Abstract
Oral focal mucinosis (OFM), an oral counterpart of cutaneous focal mucinosis, is a rare disease of unknown etiology. Its pathogenesis may be due to the overproduction of hyaluronic acid by a fibroblast, at the expense of collagen production, resulting in focal myxoid degeneration of the connective tissue, primarily affecting the mucosa overlying the bone. It has no distinctive clinical features, as the diagnosis is solely based on the histopathological features. This article reports of a 32-year-old female having the rare disease of oral focal mucinosis, involving the posterior palatal mucosa, and discusses its clinicopathological features and differential diagnosis of myxomatous lesions of the oral cavity.
Keywords: Cutaneous focal mucinosis, focal myxoid degeneration, hyaluronic acid, myxomatous lesion, oral focal mucinosis
Introduction
Oral Focal Mucinosis (OFM) is an uncommon clinicopathological condition that is considered to be the oral counterpart of cutaneous focal mucinosis (CFM). It is a disease of unknown etiology, possibly resulting from the overproduction of hyaluronic acid by fibroblasts.[1] Clinically the lesion appears as asymptomatic round elevations, which are histologically characterized by a localized area of myxomatous connective tissue, containing mucinous material, surrounded by relatively dense collagenous connective tissue.[2]
It was first described and named by Tomich in 1974. He reported eight cases as oral counterparts of cutaneous focal mucinosis. However, similar lesions were also previously described, in 1966, by Jhonson and Helwig, as solitary, asymptomatic, dome-shaped skin nodules seen usually on the face, trunk, and extremities.[2,3] A review of the literature revealed that since the original article by Tomich, 57 cases of oral focal mucinosis were reported in English literature,[2,4–13] while only three cases has been reported in Indian literature[14] including the present case. [Table 1].
Table 1.
Published reports of oral focal mucinosis
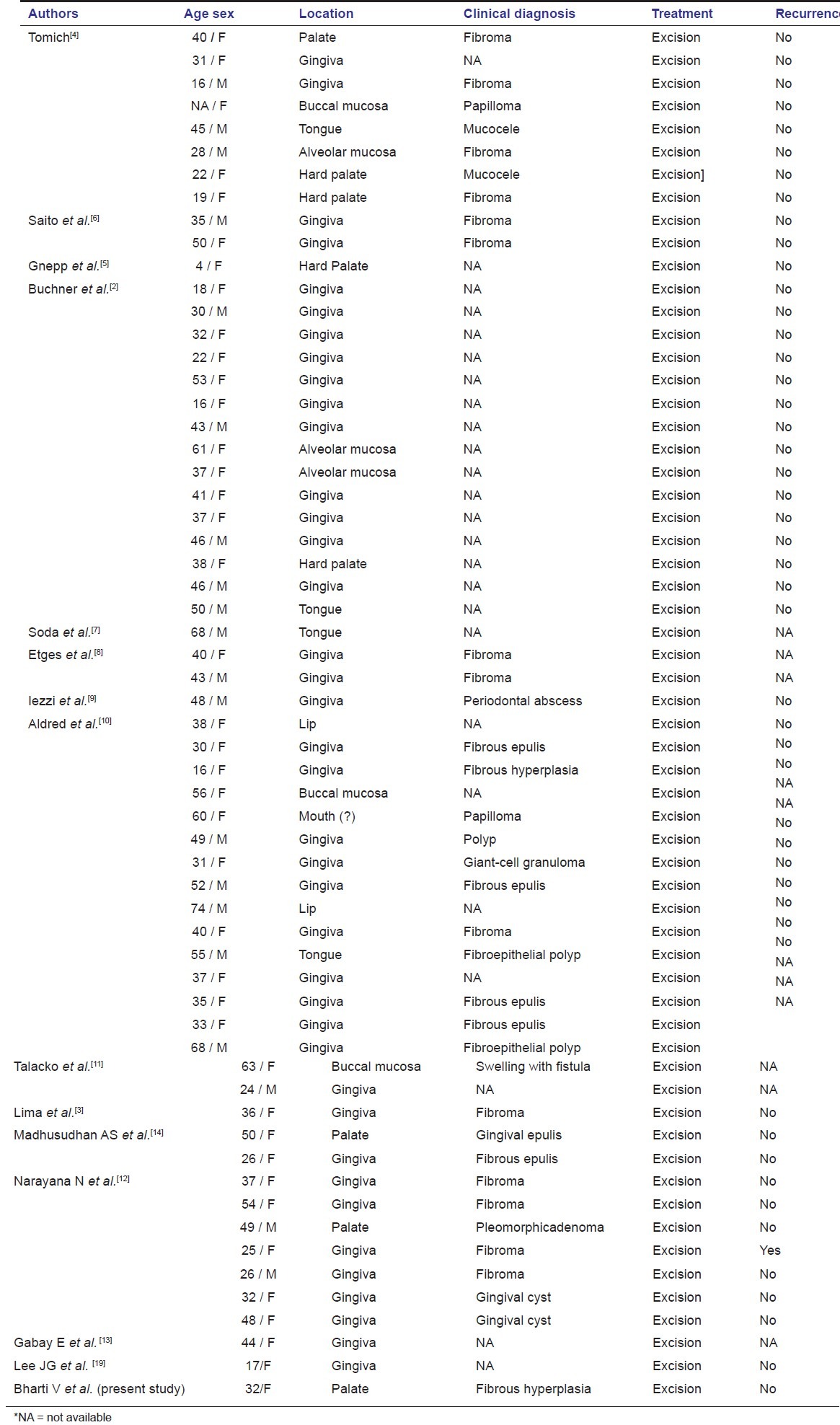
The mucosa directly overlying the bone appears to be particularly vulnerable, with the gingiva being the most common site, followed by the hard palate. Despite being the second most common site, the lesions of the hard palate are rare, with only seven cases being reported to date. The lesions are generally the same color as the surrounding normal mucosa, and skin lesions do not seem to accompany the oral lesions. The lesions are difficult to diagnose clinically, as there are no clinical distinctive features. A review of the available literature shows that it is most commonly diagnosed as gingival hyperplasia; fibroma ,or epulis.[3] Thus, the histopathological diagnosis becomes important in these conditions.
