offspring demographics1
| Class 2 AUD2 | Class 3 AUD-MDD-ANX3 | Class 4 SUD-CD4 | |
|---|---|---|---|
|
| |||
| OR (95% CI) | OR (95% CI) | OR (95% CI) | |
|
Familial risk factors
| |||
| Father’s 4-group design | |||
| Group 1, HG & HE | 1.63 (1.02–2.59) | 1.25 (0.61–2.57) | 2.18 (0.82–5.75) |
| Group 2, HG & LE | 1.44 (0.68–3.08) | 0.45 (0.11–1.84) | 1.28 (0.31–5.27) |
| Group 3, MG & LE | 1.20 (0.64–2.25) | 0.58 (0.17–1.96) | 1.42 (0.34–5.91) |
| Group 4, LG & LE | 1.0 | 1.0 | 1.0 |
| Maternal marijuana abuse/ dependence | 1.10 (0.53–2.30) | 0.51 (0.14–1.82) | 1.66 (0.60–4.55) |
| Father current or former smoker | 1.39 (0.92–2.12) | 1.33 (0.67–2.66) | 1.12 (0.54–2.29) |
| Paternal externalizing disorder | 1.01 (0.61–1.66) | 1.04 (0.48–2.24) | 2.22 (1.04–4.76) |
| Maternal depression | 1.61 (1.04–2.48) | 3.50 (1.87–6.55) | 1.92 (0.97–3.79) |
| Sibling alcohol problems | 1.01 (0.63–1.63) | 2.42 (1.26–4.64) | 1.07 (0.50–2.31) |
| Sibling drug use | |||
| Marijuana or other drug only | 1.90 (1.27–2.85) | 1.34 (0.67–2.66) | 1.58 (0.70–3.58) |
| Marijuana and other drugs | 3.94 (2.48–6.27) | 3.37 (1.72–6.58) | 6.91 (3.20–14.92) |
|
| |||
|
Demographics
| |||
| Male gender | 2.50 (1.80–3.47) | 1.06 (0.61–1.84) | 4.09 (2.18–7.65) |
| Age 18 and older | 8.45 (4.28–16.68) | 3.24 (1.20–8.76) | 7.67 (1.59–37.07) |
| Non-Caucasian | 0.98 (0.62–1.55) | 0.79 (0.32–1.91) | 0.29 (0.07–1.26) |
Class 1 is reference group; model adjusted for missing data on mothers and siblings,
AUD = alcohol abuse/dependence.
AUD-MDD-ANX = alcohol abuse/dependence, major depressive disorder and any anxiety disorder (social phobia, panic disorder, generalized anxiety disorder).
SUD – CD = alcohol abuse/dependence, marijuana abuse/dependence, nicotine dependence and conduct disorder.
Bold text = statistically significant odds ratios.
The addition of family environment variables to the model (Model 2, displayed in Table 3) yielded evidence that maternal rule inconsistency was associated with membership in all three affected classes. Childhood physical or sexual abuse was associated with membership in the AUD-MDD-ANX and SUD-CD classes, and lack of closeness to father was associated with membership in the SUD-CD class. There was evidence of an association between lack of closeness to mother and membership in the SUD-CD class.
Table 3.
Model 2, multinomial logistic regressions showing associations of class membership1 with familial risk factors (father’s 4-group design variable indicating levels of genetic and environmental risk, paternal and maternal substance use and psychiatric disorders and sibling problem substance use) and family environment adjusted for offspring demographics1
| Class 2 AUD2 | Class 3 AUD-MDD-ANX3 | Class 4 SUD-CD4 | |
|---|---|---|---|
|
| |||
| OR (95% CI) | OR (95% CI) | OR (95% CI) | |
|
Familial risk factors
| |||
| Father’s 4-group design | |||
| Group 1, HG & HE | 1.50 (0.94–2.40) | 1.02 (0.48–2.15) | 1.55 (0.56–4.25) |
| Group 2, HG & LE | 1.40 (0.63–3.08) | 0.42 (0.10–1.73) | 1.05 (0.26–4.20) |
| Group 3, MG & LE | 1.12 (0.59–2.13) | 0.53 (0.16–1.80) | 1.22 (0.27–5.49) |
| Group 4, LG & LE | 1.0 | 1.0 | 1.0 |
| Maternal marijuana abuse/ dependence | 1.11 (0.52–2.37) | 0.53 (0.14–1.94) | 2.15 (0.79–5.86) |
| Father current or former smoker | 1.33 (0.87–2.03) | 1.34 (0.66–2.71) | 1.09 (0.53–2.23) |
| Paternal externalizing disorder | 0.97 (0.57–1.65) | 1.01 (0.47–2.20) | 2.25 (0.98–5.15) |
| Maternal depression | 1.53 (0.99–2.39) | 3.42 (1.78–6.57) | 1.69 (0.83–3.46) |
| Sibling alcohol problems | 1.02 (0.62–1.68) | 2.59 (1.35–4.97) | 0.98 (0.43–2.19) |
| Sibling drug use | |||
| Marijuana or other drug only | 1.76 (1.16–2.67) | 1.26 (0.63–2.52) | 1.51 (0.64–3.57) |
| Marijuana and other drugs | 3.45 (2.13–5.59) | 2.65 (1.36–5.15) | 5.97 (2.65–13.47) |
|
| |||
|
Early family environment
| |||
| Father separated/divorced | 1.28 (0.86–1.90) | 1.01 (0.53–1.91) | 0.87 (0.43–1.75) |
| Mother inconsistent with rules | 1.65 (1.06–2.57) | 2.37 (1.26–4.46) | 3.07 (1.41–6.72) |
| Not close to father | 1.05 (0.62–1.77) | 1.36 (0.62–2.96) | 2.11 (1.01–4.40) |
| Not close to mother | 1.34 (0.66–2.72) | 1.66 (0.56–4.91) | 2.32 (0.79–6.85) |
| Childhood physical/sexual abuse | 1.54 (0.99–2.38) | 3.27 (1.80–5.94) | 3.58 (1.77–7.25) |
|
| |||
