Abstract
Background
Shortages and maldistribution of primary care physicians (PCPs) are affecting many countries today, including in Germany. As has been suggested, the ensuing problems might be alleviated by delegating some medical tasks to physicians’ assistants (PAs). This was tried in three regions of the German state of Mecklenburg–Western Pomerania under a pilot project entitled AGnES (Arztentlastende gemeindenahe E-Health-gestützte Systemische Intervention, i.e., a community-based, e-health-assisted, systemic intervention to reduce physicians’ workloads). We conducted a survey of all practicing PCPs in the state to assess their overall attitude toward the delegation of home visit tasks, and to determine what they would prefer as the job description and type of employment contract for a PA who would be hired to assist them.
Methods
All PCPs practicing in Mecklenburg–Western Pomerania were asked in a quantitative survey about their willingness to delegate home visits, their perceived barriers to and benefits of home visit delegation to a qualified assistant, the skills they would require of a PA who would be hired to carry out home visits, and their preferred type of employment contract for the PA.
Results
47% of the PCPs (515/1096) responded to the survey. 46% of the respondents were already informally delegating home visit tasks to qualified PAs. Female PCPs were more likely to do so (odds ratio [OR] 1.70), as were PCPs practicing in rural areas (OR 1.63) and those working in individual practice (OR 1.94). Most PCPs were in favor of delegating home visits to qualified PAs (77%). Main advantages were seen in reducing physicians’ workloads (70%) and in increasing their job satisfaction (48%). 34% of PCPs said they would not cover the cost of training PAs.
Conclusion
Acceptance of home visit delegation among PCPs in the state of Mecklenburg–Western Pomerania is high, mainly among the younger physicians. Perceived barriers and benefits of delegation of home visits to qualified PAs should be taken into account in the design of future health-care reforms, so that practice in rural areas can be made more attractive for the incoming generation of PCPs.
Physician shortages and uneven distributions are a reality worldwide. Since the 1960s, shortages of physicians have been reported from the US (1, 2), the UK, Canada (3), and Australia (4). These become noticeable in rural areas first. In almost all countries, the crisis primarily affects healthcare staff in in community-based primary care.
In Germany too an increasing shortage in young physicians has been observed in the past decade (5), which primarily affects the specialty of general practice in primary care. The lacking attractiveness of working as a primary care physician has been explained with the high workload, the comparatively low income, and increasing bureaucracy (6).
Even though the number of physicians rose between 2009 and 2011, a shortage of physicians exists because of an unequal distribution between rural and urban areas (7), which is accompanied by an equally disproportional distribution between the old and the new German states (8).
The regional associations of statutory health insurance physicians in the affected states are trying out different measures in order to entice physicians to regions affected by shortages. At the international level, possible solutions are seen in “task shifting,” that is, the transfer of certain tasks from one cadre to another (9– 11). Delegation of physicians’ tasks to qualified, non-physician staff—physician assistants, physician assistants, or nurses—is the favored option. These mid level health care workers are summarized in Germany under the job designation “qualified medical practice assistants” (Medizinische Fachangestellte, MFA) or “outpatient nurses.”
The problem was addressed in the intervention initiative “Arztentlastende gemeindenahe E-Health-gestützte Systemische Intervention” (AGnES project), a community-based e-health supported systemic intervention designed and implemented by the Institute for Community Medicine at Greifswald University (12– 14) and piloted between July 2007 and December 2008 in three regions in the state of Mecklenburg–Western Pomerania (14, 15). The project aimed to support primary care physicians (PCPs) in infrastructurally weak regions in looking after their increasingly older patients and relieve their workload by delegation of home visits to qualified medical practice assistants (PAs) (16). Three such assistants (outpatient nurses) conducted home visits on behalf of six PCPs, especially to multimorbid older patients. The project was internally evaluated by the project sponsor and project funder (Institute for Community Medicine at Greifswald University).
Furthermore, Mecklenburg-Western Pomerania’s regional association of statutory health insurance physicians commissioned the Institute for General Medicine of the Charité-Universitätsmedizin Berlin to independently evaluate the AGnES project, so as to add to the internal project evaluation in accordance with international guidelines for program evaluation (17).
Important in this context were:
to assess the general acceptability of home visit delegation to qualified PAs among the total number of physicians in Mecklenburg-Western Pomerania;
to elicit their perceived benefits and barriers;
to gain an insight into the physician-preferred profile of qualified PAs and their form of employment.
