Abstract
Background:
Although frameless stereotactic needle biopsy is an accepted procedure for the diagnosis of intracranial lesions, findings are nondiagnostic in 2–15% of patients and no recommendations yet exist to guide subsequent care. After reviewing the postoperative course after nondiagnostic biopsy of 28 patients, we developed a paradigm to guide management in the future.
Methods:
In reviewing the medical records of 284 frameless stereotactic needle biopsies (January 2000 to December 2006), we identified a subset of 28 patients who underwent 29 (10.2%) biopsies that did not yield a definitive diagnosis based on permanent pathologic samples. Postoperative treatment plans and clinical courses were further examined in 21 patients; 7 without follow-up were excluded.
Results:
Of the 21 patients, lesion location and characteristics guided the surgeon's decision to recommend further surgery or initiate empiric treatment. Soon after initial biopsy, five patients underwent a second procedure (biopsy or resection) that yielded diagnostic pathologic tissue. Of 16 patients who had empiric treatment, 7 (43.7%) subsequently had their treatment plan changed because of a lack of improvement and 5 underwent a second biopsy (4 diagnostic). Evolving clinical information precipitated treatment change in two patients. Of 10 patients who had a second surgery for better diagnostic information, the diagnostic yield was 90%.
Conclusions:
Considering the 90% diagnostic yield, we now recommend repeat surgery for most patients with nondiagnostic biopsies, especially for lesions considered potentially neoplastic or infectious. Empiric management, for lesions likely to be neurodegenerative, is an option but requires close follow-up examination.
Keywords: Brain tumor, diagnosis, frameless stereotactic biopsy
INTRODUCTION
Frameless stereotactic needle biopsy is now an accepted, standard tool often used in the diagnosis and management of brain lesions. This technique has been shown to be safe and effective, achieving a high diagnostic yield for most patients. [2–4,8,9,10,15,16,20] Nonetheless, prior studies have shown that in 2-15% of cases a pathologic diagnosis is not achieved, [4,6,7,10] leaving the physician and the patient uncertain as to the next step. Some studies examined the characteristics that predispose toward a nondiagnostic biopsy, such as nonneoplastic lesions, [13,21] deep lesions, and small lesions. [4,6,7,10,21] However, few studies have looked at the management of nondiagnostic biopsies and no clear paradigm exists to guide physicians. Physicians are often left with the choice of observation, empiric management, or a repeat biopsy. No data currently have addressed the success of repeat biopsy and only limited data exist regarding the success of empiric management. Therefore, to better understand the management of these patients and develop a treatment paradigm for these clinical situations, we reviewed our experience with patients for whom no pathologic diagnosis could be made by stereotactic biopsy. From this review, we developed a paradigm for the care of such patients in the future.
CLINICAL MATERIALS AND METHODS
We retrospectively reviewed pathology reports of 284 previously identified cases of frameless stereotactic needle biopsy performed from January 1, 2000 through December 31, 2006. Details of the surgical technique have been published previously. [1] Briefly summarized, the target and trajectory were planned using a frameless navigation system (BrainLab, BrainLab, Inc., Westchester, IL or Stealth, Medtronic Inc., Minneapolis, MN) and the patient registered to the system using scalp fiducials. The burr hole, and dural and pial openings were made over the entry point and the biopsy needle advanced to the target (calculated using the offset function). Samples were taken in quadrants.
We identified 29 (10.2%) cases in which no pathologic diagnosis could be made from frozen and permanent samples. In addition to samples specifically defined as nondiagnostic by the pathologist, those classified as normal brain tissue, gliosis, or cerebritis without underlying etiology were included. Further information was then abstracted from the paper and electronic charts, specifically clinical presentation, imaging findings, operative course, postoperative clinical course, and the results of any further studies or surgeries performed. Abstracted data were entered into a password-protected database accessible only by the authors, and all identifying information was deleted and files containing protected health information were destroyed. This study was completed with approval of the University of Cincinnati and TriHealth Institutional Review Boards (UC #06-08-15-03-EE and TriHealthB # 06108-0806-064).