|
Demographics
| |||
| Male gender | 2.68 (1.90–3.80) | 1.10 (0.63–1.91) | 4.79 (2.41–9.54) |
| Age 18 and older | 8.36 (4.17–16.76) | 3.31 (1.14–9.65) | 6.45 (1.32–31.43) |
| Non-Caucasian | 1.01 (0.63–1.60) | 0.75 (0.31–1.84) | 0.27 (0.07–0.99) |
Class 1 is reference group; model adjusted for missing data on mothers and siblings,
AUD = alcohol abuse/dependence.
AUD-MDD-ANX = alcohol abuse/dependence, major depressive disorder and any anxiety disorder (social phobia, panic disorder, generalized anxiety disorder).
SUD – CD = alcohol abuse/dependence, marijuana abuse/dependence, nicotine dependence and conduct disorder.
Bold text = statistically significant odds ratios.
When compared with model 1, some of the variables in model 2 lost statistical significance after the addition of family environmental variables, although their odds ratios remained largely unchanged. In the AUD class this was true for the HG-HE risk group and maternal depression. In the SUD-CD class paternal externalizing disorder was no longer significant. However, maternal depression and sibling alcohol use remained significantly associated with membership in the AUD-MDD-ANX class and sibling polydrug use remained significantly associated with each affected class as compared to the non-affected class.
Adjustment for offspring reports of peer substance use in model 3 (Table 4) showed associations of friends’ current smoking with membership in all affected classes and friends’ weekly drinking with membership in the AUD class. Few changes were observed in the magnitude of association between familial risk factors, family environment variables and class membership from Model 2. For example, the association between HG-HE risk group and membership in the AUD class was similar to that observed in models 1 and 2 (ORs =1.63, 1.50, and 1.60, respectively), and evidence for an association between maternal depression and the AUD class, and for an association of lack of paternal closeness with membership in the SUD-CD class remained. All other variables significant in model 2 retained significance after adjusting for friend substance use, and the pattern of association between family environmental variables and class membership was largely unchanged from that observed in model 2.
Table 4.
Model 3, multinomial logistic regressions showing associations of class membership1 with familial risk factors (father’s 4-group design variable indicating levels of genetic and environmental risk, paternal and maternal substance use and psychiatric disorders and sibling problem substance use), family environment and non-family environment adjusted for offspring demographics1
| Class 2 AUD2 | Class 3 AUD-MDD-ANX3 | Class 4 SUD-CD4 | |
|---|---|---|---|
|
| |||
| OR (95% CI) | OR (95% CI) | OR (95% CI) | |
|
Familial risk factors
| |||
| Father’s 4-group design | |||
| Group 1, HG & HE | 1.60 (0.98–2.63) | 1.06 (0.51–2.23) | 1.55 (0.56–4.28) |
| Group 2, HG & LE | 1.33 (0.63–2.82) | 0.38 (0.10–1.50) | 0.95 (0.24–3.78) |
| Group 3, MG & LE | 1.20 (0.60–2.42) | 0.53 (0.16–1.74) | 1.18 (0.25–5.66) |
| Group 4, LG & LE | 1.0 | 1.0 | 1.0 |
| Maternal marijuana abuse/ dependence | 1.22 (0.56–2.65) | 0.57 (0.15–2.20) | 2.81 (0.99–7.96) |
| Father current or former smoker | 1.28 (0.82–2.01) | 1.25 (0.62–2.51) | 1.02 (0.49–2.14) |
| Paternal externalizing disorder | 0.80 (0.46–1.39) | 0.87 (0.40–1.87) | 1.82 (0.81–4.12) |
| Maternal depression | 1.49 (0.93–2.37) | 3.33 (1.72–6.46) | 1.54 (0.74–3.20) |
| Sibling alcohol problems | 1.05 (0.62–1.76) | 2.76 (1.40–5.42) | 1.04 (0.44–2.46) |
| Sibling drug use | |||
| Marijuana or other drug only | 1.59 (1.02–2.46) | 1.18 (0.58–2.40) | 1.37 (0.57–3.30) |
| Marijuana and other drugs | 3.21 (1.91–5.40) | 2.53 (1.29–4.93) | 5.81 (2.52–13.40) |
|
| |||
|
Early family environment
| |||
| Father separated/divorced | 1.26 (0.82–1.94) | 1.03 (0.54–1.99) | 0.91 (0.43–1.90) |
| Mother inconsistent with rules | 1.73 (1.07–2.78) | 2.31 (1.22–4.38) | 2.75 (1.21–6.26) |
| Not close to father | 1.09 (0.63–1.89) | 1.35 (0.62–2.91) | 1.89 (0.88–4.07) |
| Not close to mother | 1.45 (0.66–3.16) | 1.80 (0.58–5.54) | 2.56 (0.82–7.99) |
| Childhood physical/sexual abuse | 1.47 (0.93–2.34) | 3.30 (1.81–6.02) | 3.42 (1.69–6.93) |
|
| |||
|
Non-family environment5
| |||