Case Report
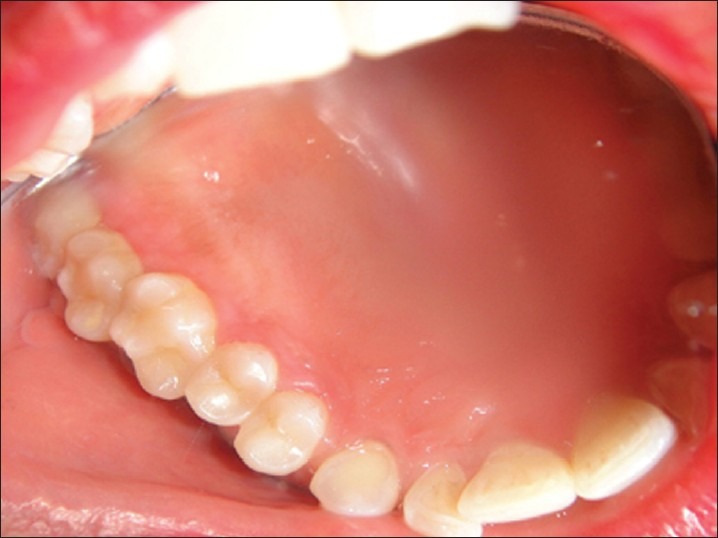
A female patient aged 32 years, reported to the Department of Periodontology, Government Dental College and Hospital, Patiala, with a chief complaint of a swelling on her right posterior palatal mucosa, since four to five months [Figure 1]. The growth had increased in size since three months, but it showed no significant increase in size since one month. The medical history was non-contributory. An intraoral examination revealed a pinkish red, painless, sessile, firm, tender mass, measuring 1.5 cm at its greatest dimension. The lesion had extended from the distal aspect of 16 to the mesial aspect of 18. No surface ulceration or secondary infection was noted and the oral hygiene of the patient was reasonably good. The first clinical impression at examination was that of fibrous hyperplasia.
Figure 1.

Clinical aspect of oral focal mucinosis involving the right maxillary second and third molar area
Investigations
The laboratory investigations for blood were within normal limits. The intraoral periapical radiographic examination revealed no evidence of crestal bone loss, and the lamina dura was intact around the roots of both the maxillary second and third molar regions.
Management
After one week of thorough scaling and root planing, the growth was surgically excised involving the second and third molar area and a thorough curettage of the area was performed under local anesthesia. The excised lesion was transported in 10% formalin to the laboratory for histopathological examination. Sutures and periodontal dressing were placed on the operated area [Figure 2]. After one week the sutures and dressing were removed.
Figure 2.

Immediate operative view following periodontal surgery
Histopathological findings
The hematoxylin and eosin-stained microscopic slide revealed a loose, myxomatous connective tissue stroma, with ovoid, fusiform or stellate-shaped fibroblasts. Fibroblasts represent delicate fibrillar processes extending from the cytoplasm into the surrounding matrix. A scarcity of inflammatory cells and reticulin fibers was observed. These histopathological features were suggestive of Oral Focal Mucinosis (OFM) [Figure 3].
Figure 3.