RESULTS
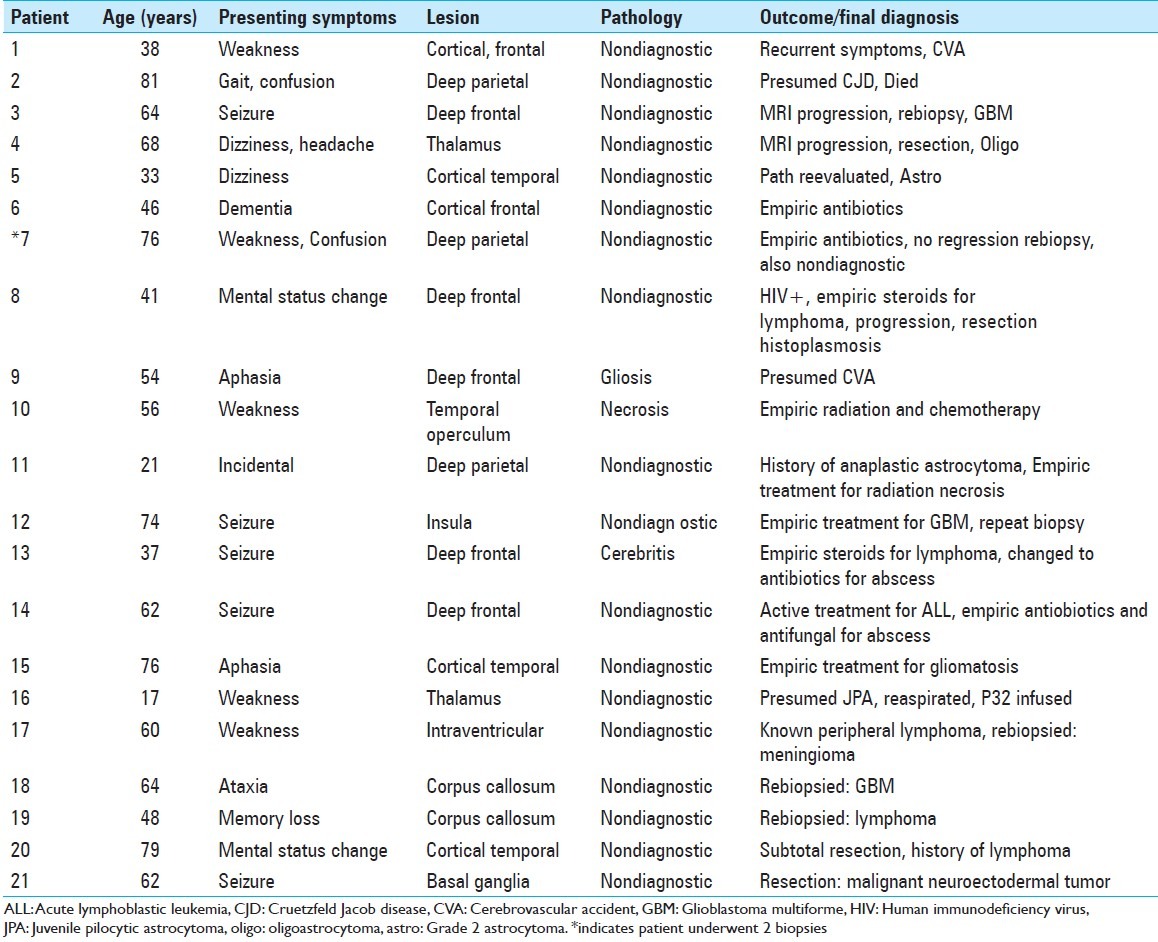
The 29 nondiagnostic biopsies were performed in 28 patients, that is, 13 females and 15 males (one male underwent two separate stereotactic biopsies of the same lesion, both nondiagnostic) who ranged in age from 17 to 83 years (mean 60 years). The procedures were performed by 11 surgeons at 5 hospitals. Although the exact number of tissue samples was not documented, samples were taken along 1-4 needle trajectories (average 1.58). Of the 28 lesions, 22 (75.6%) were considered to be deep in location. Postoperative head computed tomograpgy (CT) scans were obtained in 15 (51.7%) of 29 cases. Concordance between the actual and intended biopsy sites (as determined by small focus of air or blood) was documented on 13 (86.7%) of 15 CT scans. Of the 28 patients, no follow-up information was available for 7 (25%) and the remaining 21 patients are the basis of this retrospective study [Table 1].
