Abstract
Objective
We compared parental reports of children’s height and weight when the values were estimated vs. parent-measured to determine how these reports influence the estimated prevalence of childhood obesity.
Methods
In the 2007 and 2008 North Carolina Child Health Assessment and Monitoring Program surveys, parents reported height and weight for children aged 3–17 years. When parents reported the values were not measured (by doctor, school, or home), they were asked to measure their child and were later called back. We categorized body mass index status using standard CDC definitions, and we used Chi-square tests and the Stuart-Maxwell test of marginal homogeneity to examine reporting differences.
Results
About 80% (n=509) of the 638 parents who reported an unmeasured height and/or weight participated in a callback and provided updated measures. Children originally classified as obese were subsequently classified as obese (67%), overweight (13%), and healthy weight (19%). An estimated 28% of younger children (<10 years of age) vs. 6% of older children (aged ≥10 years) were reclassified on callback. Having parents who guessed the height and weight of their children and then reported updated values did not significantly change the overall population estimates of obesity.
Conclusion
Our findings demonstrate that using parent-reported height and weight values may be sufficient to provide reasonable estimates of obesity prevalence. Systematically asking the source of height and weight information may help improve how it is applied to research of the prevalence of childhood obesity when gold-standard measurements are not available.
Measuring the effects of public health interventions to reduce the prevalence of childhood obesity will depend on accurate measurement of body mass index (BMI). BMI for age is the most commonly used measure of obesity in children, as it is a valid estimate of adiposity1 and is recommended by the American Academy of Pediatrics and the Centers for Disease Control and Prevention (CDC) when assessing childhood obesity.2,3 In large community surveys, classification of BMI status often relies on parental report of their children’s height and weight. To accurately estimate obesity prevalence, it is critical to determine the validity of these height and weight measures.
Studies to assess whether self-reported height and weight measures from adolescents or parents can be used to correctly classify a child’s BMI status have shown mixed results. One study of parents and adolescents demonstrated that adolescent self-report accurately classifies adolescents into weight categories.4 Correct classification of young children using parent-reported height and weight is more problematic. In a Canadian study, preschoolers’ mothers overestimated weight when they were asked to report child height and weight without measuring their children, but were generally accurate in reporting height.5 Another study comparing two U.S. nationally representative survey populations showed that parents indeed overestimated weight to a small degree, but more significantly underestimated height, particularly among younger children.6 When used systematically for BMI calculations, these specific inaccuracies in the parent-reported measures can lead to an overestimation in the prevalence of childhood obesity among young children.
There is limited information about how parents derive the information they provide for their reports of child height and weight, and whether height, weight, and BMI classification differ based on their source of information. Furthermore, no studies to our knowledge have examined how parental reports may change subsequent to their own measurements of their children. We used a statewide health assessment monitoring program with a unique data collection method with regard to children’s height and weight to achieve the following goals: (1) examine the source of information used by parents reporting their child’s height and weight in a population-based telephone survey, in which parents were asked prior to the survey to measure their child, and demographic characteristics associated with that source; (2) describe change in BMI status among children whose parents reported unmeasured initial height and weight to measured follow-up height and weight; and (3) compare estimated prevalence of childhood obesity using parent-reported unmeasured and measured height and weight.
