Abstract
Objectives
To compare the efficacy of beta-blockers (BB) in congenital long QT syndrome (LQTS).
Background
BB are the mainstay in managing LQTS. Studies comparing the efficacy of commonly-used BB are lacking and clinicians generally assume they are equally effective.
Methods
ECG and clinical parameters of 382 LQT1/LQT2 patients initiated on propranolol (n=134), metoprolol (n=147), and nadolol (n=101) were analyzed, excluding patients aged <1 year at BB initiation. Symptoms prior to therapy and the first breakthrough cardiac events (BCEs) were documented.
Results
Patients (56% females, 27% symptomatic, HR 76±16 bpm, QTc 472±46 ms) were started on BB therapy at a median age of 14 years (IQR 8–32 years). QTc-shortening with propranolol was significantly greater than with other BB in the total cohort and in the subset with QTc >480 ms. None of the asymptomatic patients had BCEs. Among symptomatic patients (n=101), 15 had BCEs (all syncopes). QTc-shortening was significantly less-pronounced among patients with BCEs. There was a greater risk of BCEs for symptomatic patients initiated on metoprolol compared to users of other two BB combined, after adjustment for genotype (OR 3.95, 95% CI 1.2–13.1, p=0.025). Kaplan-Meier analysis showed a significantly lower event-free survival for symptomatic patients on metoprolol compared to propranolol/nadolol.
Conclusions
Propranolol has a significantly better QTc-shortening effect compared to metoprolol and nadolol, especially in patients with prolonged QTc. Propranolol and nadolol are equally effective whereas symptomatic patients started on metoprolol are at a significantly higher risk for BCEs. Metoprolol should not be used in symptomatic LQT1 and LQT2 patients.
Keywords: congenital long QT syndrome, propranolol, metoprolol, nadolol, breakthrough cardiac events
INTRODUCTION
Congenital long QT syndrome (LQTS) is a primary inherited arrhythmia syndrome associated with an increased propensity to arrhythmogenic syncope and sudden death. Abnormal cardiac repolarization evident as prolonged QT interval on the electrocardiogram (ECG) is the signature feature of LQTS. Since the 70’s beta-blockers have been the mainstay in managing this disorder primarily because the trigger for most life-threatening arrhythmias is a sudden increase in sympathetic activity, especially in LQT1 and LQT2 patients.1,2
The efficacy of beta-blockers in reducing LQTS-associated cardiac events is established.3,4 Propranolol, the prototypic beta-blocking agent, has been studied most extensively and was shown to either decrease or prevent an increase in transmural dispersion of repolarization in response to strong sympathetic stimulation, a mechanism contributing to its antiarrhythmic effect.5 While several studies have clearly demonstrated a very favorable response to beta-blockers in symptomatic LQTS patients, it is also evident that 20%–30% of previously symptomatic patients experience a breakthrough cardiac event (BCE) while receiving beta-blocker therapy.6–8 Concern that not all beta-blockers provide equivalent protection in LQTS and that this could contribute to treatment failure has been expressed in the past.9,10 However, actual comparisons between different beta-blockers are lacking. Recent findings concerning the differential mechanism of action of propranolol and metoprolol on the cardiac sodium (Na+) channel have thrown light on the probable physiology underlying this significant therapeutic aspect.11 The purpose of this study was to compare the efficacy of commonly used beta-blockers in LQTS by comparing the baseline and on-therapy clinical and electrocardiographic characteristics of patients treated with different beta-blockers and by correlating this with the occurrence of BCEs on follow-up.
METHODS
Study population
LQTS patients, index patients and family members, managed at the participating university hospitals were included if they had a genetically confirmed LQT1 or LQT2 mutation, were initiated on therapy with beta-blockers and had at least one pre-therapy (baseline) and one on-therapy ECG for review. Patients diagnosed with LQTS and initiated on beta-blocker therapy in their first year of life were not included in the study. Patients with LQT3–13 or multiple mutations were not included. Patients lost to follow-up after initial evaluation (n=9) and those with history of QTc-prolonging drug intake at the time of baseline evaluation (n=3) were excluded from the study. A total of 382 patients started on therapy with propranolol (n=134), metoprolol (n=147), and nadolol (n=101) were included. We did not include patients treated with other beta-blockers because of small patient numbers which might have led to incorrect inferences.
Data collection and management
Demographic data and details of personal and family history were obtained for all patients. Syncope (defined as transient loss of consciousness that was abrupt in onset and offset), near drowning, seizure episodes with associated loss of consciousness and aborted cardiac arrest (ACA, requiring external defibrillation as part of resuscitation) were considered pertinent LQTS-related symptoms. The last ECG prior to initiation of beta-blockers (baseline) and the first available ECG after initiation of therapy (on-therapy) were retrieved for analysis and the time interval between the two was documented.
ECG analyses were performed by experienced physicians blinded to therapy details. The QT interval was measured manually from the beginning of the QRS complex to the end of the T wave in lead II or V5. The end of the T wave was determined as the intersection point between the isoelectric baseline and the tangent representing the maximal downward slope of the positive T wave or maximal upward slope of the negative T wave. The mean of three consecutive QT intervals was used. Corrected QT interval (QTc) was obtained using Bazett’s formula. For purposes of this study, QTc was considered normal if ≤450 milliseconds (ms), borderline if 451–480 ms and prolonged if >480 ms.