Table 1.
Patient demographics and lesion characteristics
Follow-up course
The 21 patients followed one of two courses of initial management, either early surgery (5) or empiric treatment (16) [Figure 1 and Table 2].
Figure 1.

Clinical course following non-diagnostic stereotactic needle biopsy (bx). Numbers of patients is indicated in parentheses. Asterisk (*) indicates patients whose course was altered by additional information or second surgery. (with permission from the Mayfield Clinic).
Table 2.
Clinical course following nondiagnostic stereotactic needle biopsy in 28 patients

Early surgery (5 Patients)
Five patients underwent early surgery, either a second biopsy or resection of the lesion within 2 weeks of the initial procedure. When repeat stereotactic needle biopsy was performed in two patients, each was diagnostic, confirming one with glioblastoma multiforme (GBM) and the other with meningioma. The decision to re-biopsy one of these patients was based on a head CT that indicated the first biopsy site had missed the lesion. A third patient had an open biopsy (to ensure pial/cortical biopsy) that revealed lymphoma. In two patients who underwent lesion resection, one had a malignant neuroectodermal tumor, and one had a metastatic lymphoma. Therefore, the diagnostic yield of the second procedure in this subgroup of five patients was 100%.
Empiric therapy (16 Patients)
A management plan was developed for each of 16 patients based on the presumed diagnosis (neoplastic, infectious, or degenerative) derived from the clinical situation and corroborating studies. Serial imaging was performed, with or without empiric therapy.
Ten patients were thought most likely to have a neoplastic process. Three patients were initially monitored closely by serial MRI but, because of lesion progression, two underwent additional surgery that led to diagnosis: A repeat stereotactic needle biopsy revealed a GBM and an open resection revealed an oligodendroglioma. In the third patient, the original pathology sample was sent for analysis at another center during the inter-scan period; 2 months later, the reevaluated samples were deemed consistent with Grade 2 astrocytoma and fractionated radiotherapy was started. Empiric treatment was started in seven patients. Two of these patients had a prior history of central nervous system (CNS) tumor (anaplastic astrocytoma and pilocytic astrocytoma) whose lesions were treated as radiation necrosis and recurrence, respectively. Three patients underwent chemotherapy and radiation for presumed glial tumors. These five patients followed a clinical course that corroborated the presumed diagnosis. Steroids were administered to two patients for presumed lymphoma, neither improved. Ultimately, both patients were diagnosed with infection: One after lesion resection, the other after a history of chronic oral infection was discovered.
Three patients were presumed to have infection as the underlying etiology. With administration of antibiotics, one patient improved and the other two patients who did not improve then underwent a second biopsy. Lymphoma was diagnosed by open biopsy in one patient. When stereotactic needle biopsy was again nondiagnostic in the second patient, treatment was stopped without progression noted.
Three patients were presumed to have a neurodegenerative process. Two patients were diagnosed as having suffered a cerebrovascular accident (CVA); both suffered additional CVAs. Creutzfeld-Jacob Disease was believed to be the cause of rapid neurologic decline and death in one patient.
The initial management plan that was based on the presumed diagnosis was later modified for 7 (43.7%) of 16 patients. Modifications included a second biopsy procedure or resection in five patients, only one of which was again nondiagnostic on permanent pathology. Considering all 10 patients who underwent a second surgical procedure (immediate or delayed) the diagnostic yield was 90% (9 of 10).