METHODS
Data
We used cross-sectional data from the 2007 and 2008 North Carolina Child Health Assessment and Monitoring Program (NC CHAMP) surveys. The NC CHAMP is a follow-up to the Behavioral Risk Factor Surveillance System (BRFSS), an annual statewide telephone survey that uses a computer-assisted random-digit-dial telephone interview to assess health characteristics of noninstitutionalized adults aged 18 years and older.7 During the BRFSS interview, respondents living in households with children aged 0–17 years are asked to participate in NC CHAMP. One child is selected through a computerized randomization procedure, and the adult identified as most knowledgeable about the health of the selected child is called one to two weeks later to complete the NC CHAMP survey. The adult BRFSS participants are told during the scheduling of the call for the follow-up NC CHAMP survey that they will be asked about the child’s height and weight, given instructions on how to measure height and weight, and asked to have completed the measurements before they are called back.8
During the NC CHAMP survey, responding parents of children aged 3–17 years are asked how much their child weighs and how tall their child is now. They are then asked how they arrived at their child’s height/weight and given the following responses to choose from: (1) your child told you (his/her) height/weight, (2) you estimated or guessed your child’s height/weight, (3) you used a bathroom scale/tape measure or yardstick within the past six months, (4) the child was weighed/measured at the doctor’s office within the past six months, (5) the child was weighed/measured at school within the past six months, or (6) you determined the measurements some other way. The option for “child told height/weight” was only available for parents of children aged 10 years and older. Respondents who reported option 1, 2, or 6 were deemed to have reported unmeasured height or weight, and were flagged for specific height/weight follow-up callbacks due to concerns of accuracy.
At the conclusion of the NC CHAMP survey, respondents flagged for the height/weight callback were asked to weigh their child with a scale and/or measure with a measuring tape. Those who agreed to do so were asked to weigh the child with shoes off and to measure height with the child’s shoes off and with his/her back against the wall. Participants were provided with a toll-free number to call with the measurements; if the participant did not call, a callback occurred five days subsequent to the initial NC CHAMP interview.
Measures
BMI was calculated as weight (in kilograms) divided by height (in meters squared) for children with values for height and weight reported at initial interview (“initial BMI”). Updated measures of height and/or weight were obtained through follow-up (“callback BMI”) for children whose parents reported unmeasured height or weight at the initial interview and who agreed to the follow-up. Categories for BMI status were derived based on BMI for age and sex percentiles, as calculated using the 2000 CDC growth charts, and defined as follows:<5th percentile = underweight; 5th percentile to<85th percentile = healthy weight; 85th percentile to<95th percentile = overweight; and $95th percentile = obese.3 BMI-for-age percentiles are endorsed as the appropriate assessment of weight status in children.2
Other measures were based on parental report. Race/ethnicity was classified as white, black, Hispanic, or other. We also included the sex of the respondent, such that a female respondent could be a mother, grandmother, or other guardian.
Statistical analyses
We used bivariate and Chi-square statistics to examine differences in BMI as reported on the initial call and on callback. First, we used Pearson’s Chi-square tests to examine whether demographic characteristics differed between respondents who reported measured height/weight and those who reported an estimated, guessed, or otherwise unmeasured height or weight. Then, among those who reported unmeasured height or weight at initial interview, we examined whether children were reclassified into different BMI status categories after parents measured them at home, using a Stuart-Maxwell test of marginal homogeneity. We used Pearson’s Chi-square tests to determine whether demographic characteristics differed for reclassification. We performed all statistical analyses using Stata® 11.0.9 No adjustments for survey design were used for our analysis involving a subset of the total sample.
RESULTS
Sample description
In 2007 and 2008, 5,702 respondents participated in NC CHAMP; 4,828 were respondents with children aged 3–17 years, and their children were evenly divided by sex. More than half of the children (58%) were aged 10–17 years, 70% were non-Hispanic white, 14% were non-Hispanic black, 9% were Hispanic, and 7% were another race/ethnicity. The majority (82%) of respondents were female, with 72% of respondents being the mother of the selected child.