| Friends smoke | 2.52 (1.73–3.69) | 2.50 (1.26–4.95) | 11.0 (4.20–28.78) |
| Friends drink alcohol at least weekly | 2.99 (1.74–5.14) | 1.28 (0.60–2.72) | 1.26 (0.56–2.86) |
|
| |||
|
Demographics
| |||
| Male gender | 2.63 (1.83–3.77) | 1.06 (0.60–1.87) | 4.75 (2.35–5.60) |
| Age 18 and older | 5.27 (2.42–11.47) | 2.67 (0.89–8.02) | 4.23 (0.85–21.10) |
| Non-Caucasian | 1.30 (0.78–2.18) | 0.96 (0.40–2.31) | 0.37 (0.10–1.44) |
Class 1 is reference group; model adjusted for missing data on mothers and siblings,
AUD = alcohol abuse/dependence.
AUD-MDD-ANX = alcohol abuse/dependence, major depressive disorder and any anxiety disorder (social phobia, panic disorder, generalized anxiety disorder).
SUD – CD = alcohol abuse/dependence, marijuana abuse/dependence, nicotine dependence and conduct disorder.
excludes friend drug use due to empty cells.
Bold text = statistically significant odds ratios.
Compared to the unaffected class, odds of being older than 18 were significantly elevated in the AUD class, with evidence of an association in the other 2 affected classes. Males were significantly more likely to be assigned to the AUD and SUD-CD classes as compared to the unaffected class, but there was no association with male gender for the AUD-MDD-ANX class.
4. DISCUSSION
From latent class analyses of 831 offspring aged 12–32, we identified four distinct patterns of substance use and psychiatric disorder that were characterized as 1) unaffected, 2) alcohol abuse/dependence (AUD), 3) comorbid alcohol abuse/dependence, anxiety disorder and major depressive disorder (AUD-MDD-ANX), and 4) comorbid alcohol abuse/dependence, cannabis abuse/dependence, nicotine dependence and conduct disorder (SUD-CD). With the exception of the unaffected class, all patterns of comorbidity included SUD, with no evidence for an internalizing class without SUD. Thus the clustering of psychiatric disorders in young adult offspring of parents with SUD may most likely be characterized by SUD with or without comorbid disorders.
The present comorbidity profiles are largely consistent with LCA results obtained from other cohorts (Olino et al., 2012; Vaidyanathan et al., 2011) and from our prior modeling of comorbidity from the 1992 diagnostic interview in the full sample of male twins from the VETR (from which our twin families were a subset), in which we found a profile consisting of alcohol and nicotine dependence, a second consisting of mood and anxiety disorders, and a third with high probability of externalizing disorders and illicit drug dependence (Todorov et al., 2006).
We interpret findings in the context of broad confidence intervals due to available sample size and consistency of point estimates. Among familial vulnerability factors, we observed some evidence of specificity in the association between parental disorder and class membership. Paternal illicit drug use disorder was associated with the AUD and SUD-CD class but not the AUD-MDD-ANX class. Paternal externalizing disorder was uniquely associated with the SUD-CD class. Maternal depression was markedly and significantly associated (OR=3.33) with the AUD-MDD-ANX class and less so with the AUD and SUD-CD class (ORs = 1.49, 1.54). Together this suggests some specific familial contributions to comorbid externalizing disorders and to internalizing disorders over and above those in common with SUD. This is somewhat consistent with classical twin designs demonstrating genetic contributions specific to depression, anxiety and to conduct disorder that are not overlapping with genetic influences on SUD (Fu et al., 2007; Kendler et al. 2003).
Perceived sibling polydrug use (but not use of a single substance) was associated with general vulnerability for psychopathology. Sibling substance use has an influence on development of adolescent substance use (Duncan et al., 1996). Given that sibling polydrug use is also a marker of familial vulnerability for substance use, its association with all classes of offspring psychopathology is consistent with classical twin studies demonstrating common genetic vulnerability to substance use disorders, affective disorders and conduct disorder (Lyons et al., 2008; True et al., 1999; Xian et al., 2000; Kendler et al., 2003; Scherrer et al., 2008; Slutske et al., 1998).