DISCUSSION
Frameless stereotactic biopsy has developed as a reliable and safe procedure for the diagnosis of intracranial lesions. Although the goal of the biopsy procedure is to obtain information that leads to effective and efficient treatment for patients, even with advanced technology driving this technique, biopsies can be nondiagnostic in 2-15% of cases. [4,6,7,10,21] Many reports have examined causes increasing the risk of a failed stereotactic biopsy, such as small lesion size, deep location, and nonneoplastic diagnosis. [4,6,7,10,21] Other factors include the presence of necrosis, poorly differentiated tumors, lack of contrast enhancement, and deep tumor location. [11,12,14,17,18] Attention to these factors during preoperative planning and execution of the procedure are imperative to optimize both diagnostic yield and patient care. Unfortunately, this is not always accomplished and a pathway must be chosen for subsequent care.
With few reports focused on the management of a nondiagnostic biopsy and no clear treatment paradigm for these patients, we initiated our retrospective review to addresses the clinical dilemma presented when stereotactic needle biopsy does not provide a definitive pathologic diagnosis. Among our patients, clinical situations varied considerably and several postoperative pathways were pursued [Figure 1]. Five patients underwent immediate reoperation that yielded a definitive diagnosis, whereas the majority (16 patients) were empirically treated using the information provided by the clinical findings, lesion location, and imaging characteristics. Although 56.3% of patients followed a course consistent with the presumed diagnosis and responded effectively to the treatment, a significant 43.7% of patients had revision of their initial treatment plan because of disease progression or nonresponse to therapy. In more than a third of all patients, a second surgical procedure was used. Continuous monitoring of the patients’ progress and integration of new information was essential in leading to treatment changes.
Based on this review, we propose a framework for the care of patients when findings on needle biopsy are inconclusive [Figure 2]. Intraoperatively, the surgeon should confirm with the pathologist that diagnostic tissue has been obtained. If not, a CT or nagnetic resonance imaging (MRI) should be obtained. The timing of such imaging (intraoperatively or postoperatively) will depend on radiology and anesthesia resources available at the institution. Repeat biopsy should then be performed, guided by the imaging results.
Figure 2.

Paradigm for patient care after non-diagnostic stereotactic needle biopsy (with permission from the Mayfield Clinic).
When the pathologist and surgeon believe that diagnostic tissue was obtained during the biopsy, yet final pathology results are inconclusive, imaging should be performed to assess the concordance between the intended and actual biopsy locations. If the lesion was missed during the initial biopsy, repeat biopsy should be performed. If the target was biopsied, consideration should be given to a second pathology review. In the case of a mass lesion that is easily accessible surgically, we recommend open biopsy with or without complete resection. Inaccessible mass lesions should be re-biopsied, particularly when neoplasm or infection is suspected. Though a frame-based biopsy may be considered, two large studies have shown no difference in diagnostic yield between these techniques. [6,20] Lesions likely due to neurodegenerative disease may be treated empirically or observed as allowed based on the available information. Any patient treated empirically must be followed closely by examination and imaging to allow treatment to be revised when necessary.
Study limitations
Because this retrospective review included patients managed during a 7-year period by 11 surgeons at 5 hospitals, the clinical presentations, courses, and management varied. First, treatment decisions were made by each surgeon based on their own preferences and not according to a specific treatment paradigm. These varied approaches, as well as the small sample size, limit statistical analysis and modeling. However, analysis of multiple clinical approaches also can be seen as a strength of this report because it reflects the many ways in which patients with nondiagnostic biopsies are currently managed. Secondly, as a retrospective study, not all data were available for review and specifically lesion size could not be calculated from imaging reports for all patients. Finally, another limitation is that our true rate of biopsy misses could not be determined because of the relatively few patients (51.7%) who had postoperative CT scans. As previously reported, [19] we do not routinely obtain a CT scan after every stereotactic biopsy. As illustrated by this cohort, confirmation of the biopsy site does not guarantee that the tissue obtained will be diagnostic. However, before wound closure, the surgeon does obtain the pathologist's evaluation of the tissue samples and confirmation that diagnostic tissue was likely obtained. As others have reported, this precaution may reduce the number of inconclusive pathologic diagnoses, but does not preclude it. [5,14]
CONCLUSIONS
Although frameless stereotactic needle biopsy has a well-established place for intracranial lesions, a definitive diagnosis is not always obtained, even with appropriate precautions. In analysis of care provided to patients after a nondiagnostic needle biopsy, we found that management plans based on a presumed diagnosis were appropriate in only 53.3% of the patients. Nearly half of the patients underwent a second surgical procedure, which was typically successful. Therefore, for cases that involve potentially neoplastic or infectious lesions, we recommend a second surgical procedure. Lesions likely to be nonneoplastic and noninfectious, such as neurodegenerative lesions, can be followed and managed empirically in the majority of patients. In all patients with a nondiagnostic biopsy and without a repeat procedure, close follow-up is advised.
