Abstract
Background:
The use of easily obtainable clinical and laboratory parameters to identify hypertensive patients with increased cardiovascular risk in resource limited settings cannot be overemphasized. Prolongation of QT intervals and increased dispersion has been associated with increased risk of cardiovascular death. The study aimed at describing the epidemiology of QT interval abnormalities among newly diagnosed hypertensive subjects and associated clinical correlates.
Materials and Methods:
One hundred and forty newly diagnosed hypertensive subjects and 70 controls were used for this study. Clinical and sociodemographic characteristics were obtained. Twelve lead resting electrocardiography, QT dispersion, heart rate corrected minimum and maximum QT intervals were determined manually. Increased QTcmax was defined at QTcmax >440msec. QT parameters were compared between various groups. SPSS 16.0 was used for data analysis.
Results:
The hypertensive subjects were well matched in age and gender distribution with controls. QTmax and QTcmax were significantly higher among hypertensive subjects than controls (379.7±45.1 vs. 356.7±35.6, 447.5± 49.0 vs. 414.5 ±34.7 ms, respectively, P<0.05). QTd and QTcd were also significantly higher among hypertensive subjects than controls (62.64±25.65 vs. 46.1±17.2, 73.8 ±30.0 vs. 52.5±18.8, respectively, P<0.05). Seventy three (52.14%) of the hypertensive subjects had QTcmax >440ms compared to 21.43% of controls, P=0.01. Increased QTc dispersion was present in 36.4% of hypertensive subjects. Hypertensive subjects with QT abnormalities had significantly higher mean waist hip ratio, mean body mass index and a higher proportion of smoking than controls.
Conclusion:
QT prolongation and increased QTc dispersion are common among newly diagnosed hypertensive Nigerians and seem to be significantly associated with obesity. Effective antihypertensive therapy and control of obesity are important management modality for newly diagnosed hypertensive patients.
Keywords: Clinical correlates, hypertension, Nigeria, QT dispersion, QT prolongation
INTRODUCTION
Systemic hypertension is the commonest noncommunicable disease in Nigeria. The prevalence has been estimated to be between 10% and 20% of the Nigerian population.[1–3] A recent point population survey in Southern Nigeria revealed that the prevalence of hypertension was up to 42% among market women and majority of them were not aware of their hypertension status.[4] Adequate blood pressure control and compliance are other major issues in hypertension management in Nigeria.[4,5,6] Hypertension is often associated with many other cardiovascular risk factors with additive and multiplicative influences on their cardiovascular risk.[7,8] The severity of blood pressure and the level of blood pressure control also affect the cardiovascular risk significantly.[8,9] Hypertension is also associated with several target organ damage including left ventricular hypertrophy, microalbuminuria, heart failure, retinopathy, peripheral artery disease, coronary artery disease, and stroke.[10–12]
Patients with hypertension and especially those with left ventricular hypertrophy (LVH) are at increased risk of sudden cardiac death (SCD).[5,8,10] Hypertensive heart disease is the most common cause of SCD in Nigerians; many of whom were reported to be previously undiagnosed and hadunexpectedly high prevalence of target organ damage and other complications.[13,14] The use of easily obtainable clinical and laboratory parameters to identify hypertensive patients with increased cardiovascular risk in resource limited settings cannot be overemphasized.
The QT interval which is a measure of the duration of ventricular depolarization and repolarization is one instrument for such screening. Prolongation of QT interval has been associated with increased cardiovascular death and has been reported among subjects with diabetes, hypertrophic cardiomyopathy and cardiac failure.[15,16]
Interlead variability of the QT interval on the standard 12 lead- ECG defined as QT dispersion reflects regional differences in ventricular repolarization.[17] Increased dispersion of recovery time is associated with increased risk for serious ventricular arrhythmias. Underlying factors in increased QT dispersion include patchy myocardial fibrosis resulting from myocardial ischemia, ventricular dilatation and neurohormonal activation.[18] Increased QT dispersion have been found in myocardial infarction, hypertrophic cardiomyopathy, hypertension, left ventricular hypertrophy, diabetes, chronic heart failure, mitral valve prolapse and long QT syndrome which is genetically related.[18]
QT prolongation is associated with various components of the insulin resistance syndrome, age body mass index, left ventricular hypertrophy, persistently elevated blood pressure and in some studies the female gender.[16]
Data relating to the frequency of QT prolongation and increased QTc dispersion among newly diagnosed hypertensive Nigerians are scarce. This study, therefore, aimed to describe the epidemiology of QTc prolongation and increased QTc dispersion and further describe their associated clinical correlates among newly diagnosed hypertensive subjects in Nigeria.
