EXECUTIVE SUMMARY
Influenza is a significant public health issue. Annual influenza-associated deaths range from 3,000 to 49,000 according to recent estimates, and more than 200,000 people are hospitalized each year for respiratory illnesses and heart conditions associated with seasonal influenza infections. Immunization is the most effective method for preventing infection from influenza and possible hospitalization or death. The Advisory Committee on Immunization Practices (ACIP) recommends that all people $6 months of age receive annual influenza vaccination. In addition, vaccination of all health-care personnel (HCP) is a particular focus of recommendations by the U.S. Department of Health and Human Services (HHS), the Centers for Disease Control and Prevention (CDC), and other health-care and public health agencies and professional organizations. Despite these recommendations, influenza immunization rates for HCP in the United States remain below the Healthy People 2020 (HP 2020) annual goal for influenza vaccine coverage.
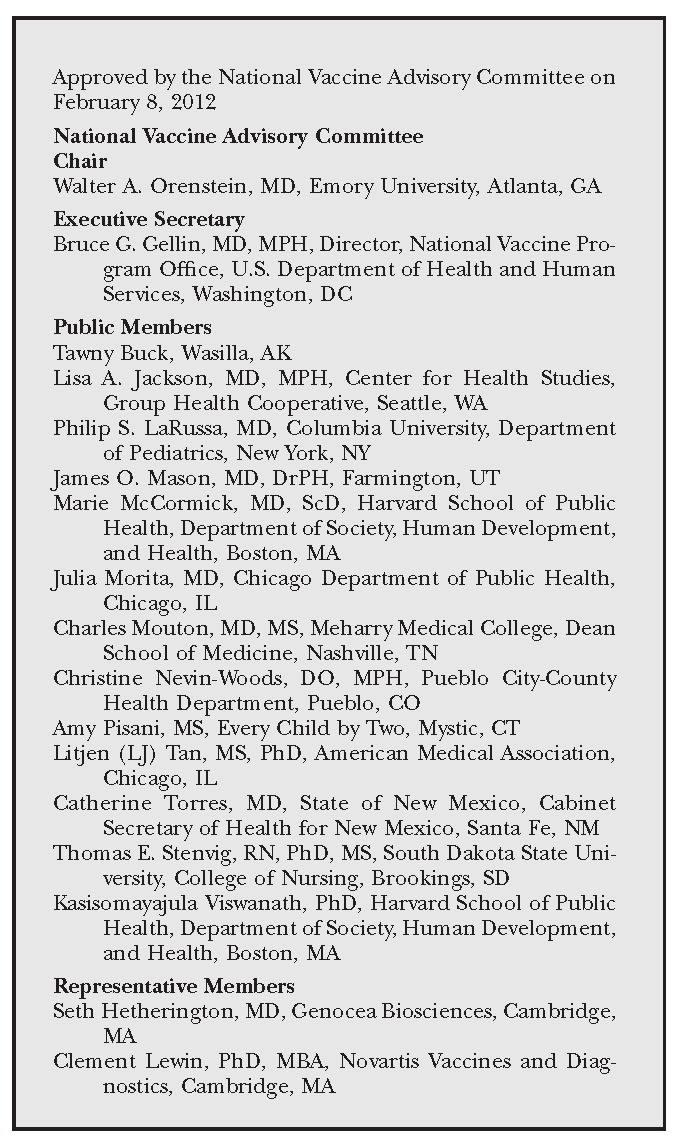
To address this gap in immunization rates for HCP, the HHS Assistant Secretary for Health (ASH) directed the National Vaccine Advisory Committee (NVAC) to develop recommendations and strategies for the specific purpose of achieving the HP 2020 coverage goal. These issues were deliberated on by a Health Care Personnel Influenza Vaccination Subgroup, a subgroup of the NVAC Adult Immunization Working Group. Based on the analysis and evaluation presented by the subgroup, these recommendations were voted on and approved by the majority of NVAC members on February 8, 2012.
These recommendations include a tiered set of strategies for achieving the HP 2020 annual goal, including implementing and managing influenza prevention and vaccination programs, measuring and reporting vaccination coverage, and addressing issues surrounding the implementation of employer requirements for HCP vaccination. In approving these recommendations, NVAC maintained that HCP who are committed to promoting patients' welfare and the health of the public, and to safeguarding their own and their colleagues' well-being, have an ethical responsibility to take appropriate measures, including vaccination, to prevent the spread of influenza infections in health-care settings. NVAC realizes that health-care employers (HCEs) range in their scope of practice, from traditional hospital settings to in-home health-care settings, and no single strategy for improving immunization rates would be appropriate for all HCP. Thus, NVAC presents the following set of tiered options that can be applied to most health-care settings to improve immunization rates of HCP to reach the HP 2020 annual influenza vaccine coverage goal for HCP:
Recommendation 1: NVAC recommends that HCEs and facilities establish comprehensive influenza infection prevention programs that include education of HCP as a key component. Comprehensive influenza infection prevention plans are recommended by CDC as an essential step for all HCEs and facilities to achieve the HP 2020 influenza vaccine coverage goal. NVAC recommends that the ASH strongly urge all HCEs and facilities to adopt these recommendations.
Recommendation 2: NVAC recommends that HCEs and facilities integrate influenza vaccination programs into their existing infection prevention programs or occupational health programs. NVAC also recommends that the ASH assure that this recommendation is implemented in HHS facilities and services (including the Public Health Service [PHS], HHS staff, and Federally Qualified Health Centers [FQHCs]) and strongly urges all HCEs and facilities to do the same.
Recommendation 3: NVAC recommends that the ASH encourage CDC and the Centers for Medicare and Medicaid Services (CMS) to continue efforts to standardize the methodology used to measure HCP influenza vaccination rates across settings. The ASH should also work with CMS to facilitate adoption of this recommendation.
Recommendation 4: For those HCEs and facilities that have implemented Recommendations 1, 2, and 3 and still have not consistently achieved the HP 2020 goal for influenza vaccination coverage of HCP in an efficient and timely manner, NVAC recommends that HCEs strongly consider an employer requirement for influenza immunization. In addition to medical exemptions, HCEs may consider other exemptions in their requirement policies. NVAC also recommends that the ASH assure that this recommendation is implemented in HHS facilities and services (including PHS, HHS staff who are HCP, and FQHCs) and urge all other HCEs and facilities to do the same.
Recommendation 5: NVAC recommends that the ASH encourage ongoing efforts to develop new and improved influenza vaccines and vaccine technologies including support for research, development, and licensure of influenza vaccines with improved effectiveness and duration of immunity, as well as steps that improve the immunogenicity and rapid production of existing influenza vaccines.
INTRODUCTION AND BACKGROUND
NVAC advises HHS on issues of vaccine policy. In 2010, the ASH and the National Vaccine Program Office charged NVAC with recommending strategies to achieve the HP 2020 objective for annual influenza vaccination coverage among HCP.1 The HP 2020 objective is intended to reduce influenza infection in HCP and their patients, thereby decreasing the physical and financial burden on the overall health-care system. NVAC established the Health Care Personnel Influenza Vaccination Subgroup, a subgroup of the Adult Immunization Working Group, to examine these issues. The Working Group developed the recommendations presented in this report based on an extensive review of the literature; discussions; and input from subject-matter experts, relevant stakeholders, and the public. A summary of stakeholder and public comments is found in the Appendix. The findings, conclusions, and recommendations of the Working Group were presented to and adopted by NVAC on February 8, 2012.
Definitions
HCP (health-care personnel), HCEs (health-care employers), and employer requirements are referred to throughout this report. The following definitions of these terms serve as the basis for discussion in this report:
HCP refers to all paid and unpaid people working in health-care settings who have the potential for exposure to patients and/or to infectious materials, including body substances, contaminated medical supplies and equipment, contaminated environmental surfaces, or contaminated air. HCP might include, but are not limited to, physicians, nurses, nursing assistants, therapists, technicians, emergency medical service personnel, dental personnel, pharmacists, laboratory personnel, autopsy personnel, students and trainees, contractual staff not employed by the health-care facility, and people (e.g., clerical, dietary, housekeeping, laundry, security, maintenance, billing, and volunteers) not directly involved in patient care but potentially exposed to infectious agents that can be transmitted to and from HCP and patients. Thus, HCP includes a range of those directly, indirectly, and not involved in patient care who have the potential for transmitting influenza to patients, other HCP, and others.
This definition for HCP is in alignment with the definition provided in the “HHS Action Plan to Prevent Healthcare-Associated Infections: Influenza Vaccination of Healthcare Personnel,”2 which in turn was adapted from the CDC/ACIP definition outlined in “Influenza Vaccination of Health-Care Personnel: Recommendations of the Healthcare Infection Control Practices Advisory Committee (HICPAC) and the Advisory Committee on Immunization Practices (ACIP), 2006.”3
HCE refers to a person or entity that has control over the wages, hours, and working conditions of HCP in health-care settings.4 Health-care settings include, but are not limited to, acute-care hospitals; adult day programs or facilities, ambulatory surgical facilities, and long-term care facilities (LTCFs), such as nursing homes and skilled nursing facilities; outpatient clinics and physicians' offices; and rehabilitation centers, residential health-care facilities, home health-care agencies, urgent-care centers, and outpatient clinics.
Employer requirements: For the purpose of this report, NVAC does not stipulate the scope and content of such requirements; it should be a decision made by the HCEs based on the concerns and needs of their HCP, their patients, and the public.
Influenza: a significant public health issue
In the U.S., CDC estimates that 3,000 to 49,000 influenza-associated deaths occur each year5 and, on average, more than 200,000 people are hospitalized each year for respiratory illnesses and heart conditions associated with seasonal influenza infections.6 Serious morbidity and mortality from influenza infection can occur in any person regardless of age. However, the following groups of people, who are often under the care of HCP in health-care settings, are at higher risk for severe outcomes due to complications from influenza infection:7
People older than 65 years of age: From 1979 to 2000, studies showed that influenza hospitalization rates for elderly patients were two to 14 times higher than in the general population, and more than 90% of the patients who died from influenza infections were elderly.6,8
Pregnant women: Pregnant women are at a higher risk of complications from influenza.9–11 In addition, newborns born from vaccinated mothers are less likely to become infected with influenza during infancy and are less likely to be born premature than those from unvaccinated mothers.12
People with chronic medical conditions: During periods of high influenza incidence, hospitalizations of adults with diabetes, cardiovascular disease, or chronic lung, renal, or liver conditions may increase two- to fivefold, depending on age group.13 Influenza-related hospitalization rates in adults, <65 years of age with cancer are significantly higher than for the general population, making this population a particularly high-risk group. In addition, all cancer patients, but especially those, <65 years of age, are at higher risk of influenza-related deaths.14
Residents of LTCFs: Residents in LTCFs have a greater risk for infection because they live in close proximity within closed settings and have contact with numerous caregivers.15 Many residents may have multiple underlying medical problems, and health-care-associated influenza outbreaks in LTCFs are often associated with significant morbidity and mortality.16–18
Newborns and infants, especially those in neonatal intensive care units: Children younger than six months of age cannot be immunized for influenza and are at high risk of hospitalization for influenza.19,20
Immunization: the most effective way to protect patients and HCP from influenza infections
NVAC's recommendations are built on the principles that influenza is a significant public health threat, that the influenza vaccine is safe and effective, and that vaccination is currently the most effective mechanism for preventing influenza infection.
