Abstract
Background. Pandemic influenza vaccination rate amongst healthcare workers in England 2009/2010 was suboptimal (40.3%). Targeting medical students before they enter the healthcare workforce is an attractive future option. This study assessed the H1N1 vaccine uptake rate amongst medical students and factors that influenced this. Methods. Anonymised, self-administered questionnaire at a medical school. Results. The uptake rate amongst 126 medical students offered the vaccine was 49.2% and intended uptake amongst 77 students was 63.6%. Amongst those offered the vaccine, the strongest barriers to acceptance were fear of side effects (67.9%), lack of vaccine information (50.9%), lack of perceived risk (45.3%), and inconvenience (35.8%). Having a chronic illness (OR 3.4 (95% CI 1.2–10.2)), 4th/5th year of study (OR 3.0 (95% CI 1.3–7.1)), and correct H1N1 knowledge (OR 2.6 (95% CI 1.1–6.0)) were positively associated with uptake. Non-white ethnicity was an independent negative predictor of uptake (OR 0.4 (95% CI 0.2–0.8)). Students who accepted the H1N1 vaccine were three times more likely (OR 3.1 (95% CI 1.2–7.7)) to accept future seasonal influenza vaccination. Conclusion. Efforts to increase uptake should focus on routine introduction of influenza vaccine and creating a culture of uptake during medical school years, evidence-based education on vaccination, and improving vaccine delivery.
1. Introduction
The novel influenza A (H1N1) outbreak was declared a pandemic by the World Health Organisation (WHO) on 11th June 2009 [1]. In the United Kingdom (UK), 474 deaths had occurred by the end of the 2009/10 influenza season with the highest case-fatality rate among the over 65-year age group [1, 2]. Vaccination is one of the intervention strategies used to mitigate an influenza pandemic [3, 4]; therefore, as part of the Department of Health (DH) vaccination policy healthcare workers were recommended to receive the H1N1 vaccine to protect themselves, protect patients, and maintain frontline services during the pandemic [5, 6]. At the University of Birmingham, clinical year (3rd–5th year) medical students were also offered the H1N1 vaccine from November 2009 [7].
Influenza vaccination of health care workers (HCW) is known to be effective in preventing seasonal influenza, reducing absenteeism, and protecting patients against nosocomial infection with a resultant decrease in morbidity and mortality [6, 8]. In spite of these benefits, seasonal influenza vaccine uptake among HCW in the UK has traditionally been disappointingly low with uptake of less than 20% in the pre-pandemic year of 2008/2009 in the UK [9]. Similarly low uptake rates have been reported in many other European countries [10]. During the pandemic year, there was a slight increase of HCW seasonal influenza vaccine uptake from 16.5% to 26.4%, while pandemic influenza vaccine uptake among HCW reached 40.3% in the UK [9].
However, vaccine uptake amongst HCW remains suboptimal. It has been frequently found that previous history of seasonal influenza vaccination is a strong predictor of both seasonal and H1N1 vaccine uptake [11–15]. Although no studies have shown a correlation between H1N1 vaccine uptake with subsequent seasonal influenza uptake, figures in England showed an increase in the latter after the H1N1 pandemic [16]. Achieving a high vaccine uptake in the early stages of a medical career might therefore improve subsequent influenza vaccine uptake as suggested by Amodio et al. [17]. Previous studies have shown suboptimal influenza uptake amongst medical students (USA 48% [18], Hong Kong 67% [19]). Since medical students in the UK are not routinely offered the influenza vaccine and nor are there data on their influenza vaccine uptake, the pandemic situation allowed us to determine H1N1 influenza vaccine uptake in this group and identify key factors influencing this. As they are HCW of the future, maximising uptake by addressing barriers in this population may help improve subsequent uptake rates.
2. Materials and Methods
2.1. Study Design
This was a cross-sectional study carried out between February and March 2010 using an anonymised self-completed questionnaire.
2.2. Subjects and Setting
The sample population consisted of 481 out of more than a thousand medical students from the University of Birmingham. 40 subjects were Graduate Entry Course 1 (GEC1) students, 70 were from year 2, 194 from year 3, 60 from year 4 and 117 from year 5. This population was selected and allocated randomly by study group by the Project Scrutiny Committee of the College of Medical and Dental Sciences, University of Birmingham. Initially, a link to the questionnaire was emailed to the allocated sample with a reminder sent after a week. The web-based survey was open for two weeks. Owing to a poor response rate using this method, paper questionnaires were subsequently distributed to the originally allocated sample and to a convenience sample of students that were on similar hospital placement as the authors. These were distributed to the selected year 2 students during their tutorials and to years 3–5 students at their respective hospital placements.
2.3. Influenza Immunisation Programme
Medical students were made aware of the availability of the pandemic influenza vaccine via notices posted on the student notice boards, emails from the hospitals where students were placed and a general email from the medical school. The vaccine was not formally offered to the medical student cohort as a whole, rather it was offered opportunistically by some hospital trusts depending on each hospital's policy.
The hospital trusts allocated a set date, time, and location where medical students could receive the vaccination from trained staff during their hospital placements. Seasonal influenza vaccination was offered simultaneously. Both vaccines were available free of charge.
2.4. Questionnaire
The questionnaire (see the appendix) collected sociodemographic data (age; sex; year of study; history of chronic illness; living with specified groups including children under 16, pregnant woman, over 65's, and healthcare workers), information regarding smoking status, previous seasonal influenza vaccination and adverse reactions, perceived severity of swine flu, reasons for and against H1N1 immunisation, influences affecting immunisation, and three knowledge items related to swine flu. Reasons for and against vaccination were adapted from questionnaires used in previous papers [12, 20, 21]. Participants were prompted to rank three reasons for acceptance or declination and three major influences. Since a significant number of respondents failed to rank their responses, we did not analyse the result according to rank. The questionnaire was piloted prior to the study.
