Abstract
BACKGROUND
For persons who have an out-of-hospital cardiac arrest, the probability of receiving bystander-initiated cardiopulmonary resuscitation (CPR) may be influenced by neighborhood characteristics.
METHODS
We analyzed surveillance data prospectively submitted from 29 U.S. sites to the Cardiac Arrest Registry to Enhance Survival between October 1, 2005, and December 31, 2009. The neighborhood in which each cardiac arrest occurred was determined from census-tract data. We classified neighborhoods as high-income or low-income on the basis of a median household income threshold of $40,000 and as white or black if more than 80% of the census tract was predominantly of one race. Neighborhoods without a predominant racial composition were classified as integrated. We analyzed the relationship between the median income and racial composition of a neighborhood and the performance of bystander-initiated CPR.
RESULTS
Among 14,225 patients with cardiac arrest, bystander-initiated CPR was provided to 4068 (28.6%). As compared with patients who had a cardiac arrest in high-income white neighborhoods, those in low-income black neighborhoods were less likely to receive bystander-initiated CPR (odds ratio, 0.49; 95% confidence interval [CI], 0.41 to 0.58). The same was true of patients with cardiac arrest in neighborhoods characterized as low-income white (odds ratio, 0.65; 95% CI, 0.51 to 0.82), low-income integrated (odds ratio, 0.62; 95% CI, 0.56 to 0.70), and high-income black (odds ratio, 0.77; 95% CI, 0.68 to 0.86). The odds ratio for bystander-initiated CPR in high-income integrated neighborhoods (1.03; 95% CI, 0.64 to 1.65) was similar to that for high-income white neighborhoods.
CONCLUSIONS
In a large cohort study, we found that patients who had an out-of-hospital cardiac arrest in low-income black neighborhoods were less likely to receive bystander-initiated CPR than those in high-income white neighborhoods. (Funded by the Centers for Disease Control and Prevention and others.)
More than 300,000 cases of out-of-hospital cardiac arrest occur in the United States each year.1 Outcomes of out-of-hospital cardiac arrest vary markedly,2 with survival rates ranging from 0.2% in Detroit3 to 16.0% in Seattle.2 This variation in survival rates can be explained, in part, by different rates of bystander-initiated cardiopulmonary resuscitation (CPR).4,5 On average, bystanders administer CPR during fewer than one third of all out-of-hospital cardiac arrests.6
Prior studies have shown racial or ethnic-group and socioeconomic disparities in the provision of bystander-initiated CPR.7–11 However, it is unclear to what extent such disparities are due to neighborhood effects, which have been shown to exert a substantial influence in explaining variations and disparities in care for other conditions.12–15 Although a few studies have examined the effect of neighborhood on the receipt of bystander-initiated CPR during out-of-hospital cardiac arrest,6,16,17 these studies were conducted within small geographic areas and therefore may not be generalizable to other settings. The performance of bystander-initiated CPR depends on the availability of a person who is prepared to attempt CPR and initiate the chain of interventions required for survival, so the effect of neighborhood may be extremely important. If neighborhood characteristics have a significant effect on the likelihood that a bystander will administer CPR, it may be appropriate to direct public health interventions, such as CPR training, to specific communities identified on the basis of the features of individual neighborhoods.
Therefore, we analyzed data from a multicenter registry to assess how income and race at the neighborhood level, independent of individual event characteristics, affected the probability of receiving bystander-initiated CPR. We hypothesized that race and income at the neighborhood level would be strongly associated with the likelihood of bystander-initiated CPR and that these associations would remain consistent across a range of settings and locations.
METHODS
DATA SOURCE AND STUDY DESIGN
We analyzed data from the Cardiac Arrest Registry to Enhance Survival (CARES), which is a multi-center registry coordinated by the Centers for Disease Control and Prevention and Emory University. Detailed information about this registry, including catchment area, emergency-medical-service (EMS) characteristics, and cardiac-arrest protocols, has been reported previously.18–21 During the study period, from October 1, 2005, through December 31, 2009, CARES collected data on all 911-activated events involving cardiac arrest that occurred in 29 U.S. sites (Fig. 1S in the Supplementary Appendix, available with the full text of this article at NEJM.org). Within a catchment area of approximately 22 million people, 54 EMS agencies submitted data for all out-of-hospital cardiac arrests. The collection of data on all cardiac arrests by the 911 call center in each city was confirmed during the data-review process. A data analyst employed by CARES validated the data and reviewed every record for completeness and accuracy.21 The study was approved by the Emory University institutional review board, which waived the requirement for informed consent because the analysis included only deidentified data.