Follow-up data on beta-blockers included the initiation date, date of switch to another beta-blocker (considering first switch if switched more than once), date of beta-blocker discontinuation (if applicable) and details of BCEs if any. BCE was defined as syncope, ACA, appropriate implantable cardioverter defibrillator (ICD) shock or sudden cardiac death (SCD) occurring while receiving beta-blockers, taking into account the first BCE for subjects with multiple BCEs. Beta-blocker compliance and the non-usage of other QT-prolonging drugs at the time of the BCEs had been verified by the caring physicians. BCEs occurring at a time of admitted non-compliance were not included. Details of ancillary LQTS therapy with ICD, pacemaker and/or surgical left cardiac sympathetic denervation (LCSD) were documented.
Statistical analysis
Continuous variables are presented as mean ± standard deviation (SD) and analysed by t-test for independent or paired samples, as appropriate, and by 1-way analysis of variance (ANOVA), according to the number of groups compared, with Bonferroni correction for multiple comparison. Whenever the distribution was skewed, continuous variables, presented as median and interquartile range (IQR), were compared by Mann-Whitney and Kruskal-Wallis tests. Categorical variables are presented as number of patients (n) and/or percentage (%) and analysed by chi-squared test. Adjusted odds-ratio (OR) with 95% CI was estimated from a multivariate logistic regression model used to determine the association between beta-blockers and occurrence of BCEs in previously symptomatic patients, while controlling for genotype. Kaplan-Meier analysis, with log-rank test for comparisons, was used to estimate the cumulative event-free survival of symptomatic patients, taking the first BCE as the endpoint. However, if beta-blocker switch occurred prior to BCE, censoring was done at the time of switch. In patients without a BCE, censoring was done at the time of beta-blocker switch or at the time of beta-blocker discontinuation or at the time of the study, whichever came first. All analyses were performed using SPSS 18.0 (SPSS Inc., Chicago, IL) and a p<0.05 was considered statistically significant.
RESULTS
Clinical characteristics of the study subjects (n=382) started on the different beta-blockers are provided in Table 1. Females constituted 56% of the study population. Symptoms prior to treatment were present in 27% of the subjects with syncope being the most common symptom. There were more LQT1 (54%) than LQT2 patients (46%) in the total cohort. The distribution of gender, genotype and symptomatic patients was different among the beta-blocker groups. The baseline heart-rate of the study population was 76±16 bpm and was comparable among the beta-blocker groups; the baseline QTc was 472±46 ms and was different among the beta-blocker groups. Median age at beta-blocker initiation was 14 years (IQR 8–32 years) in the total cohort, and differed among the 3 groups. The on-therapy heart-rate and QTc were different compared to the baseline heart-rate and QTc within each beta-blocker group, respectively (p<0.001 for all paired comparisons). However, while the change in heart-rate with beta-blocker initiation was comparable among the groups (p=0.9), the change in QTc with propranolol was greater than that with metoprolol (p=0.003) and nadolol (p=0.004). Median initial beta-blocker dosages documented at the time of on-therapy ECG were 1.8 mg/kg/day (IQR 1.2–2 mg/kg/day) of propranolol, 0.9 mg/kg/day (IQR 0.7–1.6 mg/kg/day) of metoprolol and 0.9 mg/kg/day (IQR 0.7–1.2 mg/kg/day) of nadolol. Regular propranolol was used in 99% of propranolol users and sustained-release metoprolol in 90% of metoprolol users.
Table 1.