MATERIALS AND METHODS
The study was conducted at the Ladoke Akintola University of Technology Teaching Hospital, Osogbo, Osun State, Nigeria. It was a cross-sectional study. The study population consisted of 140 adult Nigerian subjects (>18 years of age) with systemic hypertension seen at the Cardiology clinic and Medical Outpatient Department of the hospital. Seventy control subjects were recruited from the general outpatients departments and included patients’ relatives and members of staff. The inclusion criteria were newly diagnosed patients with hypertension who have not been on any antihypertensive drugs or any other drugs such as antimalarials and phenothiazines (With this the effect of drugs which can affect QT intervals was excluded). Subjects with chronic kidney disease, pregnancy, diabetes mellitus, stroke, or heart failure were excluded from the study. Subjects who had taken medications such as antimalarials, antidepressants, antipsychotics, and antibiotics such as erythromycin in the last 1 week were also excluded.
The patients were checked in detail and examined. Clinical and sociodemographic characteristics were obtained. They include age, gender, body weight, height, waist circumference, systolic and diastolic blood pressure. Laboratory investigations performed on each participant included hemogram and 12-lead resting electrocardiography. Serum urea, creatinine, and electrolytes were measured using flame photometer, diacethylmonoxime, and jaffe (picric) method in the chemical pathology laboratory.
12-Lead electrocardiography
Resting electrocardiography using a portable AT-10 Schiller machine was done. After explaining the procedure to the subjects to allay anxiety, the upper clothing, and all accessory dressings (watches, necklaces, and rings) were removed.
The ECG leads were placed accordingly, in line with the recommendation of the American Heart Association guidelines.[19] The calibrations were 1 mV=10 mm on the vertical line and ECG speed of 25 and 50 mm/s were used. Lead II was used as the rhythm strip. The ECGs were analyzed quantitatively to obtain heart rate, rhythm, QRS axis, P wave, QRS morphology, PR interval, and QRS morphology. QT intervals in each of the leads were measured.
The QT interval was taken as the interval from the beginning of Q to the end of T wave (QTo). At least three consecutive cycles were measured for each lead and then averaged. A lead was discarded in case the T wave was not distinct. When U waves were present, the end of the T wave was taken as the nadir between the T and U wave. Any ECG with less than eight clearly identifiable leads for QT measurement was discarded. The difference between the minimum QT and maximum QT is taken as QT dispersion. Heart rate-corrected-QT interval was also done to get the heart rate-corrected QT dispersion (QTcd = maximum QTc-minimum QTc). The QT was corrected for heart rate using the Bazett's formula[20] and the QTc (QT corrected) in the various leads used to calculate the QTc dispersion. QTc prolongation was defined as QTc≥440 ms while increased QTc dispersion was defined as QTcd ≥ 80 ms.
![]()
Assesment for ECG-LVH was done using the Sokolow-lyoncriteria.[21]
Data analysis
Data analysis was done using the Statistical Package for Social Sciences (SPSS version 16.0). Continuous variables were summarized as means ± standard deviation (S.D.) while categorical variables were summarized as frequencies and percentages. Student's t-test was used to assess differences between means. Differences between categorical variables were analyzed by Chi-square. P value of < 0.05 was considered significant. Approval was obtained from the Ethical and Research Committee of the LAUTECH Teaching Hospital, Osogbo for this study.