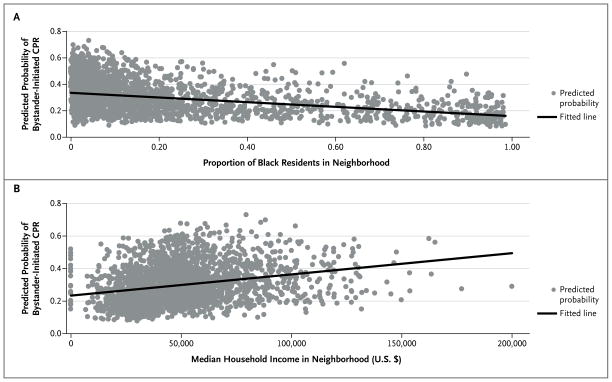
Figure 1. Predicted Probability of Bystander-Initiated Cardiopulmonary Resuscitation (CPR).
The predicted probability of bystander-initiated CPR is shown according to the proportion of black residents in a neighborhood (Panel A) and the median household income in a neighborhood (Panel B). The model that was used to calculate the predicted probability of bystander-initiated CPR included the following covariates: age (in decades), race or ethnic group, sex, witnessed or unwitnessed arrest, public or private location, and the six categories of neighborhood median household income and racial composition (low-income black, low-income integrated, low-income white, high-income black, high-income integrated, and high-income white).
SELECTION OF PARTICIPANTS
A total of 20,020 events met the criteria for an out-of-hospital cardiac arrest (see the definition and Fig. 2S in the Supplementary Appendix). We excluded 3682 events (18.4%) that did not meet our eligibility criteria (e.g., the cardiac arrest occurred in a facility with on-site health care professionals, such as a nursing home, hospital, medical clinic, or jail, or occurred in an airport [airports are typically closely monitored and have numerous trained rescuers and publicly accessible defibrillators available]). We further excluded 1883 events (9.4%) that were witnessed by EMS personnel, 82 (0.4%) for which the address at which the cardiac arrest occurred could not be determined, 8 (<0.1%) for which data documenting whether the patient received bystander-initiated CPR were missing, and 140 (0.7%) for which the clinical outcome was missing. Our final cohort comprised 14,225 patients with an out-of-hospital cardiac arrest.
DATA COLLECTION AND PROCESSING
Patient-level characteristics were obtained from the CARES database. Characteristics that were used as predictive variables included age, sex, race or ethnic group (coded by the EMS provider as white, black, Hispanic, other, or unknown), location of cardiac arrest (public vs. private), and whether the arrest was witnessed (by someone other than the first responder or EMS provider).
From CARES we also obtained data for the primary study outcome, which was performance of CPR by a bystander. We defined “bystander” as any person who was not part of the 911 response team. Additional CARES data included whether an automated external defibrillator was used, the cardiac rhythm at presentation, survival to hospital admission, survival to hospital discharge, and neurologic outcome at the time of hospital discharge. Neurologic outcome was coded by the CARES hospital contact with the use of a cerebral-performance category (CPC) scale ranging from 1 to 5, with 1 indicating conscious with normal function or only slight disability, 2 conscious with moderate disability, 3 conscious with severe disability, 4 comatose or in a vegetative state, and 5 brain-dead or dead.22–24
We geocoded the CARES data set on the basis of the address of the cardiac arrest, using the Centrus Desktop geocoder, version 4.0 (Pitney Bowes). We used census tracts as proxies for neighborhoods, because they represent socially and economically homogeneous groups of approximately 4000 to 7000 people.25 Neighborhood-level variables were linked to each geocoded address with the use of the 2000 U.S. Census Summary Files.26 From this linkage, we identified six neighborhood characteristics on the basis of a priori hypotheses from our previous work10 as possible predictors of bystander-initiated CPR. These included median age, median household income, percentage of people living below the poverty line, percentage of single-person households, racial or ethnic-group composition, and percentage of people with a high-school diploma or a higher level of education. For both the individual and census-tract characteristics, white race and black race were specified as non-Hispanic white and non-Hispanic black, respectively.
We classified neighborhoods as predominantly white (>80% white) or predominantly black (>80% black). If neither the proportion of black residents nor the proportion of white residents in a neighborhood was more than 80%, we classified the neighborhood as integrated. For our main analyses, we defined low-income and high-income neighborhoods as those census tracts in which the median annual household income was less than $40,000 and $40,000 or more, respectively. We then created a six-category variable to examine the association between the combination of neighborhood racial composition and median income and the provision of bystander-initiated CPR. The categories included low-income black, low-income integrated, low-income white, high-income black, high-income integrated, and high-income white.