Method
We conducted a quantitative postal questionnaire survey of all PCPs working in Mecklenburg–Western Pomerania at the time of the study (n = 1096).
The instrument for collecting data was a questionnaire based on a systematic national and international literature search of PCPs’ perceived barriers (5) and benefits (6) with regard to delegation to non-medical personnel (18– 20), which also included questions about the preferred organizational and preventive skills expected of a qualified PA, which were identified as relevant for the realization of home visits.
The questionnaire development was accompanied by public health specialists and statisticians from Charité Berlin. The validation of the questionnaire regarding extent and comprehensibility was done by five PCPs from Berlin. The final version of the questionnaire was conceived in such a manner that it could be completed entirely by the PCPs themselves, within a maximum of 10 minutes.
Outcome variables were captured by using a five-point scale:
Survey population, data collection, data analysis
All 1096 PCPs practicing in Mecklenburg–Western Pomerania at the time of the survey whose contact details were listed by the state association of statutory health insurance physicians were contacted by a letter in the post. Included in the survey population were the six PCPs participating in the AGnES project. In order to increase the rate of responders, a follow-up letter was mailed out two weeks later (18 April 2008). Responses arrived between 25 April 2008 and 18 August 2008. Responder monitoring was undertaken in order to be able to adjust for non-responders if required.
The questionnaire was designed using special software, which enables electronic collection of data by scanning in the responder questionnaires and supports electronic verification of the data. The database quality was checked manually for agreement with the original paper-based questionnaire by two independent scientists and was exported for the purpose of the statistical analysis into PASW Statistics 18.
The collected data were analyzed using descriptive statistical methods. Associations and differences were analyzed for the categorical variables by using Pearson’s Chi square exact sig, two-sided, and Spearman’s correlation. The comparison between first and second responders (received responses before and after the second letter) was done with logistic regression.
In order to calculate the more complex, dichotomous result “acceptability,” we used the tree method. For this purpose we combined the perceived benefits (5 items) and barriers (6 items) by taking the difference in an acceptability index. Significance was defined as p<0.05.
We used the (binary) logistic regression to calculate odds ratios and 95% confidence intervals for “skeptics/supporters.” This variable was used as a dependent variable. PCPs’ characteristics were entered as covariates (for example, age, time spent in the practice and on home visits). Sex, health insurance treatment vouchers per quarter, and number of inhabitants in the area covered by a practice were declared as “categorical covariates.”
Results
The response rate among contacted PCPs was 47% (515/1096). Fifteen of 515 questionnaires were not included in the evaluation as not enough questions had been answered, so that the analysis is based on a total of 500 participants.
The average response rate was 94% and varied between 90% and 97% depending on the question. Among the responders, five were working for the AGnEs project.
First responders were more likely to be from rural areas with populations smaller than 10 000 (odds ratio [OR]: 1.62; 95% confidence interval [CI]: 1.06 to 2.47) than second-round responders. No other differences were observed.
A comparison of the responders with the total population of PCPs in Mecklenburg–Western Pomerania showed that their characteristics were the same (Table 1) (27).
Table 1. Responder characteristics*.
| Physicians’ characteristics | Responder (n = 500)*1 | All PCPs in M-WP (n = 1096) | ||
| Sex | ||||
| Male | 221 | (44%) | 513 | (47%) |
| Female | 274 | (55%) | 583 | (53%) |
| Age | ||||
| Mean (min−max; SD) | 51.8 | (34−77; 8.9) | 52.2 | (33−76; 9.2) |
| ≤ 45 years | 125 | (25%) | 274 | (25%) |
| 46–65 years | 326 | (65%) | 718 | (65%) |
| >65 years | 43 | (9%) | 104 | (10%) |
| PCP’s specialization (licensed as)*2 | ||||
| Family doctor | 415 | (83%) | 897 | (82%) |
| Internist | 83 | (17%) | 199 | (18%) |
| Income (average number of health insurance treatment vouchers per quarter during the last year) | ||||
| <799 | 86 | (17%) | n/a | |
| 800–999 | 107 | (21%) | ||
| 1000–1199 | 112 | (21%) | ||
| 1200–1599 | 119 | (23%) | ||
| ≥ 1600 | 71 | (14%) | ||
| Number of inhabitants in the area served by the practice | ||||
| <10000 (rural) | 185 | (37%) | n/a | |
| 10000–50000 (intermediate) | 196 | (39%) | ||
| 50000–100000 (urban) | 114 | (23%) | ||
*Modified from (27)
*1Totals might not sum to 500 (100%), because not all responders answered all items.