RESULTS
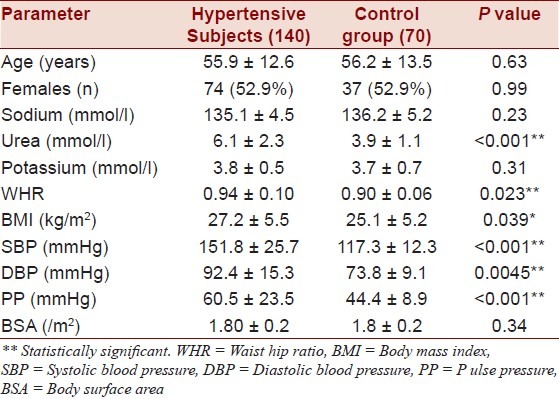
The hypertensive subjects were well matched for age and gender distribution with the control subjects. The mean age of hypertensive subjects was 55.9±12.6 compared with the mean age of control subjects 56.2±13.5, P > 0.05. Females constituted 52.9% of both the hypertensive and control subjects. Waist hip ratio and body mass index were significantly higher among hypertensive subjects than that among controls. Serum urea was also significantly higher among hypertensive subjects than that among control subjects as shown in Table 1.
Table 1.
Clinical and demographic characteristics of study population
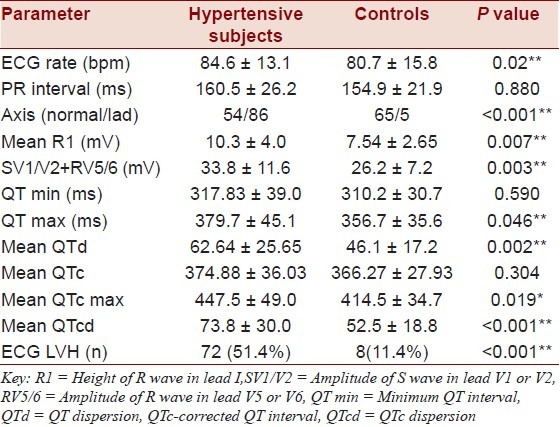
The electrocardiographic parameters among the study participants were shown in Table 2. Heart rate, mean height of R wave in lead I, addition of S wave in V1/V2 plus the R wave in V5/V6 were higher among hypertensive subjects than that among controls. Hypertensive subjects had a significantly higher proportion of electrocardiographic left ventricular hypertrophy (ECG-LVH) than that among control subjects (51.4% vs. 11.4% respectively, P<0.05). Maximum QT (QTmax) and maximum corrected QT interval (QTcmax) were significantly higher among hypertensive subjects than that among controls (379.7±45.1 vs. 356.7±35.6, P<0.05: 447.5 ± 49.0 vs. 414.5 ±34.7 ms, P<0.05 respectively). QT dispersion (QTd) and heart rate corrected QT dispersion (QTcd) were also significantly higher among hypertensive subjects than that among controls (62.64±25.65 vs. 46.1±17.2, P<0.05; 73.8 ±30.0 vs. 52.5±18.8, P<0.05, respectively) as shown in Table 2.
Table 2.
Electrocardigraphic parameters in the study population
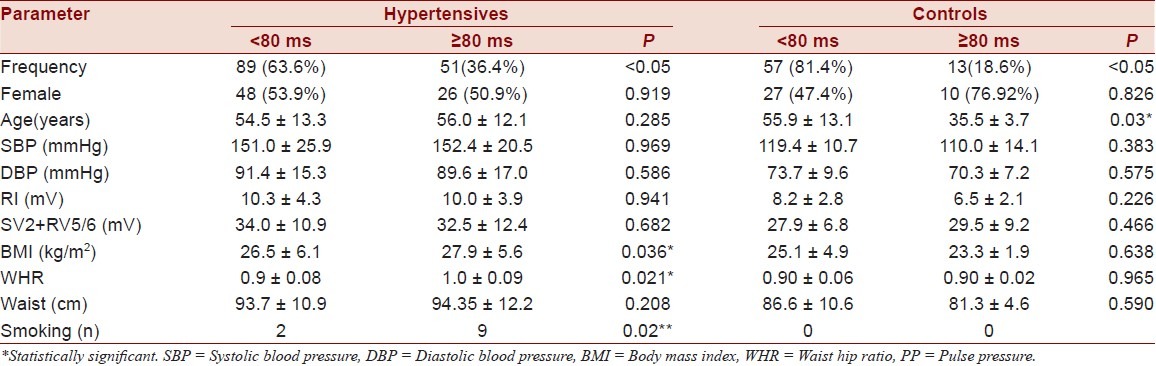
Tables 3 and 4 shows a comparism of clinical and demographic parameters between subjects with prolonged QTc and increased QTcd within the hypertensive group compared with normal controls. Seventy three (52.14%) of the hypertensive subjects had prolongation of QTc max as against 21.43% in the normal controls (P=0.01). Increased QTc dispersion was present in 36.4% of hypertensive subjects compared to 18.1% of controls. Hypertensive subjects with increased QTc dispersion and prolonged QT interval had significantly higher mean waist hip ratio, mean body mass index and a higher frequency of smoking than that among controls. The diastolic blood pressure, systolic blood pressure, maximum amplitude of R wave in lead I on ECG and summation of amplitude of V2 and V5/V6 on ECG were higher among the hypertensive group with prolonged QTc max although it did not reach statistical significance. A similar pattern was observed among control subjects.