STATISTICAL ANALYSIS
The primary outcome for all analyses was performance of bystander-initiated CPR. To determine the associations of individual-level and neighborhood-level characteristics with the performance of bystander-initiated CPR, we used a three-level hierarchical logistic-regression model. This allowed us to account for the nesting of 14,225 patients (level 1) within 2403 neighborhoods defined as census tracts (level 2), and 29 U.S. CARES sites (level 3). Individual-level characteristics (model 1) and neighborhood-level characteristics (model 2) were added to the model as fixed effects and CARES sites were added as random effects in order to examine their independent contributions. The final model was chosen on the basis of the greatest proportion of variance that was explained by individual and neighborhood variables. We then conducted 10-fold cross-validation (i.e., the data were divided into 10 validation subsets) to assess the calibration and discrimination of the model. Finally, we conducted posterior predictions, stratified according to type of cardiac arrest (unwitnessed in a private location [i.e., home], witnessed in a private location, unwitnessed in a public location, or witnessed in a public location), to show the associations between neighborhood and performance of bystander-initiated CPR.
Several sensitivity analyses were conducted to assess the potential effect of different thresholds on the associations in our model (e.g., high vs. low income and black vs. white race). All statistical analyses were conducted with the use of Stata software, version 11.2 (StataCorp). P values are based on a two-sided significance level of 0.05.
RESULTS
PATIENT AND NEIGHBORHOOD CHARACTERISTICS
Of 14,225 patients with out-of-hospital cardiac arrests that met the criteria for inclusion in the study, 4068 (28.6%) received bystander-initiated CPR. The individual-level and neighborhood-level characteristics of the cardiac arrests that were included in the predictive analyses are shown in Table 1, according to whether bystander-initiated CPR was performed. Patients with cardiac arrest who received bystander-initiated CPR were more likely to be male than female, more likely to be white than another race or ethnic group, more likely to be in a public location than a private location at the time of the arrest, and more likely to have a witnessed arrest than an unwitnessed arrest. Patients were less likely to receive bystander-initiated CPR if they had a cardiac arrest in a neighborhood that was low-income or predominantly black (Table 1 and Fig. 1).
Table 1.
Demographic, Cardiac-Arrest, and Neighborhood Characteristics According to Whether Bystander-Initiated Cardiopulmonary Resuscitation (CPR) Was Performed.*
| Characteristic | Bystander-Initiated CPR (N = 4068) | No Bystander-Initiated CPR (N = 10,157) |
|---|---|---|
| Individual level | ||
| Age — yr† | 60.1±19 | 61.8±19 |
| Sex — no./total no. (%) | ||
| Female | 1402/5299 (26) | 3897/5299 (74) |
| Male | 2666/8921 (30) | 6255/8921 (70) |
| Missing data | 0/5 | 5/5 (100) |
| Race or ethnic group — no./total no. (%)‡ | ||
| White | 1780/5464 (33) | 3684/5464 (67) |
| Black | 886/3950 (22) | 3064/3950 (78) |
| Hispanic | 234/857 (27) | 623/857 (73) |
| Other | 107/364 (29) | 257/364 (71) |
| Missing data | 1061/3590 (30) | 2529/3590 (70) |
| Cardiac arrest witnessed — no./total no. (%) | ||
| Yes | 2285/6082 (38) | 3797/6082 (62) |
| No | 1783/8140 (22) | 6357/8140 (78) |
| Missing data | 0/3 | 3/3 (100) |
| Location of cardiac arrest — no./total no. (%) | ||
| Home | 2959/11,500 (26) | 8541/11,500 (74) |
| Public building | 478/1024 (47) | 546/1024 (53) |
| Street | 222/825 (27) | 603/825 (73) |
| Recreational facility | 154/244 (63) | 90/244 (37) |
| Industrial building | 78/149 (52) | 71/149 (48) |
| Educational building | 29/50 (58) | 21/50 (42) |
| Other | 148/433 (34) | 285/433 (66) |
| Neighborhood level | ||
| Racial composition — no./total no. (%) | ||
| >80% black | 337/1828 (18) | 1491/1828 (82) |
| Integrated | 2217/8062 (27) | 5845/8062 (73) |
| >80% white | 1514/4335 (35) | 2821/4335 (65) |
| Median household income — no./total no. (%) | ||
| ≤$25,000 | 447/2079 (22) | 1632/2079 (78) |
| $25,001–$40,000 | 1169/4606 (25) | 3437/4606 (75) |
| $40,001–$50,000 | 786/2612 (30) | 1826/2612 (70) |
| $50,001–$65,000 | 789/2548 (31) | 1759/2548 (69) |
| >$65,000 | 877/2380 (37) | 1503/2380 (63) |
| Median household income and racial composition — no./total no. (%) | ||
| $50,000 and 80% threshold | ||
| <$50,000 and >80% black | 316/1744 (18) | 1428/1744 (82) |
| <$50,000 and integrated | 1711/6337 (27) | 4626/6337 (73) |
| <$50,000 and >80% white | 375/1215 (31) | 840/1215 (69) |
| ≥$50,000 and >80% black | 21/84 (25) | 63/84 (75) |
| ≥$50,000 and integrated | 506/1725 (29) | 1219/1725 (71) |
| ≥$50,000 and >80% white | 1139/3120 (37) | 1981/3120 (63) |
| $40,000 and 80% threshold | ||
| <$40,000 and >80% black | 300/1693 (18) | 1393/1693 (82) |
| <$40,000 and integrated | 1170/4486 (26) | 3316/4486 (74) |
| <$40,000 and >80% white | 144/499 (29) | 355/499 (71) |
| ≥$40,000 and >80% black | 37/135 (27) | 98/135 (73) |
| ≥$40,000 and integrated | 1047/3576 (29) | 2529/3576 (71) |
| ≥$40,000 and >80% white | 1370/3836 (37) | 2466/3836 (63) |
| $30,000 and 80% threshold | ||
| <$30,000 and >80% black | 230/1287 (18) | 1057/1287 (82) |
| <$30,000 and integrated | 562/2193 (26) | 1631/2193 (74) |
| <$30,000 and >80% white | 35/124 (28) | 89/124 (72) |
| ≥$30,000 and >80% black | 107/541 (20) | 434/541 (80) |
| ≥$30,000 and integrated | 1655/5869 (28) | 4214/5869 (72) |
| ≥$30,000 and >80% white | 1479/4211 (35) | 2732/4211 (65) |
Plus–minus values are means ±SD.