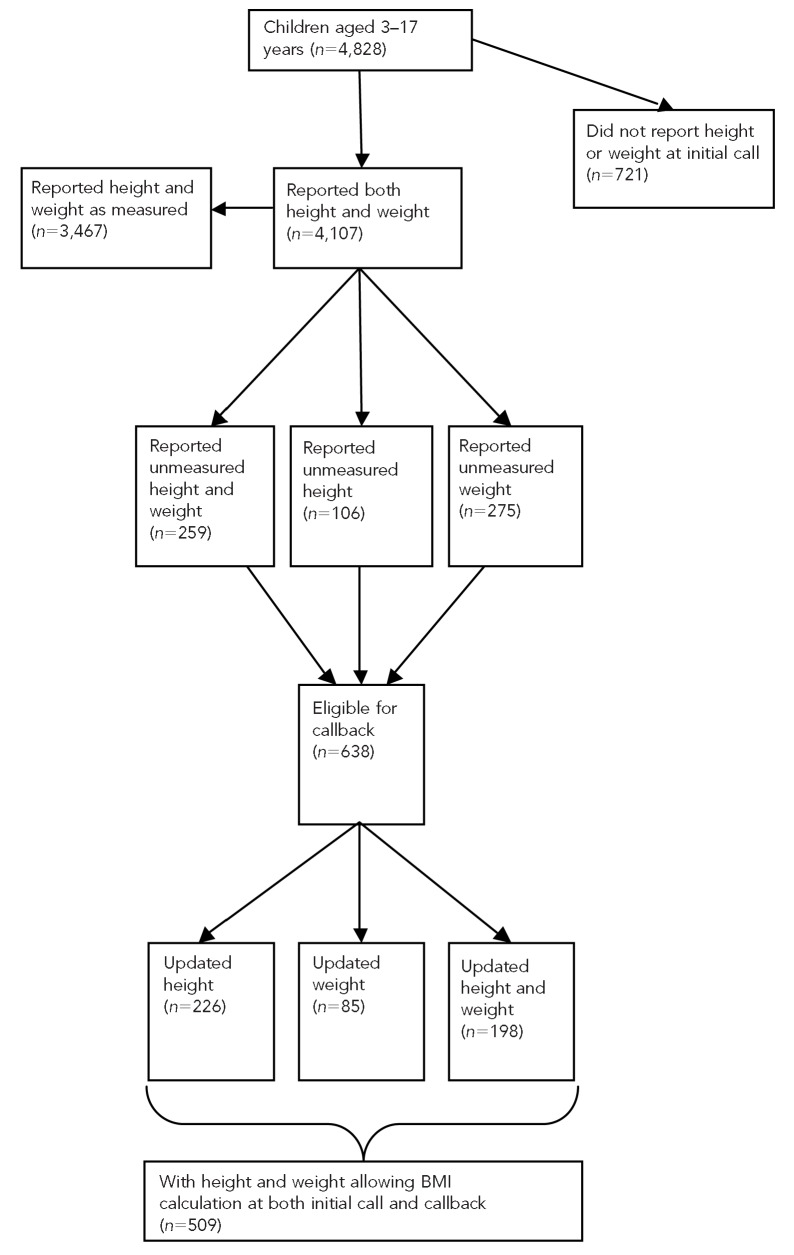
Of the 4,828 respondents who were asked about child height and weight, 4,107 reported height and weight during the initial interview. Of those reporting child height/weight at initial interview, 3,467 (84.4%) reported that both height and weight were measured. The majority of parents reported that height was measured in the doctor’s office (47.2%) or by the parents at home (33.5%), with similar reports for weight (50.7% at the doctor’s office and 35.9% by parents at home). Those who reported an unmeasured, guessed, or estimated height and/or weight (n5638) were flagged for height/weight callback. An additional 721 reporting neither height nor weight at initial call were also flagged for callback, but were not included because this study focused on changes between initial and callback reports. Of those flagged for height/weight callback, 509 (79.8%) ultimately participated and provided updated measures of their child’s height and/or weight: 85 provided updated weight, 226 provided updated height, and 198 provided updates to both height and weight measures. The Figure presents a schematic of sample sizes for reporting of child’s height and weight during initial interview, those identified for height/weight callback, and those who participated in height/weight callback.
Figure.
Schematic of reaching 509 subjects aged 3–17 years for whom information was provided to allow BMI calculation based on unmeasured and measured data: NC CHAMP surveys, 2007 and 2008
BMI = body mass index
NC CHAMP = North Carolina Child Health Assessment and Monitoring Program
Parents reporting measured vs. unmeasured height and weight
There were significant differences by demographics in whether the initially reported height and weight were measured or unmeasured (Table 1). Parents of younger children (aged 3–9 years) and non-Hispanic white or Hispanic children, compared with parents of black children or children of other race/ethnicity, were more likely to report measured height and weight. Female caregivers were more likely than male caregivers to report measured weight but not height. There were no differences in reports of measured vs. unmeasured height and weight based on the sex of the child.