*2Specialties do not exclude one another, 4% of primary care physicians are known under two of the listed specialties. M-WP, Mecklenburg–Western Pomerania, PCP primary care physician
73% of responders worked in individual practice, 18% in group practices, and 9% in ambulatory healthcare centres. Most practices employed two qualified medical practice assistants (47%), 43% of physicians employed three or more, and 10% only one such staff member.
When asked whether they delegated home visits, 46% of participants confirmed that they already did this to a certain extent. Delegating physicians were more likely to be younger (OR: 0.96, 95% CI: 0.93 to 0.99), female (OR: 1.70, 95% CI: 1.12 to 2.58), to be working in rural areas (OR: 1.63, 95% CI: 1.07 to 2.49), to run individual practices (OR: 1.94, 95% CI: 1.14 to 3.28), and to employ three or more qualified PAs (OR: 0.39, 95% CI: 0.23 to 0.67).
Willingness to qualify medical practice personnel to undertake home visits
The general willingness among PCPs to delegate to qualified PAs, if they would be reimbursed for home visit tasks performed by their PAs, existed in 47% of participants (“positive” 24%, “fairly positive” 23%). 30% of PCPs were not willing (15% “not really; 15% “no”). 20% had not yet adopted an unequivocal position.
Attitudes towards the AGnES project and willingness to delegate were highly correlated (Pearson’s Chi square 80.83, p>0.001; Spearman’s correlation 0.32, p = 0.045).
Perceived benefits and barriers to home visit delegation
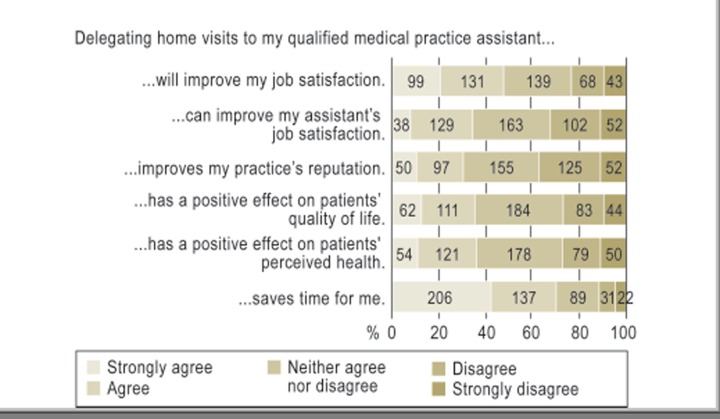
The most commonly cited benefit was time saved as a result of home visit delegation to qualified PAs (70% of PCPs), followed by an increase in physician’s own job satisfaction (48%). One third of those surveyed suspected that such delegation would improve job satisfaction among PAs, improve the reputation of their practice, and could have a positive impact on patients’ quality of life or perceived health (Figure 1).
Figure 1.
Benefits of home visit delegation to an AGnES nurse. Modified from (27). AGnES, Arztentlastende gemeindenahe E-Health-gestützte Systemische Intervention (a community-based, e-health-assisted systemic support for primary care)
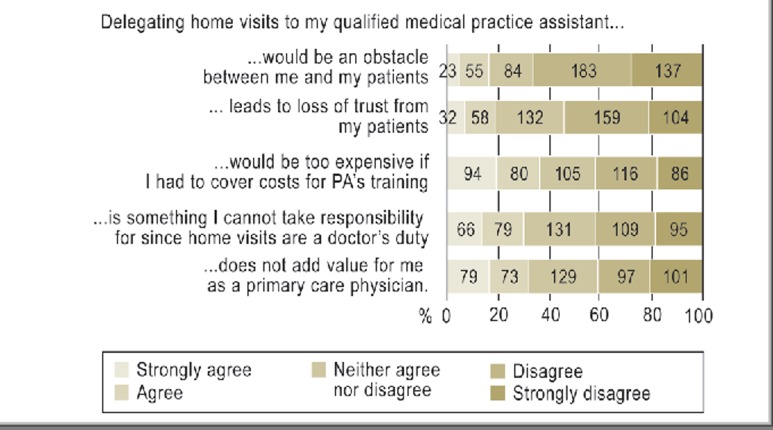
The most important barrier was the cost of qualification: 34% of physicians thought it was too expensive for them to fund the qualification themselves. For almost one-third of physicians, delegation did not add any value for the PCPs. 30% of those surveyed regarded home visits as an activity exclusively for physicians. Only 15% of PCPs assumed that home visit delegation to qualified PAs might create a barrier between physicians and patients or result in patients’ loss of trust (Figure 2)
Figure 2.