2.5. Outcomes
The primary outcome was receipt of H1N1 vaccine, but for those not offered H1N1 vaccine, there was an option to reply with “intention to vaccinate”.
2.6. Statistical Analysis
Analysis was performed using Statistical Package for the Social Sciences (SPSS) v19. Basic descriptive statistics were performed. In order to identify factors significantly associated with H1N1 uptake, odds ratios and 95% CIs were calculated using binary logistic regression among those offered the vaccine. Factors with a P value < 0.05 and clinical factors known to be associated with vaccine uptake (sex, ethnicity, chronic illness, and year of study) were then entered into multiple logistic regression analysis. Due to small numbers, smoking status was re-categorised into “never” and “ever” smokers and ethnicity as “White” and “Non-white”. For the perception of H1N1 severity question, “Quite severe”, “Severe” and “Very severe” were merged together as “severe.”
3. Results
3.1. Response Rate
We received 31 responses as a result of the initial email. After the reminder, the total number of respondents was 68 (14.1% response rate). After the paper-based approach, where 481 questionnaires were distributed, 137 (28.5%) were returned. The data from both methods were combined for analysis (205, 42.6%). Respondents with incomplete H1N1 vaccination status (2/205) were excluded. In total, 203 (42.2%) entries were included in the study.
3.2. Characteristics of the Survey Respondents
The characteristics of the survey respondents are shown in Table 1. Of the 203 participants, 126 respondents were offered the vaccine whilst 77 were not. The majority were females [n = 148 (72.9%)], and in their third year of medical school [93, [45.8%]]. Previous uptake of seasonal influenza vaccine was low and amongst those who had received vaccine, 20 (28.2%) had suffered side effects. Patterns were largely similar between those who were and were not offered the vaccine, but those offered were largely from year 3 and over, were more likely to be Asian, have a chronic illness and have had seasonal influenza vaccination that season or previous seasons.
Table 1.
Characteristics of respondents.
| Factor | Vaccine offered group, n = 126 (%) |
Vaccine not offered group, n = 77 (%) |
Total n = 203 (%) |
|
|---|---|---|---|---|
| Sex | Male | 34 (27.0) | 20 (26.0) | 54 (26 .6) |
| Female | 92 (73.0) | 56 (72.7) | 148 (72.9) | |
| Missing data | 1 (1.3) | 1 (0.5) | ||
|
| ||||
| Age (mean (SD)) | 21.5 (1.8) | 21.2 (2.4) | 21.4 (2.1) | |
| Missing data | 2 | 2 | 4 | |
|
| ||||
| Ethnicity | White | 77 (61.1) | 63 (81.8) | 140 (69.0) |
| Asian | 28 (22.2) | 9 (11.7) | 37 (18.2) | |
| Chinese | 11 (8.7) | 2 (2.6) | 13 (6.4) | |
| Mixed | 2 (1.6) | 0 (0) | 2 (1.0) | |
| Other | 7 (5.6) | 2 (2.6) | 9 (4.4) | |
| Missing data | 1 (0.8) | 1 (1.3) | 2 (1.0) | |
|
| ||||
| Smoking status | Never smoker | 116 (92.1) | 69 (89.6) | 185 (91.1) |
| Ex-smoker | 3 (2.4) | 2 (2.6) | 13 (6.4) | |
| Smoker | 7 (5.6) | 6 (7.8) | 5 (2.5) | |
|
| ||||
| Chronic illness | No | 107 (84.9) | 70 (90.9) | 177 (87.2) |
| Yes | 19 (15.1) | 7 (9.1) | 26 (12.8) | |
| Asthma | 13 (10.3) | 6 a (7.8) | 19a (9.4) | |
| Other | 6 (4.8) | 4 (5.2) | 9 (4.4) | |
|
| ||||
| Year of study | GECb 1 | 0 (0) | 6 (7.8) | 6 (3.0) |
| Year 2 | 10 (7.9) | 43 (55.8) | 53 (26.1) | |
| Year 3 | 83 (65.9) | 10 (13.0) | 93 (45.8) | |
| Year 4 | 16 (12.7) | 5 (6.5) | 21 (10.3) | |
| Year 5 | 17 (13.5) | 13 (16.9) | 30 (14.8) | |
|
| ||||
| Lives with susceptible individuals | Under 16 | 7 (5.6) | 2 (2.6) | 9 (4.4) |
| Pregnant | 1 (0.8) | 1 (1.3) | 2 (1.0) | |
| Over 65 | 5 (4.0) | 1 (1.3) | 6 (3.0) | |
| HCW | 20 (15.9) | 12 (15.6) | 32 (15.8) | |
| None of the above | 95 (75.4) | 62 (80.5) | 157 (77.3) | |
| Missing data | 1 (0.8) | |||
|
| ||||
| Seasonal influenza vaccination history | Never | 67 (53.2) | 61 (79.2) | 128 (63.1) |
| This year | 35 (27.8) | 5 (6.5) | 40 (19.7) | |
| Previous years | 23 (18.3) | 8 (10.4) | 31 (15.3) | |
| Missing data | 1 (0.8) | 3 (3.9) | 4 (2.0) | |
|
| ||||
| H1N1 vaccine | Accept/would accept | 62 (49.2) | 49 (63.6) | 111 (54.7) |
| Decline | 64 (50.8) | 28 (36.4) | 92 (45.3) | |
|
| ||||
| Knows anyone who contracted H1N1 | No | 32 (27.8) | 28 (36.4) | 60 (29.6) |
| Yes | 94 (74.6) | 49 (63.6) | 143 (70.4) | |
a3 Respondents had both asthma and other chronic illness.
bGEC stands for Graduate Entry Course.