Among environmental factors, maternal rule inconsistency and childhood trauma were associated with all comorbidity classes while lack of paternal and maternal closeness was most strongly associated with the SUD-CD class (although the estimates included 1). The association between maternal rule inconsistency and vulnerability for all classes of psychopathology is partly supported by our previous reports that this parenting behavior is a risk factor for offspring nicotine dependence (Scherrer et al., 2012), but is not in line with our earlier report of no association between maternal rule inconsistency and offspring marijuana abuse/dependence (Scherrer et al., 2008). These inconsistent results may reflect the limitation to using a single measure of psychopathology as an outcome. The association between familial risk factors and substance use disorders may best be modeled by considering comorbidity in the outcome. The association between parental closeness and SUD is consistent with evidence of a protective association between parental emotional warmth and externalizing behaviors (Sentse et al., 2009). Additional research is warranted to clarify the independent association between specific parenting behaviors and offspring psychopathology as these offspring age through the period of risk for each type of psychopathology.
Childhood physical/sexual abuse was less strongly associated with the AUD class compared to its association with the AUD-MDD-ANX and SUD-CD classes. This agrees with evidence from previous research showing that comorbid depression, as compared to pure depression, is more strongly associated with childhood trauma (Hovens et al., 2010), and that stressful life events, inclusive but not specific to trauma, are more strongly associated with comorbid SUD and affective disorder as compared to pure SUD (de Graaf et al., 2004).
Perceived peer smoking was associated with each class of comorbidity, while perceived weekly alcohol use by peers was only associated with the AUD class. Perceived peer smoking is an established correlate of young adult substance use disorders (Agrawal et al., 2007; Jenkins et al., 2011). We are not aware of previous reports that perceived peer smoking is associated with affective disorders comorbid with AUD. It is possible that the association with affective disorders is accounted for by comorbid AUD. Further research on the association between peer smoking and affective disorders is warranted.
We have previously reported (Scherrer et al., 2008, 2012) that offspring marijuana abuse/dependence is primarily associated with perceived drug use of friends and offspring nicotine dependence with perceived smoking of friends in models that accounted for perceived use of cigarettes, alcohol and drugs. The current finding that perceived weekly alcohol use by peers was only associated with the AUD class providers further support that type of substance use disorder is associated with type of perceived substance use. It is suggestive that social networks linked to substance use may be specific to those associated with drinking and those associated with drug use and smoking.
Our results suggest some demographic factors impart general vulnerability and others may be specific to subtypes of psychiatric comorbidity. Male gender was associated with AUD and SUD-CD comorbidity profiles. The association between male gender and AUD and SUD-CD classes, but not the AUD-MDD-ANX class, is in line with a considerable literature demonstrating males are more likely to have lifetime alcohol abuse/dependence, poly-substance abuse/dependence and conduct disorder (Kessler et al., 2005; Huang et al., 2006) and less likely to experience lifetime depression and anxiety disorders (Kessler et al., 2005). Whether this reflects differential exposure, as opposed to differential vulnerability, is beyond the scope of this report but is worthy of further investigation.
The present report addresses several gaps in the literature. First, while numerous other studies have reported that parental drug abuse and dependence is a risk factor for offspring licit and illicit drug abuse/dependence, affective disorders and conduct disorder, to our knowledge the present report is novel in demonstrating that familial vulnerability associated with maternal marijuana abuse/dependence and depression is associated with comorbidity among offspring disorders, and a suggestion of specificity of transmission for major depression in particular from mother to child. Second, measured early environmental factors such as parenting practices and childhood trauma are associated with offspring comorbidity even after accounting for familial risk. Third, our report suggests there are both generalized and specific influences of measured environmental risk on subtypes of comorbid psychopathology.
4.1. Strengths
The breadth of the diagnostic survey allowed us to identify multiple, clinically meaningful latent classes of psychiatric disorder in the offspring. Our study is unusual in its simultaneous modeling of familial and measured environmental risk factors. The twin fathers, in particular, are well-characterized by their own reports of psychopathology, obviating the need to rely on maternal report of paternal psychopathology, with their known limitations (Waldron et al 2012). Additional strengths include the large sample size and the non-clinical nature of the samples that enhance generalizability and permit modeling a wide array of environmental factors, while avoiding bias inherent to treatment l samples. The structured, systematic method of data collection reduces interviewer bias.