According to ACIP, “The most effective strategy for preventing influenza is annual vaccination,” and routine influenza vaccination is now recommended for all people ≥6 months of age.11 ACIP and the Healthcare Infection Control Practices Advisory Committee (HICPAC), in addition to many other medical organizations and leaders, recommend that all HCP in the U.S. be vaccinated annually against influenza, establishing influenza vaccination as a standard of care.21 Immunizing HCP has two potential benefits: (1) directly protecting HCP from influenza for their own health, allowing them to continue to work and, thus, minimizing the disruption of health-care services; and (2) indirectly protecting other HCP and patients with whom they come in contact who may be at high risk for complications of influenza.15,22–25
Vaccination is the best-documented and most effective intervention to prevent influenza transmission.26 Determining the overall effects of HCP vaccination on patient outcomes is methodologically challenging, and the outcomes measured often vary between studies. Findings specific to the effectiveness of HCP influenza vaccination in protecting patients vary by setting, year, and population studied and may lead to differing interpretations of the available data.3,24,27–30 Collectively, the impact of HCP vaccination on patient morbidity and mortality in health-care settings requires continued investigation. While the Working Group discussed several scientific studies that evaluated the impact of HCP influenza vaccination on reducing health-care-associated influenza infection among patients, evaluating the full merits of HCP vaccination was not included in the charge of the Working Group; therefore, it is not directly addressed in this report.
HCP immunization rates are well below the HP 2020 goal
HCP vaccination rates vary from year to year but are consistently well below the HP 2020 goal. For the 2009–2010 influenza season, 61.9% of HCP were vaccinated; for the 2010–2011 season, 63.5% were vaccinated. In a 2011 CDC report, vaccination coverage was reported to be higher among HCP working in hospitals (71.1%) than among HCP working in ambulatory or outpatient centers (61.5%), patient homes (53.6%), and other health-care settings (46.7%).31
Vaccination coverage among physicians and dentists (84.2%) was similar to coverage among nurse practitioners and physician assistants (82.6%), and was significantly higher than for those working in all other occupational groups. Coverage also was significantly higher among HCP aged $60 years (74.2%) compared with those aged 18–29 years (56.4%) and 30–44 years (57.8%).31
FINDINGS AND RECOMMENDATIONS
Implementing a comprehensive influenza prevention program for HCP in all health-care settings
HCP can acquire influenza infection and transmit it to patients.
Exposure to influenza infection in health-care settings is an occupational hazard for HCP. Influenza infections range from asymptomatic/mild infections to severe infections and death. Asymptomatic HCP, along with those who come to work ill, can potentially transmit the virus to colleagues, their families, and patients. One study looking at serological testing of HCP in acute care hospitals found that 120 of 518 (23%) of HCP tested positive for influenza infection.29,32 Of these, 71 of 120 (59%) could not recall having an influenza infection, and 32 of 120 (27%) did not report experiencing any respiratory infection.32
Patients who are at higher risk for influenza and its associated complications have frequent, close contact with HCP while seeking inpatient and outpatient medical services. Some of these patients may not always be easily identified as high risk. While unvaccinated HCP have been implicated as sources of influenza infections in outbreaks among adults and children in both acute and long-term care settings,16,24,30 attribution of the source of such infections is often difficult. One study at the University of Virginia Health System, a tertiary care center, reported an association between increased influenza vaccination among HCP (defined as hospital employees) and decreased health-care-associated influenza in hospitalized patients. In this study, a rise in HCP vaccination rates from 4% to 67% was associated with a significant decrease in the proportion of laboratory-confirmed influenza cases in HCP from 42% to 9% and a decrease in the number of health-care-associated influenza cases in hospitalized patients (32% to 0%).33 However, because influenza vaccination was part of a comprehensive multipronged intervention, these results cannot be attributed solely to the vaccination of HCP. Therefore, HCP immunization should be considered a necessary and vital component of infection-control programs intended to protect those at high risk from severe influenza infection. Patients have the right to be protected against influenza infection transmission by the HCP responsible for their care.
Comprehensive infection prevention plans that include immunization for influenza are the most effective method to protect HCP and their patients from infection.
Other infection prevention practices, when used in conjunction with influenza immunization, may enhance the protection of HCP and their patients from infection. A comprehensive influenza prevention plan should include, but not be limited to, (1) offering free influenza vaccination to all HCP across varying work shifts, locations, and days; (2) providing targeted, interactive education programs annually to all HCP to explain the impact of influenza, particularly among high-risk patients, and to address misconceptions and concerns about the safety of influenza vaccination; and (3) educating HCP about the importance of influenza vaccination in promoting patient and employee safety.3,34
A comprehensive influenza prevention plan should include implementation of hand and respiratory hygiene and cough etiquette, screening for and appropriate isolation of HCP and patients identified with acute respiratory tract infections, appropriate management of ill HCP, adherence to standard precautions for all patient care activities as well as implementation of transmission-based precautions as indicated, and implementation of engineering and environmental infection prevention measures as outlined in CDC's “Prevention Strategies for Seasonal Influenza in Health-care Settings.”34
Comprehensive infection prevention plans that include voluntary influenza vaccination have been shown to improve influenza vaccination rates in HCP in some health-care facilities.
St. Jude Children's Research Hospital in Memphis, Tennessee, specializes in the care of severely immunocompromised children, and essentially all patients are at a significant risk for complications from severe influenza infection. The hospital achieved and sustained high voluntary compliance to influenza vaccination among HCP (defined in this analysis as any staff member with direct patient care duties) due to implementation of a comprehensive program that included focused educational campaigns, increased availability of vaccine, and individual follow-up with an infection-control officer. Prior to the introduction of a comprehensive program, the hospital reported HCP vaccination rates of 44.7%. However, the introduction of a comprehensive program was successful in increasing and sustaining rates of 80%–96%. The program's success was attributed to educating HCP on the importance of HCP vaccination in protecting vulnerable patients, an idea reflected in surveyed HCP's attitudes toward vaccination. On the other hand, it was also acknowledged that these results may be unique to St. Jude Children's Research Hospital due to its high-risk patient population and the impact of the hospital's medical director, who championed a culture of individual accountability.35
The Iowa Healthcare Collaborative (IHC), a provider-led organization, initiated a program to increase influenza vaccination rates among HCP (defined as paid employees) in acute care hospitals throughout the state. This program included a number of evidence-based strategies for improving HCP vaccination rates, including common educational materials and a data reporting system that enabled individual hospitals to track their performance compared with the target vaccination rate of 95% established by the IHC. Within two years, the median vaccination rate had increased from 73% to 82% (2006–2008).36 A follow-up report tracking the program's success showed that median vaccination rates among acute care hospitals had reached 93% after four influenza seasons. Several factors may have contributed to the program's overall success including strong leadership support, strong collaborations with the Iowa Infection Control and Epidemiology Education and Consultation program, a challenging and time-limited vaccination target goal, reporting of vaccination coverage rates among hospitals, and the use of several evidence-based strategies for increasing vaccinations among HCP. In addition, several hospitals reported implementing mandatory vaccination policies in the fourth influenza season, and this strategy likely contributed to a number of hospitals reaching their target goal. In this study, the median vaccination rate in hospitals that implemented mandatory policies was 96% vs. 87% in hospitals without such policies.37
Conclusions.
Annual influenza vaccination has been determined by many health-care organizations to be the most effective strategy for preventing influenza. Coupling vaccination with a comprehensive infection prevention plan may improve protection of HCP and their patients from influenza infection. Influenza vaccination programs that include a number of evidence-based strategies can achieve increased rates if they are strongly supported by leadership and are backed by an aggressive focus on vaccination as a patient safety measure. However, these strategies may not be as effective in all health-care settings, and HCEs may need to employ additional strategies to reach target vaccination rates among all HCP.
NVAC believes that HCEs and HCP have a joint responsibility to protect patients by adopting all reasonable interventions to reduce the transmission of influenza, including vaccination.
Recommendation 1.
NVAC recommends that HCEs and facilities establish comprehensive influenza infection prevention programs that include education of HCP as a key component. Comprehensive influenza infection prevention plans are recommended by CDC as an essential step for all HCEs and facilities to achieve the HP 2020 influenza vaccine coverage goal. NVAC recommends that the ASH strongly urge all HCEs and facilities to adopt these recommendations.
Managing influenza vaccination programs
Comprehensive influenza vaccination programs are multifaceted and have proven to be successful.
Vaccination of HCP should be part of a multifaceted, comprehensive influenza prevention program that emphasizes all aspects of an influenza prevention program, such as full, visible leadership support with the expectation for vaccination fully and clearly communicated to all HCP; provision of adequate resources and support for the HCP vaccination program; and inclusion of all practices necessary to reduce the spread of influenza in health-care settings, including patient isolation, use of personal protective equipment, applying hand and respiratory hygiene and cough etiquette, and restriction of ill visitors and ill HCP.38 These practices have been proven to reduce the spread of influenza. Additionally, leadership support and the provision of adequate resources have been shown to have a direct impact on HCP compliance with disease prevention strategies.
CDC finds that successful HCP vaccination programs are multifaceted and that single-component interventions will likely be minimally effective in achieving desired vaccination coverage levels. CDC recommends the following:3
Education and campaigns: Basic knowledge about influenza and influenza vaccination has been associated with vaccine receipt. Participation in structured in-service education or conferences has been associated with improved vaccination rates.
Role models: Vaccination of senior medical staff or opinion leaders has been associated with higher vaccination acceptance among staff.
Improved access: Removing administrative barriers and providing vaccine in locations and at times easily accessible by HCP can substantially improve vaccine acceptance.
Measurement and feedback: Posting of vaccination coverage levels in different areas of the hospital is a component of successful vaccination programs.
Influenza vaccination programs are cost-effective and cost-saving approaches to influenza prevention.
Three entities have offered evidence to support that influenza vaccination programs are cost-effective and cost-saving approaches to influenza prevention.