3.3. H1N1 Influenza Vaccination: Intended and Actual Uptake
Of the 126 respondents who were offered the H1N1 vaccine, 62 (49.2% (95% CI 40.2–58.3%)) accepted the vaccine. Of the 77 not offered, 49 (63.6% (95% CI 51.9–74.3%)) stated they would accept the vaccine if offered. Those not offered were significantly more likely (P = 0.046) to state that they would accept the vaccine compared to those offered (OR 1.8 (95% CI 1.01–3.2)).
3.4. Reasons for Acceptance or Declination of Influenza Vaccine
The three most frequently quoted reasons given for acceptance amongst both those offered and not offered the vaccine (although in a slightly different order) were to decrease the likelihood of getting H1N1 (86.2% (50/58) and 77.5% (31/40), respectively), reduce transmission to patients (75.9% (44/58) and 82.5% (33/40)), and to decrease the likelihood of transmission to family members (63.8% (37/58) and 72.5% (29/40)), (Figure 1).
Figure 1.
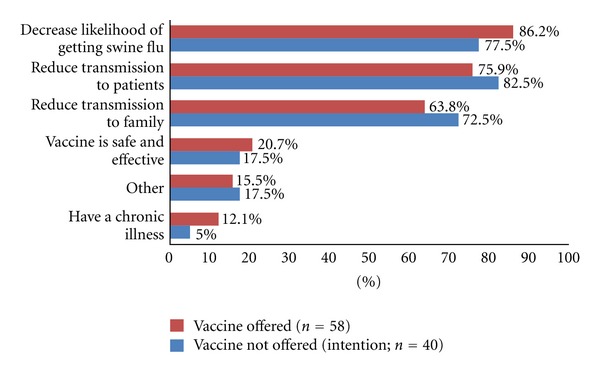
Main reasons for H1N1 vaccine acceptance/intention to be vaccinated among medical students.
The main reason given for declination of the vaccine amongst those offered was worry about side effects (67.9% (36/53)), followed by lack of information about vaccination (50.9% (27/53)) and perceiving they were not at risk (45.3% (24/53)), (Figure 2). However, a further key reason for having been offered but not actually having received the vaccination was “inconvenient timing” (35.8% (19/53)). For those who were not offered the vaccine, the main reasons for intention to decline were perception that they were not at risk (52.2% (12/23)), lack of information (47.8% (11/23)) and worry about side effects (43.5% (10/23)), (Figure 2).
Figure 2.
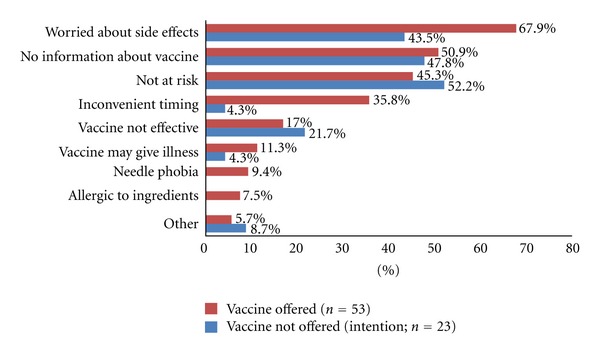
Main reasons for H1N1 vaccine declination/intention to decline among medical students.
The three major reported extrinsic influences affecting actual H1N1 vaccine uptake were medical training (79.4% (81/102)), DH recommendations (52.9% (54/102)) and social influences (50.0% (51/102)). For those who had not been offered the vaccine, they also reported medical training and DH guidelines as important (73.8% (45/61) and 49.2% (30/61), resp.), although the third most important influence cited was the media (39.3% (24/61)) (Figure 3).
Figure 3.
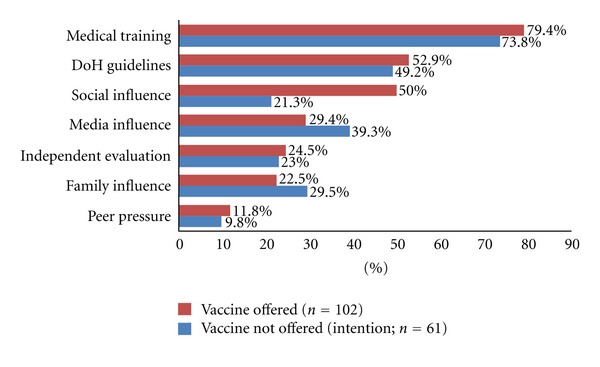
Extrinsic factors affecting H1N1 vaccine uptake/intention to be vaccinated among medical students.
3.5. Knowledge Regarding H1N1 Pandemic
Table 2 describes the students' knowledge and attitudes about the swine flu epidemic. Only a third of the respondents correctly identified all the priority groups (35.5%), and only 23.2% correctly identified methods of H1N1 virus transmission. Almost half of participants (59 (46.8%)) thought the swine flu epidemic was not severe. Level of knowledge and perceived severity were similar across both the students offered and those not offered the vaccine.
Table 2.