Footnotes
Disclaimer: The authors of this paper have received no outside funding, and have nothing to disclose.
Available FREE in open access from: http://www.surgicalneurologyint.com/text.asp?2012/3/5/315/103026
Contributor Information
Ellen L. Air, Email: Eair@mayfieldclinic.com.
Ronald E. Warnick, Email: nsgymd@mac.com.
Christopher M. McPherson, Email: Cmcpherson@mayfieldclinic.com.
REFERENCES
- 1.Air EL, Leach JL, Warnick RE, McPherson CM. Comparing the risks of frameless stereotactic biopsy in eloquent and non-eloquent regions of the brain: A retrospective review of 284 Cases. J Neurosurg. 2009;111:820–4. doi: 10.3171/2009.3.JNS081695. [DOI] [PubMed] [Google Scholar]
- 2.Apuzzo ML, Chandrasoma PT, Cohen D, Zee CS, Zelman V. Computed imaging stereotaxy: Experience and perspective related to 500 procedures applied to brain masses. Neurosurgery. 1987;20:930–7. doi: 10.1227/00006123-198706000-00019. [DOI] [PubMed] [Google Scholar]
- 3.Barnett GH, Miller DW, Weisenberger J. Frameless stereotaxy with scalp-applied fiducial markers for brain biopsy procedures: Experience in 218 cases. J Neurosurg. 1999;91:569–76. doi: 10.3171/jns.1999.91.4.0569. [DOI] [PubMed] [Google Scholar]
- 4.Bernays RL, Kollias SS, Khan N, Brandner S, Meier S, Yonekawa Y. Histological yield, complications, and technological considerations in 114 consecutive frameless stereotactic biopsy procedures aided by open intraoperative magnetic resonance imaging. J Neurosurg. 2002;97:354–62. doi: 10.3171/jns.2002.97.2.0354. [DOI] [PubMed] [Google Scholar]
- 5.Colbassani HJ, Nishio S, Sweeney KM, Bakay RA, Takei Y. CT-assisted stereotactic brain biopsy: Value of intraoperative frozen section diagnosis. J Neurol Neurosurg Psychiatry. 1988;51:332–41. doi: 10.1136/jnnp.51.3.332. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Fountas KN, Kapsalaki EZ, Smisson HF, 3rd, Hartman LP, Johnston KW, Robinson JS Jr. Results and complications from the use of a frameless stereotactic microscopic navigator system. Stereotact Funct Neurosurg. 1998;71:76–82. doi: 10.1159/000029650. [DOI] [PubMed] [Google Scholar]
- 7.Gralla J, Nimsky C, Buchfelder M, Fahlbusch R, Ganslandt O. Frameless stereotactic brain biopsy procedures using the Stealth Station: Indications, accuracy and results. Zentralbl Neurochir. 2003;64:166–70. doi: 10.1055/s-2003-44620. [DOI] [PubMed] [Google Scholar]
- 8.Grossman R, Sadetzki S, Spiegelmann R, Ram Z. Haemorrhagic complications and the incidence of asymptomatic bleeding associated with stereotactic brain biopsies. Acta Neurochir (Wien) 2005;147:627–31. doi: 10.1007/s00701-005-0495-5. discussion 631. [DOI] [PubMed] [Google Scholar]
- 9.Hall WA. The safety and efficacy of stereotactic biopsy for intracranial lesions. Cancer. 1998;82:1749–55. doi: 10.1002/(sici)1097-0142(19980501)82:9<1756::aid-cncr23>3.0.co;2-2. [DOI] [PubMed] [Google Scholar]
- 10.Heper AO, Erden E, Savas A, Ceyhan K, Erden I, Akyar S, Kanpolat Y, et al. An analysis of stereotactic biopsy of brain tumors and nonneoplastic lesions: A prospective clinicopathologic study. Surg Neurol. 2005;64(Suppl 2):S82–88. doi: 10.1016/j.surneu.2005.07.055. [DOI] [PubMed] [Google Scholar]