Clinical characteristics of patients based on initial beta-blocker
| Total n = 382 |
Propranolol n = 134 |
Metoprolol n = 147 |
Nadolol n = 101 |
p | |
|---|---|---|---|---|---|
| Females, n (%) | 215 (56) | 65 (49) | 94 (64) | 56 (55) | 0.03 |
| Symptoms prior to therapy | |||||
| Syncope, n (%) | 90 (24) | 46 (34) | 30 (20) | 14 (14) | 0.001 |
| ACA, n (%) | 11 (3) | 5 (4) | 5 (3) | 1 (1) | 0.4 |
| Genotype | <0.001 | ||||
| LQT1, n (%) | 207 (54) | 79 (59) | 59 (40) | 69 (68) | |
| LQT2, n (%) | 175 (46) | 55 (41) | 88 (60) | 32 (32) | |
| Baseline HR, bpm | 76 ± 16 | 78 ± 18 | 75 ± 15 | 74 ± 13 | 0.06 |
| Baseline QTc, ms | 472 ± 46 | 480 ± 47* | 469 ± 49 | 465 ± 40 | 0.03 |
| Median age at start of BB (IQR), years | 14 (8–32) | 10 (6–22) | 21 (11–38) | 14 (9–30) | <0.001 |
| On-therapy HR, bpm | 64 ± 14 | 67 ± 16 | 64 ± 12 | 62 ± 13 | 0.05 |
| On-therapy QTc, ms | 454 ± 39 | 453 ± 37 | 456 ± 44 | 452 ± 34 | 0.8 |
| Median TI (IQR), months | 8 (4–13) | 8 (3–13) | 6 (3–13) | 12 (8–14) | <0.001 |
| ΔHR, bpm | 11 ± 12 | 12 ± 12 | 11 ± 12 | 11 ± 12 | 0.9 |
| ΔQTc, ms | 18 ± 34 | 27 ± 38† | 14 ± 34 | 12 ± 28 | 0.001 |
p<0.05 vs. nadolol;
p<0.01 vs. metoprolol and vs. nadolol; ACA, aborted cardiac arrest; BB, beta-blocker; HR, heart rate; IQR, interquartile range; TI, time interval between baseline and on-therapy ECG; Δ, change in ECG parameter with BB initiation
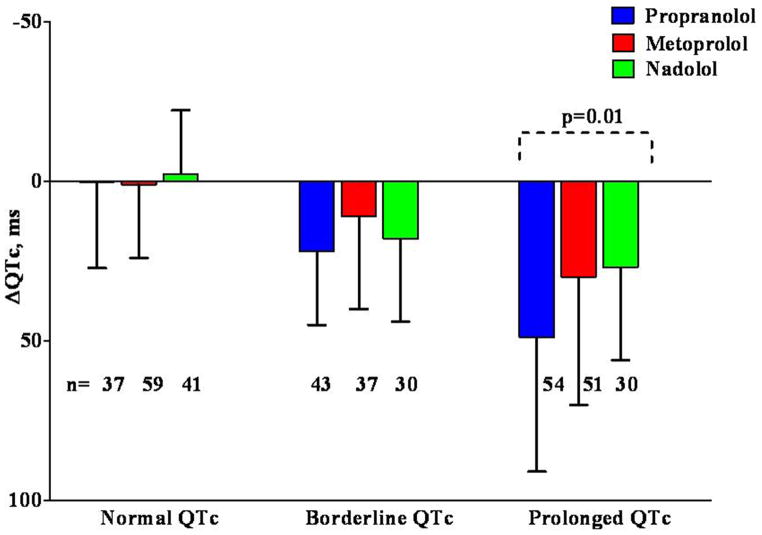
QTc-shortening based on baseline QTc
Given the longer baseline QTc in the propranolol group compared to the other groups, and the appearance of dependence of QTc-shortening on the baseline QTc, all subjects were further subdivided based on whether the baseline QTc was normal (≤450 ms), borderline (451–480 ms) or prolonged (>480 ms) (Figure 1). The baseline heart-rate differed among beta-blocker groups within the normal QTc subset and the age at therapy initiation differed within the normal and prolonged QTc subsets. Now, the baseline QTc was expectedly comparable within all 3 QTc subsets. QTc-shortening with propranolol, metoprolol and nadolol in the normal QTc subset (0±27 ms, 1±23 ms, −2±20 ms, p=0.8) and in the borderline QTc subset (22±23 ms, 11±29 ms, 18±26 ms, p=0.2) were comparable but was significantly different in the prolonged QTc subset (49±42 ms, 30±40 ms, 27±29 ms, p=0.01). Bonferroni test showed the QTc-shortening with propranolol to be different from that with metoprolol (p=0.04) and nadolol (p=0.04) in the prolonged QTc subset.
Figure 1.
Effect of baseline QTc on QTc-shortening.
Baseline QTc was taken as normal if ≤450 ms, borderline if 451–480 ms and prolonged if >480 ms. Δ indicates change in ECG parameter with beta-blocker initiation.
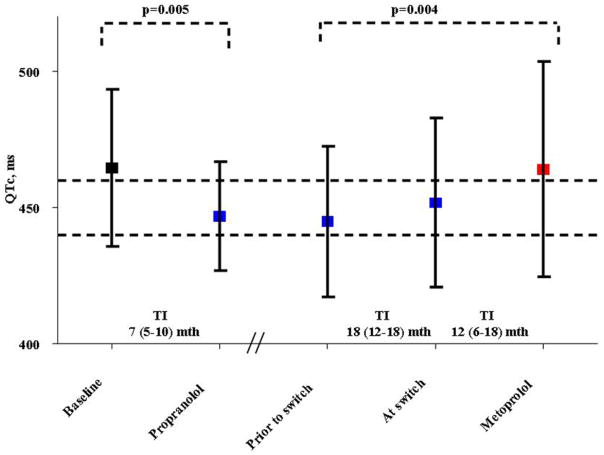
Progression of QTc in subjects switched from propranolol to metoprolol
A subset of patients (n=14, from two participating centres) initiated on propranolol and switched to metoprolol during follow-up were retrospectively analyzed to study QTc progression (Figure 2). In this subset, there were 11 LQT1 and 3 LQT2 patients. Median age at start of propranolol was 6 years (IQR 6–7 years) and median age at switch to metoprolol was 11 years (IQR 9–13 years). On-therapy QTc (447±20 ms) with propranolol measured at a median time of 7 months (IQR 5–10 months) after initiation differed significantly from the baseline QTc (465±29 ms, p=0.005). QTc (464±39 ms) on metoprolol measured at a median time of 12 months (IQR 6–18 months) after the switch was significantly longer than the QTc (445±28 ms) on propranolol measured at a median time of 18 months (IQR 12–18 months) prior to the switch (p=0.004).