Knowledge and attitude of medical students towards the H1N1 pandemic.
| Knowledge questions | Respondents with correct answers, n (%) | |||
|---|---|---|---|---|
| Vaccine-offered group n = 126 (%) |
Vaccine-not-offered group n = 77 (%) |
Total n = 203 (%) |
||
| Priority groups receiving H1N1 vaccine | Answered correctly | 45 (35.7) | 27 (35.1) | 72 (35.5) |
| Over 65 √ a | ||||
| Under 16 | ||||
| Pregnant women √ | ||||
| Healthcare workers √ | ||||
| People with chronic health conditions √
|
||||
|
| ||||
| Methods of transmission of H1N1 virus | Answered correctly | 30 (23.8) | 17 (22.1) | 47 (23.2) |
| Cough/sneezes √ | ||||
| Eating infected meat | ||||
| Direct contact with an infected person √ | ||||
| Touching contaminated object √
|
||||
|
| ||||
| Fatality rate of H1N1 | Answered correctly | 45 (35.7) | 29 (37.7) | 74 (36.5) |
| 0.01% √ | ||||
| 0.1% | ||||
| 1% | ||||
| 10% | ||||
| 20% | ||||
| 50% |
||||
|
| ||||
| Attitude | n = 126 (%) | n = 77 (%) | n = 203 (%) | |
|
| ||||
| Perception of H1N1 severity | Not severe | 59 (46.8) | 35 (45.5) | 94 (46.3) |
| Quite severe/Severe/Very severe | 67 (53.2) | 42 (54.6) | 109 (53.7) | |
a √ Indicates the correct answer for the knowledge questions.
3.6. Determinants of H1N1 Vaccination Uptake
Table 3 presents the factors which affected actual vaccine uptake amongst those offered the vaccine. On univariate analysis, there was no significant difference in uptake between the sexes, amongst smokers compared with ever smokers, or among students living with “at risk” groups. Students of non-white ethnicity were significantly less likely to take up the vaccine (OR 0.4 (95% CI 0.2–0.8)), although those reporting a chronic illness were more likely to do so (OR 3.4 (95% CI 1.2–10.2)). Students in years 4 and 5 were more likely to receive the vaccine (OR 3.0 (95% CI 1.3–7.1)), and those who were correct in at least one of the knowledge questions were also more likely to accept the vaccine (OR 2.6 (95% CI 1.1–6.0)).
Table 3.
Determinants of vaccine uptake in the vaccine offered group.
| Variables | Numbers receiving vaccine (%) | Univariate analysis |
Multivariate analysis: model 1a | Multivariate analysis: model 2 including term for previous seasonal vaccinationb | |
|---|---|---|---|---|---|
| Sex | Male | 14 (22.6) | 1.0 | 1.0 | 1.0 |
| Female | 48 (77.4) | 0.6 (0.3–1.4) | 1.1 (0.4–2.6) | 1.4 (0.4–4.7) | |
|
| |||||
| Ethnicity | White | 45 (72.6) | 1.0 | 1.0 | 1.0 |
| Nonwhite | 17 (27.4) | 0.4 (0.2–0.8) | 0.4 (0.2–0.8) | 0.3 (0.1–0.8) | |
|
| |||||
| Smoking status | Never smoker | 58 (93.5) | 1.0 | ||
| Ever smoker | 4 (6.5) | 0.7 (0.2–2.5) | |||
|
| |||||
| Chronic illness | No | 48 (77.4) | 1.0 | 1.0 | 1.0 |
| Yes | 14 (22.6) | 3.4 (1.2–10.2) | 3.5 (1.0–12.1) | 1.8 (0.3–9.9) | |
|
| |||||
| Year of study | GEC 1 and | 3 (4.8) | 0.6 (0.1–2.3) | 0.3 (0.1–1.6) | 0.3 (0.02–3.2) |
| Year 2 | 36 (58.1) | 1.0 | 1.0 | 1.0 | |
| Year 3 | 23 (37.1) | 3.0 (1.3–7.1) | 2.6 ( 1.0–6.7) | 5.2 (1.6–17.4) | |
| Years 4 and 5 |
|||||
|
| |||||
| Lives with 1 of more risk groups | No | 49 (79.0) | 1.0 | ||
| Yes | 13 (21.0) | 0.7 (0.3–1.6) | |||
|
| |||||
| Seasonal influenza vaccination history | Never | 22 (35.5) | 1.0 | 1.0 | |
| Previous years | 10 (16.1) | 1.6 (0.6–4.1) | 3.0 (0.8–10.8) | ||
|
| |||||
| Knows anyone who contracted H1N1 | No | 18 (29.0) | 1.0 | ||
| Yes | 44 (71.0) | 0.7 (0.3–1.5) | |||
|
| |||||
| Number of correct answers | None | 11 (17.7) | 1.0 | 1.0 | 1.0 |
| At least 1 correct answer | 51 (82.3) | 2.6 (1.1–6.0) | 2.4 (1.0–6.0) | 3.1 ( 0.9–11.2) | |
aAdjusted for sex, ethnicity, year, of study and knowledge.
bAdjusted for sex, ethnicity, year of study, knowledge, and previous seasonal influenza vaccine.
After adjustment for sex, ethnicity, year of study, presence of chronic illness and correct knowledge answers (model 1), students of non-white ethnicity remained as an important independent negative predictor of vaccine uptake (OR 0.4 (95% CI 0.2–0.8)). Having a chronic illness (OR 3.4 (95% CI 1.2–10.2)), being in years 4 or 5 (OR 3.0 (95% CI 1.3–7.1)) and having accurate knowledge on the H1N1 pandemic (OR 2.6 (95% CI 1.1–6.0)) were positive predictors of vaccine uptake although they were of borderline significance.
The addition of previous seasonal vaccination to the multivariate model suggested that prior influenza vaccination might be a predictor of vaccine uptake, but was not statistically significant and may be explained partly by the presence of chronic illness.