The National Business Group on Health, representing approximately 330 large employers who provide coverage to 55 million Americans, reports that direct medical costs of influenza average $10.4 billion annually and that lost earnings due to illness and loss of life associated with influenza epidemics average $16.3 billion each year.39
The National Foundation for Infectious Diseases cites studies in which vaccination has been found to be a highly cost-effective and cost-saving measure. One study reported those who received the influenza vaccine had 25% fewer episodes of respiratory illness, 43% fewer days of sick leave from work due to respiratory illness, and 44% fewer visits to physicians' offices for upper respiratory illness than those who received a placebo.40
CDC finds that vaccination can reduce medical costs and indirect costs such as those from lost work productivity. The report states that vaccination could result in 13%–44% fewer health-care provider visits, 18%–45% fewer lost workdays, 18%–28% fewer days working with reduced effectiveness, and a 25% decrease in antibiotic use for influenza-like illness (ILI). In addition, vaccination may contribute to $60–$4,000 in savings per illness in healthy adults,65 years of age depending on the cost of vaccination, the influenza attack rate, and vaccine effectiveness against ILI.3
Employers of HCP will encounter barriers to immunizing HCP.
An in-depth literature review describing universal influenza vaccination attitudes among hospital-based HCP identified a number of reasons commonly cited for not receiving the vaccine. In 21 studies in nine countries, the authors reported that the five most frequently reported categories for vaccine refusal included (1) fear of adverse reactions, (2) lack of concern (i.e., perception that influenza does not pose a serious public health risk), (3) inconvenient delivery, (4) lack of perception of own risk, and (5) doubts regarding vaccine efficacy. These studies also found that HCP are more likely to be vaccinated to protect themselves against influenza than to be vaccinated for the protection of patients.41 Similarly, a recent CDC report found that beliefs regarding influenza and influenza vaccination differ between vaccinated and unvaccinated HCP. This study found that 92.7% of vaccinated HCP believed that getting vaccinated could protect them from influenza infection, while only 54.2% of those who were unvaccinated shared that belief. Notably, the CDC study also indicated that 55.4% of unvaccinated HCP do not believe that vaccination better protects those around them from influenza infection. The most important factor facilitating vaccine acceptance was a desire for self-protection, with previous receipt of influenza vaccine, perceived effectiveness of vaccine, and older age also contributing to vaccine acceptance.31 Collectively, these studies highlight the importance of educating HCP on the seriousness of influenza as a public health threat and the importance of vaccination as a safe and important infection prevention measure.
The use of a signed declination statement for HCP who refuse vaccination has had mixed results in increasing vaccination rates.
The Society for Healthcare Epidemiology of America (SHEA) supported the use of signed declination statements in 2005. As more data on the impact of these statements became available, showing only modest increases in vaccination rates, SHEA has altered its position, now stating that declination statements work best as part of a comprehensive program.42 The American Academy of Pediatrics notes that the use of declination statements in 22 hospitals resulted in only a modest increase in influenza immunization.43 The American College of Occupational and Environmental Medicine finds mixed results from the use of declination statements to document vaccine refusal, from improved rates to no effect.44
Education and training are vital components of a comprehensive influenza vaccination program.
Providing comprehensive education and training about the risks of influenza and the safety and efficacy of influenza vaccine are essential components of a comprehensive approach. Comprehensive training required under the Occupational Safety and Health Administration's (OSHA's) Bloodborne Pathogens Standard has contributed to increasing hepatitis B vaccination rates and reducing hepatitis B cases among HCP from 17,000 a year to fewer than 400 a year based on a 1995 study.45 A similar comprehensive educational approach may also contribute to improving influenza vaccination coverage.
It is important that educational materials are appropriate in content and vocabulary for the educational level, literacy, and language of targeted HCP. HCP should be educated regarding the benefits of influenza vaccination and the potential health consequences of influenza illness for themselves and their patients; the epidemiology and modes of transmission; diagnosis; treatment; and non-vaccine infection prevention strategies, in accordance with their level of responsibility in preventing health-care-associated influenza.3,41 The completion of required education must be monitored and enforced by the health-care facility staff, and compliance with education should be tracked in conjunction with vaccination rates.
Conclusions.
Annual influenza vaccination is the most effective strategy for preventing influenza, especially when provided as a component of a comprehensive influenza vaccination and prevention program. A comprehensive influenza vaccination program should be multifaceted, consider known barriers to immunization, and provide for substantial education and training on influenza regarding both the benefits and risks of receiving influenza vaccination. As with Recommendation 1, the implementation of a comprehensive influenza vaccination program can improve HCP vaccination rates.
NVAC believes that the best practices for vaccinating HCP are for HCEs and facilities to integrate influenza vaccination programs into their existing infection prevention or occupational health programs. To implement these best practices, HCEs will need to prioritize building capacity for a comprehensive influenza vaccination program within the context of their overall infection prevention programs and assess which mechanisms, or combination of mechanisms, are appropriate for their particular institution and workforce.
A comprehensive influenza vaccination program should be only one component of a multicomponent influenza prevention program. Each HCE should implement as many components as are applicable to protect both patients and HCP against influenza infection. HCEs and facilities should involve HCP, their representatives, managers, and professional staff in the planning, implementation, and evaluation of their programs to improve quality and increase the opportunity for program success. Factors to consider include the content and delivery of infection prevention education, HCP access to vaccination, involvement of senior leadership, local community variables, and how other health-care settings have met HP 2020 goals.
Recommendation 2.
NVAC recommends that HCEs and facilities integrate influenza vaccination programs into their existing infection prevention or occupational health programs. NVAC also recommends that the ASH assure that this recommendation is implemented in HHS facilities and services (including PHS, HHS staff, and FQHCs) and strongly urges all HCEs and facilities to do the same.
Measuring and reporting HCP influenza vaccination coverage
Measuring and reporting influenza vaccination rates helps to increase vaccination of HCP.
Reporting individual facility influenza vaccination rates as an indicator of an institution's commitment to the delivery of safe, quality care can help to increase influenza vaccination rates. In a study of influenza vaccination rates in acute care hospitals in Iowa, the authors observed a 10% increase in vaccination rates that they attributed to the anticipation of the public release of hospital vaccination rates.37 Likewise, significant increases in voluntary vaccination rates among HCP within BJC HealthCare hospitals were attributed to the use of a “Best in Class” scorecard, a quality report provided to leadership at each hospital to reach target goals.46 In addition, ACIP suggests that monitoring vaccination coverage by facility area (e.g., ward or unit) or occupational group could pinpoint areas where vaccination levels are low and interventions should be targeted.3
Standardized methodologies are being developed to facilitate measuring and reporting of HCP influenza vaccination rates within specified health-care facilities.
Work is currently under way to standardize methodologies used to measure and report HCP influenza vaccination rates within health-care facilities. In 2008, CDC proposed a standardized measure for assessing influenza vaccination of HCP to the National Quality Forum (NQF). The measure (NQF #0431, Influenza Vaccination Coverage Among Healthcare Personnel) was designed to ensure that reported HCP influenza vaccination rates were comprehensive within a single health-care facility and comparable across facilities, and was pilot-tested in a number of health-care facilities including acute care hospitals, ambulatory surgical centers, LTCFs, outpatient clinics, and renal dialysis centers. A revised measure was endorsed by the NQF.47
CMS recently adopted a rule for reporting influenza vaccination rates among HCP. Starting in January 2013, CMS will require acute care hospitals to report HCP influenza vaccination rates through CDC's National Healthcare Safety Network system using the NQF measure as part of the Hospital Inpatient Quality Reporting (IQR) program. Data from the IQR program will be made publicly available on the HospitalCompare.gov website. In addition, starting in 2015, acute care hospitals that fail to report these quality measures will be subject to a 2% payment reduction in the annual payment update from CMS. CMS also has proposed implementing this measure in outpatient and ambulatory care settings. However, this proposal is still under review. Details on this measure can be found at http://www.cdc.gov/nhsn.48
Conclusions.
Measuring and reporting HCP influenza vaccination rates leads to improved vaccination levels among HCP. While HCEs may differ in their HCP populations, it is important that all HCEs develop strategies for measuring HCP vaccination coverage with the purpose of using these data to evaluate and inform existing influenza vaccination programs. Likewise, standardized methodologies to measure and report HCP vaccination rates within specified health-care facilities will provide comparable data that can be used to help improve HCP vaccination rates. NVAC believes that measuring influenza vaccination coverage of HCP is a prerequisite for achieving and sustaining high coverage levels.
Recommendation 3.
NVAC recommends that the ASH encourage CDC and CMS to continue efforts to standardize the methodology used to measure HCP influenza vaccination rates across settings. The ASH should also work with CMS to facilitate adoption of this recommendation.
The role of employer requirements for HCP vaccination in influenza infection prevention
Many health-care facilities have difficulty achieving and maintaining high vaccination coverage rates of HCP despite efforts to implement comprehensive infection prevention and voluntary influenza vaccination programs.
Although ACIP has long recommended annual influenza vaccination for HCP, a national estimate of influenza vaccination coverage of HCP for the 2010–2011 influenza season was 63.5%.31 At the institutional level, the progressive incorporation of evidence-based strategies into voluntary influenza vaccination campaigns has often produced marginal increases in vaccine uptake during the course of several seasons.49
For example, a study conducted at BJC HealthCare hospitals analyzed 10 years of aggregate data on vaccination coverage of HCP (defined as hospital employees) and found that progressive voluntary interventions implemented during a period of several years were not sufficient to reach the hospital system's target vaccination rate of 80%.46 More generally, voluntary opt-in programs have not been successful as an approach to achieve and sustain high influenza vaccination coverage worldwide among health-care organizations.50 The HP 2020 objective for influenza vaccination coverage for HCP, and its inclusion in proposed Joint Commission hospital accreditation requirements, may result in additional efforts to increase uptake.49
Employer requirements are effective in increasing HCP immunization rates.
