Abstract
Mycetoma or Maduramycosis is a localized chronic suppurative infection characterized by exuberant granulation tissue, discharging sinuses, and bone involvement later in the course of the disease. Early clinical diagnosis before the appearance of sinuses and grains (aggregates of organism surrounded by granulation tissue, which are discharged from the draining sinuses) is difficult. Delay in diagnosis may lead to amputation of the affected part. Definitive diagnosis is through biopsy and microbiological examination. However, at times diagnosis may still be difficult. The recently described “dot in circle” sign on magnetic resonance imaging (MRI) is easy to recognize and highly specific. We present a case of mycetoma foot with characteristic MRI features.
Keywords: Dot in circle sign, maduramycosis, MRI, mycetoma
INTRODUCTION

Mycetoma pedis, or Madura foot, was first described as a clinical entity by Gill in 1842, from a clinic in Madurai, India. In 1880, Carter coined the term “mycetoma”.[1] The disease can be caused by one of two organisms, the Eumyces, or true fungi (eumycetoma), or Actinomyces, filamentous bacteria of the Order actinomycetales (actinomycetoma).[2] It is a localized, chronic, suppurative infection characterized by exuberant granulation tissue and discharging sinuses and bone involvement later in the course of the disease. Early clinical diagnosis before the appearance of discharging sinuses is difficult as the entity may clinically mimic a low grade neoplasm or a chronic bacterial or tubercular infection.[2] The recently described “dot in circle sign” on magnetic resonance imaging (MRI) is easy to recognize and specific to this condition and establishes the role of MRI in early diagnosis.[3–5] We present a case of mycetoma foot that demonstrated the “dot-in-circle sign” on MRI.
CASE REPORT
A 48-year-old man complained of painless swelling in the left foot that had been present for the past 6 years. The patient had been treated with multiple courses of oral and intravenous antibiotics in a primary health center. The patient did not respond to the treatment. At the peripheral hospital two attempts were made to incise and drain the lesion. For the past 1 month, the patient had experienced mild dull aching pain in the foot, mainly during the night. He was nondiabetic and nonimmunocompromised. Physical examination revealed the swelling in the dorsal aspect of the left foot. Skin in that area was hyperpigmented and showed encrustation and ulceration. No discharging sinuses were seen. The patient did not mention a history of past discharge of granules from any area of the foot. There was no history of fever. General examination, blood and serum biochemistry were also unremarkable. Plain radiograph of the left foot showed mild soft tissue swelling with changes of chronic osteomyelitis involving the tarsal and metatarsals [Figure 1]. MRI was performed to characterize the lesion and to evaluate the extent of the disease. The scan revealed extensive soft tissue and osseus inflammation. Multiple discrete, as well as, conglomerate small spherical hyperintense lesions with peripheral hypointense rim were seen. Few of these lesions showed a central tiny hypointense focus suggestive of “dot in circle” sign [Figure 2]. T2-weighted fat saturated (T2W FS) and T1-weighted fat saturated (T1W FS) postcontrast images depicted the proximal extent of the lesion up to the distal half of the leg with ankle joint effusion and synovial thickening [Figure 3]. On the basis of MRI findings, the diagnosis of mycetoma was considered and a biopsy was performed. The biopsy revealed granulomatous inflammation. The final microbiological test showed the presence of Curvularia lunata (Eumycetoma Sp.) [Figure 4]. The patient was amputated 10 inches below the knee joint and put on 400 mg oral Itraconazole daily for 6 months.
Figure 1.

Chronic osteomyelitis. A 48-year-old man with painless swelling of left foot. Frontal radiograph shows moth eaten area of destruction involving tarsal (white arrow) and metatarsals (black arrow) with patchy erosions and mild soft tissue swelling (yellow arrow).
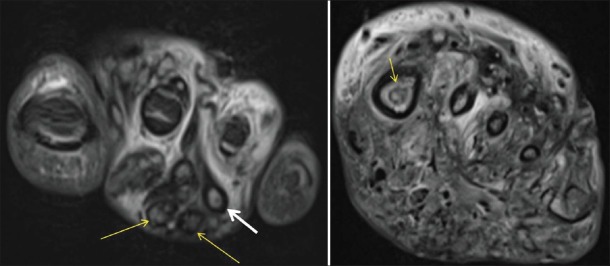
Figure 2.