3.7. Future Seasonal Influenza Vaccination
When asked, students who had actually received the H1N1 vaccine were three times more likely (OR 3.1 (95% CI 1.2–7.7)) to say that they would accept the seasonal influenza vaccination in the future compared to respondents who declined the HIN1 vaccine.
4. Discussion
4.1. Main Findings of This Study
The H1N1 vaccine uptake among medical students was 49.2% and intended uptake was 63.3%. This uptake is higher than the 40.3% H1N1 vaccine uptake among frontline healthcare workers overall in England in 2009/10 although the figure is more similar to general practitioners' uptake (50.1%) [9]. It is also noted that this uptake rate is substantially higher than the seasonal influenza vaccine uptake rate amongst HCW of 16.5% in 2008/9, 26.4% in 2009/10 [9], and even the improved postpandemic levels of 34.7% in the winter season of 2010/11 [16]. Studies in other countries found H1N1 vaccine uptake rates among medical students varied between 8% in Greece [22] to 93% in Sweden [23].
Main barriers to uptake included fear of side effects, lack of vaccine information, lack of perceived risk, and inconvenience. Main reasons for acceptance were to protect themselves, patients, and family. The main influences on uptake were medical training, DH recommendation, and social influences (much of which would probably be from other medical personnel). Having a chronic illness, 4th/5th year of study, and correct H1N1 knowledge were associated with uptake whilst non-white ethnicity was a negative predictor. Students in years 4/5 were more likely to accept the vaccine as more years of clinical experience may have led to better understanding of the importance of vaccination and a greater sense of responsibility. This is consistent with the finding where those with better H1N1 knowledge were also more likely to accept the vaccine. Finally, H1N1 vaccine uptake predicted future seasonal influenza vaccine uptake.
4.2. What Is Already Known on This Topic
Consistent with the findings of our study, many studies of seasonal and pandemic influenza vaccine have demonstrated that the most common reasons for acceptance were for self-protection and patient protection whereas the main reasons for declining were fear of side effects and doubts of efficacy [11, 24–35]. Fear of side effects, the most frequently quoted barrier to uptake of H1N1 vaccine, could be due to media interest in the association between swine flu vaccine and Guillain Barré syndrome in 1976 [36, 37], and indeed media influence played an important role in the decision making of our study group, although not the main role. Inconvenient vaccine delivery was the fourth common reason for vaccine rejection in our study which accords with a past study of healthcare workers [38]. To increase the convenience of vaccine delivery, measures such as flexible appointment times, mobile carts, and electronic reminders could be implemented [39].
In contrast to findings of other studies that showed previous seasonal influenza vaccination as a positive predictor of the pandemic influenza vaccine uptake [11–15, 40], our study did not find a significant association; this is most likely because few students would have been offered the vaccine in the past except for those few with a chronic illness such as asthma.
Some studies have shown that ethnic minorities, particularly the black ethnic group, are less likely to accept the H1N1 or seasonal influenza vaccine as they are most likely to perceive the vaccine as unsafe [41–44]. Galarce et al. found that in the USA, blacks were most likely to have tried getting the H1N1 vaccine but found it unavailable [44]. There is little other data on uptake amongst South Asians, which is the most prevalent ethnic minority in our study and non-white ethnicity was shown to be a negative predictor of H1N1 vaccine uptake in our study.
4.3. What This Study Adds
As far as we are aware, this study is the first to report H1N1 vaccination uptake among medical students in the UK. As such, it sets the scene for potential future influenza vaccination campaigns to begin during medical school.
Uptake/intention to receive H1N1 vaccine amongst medical students appears to be higher than that of HCW (40.3%) [9], although this is still below optimal levels. The barriers mentioned could be overcome by education about the efficacy and safety of the vaccine and reassurance that side effects are infrequent and usually mild. The formal medical training environment and guidance from the DH are clearly cited as the most important influencing factors and the medical course is a prime opportunity to exploit this, perhaps particularly in years 4 and 5. It is also important to increase awareness that medical students are at greater risk of contracting H1N1 due to the nature and extent of their patient contact during placements. Informing students about the potential for transmission to patients should also become a priority in the effort to improve uptake. This is an important aim of interventions as our findings show that even a minimal knowledge about H1N1, its severity and transmission can increase uptake significantly.
Our study showed that subjects who accepted the H1N1 vaccine were three times more likely to state they would accept future seasonal influenza vaccines. This reinforces the importance of taking actions to increase H1N1 vaccine uptake amongst medical students. Acceptance of both pandemic and seasonal influenza vaccine is proven to be strongly associated with previous seasonal influenza vaccine uptake among HCW later in their careers [13, 14]. Hence, efforts to create a culture of seasonal influenza vaccination during student years are likely to impact on vaccine uptake in later years. Mandatory vaccination of healthcare workers against influenza is increasingly being called for on both moral and professional ethical grounds [45]. Perhaps medical school is the place to start.
4.4. Limitations of This Study
Valid responses were received from 201 students, who although were randomly selected, may not reflect the views and responses of all medical students in the UK. There were more year 3 respondents, which maybe because students from the same year as the authors (year 3) may be more willing to respond to the questionnaire. Many respondents failed to rank their responses to the reasons for uptake/declination which resulted in our data analysis changing from a weighted ranking as originally planned to a tally of reasons. However this data analysis approach is consistent with other published studies.
We attempted to establish any association between knowing someone who had contracted H1N1 and vaccine uptake. A significant majority (143 (70.4%)) answered yes. This question could have focused specifically on first person contact and explored further how this could influence vaccination.
