Abstract
Introduction
Previous reviews have demonstrated that patient outcomes following orthopaedic surgery are strongly influenced by the presence of Workers’ Compensation. However, the variability in the reviews’ methodology may have inflated the estimated strength of this association. The main objective of this meta-analysis is to evaluate the influence of Workers’ Compensation on the outcomes of orthopaedic surgical procedures.
Methods
We conducted a systematic search of the literature published in this area from 1992–2012, with no language restrictions. The following databases were used MEDLINE (Ovid), Embase (Ovid), CINAHL, Google Scholar, LILACS and Pubmed. We also hand-searched the reference sections of all selected papers. We included all prospective studies evaluating the effect of compensation status on outcomes in adult patients who had undergone surgery due to orthopaedic conditions or diseases. Outcomes of interest included disease specific, region specific and/or overall quality of life scales/questionnaires and surgeons’ personal judgment of the results. We used an assessment tool to appraise the quality of all included studies. We used Review Manager to create forest plots to summarize study data and funnel plots for the assessment of publication bias.
Results
Twenty studies met our eligibility criteria. The overall risk ratio for experiencing an unsatisfactory result after orthopaedic surgery for patients with compensation compared to non-compensated patients is 2.08 (95% CI 1.54–2.82). A similar association was shown for continuous data extracted from the studies using assessment scales or questionnaires (Standard Mean Difference = −0.70 95% CI -0.97- −0.43).
Conclusions
Among patients who undergo orthopaedic surgical procedures, those receiving Workers’ Compensation experience a two-fold greater risk of a negative outcome. Our findings show a considerably lower estimate of risk compared to previous reviews that include retrospective data. Further research is warranted to determine the etiological explanation for the influence of compensation status on patient outcomes.
Systematic Review Registration Number
CRD42012002121
Introduction
The success of a surgical intervention in orthopaedic medicine is influenced by several factors including the appropriateness of the surgical indication and the surgeon’s skill level and experience with the specific procedure. A patient’s compensation status may also influence how a patient fares following orthopaedic surgery. In clinical practice, orthopaedic surgeons often treat patients who are receiving Workers’ Compensation benefits for their injuries and/or conditions [1]–[4]. Several studies demonstrate that receiving Workers’ Compensation may correlate to a negative prognosis following treatment for a vast range of health conditions [5]–[11]. It is important to understand this phenomenon and to encourage orthopaedic surgeons to consider patients’ compensation status when assessing their expected outcomes[12]–[14].
Surgeons should utilize the best available studies as a guide when attempting to assess the influence of compensation status on patients’ outcomes following orthopaedic surgery. Despite the well-established merit of randomized controlled trials in evidence-based medicine, incorporating randomization and blinding into a study’s design is wrought with challenges and often is not feasible or ethical in the field of orthopaedic surgery[15]–[17]. Therefore, the results from high-quality observational studies are often the best source of evidence to be considered in clinical decision-making within orthopaedic medicine[16]–[19]. This recognition that observational studies have a critical place within evidence-based medicine is supported extensively in the literature [16], [17], [20], [21].
The influence that compensation status has on the prognosis of patients undergoing surgical treatment for musculoskeletal disorders has been investigated by a number of clinical studies [2], [7], [22], [23] and systematic or meta-analytic reviews[24]–[27]. However, there are methodological flaws in the design of many of these studies which diminishes the confidence one may have in their findings. For example, two of the systematic reviews [24], [27] considered only disease-specific studies and were therefore limited to a very small number of studies. This approach leads to results that lack generalizability across patient populations. Another review on this topic featured a very broad eligibility criteria and included retrospective studies as well as studies that were conducted in the 1960s. We feel that this may had lead to an imprecise magnitude of the present-day relationship between compensation status and patient outcomes as the working world has undergone substantial changes in the past several decades. One study reported a 4.72 odds ratio, showing that patient outcomes are negatively influenced by Worker’s compensation [26]. From our experience in clinical practice, this finding seems somewhat unrealistic and serves as an illustrative example of the possible inflated estimates from existing clinical studies and systematic and meta-analytic reviews.
As such, no best-evidence approach is currently available in the literature to effectively demonstrate the magnitude of the influence of the compensation status on patient outcomes following orthopaedic surgery. We feel this is valuable information for practicing surgeons who encounters this type of patient population in their practice. We conducted a systematic review and meta-analysis to resolve this issue and to obtain evidence with a greater confidence and power due to the synthesis of the results of primary studies [28], [29].
The objective of this systematic review and meta-analysis is threefold, to assess: 1) the general influence of compensation status on patient outcomes through inclusion of only high quality prospective studies focusing on adult patients who undergo surgery for a variety of musculoskeletal orthopaedic conditions (both traumatic and non-traumatic); 2) if this relationship varies between traumatic and non-traumatic injuries; and 3) if outcomes vary for well-known Workers' Compensation surgical populations: upper extremity non-traumatic surgery (e.g. rotator cuff tears and nerve compression syndromes) and spine surgery (primarily degenerative disk diseases).
Materials and Methods
This meta-analysis follows the PRISMA Statement [30] reporting recommendations. This review’s protocol can be found in the PROSPERO database (http://www.crd.york.ac.uk/prospero/) under the registration number CRD42012002121.
Search Strategy
A literature search was conducted with the assistance of a third investigator not related to the study. We utilized the following databases: MEDLINE (Ovid), Embase (Ovid), CINAHL, Google Scholar, LILACS and the Cochrane Library. Following this initial review, we hand-search the references sections of papers we had included at this stage in order to locate additional studies and to avoid missing relevant papers. We did not exclude any studies on the basis of language. We included papers published between 1992 and 2012 (May, 02). Our search strategy is shown in Appendix S1.