4.2. Limitations
Not all offspring have passed through that age of risk for substance use disorder and affective disorders. The patterns of comorbidity identified in this high risk sample may limit generalizability to other young adult cohorts at less risk, but these unique data from offspring of twins provide an insight into patterns of familial risk and developmental psychopathology not otherwise available. Analysis of longitudinal data from the offspring is planned to determine how patterns of comorbidity may change as the offspring age. In addition, it is possible that some offspring were misclassified (e.g., those in the LG, LE group), if their fathers developed SUD later in life. However, the fathers were assessed during middle age (avg. age 42), and epidemiological evidence suggests that the likelihood of an onset of SUD in middle age is quite rare (Wagner and Anthony 2002; Compton et al., 2007), particularly among men of European Ancestry (Grant et al., 2012) as is the case for these twin fathers. It is not possible to measure all environmental influences on offspring. For instance the present study modeled perceptions of sibling substance use but not self reported measures from all siblings. Expansion of the shared environment assessment may reveal key parent, sibling and peer level variables that have not been adequately measured. Maternal characteristics, here included as covariates, might be better treated in the context of analyses that model assortative mating, which is beyond the scope of the present report. Finally, temporal relationships cannot be established by these cross sectional data. For instance, parental behavior may be a response to, as well as a predictor of childhood psychopathology, and peer substance use may signify either deviant socialization or peer selection. Future research is warranted to determine if patterns of comorbidity hold as offspring age and to assess the relative contributions of familial and non-familial factors to psychiatric comorbidity in a longitudinal perspective.
4.3. Conclusions
We conclude that subtypes of comorbidity exist in adolescent and young adults and are associated with familial vulnerability. Because parenting, childhood physical/sexual abuse, sibling and peer behaviors remain associated with comorbidity, even after adjusting for familial vulnerability, public health interventions to prevent psychiatric and substance use disorder might also be focused on rearing environment and peer influences.
Acknowledgments
Role of funding source: This study was supported by NIH grants DA14363, AA11998 and AA13717 and by the Department of Veterans Affairs Health Services Research and Development Service and the Cooperative Studies Program (Study 992). Dr. Scherrer is also supported by a Career Development Award-2 from the Department of Veterans Affairs Health Services Research and Development Service. Funding sources had no further role in study design; in the collection, analysis and interpretation of data; in the writing of the report; or in the decision to submit the paper for publication.
The United States Department of Veterans Affairs has provided financial support for the development and maintenance of the Vietnam Era Twin Registry (VETR). Numerous organizations have provided invaluable assistance in the conduct of this study, including: Department of Defense; National Personnel Records Center, National Archives and Records Administration; the Internal Revenue Service; National Opinion Research Center; National Research Council, National Academy of Sciences; the Institute for Survey Research, Temple University. Most importantly, the authors gratefully acknowledge the continued cooperation and participation of the members of the VET Registry and their families. Without their contribution this research would not have been possible.
Footnotes
Contributors: All authors have materially participated in the research and/or manuscript preparation. Authors Scherrer, Grant, Haber, Jacob and Bucholz designed the study and wrote the protocol. Authors McCutcheon and Bucholz undertook the statistical analysis. Authors McCutcheon, Scherrer and Bucholz wrote the first draft of the manuscript. All authors have approved the final manuscript.
Conflict of interest: none
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- Agrawal A, Lynskey MT, Bucholz KK, Madden PA, Heath AC. Correlates of cannabis initiation in a longitudinal sample of young women: the importance of peer influences. Prev Med. 2007;45:31–34. doi: 10.1016/j.ypmed.2007.04.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Barnow S, Schuckit MA, Lucht M, John U, Freyberger HJ. The importance of a positive family history of alcoholism, parental rejection and emotional warmth, behavioral problems and peer substance use for alcohol problems in teenagers: a path analysis. J Stud Alcohol. 2002;63:305–315. doi: 10.15288/jsa.2002.63.305. [DOI] [PubMed] [Google Scholar]