- 11.Jain D, Sharma MC, Sarkar C, Deb P, Gupta D, Mahapatra AK. Correlation of diagnostic yield of stereotactic brain biopsy with number of biopsy bits and site of the lesion. Brain Tumor Pathol. 2006;23:71–5. doi: 10.1007/s10014-006-0204-y. [DOI] [PubMed] [Google Scholar]
- 12.Javedan SP, Tamargo RJ. Diagnostic yield of brain biopsy in neurodegenerative disorders. Neurosurgery. 1997;41:823. doi: 10.1097/00006123-199710000-00011. [DOI] [PubMed] [Google Scholar]
- 13.Kim JE, Kim DG, Paek SH, Jung HW. Stereotactic biopsy for intracranial lesions: Reliability and its impact on the planning of treatment. Acta Neurochir (Wien) 2003;145:547. doi: 10.1007/s00701-003-0048-8. [DOI] [PubMed] [Google Scholar]
- 14.McGirt MJ, Woodworth GF, Coon AL, Frazier JM, Amundson E, Garonzik I, et al. Independent predictors of morbidity after image-guided stereotactic brain biopsy: A risk assessment of 270 cases. J Neurosurg. 2005;102:897–901. doi: 10.3171/jns.2005.102.5.0897. [DOI] [PubMed] [Google Scholar]
- 15.Paleologos TS, Dorward NL, Wadley JP, Thomas DG. Clinical validation of true frameless stereotactic biopsy: Analysis of the first 125 consecutive cases. Neurosurgery. 2001;49:830. doi: 10.1097/00006123-200110000-00009. [DOI] [PubMed] [Google Scholar]
- 16.Ranjan A, Rajshekhar V, Joseph T, Chandy MJ, Chandi SM. Nondiagnostic CT-guided stereotactic biopsies in a series of 407 cases: Influence of CT morphology and operator experience. J Neurosurg. 1993;79:839–44. doi: 10.3171/jns.1993.79.6.0839. [DOI] [PubMed] [Google Scholar]
- 17.Roessler K, Czech T, Dietrich W, Ungersboeck K, Nasel C, Hainfellner JA, et al. Frameless stereotactic-directed tissue sampling during surgery of suspected low-grade gliomas to avoid histological undergrading. Minim Invasive Neurosurg. 1998;41:183–6. doi: 10.1055/s-2008-1052038. [DOI] [PubMed] [Google Scholar]
- 18.Savas A, Kanpolat Y. Safety and efficacy of frameless and frame-based intracranial biopsy techniques. Acta Neurochir (Wien) 2008;150:737. doi: 10.1007/s00701-008-1612-z. [DOI] [PubMed] [Google Scholar]
- 19.Warnick RE, Longmore LM, Paul CA, Bode LA. Postoperative management of patients after stereotactic biopsy: Results of a survey of the AANS/CNS section on tumors and a single institution study. J Neurooncol. 2003;62:289–96. doi: 10.1023/a:1023315206736. [DOI] [PubMed] [Google Scholar]
- 20.Woodworth GF, McGirt MJ, Samdani A, Garonzik I, Olivi A, Weingart JD. Frameless image-guided stereotactic brain biopsy procedure: Diagnostic yield, surgical morbidity, and comparison with the frame-based technique. J Neurosurg. 2006;104:233–7. doi: 10.3171/jns.2006.104.2.233. [DOI] [PubMed] [Google Scholar]
- 21.Zoeller GK, Benveniste RJ, Landy H, Morcos JJ, Jagid J. Outcomes and management strategies after nondiagnostic stereotactic biopsies of brain lesions. Stereotact Funct Neurosurg. 2009;87:174–81. doi: 10.1159/000222661. [DOI] [PubMed] [Google Scholar]