Barriers to home visit delegation to an AGnES nurse. Modified from (27). AGnES, Arztentlastende gemeindenahe E-Health-gestützte Systemische Intervention (a community-based, e-health-assisted systemic support for primary care)
Acceptability of home visit delegation
Physicians accepted home visit delegation to qualified PAs as positive: More than three-quarters (77.2%) of physicians spoke in favor of delegation
99 colleagues (19.8%) were skeptical.
Of the 380 physicians in favor, 88% (203) already delegated some home visits to qualified PAs; compared with only 12% (27) of skeptical physicians. Those in favor were younger (OR: 0.96, 95% CI: 0.92 to 0.99), spent slightly less time in the office (OR: 0.97, 95% CI: 0.95 to 0.99), and delegated more than the skeptics (OR: 3.31, 95% CI: 1.73 to 5.23) (Table 2).
Table 2. Odds ratio of acceptance of home visit delegation, logistic regression skeptics (0) versus supporters (1).
| OR supporters | (95-%-CI) | P | |
| Sex (female) (reference value: male, OR=1) | 1.29 | (0.77−2.16) | 0.34 |
| Age (years) | 0.96 | (0.92−0.99) | 0.03 |
| Specialty (primary care physician) (reference value: specialists in internal medicine practicing as primary care physicians, OR=1) | 0.82 | (0.39−1. 71) | 0.59 |
| Population in practice area (reference:<10000, or=1) | |||
| 10000−50000 | 1.11 | (0.62−1.97) | 0.70 |
| >50000 | 2.12 | (0.98−4.58) | 0.06 |
| Average number of health insurance certificates per quarter (reference value: <800 certificates, or=1) | |||
| 800–999 certificates | 1.40 | (0.53−3.68) | 0.49 |
| 1000–1199 certificates | 1.56 | (0.61−3.98) | 0.35 |
| 1200–1599 certificates | 1.61 | (0.66−3.90) | 0.30 |
| ≥ 1600 certificates | 2.99 | (1.24−7.22) | 0.02 |
| Average number of home visits in the past quarter (reference value: up to 5 per week, OR=1) | |||
| 6−10 per week | 1.52 | (0.52−4.49) | 0.45 |
| 11−15 per week | 1.11 | (0.44−2.79) | 0.83 |
| 16−20 per week | 1.20 | (0.49−2.96) | 0.70 |
| 21 and more per week | 1.74 | (0.71−4.28) | 0.23 |
| Time spent on home visits (including traveling time in hours) | 1.04 | (0.99−1.10) | 0.15 |
| Time spent in the practice (total time spent in hours) | 0.97 | (0.95−0.99) | <0.01 |
| Number of qualified medical practice assistants in the office (less than 3) (reference value: <10000. or=1) | 0.69 | (0.36−1.33) | 0.27 |
| Current home visit delegation to qualified medical practice assistants (yes)(Referenz: No, OR=1) | 3.31 | (1.73−5.23) | <0.01 |
95-% CI, 95-% confidence interval
Preferred profile and employment status of qualified medical practice assistants
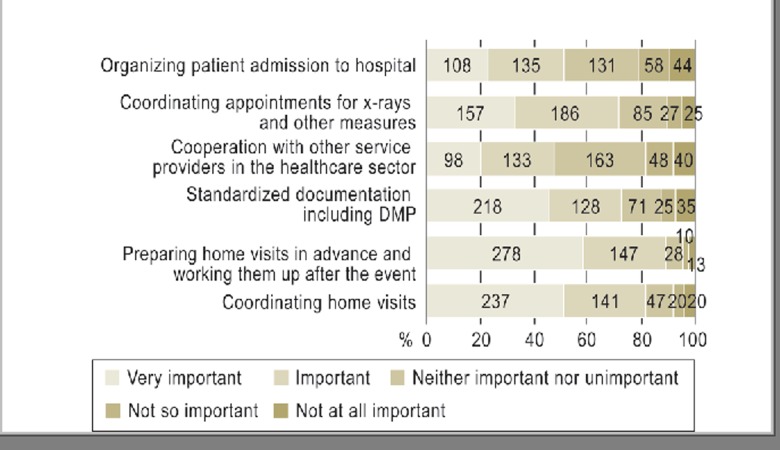
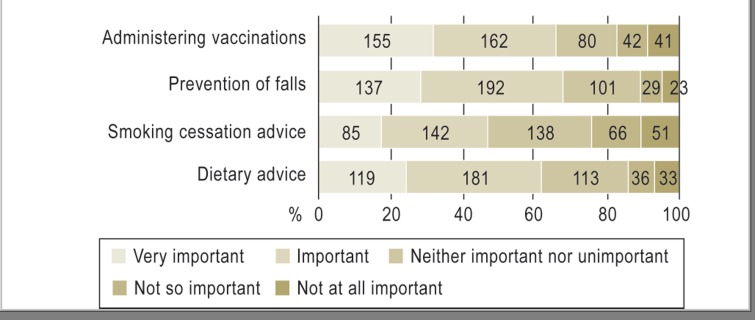
Qualified medical practice assistants’ organizational skills for preliminary care and aftercare (90%) and the coordination of home visits (82%) were rated particularly highly by the participants. More than 70% of physicians rated skills regarding the standardized documentation including disease management programs and coordination of x-rays and other measures as important. Half of the study participants valued cooperation with physicians and other healthcare professionals and organizing patients’ admission to hospital as relevant (Figure 3). In terms of prevention more than 60% of PCPs rated prevention of falls and administering vaccinations as important. Less than 50% of those surveyed found a qualified medical practice assistant’s skill to provide smoking cessation advice as effective for the practice (Figure 4).