Table 1.
Percentage of respondents to the 2007 and 2008 NC CHAMP surveys who reported measured vs. unmeasured height, weight, and BMI, by selected child and parent characteristics
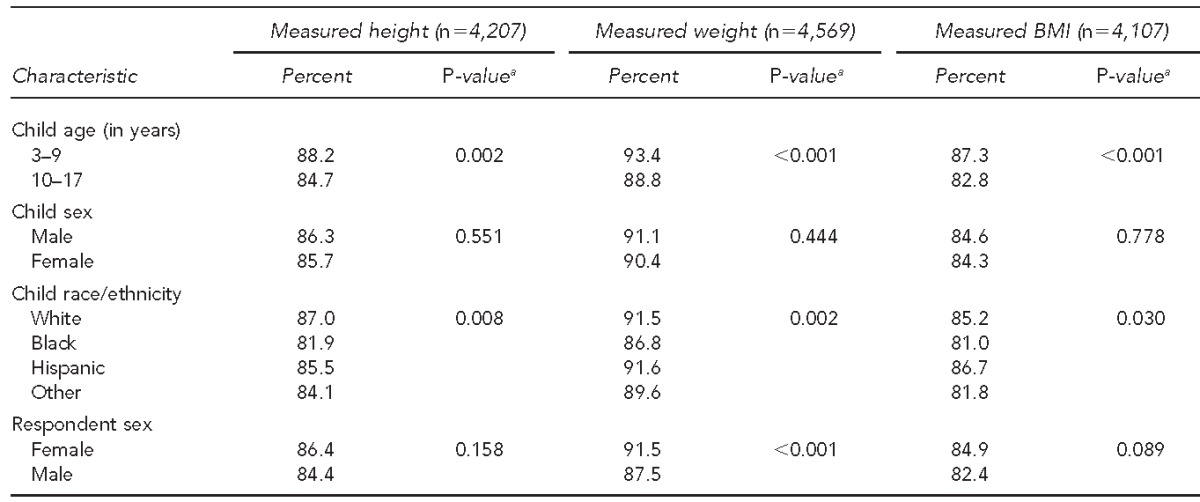
aP-values from Chi-square tests of differences in reporting a measured value by demographic categories
NC CHAMP = North Carolina Child Health Assessment and Monitoring Program
BMI = body mass index
Changes in BMI status based on unmeasured vs. measured height and weight
Based on initial parental reports of height and weight, 5.7% of children were classified as underweight, 50.3% were classified as healthy weight, 19.1% were considered overweight, and 25.0% were obese. When comparing initial unmeasured reports with measured callback reports, most children (66.9%) who were originally classified as obese remained classified as obese, with 13.4% of those originally classified as obese reclassified as overweight and 19.7% reclassified as healthy weight (Table 2). More than half (57.7%) of overweight children remained classified as overweight. Overweight children were equally likely to be reclassified as having a higher BMI status as they were a lower BMI status, with 21.7% subsequently reclassified as obese and 19.6% reclassified as healthy weight following callback. The great majority of healthy weight children (89.5%) at initial report remained categorized as healthy weight. Most children (72.4%) originally classified as underweight were subsequently categorized as healthy weight on callback.
Table 2.