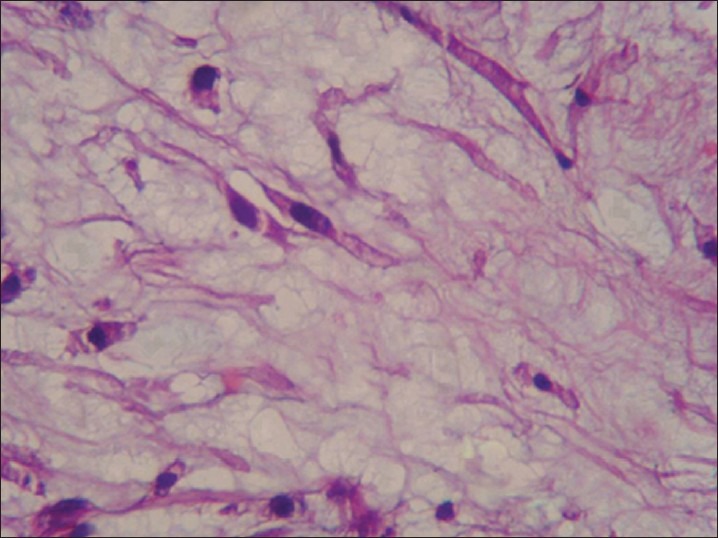
Shows loose myxomatous connective tissue stroma with fusiform or stellate-shaped fibroblasts. ×400 (H and E)
Clinical course
The patient has been observed on a regular basis; no recurrence was observed at the one-year follow-up [Figure 4].
Figure 4.
Shows no sign of recurrence at the one-year follow-up
Discussion
Oral focal mucinosis is a rare disease of unknown etiology where the connective tissue undergoes focal myxoid degeneration, first described by Tomich, in 1974.[4] It is the oral counterpart of cutaneous focal mucinosis and the cutaneous myxoid cyst. Cutaneous focal mucinosis seems to be a mesenchymally derived lesion, composed predominantly of fibroblasts.[15] Oral focal mucinosis may be the result of the overproduction of hyaluronic acid by fibroblasts at the expense of collagen production.[2,4,5–7] There is a predilection for the mucosa of the overlying bone, and keratinized mucosa is involved almost exclusively, with 80% of the lesions developing on the gingiva and the remainder on the palate;[4] other locations are the alveolar mucosa and tongue.[6]
From a clinical point of view, the differential diagnosis must be made with inflammatory lesions (i.e., fibrous hyperplasia, peripheral giant cell granuloma, epulis fissuratum, pyogenic granuloma) and tumors (i.e., peripheral fibroma and peripheral ossifying fibroma).[16] Also, other lesions such as primary benign (i.e., peripheral ameloblastoma and peripheral odontogenic fibroma), malignant, or metastatic lesions may appear as a gingival mass. Finally, a number of non-plaque–related lesions (irritation fibroma, fibrous hyperplasia) must be included in the differential diagnosis.[16] A review of all reported cases show that they were never diagnosed clinically as oral focal mucinosis.[16] The histological features are always the basis for diagnosis.
The histological differential diagnosis of oral focal mucinosis includes, inflammatory fibroepithelial hyperplasia, mucocele, nerve sheath myxoma, and myxoma.[5,6,8] Similar myxoid areas may be found in inflammatory fibroepithelial hyperplasia, but unlike oral focal mucinosis, these are accompanied by inflammation and fibrosis elsewhere. Unlike oral focal mucinosis, extravasation mucoceles (that result from minor trauma of the lips) have an associated inflammatory cell infiltrate and a granulation tissue wall. Nerve sheath myxoma is characterized by a whorled arrangement of tumor cells in an organoid, multinodular, or lobular structure.[17] The myxoma is a true neoplasm resembling embryonal mesenchyme, consisting of widely separated stellate and sometimes spindle-shaped cells in a loose mucoid stroma, with a network of delicate reticular fibers.[17] Myxoma may present as an infiltrative growth pattern, while focal mucinosis usually manifests as a localized area of myxomatous connective tissue.[4] Small pools of mucinous material are a feature in many cases of focal mucinosis, but are not present in myxomas.[18]
Conclusion
It must be emphasized that in many of the focal gingival lesions, a preoperative diagnosis is almost impossible, due to their rarity. The histological evaluation is always the basis for diagnosis. Oral focal mucinosis is an uncommon condition that occurs predominantly in females and in adults. The gingiva is the most common site of its occurrence, followed by the hard palate. Despite being the second most common site, the lesions of the palatal mucosa are rare, with only seven cases being reported to date. Oral focal mucinosis rarely occurs upon surgical excision of the lesion.[19]
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
References