Figure 3.
Preferred profile of qualified medical practice assistants undertaking home visits, organizational skills. DMP, disease management program. Modified from (27)
Figure 4.
Preferred profile of qualified medical practice assistants undertaking home visits, preventive skills. Modified from (27)
With regard to the preferred employment status of qualified PAs, PCPs favored an exclusive staff member, who undertakes home visits only for the main practice (80%). Other variants—”undertakes home visits for other PCPs” or “is employed by other PCPs and undertakes home visits on my behalf”—were rejected by 90% of participants.
Discussion
This is the first study to survey all PCPs in Mecklenburg–Western Pomerania about delegating medical practice activities, and 47% of physicians participated. With regard to the PCPs’ characteristics, respondents did not differ from the total PCP population in the state of Mecklenburg–Western Pomerania (21, 22).
Compared with other studies in the outpatient sector, this study had a very high participation rate (23, 24). A survey conducted among PCPs in Hesse by Klingenberg et al. in 2010 had a participation rate of below 25% (25). As early as in 2007 McFarlaine et al. reported the falling participation rates of PCPs in postal surveys (21). Our high participation rate is likely to be due to PCPs’ interest in this important question of what the future shape of primary care will be. The high relevance of the topic is supported by the fact that some 40% of PCPs practicing in rural and eastern regions will reach retirement age within the next decade (26).
Even now, 46% of PCPs—especially younger physicians and women physicians—delegate home visits, to their qualified PAs (27). The sex-specific influence has not been analyzed in previous studies. The study reported by Snijder et al showed an influence of patients’ sex and age on the frequency of home visits: Home visits were more likely to be undertaken to older female patients. However, the study did not investigate the characteristics of the PCPs (28). The fact that female PCPs delegated almost twice the amount of home visits as male PCPs (OR: 1.7) may be explained by gender concordance. It may be assumed that female PCPs are more likely to be confident enough to assess their staff’s technical and social competences than male PCPs. This would make delegation from women to woman more likely than from man to woman. Another explanation of the fact might be the traditional attitudes among male physicians, that they are the only ones qualified to make home visits.
In view of the increasing underprovision of medical care in rural regions and the higher workload among the remaining physicians, the pressure for change is increasing and the perspective on how this problem has been solved in other countries is widening. For example, in the 1960s the model of “physician assistants” (PAs) was developed in the USA in order to counteract the shortage of physicians. PAs receive a three-year education in basic medical skills, including clinical activities under supervision. The training ends with a standardized exam. The job profile requires quality assurance by means of regular further training. PAs do their jobs, which include home visits, under the supervision of a physician (29).