Weight status of children aged 3–17 years at the time of callback, based on weight status from initial unmeasured height and weight reports: NC CHAMP surveys, 2007 and 2008 (n=509)a
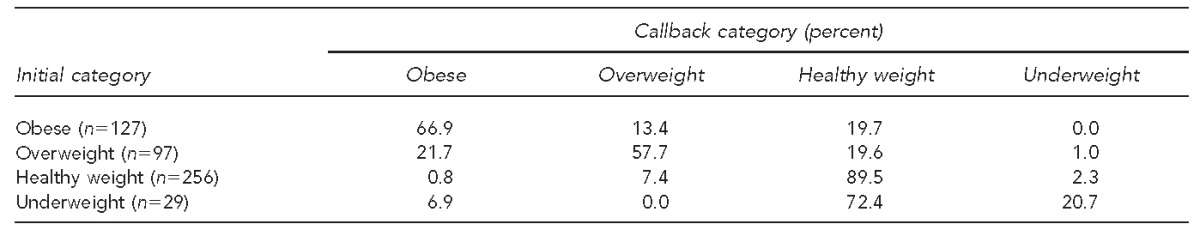
ap<0.001; Stuart-Maxwell test of marginal homogeneity
NC CHAMP = North Carolina Child Health Assessment and Monitoring Program
There were no significant differences in reclassification by race/ethnicity or sex of caretaker who served as the reporter (Table 3). However, younger children were significantly more likely to be reclassified on callback, with 28% of children younger than 10 years of age reclassified into a lower weight category, compared with only 6% of children aged 10 years and older. For children aged 10 years and older, when the child told the parent his/her height or weight, he/she was significantly more likely to remain in the same weight category than if the parent had guessed the child’s measurements.
Table 3.
Change in BMI status category of children aged 3–17 years from initial contact to callback, by demographic characteristics and reported data source: NC CHAMP surveys, 2007 and 2008
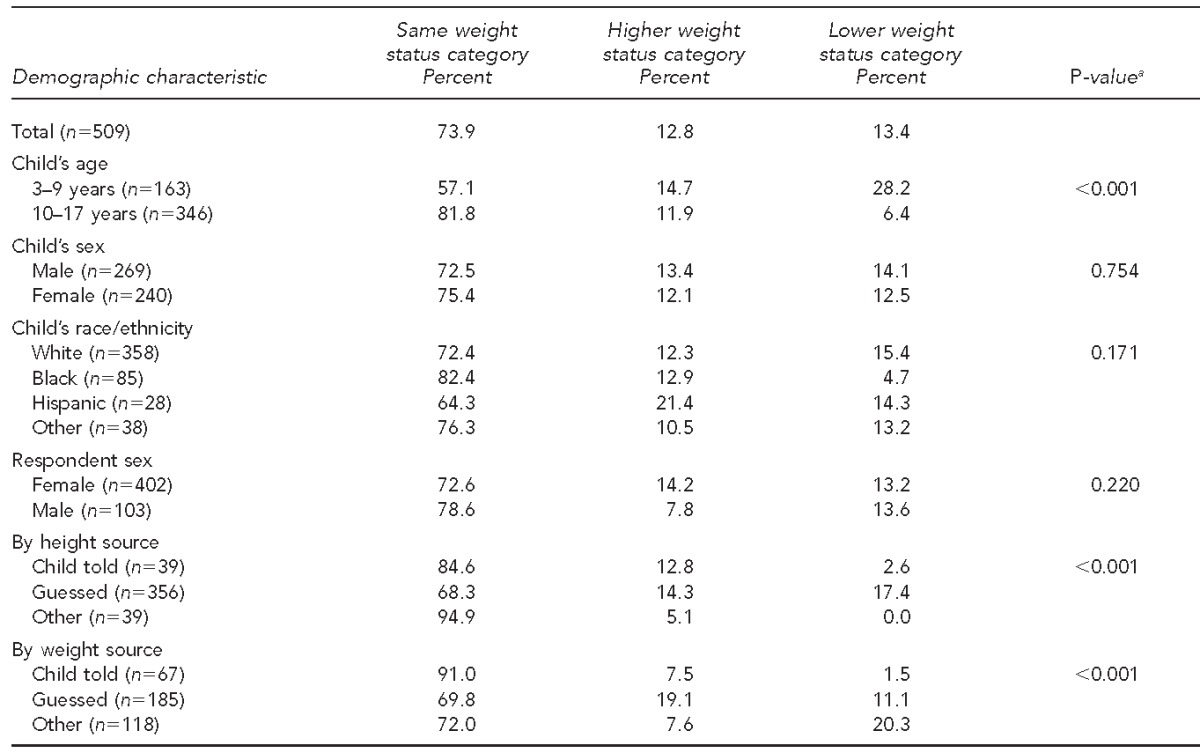
aP-values from Chi-square tests of differences in weight category changes by demographic characteristics and reported data source
BMI = body mass index
NC CHAMP = North Carolina Child Health Assessment and Monitoring Program
On average, both height and weight were underreported when comparing measurements collected at callback and guessing at initial interview. The largest difference was in children younger than 10 years of age, whose parents reported height as 5.4 cm higher, on average, during callback, which resulted in a BMI percentile that was 7.2 points lower upon callback. There were no significant differences by race/ethnicity or child’s sex.