During the 2010–2011 influenza season, CDC found that approximately 13% of HCP reported that their employers required influenza vaccination as a condition of employment. Among this group, vaccination coverage was 98.1%, compared with 58.3% among those without an employer requirement.31 A national survey of acute care hospitals conducted by Miller et al. found that 55.6% of the hospitals surveyed had implemented an institutional requirement,51 but that vaccination coverage rates increased most significantly in hospitals that also enforced consequences for vaccine refusal.49 Consequences ranged in severity from mandatory masking to employee termination for noncompliance. Examples of employer-required influenza vaccination policies and their impact on HCP vaccination rates include the following:
Septimus et al. evaluated an influenza vaccination requirement for HCP (defined as clinical employees and individuals with access to patient care areas) implemented throughout the Hospital Corporation of America (HCA), Inc. national health-care system. Vaccination among HCP was required, but this policy permitted medical, religious, and philosophical exemptions. Unvaccinated HCP were required to either wear a surgical mask for the duration of the influenza season or revise their workflow to eliminate patient contact. Prior to the requirement, the study reported mean vaccination rates of 58%; post-requirement coverage levels rose to 96%.52
The Virginia Mason Medical Center in Seattle, Washington, was one of the first hospitals to report on its success using a mandatory vaccination program for HCP (defined in this study as employees of the medical center including students, vendors, contractors, outside physicians, and volunteers) as a condition of employment. Medical and religious exemptions were considered, and exempt HCP were required to wear a surgical mask. Unionized nurses were also exempt from this policy. Within the first year of implementation, vaccination coverage rates increased from 54.0% in 2003 to 97.6% in 2005, and coverage levels were sustained at .98.0% for subsequent influenza seasons (2006–2009).53
A mandatory influenza vaccination policy as a condition of employment was also implemented in hospitals within BJC HealthCare, following failed attempts by the organization to achieve target influenza vaccination rates through voluntary mechanisms. This policy defined HCP as all employed hospital staff (both clinical and nonclinical, including volunteers and vendors). Medical and religious exemptions were considered, and HCP that qualified for an exemption were encouraged to wear masks for the remainder of the influenza season. Noncompliant HCP were terminated for not meeting the conditions of employment. The authors reported increases in HCP vaccination coverage from 71% in 2007 to 98% in 2008. Within the BJC HealthCare system, 0.03% were terminated for failing to comply with hospital policy, similar to reports from the Virginia Mason experience.54
A comprehensive list of HCEs and facilities that have implemented employer requirements for influenza vaccination can be found on the Immunization Action Coalition Honor Roll for Patient Safety website.55
Requirements for vaccination are broadly used for HCP.
In general, HCP must accept a number of strategies as necessary occupational precautions for mitigating the spread of disease, including hand hygiene, personal protective equipment (e.g., gloves), and vaccination against a number of communicable diseases. These policies are generally intended to improve workplace safety by reducing the risk of infectious disease transmission to HCP. Requirements for immunity to, or vaccination against, varicella, measles, mumps, and rubella are standard for most health-care facilities. Hepatitis B vaccination or documented declination is required under OSHA's Bloodborne Pathogens Standard. While influenza vaccination must be completed annually, there are other comparable periodic requirements, such as tuberculin skin testing. However, tuberculin skin testing requirements are -generally stratified according to occupational risk and are variably -implemented with respect to documentation requirements and consequences for noncompliance.
PHS requires vaccination of its Commissioned Corps officers. The U.S. Department of Defense (DoD) requires vaccination for all civilian HCP who provide direct patient care in DoD treatment facilities.56 Additionally, as noted previously, HCEs and facilities require specific vaccines and a tuberculin skin test with varying policies regarding individual exemptions.
A state's power to mandate vaccinations in the interest of the public health was established in 1905 with the smallpox vaccination. Some states simply require hospitals to have an influenza vaccination policy, some states require health-care facilities to offer influenza vaccination to their employees, while still other states require that some HCP receive influenza vaccination or indicate a religious, medical, or philosophical reason for not being vaccinated.43
Employer requirement programs need leadership buy-in, education, and resource allocation to be successful.
Visible and vigorous leadership and accountability for vaccination are essential for programs requiring influenza vaccination as a condition for employment.38 The key points to consider in implementing an employer-required influenza vaccination policy include (1) having full support of health-care leadership; (2) tailoring the policy to the geographic setting, educational resources, financial assets, local culture, and potential language barriers; (3) providing free vaccinations to all HCP; (4) publicizing the program to HCP at all levels; (5) offering convenient times and locations for education and immunization administration; (6) clearly defining applicable exemption policies; and (7) developing policies for managing employees who are exempt from immunization or refuse immunization.43
Taking all appropriate measures to prevent the spread of infectious disease in health-care settings, including influenza vaccination, represents a duty of care among HCP.57
Arthur Caplan, the Emmanuel and Robert Hart Professor of Bioethics and director of the Center for Bioethics at the University of Pennsylvania, elaborates on three ethical reasons for requiring vaccination of HCP. First, Caplan points out that every code of ethics adopted by physicians, nurses, nurse aides, social workers, pharmacists, and other HCP states that the best interests of the patient must come first. Secondly, Caplan states that HCP are obligated to honor the core medical ethics requirement of “first, do no harm,” which includes taking necessary precautions to prevent transmission of infectious diseases, including influenza vaccinations. Finally, Caplan argues that HCP have a special duty to protect vulnerable patients, especially those that cannot protect themselves, such as newborn babies, infants, and the seriously immunocompromised.58 Patient advocacy groups have echoed this sentiment.59
Some have argued that vaccination programs should focus predominantly on HCP with direct contact to high-risk patients.60 This argument assumes that an individual patient's risk category can be promptly and easily determined so that appropriate staff assignments or patient placement can be arranged. The rights of all patients should include knowledge that they will be cared for by HCP who are using all available infection-control methods including vaccination to decrease transmission.61 This inclusion should be done for both high-risk and lower-risk patients. Therefore, receiving influenza vaccination may not only be an ethical obligation of HCP, but non-vaccination can be considered a failure to provide patients with an appropriate standard of care.60,62 Patients are justified in the expectation that they should be informed if they are not being provided with health care that meets the national standard of care and current recommendations. They should then be given the opportunity to request an alternative. Caplan emphasizes that “Few people pick their health-care providers or even know to ask if they have been vaccinated.”58
George Annas, professor of health law, bioethics, and human rights at Boston University School of Public Health, also states that HCP have an ethical obligation to take all reasonable steps to protect their patients. However, he argues against mandatory influenza vaccination for HCP. Annas states that influenza vaccination should be based on an informed choice and that HCP should not be forced to become non-consenting patients. He argues that mandatory influenza vaccination may have negative impacts, including building opposition that could result in an unenforceable mandate if a significant number of HCP refuse vaccination. This refusal, in turn, could confuse the public regarding the safety of the influenza vaccine. Annas concludes, “The most effective way to maximize the numbers of the public being vaccinated is to send the message that physicians and nurses believe this is the most reasonable approach to take to prevent wide-scale death and disease.. . .”63
Hospitals that have implemented mandatory influenza vaccination programs have not reported the backlash by HCP predicted by Annas. The Children's Hospital of Philadelphia surveyed a number of paid HCP (both clinical and nonclinical staff) and found that 74.4% of respondents indicated they agreed with the hospital's vaccination policy even though a number of them (72.0%) described the influenza vaccine requirement as coercive.64 Finally, in addition to the protective benefits to HCP and their patients against influenza infection, requiring HCP to be vaccinated sets a good example to the public and could help to promote influenza vaccination in all populations.64,65
Ethical and social concerns regarding employer requirements
HCP may oppose employer-required vaccination on the basis of worker autonomy, culture, or religion.
When considering employer-required vaccination of HCP, HCEs should consider the following arguments:
Worker autonomy: The rights of HCP to make their own health-care choices and have their autonomy respected are ethical considerations.66 One of the many ways autonomy is protected under the law is through the right to refuse medical treatment. Mandatory approaches are coercive, and it can be argued that these policies infringe on individuals' autonomy to make informed choices about their health. However, an individual's autonomy is not unlimited,67 and the duty of HCP to limit the transmission of influenza through vaccination to avoid causing significant harm to vulnerable patients may override personal autonomy.60
Culture: A Joint Commission report noted that cultural considerations may play an important role in HCP decisions to accept or decline vaccination. In studies comparing differences in HCP influenza vaccination declination, the authors found that HCP in North America cited fear of adverse reactions as the primary reason for refusing vaccination. In contrast, HCP in Switzerland cited the perception that they did not feel at risk for illness as the primary reason for refusing vaccination.66
Religion: Some HCP may oppose influenza vaccination based on religious convictions, and many mandatory vaccination policies have allowed religious exemptions for HCP who decline vaccination in good faith because of strongly held beliefs.67 However, HCEs should ensure that their exemption policies are in accordance with state-defined legislation.
Employer requirements for vaccination may be subject to the collective bargaining process for unionized workers.
Employees represented by labor unions have successfully challenged mandatory influenza vaccination policies. These cases do not directly address whether influenza vaccination is safe or effective, but rather whether the implementation of mandatory influenza vaccination policies that affect the job security and working conditions of HCP are subject to the collective bargaining process.
Several HCEs have indicated that mandatory influenza vaccination policies are necessary to achieve the core purpose of their facilities, which is to promote patient health and safety. These HCEs have argued that mandatory influenza vaccination policies are designed as patient protection measures, such that HCEs should not be obligated to negotiate these policies and the implementing procedures with unions. However, union representatives have successfully argued that mandatory influenza vaccination policies are subject to the usual collective bargaining process because the requirements constitute a change in the terms and conditions of employment.
Relevant decisions include the following:
-
SEIU 121RN and United Healthcare Workers West, and California HCA Hospitals:
In arbitration between five HCA-owned hospitals and the Service Employees International Union (SEIU), HCA contested that the majority of patient care policies outlined in the hospitals' infection-control manuals were not subject to the collective bargaining process and claimed that implementation of the mandatory influenza vaccination policy was a management right. The Union argued that this policy was subject to the collective bargaining process because it proposed new terms and conditions of employment and the mandatory masking requirement created a discriminatory working environment that stigmatized unvaccinated HCP.
The arbitrator upheld the right of the employer to implement the mandatory influenza vaccination policy as a patient safety measure, but ordered the employer to bargain with the Union “to determine a mutually agreeable means of enforcing its policy without violating the provisions cited, and reducing the potential for discrimination and/or violation of the just cause provisions of the Contract.”68
-
Board of Regents, University of Iowa Hospitals and SEIU:
The hospital claimed that the implementation of a mandatory influenza vaccination policy was a management right directly related to patient safety and was contractually protected under the employer's right “to change and modify programs and practices related to health and safety to address ongoing health and safety concerns as required or deemed necessary by regulatory agencies and changes in technology and information.”69
The arbitrator disagreed and ruled that the hospital had violated the collective bargaining agreement by implementing a mandatory influenza vaccination policy that instituted unpaid leave as a consequence for noncompliance. Instead of negotiating with the Union, the employer chose to unilaterally rescind its policy for both unionized and nonunionized HCP.69
-
Virginia Mason Medical Center and Washington State Nurses Association:
The Washington State Nurses Association (WSNA) filed a successful grievance against the Virginia Mason Medical Center regarding its mandatory influenza vaccination program. As a result, the hospital modified its influenza prevention policy to require all unvaccinated nurses to initiate influenza antiviral drug prophylaxis or wear a mask as part of a comprehensive influenza infection prevention program.