This model introducing physician assistants who act independently and perform clinical tasks has been debated, renamed, and been introduced in England (30– 33), Scotland (34), the Netherlands, Canada, Australia (35), Taiwan, Japan, and New Zealand, among others. Reports from these countries support the delegation of medical services, especially in rural areas (36), including home visits. In Australia and New Zealand, the use of medical assistants/nurses has been regarded as an option for enabling access to appropriate healthcare provision in rural regions (4).
In the meantime, the introduction of community medicine nurses into regular healthcare provision has become a topic of discussion in Germany as well. However, according to a decision by the Federal Joint Committee (GBA, summer 2011), to-date, this task shifting is exclusively possible for regions where underprovision is a problem, and in the context of model projects (37).
Since April 2009 a flat rate for home visit delegation to qualified PAs has been set out in the physicians’ fee scale within the statutory health insurance scheme. However, this can be billed only by PCPs in regions with shortages in medical provision, and only for certain patients (38).
Limitations
The questionnaire was validated by a small number of Berlin PCPs. The possibility of bias cannot be ruled out. Although the survey was conducted on the basis of a complete and current list from the health insurers, selection bias is a possibility. Self-selection bias of the “extreme supporters” or “extreme skeptics” may also be a factor. Social desirability bias is not to be expected in anonymous postal surveys but is still possible. The results cannot be translated to the remaining regions in Germany on the basis of the study as it was conducted.
Conclusion
Delegation of home visits is highly acceptable, especially to younger PCPs. Perceived benefits and barriers in the context of prognostic opinion surveys should therefore be considered to a larger extent when developing future healthcare concepts intended to relieve physicians, in order to increase the appeal of structurally weak regions for future generations of physicians. In future, complex, population-based, cross-sectoral healthcare networks may provide solutions according to regional requirements.
Key Messages.
Home visit delegation to qualified medical practice assistants (PAs) was supported by the majority of primary care physicians (PCPs) in Mecklenburg–Western - Pomerania, provided they could bill for the service.
PCPs were, however, mostly unable to pay the costs of the qualifications required for such PAs.
Qualified PAs who undertake home visits should have organizational and preventive skills in addition to their technical qualification.
Those in support of the measure were younger and already delegated some of their home visits.
Acknowledgments
Translated from the original German by Dr Birte Twisselmann.
The authors thank Mecklenburg–Western Pomerania’s PCPs for participating in the survey, and the National Association of Statutory
Health Insurance Physicians and Mecklenburg–Western Pomerania’s Association of Statutory Health Insurance Physicians for funding the research project “Evaluation of the AGnES project in Mecklenburg–Western Pomerania.”
Footnotes
Conflict of interest statement
The authors declare that no conflict of interest exists.
Figures 1–4 appear with permission from Oxford University Press. Published in Dini L, et al: German GP’s willingness to expand roles of physician assistants: a regional survey of perceptions and informal practices influencing uptake of health reforms in primary health care. Family Practice 2012; 29: 448–54.