Figure 2.
Progression of QTc (mean ± SD) with initiation of propranolol and subsequent switch to metoprolol in a subset of 14 patients.
‘Baseline’ indicates QTc immediately prior to initiation of propranolol therapy; ‘Propranolol’ indicates first QTc measurement on propranolol; ‘Prior to switch’, QTc on propranolol prior to switch; ‘At switch’, QTc on propranolol at the time the decision to switch was made; ‘Metoprolol’, QTc on metoprolol after switch; TI, time interval in months.
Comparison of LQT1 and LQT2 subjects
A similar proportion of LQT1 and LQT2 subjects were symptomatic prior to therapy (Table 2). While baseline heart-rate was comparable between the genotypes, LQT2 subjects had a longer baseline QTc (p=0.01) than LQT1 subjects. Age at beta-blocker initiation was greater (p=0.04) in LQT2 subjects. Overall QTc-shortening and that due to initiation of propranolol, metoprolol and nadolol were comparable between the genotypes.
Table 2.
Clinical characteristics of patients based on genotype
| LQT1 n = 207 |
LQT2 n = 175 |
p | |
|---|---|---|---|
| Symptoms prior to therapy, n (%) | 56 (27) | 45 (26) | 0.8 |
| Baseline HR, bpm | 77 ± 15 | 74 ± 16 | 0.08 |
| Baseline QTc, ms | 467 ± 42 | 478 ± 50 | 0.01 |
| Median age at start of BB (IQR), years | 12 (7–30) | 18 (10–34) | 0.04 |
| ΔHR, bpm | 11 ± 12 | 11 ± 12 | 0.9 |
| ΔQTc, ms | 18 ± 32 | 18 ± 37 | 0.9 |
| ΔQTc with propranolol, ms | 25 ± 35 | 29 ± 43 | 0.6 |
| ΔQTc with metoprolol, ms | 16 ± 29 | 12 ± 37 | 0.5 |
| ΔQTc with nadolol, ms | 11 ± 30 | 14 ± 22 | 0.6 |
BB, beta-blocker; HR, heart rate; IQR, interquartile range; Δ, change in ECG parameter with BB initiation
Analysis of occurrence of BCEs based on symptoms prior to treatment
Among asymptomatic subjects (n=281), 30% were initiated on propranolol, 40% on metoprolol and 30% on nadolol. There were no BCEs documented during a median follow-up period of 6 years (IQR 2–10 years) on propranolol, 6 years (IQR 3–9 years) on metoprolol and 4 years (IQR 3–6 years) on nadolol.
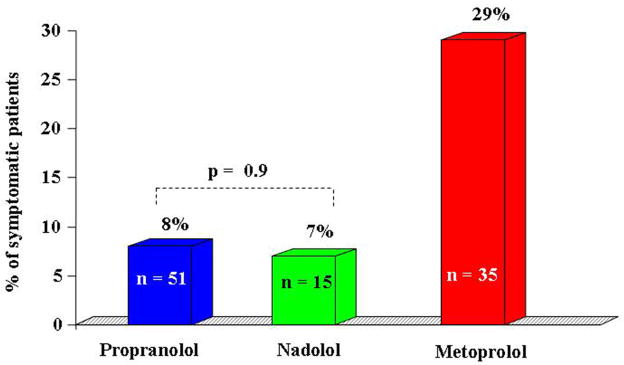
The clinical characteristics of previously symptomatic (n=101) subjects initiated on the 3 beta-blockers are shown in Table 3. Gender, genotype and age at beta-blocker initiation were comparable among the subjects in the 3 beta-blocker groups in this cohort of patients with symptoms prior to treatment. With baseline and on-therapy ECG parameters being comparable, there was an overall significant difference (p=0.018) in the occurrence of BCEs among the 3 beta-blocker groups (Figure 3). All 15 BCEs were syncopes. Median beta-blocker dosages documented at the time of BCEs were 2.5 mg/kg/day (IQR 1.3–3 mg/kg/day) of propranolol and 1.4 mg/kg/day (IQR 0.9–2.5 mg/kg/day) of metoprolol. The only one patient who suffered a BCE while on nadolol therapy was receiving a dose of 0.8 mg/kg/day. BCEs were more frequent among patients using regular metoprolol at a twice-daily dosing than among patients using sustained-release metoprolol at once-a-day dosing (18% vs. 5%, p=0.04). There was only one SCD which, however, did not occur as a first BCE: a previously symptomatic LQT1 male patient initiated on propranolol at age 5 years was switched to metoprolol at the age of 8 years. He experienced a syncope (first BCE) at the age of 11 years while playing football and died a few months later due to an out-of-hospital cardiac arrest (second BCE) while swimming, still under therapy with metoprolol.
Table 3.