Data on age were missing for 7 patients who received bystander-initiated CPR and 38 who did not.
Race or ethnic group was coded by the emergency-medical-services provider.
Of the 14,225 patients included in the study, 1144 (8.0%) survived to hospital discharge; 587 patients (4.1%) were discharged home with a CPC score of 1. As compared with patients who did not receive bystander-initiated CPR, those who did were more likely to be found with a shockable rhythm such as ventricular fibrillation or ventricular tachycardia, to receive treatment with an automated external defibrillator, to survive to hospital admission and discharge, and to have a CPC score of 1 or 2 at the time of discharge. Additional characteristics of the study cohort are provided in Table 1S in the Supplementary Appendix.
MULTIVARIABLE PREDICTIVE MODEL
Table 2 shows the final multivariable model and the adjusted odds ratios and 95% confidence intervals for performance of bystander-initiated CPR. At the individual level, patients who were black or Hispanic were less likely to receive bystander-initiated CPR than those who were white. As compared with persons with cardiac arrest in high-income white neighborhoods, those in low-income black neighborhoods were less likely to receive bystander-initiated CPR. Patients with cardiac arrest in low-income white, low-income integrated, and high-income black neighborhoods were also less likely to receive bystander-initiated CPR. High-income integrated neighborhoods were similar to high-income white neighborhoods with respect to receipt of bystander-initiated CPR. Cross-validation of the final model showed excellent calibration and modest discrimination (Fig. 3AS and 3BS in the Supplementary Appendix). Sensitivity analyses showed that our findings remained unchanged when different thresholds were used to define median income and racial composition of the neighborhoods (Table 2S in the Supplementary Appendix).
Table 2.
Final Adjusted Model for Provision of Bystander-Initiated CPR.*
| Variable | Odds Ratio (95% CI) | P Value |
|---|---|---|
| Individual level | ||
| Age in decades† | 0.94 (0.92–0.96) | <0.001 |
| Sex | ||
| Male | 1.00 | |
| Female | 1.01 (0.93–1.09) | 0.87 |
| Race or ethnic group | ||
| White | 1.00 | |
| Black | 0.78 (0.70–0.87) | <0.001 |
| Hispanic | 0.73 (0.61–0.87) | 0.001 |
| Other | 0.94 (0.74–1.21) | 0.65 |
| Unknown | 0.80 (0.72–0.89) | <0.001 |
| Witnessing of cardiac arrest | ||
| Unwitnessed | 1.00 | |
| Witnessed | 2.01 (1.85–2.17) | <0.001 |
| Location of cardiac arrest | ||
| Private | 1.00 | |
| Public | 1.70 (1.54–1.87) | <0.001 |
| Neighborhood level | ||
| Median household income and racial composition | ||
| ≥$40,000 and >80% white | 1.00 | |
| ≥$40,000 and integrated | 1.03 (0.64–1.65) | 0.90 |
| ≥$40,000 and >80% black | 0.77 (0.68–0.86) | <0.001 |
| <$40,000 and >80% white | 0.65 (0.51–0.82) | <0.001 |
| <$40,000 and integrated | 0.62 (0.56–0.70) | <0.001 |
| <$40,000 and >80% black | 0.49 (0.41–0.58) | <0.001 |
The predictive accuracy of this model was assessed with the use of measures of calibration and discrimination. The goodness-of-fit P value on Hosmer–Lemeshow testing was 0.23 (calibration), and the area under the receiver- operating-characteristic curve was 0.64 (discrimination) (see the Supplementary Appendix).
For every 10-year increase in age after the age of 18, there was an associated decrease in the likelihood of having bystander-initiated CPR performed.