The Union then filed a second grievance, claiming that the hospital policy to require nonvaccinated HCP, who were not taking antiviral medication, to wear a facemask while at work constituted an unfair labor practice for failure to bargain and the implementation of unilateral change. The Administrative Law Judge (ALJ) sided with Virginia Mason, holding that the hospital was not required to bargain because the masking/antiviral requirement relates to the “core purpose” of the hospital.
The Union appealed to the National Labor Relations Board. In August 2011, the Board issued a split decision that reversed the ALJ's holding. The Board indicated that the unilateral implementation of a masking or medication policy is subject to the bargaining process and that the policy was outside the core purpose of the hospital. The case was remanded to permit the ALJ to prepare another decision. In November 2011, the ALJ found that the employer policy was protected under the management's rights clause and that the policy did not constitute an unfair labor practice. The complaint was dismissed.70
Employer requirements raise vaccination rates, but the impact on patient safety needs continued evaluation.
The primary intent of all influenza vaccination programs for HCP is to reduce influenza infections in patients and in HCP. Surveillance for health-care-associated influenza is not routine. Without ongoing measurement of health-care-associated influenza or prospective controlled studies, significant gaps in understanding the impact of increasing vaccination rates on patient safety will persist. Further studies are also needed to determine if patient risk assignment (i.e., high risk vs. lower risk) is reasonable and effective in preventing health-care-associated influenza infections.
Conclusions.
NVAC realizes that employer-required vaccination of HCP against influenza is the subject of fervent discussion, both for the concept and against it. Such requirements have been shown to be effective methods of achieving high coverage but may face ethical, cultural, or collective bargaining issues. For those HCEs who cannot achieve the HP 2020 annual goals for influenza immunization of HCP through implementing a comprehensive influenza prevention program, managing influenza vaccination programs, or measuring and reporting HCP influenza vaccination coverage, employer-required vaccination then becomes the next option for increasing influenza immunization rates of their HCP. NVAC considered a variety of factors when evaluating the merits of employer requirements, including target vaccination rates, vaccine efficacy, whether herd immunity might reasonably be expected to decrease disease rates, and vaccine policy options, such as exemptions and consequences for noncompliance. NVAC does not stipulate the scope and content of employer requirement policies; these policies must be decided by the HCE based on the concerns and needs of HCP, patients, and the public.
NVAC believes that, at present, HCE or facility requirements for influenza vaccination are the most effective mechanism to rapidly reach and maintain the HP 2020 goal. Factors to consider when implementing such a policy include the vulnerability of the patient population cared for, what will be considered acceptable reasons for exemption from influenza vaccination, applicable bargaining agreements, and consequences of noncompliance with the policy. It is critical that patients know that everything possible is being done to protect them from health-care-associated influenza infection while in an inpatient, outpatient, or home situation.
NVAC recognizes that prior to the development of these recommendations, many HCEs have already implemented employer requirements in conjunction with, or following the implementation of, Recommendations 1, 2, and 3. This approach is consistent with NVAC recommendations. NVAC recognizes that local resources, patient safety needs, available expertise, labor concerns, and target vaccination goals must be taken into consideration when developing such policies. HCE or facility requirement policies should define affected workers and the affected employer, outline affected worker and employer obligations, and incorporate an exemption policy. NVAC notes that employer requirements need strong leadership, messaging and partnership with all HCP, and a focus on the goals of protecting patients and HCP consistent with the ethics of the health-care profession.
Recommendation 4.
For those HCEs and facilities that have implemented Recommendations 1, 2, and 3 and still have not consistently achieved the HP 2020 goal for influenza vaccination coverage of HCP in an efficient and timely manner, NVAC recommends that HCEs strongly consider an employer requirement for influenza immunization. In addition to medical exemptions, HCEs may consider other exemptions in their requirement policies. NVAC also recommends that the ASH assure that this recommendation is implemented in HHS facilities and services (including PHS, HHS staff who are HCP, and FQHCs) and urge all other HCEs and facilities to do the same.
Supporting influenza vaccine development
Influenza vaccine effectiveness is highest when the vaccine strains are well matched to a circulating virus.
In years when the circulating virus strains vary from the vaccine strains, vaccinated HCP and their patients may have an increased risk for contracting and spreading influenza infection compared with years when the vaccine is well matched. Vaccine efficacy can vary from year to year and from person to person, but usually some protection is provided against illness or severe illness. There is a great deal of debate regarding the effectiveness of the influenza vaccine. Previous studies found that annual immunization with a vaccine antigenically well matched to circulating strains reduced serologically confirmed influenza cases by 70% to 90% among healthy adults,65 years of age.27,71–75 However, recent studies estimate that vaccine effectiveness may be considerably lower. Osterholm et al. reported a pooled efficacy of only 59% in adults 18–65 years of age.76 Others have also reported reduced vaccine effectiveness in the range of 45%–75%.28 The lower estimates in more recent studies may reflect new information regarding diagnostic testing; vaccine effectiveness is overestimated when serology is used as an endpoint.77 While current vaccines are a critical component of reducing influenza infection, an opportunity exists to provide next-generation vaccines with improved effectiveness, broader protection, and increased duration of immunity. Additionally, novel approaches to improving influenza vaccines could result in vaccines that offer multiyear protection against numerous influenza strains, which could reduce the frequency of immunization.78–80
Despite the significant progress in influenza vaccine technologies and manufacturing since 2009, vaccine shortages could remain a challenge to implementing vaccination as an employer requirement.
In response to the 2009 H1N1 influenza pandemic, New York State became the first state to issue a mandate requiring HCP to be vaccinated against influenza. However, this regulation was stayed in a lawsuit brought by SEIU Local 4053, the New York State Public Employees Federation. A week after the regulation was stayed, the New York Department of Health rescinded the regulation due to a shortage of vaccine supplies. The Commissioner of Health noted that the requirement “.. . set up a dynamic where HCP covered under the regulation might compete for vaccine with people with underlying risk factors for adverse outcome of influenza infection.”81 Since the 2009 H1N1 response, national strategies have included improvements to the vaccine supply chain. Improved vaccine availability and stable supply chains will be necessary to ensure that HCEs and facilities can attain vaccination coverage rates that meet quality measures.82
Conclusions.
Improved efficacy and reduction in the need for annual vaccinations will make it easier to achieve and sustain high vaccination coverage rates among HCP. Ensuring that adequate vaccine supplies are available will also help HCEs and facilities to provide vaccine free of charge to HCP and, ultimately, achieve the HP 2020 annual goal of vaccination of HCP or even higher coverage rates.
An influenza vaccine that confers multiyear protection against influenza with increased efficacy and comparable safety relative to the current annual vaccines could facilitate achieving and maintaining high coverage rates for influenza immunization in HCP and other populations. An ideal influenza vaccine would not need to be updated each year depending on circulating influenza strains and could provide extended or lifetime immunity.78–80 A longer-lasting vaccine may contribute to higher coverage, reducing the need for employer requirements.
Recommendation 5.
NVAC recommends that the ASH encourage ongoing efforts to develop new and improved influenza vaccines and vaccine technologies including support for research, development, and licensure of influenza vaccines with improved effectiveness and duration of immunity, as well as steps that improve the immunogenicity and rapid production of existing influenza vaccines.
CONCLUSIONS
Influenza is a significant public health issue. Annual influenza-associated deaths range from 3,000 to 49,000 according to recent estimates, and more than 200,000 people are hospitalized each year for respiratory illnesses and heart conditions associated with seasonal influenza infection. Immunization is the most effective method for preventing infection from influenza and possible hospitalization or death. For this reason, HHS, CDC, and other health-care and public health agencies and organizations recommend vaccination as a critical influenza prevention strategy. Despite these recommendations, immunization rates for HCP in the U.S. remain low.
To address this gap in immunization rates for HCP, NVAC, as directed by the ASH, developed the recommendations and strategies presented in this report for the specific purpose of achieving the HP 2020 objective for annual influenza vaccine coverage for HCP. These recommendations were carefully reviewed, deliberated, debated, and then approved by a majority of NVAC members. These recommendations present a tiered set of strategies for achieving the HP 2020 annual objective for influenza vaccination of HCP, including the implementation and management of influenza prevention and vaccination programs, and measuring and reporting vaccination coverage to employer requirements for HCP vaccination. NVAC realizes that HCEs range in their scope of practice, from the traditional hospital setting to the in-home health-care setting, and no single option for improving HCP immunization rates would work for all HCEs. Thus, a set of recommended options is presented that can be applied to most health-care settings to improve immunization rates of HCP.
In presenting these recommendations, NVAC acknowledges that there are individuals or groups that may be opposed to each recommendation in whole or in part for varied reasons, such as concerns about the quality of evidence in the literature regarding the impact of HCP vaccination on patient risk of health-care-associated influenza and the issue of workers' rights. NVAC carefully considered all sides of the argument for each recommendation and believes that the recommendations made represent the most effective approach to achieving the stated goal of achieving the HP 2020 annual influenza vaccine coverage objective for HCP.
APPENDIX. SUPPLEMENTARY MATERIAL: SUMMARY OF PUBLIC COMMENTS
This summary represents the public comments received by the National Vaccine Program Office as of January 20, 2012.Hard copies of the public comment are available upon request from the National Vaccine Program Office, Department of Health and Human Services, Hubert H. Humphrey Building, 200 Independence Ave. SW, Room 733G, Washington, DC 20201.
I. SOLICITATION OF PUBLIC COMMENT
The draft report and draft recommendations were released for public comment through the Federal Register process to solicit additional input on strategies and/or potential barriers to achieving the Healthy People 2020 (HP 2020) annual goal of 90% influenza vaccine coverage among health-care personnel (HCP) that are not addressed in the current report. Public comment was collated and summarized for consideration and deliberation by the National Vaccine Advisory Committee (NVAC).
II. SUMMARY OF PUBLIC COMMENT SUBMITTED BY INDIVIDUALS
Public comment was submitted by 145 individuals including a number of HCP across the health-care sector. These comments are almost exclusively in response to Recommendation 4 and represent opinions and personal accounts. In general, the majority of individual comments can be categorized into themes (themes represent $5 common responses).
Recommendation 4: For those health-care employers (HCEs) and facilities that have implemented Recommendations 1, 2, and 3 and cannot achieve and maintain the HP 2020 goal of 90% influenza vaccination coverage of HCP in an efficient and timely manner, the Health Care Personnel Influenza Vaccination Subgroup (HCPIVS) recommends that HCEs and facilities strongly consider an employer requirement for influenza immunization.