Clinical characteristics of symptomatic subjects based on initial beta-blocker
| Total n = 101 |
Propranolol n = 51 |
Metoprolol n = 35 |
Nadolol n = 15 |
p | |
|---|---|---|---|---|---|
| Females, n (%) | 73 (72) | 36 (71) | 26 (74) | 11 (73) | 0.9 |
| LQT1, n (%) | 56 (55) | 32 (62) | 14 (41) | 10 (67) | 0.07 |
| Baseline HR, bpm | 74 ± 14 | 74 ± 14 | 75 ± 14 | 69 ± 11 | 0.3 |
| Baseline QTc, ms | 499 ± 51 | 502 ± 52 | 497 ± 48 | 493 ± 54 | 0.8 |
| Median age at start of BB, (IQR), years | 22 (10–34) | 18 (8–34) | 25 (17–38) | 22 (9–32) | 0.2 |
| On-therapy HR, bpm | 62 ± 12 | 63 ± 14 | 61 ± 9 | 60 ± 13 | 0.7 |
| On-therapy QTc, ms | 474 ± 41 | 469 ± 40 | 478 ± 44 | 478 ± 35 | 0.5 |
| Median TI (IQR), months | 6 (3–17) | 8 (3–16) | 5 (2–17) | 8 (3–20) | 0.7 |
| ΔHR, bpm | 12 ± 12 | 11 ± 12 | 14 ± 12 | 9 ± 9 | 0.3 |
| ΔQTc, ms | 26 ± 37 | 33 ± 39 | 19 ± 37 | 15 ± 28 | 0.1 |
| BCEs, n (%) | 15 (15) | 4 (8) | 10 (29) | 1 (7) | 0.02 |
TI, time interval between baseline and on-therapy ECG; BB, beta-blocker; BCEs, breakthrough cardiac events; HR, heart rate; IQR, interquartile range; Δ, change in ECG parameter with BB initiation
Figure 3.
Occurrence of BCEs in patients with symptoms prior to therapy.
BCEs occurred in 8% of patients on propranolol, 7% of patients on nadolol, and 29% of patients on metoprolol.
As expected, the use of ICD (18% vs. 0.4%, p<0.001), pacemakers (3% vs. 0.7%, p=0.09) and LCSD (7% vs. 0, p<0.001) differed between symptomatic and asymptomatic individuals.
Comparison of symptomatic subjects with and without BCEs
Gender, baseline heart-rate, baseline QTc and age at therapy initiation were comparable between symptomatic patients with and without BCEs (Table 4). However, symptomatic LQT2 patients had more BCEs compared to symptomatic LQT1 patients (p=0.02). Also, patients with BCEs had lesser QTc-shortening (p=0.02) than those without BCEs. Median follow-up time on the initial beta-blocker among symptomatic subjects was 2 years (IQR 1–6 years) for propranolol, 4 years (IQR 2–8 years) for metoprolol and 3 years (IQR 2–5 years) for nadolol (p=0.4).
Table 4.
Comparison of symptomatic patients based on occurrence of BCEs on initial beta-blocker
| BCEs on initial BB | p | ||
|---|---|---|---|
| Yes n = 15 |
No n = 86 |
||
| Females, n (%) | 11 (73) | 62 (72) | 0.9 |
| Genotype | 0.02 | ||
| LQT1, n (%) | 4 (27) | 52 (60) | |
| LQT2, n (%) | 11 (73) | 34 (40) | |
| Baseline HR, bpm | 72 ± 11 | 74 ± 14 | 0.6 |
| Baseline QTc, ms | 488 ± 42 | 501 ± 52 | 0.3 |
| Median age at start of BB (IQR), years | 17 (14–26) | 22 (10–34) | 0.8 |
| ΔHR, bpm | 12 ± 12 | 12 ± 11 | 0.9 |
| ΔQTc, ms | 4 ± 24 | 30 ± 38 | 0.02 |
BB, beta-blocker; BCEs, breakthrough cardiac events; HR, heart rate; IQR, interquartile range; Δ, change in ECG parameter with BB initiation
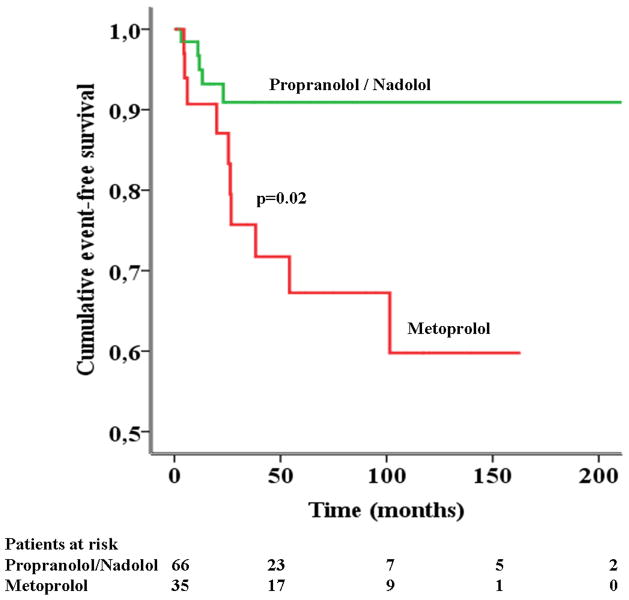
Figure 3 shows that the occurrence of BCEs was significantly different according to the initial beta-blocker used. Indeed, while the proportion of BCEs was almost identical (p=0.9) for symptomatic patients initiated on propranolol (8%) and nadolol (7%), it strikingly increased to 29% for those initiated on metoprolol. This corresponded to a substantially greater risk of suffering a BCE for symptomatic patients initiated on metoprolol compared to those started on either of the other two beta-blockers combined together (OR 3.95, 95% CI 1.2–13.1, p=0.025), after adjusting for genotype. Consequently, the Kaplan-Meier analysis plotting symptomatic patients initiated on metoprolol (n=35) against those initiated on propranolol and nadolol combined (n=66) showed a significant difference (p=0.02) in the cumulative event-free survival of the patients (Figure 4). Indeed, by 10 years on beta-blocker therapy, the cumulative event-free survival for propranolol / nadolol users was 91% compared to 60% for metoprolol users.