The magnitude of census-tract effects on the provision of bystander-initiated CPR stratified according to type of cardiac arrest is shown in Table 3S in the Supplementary Appendix. All other things being equal, patients with a witnessed arrest in a public location in a high-income white neighborhood had a higher probability of receiving bystander-initiated CPR than did patients with a witnessed arrest in a public location in a low-income black neighborhood. There was a similar relationship across all four subgroups of cardiac-arrest types (unwitnessed in a private location, witnessed in a private location, unwitnessed in a public location, and witnessed in a public location); patients with cardiac arrest in a high-income white neighborhood were more likely to receive bystander-initiated CPR than those in a low-income black neighborhood.
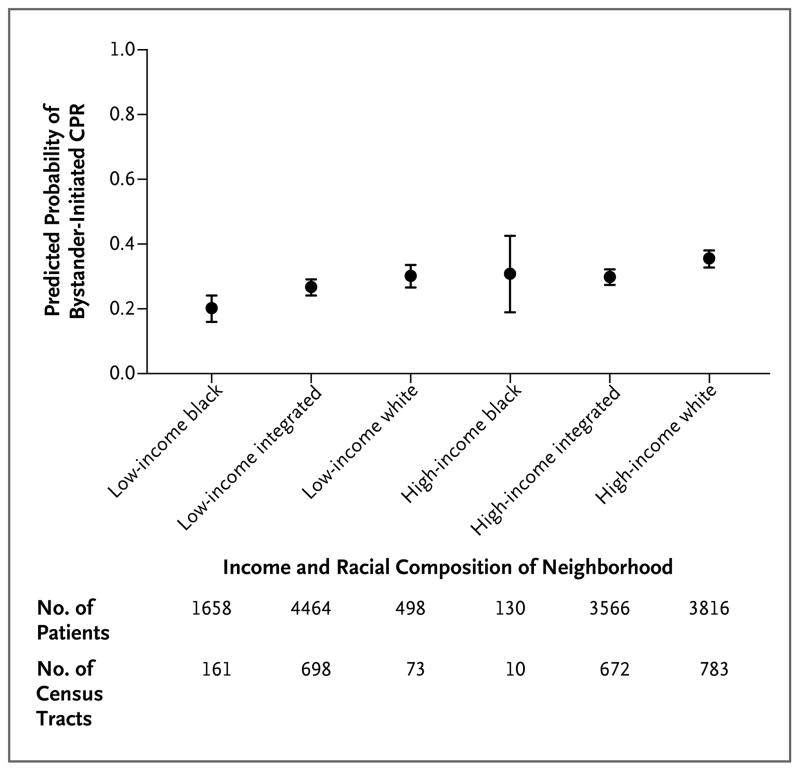
PROBABILITY OF RECEIVING CPR
Using the estimates from the adjusted model, we determined the probability of receiving bystander-initiated CPR across the six categories of median income and racial composition. Figure 2 shows how the mean probability of receiving bystander-initiated CPR and corresponding 95% confidence intervals differed across these categories.
Figure 2. Predicted Probability of Bystander-Initiated CPR According to the Median Income and Racial Composition of the Neighborhood.
Point estimates with 95% confidence intervals, indicated by I bars, are shown. The predicted probabilities were missing for six census tracts and 93 individual patients.
Because CARES data were submitted by 29 U.S. sites with a combined base population of approximately 22 million, we also wanted to determine how predicted probabilities differed across sites within the same six categories of median income and racial composition (Fig. 4S in the Supplementary Appendix). In 13 of the 14 CARES sites that had low-income black neighborhoods, patients who had cardiac arrest in these types of neighborhoods had the lowest mean predicted probability of receiving bystander-initiated CPR. In 22 of the total 29 CARES sites, patients who had cardiac arrest in high-income white neighborhoods had the highest mean predicted probability of receiving bystander-initiated CPR.
DISCUSSION
We found a direct relationship between the median income and racial composition of a neighborhood and the probability that a person with out-of-hospital cardiac arrest received bystander-initiated CPR. This association was most apparent in low-income black neighborhoods, where the odds of receiving bystander-initiated CPR were approximately 50% lower than in high-income non-black neighborhoods. Even in high-income black neighborhoods, patients with out-of-hospital cardiac arrest were approximately 23% less likely to receive bystander-initiated CPR than were patients in high-income nonblack neighborhoods. In 13 of 14 CARES sites that had low-income black neighborhoods, we found that patients with cardiac arrest were disproportionately less likely to receive bystander-initiated CPR, whereas in 22 of 29 CARES sites, persons with cardiac arrest in a high-income white neighborhood were the most likely to receive bystander-initiated CPR.