Individuals who oppose Recommendation 4:
Personal autonomy (94 responses)
Concern regarding adverse events (specific to the influenza vaccine) (45 responses)
Concern regarding vaccine effectiveness (specific to the influenza vaccine) (43 responses)
Concern regarding vaccine safety (specific to the influenza vaccine) (26 responses)
Concern regarding exemption policies that did not include religious, philosophical, and personal exemptions (26 responses)
Concern that there is an insufficient scientific basis for mandatory vaccine policies (23 responses)
Concerns regarding vaccine safety (general) (20 responses)
Concerns regarding adverse events (vaccinations in general) (19 responses)
Liability for adverse events under mandatory policies (eight responses)
Individuals who support Recommendation 4:
Support for draft recommendations (general) (10 responses)
Support for draft Recommendation 4 (as a patient safety measure) (five responses)
III. SUMMARY OF PUBLIC COMMENT SUBMITTED BY ORGANIZATIONS/ASSOCIATIONS
Public comment was also submitted on behalf of 37 organizations/associations representing the following:
15 professional associations
13 labor organizations
Five nonprofit organizations
Two public health departments
One federal agency
One other
Public comments submitted by organizations/associations have also been grouped into themes that include general comments, recommendation-specific comments, and comments that directly address Recommendation 4.
General comments
Definitions of HCP and HCEs:
Definitions should be expanded (three responses).
HCPIVS definitions of HCP and HCEs do not match the definitions outlined in the National Quality Forum (NQF) and Centers for Medicare – Medicaid Services (CMS) reporting measures (two responses).
Additional resources are needed to implement the recommendations (five responses).
Education (general):
Education is mentioned throughout the report but is not explicitly called out in the five recommendations (four responses).
Comments on Recommendations 1, 2, and 3
Recommendations 1 and 2:
Recommendation 1 and 2 should state that HCP and their representatives should be directly involved in the development and implementation of influenza prevention programs and influenza vaccination programs (three responses).
Vaccination programs should include free vaccine available during multiple shifts, locations, and days (general) (five responses).
Recommendation 3:
HCPIVS should indicate the effects of vaccine shortages on CMS reporting (one response).
HCPIVS should recommend that NQF measures be applied to ambulatory and outpatient settings (one response).
Other key agencies such as the Occupational Safety and Health Administration (OSHA) should be included in defining incentives and requirements (one response).
Comments on Recommendation 4
Similar to the public comment submitted by individuals, the majority of public comment from organizations/associations focused on Recommendation 4.
Fifteen organizations/associations directly stated support for Recommendation 4:
13 professional associations
Two nonprofit organizations
Sixteen organizations/associations directly opposed Recommendation 4:
12 labor organizations
Two nonprofit organizations
One professional association
One federal agency
Six organizations/associations did not directly address Recommendation 4 in their comments.
Comments specific to Recommendation 4
Employer requirements (general):
Language should be modified to more strongly support employer requirements (three responses).
Recommendation should be changed to state that employer requirements include vaccination as a condition of employment and credentialing unless documented medical contraindications exist, or in states that allow personal exemptions (two responses).
Recommendation 4 should be eliminated (six responses).
Recommendation 4 should state that it does not support vaccination as a condition of employment (seven responses).
Requirements should be modeled after the OSHA Bloodborne Pathogens Standard for hepatitis B, which includes mandatory education/training and mandatory offering of vaccine (nine responses).
Exemptions/personal autonomy:
Language in the report should state that exemptions are a state-specific decision in accordance with state legislation (one response).
Recommendation 4 should support flexible exemptions (religious, philosophical, and personal) and should not indicate any punitive measures or discrimination for employees that opt out (10 responses).
Concern that vaccine effectiveness does not support mandatory policies (12 responses)
Concern that there is insufficient scientific evidence of the impact of HCP vaccination on patient safety to support policies that require influenza vaccination without exemptions (other than medical exemptions):
General (eight responses)
Suggestion to include a sixth recommendation that addresses surveillance and research evidence on vaccine impact and efficacy in HCP (two responses)
Limited to no data outside of long-term care facilities (LTCFs) on the impact of HCP vaccination on patient safety (three responses)
Concern that an overemphasis on vaccination as a preventive measure may lead to poor adherence to other infection-control practices:
General (eight responses)
Overreliance on vaccination as a public health measure during years of vaccine mismatch, unsuccessfully vaccinated HCP, or during vaccine shortages (three responses)
Employer requirements would be considered a unilateral change to the conditions and terms of employment and could be subject to collective bargaining negotiations (four responses).
Other comments general to Recommendation 4
HP 2020:
HP 2020 goals are voluntary objectives to strive for and are not public health mandates (two responses).
Evidence that a 90% vaccination coverage rate is the appropriate level (five responses)
Liability for adverse events under mandatory policies (not commented on in the draft report):
Compensation for employees who suffer any adverse effects under mandatory policies (one response)
Need to cover vaccine injuries under the National Vaccine Injury Compensation program and not workers' compensation programs (one response)
Masking (not commented on in the draft report):
Request that recommendations state the infection prevention measures for unvaccinated HCP including the use of masks or to be precluded from working in certain areas (one response)
Request that LTCFs be exempt from any masking policies because of difficulties communicating with hearing-impaired patients and patients with dementia (one response)
Request that the report not endorse masking for unvaccinated HCP (three responses)
Request that the report comment on the safety and appropriateness of this type of requirement for vaccine refusal (one response)
Footnotes
This report was adopted by the National Vaccine Advisory Committee (NVAC) on February 8, 2012. Authors/contributors are acknowledged based on their important contributions as subject-matter experts. The positions expressed and recommendations made in this report do not necessarily represent those of the U.S. government, those of individual NVAC members, or of the working group members who served as authors of, or otherwise contributed to, this report.
Members of the Healthcare Personnel Influenza Vaccination Subgroup are as follows: cochairs: Christine Nevin-Woods, DO, MPH, Pueblo (Colorado) City-County Health Department; and Julie Morita, MD, Chicago Department of Public Health; NVAC chair: Guthrie Birkhead, MD, MPH, New York State Department of Health; Jon Almquist, MD, American Academy of Pediatrics; Hilary Babcock, MD, MPH, Society for Healthcare Epidemiology of America and Infectious Diseases Society of America; Robert Bednarczyk, PhD, New York State Department of Health; Richard Beigi, MD, MSc, American College of Obstetricians and Gynecologists; Nancy Berlinger, PhD, MDiv, The Hastings Center; William Bleser, MSPH, U.S. Department of Health and Human Services (HHS), National Vaccine Program Office (NVPO); William Borwegen, MPH,Service Employees International Union; Katherine Brewer, MSN,American Nurses Association; Benedict Diniega, MD, MPH, U.S. Department of Defense, Health Affairs; Jeffrey Duchin, MD, Advisory Committee on Immunization Practices; Jennifer Gordon, PhD, HHS, NVPO; Mark Grabowsky, MD, MPH, HHS, NVPO; Amy Groom, MPH, HHS, Indian Health Service; Kathleen Harriman, PhD, MPH, California Department of Public Health; Rachel Hart-Malloy, PhD, MPH, New York State Department of Health; Jennifer Hilliard, MMH, JD, Leading Age (formerly American Association of Homes and Services for the Aging); Nancy Hughes, MS, RN, American Nurses Association; Anna Jacobs, HHS, Office of the General Counsel; Clement Lewin, PhD, MBA, Novartis Vaccines and Diagnostics; Atkinson Longmire, MD, Occupational Safety and Health Administration (OSHA); Charlene Ludlow, RN, MHA, CIC, American Hospital Association; Richard Martinello, MD, Department of Veterans Affairs; John Piacentino, MD, MPH, Centers for Disease Control and Prevention (CDC), National Institute for Occupational Safety and Health (NIOSH); Gregory Poland, MD, American College of Physicians; Shane Ryan, CDC; Mitchel Rothholz, RPh, MBA, American Pharmacists Association; Alexandra Stewart, JD, The George Washington University Medical Center, School of Public Health and Health Policy; Rosemary Sokas, MD, MOH, OSHA; Melanie Swift, MD, FACOEM, American College of Occupational and Environmental Medicine; Litjen Tan, PhD, MS, American Medical Association; David Weissman, MD, CDC, NIOSH; Melinda Wharton, CDC; Lauren Wu, MHS, HHS, NVPO; Ted Yee, MD, MPH, OSHA; and Janice Zalen, MPA, American Health Care Association.
REFERENCES
- 1.Department of Health and Human Services (US). Healthy People 2020: immunization and infectious diseases. 2020. [cited 2011 Dec 3]. Available from: URL: http://healthypeople.gov/2020/topicsobjectives2020/objectiveslist.aspx?topicId=23.
- 2.Department of Health and Human Services (US). HHS action plan to prevent healthcare-associated infections: influenza vaccination of healthcare personnel. [cited 2011 Dec 3]. Available from: URL: http://www.hhs.gov/ash/initiatives/hai/tier2_flu.html.
- 3.Pearson ML, Bridges CB, Harper SA. Influenza vaccination of health-care personnel: recommendations of the Healthcare Infection Control Practices Advisory Committee (HICPAC) and the Advisory Committee on Immunization Practices (ACIP) MMWR Recomm Rep. 2006;55(RR-2):1–16. [PubMed] [Google Scholar]
- 4.Centers for Disease Control and Prevention (US). Prevention strategies for seasonal influenza in healthcare settings: guidelines and recommendations. [cited 2011 Aug 17]. Available from: URL: http://www.cdc.gov/flu/professionals/infectioncontrol/healthcaresettings.htm.
- 5.Centers for Disease Control and Prevention (US). Estimating seasonal influenza-associated deaths in the United States: CDC study confirms variability of flu. [cited 2011 Nov 17]. Available from: URL: http://www.cdc.gov/flu/about/disease/us_flu-related_deaths.htm.
- 6.Thompson WW, Shay DK, Weintraub E, Brammer L, Bridges CB, Cox NJ, et al. Influenza-associated hospitalizations in the United States. JAMA. 2004;292:1333–40. doi: 10.1001/jama.292.11.1333. [DOI] [PubMed] [Google Scholar]
- 7.American Public Health Association. Annual influenza vaccination requirements for health workers. [cited 2011 Dec 20]. Available from: URL: http://www.apha.org/advocacy/policy/policysearch/default.htm?id=1410.