Authors' Contribution
G. D. Palaniandy, S. Mummadi, I. S. Chin, E. M. Aung, J. W. Hing, S. I. Lee did the literature review, designed the study, wrote the manuscript, collated the survey data, administered the survey and wrote the discussion; J. W. Hing, E. M. Aung and S. I. Lee performed statistical analyses; R. Jordan supervised the study. All authors, external and internal, had full access to all of the data (including statistical reports and tables) in the study and can take responsibility for the integrity of the data and the accuracy of the data analysis.
Conflict of Interests
The authors declare that they have no conflict of interests.
Acknowledgment
R. Jordan is funded by a National Institute for Health Research (NIHR) research fellowship. This study did not receive any other external funding.
Appendix
Questionnaire
Sex: □ M □ F
Age at last birthday: _________
Year of study: □ 1st □ GEC1 □ 2nd
□ 3rd/GEC2 □ 4th/GEC3 5th/GEC4
Smoker: □ Current regular □ Current occasional □ Ex-smoker
□ Never smoker
Do you have a long term medical condition? □ No
□ if Yes—Please tick as appropriate below:
□ Asthma □ Diabetes □ Epilepsy
□ Hypertension
□ Inflammatory Bowel Disease □ Other Please state: ____________________
Do you live with anyone who is: (Please tick any that apply)
□ Under 16 □ Pregnant □ Over 65
□ Healthcare professional
Have you ever had seasonal flu vaccine? (Please tick any that apply)
□ This year □ Last year □ Previous years □ Never
If yes, have you had any side effects? □ No □ Yes Please state: ___________________
Would you have a seasonal flu vaccine in the future? □ Yes □ No
Who do you think are the priority groups for receiving the swine flu vaccine? Please select all relevant answers:
□ Over 65 □ Under 16 □ Pregnant women □ Healthcare workers □ People with chronic health conditions
How do you think swine flu is transmitted?
Please select all relevant answers:
□ Coughs/Sneezes □ Eating infected meat
□ Direct contact with an infected person
□ Touching a contaminated object □ Other Please state: ____________________
How severe do you think is the swine flu pandemic?
□ Not severe □ Quite severe □ Severe
□ Very Severe
What do you think is the swine flu case-fatality rate? □ 0.01% □ 0.1% □ 1% □ 10%
□ 20% □ 50%
Do you know anyone who had swine flu?
□ Yes □ No
Have you been offered the swine flu vaccine?
□ Yes, and I accepted the vaccine □ Yes, but I declined the vaccine
□ No, but I will have the vaccine □ No, and I will not have the vaccine
If you have accepted or will accept the vaccine, why? Please rank the 3 most relevant reasons in order, 1 being most important
□ Reduce transmission to patients □ Reduce transmission to relatives/friends □ Decrease the likelihood of getting swine flu □ Vaccine is safe and effective □ I have a chronic condition □ Other Please state: ____________________
Which source of information influenced your decision on vaccination the most? Please rank the 3 most relevant reasons in order, 1 being most important
□ Social influence □ Media influence
□ Department of Health guidelines □ Peer pressure □ Family □ Medical training
□ Independent evaluation of scientific papers
If you have declined or will decline the vaccine, why? Please rank the 3 most relevant reasons in order, 1 being most important
□ Do not think myself at risk of swine flu □ Lack of information about the vaccine □ Do not think the vaccine is effective □ Needle phobia □ Worried about the side effects □ Timing of vaccination was inconvenient □ Vaccine might give me swine flu □ Allergies to constituents of vaccine □ Other Please state: ______________________
Ethnicity: Please circle as appropriate if selecting “other” please state:
| White | Asian | Black | Mixed | Other ethnicities |
| White British | Indian | Caribbean | White/Black Caribbean | Chinese |
| White Irish | Pakistani | African | White/Asian | Other groups |
| Other | Bangladesh | Other Black | Other mixed | |
| Other Asian |
References
- 1.Chan M. June 2009, World Health Organisation press statement, http://www.who.int/mediacentre/news/statements/2009/h1n1_pandemic_phase6_20090611/en/index.html.
- 2.Health Protection Agency. August 2011, Epidemiological report of pandemic (H1N1) 2009 in the UK, April 2009-May 2010, http://www.hpa.org.uk/webc/HPAwebFile/HPAweb_C/1284475321350.
- 3.Ferguson NM, Cummings DAT, Fraser C, Cajka JC, Cooley PC, Burke DS. Strategies for mitigating an influenza pandemic. Nature. 2006;442(7101):448–452. doi: 10.1038/nature04795. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Luke CJ, Subbarao K. Vaccines for pandemic influenza. Emerging Infectious Diseases. 2006;12(1) doi: 10.3201/eid1201.051147. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Donaldson L. December 2009, Further details about the H1N1 swine flu vaccination programme 2009-2010, http://www.dh.gov.uk/prod_consum_dh/groups/dh_digitalassets/documents/digitalasset/dh_104315.pdf.
- 6.Orr P. Influenza vaccination for health care workers: a duty of care. Canadian Journal of Infectious Diseases. 2000;11(5):225–226. doi: 10.1155/2000/461308. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Grant S. REMINDER: Vaccinations against Swine Flu for Medical Students. E-mail received by all medical students at the University of Birmingham on 19/11/2009.
- 8.Jordan R, Wake B, Hawker J. 48. Birmingham, UK: Department of Public Health and Epidemiology, University of Birmingham; 2004. Influenza vaccination of health care workers (HCW) to reduce influenza-related outcomes in high risk patients: a systematic review of clinical and cost effectiveness. [Google Scholar]
- 9.Sethi M, Pebody R. August, 2011, Pandemic H1N1 (Swine Flu) and Seasonal Influenza Vaccine Uptake amongst Frontline Healthcare Workers in England 2009/10, https://www.wp.dh.gov.uk/immunisation/files/2012/06/FluVaccine-Uptake_HCWs_acc2.pdf.