Studies from Canada11 and Seattle27 have shown that patients with out-of-hospital cardiac arrest who collapse in an area of higher socioeconomic status, which is associated with higher educational attainment, are more likely to receive CPR. In contrast, data from Chicago in the 1980s suggested that the racial composition of a neighborhood, but not the median income, was an important predictor of the likelihood of receiving bystander-initiated CPR.16 Our study, conducted with data from a large national registry, shows that both the racial composition and the median income of a neighborhood have a significant effect on the likelihood of receiving bystander-initiated CPR. This finding suggests that CPR training targeted to neighborhoods with racial and economic characteristics associated with a low probability of bystander-initiated CPR may constitute an evidence-based approach to public health planning. Further research is needed to determine how these neighborhood characteristics affect survival after out-of-hospital cardiac arrest.
We also found that, independent of the neighborhood in which the cardiac arrest occurs, blacks and Hispanics were approximately 30% less likely than whites to receive bystander-initiated CPR, an observation that is consistent with prior research.7–9,28 This suggests that neighborhood effects, although important, do not fully account for observed racial differences. In this and prior studies, a person’s race or ethnic group remained associated with differences in outcomes within the same neighborhood or hospital.29 We did not have data on individual household income in the CARES database and thus could not assess the independent effect of this factor on the likelihood of receiving bystander-initiated CPR.
A 2008 American Heart Association scientific statement highlighted the importance of bystander-initiated CPR and expressed concern that only 15 to 30% of persons with out-of-hospital cardiac arrest receive it.30 That report recommended efforts to broaden CPR training as well as research into improving the dissemination of CPR training. The current study shows, however, that although rates of bystander-initiated CPR are too low in general, there are also wide disparities in those rates according to neighborhood characteristics. Our previous research has shown that within the same community, certain neighborhoods can be identified that have an incidence of out-of-hospital cardiac arrest that is 2 to 3 times as high as that in other neighborhoods, with a percentage of bystander-initiated CPR that is one fifth as high.17 A tailored approach targeting CPR training to these high-risk neighborhoods may therefore be particularly effective in increasing nationwide performance of bystander-initiated CPR. In addition, once the barriers to CPR training and performance are better understood, it may be possible to design more linguistically appropriate and culturally sensitive CPR training programs that can be implemented in neighborhoods with low rates of bystander-initiated CPR.
There are several important limitations of our study. First, individual-level data on race or ethnic group were missing or coded as “unknown” in approximately 25% of our sample. The fact that this subgroup of patients had a lower likelihood of receiving bystander-initiated CPR, which was similar to the likelihood for blacks, suggests that data on race or ethnic group were not missing at random in our study cohort. Second, we do not have data on EMS activation times (i.e., the time between the initial witnessing of the arrest and the 911 call) or EMS response times. Further research will need to explore the relationship between these two important variables and the median income and racial composition of neighborhoods. In addition, although we included a random effect for each CARES site, we chose not to include any site-level variables in our hierarchical models because of a lack of standardized data collection for specific variables that may influence the variation in CPR performance across sites. Unmeasured confounders could include level of funding of the EMS system, the implementation of large-scale public education campaigns for CPR, and variations in neighborhood cohesiveness among low-income and black neighborhoods. However, our use of random-effects hierarchical modeling should have reduced bias in our results from unmeasured confounders.
The cities included in the CARES data set are primarily moderate-to-large metropolitan areas and do not include rural areas. As a result, our conclusions may not be generalizable to the entire nation, especially to persons living in rural areas. Finally, we chose to use census tract as a proxy for neighborhood. Although a neighborhood may not be located specifically within one census tract, this method has been validated as a feasible and acceptable alternative approach to examining the contextual effects of neighborhood on health outcomes.25,31,32
In conclusion, we found that the racial and socioeconomic composition of neighborhoods has important effects on the likelihood of bystander-initiated CPR for a person with an out-of-hospital cardiac arrest. Public health efforts that target CPR training to low-income black neighborhoods may help reduce these disparities.
Supplementary Material
Acknowledgments
Supported by a cooperative agreement between the Cardiac Arrest Registry to Enhance Survival and the Centers for Disease Control and Prevention (U18 PS000314); grants from the Emergency Medicine Foundation and the American Heart Association (to Dr. Sasson); an Independent Scientist Award from the Agency for Healthcare Research and Quality (K02 HS017526, to Dr. Haukoos); and a grant from the National Heart, Lung, and Blood Institute (K23HL102224, to Dr. Chan).
We thank the following people from the Centers for Disease Control and Prevention: Efomo Woghiren, B.Sc., for assistance with geocoding; Amy Valderrama, Ph.D., and Robert Merritt, M.A., for assistance with data collection and review of an earlier version of the manuscript; and Rachel Robb, Kimberly Vallano, Monica Mehta, and Amanda Bray-Perez for assistance with data collection.
Footnotes
Disclosure forms provided by the authors are available with the full text of this article at NEJM.org.