- 8.Thompson WW, Shay DK, Weintraub E, Brammer L, Cox NJ, Anderson LJ, et al. Mortality associated with influenza and respiratory syncytial virus in the United States. JAMA. 2003;289:179–86. doi: 10.1001/jama.289.2.179. [DOI] [PubMed] [Google Scholar]
- 9.Rasmussen SA, Jamieson DJ, Bresee JS. Pandemic influenza and pregnant women. Emerg Infect Dis. 2008;14:95–100. doi: 10.3201/eid1401.070667. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Siston AM, Rasmussen SA, Honein MA, Fry AM, Seib K, Callaghan WM, et al. Pandemic 2009 influenza A (H1N1) virus illness among pregnant women in the United States. JAMA. 2010;303:1517–25. doi: 10.1001/jama.2010.479. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Fiore AE, Uyeki TM, Broder K, Finelli L, Euler GL, Singleton JA, et al. Prevention and control of influenza with vaccines: recommendations of the Advisory Committee on Immunization Practices (ACIP), 2010. MMWR Recomm Rep. 2010;59(RR-8):1–62. [PubMed] [Google Scholar]
- 12.Omer SB, Goodman D, Steinhoff MC, Rochat R, Klugman KP, Stoll BJ, et al. Maternal influenza immunization and reduced likelihood of prematurity and small for gestational age births: a retrospective cohort study. PLoS Med. 2011;8:e1000441. doi: 10.1371/journal.pmed.1000441. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Van Kerkhove MD, Vandemaele KA, Shinde V, Jaramillo-Gutierrez G, Koukounari A, Donnelly CA, et al. Risk factors for severe outcomes following 2009 influenza A (H1N1) infection: a global pooled analysis. PLoS Med. 2011;8:e1001053. doi: 10.1371/journal.pmed.1001053. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Cooksley CD, Avritscher EBC, Bekele BN, Rolston KV, Geraci JM, Elting LS. Epidemiology and outcomes of serious influenza-related infections in the cancer population. Cancer. 2005;104:618–28. doi: 10.1002/cncr.21203. [DOI] [PubMed] [Google Scholar]
- 15.Hayward AC, Harling R, Wetten S, Johnson AM, Munro S, Smedley J, et al. Effectiveness of an influenza vaccine programme for care home staff to prevent death, morbidity, and health service use among residents: cluster randomised controlled trial. BMJ. 2006;333:1241. doi: 10.1136/bmj.39010.581354.55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Outbreaks of 2009 pandemic influenza A (H1N1) among longterm-care facility residents—three states, 2009. MMWR Morb Mortal Wkly Rep. 2010;59(3):74–7. [PubMed] [Google Scholar]
- 17.Ellis SE, Coffey CS, Mitchel EF, Jr, Dittus RS, Griffin MR. Influenza- and respiratory syncytial virus-associated morbidity and mortality in the nursing home population. J Am Geriatr Soc. 2003;51:761–7. doi: 10.1046/j.1365-2389.2003.51254.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Gaillat J, Chidiac C, Fagnani F, Pecking M, Salom M, Veyssier P, et al. Morbidity and mortality associated with influenza exposure in long-term care facilities for dependent elderly people. Eur J Clin Microbiol Infect Dis. 2009;28:1077–86. doi: 10.1007/s10096-009-0751-3. [DOI] [PubMed] [Google Scholar]
- 19.Cunney RJ, Bialachowski A, Thornley D, Smaill FM, Pennie RA. An outbreak of influenza A in a neonatal intensive care unit. Infect Control Hosp Epidemiol. 2000;21:449–54. doi: 10.1086/501786. [DOI] [PubMed] [Google Scholar]
- 20.Poehling KA, Edwards KM, Weinberg GA, Szilagyi P, Staat MA, Iwane MK, et al. The underrecognized burden of influenza in young children. N Engl J Med. 2006;355:31–40. doi: 10.1056/NEJMoa054869. [DOI] [PubMed] [Google Scholar]
- 21.Shefer A, Atkinson W, Friedman C, Kuhar DT, Mootrey G, Bialek SR, et al. Immunization of health-care personnel: recommendations of the Advisory Committee on Immunization Practices (ACIP) MMWR Recomm Rep. 2011;60(RR-7):1–45. [PubMed] [Google Scholar]
- 22.Benowitz I, Esposito DB, Gracey KD, Shapiro ED, Vázquez M. Influenza vaccine given to pregnant women reduces hospitalization due to influenza in their infants. Clin Infect Dis. 2010;51:1355–61. doi: 10.1086/657309. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Carman WF, Elder AG, Wallace LA, McAulay K, Walker A, Murray GD, et al. Effects of influenza vaccination of health-care workers on mortality of elderly people in long-term care: a randomised controlled trial. Lancet. 2000;355:93–7. doi: 10.1016/S0140-6736(99)05190-9. [DOI] [PubMed] [Google Scholar]
- 24.Potter J, Stott DJ, Roberts MA, Elder AG, O'Donnell B, Knight PV, et al. Influenza vaccination of health care workers in long-term-care hospitals reduces the mortality of elderly patients. J Infect Dis. 1997;175:1–6. doi: 10.1093/infdis/175.1.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Lester RT, McGeer A, Tomlinson G, Detsky AS. Use of, effectiveness of, and attitudes regarding influenza vaccine among house staff. Infect Control Hosp Epidemiol. 2003;24:839–44. doi: 10.1086/502146. [DOI] [PubMed] [Google Scholar]
- 26.Cox NJ, Subbarao K. Influenza. Lancet. 1999;354:1277–82. doi: 10.1016/S0140-6736(99)01241-6. [DOI] [PubMed] [Google Scholar]
- 27.Jefferson T, Di Pietrantonj C, Rivetti A, Bawazeer GA, Al-Ansary LA, Ferroni E. Vaccines for preventing influenza in healthy adults. Cochrane Database of Syst Rev. 2010;(7):CD001269. doi: 10.1002/14651858.CD001269.pub4. [DOI] [PubMed] [Google Scholar]
- 28.Michiels B, Govaerts F, Remmen R, Vermeire E, Coenen S. A systematic review of the evidence on the effectiveness and risks of inactivated influenza vaccines in different target groups. Vaccine. 2011;29:9159–70. doi: 10.1016/j.vaccine.2011.08.008. [DOI] [PubMed] [Google Scholar]
- 29.Thomas RE, Jeff TO, Demicheli V, Rivetti D. Influenza vaccination for health-care workers who work with elderly people in institutions: a systematic review. Lancet Infect Dis. 2006;6:273–9. doi: 10.1016/S1473-3099(06)70462-5. [DOI] [PubMed] [Google Scholar]
- 30.Vanhems P, Voirin N, Roche S, Escuret V, Regis C, Gorain C, et al. Risk of influenza-like illness in an acute health care setting during community influenza epidemics in 2004–2005, 2005–2006, and 2006–2007: a prospective study. Arch Intern Med. 2011;171:151–7. doi: 10.1001/archinternmed.2010.500. [DOI] [PubMed] [Google Scholar]
- 31.Influenza vaccination coverage among health-care personnel—United States, 2010–11 influenza season. MMWR Morb Mortal Wkly Rep. 2011;60(32):1073–7. [PubMed] [Google Scholar]
- 32.Elder AG, O'Donnell B, McCruden EA, Symington IS, Carman WF. Incidence and recall of influenza in a cohort of Glasgow healthcare workers during the 1993-4 epidemic: results of serum testing and questionnaire. BMJ. 1996;313:1241–2. doi: 10.1136/bmj.313.7067.1241. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Salgado CD, Giannetta ET, Hayden FG, Farr BM. Preventing nosocomial influenza by improving the vaccine acceptance rate of clinicians. Infect Control Hosp Epidemiol. 2004;25:923–8. doi: 10.1086/502321. [DOI] [PubMed] [Google Scholar]
- 34.Centers for Disease Control and Prevention (US). Prevention strategies for seasonal influenza in healthcare settings. [cited 2011 Nov 17]. Available from: URL: http://www.cdc.gov/flu/professionals/infectioncontrol/healthcaresettings.htm.
- 35.Hakim H, Gaur AH, McCullers JA. Motivating factors for high rates of influenza vaccination among healthcare workers. Vaccine. 2011;29:5963–9. doi: 10.1016/j.vaccine.2011.06.041. [DOI] [PubMed] [Google Scholar]
- 36.Polgreen PM, Polgreen LA, Evans T, Helms C. A statewide system for improving influenza vaccination rates in hospital employees. Infect Control Hosp Epidemiol. 2009;30:474–8. doi: 10.1086/596780. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Helms C, Polgreen P, Polgreen L, Evans T, Roberts LL, Clabaugh G, et al. Voluntary reporting of employee influenza vaccination rates by acute care hospitals in Iowa: the impact of a four year provider-based statewide performance improvement project. Vaccine. 2011;29:3483–8. doi: 10.1016/j.vaccine.2011.02.056. [DOI] [PubMed] [Google Scholar]
- 38.Talbot TR, Babcock H, Caplan AL, Cotton D, Maragakis LL, Poland GA, et al. Revised SHEA position paper: influenza vaccination of healthcare personnel. Infect Control Hosp Epidemiol. 2010;31:987–95. doi: 10.1086/656558. [DOI] [PubMed] [Google Scholar]
- 39.National Business Group on Health. Hospitals should require flu vaccination for all personnel to protect patients' health and their own health. [cited 2011 Dec 3]. Available from: URL: http://www.businessgrouphealth.org/pdfs/Position Statement - National Business Group on Health Position Statement on Influenza Vaccination of Health Care Personnel FINAL.pdf.
- 40.National Foundation for Infectious Diseases. Washington: National Foundation for Infectious Diseases; 2004. [cited 2011 Dec 3]. Improving influenza vaccination rates in health care workers: strategies to increase protection for workers and patients. Also available from: URL: http://ideha.dhmh.maryland.gov/OIDEOR/IMMUN/SharedDocuments/hcwmonograph.pdf. [Google Scholar]
- 41.Hollmeyer HG, Hayden F, Poland G, Buchholz U. Influenza vaccination of health care workers in hospitals—a review of studies on attitudes and predictors. Vaccine. 2009;27:3935–44. doi: 10.1016/j.vaccine.2009.03.056. [DOI] [PubMed] [Google Scholar]
- 42.Talbot TR, Bradley SE, Cosgrove SE, Ruef C, Siegel JD, Weber DJ. Influenza vaccination of healthcare workers and vaccine allocation for healthcare workers during vaccine shortages. Infect Control Hosp Epidemiol. 2005;26:882–90. doi: 10.1086/502512. [DOI] [PubMed] [Google Scholar]
- 43.Bernstein HH, Starke JR. Policy statement—recommendation for mandatory influenza immunization of all health care personnel. Pediatrics. 2010;126:809–15. doi: 10.1542/peds.2010-2376. [DOI] [PubMed] [Google Scholar]
- 44.American College of Occupational and Environmental Medicine. Seasonal influenza prevention in health care workers. 2008. Nov 17, [cited 2011 Dec 14]. Available from: URL: http://www.acoem.org/SeasonalInfluenzaPrevention_HealthCareWorkers.aspx. [DOI] [PubMed]
- 45.Mahoney FJ, Stewart K, Hu H, Coleman P, Alter MJ. Progress toward the elimination of hepatitis B virus transmission among health care workers in the United States. Arch Intern Med. 1997;157:2601–5. [PubMed] [Google Scholar]
- 46.Ajenjo MC, Woeltje KF, Babcock HM, Gemeinhart N, Jones M, Fraser VJ. Influenza vaccination among healthcare workers: ten-year experience of a large healthcare organization. Infect Control Hosp Epidemiol. 2010;31:233–40. doi: 10.1086/650449. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.National Quality Forum. Influenza vaccination coverage among healthcare personnel. Atlanta: Centers for Disease Control and Prevention (US); 2012. [Google Scholar]
- 48.Centers for Disease Control and Prevention (US). National Healthcare Safety Network. [cited 2012 Oct 15]. Available from: URL: http://www.cdc.gov/nhsn.