Figure 4.
Kaplan-Meier estimates of event-free survival of symptomatic patients initiated on different beta-blockers.
The cumulative event-free survival of symptomatic patients initiated on metoprolol (n=35) was significantly different (p=0.02) from those initiated on propranolol and nadolol combined (n=66).
DISCUSSION
Contrary to the currently prevailing views, in the management of LQTS, not all beta-blockers are equal. The main finding of the present study is that symptomatic patients treated with metoprolol are 4 times more likely to suffer BCEs than those treated with propranolol and nadolol. This finding will unavoidably impact the clinical management of LQTS. The other major finding of this study is the evidence for a correlation between the antiarrhythmic efficacy of beta-blockers and their ability to shorten the QT interval.
LQTS, beta-blockers, Na+ channel block and QTc-shortening
LQTS is a genotypically and phenotypically heterogeneous disease. The mortality rate among untreated symptomatic LQTS patients was as high as 60%–65% when the first assessment of the beneficial effect of beta-blockers in a large group of patients was made in 1975.1 Since then, beta-blockers, the mainstay of therapy in LQTS, have been highly effective in reducing mortality.4,10 While propranolol and nadolol are non-selective beta-blockers, metoprolol is relatively beta-1 cardio-selective. The largest experience with beta-blockers in LQTS has been that with propranolol. Its main advantages are the good tolerability and the lipophilia that allows it to cross the blood brain barrier while the need for multiple daily dosing due to its rapid metabolization is the prime disadvantage. Although long-acting, sustained-release preparations of propranolol exist, they are not available in a form suitable for use in children. To overcome the inconvenient dosing schedule with propranolol, an increasing number of patients have been treated with longer-acting beta-blockers like nadolol and sustained-release metoprolol. Ancillary LQTS therapy in the form of ICD, pacemaker and/or LCSD is reserved for patients with symptoms despite beta-blockers and for high-risk patients.12 Additionally, when non-selective beta-blockers are contraindicated such as in asthma patients, LCSD has been performed with excellent results (unpublished data).
In some of the participating centres it is common practice to initiate treatment with propranolol or nadolol (based on availability) in young children mainly due to their proven safety in this age group of patients. Propranolol-users are quite often switched to another beta-blocker during adolescence to optimize compliance. Similarly, sustained-release metoprolol is used as the initial beta-blocker in adults mainly due to its dosing convenience. These policies explain to some extent the lesser age at therapy-initiation for propranolol and nadolol compared to metoprolol. We consider the difference in baseline QTc to have been an effect of these age-based choices rather than being an underlying reason for therapeutic decision-making.
Initial concern that all beta-blockers are not equally protective in LQTS and therefore should not be viewed as equivalent choices was raised by Chatrath et al9 but the small size of that study has limited its impact. The current practice is that physicians typically choose a beta-blocker based on personal experience and then make appropriate changes based on side-effects and dosing preferences.
Both beta-adrenoceptor blocking properties and non-beta-adrenoceptor-mediated actions of propranolol have been proposed to contribute to the antiarrhythmic actions of propranolol.13 While the Na+ channel-blocking efficacy of propranolol has been known for long, a recent study has demonstrated that its blocking effect is particularly more on the late non-inactivating Na+ current than on the peak Na+ current, an effect not seen with metoprolol.11 There were no data available on nadolol earlier but, quite recently, it has been found that nadolol has a ~20% non use-dependent blocking effect on peak Na+ current and no effect on the late current whereas metoprolol has no effect on either the peak or late current.14 Analysis of the biophysical properties of the channel revealed that both nadolol and propranolol cause hyperpolarizing shifts on voltage-dependence of activation and steady-state inactivation whereas metoprolol shifts only the activation curve. These biophysical data clearly explain the differences between propranolol and metoprolol, and provide a partial explanation for the difference between nadolol and metoprolol. Also, the mechanism of the similar clinical efficacy of nadolol and propranolol is not fully understood.