Eligibility Criteria
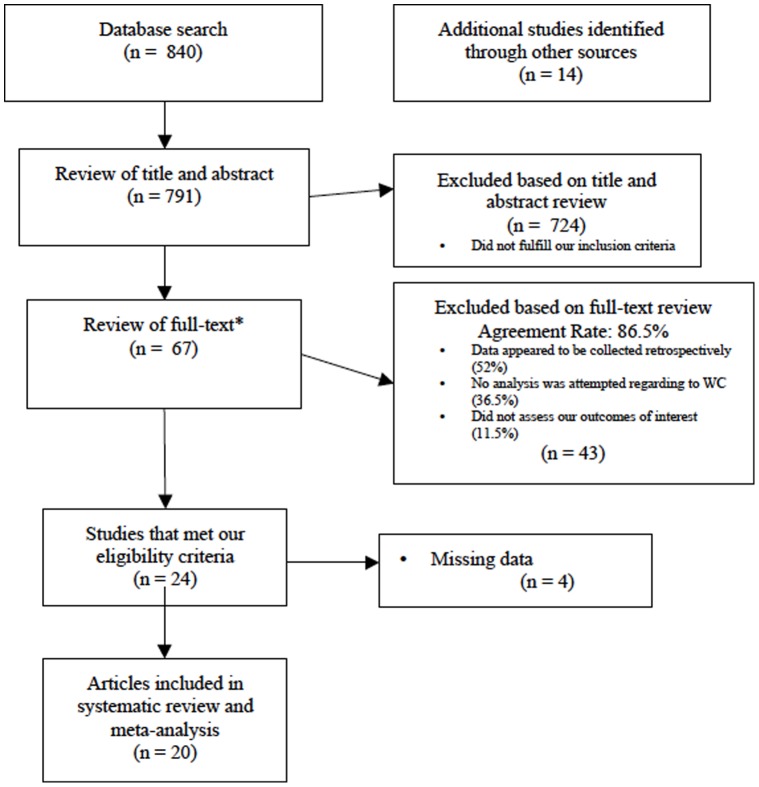
Studies were included if they met the following criteria: 1) The data was collected and analyzed prospectively; 2) The authors assessed the influence of compensation status specifically; 3) Orthopaedic surgery was the main intervention; and 4) The study was published in the last 20 years, between 1992 and 2012. Also, to be included, the study had to report at least one of the following outcomes: region or disease-specific scales or questionnaires (e.g. the Disabilities of the Arm, Shoulder and Hand measure [32] or Oswestry Disability Index [33]); quality of life assessment scales (e.g. the SF-36); pain assessment scales (e.g. through use of a Visual Analogical Scale), study-specific developed grading criteria for assessing the outcomes. We excluded studies that met any of the following criteria: 1) The study involved non-surgical treatments; 2) Patient data was collected retrospectively; and 3) The study did not report any of the outcomes of interest, as described above. We included studies after a 2-stage assessment, as depicted in the study flow chart ( Figure 1 ). Disagreement regarding which studies should be included were resolved by group discussion (VY, KG). We foresaw a third part consultation (JB, MB) if consensus was not reached.
Figure 1. Flow Chart of Study Process.
This figure demonstrates the various stages of our systematic review and depicts the reasons why certain papers were excluded.
Data Management: Collection and Extraction
Both qualitative and quantitative data were extracted following full text analysis of the included studies. We also extracted additional information on the studies’ design, funding, population under investigation, intervention, control (if applicable), outcome, duration of follow-up, criteria for Workers’ Compensation identification and the population’s working demands. We also grouped included studies by the condition that was treated in the patient population as follows: 1) Non-traumatic spine surgery (e.g. disc diseases and fusion surgery); 2) Upper limb surgery (e.g. rotator cuff tear repairs, carpal tunnel release surgery); and 3) Fractures. We also grouped studies based on the patients’ cause of injury or condition (traumatic versus non-traumatic). If authors included populations from both traumatic and non-traumatic cases, we decided to group the study based on the authors’ most reported case. We grouped the studies in these ways in order to perform valuable subgroup analyses.
We collected both continuous and dichotomous data from the included studies and analyses were performed in individual forest plots. Many of studies reported several outcomes using different scales and measures for assessment of their patient population. Whenever possible, we focused on one dichotomous and one continuous outcome per study. In the event that a study reported more than one dichotomous or continuous outcome, we extracted data preferentially based on the type of measure. We extracted data based on the following order: 1) Authors’ categorizations of outcomes, based on region or disease-specific tools (e.g. patient scores <80 = unsatisfactory outcome; >80 = satisfactory outcome); 2) Authors’ judgment of the outcome, based on quality of life scales or questionnaires; 3) Authors’ judgment of the outcome, based on pain measurements; 4) Authors’ judgment of the outcome, based in his/her subjective clinical appraisal. We categorized data from poor, fair or unsatisfactory groups as unsatisfactory outcomes. Dichotomous data from items 1 to 4 were collected as the number of unsatisfactory results from Workers’ Compensation patients versus patients receiving no compensation. When the results were reported in a non-categorized manner, we obtained scores from studies that reported continuous outcomes and then plotted them in a meta-analysis. We did not categorize the patients’ outcomes based on our personal judgments, since we believed this may introduce bias.
Continuous data was collected from reported means, standard deviations, and the number of patients in each group. When study data was missing and/or unclear in the published paper, we attempted to contact the authors by email to clarify or provide us with additional data from their study. After it was entered, all data was verified by two authors (VY, JB).
Study Quality Assessment
Two authors (VY, KG) assessed the quality of all included studies by a tool developed specifically to appraise the risk of bias within observational studies [34]. This tool contains objective questions that appraise the risk of bias in eight areas: selection bias, confidence in the assessment of the exposure, confidence in the recognition of the outcome, matching or statistical adjustments for comparisons, confidence in the assessment of the outcome, confidence in the assessment of the presence or absence of prognostic factors, adequateness of the follow-up period and similarities between co-interventions. All the eight aspects were graded in a four-category scale from the highest to the lowest risk of bias. The tool can be seen in Appendix S2.
Statistical Analysis
A priori, we decided to analyze data according to the following groups: 1) A comprehensive analysis, with the inclusion of all studies; 2) A subgroup analysis of traumatic versus non-traumatic conditions; and 3) Additional subgroup analyses for each of the following: spine, upper limb non-traumatic conditions and fractures. An overall and subgroup meta-analysis was performed for all subgroups if there were at least three studies available for pooling.