MRI T2 weighted coronal images show inflammatory changes with multiple soft tissue and osseus small hyperintense lesions with peripheral hypointense rim corresponding to mycetoma grains (yellow arrows). Few of them showing “dot in circle” sign (thicker white arrow).
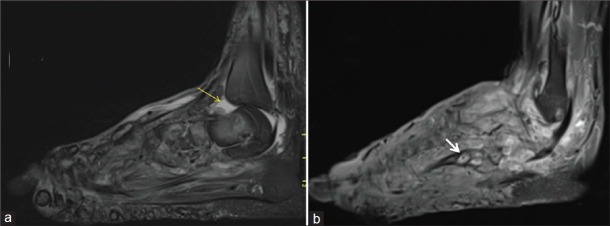
Figure 3.
(a) T2 weighted fat suppressed sagittal and (b) T1W fat suppressed postcontrast sagittal images show extension of inflammation proximally up to distal leg with ankle joint effusion (yellow arrow) and synovial thickening. “Dot in circle” sign (white arrow) is seen in postcontrast image.
Figure 4.
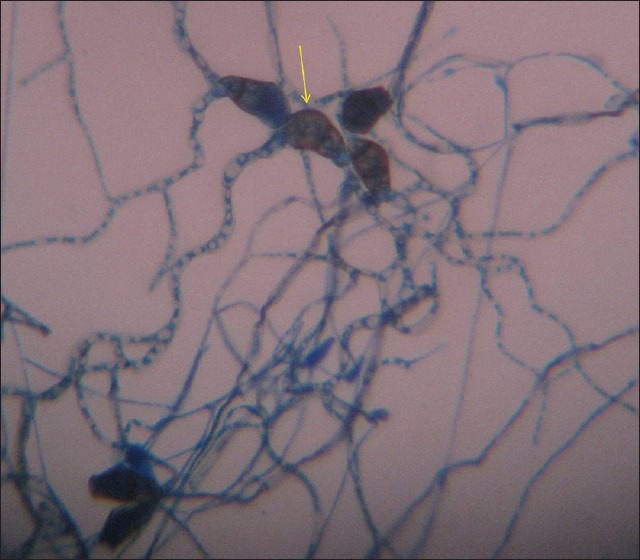
Histopathology slide prepared using lactophenol cotton blue shows septated conidia which is curved at 3rd cell from the base (yellow arrow) confirming the diagnosis of curvularia lunata (eumycetoma sp.) ×1500.
DISCUSSION
Mycetoma is a chronic debilitating granulomatous disease that is prevalent in tropical and subtropical regions.[1,3] The term mycetoma is a clinical entity, which applies to a chronic inflammatory process of soft tissue, usually of the foot, resulting from infection by one or more fungi or actinomycetes (a Gram-positive bacillus). Initially, there is formation of soft tissue swelling with induration due to underlying granulation tissue, which progresses to the formation of discharging sinuses. The lesion may be confined to the soft tissue for years before bone involvement occurs. The diagnosis of mycetoma should be considered when a patient presents with soft tissue lesion and discharging sinuses with or without bone involvement. Histopathological examination usually reveals granulomatous inflammation.[3] Although various radiographic bone changes have been described in cases of mycetoma, bone involvement usually occurs late in the course of the disease. Gross bony involvement makes nonsurgical cure unlikely.[6] Noninvasive imaging with MRI can characterize the soft tissue lesion of mycetoma and aid in early diagnosis.
Mycetoma is characterized by the formation of aggregates of the organism, known as “grains”, which are found within abscesses surrounded by abundant granulation tissue.[7] This could account for the appearance observed on MRI of conglomerates of small (2–5 mm) round hyperintense lesions, representing the granulation tissue, surrounded by low-signal intensity rim, representing intervening fibrous septa. The central low-signal intensity dot is the result of susceptibility effect caused by the presence of fungal grains. This unique appearance known as “dot in circle sign” appears to be highly suggestive of mycetoma.[3–5] This sign was first proposed by Sarris et al.,[4] in 2003 on T2-weighted short-tau inversion recovery (STIR), and T1-weighted Fast Spin gadolinium-enhanced images in a series of two cases. They also correlated the MRI finding with histological findings.[4] Cherian et al., described similar appearance in a series of three cases.[5] The distinction between the two forms of mycetoma is not possible with MRl.[3]
Czechowski et al., described small T1 and T2 hypointense lesion on MRI caused by the susceptibility effect of the fungal grains.[8] However, they did not describe the “dot in circle” sign in their study. In our case, MRI clearly depicted the conglomerate as well as discrete small round T2 hyperintense lesions with central hypointense foci in some of them.