References
- 1.Roger VL, Go AS, Lloyd-Jones DM, et al. Heart disease and stroke statistics — 2012 update. Circulation. 2012;125(1):e2–e220. doi: 10.1161/CIR.0b013e31823ac046. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Nichol G, Thomas E, Callaway CW, et al. Regional variation in out-of-hospital cardiac arrest incidence and outcome. JAMA. 2008;300:1423–31. doi: 10.1001/jama.300.12.1423. (Erratum, JAMA 2008;300:1763.) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Dunne RB, Compton S, Zalenski RJ, Swor R, Welch R, Bock BF. Outcomes from out-of-hospital cardiac arrest in Detroit. Resuscitation. 2007;72:59–65. doi: 10.1016/j.resuscitation.2006.04.017. [DOI] [PubMed] [Google Scholar]
- 4.Cummins RO. Emergency medical services and sudden cardiac arrest: the “chain of survival” concept. Annu Rev Public Health. 1993;14:313–33. doi: 10.1146/annurev.pu.14.050193.001525. [DOI] [PubMed] [Google Scholar]
- 5.2005 American Heart Association guidelines for cardiopulmonary resuscitation and emergency cardiovascular care. Circulation. 2005;112(24 Suppl):IV1–IV203. doi: 10.1161/CIRCULATIONAHA.105.166550. [DOI] [PubMed] [Google Scholar]
- 6.Sasson C, Rogers MA, Dahl J, Kellermann AL. Predictors of survival from out-of-hospital cardiac arrest: a systematic review and meta-analysis. Circ Cardiovasc Qual Outcomes. 2010;3:63–81. doi: 10.1161/CIRCOUTCOMES.109.889576. [DOI] [PubMed] [Google Scholar]
- 7.Brookoff D, Kellermann AL, Hackman BB, Somes G, Dobyns P. Do blacks get bystander cardiopulmonary resuscitation as often as whites? Ann Emerg Med. 1994;24:1147–50. doi: 10.1016/s0196-0644(94)70246-2. [DOI] [PubMed] [Google Scholar]
- 8.Becker LB, Han BH, Meyer PM, et al. Racial differences in the incidence of cardiac arrest and subsequent survival. N Engl J Med. 1993;329:600–6. doi: 10.1056/NEJM199308263290902. [DOI] [PubMed] [Google Scholar]
- 9.Galea S, Blaney S, Nandi A, et al. Explaining racial disparities in incidence of and survival from out-of-hospital cardiac arrest. Am J Epidemiol. 2007;166:534–43. doi: 10.1093/aje/kwm102. [DOI] [PubMed] [Google Scholar]
- 10.Sasson C, Keirns CC, Smith DM, et al. Examining the contextual effects of neighborhood on out-of-hospital cardiac arrest and the provision of bystander cardiopulmonary resuscitation. Resuscitation. 2011;82:674–9. doi: 10.1016/j.resuscitation.2011.02.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Vaillancourt C, Lui A, De Maio VJ, Wells GA, Stiell IG. Socioeconomic status influences bystander CPR and survival rates for out-of-hospital cardiac arrest victims. Resuscitation. 2008;79:417–23. doi: 10.1016/j.resuscitation.2008.07.012. [DOI] [PubMed] [Google Scholar]
- 12.Petersen LA, Wright SM, Peterson ED, Daley J. Impact of race on cardiac care and outcomes in veterans with acute myocardial infarction. Med Care. 2002;40(1 Suppl):I86–I96. doi: 10.1097/00005650-200201001-00010. [DOI] [PubMed] [Google Scholar]
- 13.Lisabeth LD, Diez Roux AV, Escobar JD, Smith MA, Morgenstern LB. Neighborhood environment and risk of ischemic stroke: the Brain Attack Surveillance in Corpus Christi (BASIC) Project. Am J Epidemiol. 2007;165:279–87. doi: 10.1093/aje/kwk005. [DOI] [PubMed] [Google Scholar]
- 14.Ding J, Diez Roux AV, Nieto FJ, et al. Racial disparity in long-term mortality rate after hospitalization for myocardial infarction: the Atherosclerosis Risk in Communities study. Am Heart J. 2003;146:459–64. doi: 10.1016/S0002-8703(03)00228-X. [DOI] [PubMed] [Google Scholar]
- 15.Diez-Roux AV, Link BG, Northridge ME. A multilevel analysis of income inequality and cardiovascular disease risk factors. Soc Sci Med. 2000;50:673–87. doi: 10.1016/s0277-9536(99)00320-2. [DOI] [PubMed] [Google Scholar]
- 16.Iwashyna TJ, Christakis NA, Becker LB. Neighborhoods matter: a population-based study of provision of cardiopulmonary resuscitation. Ann Emerg Med. 1999;34:459–68. doi: 10.1016/s0196-0644(99)80047-x. [DOI] [PubMed] [Google Scholar]
- 17.Sasson C, Keirns CC, Smith D, et al. Small area variations in out-of-hospital cardiac arrest: does the neighborhood matter? Ann Intern Med. 2010;153:19–22. doi: 10.1059/0003-4819-153-1-201007060-00255. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.McNally B, Stokes A, Crouch A, Kellermann AL. CARES: Cardiac Arrest Registry to Enhance Survival. Ann Emerg Med. 2009;54(5):674.e2–683.e2. doi: 10.1016/j.annemergmed.2009.03.018. [DOI] [PubMed] [Google Scholar]