We utilized Review Manager [35] (version 5.1) to conduct the meta-analysis. Since we sought to investigate both dichotomous and continuous variables, we used two different approaches. All calculations for dichotomous data were performed using a random-effects model [36] and Mantel-Haenszel method. Continuous data was calculated using an inverse variance method and also in a random-effects model. We provided measures as risk ratios using a 95% confidence intervals. We demonstrated a sum of the risk or mean difference from the studies where this was possible. For dichotomous variables, comparisons between the subgroups were performed using a chi-square test, within Review Manager software.
Mean differences and 95% confidence intervals were also summarized in forest plots. Heterogeneity was assessed by I2 statistics. We analyzed publication bias by funnel plots.
Results
Of the 805 references screened by title and abstract, sixty-seven were selected for full text assessment. From these, 20 fulfilled the eligibility criteria and were included in the meta-analysis[37]–[56]. The included studies contain data from 2608 patients, all of whom underwent orthopaedic surgical procedures. Four studies [39], [47], [48], [50] provided continuous and dichotomous data and were included in dichotomous and continuous data pooling. Figure 1 provides a pictorial representation of the stages of the review process.
The majority of the studies (14/20, 70%) included in our review were conducted in the United States[37]–[39], [41], [43], [44], [46], [48], [49], [51]–[56], and almost three-quarters of the studies report the results of surgical outcomes for one of three important Workers’ Compensation populations: lumbar spine injuries [38], [39], [43], [45], [49], rotator cuff diseases [40], [46], [47], [50], [52], [54] and carpal or ulnar tunnel syndrome [44], [51], [55]. The characteristics of included studies are detailed in Table 1 .
Table 1. Characteristics of Included Studies.
| Characteristic | N (%) |
| Origin of Study | |
| United States | 14 (70) |
| Canada | 4 (20) |
| Europe | 2 (10) |
| Study Design | |
| Prospective case series | 16 (80) |
| Randomized controlled trials | 4 (20) |
| Study Designed to Assess Influence of CompensationStatus | |
| Yes | 5 (25) |
| Surgical Intervention | |
| Lumbar spine discectomy, with or without fusion | 5 (25) |
| Rotator cuff repair, with or without acromioplasty | 6 (30) |
| Carpal or cubital tunnel release | 3 (15) |
| Knee reconstruction | 2 (10) |
| Other | 4 (20) |
| Number of Surgeons | |
| 1 | 3 (15) |
| 2 | 9 (25) |
| >2 | 8(40) |
| Mean Follow-up | |
| <6 months | 0 (0) |
| 6–24 months | 10 (50) |
| >24 months | 10 (50) |
| Method of Outcome Assessment | |
| Region or disease-specific or quality of lifeinstrument/scale | 12 (60) |
| Pain instrument/scale | 4 (20) |
| Patient self-reported satisfaction | 2 (10) |
| Surgeon’s subjective appraisal | 2 (10) |
| Gender * | Mean (Range) |
| % male patients | 58 (35–83) |
| % of Patients Lost to Follow-up** | 13.9(0–28.7) |
| # of Patients* | 129.3(16–539) |
| Mean Age of Participants*** | 28–56 (Range) |
Data available from 16 studies.
Data available from 10 studies.
Data available from 15 studies.
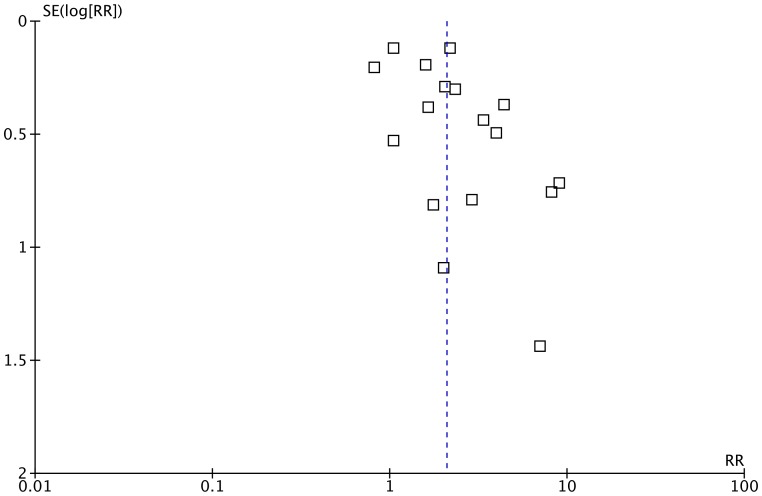
Following an assessment of the studies’ quality, six (30%) of the twenty studies were considered to be of low quality [43], [44], [48], [49], [51], [55]. Table 2 and 3 displays the findings from the study quality appraisal. Assessment of the funnel plot demonstrates that publication bias was unlikely a considerable factor ( Figure 2 ).
Table 2. Quality Assessment.
| Study/Quality Scale | Q1 | Q2 | Q3 | Q4 | Q5 | Q6 | Q7 | Q8 | Overall Rating |
| Antoniou, 2000 | I | I | II | II | II | II | II | I | *** |
| Asch, 2002 | II | II | II | III | II | II | I | III | ** |
| Atlas, 2009 | III | II | II | II | II | II | II | III | ** |
| Balyk, 2008 | II | II | I | II | II | I | III | II | *** |
| Barrett, 2001 | II | II | II | III | III | II | II | I | ** |
| Buckley, 2002 | III | II | II | III | III | II | II | II | ** |
| Deustsch, 2006 | II | II | II | IIII | III | III | III | III | * |
| Glowacki, 1997 | III | II | II | IIII | III | IIII | III | II | * |
| Greenough, 1994 | II | II | II | III | II | III | II | II | ** |
| Henn III, 2008 | III | II | II | I | I | II | II | II | *** |
| Johannsen, 1997 | II | II | II | II | III | II | II | II | ** |
| Lin, 2000 | II | II | II | III | III | III | II | II | * |
| MacKay, 1995 | II | II | II | III | III | IIII | III | III | * |
| McKee, 2000 | II | II | II | II | III | II | III | II | ** |
| Nagle, 1994 | II | II | II | III | IIII | III | III | II | * |
| Nicholson, 2003 | II | II | II | II | II | II | II | I | *** |
| Rosenberger, 2008 | I | II | II | III | II | II | II | I | *** |
| Spangehl, 2002 | I | II | II | II | II | I | III | II | *** |
| Straub, 1999 | III | II | II | IIII | III | III | II | IIII | * |
| Westkaemper, 1998 | II | II | I | IIII | II | II | II | II | ** |
Table 3. Quality Assessment Ratings.