It is clear that in addition to the membrane-stabilizing effect of propranolol and nadolol brought about by peak Na+ current blockade, propranolol has a pronounced late non-inactivating Na+ current blocking ability which contributes directly to shortening of the action potential duration and thereby the QTc. The association between QTc-shortening and reduction in cardiac events has been shown in earlier studies4 and is confirmed by the present study. Though beta-blockers do not seem to act on the cardiac potassium channels which are dysfunctional in LQT1 and LQT2, their aforementioned properties are likely to contribute to a major extent to the drastic reduction in cardiac events in LQT1 and LQT2 patients. The clinical implication of these findings is that prolonged cardiac repolarization in LQTS is shortened more effectively by propranolol than by metoprolol, as the present study confirms. Indeed, by comparing all patients based on their initial beta-blocker, we observed that propranolol had a significantly better QTc-shortening effect compared to metoprolol and nadolol. Furthermore, by grouping subjects based on baseline QTc, the differences in baseline parameters were reduced and we were able to make comparisons in more homogenous patient subgroups. The pronounced QTc-shortening effect of propranolol in comparison to that of metoprolol and nadolol in subjects with QTc >480 ms can be explained by the fact that the net late Na+ inward current is largest when the action potential duration is longer.
LQTS and efficacy of beta-blockers
Gender, QTc and the locus of causative mutation have all been identified as factors influencing the clinical course of LQTS patients.2,15 In the present study, the type of LQTS (LQT1 or LQT2) did not influence the occurrence of symptoms prior to treatment nor did it affect the QTc-shortening with beta-blocker initiation. The occurrence of BCEs was significantly influenced by the occurrence of cardiac symptoms prior to therapy, confirming previous observations.16 While there were no BCEs among asymptomatic patients, 15% of symptomatic patients had BCEs while still on the initial beta-blocker. LQT2 genotype and modest QTc-shortening with beta-blockers were risk factors for BCEs in this group of patients. Goldenberg et al17 have shown that male patients with LQT1 in the <14 years age-group and female patients with LQT2 in the 15–40 years age-group are at a high risk for cardiac events and that the risk-reduction with beta-blockers is significantly high in both groups of patients. The present study, performed with this cross-over phenomenon in mind, has analyzed the occurrence of BCEs only in the previously symptomatic patients with comparable baseline characteristics. The clinically important finding of our study is that the incidence of first BCEs was rather low, did not include lethal events, and was almost identical among patients receiving propranolol (8%) and nadolol (7%) whereas it was unacceptably high (29%) among those treated with metoprolol. Given the evidence that patients with syncope during beta-blocker therapy are those at a truly high risk of life-threatening events,18 this finding carries significant clinical implications in the management of young symptomatic LQTS patients.
Study limitations
Although this is to the best of our knowledge the largest multicentre study to date comparing the efficacy of commonly used beta-blockers in LQTS, it has the inherent limitation of a retrospective study namely lack of homogeneity among patients treated with different beta-blockers. However, grouping patients based on their baseline QTc enabled comparison of the QTc-shortening produced by beta-blockers in more homogeneous subgroups of patients. Further, among previously symptomatic patients, where baseline parameters such as gender, genotype, heart-rate, QTc and age at therapy initiation were all comparable, we were able to compare the incidence of BCEs which was found to be significantly more in patients initiated on one of the beta-blockers. The multivariate logistic regression analysis allowed confirmation of the higher risk of BCEs among metoprolol-users even after adjusting for genotype. However, the relatively small number of patients with BCEs and the possibility of residual confounding are recognized as limitations of this study.
CONCLUSIONS
This multicenter study on LQTS patients receiving beta-blocker therapy has shown for the first time that propranolol and nadolol are significantly more effective than metoprolol in preventing BCEs in symptomatic patients. Also, propranolol was superior to both nadolol and metoprolol in terms of shortening the cardiac repolarization time, particularly in high-risk patients with markedly prolonged QTc. Symptomatic patients with BCEs had significantly less QTc-shortening than the event-free patients. As we have documented an increased risk for symptomatic patients to suffer BCEs with metoprolol, we recommend treatment of symptomatic LQT1 and LQT2 patients with either propranolol or nadolol, as clearly not all beta-blockers are equal in their antiarrhythmic efficacy in LQTS.
Acknowledgments
Sources of Funding: Dr. Wilde’s and Dr. Kääb’s research programs are supported by the Leducq program grant Alliance Against Sudden Cardiac Death (CVR05). Dr. Schwartz’s and Dr. Crotti’s research programs are supported by NIH grant HL083374 and Telethon grant GGP09247. Dr.Spazzolini’s work is partly supported by Fondazione IRCCS Policlinico S. Matteo, Pavia, Italy.