Effect of callback on overall prevalence of overweight and obesity
Finally, we examined the effect on overall estimates of obesity prevalence of including a callback requesting measured height and weight. Due to expected differences in reporting by age, we examined children younger than 10 years of age and children aged 10 years and older separately. Within each age category, overall estimates of the prevalence of obesity were similar whether using the initially collected data or the callback data, which included updated information for parents who reported that the initial weight was not measured. Specifically, including the callback changed the estimated prevalence of obesity among those younger than 10 years of age from 28.2% to 26.8%, and from 17.2% to 17.7% among those aged 10 years and older (data not shown).
DISCUSSION
In summary, our study demonstrated that when parents who report an unmeasured height or weight for their child are asked to subsequently provide a home-measured value, most children remain in the same BMI status category, especially healthy weight children. Parental guessing correctly categorizes children three-quarters of the time, and more than 80% of the time when collapsing overweight and obese. The greatest difference was seen in those initially reported as underweight, who, much of the time, are subsequently categorized as healthy weight. This finding is consistent with previous studies showing largely accurate weight status classification based on parental and adolescent reports.4,10
However, when parents provided an unmeasured height or weight value (e.g., by guessing), young children were more likely to be reclassified to a lower BMI status category following parental measurement. The largest difference was seen among children younger than 10 years of age, for whom the underreporting of height, specifically, leads to an overestimation of obesity. There were no significant differences in BMI recategorization by race, sex of the child, or sex of the reporter.
One important finding was that when the reported height and weight were not based on measured values, but the parent indicated his/her child provided the values, weight classification was largely unchanged when parents subsequently reported a measured value. This finding demonstrates that children older than 10 years of age may be able to provide reports that are accurate enough for appropriate broad weight classification.
Adult research shows that height is generally overreported while weight is underreported.11 Although we were unable to compare our data with clinically measured values, parents in our study generally underreported height, which contrasted adult findings. However, this underreporting of height was much greater among children younger than 10 years of age as compared with older children and adolescents. Importantly, underreporting of height is amplified when calculating BMI, because height is squared in the denominator, leading to an overestimation of obesity prevalence. This underreporting is demonstrated in our finding that young children are frequently reclassified into a lower weight category, in contrast with adults whose overreporting of height contributes to underestimations of obesity prevalence.11 The reason for this underreporting is likely due to height being an ever-changing value among growing children.
Overall, our findings demonstrate that using parent-reported height and weight values, even when identified as unmeasured, may provide reasonable estimates of population-level obesity prevalence when combined with a complete sample of parents who report measuring their child. Measured height and weight are clearly the gold standard, and some large surveys (e.g., the National Health and Nutrition Examination Survey) are able to achieve this standard. However, many other surveys requiring information about obesity are not able to achieve this gold standard. When measured height and weight are not feasible in survey research, it may be possible to obtain additional information that can minimize the effects of misreporting. Identifying the source of the data can flag children who may be more likely to be incorrectly categorized—particularly young children whose height is reported as unmeasured and those initially identified as underweight. Based on previous studies,4,10 and our findings from children who told parents their height or weight, older children may be able to provide height and weight information that is accurate enough for population-based categorization. Systematically asking the source of height and weight information may help to tease apart the more accurate from the less accurate reporters.