| Scores | Ratings |
| I | Very Low Risk of Bias |
| II | Low Risk of Bias |
| III | High Risk of bias |
| IIII | Very High Risk of Bias |
| * | Low Quality |
| ** | Moderate Quality |
| *** | High Quality |
Figure 2. Funnel Plot for Publication Bias.
This funnel plot was used to assess whether publication bias was potentially present in our meta-analysis.
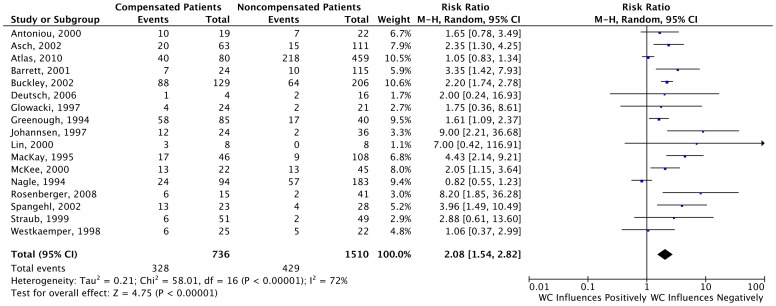
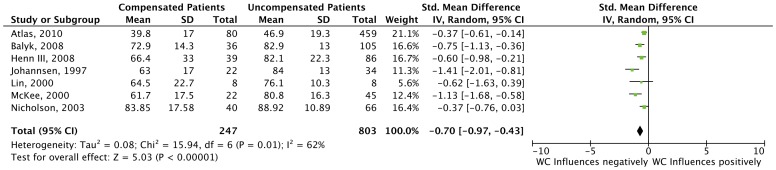
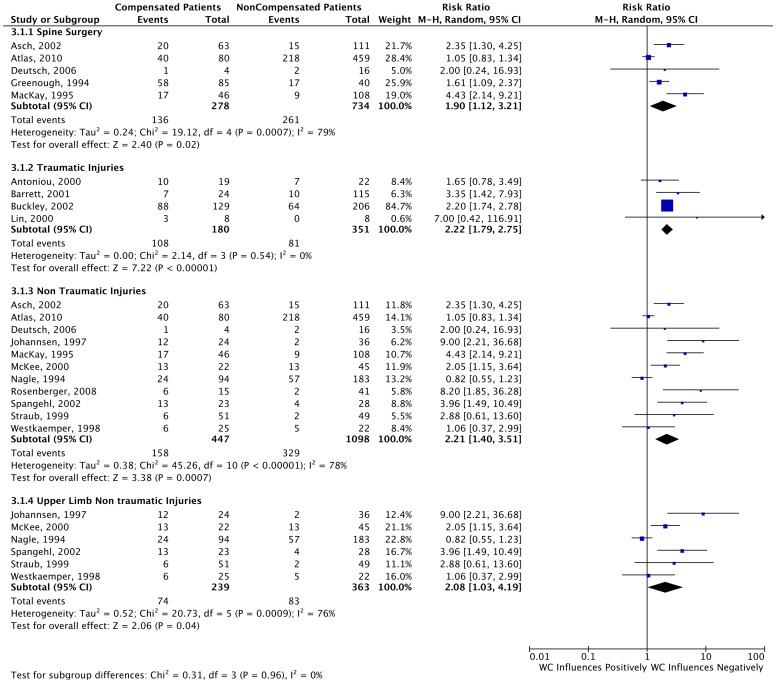
In the overall analysis of all studies reporting dichotomous outcomes (n = 17), our results demonstrated that Workers’ Compensation patients have worse outcomes when compared to non-compensated patients (RR = 2.08, 95% CI 1.54–2.82), as shown in Figure 3 . The overall comparison of the seven studies that reported only continuous data from the scales or questionnaires showed the same trend, (Standard Mean Difference = −0.70 95% CI -0.97- −0.43). The results of this are shown in Figure 4 .
Figure 3. Forest Plots for Studies Reporting Dichotomous Data.
This forest plot depicts the results of the 17 studies that reported dichotomous data.
Figure 4. Forest Plots for Studies Reporting Continuous Data.
This forest plot depicts the results of the 7 studies that reported continuous data.
We further examined if the relationship between compensation status and outcome varied depending on the condition/disease being treated. The results of our subgroup analyses are as follows: 1) lumbar spine injuries, five studies (RR = 1.90 95% CI 1.12–3.21); 2) upper limb injuries, six studies (RR = 2.08 95% CI 1.03–4.19); 3) traumatic injuries [37], [41], [42], [48], four studies (RR = 2.22 95% CI 1.79–2.75); and 4) non-traumatic injuries[38]–[40], [43]–[47], [49]–[56], eleven studies (RR = 2.21 95% CI 1.40–3.51). We found no differences between these subgroups (p = 0.96). These subgroup analyses are depicted in Figure 5 .
Figure 5. Forest Plots for Studies Reporting Dichotomous Data.
This forest plot depicts the results of the subgroups that we decided to analyze a priori.
We also performed further explorative analyses that were not initially set in our protocol. The additional subgroups were 1) grouped by studies’ country of origin; 2) studies that specially assessed Workers’ Compensation; and 3) only high-quality studies. Again, the results from these analyses reflected the same findings as seen in our overall comparison. We provide the sum of the risks from these studies in Table 4 .