- 19.Sasson C, Hegg AJ, Macy M, Park A, Kellermann A, McNally B. Prehospital termination of resuscitation in cases of refractory out-of-hospital cardiac arrest. JAMA. 2008;300:1432–8. doi: 10.1001/jama.300.12.1432. [DOI] [PubMed] [Google Scholar]
- 20.Govindarajan P, Lin L, Landman A, et al. Practice variability among the EMS systems participating in Cardiac Arrest Registry to Enhance Survival (CARES) Resuscitation. 2012;83:76–80. doi: 10.1016/j.resuscitation.2011.06.026. [DOI] [PubMed] [Google Scholar]
- 21.McNally B, Robb R, Mehta M, et al. Out-of-Hospital Cardiac Arrest Surveillance — Cardiac Arrest Registry to Enhance Survival (CARES), United States, October 1, 2005–December 31, 2010. MMWR Surveill Summ. 2011;60:1–19. [PubMed] [Google Scholar]
- 22.Safar P. Resuscitation after brain ischemia. In: Grenvik A, Safar P, editors. Brain failure and resuscitation. New York: Churchill Livingstone; 1981. pp. 155–84. [Google Scholar]
- 23.Cummins RO, Chamberlain DA, Abramson NS, et al. Recommended guidelines for uniform reporting of data from out-of-hospital cardiac arrest: the Utstein Style: a statement for health professionals from a task force of the American Heart Association, the European Resuscitation Council, the Heart and Stroke Foundation of Canada, and the Australian Resuscitation Council. Circulation. 1991;84:960–75. doi: 10.1161/01.cir.84.2.960. [DOI] [PubMed] [Google Scholar]
- 24.Jacobs I, Nadkarni V, Bahr J, et al. Cardiac arrest and cardiopulmonary resuscitation outcome reports: update and simplification of the Utstein templates for resuscitation registries: a statement for healthcare professionals from a task force of the International Liaison Committee on Resuscitation (American Heart Association, European Resuscitation Council, Australian Resuscitation Council, New Zealand Resuscitation Council, Heart and Stroke Foundation of Canada, InterAmerican Heart Foundation, Resuscitation Councils of Southern Africa) Circulation. 2004;110:3385–97. doi: 10.1161/01.CIR.0000147236.85306.15. [DOI] [PubMed] [Google Scholar]
- 25.Krieger N. Overcoming the absence of socioeconomic data in medical records: validation and application of a census-based methodology. Am J Public Health. 1992;82:703–10. doi: 10.2105/ajph.82.5.703. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.U.S. Census Bureau. Topologically Integrated Geographic Encoding and Referencing (TIGER) system. ( http://www.census.gov/geo/www/tiger)
- 27.Mitchell MJ, Stubbs BA, Eisenberg MS. Socioeconomic status is associated with provision of bystander cardiopulmonary resuscitation. Prehosp Emerg Care. 2009;13:478–86. doi: 10.1080/10903120903144833. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Vadeboncoeur TF, Richman PB, Darkoh M, Chikani V, Clark L, Bobrow BJ. Bystander cardiopulmonary resuscitation for out-of-hospital cardiac arrest in the Hispanic vs the non-Hispanic populations. Am J Emerg Med. 2008;26:655–60. doi: 10.1016/j.ajem.2007.10.002. [DOI] [PubMed] [Google Scholar]
- 29.Chan PS, Nichol G, Krumholz HM, et al. Racial differences in survival after inhospital cardiac arrest. JAMA. 2009;302:1195–201. doi: 10.1001/jama.2009.1340. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Abella BS, Aufderheide TP, Eigel B, et al. Reducing barriers for implementation of bystander-initiated cardiopulmonary resuscitation: a scientific statement from the American Heart Association for healthcare providers, policymakers, and community leaders regarding the effectiveness of cardiopulmonary resuscitation. Circulation. 2008;117:704–9. doi: 10.1161/CIRCULATIONAHA.107.188486. [DOI] [PubMed] [Google Scholar]
- 31.Krieger N, Chen JT, Waterman PD, Soobader MJ, Subramanian SV, Carson R. Geocoding and monitoring of US socioeconomic inequalities in mortality and cancer incidence: does the choice of area-based measure and geographic level matter? Am J Epidemiol. 2002;156:471–82. doi: 10.1093/aje/kwf068. [DOI] [PubMed] [Google Scholar]
- 32.Diez-Roux AV. Multilevel analysis in public health research. Annu Rev Public Health. 2000;21:171–92. doi: 10.1146/annurev.publhealth.21.1.171. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.