References
- 1.Weiner JP. Expanding the US medical workforce: global perspectives and parallels. BMJ. 2007;335:236–238. doi: 10.1136/bmj.39246.598345.94. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Freed GL, Stockman JA. Oversimplifying primary care supply and shortages. JAMA. 2009;301:1920–1922. doi: 10.1001/jama.2009.619. [DOI] [PubMed] [Google Scholar]
- 3.Hooker RS, MacDonald K, Patterson R. Physician assistants in the Canadian Forces. Mil Med. 2003;168:948–950. [PubMed] [Google Scholar]
- 4.Gorman DF, Brooks PM. On solutions to the shortage of doctors in Australia and New Zealand. Med J Aust. 2009;190:152–156. doi: 10.5694/j.1326-5377.2009.tb02320.x. [DOI] [PubMed] [Google Scholar]
- 5.Bundesärztekammer. Deutschen Ärztetages vom. Ulm: 2008. Mai. Beschlussprotokoll des 111. (Last accessed on 2 December 2010, www.bäk.de/downloads/111daetbeschlussprotokoll200808251.pdf.) [Google Scholar]
- 6.Deutscher Ärztetag. Gesundheits-, Sozial- und ärztliche Berufspolitik. Beschlussprotokoll Drucksache I-3 2002;105. Punkt I der Tagesordnung; 8 pp. [Google Scholar]
- 7.Crisp N, Gawanas B, Sharp I. Training the health workforce: scaling up, saving lives. Lancet. 2008;371:689–691. doi: 10.1016/S0140-6736(08)60309-8. [DOI] [PubMed] [Google Scholar]
- 8.Kopetsch T. 5th revised edition. Berlin: Bundesärztekammer und Kassenärztliche Bundesvereinigung; 2010. Dem deutschen Gesundheitswesen gehen die Ärzte aus! Studie zur Altersstruktur und Arztzahlentwicklung; pp. 1–146. [Google Scholar]
- 9.Fulton BD, Scheffler RM, Sparkes SP, Auh EY, Vujicic M, Soucat A. Health workforce skill mix and task shifting in low income countries: a review of recent evidence. Hum Resour Health. 2011;9 doi: 10.1186/1478-4491-9-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Laurant M, Reeves D, Hermens R, Braspenning J, Grol R, Sibbald B. Substitution of doctors by nurses in primary care. Cochrane Database Syst Rev. 2009 doi: 10.1002/14651858.CD001271.pub2. CD001271. [DOI] [PubMed] [Google Scholar]
- 11.Clark CE, Smith LF, Taylor RS, Campbell JL. Nurse led interventions to improve control of blood pressure in people with hypertension: systematic review and meta-analysis. BMJ. 2010;341 doi: 10.1136/bmj.c3995. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Korzilius H, Rabbata S. Gemeindeschwestern: Geheimwaffe gegen Überlastung und Unterversorgung. Dtsch Arztebl. 2006;103(44) [Google Scholar]
- 13.van den Berg N, Fiss T, Meinke C, Heymann R, Scriba S, Hoffmann W. GP-support by means of AGnES-practice assistants and the use of telecare devices in a sparsely populated region in Northern Germany-proof of concept. BMC Fam Pract. 2009;10 doi: 10.1186/1471-2296-10-44. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.van den Berg N, Meinke C, Heymann R, et al. AGnES: Supporting general practitioners with qualified medical practice personnel - model project evaluation regarding quality and acceptance. Dtsch Arztebl Int. 2009;106(1-2):3–9. doi: 10.3238/arztebl.2009.0003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.van den Berg N, Kleinke S, Heymann R, Oppermann RF, Jakobi B, Hoffmann W. Transfer of the AGnES concept to the regular German health-care system: legal evaluation, reimbursement, qualification. Gesundheitswesen. 2010;72:285–292. doi: 10.1055/s-0029-1233472. [DOI] [PubMed] [Google Scholar]
- 16.Hoffmann W, van den Berg N. AGnES: Supporting general practitioners with qualified medical practice personnel-model project evaluation regarding quality and acceptance. In Reply. Dtsch Arztebl Int. 2009;106(20):357–358. doi: 10.3238/arztebl.2009.0003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Austrian Development Agency. Österreichischen Entwicklungszusammenarbeit. Wien: 2008. Leitfaden für Projekt-und Programmevaluierungen. [Google Scholar]
- 18.Bowling A. Delegation to nurses in general practice. J R Coll Gen Pract. 1981;31:485–490. [PMC free article] [PubMed] [Google Scholar]
- 19.Jones K, Gilbert P, Little J, Wilkinson K. Nurse triage for house call requests in a Tyneside general practice: patients’ views and effect on doctor workload. Br J Gen Pract. 1998;48:1303–1306. [PMC free article] [PubMed] [Google Scholar]