Table 4. Additional Subgroup Analyses.
| Sugroup Analysis | RR (95% CI) |
| Country | |
| United States, 13 studies | 1.95 (1.28–2.97)* |
| Canada/Europe, 4 studies | 2.25 (1.61–3.14)* |
| Study Design | |
| High Quality, 3 studies | 3.22 (1.32–7.85)* |
| Study Designed To Assess the Influence of Compensation | |
| Dichotomous Data, 2 studies | 1.74 (0.56–5.38) |
| Continuous Data, 4 studies | −8.05 (−11.08−5.03)* |
Demonstrates the negative influence of Workers’ Compensation.
Discussion
This systematic review and meta-analysis demonstrates the negative influence that the presence of Workers’ Compensation has on patient outcomes following orthopaedic and trauma surgery. This comprehensive, best-evidence focused meta-analysis also showed consistent internal validity, reflecting our well-developed methodology, since the results are consistent in both overall and subgroup analyses. Our results demonstrate, in a simplified manner, that when a surgery is performed on a compensated patient with is known to be receiving compensation, surgeons should expect a 2-fold higher chance of obtaining an unsatisfactory outcome, when compared with non-compensated patients. The summary of this effect may used as a reference and taken into consideration for surgical decisions.
Studies have demonstrated that outcomes following orthopaedic surgery may be associated with factors other than compensation status. These studies suggest that this phenomenon may be influenced by biopsychological variables [57], [58], expectations or uncertainty regarding recovery [57], and low pain threshold [59]. However, though these associations are not strong [46].
In our protocol [31], we predicted that certain subgroups (e.g. non-traumatic spine or upper limb injuries) would demonstrate a higher risk of unsatisfactory results after surgery compared to the group as a whole. These hypotheses stemmed from reports that show a high prevalence of Workers’ Compensation patients within these populations[1], [5], [38], [55], [60]–[65]. Our results show no significant difference between these groups and our results showed a clear overlap of the confidence intervals between the overall and subgroup analyses. Two relevant issues should be raised to this point: 1) some subgroups may be more prone to selection bias; 2) certain subgroups may comprise of more complex patients who’s outcomes may be affected by other factors (as discussed above); and 3) we have made comparisons between patient cohorts that have been assessed using different criteria. This is was likely a considerable factor in the heterogeneity among our studies.
An additional subgroup analysis was performed, comparing cohorts grouped by country of origin, only high quality studies (judged by the risk of bias assessment tool) and studies specifically designed for assessing Workers’ Compensation cohorts. Only two of our included studies were specifically designed for assessing Workers’ Compensation and analysis did not show any differences between compensated and non-compensated cohorts. Since we have pooled only two studies for this particular analysis, we feel that this is underpowered.
It is important to compare the methodology of this systematic review with that of existing reviews in this area. In their review, Harris and colleagues [26] included all English studies in the existing literature relating to Workers’ Compensation and surgery outcomes. They included studies with both retrospective and prospective designs and did not seek to contact authors when additional data was needed from individual studies. Our approach differed in many aspects. For one, we only included prospective studies and studies that were published in the last 20 years. Secondly, we accounted for the quality of the included studies through use of an established tool. Thirdly, we performed several different subgroup analyses and lastly, we made attempts to contact the authors for missing data. We feel that by including non-prospective and older studies we would yield a biased magnitude of the risk, since these reports are related to a different employer-employee relation and retrospective designs may be prone to selection and measurement biases. Despite these methodological differences, our findings were similar. Harris reported an overall odds ratio of 3.79, (95% CI 3.28–4.37). Our results in the overall analysis can be converted to an odds ratio of 3.12 (95% CI 1.97–4.93). Despite of these overlapping confidence intervals, we feel that the results of Harris’ review maybe somewhat overestimated due to reporting bias.
The findings of this review have clear, direct implications on practice. The most explicit is the overall risk that is robust and homogeneous between the included subgroups. We also feel that the cohorts included in this systematic review are representative of the typical population of adults preparing for orthopaedic surgical intervention, which contributes to its high external validity. Also, because we specifically identified a subgroup of studies that focus on patient populations that are known to have a high prevalence of Workers’ Compensation cases, we can make the assumption that no subgroup of patients is more likely to be compensated in clinical practice. There is a less obvious message one can also gather from our review: the literature consistently demonstrated that compensated patients improve after surgical procedure, even if this improvement is delayed. Instead of avoiding surgical procedures for these populations, we recommend that surgeons take a patient-centred approach by balancing surgical indications and procedures with their own and the patient’ expectations.
From a practical perspective, we might state that our findings demonstrate with great external validity- that the surgical outcomes of Workers’ Compensation patients following orthopaedic surgery are somewhat worse than of similar patients who are not receiving compensation for their injuries. However, there is a notable lack of well-designed studies that explore the root causes of this clear association. This is an important consideration, given the current shift within surgery from a surgeon-centred responsibility to a circumstance-centred situation. A possible solution to this is to involve a multi-professional team in the management of Workers’ Compensation patients seeking care for their orthopaedic injuries. We also recommend that in addition to the standard medical history, physicians actively seek information to develop a comprehensive patient profile. Identifying potentially relevant social, economic, employment-related, and psychological issues may assist in establishing the prognosis following surgery and can aid in the decision-making process in practice regarding the patient’s treatment options.
We feel that we strengthened our review through inclusion of the rigorous quality assessment of the included studies. Our approach also recognized that no studies have previously reported sample size calculations for measuring this magnitude of the effect and as a way for establishing this cohort as representative of the population of interest. One possible sources of bias within our view is the fact that in most studies, the authors did not provide explicit criteria for what constitutes as a “Workers’ Compensation” patient. However, we feel confident in the definition of these patients, because there is little subjectivity in the assessment of how a patient is compensated.