Abbreviations
- ACA
aborted cardiac arrest
- ANOVA
analysis of variance
- BCE
breakthrough cardiac event
- CI
confidence interval
- ECG
electrocardiogram
- ICD
implantable cardioverter defibrillator
- IQR
interquartile range
- LCSD
left cardiac sympathetic denervation
- LQTS
congenital long QT syndrome
- LQT1
congenital long QT syndrome type 1
- LQT2
congenital long QT syndrome type 2
- OR
odds ratio
- QTc
heart rate corrected QT interval
- SCD
sudden cardiac death
- SD
standard deviation
Footnotes
Disclosures: Dr. Wilde is a member of the scientific advisory board of Transgenomics and Sorin. Dr. Ackerman is a consultant for Biotronik, Boston Scientific, Medtronic, PGx Health and St. Jude Medical; and has intellectual property in PGx Health.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Schwartz PJ, Periti M, Malliani A. The long Q-T syndrome. Am Heart J. 1975;89:378–90. doi: 10.1016/0002-8703(75)90089-7. [DOI] [PubMed] [Google Scholar]
- 2.Moss AJ, Shimizu W, Wilde AA, et al. Clinical aspects of type-1 long-QT syndrome by location, coding type, and biophysical function of mutations involving the KCNQ1 gene. Circulation. 2007;115:2481–9. doi: 10.1161/CIRCULATIONAHA.106.665406. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Schwartz PJ. Idiopathic long QT syndrome: Progress and Questions. Am Heart J. 1985;109:399–411. doi: 10.1016/0002-8703(85)90626-x. [DOI] [PubMed] [Google Scholar]
- 4.Moss AJ, Zareba W, Hall WJ, et al. Effectiveness and limitations of beta-blocker therapy in congenital long-QT syndrome. Circulation. 2000;101:616–23. doi: 10.1161/01.cir.101.6.616. [DOI] [PubMed] [Google Scholar]
- 5.Shimizu W, Tanabe Y, Aiba T, et al. Differential effects of beta-blockade on dispersion of repolarization in the absence and presence of sympathetic stimulation between the LQT1 and LQT2 forms of congenital long QT syndrome. J Am Coll Cardiol. 2002;39:1984–91. doi: 10.1016/s0735-1097(02)01894-6. [DOI] [PubMed] [Google Scholar]
- 6.Priori SG, Napolitano C, Schwartz PJ, et al. Association of long QT syndrome loci and cardiac events among patients treated with beta-blockers. JAMA. 2004;292:1341–44. doi: 10.1001/jama.292.11.1341. [DOI] [PubMed] [Google Scholar]
- 7.Villain E, Denjoy I, Lupoglazoff JM, et al. Low incidence of cardiac events with beta-blocking therapy in children with long QT syndrome. Eur Heart J. 2004;25:1405–11. doi: 10.1016/j.ehj.2004.06.016. [DOI] [PubMed] [Google Scholar]
- 8.Vincent GM, Schwartz PJ, Denjoy I, et al. High efficacy of beta-blockers in long-QT syndrome type 1: contribution of noncompliance and QT-prolonging drugs to the occurrence of beta-blocker treatment “failures”. Circulation. 2009;119:215–21. doi: 10.1161/CIRCULATIONAHA.108.772533. [DOI] [PubMed] [Google Scholar]
- 9.Chatrath R, Bell CM, Ackerman MJ. Beta-blocker therapy failures in symptomatic probands with genotyped long-QT syndrome. Pediatr Cardiol. 2004;25:459–65. doi: 10.1007/s00246-003-0567-3. [DOI] [PubMed] [Google Scholar]
- 10.Schwartz PJ. The congenital long QT syndromes from genotype to phenotype: clinical implications. J Intern Med. 2006;259:39–47. doi: 10.1111/j.1365-2796.2005.01583.x. [DOI] [PubMed] [Google Scholar]
- 11.Bankston JR, Kass RS. Molecular determinants of local anesthetic action of beta-blocking drugs: Implications for therapeutic management of long QT syndrome variant 3. J Mol Cell Cardiol. 2010;48:246–53. doi: 10.1016/j.yjmcc.2009.05.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Schwartz PJ, Crotti L, Insolia R. Arrhythmognic disorders of genetic origin: long QT syndrome: from genetics to management. Circ Arrhythm Electrophysiol. 2012 doi: 10.1161/circep.111.962019. [In press] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Duff HJ, Mitchell LB, Wyse DG. Antiarrhythmic Efficacy of Propranolol: Comparison of Low and High Serum Concentrations. J Am Coll Cardiol. 1986;8:959–65. doi: 10.1016/s0735-1097(86)80441-7. [DOI] [PubMed] [Google Scholar]
- 14.Besana A, Wang DW, George AL, Schwartz PJ. Nadolol block of Nav 1.5 does not explain its efficacy in the long QT syndrome. J Cardiovasc Pharmacol. 2012;59:249–53. doi: 10.1097/FJC.0b013e31823d2fd1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Shimizu W, Moss AJ, Wilde AAM, et al. Genotype-Phenotype Aspects of Type-2 Long-QT Syndrome. J Am Coll Cardiol. 2009;54:2052–62. doi: 10.1016/j.jacc.2009.08.028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Moss AJ, Schwartz PJ, Crampton RS, et al. The long QT syndrome: prospective longitudinal study of 328 families. Circulation. 1991;84:1136–44. doi: 10.1161/01.cir.84.3.1136. [DOI] [PubMed] [Google Scholar]
- 17.Goldenberg I, Bradley J, Moss A, et al. Beta-blocker efficacy in high-risk patients with the congenital long-QT syndrome types 1 and 2: implications for patient management. J Cardiovasc Electrophysiol. 2010;21:893–901. doi: 10.1111/j.1540-8167.2010.01737.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Jons C, Moss AJ, Goldenberg I, et al. Risk of fatal arrhythmic events in long QT syndrome patients after syncope. J Am Coll Cardiol. 2010;55:783–8. doi: 10.1016/j.jacc.2009.11.042. [DOI] [PubMed] [Google Scholar]