- 20.Stuck AE, Minder CE, Peter-Wuest I, et al. A randomized trial of in-home visits for disability prevention in community-dwelling older people at low and high risk for nursing home admission. Arch Intern Med. 2000;160:977–986. doi: 10.1001/archinte.160.7.977. [DOI] [PubMed] [Google Scholar]
- 21.McFarlane E, Olmsted MG, Murphy J, Hill CA. Nonresponse bias in a mail survey of physicians. Eval Health Prof. 2007;30:170–185. doi: 10.1177/0163278707300632. [DOI] [PubMed] [Google Scholar]
- 22.Templeton L, Deehan A, Taylor C, Drummond C, Strang J. Surveying general practitioners: does a low response rate matter? Br J Gen Pract. 1997;47:91–94. [PMC free article] [PubMed] [Google Scholar]
- 23.Asch DA, Jedrziewski MK, Christakis NA. Response rates to mail surveys published in medical journals. J Clin Epidemiol. 1997;50:1129–1136. doi: 10.1016/s0895-4356(97)00126-1. [DOI] [PubMed] [Google Scholar]
- 24.Schoen C, Osborn R, Doty MM, Squires D, Peugh J, Applebaum S. A survey of primary care physicians in eleven countries, 2009: perspectives on care, costs, and experiences. Health Aff (Millwood) 2009;28:w1171–w1183. doi: 10.1377/hlthaff.28.6.w1171. [DOI] [PubMed] [Google Scholar]
- 25.Klingenberg A, Broge B, Herholz H, Szecsenyi J, Ose D. Evaluation of special GP-centered health care contracts in Germany by the participating GPs. present situation and future perspectives. Med Klin. 2010;105:89–95. doi: 10.1007/s00063-010-1012-8. [DOI] [PubMed] [Google Scholar]
- 26.Kolpetsch T Bundesärztekammer - Kassenärztliche Bundesvereinigung. Daten, Fakten, Trends Symposium. Berlin: „Demografischer Wandel und ärztliche Versorgung in Deutschland“; 2009. Studie zur Altersstruktur-und Arztzahlentwicklung. [Google Scholar]
- 27.Dini L, Sarganas G, Boostrom E, Ogawa S, Heintze C, Braun V. German GPs’ willingness to expand roles of physician assistants: a regional survey of perceptions and informal practices influencing uptake of health reforms in primary health care. Fam Pract. 2012;29:448–454. doi: 10.1093/fampra/cmr127. [DOI] [PubMed] [Google Scholar]
- 28.Snijder EA, Kersting M, Theile G, et al. Home visits in German general practice: findings from routinely collected computer data of 158,000 patients. Gesundheitswesen. 2007;69:679–685. doi: 10.1055/s-2007-993181. [DOI] [PubMed] [Google Scholar]
- 29.Frossard LA, Liebich G, Hooker RS, Brooks PM, Robinson L. Introducing physician assistants into new roles: international experiences. Med J Aust. 2008;188:199–201. doi: 10.5694/j.1326-5377.2008.tb01583.x. [DOI] [PubMed] [Google Scholar]
- 30.Paniagua H, Stewart A. Medical care practitioners: introducing a new profession into the UK. Br J Nurs. 2005;14:405–408. doi: 10.12968/bjon.2005.14.7.17949. [DOI] [PubMed] [Google Scholar]
- 31.Castledine G. Do we need physician assistants in the UK? Br J Nurs. 1996;5 doi: 10.12968/bjon.1996.5.2.124. [DOI] [PubMed] [Google Scholar]
- 32.Parle JV, Begg P. Physician assistants. UK universities are on the case. BMJ. 2009;339 doi: 10.1136/bmj.b4520. [DOI] [PubMed] [Google Scholar]
- 33.Sibbald B, Laurant MG, Reeves D. Advanced nurse roles in UK primary care. Med J Aust. 2006;185:10–12. doi: 10.5694/j.1326-5377.2006.tb00440.x. [DOI] [PubMed] [Google Scholar]
- 34.Buchan J, O’May F, Ball J. New role, new country: introducing US physician assistants to Scotland. Hum Resour Health. 2007;5 doi: 10.1186/1478-4491-5-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.O’Connor TM, Hooker RS. Extending rural and remote medicine with a new type of health worker: physician assistants. Aust J Rural Health. 2007;15:346–351. doi: 10.1111/j.1440-1584.2007.00926.x. [DOI] [PubMed] [Google Scholar]
- 36.Duttera MJ, Harlan WR. Evaluation of physician assistants in rural primary care. Arch Intern Med. 1978;138:224–228. [PubMed] [Google Scholar]
- 37.Osterloh F. Übertragung heilkundlicher Tätigkeiten: Substitution versus Delegation. Dtsch Arztebl. 2011;108(43) [Google Scholar]
- 38.Gerst T. EBM-Vergütung für Praxisassistentin: Nicht üppig, aber extrabudgetär. Dtsch Arztebl. 2009;106(15) [Google Scholar]