A minor limitation that we encountered when conducting review was related to data abstraction. At times, the best available data may have been missed due to the inaccurateness of reporting and barriers to gathering data from the authors. Our experience showed that at least 70% of the unreported data was unavailable from the authors upon request. In this study, we experienced a 30% response rate after requesting unpublished data from authors, however only 1 of the 6 authors who responded was able to provide the data we requested.
This methodology and results of this study are quite comprehensive, robust and reproducible. Heterogeneity and publication bias may be a concern, but is inevitable when summarizing data from studies with different populations, measurements tools, and criteria. This is a recognized difficulty within orthopaedic research.
In future studies, comparisons between groups should be performed utilizing matched controls and should include statistical modifications to control group disparities, if any are present. In an ideal situation, matching should be introduced, which would eliminate the need for statistical adjustment. Another relevant factor that could be further explored is the standardizing surgical procedures and co-interventions (e.g. rehabilitation). Outcome assessors should be blinded to the patients’ compensation status and the patients should all be follow up for a similar time period. We feel that none of the studies included in this systematic review have reached these high methodological standards and we recommend that further research be initiated to resolve this relevant clinical question.
Supporting Information
Search Strategy
(DOC)
Quality Assessment Tool
(DOC)
Funding Statement
Dr. Bhandari is funded, in part, by a Canada Research Chair. Part of the funding for this study was provided by CAPES (Coordenadoria de Aperfeiçoamento de Pessoal de Nível Superior) - São Paulo, Brazil, Process number: 11/21611-2. No additional external funding received for this study. The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
References
- 1. Duncan SF, Calandruccio JH, Merritt MV, Crockarell JR, Kakinoki R (2010) A comparison of workers’ compensation patients and nonworkers’ compensation patients undergoing endoscopic carpal tunnel release. Hand Surg 15: 75–80. [DOI] [PubMed] [Google Scholar]
- 2. Day CS, Alexander M, Lal S, Horton H, Ahn CS, et al. (2010) Effects of workers’ compensation on the diagnosis and surgical treatment of patients with hand and wrist disorders. J Bone Joint Surg Am 92: 2294–2299. [DOI] [PubMed] [Google Scholar]
- 3.Balk ML, Hagberg WC, Buterbaugh GA, Imbriglia JE (2005) Outcome of surgery for lateral epicondylitis (tennis elbow): effect of worker’s compensation. Am J Orthop (Belle Mead NJ) 34: 122–126; discussion 126. [PubMed]
- 4. Saleh K, Nelson C, Kassim R, Yoon P, Haas S (2004) Total knee arthroplasty in patients on workers’ compensation: a matched cohort study with an average follow-up of 4.5 years. J Arthroplasty 19: 310–312. [DOI] [PubMed] [Google Scholar]
- 5. Anderson PA, Subach BR, Riew KD (2009) Predictors of outcome after anterior cervical discectomy and fusion: a multivariate analysis. Spine (Phila Pa 1976) 34: 161–166. [DOI] [PubMed] [Google Scholar]
- 6. Hou WH, Tsauo JY, Lin CH, Liang HW, Du CL (2008) Worker’s compensation and return-to-work following orthopaedic injury to extremities. J Rehabil Med 40: 440–445. [DOI] [PubMed] [Google Scholar]
- 7. Bhatia S, Piasecki DP, Nho SJ, Romeo AA, Cole BJ, et al. (2010) Early return to work in workers’ compensation patients after arthroscopic full-thickness rotator cuff repair. Arthroscopy 26: 1027–1034. [DOI] [PubMed] [Google Scholar]
- 8. Brinker MR, Savory CG, Weeden SH, Aucoin HC, Curd DT (1998) The results of total knee arthroplasty in workers’ compensation patients. Bull Hosp Jt Dis 57: 80–83. [PubMed] [Google Scholar]
- 9. Denard PJ, Ladermann A, Burkhart SS (2012) Long-term outcome after arthroscopic repair of type II SLAP lesions: results according to age and workers’ compensation status. Arthroscopy 28: 451–457. [DOI] [PubMed] [Google Scholar]
- 10. Holtby R, Razmjou H (2010) Impact of work-related compensation claims on surgical outcome of patients with rotator cuff related pathologies: a matched case-control study. J Shoulder Elbow Surg 19: 452–460. [DOI] [PubMed] [Google Scholar]
- 11. Wexler G, Bach BR Jr, Bush-Joseph CA, Smink D, Ferrari JD, et al. (2000) Outcomes of anterior cruciate ligament reconstruction in patients with Workers’ Compensation claims. Arthroscopy 16: 49–58. [DOI] [PubMed] [Google Scholar]
- 12. Cowan J, Makanji H, Mudgal C, Jupiter J, Ring D (2012) Determinants of return to work after carpal tunnel release. J Hand Surg Am 37: 18–27. [DOI] [PubMed] [Google Scholar]
- 13. Watson EM, Sonnabend DH (2002) Outcome of rotator cuff repair. J Shoulder Elbow Surg 11: 201–211. [DOI] [PubMed] [Google Scholar]
- 14. Byrd JW, Jones KS (2000) Prospective analysis of hip arthroscopy with 2-year follow-up. Arthroscopy 16: 578–587. [DOI] [PubMed] [Google Scholar]
- 15. Heckerling PS (2006) Placebo surgery research: A blinding imperative. Journal of Clinical Epidemiology 59: 876–880. [DOI] [PubMed] [Google Scholar]
- 16. Hoppe DJ, Schemitsch EH, Morshed S, Tornetta P, 3rd, Bhandari M (2009) Hierarchy of evidence: where observational studies fit in and why we need them. J Bone Joint Surg Am 91 Suppl 32–9. [DOI] [PubMed] [Google Scholar]