- 49.Miller BL, Ahmed F, Lindley MC, Wortley PM. Increases in vaccination coverage of healthcare personnel following institutional requirements for influenza vaccination: a national survey of U.S. hospitals. Vaccine. 2011;29:9398–403. doi: 10.1016/j.vaccine.2011.09.047. [DOI] [PubMed] [Google Scholar]
- 50.McLennan S, Wicker S. Reflections on the influenza vaccination of healthcare workers. Vaccine. 2010;28:8061–4. doi: 10.1016/j.vaccine.2010.10.019. [DOI] [PubMed] [Google Scholar]
- 51.Miller BL, Ahmed F, Lindley MC, Wortley PM. Institutional requirements for influenza vaccination of healthcare personnel: results from a nationally representative survey of acute care hospitals—United States, 2011. Clin Infect Dis. 2011;53:1051–9. doi: 10.1093/cid/cir633. [DOI] [PubMed] [Google Scholar]
- 52.Septimus EJ, Perlin JB, Cormier SB, Moody JA, Hickok JD. A multifaceted mandatory patient safety program and seasonal influenza vaccination of health care workers in community hospitals. JAMA. 2011;305:999–1000. doi: 10.1001/jama.2011.244. [DOI] [PubMed] [Google Scholar]
- 53.Rakita RM, Hagar BA, Crome P, Lammert JK. Mandatory influenza vaccination of healthcare workers: a 5-year study. Infect Control Hosp Epidemiol. 2010;31:881–8. doi: 10.1086/656210. [DOI] [PubMed] [Google Scholar]
- 54.Babcock HM, Gemeinhart N, Jones M, Dunagan WC, Woeltje KF. Mandatory influenza vaccination of health care workers: translating policy to practice. Clin Infect Dis. 2010;50:459–64. doi: 10.1086/650752. [DOI] [PubMed] [Google Scholar]
- 55.Immunization Action Coalition. Honor roll for patient safety: mandatory influenza vaccination for healthcare workers. [cited 2012 Oct 15]. Available from: URL: http://www.imunize.org/honor-roll.
- 56.Department of Defense (US). Mandatory influenza vaccination for all DoD health care workers. 2005. Dec 19, [cited 2011 Dec 10]. Available from: URL: http://www.vaccines.mil/documents/923HCWflu.pdf.
- 57.American College of Physicians. ACP policy on influenza vaccination of health care workers. [cited 2011 Dec 3]. Available from: URL: http://www.acponline.org/clinical_information/resources/adult_immunization/flu_hcw.pdf.
- 58.Caplan A. Time to mandate influenza vaccination in health-care workers. Lancet. 2011;378:310–1. doi: 10.1016/s0140-6736(11)61156-2. [DOI] [PubMed] [Google Scholar]
- 59.National Patient Safety Foundation. Media alert: NPSF supports mandatory flu vaccinations for healthcare workers. 2009. Nov 18, [cited 2011 Dec 3]. Available from: URL: http://www.npsf.org/updates-news-press/press/media-alert-npsf-supports-mandatory-flu-vaccinations-for-healthcare-workers.
- 60.McLennan S, Gillett G, Celi LA. Healer, heal thyself: health care workers and the influenza vaccination. Am J Infect Control. 2008;36:1–4. doi: 10.1016/j.ajic.2007.07.010. [DOI] [PubMed] [Google Scholar]
- 61.Miller AC, Ross DW. Mandated influenza vaccines and health care workers' autonomy. Virtual Mentor. 2010;12:706–10. doi: 10.1001/virtualmentor.2010.12.9.ccas2-1009. [DOI] [PubMed] [Google Scholar]
- 62.Poland GA. Mandating influenza vaccination for health care workers: putting patients and professional ethics over personal preference. Vaccine. 2010;28:5757–9. doi: 10.1016/j.vaccine.2010.07.057. [DOI] [PubMed] [Google Scholar]
- 63.Annas GJ. Opinion: don't force medical pros to get H1N1 vaccine. 2009. Oct 2, [cited 2012 Jul 23]. Available from: URL: http://www.newsday.com/opinion/opinion-don-t-force-medical-pros-to-get-h1n1-vaccine-1.1496620.
- 64.Feemster KA, Prasad P, Smith MJ, Feudtner C, Caplan A, Offit P, et al. Employee designation and health care worker support of an influenza vaccine mandate at a large pediatric tertiary care hospital. Vaccine. 2011;29:1762–9. doi: 10.1016/j.vaccine.2010.12.115. [DOI] [PubMed] [Google Scholar]
- 65.Trust for America's Health. Fighting flu fatigue. [cited 2011 Dec 3]. Available from: URL: http://healthyamericans.org/assets/files/TFAH2010FluBriefFINAL.pdf.
- 66.The Joint Commission. Oakbrook Terrace (IL): The Joint Commission; 2009. [cited 2011 Dec 3]. Providing a safer environment for health care personnel and patients through influenza vaccination: strategies from research and practice. Also available from: URL: http://www.jointcommission.org/assets/1/18/Flu_Monograph.pdf. [Google Scholar]
- 67.American Medical Association. Report of the Council on Ethical and Judicial Affairs. CEJA report 5-1-10. [cited 2011 Dec 3]. Available from: URL: http://www.ama-assn.org/resources/doc/ethics/ceja-5i10.pdf.
- 68.Arbitrator's opinion and reward. In the matter of a controversy between: SEIU 121RN and United Healthcare Workers-West Union and Los Robles Regional Medical Center, Riverside Healthcare Community Hospital, West Hills Hospital, San Jose Healthcare System, and Good Samaritan Hospital. [cited 2012 Mar 7]. Available from: URL: http://seiu121rn.wtf.localsonline.org/admin/Assets/AssetContent/0293f717-13dc-4603-a412-31c56eaa16a2/546bfa9e-94e2-495f-9d30-54cc81f55e47/7669cf93-d86d-410b-a575-bab5e53a0470/1/Arbitrator_s_Opinion_and_Award-HCA_mand_flu_arb.pdf.
- 69.Grievance Arbitration Award. In the matter of grievance arbitration between: Board of Regents, State of Iowa, University of Iowa Hospitals and Clinics, and Service Employees International Union, Local 199 as grievant. [cited 2012 Mar 7]. Available from: URL: http://www.seiu722.org/PDF/Flu0911/flu vaccine mandate arbritation victory 11-2-09.pdf.
- 70.National Labor Relations Board (US). Administrative law judge decisions: case 19-CA-030154 JD(SF)-44-11 Supplemental Decision-Virginia Mason Hospital and Washington State Nurses Association. [cited 2012 Mar 6]. Available from: URL: http://www.nlrb.gov/cases-decisions/case-decisions/administrative-law-judge-decisions.
- 71.Monto AS, Ohmit SE, Petrie JG, Johnson E, Truscon R, Teich E, et al. Comparative efficacy of inactivated and live attenuated influenza vaccines. N Engl J Med. 2009;361:1260–7. doi: 10.1056/NEJMoa0808652. [DOI] [PubMed] [Google Scholar]
- 72.Nichol KL, Lind A, Margolis KL, Murdoch M, McFadden R, Hauge M, et al. The effectiveness of vaccination against influenza in healthy, working adults. N Engl J Med. 1995;333:889–93. doi: 10.1056/NEJM199510053331401. [DOI] [PubMed] [Google Scholar]
- 73.Treanor JJ, Kotloff K, Betts RF, Belshe R, Newman F, Iacuzio D, et al. Evaluation of trivalent, live, cold-adapted (CAIV-T) and inactivated (TIV) influenza vaccines in prevention of virus infection and illness following challenge of adults with wild-type influenza A (H1N1), A (H3N2), and B viruses. Vaccine. 1999;18:899–906. doi: 10.1016/s0264-410x(99)00334-5. [DOI] [PubMed] [Google Scholar]
- 74.Campbell DS, Rumley MH. Cost-effectiveness of the influenza vaccine in a healthy, working-age population. J Occup Environ Med. 1997;39:408–14. doi: 10.1097/00043764-199705000-00006. [DOI] [PubMed] [Google Scholar]
- 75.Couch RB, Keitel WA, Cate TR. Improvement of inactivated influenza virus vaccines. J Infect Dis. 1997;176(Suppl 1):S38–44. doi: 10.1086/514173. [DOI] [PubMed] [Google Scholar]
- 76.Osterholm MT, Kelley NS, Sommer A, Belongia EA. Efficacy and effectiveness of influenza vaccines: a systematic review and meta-analysis. Lancet Infect Dis. 2012;12:36–44. doi: 10.1016/S1473-3099(11)70295-X. [DOI] [PubMed] [Google Scholar]
- 77.Petrie JG, Ohmit SE, Johnson E, Cross RT, Monto AS. Efficacy studies of influenza vaccines: effect of end points used and characteristics of vaccine failures. J Infect Dis. 2011;203:1309–15. doi: 10.1093/infdis/jir015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Ellebedy AH, Webby RJ. Influenza vaccines. Vaccine. 2009;27(Suppl 4):D65–8. doi: 10.1016/j.vaccine.2009.08.038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Osterhaus A, Fouchier R, Rimmelzwaan G. Towards universal influenza vaccines? Philos Trans R Soc London B Biol Sci. 2011;366:2766–73. doi: 10.1098/rstb.2011.0102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Zakay-Rones Z. Human influenza vaccines and assessment of immunogenicity. Expert Rev Vaccines. 2010;9:1423–39. doi: 10.1586/erv.10.144. [DOI] [PubMed] [Google Scholar]
- 81.New York State Department of Health. Dear Administrator letter: suspension of flu vaccine mandate for health care workers. [cited 2012 Jul 23]. Available from: URL: http://www.health.ny.gov/diseases/communicable/influenza/seasonal/providers/2009-10-23_-suspension_of_mandatory_influenza_immunization.htm.
- 82.Chua JV, Chen WH. Bench-to-bedside review: vaccine protection strategies during pandemic flu outbreaks. Crit Care. 2010;14:218. doi: 10.1186/cc8891. [DOI] [PMC free article] [PubMed] [Google Scholar]