- Bucholz KK, Cadoret R, Cloninger CR, Dinwiddie SH, Hesselbrock VM, Nurnberger JIJ, Reich T, Schmidt I, Schuckit MA. A new, semi-structured psychiatric interview for use in genetic linkage studies: a report on the reliability of the SSAGA. J Stud Alcohol. 1994;55:149–158. doi: 10.15288/jsa.1994.55.149. [DOI] [PubMed] [Google Scholar]
- Chassin L, Pitts SC, DeLucia C, Todd M. A longitudinal study of children of alcoholics: predicting young adult substance use disorders, anxiety and depression. J Abnorm Psychol. 1999;108:106–119. doi: 10.1037//0021-843x.108.1.106. [DOI] [PubMed] [Google Scholar]
- Compton WM, Thomas YF, Stinson FS, Grant BF. Prevalence, correlates, disability, and comorbidity of DSM-IV drug abuse and dependence. Results from the National Epidemiologic Survey on Alcohol and Related Conditions. Arch Gen Psychiatry. 2007;64:566–576. doi: 10.1001/archpsyc.64.5.566. [DOI] [PubMed] [Google Scholar]
- Dawson DA, Goldstein RB, Moss HB, Li TK, Grant BF. Gender differences in the relationship of internalizing and externalizing psychopathology to alcohol dependence: likelihood, expression and course. Drug Alcohol Depend. 2010;112:9–17. doi: 10.1016/j.drugalcdep.2010.04.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- De Graaf R, Bijl RV, ten Have M, Beekman ATF, Vollebergh WAM. Rapid onset of comorbidity of common mental disorders: findings from the Netherlands Mental Health Survey and Incidence Study (NEMESIS) Acta Psychiatr Scand. 2004;109:55–63. doi: 10.1046/j.0001-690x.2003.00222.x. [DOI] [PubMed] [Google Scholar]
- Dinwiddie SH, Reich T. Epidemiological Perspectives on Children of Alcoholics. Rec Dev Alcohol. 1991;9:287–299. [PubMed] [Google Scholar]
- Duncan AE, Sartor CE, Scherrer JF, Grant JD, Heath AC, Nelson EC, Jacob T, Bucholz KK. The association between cannabis abuse and dependence and childhood physical and sexual abuse: evidence from an offspring of twins design. Addiction. 2008;103:990–997. doi: 10.1111/j.1360-0443.2008.02210.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Duncan TE, Duncan SC, Hops H. The role of parents and older siblings in predicting adolescent substance use: modeling development via structural equation latent growth methodology. J Fam Psychol. 1996;10:158–172. [Google Scholar]
- Eisen S, Neuman R, Goldberg J, Rice J, True W. Determining zygosity in the Vietnam Era Twin Registry: an approach using questionnaires. Clin Genet. 1989;35:423–432. doi: 10.1111/j.1399-0004.1989.tb02967.x. [DOI] [PubMed] [Google Scholar]
- Eisen S, True W, Goldberg J, Henderson W, Robinette CD. TheVietnam Era Twin (VET) Registry: method of construction. Acta Genet Med Gemellol (Roma) 1987;36:61–66. doi: 10.1017/s0001566000004591. [DOI] [PubMed] [Google Scholar]
- Fu Q, Heath AC, Bucholz KK, Lyons MJ, Tsuang MT, True WR, Eisen SA. Common genetic risk of major depression and nicotine dependence: the contribution of antisocial traits in a United States male twin cohort. Twin Res Hum Genet. 2007;10:470–478. doi: 10.1375/twin.10.3.470. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grant JD, Verges A, Jackson KM, Trull TJ, Sher KJ, Bucholz KK. Age and ethnic differences in the onset, persistence and recurrence of alcohol use disorder. Addiction. 2012;107:756–765. doi: 10.1111/j.1360-0443.2011.03721.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hartman CA, Lessem JM, Hopfer CJ, Crowley TJ, Stallings MC. The family transmission of adolescent alcohol abuse and dependence. J Stud Alcohol. 2006;67:657–664. doi: 10.15288/jsa.2006.67.657. [DOI] [PubMed] [Google Scholar]
- Hayatbakhsk MR, Mamun AA, Najman JM, O’Callaghan MJ, Bor W, Alati R. Early childhood predictors of early substance use and substance use disorders: prospective study. Aust N Z J Psychiatry. 2008;42:720–731. doi: 10.1080/00048670802206346. [DOI] [PubMed] [Google Scholar]
- Henderson WG, Eisen S, Goldberg J, True WR, Barnes JE, Vitek ME. The Vietnam Era Twin Registry: a resource for medical research. Public Health Rep. 1990;105:368–373. [PMC free article] [PubMed] [Google Scholar]
- Hesselbrock M, Easton C, Bucholz KK, Schuckit M, Hesselbrock V. A validity study of the SSAGA--a comparison with the SCAN. Addiction. 1999;94:1361–70. doi: 10.1046/j.1360-0443.1999.94913618.x. [DOI] [PubMed] [Google Scholar]
- Hovens JGFM, Wiersma JE, Giltary EJ, van Oppen P, Spinhoven P, Pennix BWJH, Zitman FG. Childhood life events and childhood trauma in adult patients with depressive, anxiety and comorbid disorders vs. controls. Acta Psychiatr Scand. 2010;122:66–74. doi: 10.1111/j.1600-0447.2009.01491.x. [DOI] [PubMed] [Google Scholar]