- 10.Mereckiene J, Cotter S, Nicoll A, et al. National seasonal influenza vaccination survey in Europe, 2008. Eurosurveillance. 13(43, article 2) doi: 10.2807/ese.13.43.19017-en. [DOI] [PubMed] [Google Scholar]
- 11.Vírseda S, Restrepo MA, Arranz E, et al. Seasonal and pandemic A (H1N1) 2009 influenza vaccination coverage and attitudes among health-care workers in a Spanish university hospital. Vaccine. 2010;28(30):4751–4757. doi: 10.1016/j.vaccine.2010.04.101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Pareek M, Clark T, Dillon H, Kumar R, Stephenson I. Willingness of healthcare workers to accept voluntary stockpiled H5N1 vaccine in advance of pandemic activity. Vaccine. 2009;27(8):1242–1247. doi: 10.1016/j.vaccine.2008.12.006. [DOI] [PubMed] [Google Scholar]
- 13.Seale H, Kaur R, Wang Q, et al. Acceptance of a vaccine against pandemic influenza A (H1N1) virus amongst healthcare workers in Beijing, China. Vaccine. 2011;29(8):1605–1610. doi: 10.1016/j.vaccine.2010.12.077. [DOI] [PubMed] [Google Scholar]
- 14.Chor JSY, Pada SK, Stephenson I, et al. Seasonal influenza vaccination predicts pandemic H1N1 vaccination uptake among healthcare workers in three countries. Vaccine. 2011;29(43):7364–7369. doi: 10.1016/j.vaccine.2011.07.079. [DOI] [PubMed] [Google Scholar]
- 15.Glaser MS, Chui S, Webber MP, et al. Predictors of acceptance of H1N1 influenza vaccination by FDNY firefighters and EMS workers. Vaccine. 2011;29(34):5675–5680. doi: 10.1016/j.vaccine.2011.06.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. DH/HPA, October 2011, Seasonal influenza vaccine uptake amongst frontline healthcare workers (HCW) in England. Winter season 2010/2011 https://www.wp.dh.gov.uk/immunisation/files/2012/06/FluVaccine-Uptake_HCWs_acc2.pdf.
- 17.Amodio E, Tramuto F, Maringhini G, Asciutto R, Firenze A, Vitale F. Are medical residents a, “core group” for future improvement of influenza vaccination coverage in health-care workers? A study among medical residents at the university hospital of Palermo (Sicily) Vaccine. 2011;29(45):8113–8117. doi: 10.1016/j.vaccine.2011.08.033. [DOI] [PubMed] [Google Scholar]
- 18.Milunic SL, Quilty JF, Super DM, Noritz GH. Patterns of influenza vaccination among medical students. Infection Control and Hospital Epidemiology. 2010;31(1):85–88. doi: 10.1086/649219. [DOI] [PubMed] [Google Scholar]
- 19.Mak KK, Yiu YF, Ko KL, et al. Attitudes and perceptions of influenza vaccination among Hong Kong doctors and medical students before the 2009 pandemic. doi: 10.1093/eurpub/cks014. European Journal of Public Health. In press. [DOI] [PubMed] [Google Scholar]
- 20.Toy WC, Janosky JE, Laird SB. Influenza immunization of medical residents: knowledge, attitudes, and behaviors. American Journal of Infection Control. 2005;33(8):473–475. doi: 10.1016/j.ajic.2005.06.003. [DOI] [PubMed] [Google Scholar]
- 21.Zimmerman RK, Santibanez TA, Janosky JE. What affects influenza vaccination rates among older patients? An analysis from inner-city, suburban, rural, and veterans affairs practices. American Journal of Medicine. 2003;114(1):31–38. doi: 10.1016/s0002-9343(02)01421-3. [DOI] [PubMed] [Google Scholar]
- 22.Mavros MN, Mitsikostas PK, Kontopidis IG, Moris DN, Dimopoulos G, Falagas ME. H1N1v influenza vaccine in Greek medical students. European Journal of Public Health. 2011;21(3):329–332. doi: 10.1093/eurpub/ckq109. [DOI] [PubMed] [Google Scholar]
- 23.Faresjö T, Arvidsson L, Boberg P, Hagert B, Gursky EA, Timpka T. Swedish nursing and medical students' high vaccination adherence during the influenza A, (H1N1) pandemic 2009: insights for pandemic preparedness. Scandinavian Journal of Infectious Diseases. 2012;44(3):237–241. doi: 10.3109/00365548.2011.620000. [DOI] [PubMed] [Google Scholar]
- 24.Wicker S, Rabenau HF, Doerr HW, Allwinn R. Influenza vaccination compliance among health care workers in a German university hospital. Infection. 2009;37(3):197–202. doi: 10.1007/s15010-008-8200-2. [DOI] [PubMed] [Google Scholar]
- 25.O’Reilly FW, Cran GW, Stevens AB. Factors affecting influenza vaccine uptake among health care workers. Occupational Medicine. 2005;55(6):474–479. doi: 10.1093/occmed/kqi099. [DOI] [PubMed] [Google Scholar]
- 26.Wodi AP, Samy S, Ezeanolue E, et al. Influenza vaccine: Immunization rates, knowledge, and attitudes of resident physicians in an urban teaching hospital. Infection Control and Hospital Epidemiology. 2005;26(11):867–872. doi: 10.1086/502510. [DOI] [PubMed] [Google Scholar]
- 27.Heininger U, Bächler M, Schaad UB. Attitudes of pediatricians regarding influenza self-immunization: a survey in a Swiss university children’s hospital. Pediatric Infectious Disease Journal. 2003;22(5):391–394. doi: 10.1097/01.inf.0000066901.59298.a8. [DOI] [PubMed] [Google Scholar]