Limitations
There were several important limitations to our study. The most important was that we relied on parental report of whether the child’s height and weight were measured. We were also not able to compare parent-reported values with the gold standard of clinically measured values. However, we were able to use a large sample to assess changes when parents indicated the value had been measured, compared with a previous unmeasured report. Additionally, NC CHAMP is based on landline telephones only, meaning the study subjects may not accurately reflect the demographics of the population.
CONCLUSION
Although most parents report that they know their child’s height/weight based on a recently measured value, a substantial percentage of parents provide a guess that is not based on their recollection of a measured value. Gathering information about the source of the data may help to improve the use of parent-reported height and weight data in surveys where clinical measurement is not possible. The two specific pieces of information that are most important are (1) identifying that height was measured among young children and (2) identifying if the child told the parent his/her height and weight. This information about the source of data may help improve the use of parental reports in childhood obesity research.
Footnotes
This study was determined to be exempt from Institutional Review Board review by the University of North Carolina under federal regulation 45 C.F.R. §46.101(b), due to the use of secondary, de-identified data.
References
- 1.Mei Z, Grummer-Strawn LM, Pietrobelli A, Goulding A, Goran MI, Dietz WH. Validity of body mass index compared with other body-composition screening indexes for the assessment of body fatness in children and adolescents. Am J Clin Nutr. 2002;75:978–85. doi: 10.1093/ajcn/75.6.978. [DOI] [PubMed] [Google Scholar]
- 2.Barlow SE. Expert committee recommendations regarding the prevention, assessment, and treatment of child and adolescent overweight and obesity: summary report. Pediatrics. 2007;120(Suppl 4):S164–92. doi: 10.1542/peds.2007-2329C. [DOI] [PubMed] [Google Scholar]
- 3.Kuczmarski RJ, Ogden CL, Guo SS, Grummer-Strawn LM, Flegal KM, Mei Z, et al. 2000 CDC growth charts for the United States: methods and development. Vital Health Stat. 11 2002(246) [PubMed] [Google Scholar]
- 4.Goodman E, Hinden BR, Khandelwal S. Accuracy of teen and -parental reports of obesity and body mass index. Pediatrics. 2000;106(1 Pt 1):52–8. doi: 10.1542/peds.106.1.52. [DOI] [PubMed] [Google Scholar]
- 5.Dubois L, Girad M. Accuracy of maternal reports of pre-schoolers’ weights and heights as estimates of BMI values. Int J Epidemiol. 2007;36:132–8. doi: 10.1093/ije/dyl281. [DOI] [PubMed] [Google Scholar]
- 6.Akinbami LJ, Ogden CL. Childhood overweight prevalence in the United States: the impact of parent-reported height and weight. Obesity (Silver Spring) 2009;17:1574–80. doi: 10.1038/oby.2009.1. [DOI] [PubMed] [Google Scholar]
- 7.North Carolina State Center for Health Statistics. Behavioral Risk Factor Surveillance System. [cited 2012 Sep 4]; Available from: URL: http://www.schs.state.nc.us/SCHS/brfss. [Google Scholar]
- 8.Miles DR, Herrick H, Ford CA. The North Carolina Child Health Assessment and Monitoring Program: survey methodology and data collection. Statistical Primer. 2010;18:1–14. [Google Scholar]
- 9.StataCorp. Stata®: Release 11.0. College Station (TX): StataCorp.; 2009. [Google Scholar]
- 10.Fonseca H, Silva AM, Matos MG, Esteves I, Costa P, Guerra A, et al. Validity of BMI based on self-reported weight and height in adolescents. Acta Paediatr. 2010;99:83–8. doi: 10.1111/j.1651-2227.2009.01518.x. [DOI] [PubMed] [Google Scholar]
- 11.Roberts RJ. Can self-reported data accurately describe the prevalence of overweight? Public Health. 1995;109:275–84. doi: 10.1016/s0033-3506(95)80205-3. [DOI] [PubMed] [Google Scholar]