- Huang B, Dawson DA, Stinson FS, Hasin DS, Ruan WJ, Saha TD, Smith SM, Goldstein RB, Grant BF. Prevalence, correlates, and comorbidity of nonmedical prescription drug use and drug use disorders in the United States: Results of the National Epidemiologic Survey on Alcohol and Related Conditions. J Clin Psychiatry 2006. 2006;67:1062–1073. doi: 10.4088/jcp.v67n0708. [DOI] [PubMed] [Google Scholar]
- Hussong A, Bauer D, Chassin L. Telescoped trajectories from alcohol initiation to disorder in children of alcoholic parents. J Abnorm Psychol. 2008;117:63–78. doi: 10.1037/0021-843X.117.1.63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jacob T, Waterman B, Heath A, True W, Bucholz KK, Haber R, Scherrer J, Fu Q. Genetic and environmental effects on offspring alcoholism: new insights using an offspring-of-twins design. Arch Gen Psychiatry. 2003;60:1265–1272. doi: 10.1001/archpsyc.60.12.1265. [DOI] [PubMed] [Google Scholar]
- Jenkins BM, Agrawal A, Lynskey MT, Nelson EC, Madden PAF, Bucholz KK, Heath AC. Correlates of alcohol abuse/dependence in early-onset alcohol-using women. Am J Addict. 2011;20:429–434. doi: 10.1111/j.1521-0391.2011.00151.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kendler KS, Prescott CA, Myers J, Neale MC. The structure of genetic and environmental risk factors for common psychiatric and substance use disorders in men and women. Arch Gen Psychiatry. 2003;60:929–937. doi: 10.1001/archpsyc.60.9.929. [DOI] [PubMed] [Google Scholar]
- Kessler RC, Chiu WTAM, Demier O, Walters EE. Prevalence, severity, and comorbidity of twelve-month DSM-IV disorders in the National Comorbidity Survey Replication (NCS-R) Arch Gen Psychiatry. 2005;62:617–627. doi: 10.1001/archpsyc.62.6.617. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lindhout IE, Markus MT, Hoogendijk TH, Boer F. Temperament and parental child-rearing style: unique contributions to clinical anxiety disorders in childhood. Eur Child Adolesc Psychiatry. 2009;18:439–446. doi: 10.1007/s00787-009-0753-9. [DOI] [PubMed] [Google Scholar]
- Lyons M, Hitsman B, Xian H, Panizzon MS, Jerskey BA, Santangelo S, Grant MD, Rende R, Eisen S, Eaves L, Tsuang MT. A twin study of smoking, nicotine dependence, and major depression in men. Nicotine Tob Res. 2008;10:97–108. doi: 10.1080/14622200701705332. [DOI] [PubMed] [Google Scholar]
- Marmorstein NR, Iacono WG, McGue M. Alcohol and illicit drug dependence among parents: associations with offspring externalizing disorders. Psychol Med. 2009;39:149–155. doi: 10.1017/S0033291708003085. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Martin G, Bergen HA, Roeger L, Allison S. Depression in young adolescents: investigations using 2 and 3 factor versions of the Parental Bonding Instrument. J Nerv Ment Dis. 2004;192:650–657. doi: 10.1097/01.nmd.0000142028.10056.c6. [DOI] [PubMed] [Google Scholar]
- Morgan P, Desai RA, Potenza MN. Gender-related influences of parental alcoholism on the prevalence of psychiatric illnesses: analysis of the National Epidemiologic Survey on Alcohol and Related Conditions. Alcohol Clin Exp Res. 2010;34:1759–1767. doi: 10.1111/j.1530-0277.2010.01263.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Muthen L, Muthen B. Mplus User’s Guide. 3. Muthen & Muthen; Los Angeles: 2001. [Google Scholar]
- Olino TM, Klein DN, Farmer RF, Seeley JR, Lewinsohn PM. Examination of the structure of psychopathology using latent class analysis. Compr Psychiatry. 2012;53:323–332. doi: 10.1016/j.comppsych.2011.05.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Robins LN. Diagnostic grammar and assessment: translating criteria into questions. Psychol Med. 1989;19:57–68. doi: 10.1017/s0033291700011028. [DOI] [PubMed] [Google Scholar]
- Robins LN, Schoenberg SP, Holmes SJ, Ratcliff KS, Benham A, Works J. Early home environment and retrospective recall: a test for concordance between siblings with and without psychiatric disorders. Am J Orthopsychiatry. 1985;55:27–41. doi: 10.1111/j.1939-0025.1985.tb03419.x. [DOI] [PubMed] [Google Scholar]
- Sarason BR, Pierce GR, Shearin EN, Sarason IG, Waltz JA, Poppe L. Perceived social support and working models of self and actual others. J Pers Soc Psychol. 1991;60:273–287. [Google Scholar]