- 28.Mah MW, Hagen NA, Pauling-Shepard K, et al. Understanding influenza vaccination attitudes at a Canadian cancer center. American Journal of Infection Control. 2005;33(4):243–250. doi: 10.1016/j.ajic.2004.12.006. [DOI] [PubMed] [Google Scholar]
- 29.Hakim H, Gaur AH, McCullers JA. Motivating factors for high rates of influenza vaccination among healthcare workers. Vaccine. 2011;29(35):5963–5969. doi: 10.1016/j.vaccine.2011.06.041. [DOI] [PubMed] [Google Scholar]
- 30.Rubin GJ, Potts HWW, Michie S. Likely uptake of swine and seasonal flu vaccines among healthcare workers. A cross-sectional analysis of UK telephone survey data. Vaccine. 2011;29(13):2421–2428. doi: 10.1016/j.vaccine.2011.01.035. [DOI] [PubMed] [Google Scholar]
- 31.Blasi F, Palange P, Rohde G, Severin T, Cornaglia G, Finch R. Healthcare workers and influenza vaccination: an ERS-ESCMID Web-based survey. Clinical Microbiology and Infection. 2011;17(8):1223–1225. doi: 10.1111/j.1469-0691.2011.03501.x. [DOI] [PubMed] [Google Scholar]
- 32.Boyeau C, Tanguy M, Pean S, Delhumeau A, Fanello S. Seasonal and pandemic A, (H1N1) 2009 influenza vaccination coverage among health-care workers in a French university hospital. Santé Publique. 23(1):19–29. [PubMed] [Google Scholar]
- 33.Grau S, Luque S, Pi-Sunyer J, et al. Low adherence to 2009 pandemic influenza A(H1N1)vaccination program among health care workers of a medical centre during the pandemic phase. Enfermedades Infecciosas y Microbiologia Clinica. 2011;29(4):269–275. doi: 10.1016/j.eimc.2010.09.013. [DOI] [PubMed] [Google Scholar]
- 34.To KW, Lee S, Chan TO, Lee SS. Exploring determinants of acceptance of the pandemic influenza A (H1N1) 2009 vaccination in nurses. American Journal of Infection Control. 2010;38(8):623–630. doi: 10.1016/j.ajic.2010.05.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Maltezou HC, Dedoukou X, Patrinos S, et al. Determinants of intention to get vaccinated against novel (pandemic) influenza A H1N1 among health-care workers in a nationwide survey. Journal of Infection. 2010;61(3):252–258. doi: 10.1016/j.jinf.2010.06.004. [DOI] [PubMed] [Google Scholar]
- 36.Rachiotis G, Mouchtour VA, Kremastinou J. Low acceptance of vaccination against the 2009 pandemic influenza A, (H1N1) among healthcare workers in Greece. Eurosurveillance. 15(6, article 3) [PubMed] [Google Scholar]
- 37.Breman JG, Hayner NS. Guillain-Barre syndrome and its relationship to swine influenza vaccination in Michigan, 1976-1977. American Journal of Epidemiology. 1984;119:880–889. doi: 10.1093/oxfordjournals.aje.a113810. [DOI] [PubMed] [Google Scholar]
- 38.Hollmeyer HG, Hayden F, Poland G, Buchholz U. Influenza vaccination of health care workers in hospitals—a review of studies on attitudes and predictors. Vaccine. 2009;27(30):3935–3944. doi: 10.1016/j.vaccine.2009.03.056. [DOI] [PubMed] [Google Scholar]
- 39.Jordan R, Hayward A. Should healthcare workers have the swine flu vaccine? British Medical Journal. 2009;339 doi: 10.1136/bmj.b3398.b3398 [DOI] [PubMed] [Google Scholar]
- 40.Boulton ML, Grossman AM, Potter R, Vranesich PA, Clayton J. Assessing the relationship between seasonal and H1N1 influenza vaccination status in Michigan children, 2009-2010. Public Health Reports. 126(supplement 2):70–77. doi: 10.1177/00333549111260S209. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Hebert PL, Frick KD, Kane RL, McBean AM. The causes of racial and ethnic differences in influenza vaccination rates among elderly medicare beneficiaries. Health Services Research. 2005;40(2):517–537. doi: 10.1111/j.1475-6773.2005.00370.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Myers LB, Goodwin R. Determinants of adults’ intention to vaccinate against pandemic swine flu. BMC Public Health. 2011;11, article 15 doi: 10.1186/1471-2458-11-15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Hennessy-Fiske M. Times/USC poll finds majority of California's registered voters have no plans to get H1N1 vaccine. Los Angeles Times, http://latimesblogs.latimes.com/lanow/2009/11/timesusc-poll-finds-majority-of-californias-registered-voter-have-no-plans-to-get-h1n1-vaccine.html.
- 44.Galarce EM, Minsky S, Viswanath K. Socioeconomic status, demographics, beliefs and A(H1N1) vaccine uptake in the United States. Vaccine. 2011;29(32):5284–5289. doi: 10.1016/j.vaccine.2011.05.014. [DOI] [PubMed] [Google Scholar]
- 45.Caplan A. Time to mandate influenza vaccination in health-care workers. The Lancet. 2011;378(9788):310–311. doi: 10.1016/s0140-6736(11)61156-2. [DOI] [PubMed] [Google Scholar]