- 1.Neville BW, Damm DD, Allen CM, Bouquot JE. Oral and maxillofacial pathology. 2nd ed. Philadelphia, Pennsylvania: Elsevier; 2002. pp. 446–7. [Google Scholar]
- 2.Buchner A, Merrell PW, Leider AS, Hansen LS. Oral focal mucinosis. Int J Oral Maxillofac Surg. 1990;19:337–40. doi: 10.1016/s0901-5027(05)80076-1. [DOI] [PubMed] [Google Scholar]
- 3.Soares de Lima AA, Naval Machado MA, Martins WD, Trindade Grégio AM, Dirschnabel AJ, Folador Mattioli TM, et al. Oral focal mucinosis. Quintessence Int. 2008;39:611–5. [PubMed] [Google Scholar]
- 4.Tomich CE. Oral focal mucinosis. A clinicopathologic and histochemical study of eight cases. Oral Surg Oral Med Oral Pathol. 1974;38:714–24. doi: 10.1016/0030-4220(74)90392-2. [DOI] [PubMed] [Google Scholar]
- 5.Gnepp DR, Vogler C, Sotelo-Avila C, Kielmovitch IH. Focal mucinosis of the upper aerodigestive tract in children. Hum Pathol. 1990;21:856–8. doi: 10.1016/0046-8177(90)90056-b. [DOI] [PubMed] [Google Scholar]
- 6.Saito I, Ide F, Enomoto T, Kudo I. Oral focal mucinosis. J Oral Maxillofac Surg. 1985;43:372–4. doi: 10.1016/0278-2391(85)90259-9. [DOI] [PubMed] [Google Scholar]
- 7.Soda G, Baiocchini A, Bosco D, Nardoni S, Melis M. Oral focal mucinosis of the tongue. Pathol Oncol Res. 1998;4:304–7. doi: 10.1007/BF02905222. [DOI] [PubMed] [Google Scholar]
- 8.Etges A. Oral focal mucinosis: clinical, histopathological and histochemical study. RGP Rev Pos Grad. [Internet] 2007;7:140–4. Available from: www.LILACS.com . [Google Scholar]
- 9.Iezzi G, Rubini C, Fioroni M, Piatelli A. Oral focal mucinosis of the gingiva: Case report. J Periodontol. 2001;72:1100–2. doi: 10.1902/jop.2001.72.8.1100. [DOI] [PubMed] [Google Scholar]
- 10.Aldred MJ, Talacko AA, Ruljancich K, Story RD, Newland S, Chen ST, et al. Oral focal mucinosis: Report of 15 cases and review of the literature. Pathology. 2003;35:393–6. doi: 10.1080/00313020310001602639. [DOI] [PubMed] [Google Scholar]
- 11.Talacko AA, Lacy MF, Besly W, Aldred MJ. Oral focal mucinosis: Report of two cases with ulceration. Pathology. 2004;36:582–3. doi: 10.1080/00313020400011235. [DOI] [PubMed] [Google Scholar]
- 12.Narayana N, Casey J. Oral focal mucinosis: Review of the literature and seven additional cases. Gen Dent. 2009;57:e11–3. [PubMed] [Google Scholar]
- 13.Gabay E, Akrish S, Sharon A, Machtei EE. Oral focal mucinosis associated with cervical external root resorption: A case report. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2010;110:75–8. doi: 10.1016/j.tripleo.2010.04.002. [DOI] [PubMed] [Google Scholar]
- 14.Madhusudhan AS, Nagarajappa Das, Manjunatha BS, Swati S, Charan Babu HS. Oral focal mucinosis: Report of two cases. Rev Odonto Ciênc. 2010;25:310–3. [Google Scholar]
- 15.Wilk M, Schmoeckel C. Cutaneous focal mucinosis: A histopathological and immunohistochemical analysis of 11 cases. J Cutan Pathol. 1994;21:446–52. doi: 10.1111/j.1600-0560.1994.tb00287.x. [DOI] [PubMed] [Google Scholar]
- 16.Manor Y, Merdinger O, Katz J, Taicher S. Unusual peripheral odontogenic tumors in the differential diagnosis of gingival swelling. J Clin Periodontol. 1999;26:806–9. doi: 10.1111/j.1600-051x.1999.tb02524.x. [DOI] [PubMed] [Google Scholar]
- 17.Enzinger FM, Weiss SW. Soft tissue tumours. 2nd ed. St Louis: Mosby; 1988. p. 769. [Google Scholar]
- 18.Johnson WC, Graham JH, Helwig EB. Cutaneous myxoid cyst: A clinicopathological and histochemical study. JAMA. 1965;191:15–20. doi: 10.1001/jama.1965.03080010021004. [DOI] [PubMed] [Google Scholar]
- 19.Lee JG, Allen G, Moore L, Gue S. Oral focal mucinosis in an adolescent: A case report. Aust Dent J. 2012;57:90–2. doi: 10.1111/j.1834-7819.2011.01649.x. [DOI] [PubMed] [Google Scholar]