- 17. Simunovic N, Sprague S, Bhandari M (2009) Methodological issues in systematic reviews and meta-analyses of observational studies in orthopaedic research. J Bone Joint Surg Am 91 Suppl 387–94. [DOI] [PubMed] [Google Scholar]
- 18. Tunis SR, Stryer DB, Clancy CM (2003) Practical clinical trials: increasing the value of clinical research for decision making in clinical and health policy. JAMA 290: 1624–1632. [DOI] [PubMed] [Google Scholar]
- 19. Moraes VY, Belloti JC, Moraes FY, Galbiatti JA, Palacio EP, et al. (2011) Hierarchy of evidence relating to hand surgery in Brazilian orthopedic journals. Sao Paulo Med J 129: 94–98. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Bhandari M, Morshed S, Tornetta P, 3rd, Schemitsch EH (2009) Design, conduct, and interpretation of nonrandomized orthopaedic studies: a practical approach. (All) evidence matters. J Bone Joint Surg Am 91 Suppl 31. [DOI] [PubMed] [Google Scholar]
- 21.Audigue L, Bhandari M, Griffin D, Middleton P, Reeves BC (2004) Systematic Reviews of Nonrandomized Clinical Studies in the Orthopaedic Literature. Clinical Orthopaedics and Related Research 427: 249–257 210.1097/1001.blo.0000137558.0000197346.fb. [DOI] [PubMed]
- 22. Park MJ, Hsu JE, Harper C, Sennett BJ, Huffman GR (2011) Poly-L/D-lactic acid anchors are associated with reoperation and failure of SLAP repairs. Arthroscopy 27: 1335–1340. [DOI] [PubMed] [Google Scholar]
- 23. Schwartz CE, Martha JF, Kowalski P, Wang DA, Bode R, et al. (2009) Prospective evaluation of chronic pain associated with posterior autologous iliac crest bone graft harvest and its effect on postoperative outcome. Health Qual Life Outcomes 7: 49. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Kemp KA, Sheps DM, Luciak-Corea C, Styles-Tripp F, Buckingham J, et al. (2011) Systematic review of rotator cuff tears in workers’ compensation patients. Occup Med (Lond) 61: 556–562. [DOI] [PubMed] [Google Scholar]
- 25. Gougoulias N, Khanna A, McBride DJ, Maffulli N (2009) Management of calcaneal fractures: systematic review of randomized trials. Br Med Bull 92: 153–167. [DOI] [PubMed] [Google Scholar]
- 26. Harris I, Mulford J, Solomon M, van Gelder JM, Young J (2005) Association between compensation status and outcome after surgery: a meta-analysis. JAMA 293: 1644–1652. [DOI] [PubMed] [Google Scholar]
- 27. Koljonen P, Chong C, Yip D (2009) Difference in outcome of shoulder surgery between workers’ compensation and nonworkers’ compensation populations. Int Orthop 33: 315–320. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Cook DJ, Mulrow CD, Haynes RB (1997) Systematic reviews: synthesis of best evidence for clinical decisions. Ann Intern Med 126: 376–380. [DOI] [PubMed] [Google Scholar]
- 29.Higgins J, S G (2005) Cochrane handbook for systematic reviews of interventions 4.2.4 [updated March 2005].
- 30. Liberati A, Altman DG, Tetzlaff J, Mulrow C, Gøtzsche PC, et al. (2009) The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate health care interventions: explanation and elaboration. Journal of Clinical Epidemiology 62: e1–e34. [DOI] [PubMed] [Google Scholar]
- 31.Moraes VY, Belloti JC, Godin K, Bhandari M (2012) Influence from presumed compensation status in orthopedic surgery: does it affect the outcomes? A systematic review of prospective studies. PROSPERO Database CRD42012002121.
- 32. Hudak PL, Amadio PC, Bombardier C (1996) Development of an upper extremity outcome measure: the DASH (disabilities of the arm, shoulder and hand) [corrected]. The Upper Extremity Collaborative Group (UECG). Am J Ind Med 29: 602–608. [DOI] [PubMed] [Google Scholar]
- 33.Fairbank JC, Pynsent PB (2000) The Oswestry Disability Index. Spine (Phila Pa 1976) 25: 2940–2952; discussion 2952. [DOI] [PubMed]
- 34.Guyatt G, Busse J (2011) Tool to Assess Risk of Bias in Cohort Studies.
- 35.Manager(RevMan) R (2011) [Computer program]. Version 5.1. Copenhagen: The Nordic Cochrane Centre, The Cochrane Collaboration.
- 36. Dersimonian R, Laird N (1986) Metaanalysis in Clinical-Trials. Controlled Clinical Trials 7: 177–188. [DOI] [PubMed] [Google Scholar]
- 37. Antoniou J, Duckworth DT, Harryman DT (2000) Capsulolabral augmentation for the management of posteroinferior instability of the shoulder. Journal of Bone and Joint Surgery-American Volume 82A: 1220–1230. [DOI] [PubMed] [Google Scholar]
- 38. Asch HL, Lewis PJ, Moreland DB, Egnatchik JG, Yu YJ, et al. (2002) Prospective multiple outcomes study of outpatient lumbar microdiscectomy: should 75 to 80% success rates be the norm? Journal of Neurosurgery 96: 34–44. [DOI] [PubMed] [Google Scholar]
- 39. Atlas SJ, Tosteson TD, Blood EA, Skinner JS, Pransky GS, et al. (2010) The impact of workers’ compensation on outcomes of surgical and nonoperative therapy for patients with a lumbar disc herniation: SPORT. Spine (Phila Pa 1976) 35: 89–97. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Balyk R, Luciak-Corea C, Otto D, Baysal D, Beaupre L (2008) Do Outcomes Differ after Rotator Cuff Repair for Patients Receiving Workers’ Compensation? Clinical Orthopaedics and Related Research 466: 3025–3033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Barrett GR, Rook RT, Nash CR, Coggin MR (2001) The effect of Workers’ Compensation on clinical outcomes of arthroscopic-assisted autogenous patellar tendon anterior cruciate ligament reconstruction in an acute population. Arthroscopy 17: 132–137. [DOI] [PubMed] [Google Scholar]