- Scherrer JF, Grant JD, Duncan AE, Pan H, Waterman B, Jacob T, Haber JR, True WR, Heath AC, Bucholz KK. Measured environmental contributions to cannabis abuse/dependence in an offspring of twins design. Addict Behav. 2008;33:1255–1266. doi: 10.1016/j.addbeh.2008.05.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Scherrer JF, Xian H, Pan H, Pergadia ML, Madden PA, Grant JD, Sartor CE, Haber JR, Jacob T, Bucholz KK. Parent, sibling and peer influences on smoking initiation, regular smoking and nicotine dependence. Results from a genetically informative design. Addict Behav. 2012;37:240–247. doi: 10.1016/j.addbeh.2011.10.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Scherrer JF, Xian H, Lyons MJ, Goldberg J, Eisen SA, True WR, Tsuang M, Bucholz KK, Koenen KC. Posttraumatic stress disorder; combat exposure; and nicotine dependence, alcohol dependence, and major depression in male twins. Compr Psychiatry. 2008;49:297–304. doi: 10.1016/j.comppsych.2007.11.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sentse M, Veenstra R, Lindenberg S, Verhulst FC, Ormel J. Buffers and risks in temperament and family for early adolescent psychopathology: generic, conditional, or domain-specific effects? The TRAILS Study. Dev Psychol. 2009;45:419–430. doi: 10.1037/a0014072. [DOI] [PubMed] [Google Scholar]
- Slutske WS, Heath AC, Dinwiddie SH, Madden PA, Bucholz KK, Dunne MP, Statham DJ, Martin NG. Common genetic risk factors for conduct disorderand alcohol dependence. J Abnorm Psychol. 1998;107:363–374. doi: 10.1037//0021-843x.107.3.363. [DOI] [PubMed] [Google Scholar]
- Sher KJ. Children of Alcoholics: A Critical Appraisal of Theory and Research. The University of Chicago Press; Chicago: 1991. [Google Scholar]
- Statacorp. Stata Statistical Software: Release 11.0. StataCorp LP; College Station, TX: 2009. [Google Scholar]
- Sullivan PF, Kendler KS. Typology of common psychiatric syndromes. An empirical study. Br J Psychiatry. 1998;173:312–319. doi: 10.1192/bjp.173.4.312. [DOI] [PubMed] [Google Scholar]
- Thompson RGJ, Lizardi D, Keyes KM, Hasin DS. Childhood or adolescent parental divorce/separation, parental history of alcohol problems, and offspring lifetime alcohol dependence. Drug Alcohol Depend. 2008;98:264–269. doi: 10.1016/j.drugalcdep.2008.06.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Todorov AA, Lynskey MT, Grant JD, Scherrer JF, Todd RD, Bucholz KK. Psychiatric comorbidity and progression in drug use in adult male twins: implications for the design of genetic association studies. Addict Behav. 2006;31:948–961. doi: 10.1016/j.addbeh.2006.03.046. [DOI] [PubMed] [Google Scholar]
- True WR, Heath AC, Scherrer JF, Xian H, Lin N, Eisen SA, Lyons MJ, Goldberg J, Tsuang MT. Interrelationship of genetic and environmental influences on conduct disorder and alcohol and marijuana dependence symptoms. Am J Med Genet. 1999;88:391–397. doi: 10.1002/(sici)1096-8628(19990820)88:4<391::aid-ajmg17>3.0.co;2-l. [DOI] [PubMed] [Google Scholar]
- Tsuang MT, Lyons MJ, Eisen SA, Goldberg J, True W, Lin N, Meyer JM, Toomey R, Faraone SV, Eaves L. Genetic influences on DSM-III-R drug abuse and dependence: a study of 3,372 twin pairs. Am J Med Genet. 1996;67:473–477. doi: 10.1002/(SICI)1096-8628(19960920)67:5<473::AID-AJMG6>3.0.CO;2-L. [DOI] [PubMed] [Google Scholar]
- Tsuang MT, Lyons MJ, Meyer JM, Doyle T, Eisen SA, Goldberg J, True W, Lin N, Toomey R, Eaves L. Co-occurrence of abuse of different drugs in men: the role of drug-specific and shared vulnerabilities. Arch Gen Psychiatry. 1998;55:967–972. doi: 10.1001/archpsyc.55.11.967. [DOI] [PubMed] [Google Scholar]
- Vaidyanathan U, Patrick CJ, Iacono WG. Patterns of comorbidity among mental disorders: a person-centered approach. Compr Psychiatry. 2011;52:527–535. doi: 10.1016/j.comppsych.2010.10.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wagner FA, Anthony JC. From first drug use to drug dependence: developmental periods of risk for dependence upon marijuana, cocaine, and alcohol. Neuropsychopharmacology. 2002;26:479–488. doi: 10.1016/S0893-133X(01)00367-0. [DOI] [PubMed] [Google Scholar]
- Waldron M, Madden PA, Nelson EC, Knopik VS, Glowinski AL, Grant JD, Lynskey MT, Jacob T, Sher KJ, Bucholz KK, Heath AC. The interpretability of family history reports of alcoholism in general community samples: findings in a midwestern U.S. Twin birth cohort. Alcohol Clin Exp Res. 2012;36:590–597. doi: 10.1111/j.1530-0277.2011.01698.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Webster-Stratton C, Hammond M. Marital conflict management skills, parenting style, and early-onset conduct problems: processes and pathways. J Child Psychol Psychiatry. 1999;40:917–927. [PubMed] [Google Scholar]
- Xian H, Scherrer JF, Pergadia ML, Madden PAF, Grant JD, Sartor CE, Haber JR, Jacob T, Bucholz KK. Contribution of parental psychopathology to offspring smoking and nicotine dependence in a genetically informative design. J Stud Alcohol Drugs. 2010;71:664–673. doi: 10.15288/jsad.2010.71.664. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Xian H, Chantarujikapong SI, Scherrer JF, Eisen SA, Lyons MJ, Goldberg J, Tsuang M, True WR. Genetic and environmental influences on posttraumatic stress disorder, alcohol and drug dependence in twin pairs. Drug Alcohol Depend. 2000;61:95–102. doi: 10.1016/s0376-8716(00)00127-7. [DOI] [PubMed] [Google Scholar]