Few radiographic bone changes have been described to distinguish between actinomycetoma and eumycetoma. Eumycotic lesions tend to form a few cavities in the bone ≥1 cm in diameter, while actinomycetes often form smaller, but more numerous cavities. In a study by Lewall et al., a moth eaten appearance caused by a combination of irregular periosteal reaction, periosteal erosion, and small cavities within bone were seen in 25% of cases of actinomycetoma, but in none of the patients with eumycetoma.[2]
Modern chemotherapeautic drugs are effective in early stage of the disease when combined with surgery. Difficulty in accurately identifying the extent of the lesion during surgery is the chief cause of recurrence. The recurrence rate can vary between 20% and 90%.[9] MRI can be helpful in early diagnosis and to monitor recurrence.
In the absence of typical clinical features of discharging sinuses, mycetoma foot may clinically mimic a low grade neoplasm or a chronic bacterial or tubercular infection.[2] “Dot in circle” sign is easy to recognize and is specific to this condition. MRI could aid in the early diagnosis of this chronic infection and may differentiate it from other clinically similar conditions. The demonstration of the organism in the lesion by biopsy and microbiological examination can be difficult. In India, the disease is still endemic and MRI may help in early recognition and prevention of amputations that maybe required because of delayed diagnosis.
Footnotes
Available FREE in open access from: http://www.clinicalimagingscience.org/text.asp?2012/2/1/66/103056
Source of Support: Nil
Conflict of Interest: None declared.
REFERENCES
- 1.Carroll DS. Mycetoma pedis. Radiology. 1949;53:81–4. doi: 10.1148/53.1.81. [DOI] [PubMed] [Google Scholar]
- 2.Lewall DB, Ofole S, Bendl B. Mycetoma. Skeletal Radiol. 1985;14:257–62. doi: 10.1007/BF00352615. [DOI] [PubMed] [Google Scholar]
- 3.Kumar J, Kumar A, Sethy P, Gupta S. The dot-in-circle sign of mycetoma on MRI. Diagn Interv Radiol. 2007;13:193–5. [PubMed] [Google Scholar]
- 4.Sarris I, Berendt AR, Athanasous N, Ostlere SJ OSIRIS collaborative study group. MRI of mycetoma of the foot: Two cases demonstrating the dot-in-circle sign. Skeletal Radiol. 2003;32:179–83. doi: 10.1007/s00256-002-0600-2. [DOI] [PubMed] [Google Scholar]
- 5.Cherian RS, Betty M, Manipadam MT, Cherian VM, Poonnoose PM, Oommen AT, et al. The “dot-in-circle” sign - A characteristic MRI finding in mycetoma foot: A report of three cases. Br J Radiol. 2009;82:662–5. doi: 10.1259/bjr/62386689. [DOI] [PubMed] [Google Scholar]
- 6.Abd El, Bagi ME. New radiographic classification of bone involvement in pedal mycetoma. AJR Am J Roentgenol. 2003;180:665–8. doi: 10.2214/ajr.180.3.1800665. [DOI] [PubMed] [Google Scholar]
- 7.Hay RJ. Fitzpatrick's dermatology in general medicine. 7th ed. New York: McGraw Hill; 2008. Deep fungal infection; pp. 1832–3. [Google Scholar]
- 8.Czechowski J, Nork M, Haas D, Lestringant G, Ekelund L. MR and other imaging methods in the investigation of mycetomas. Acta Radiol. 2001;42:24–6. doi: 10.1080/028418501127346413. [DOI] [PubMed] [Google Scholar]
- 9.Fahal AH, Hassan MA. Mycetoma. Br J Surg. 1992;79:1138–41. doi: 10.1002/bjs.1800791107. [DOI] [PubMed] [Google Scholar]