- 42. Buckley R, Tough S, McCormack R, Pate G, Leighton R, et al. (2002) Operative compared with nonoperative treatment of displaced intra-articular calcaneal fractures: a prospective, randomized, controlled multicenter trial. J Bone Joint Surg Am 84-A: 1733–1744. [DOI] [PubMed] [Google Scholar]
- 43. Deutsch H, Musacchio MJ Jr (2006) Minimally invasive transforaminal lumbar interbody fusion with unilateral pedicle screw fixation. Neurosurg Focus 20: E10. [DOI] [PubMed] [Google Scholar]
- 44. Glowacki KA, Weiss AP (1997) Anterior intramuscular transposition of the ulnar nerve for cubital tunnel syndrome. J Shoulder Elbow Surg 6: 89–96. [DOI] [PubMed] [Google Scholar]
- 45.Greenough CG, Taylor LJ, Fraser RD (1994) Anterior Lumbar Fusion - a Comparison of Noncompensation Patients with Compensation Patients. Clinical Orthopaedics and Related Research: 30–37. [PubMed]
- 46. Henn F, Kang L, Tashjian RZ, Green A (2008) Patients with Workers’ Compensation Claims Have Worse Outcomes After Rotator Cuff Repair. Journal of Bone and Joint Surgery-American Volume 90A: 2105–2113. [DOI] [PubMed] [Google Scholar]
- 47. Johannsen HV, Andersen NH, Sojbjerg JO, Sneppen O (1997) [Arthroscopic subacromial decompression]. Ugeskr Laeger 159: 166–170. [PubMed] [Google Scholar]
- 48. Lin SS, Bono CM, Treuting R, Shereff MJ (2000) Limited intertarsal arthrodesis using bone grafting and pin fixation. Foot Ankle Int 21: 742–748. [DOI] [PubMed] [Google Scholar]
- 49. Mackay MA, Fischgrund JS, Herkowitz HN, Kurz LT, Hecht B, et al. (1995) The Effect of Interposition Membrane on the Outcome of Lumbar Laminectomy and Diskectomy. Spine 20: 1793–1796. [DOI] [PubMed] [Google Scholar]
- 50. McKee MD, Yoo DJ (2000) The effect of surgery for rotator cuff disease on general health status - Results of a prospective trial. Journal of Bone and Joint Surgery-American Volume 82A: 970–979. [DOI] [PubMed] [Google Scholar]
- 51. Nagle D, Harris G, Foley M (1994) Prospective review of 278 endoscopic carpal tunnel releases using the modified chow technique. Arthroscopy 10: 259–265. [DOI] [PubMed] [Google Scholar]
- 52. Nicholson GP (2003) Arthroscopic acromioplasty: A comparison between workers’ compensation and non-workers’ compensation populations. Journal of Bone and Joint Surgery-American Volume 85A: 682–689. [PubMed] [Google Scholar]
- 53. Rosenberger RE, Gomoll AH, Bryant T, Minas T (2008) Repair of Large Chondral Defects of the Knee With Autologous Chondrocyte Implantation in Patients 45 Years or Older. American Journal of Sports Medicine 36: 2336–2344. [DOI] [PubMed] [Google Scholar]
- 54. Spangehl MJ, Hawkins RH, McCormack RG, Loomer RL (2002) Arthroscopic versus open acromioplasty: A prospective, randomized, blinded study. Journal of Shoulder and Elbow Surgery 11: 101–107. [DOI] [PubMed] [Google Scholar]
- 55. Straub TA (1999) Endoscopic carpal tunnel release: a prospective analysis of factors associated with unsatisfactory results. Arthroscopy 15: 269–274. [DOI] [PubMed] [Google Scholar]
- 56. Westkaemper JG, Mitsionis G, Giannakopoulos PN, Sotereanos DG (1998) Wrist arthroscopy for the treatment of ligament and triangular fibrocartilage complex injuries. Arthroscopy 14: 479–483. [DOI] [PubMed] [Google Scholar]
- 57. Cole DC, Mondloch MV, Hogg-Johnson S (2002) Listening to injured workers: how recovery expectations predict outcomes–a prospective study. CMAJ 166: 749–754. [PMC free article] [PubMed] [Google Scholar]
- 58. DeBerard MS, Masters KS, Colledge AL, Holmes EB (2003) Presurgical biopsychosocial variables predict medical and compensation costs of lumbar fusion in Utah workers’ compensation patients. Spine J 3: 420–429. [DOI] [PubMed] [Google Scholar]
- 59. Fadyl J, McPherson K (2008) Return to work after injury: a review of evidence regarding expectations and injury perceptions, and their influence on outcome. J Occup Rehabil 18: 362–374. [DOI] [PubMed] [Google Scholar]
- 60. Atlas SJ, Deyo RA, Keller RB, Chapin AM, Patrick DL, et al. (1996) The Maine Lumbar Spine Study, Part II. 1-year outcomes of surgical and nonsurgical management of sciatica. Spine (Phila Pa 1976) 21: 1777–1786. [DOI] [PubMed] [Google Scholar]
- 61. Dzioba RB, Doxey NC (1984) A prospective investigation into the orthopaedic and psychologic predictors of outcome of first lumbar surgery following industrial injury. Spine (Phila Pa 1976) 9: 614–623. [DOI] [PubMed] [Google Scholar]
- 62.Hinkley BS, Jaremko ME (1997) Effects of 360-degree lumbar fusion in a workers’ compensation population. Spine (Phila Pa 1976) 22: 312–322; discussion 323. [DOI] [PubMed]
- 63. Hodges SD, Humphreys SC, Eck JC, Covington LA, Harrom H (2001) Predicting factors of successful recovery from lumbar spine surgery among workers’ compensation patients. J Am Osteopath Assoc 101: 78–83. [PubMed] [Google Scholar]
- 64. Day CS, Makhni EC, Mejia E, Lage DE, Rozental TD (2010) Carpal and cubital tunnel syndrome: who gets surgery? Clin Orthop Relat Res 468: 1796–1803. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65. Olney JR, Quenzer DE, Makowsky M (1999) Contested claims in carpal tunnel surgery: outcome study of worker’s compensation factors. Iowa Orthop J 19: 111–121. [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Search Strategy
(DOC)
Quality Assessment Tool
(DOC)