Table 3.
Clinical and demographic parameters among the QTc max groupings
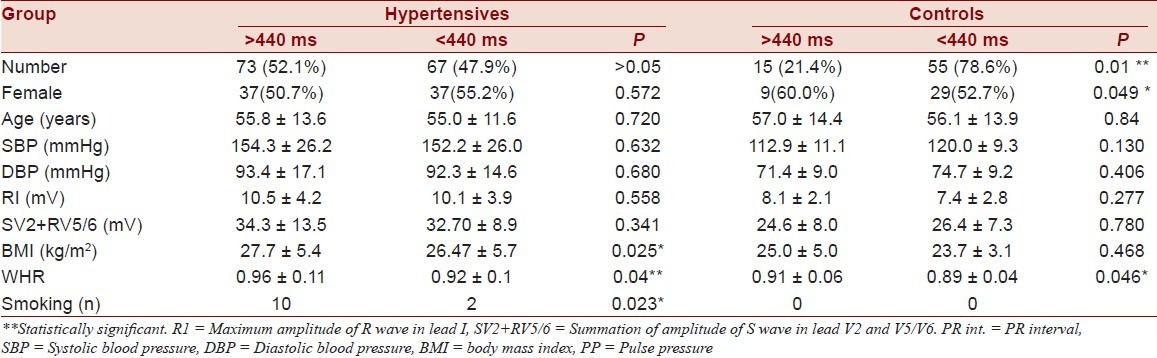
Table 4.
Clinical and demographic parameters among the QTcd groupings
DISCUSSION
The study revealed that a significant proportion of newly diagnosed hypertensive Nigerian seen in the cardiac clinic are already at increased cardiovascular risk considering the fact that abnormal QT interval (both prolonged maximum QT interval and increased QT dispersion are associated with increased cardiovascular risk. The prevalence of prolonged QTc in this study was 52.14%. Over 54% of the male population and about half of the females had prolonged QTc max. This is similar to the report by Familoni and Olunuga among subjects with acute ischemic stroke.[21] The study also revealed that the prevalence of increased QTcd≥80ms was 36.43% among hypertensive subjects in this study and 18.57% among normal controls. The frequency of occurence of increased QTcd≥80ms was however greater in this study than that by Familoni et al.[21]
This study corroborates similar conclusions by other authors that newly diagnosed hypertensive subjects in developing nations like Nigeria are already more likely to have more target organ damage and excessive cardiovascular morbidity.[9,10] A similar study in Northern Nigeria reported that 92% of treated hypertensive subjects had QTcd>39 milliseconds.[22] The same study also reported that QTcd was well correlated with systolic blood pressure and left ventricular mass index among treated hypertensive subjects. They also demonstrated that prolonged QTc was found in hypertensives with more severe disease as reported among Caucasians.[23] There seems to be no gender association with QT abnormalities in this study. Other studies have shown that QT interval abnormalities are more common among females. However, majority of the female participants are premenopausal and the increased cardiovascular risk associated with menopause may play a role in the female gender association with QT abnormalities.
Hypertensive subjects with prolonged QT intervals were likely to be obese than those with normal QT intervals. Obesity may, therefore, contribute more significantly to prolonged QT intervals among newly diagnosed hypertensive subjects than the level of systolic or diastolic blood pressure. Body mass index and waist circumference are important determinants of left ventricular mass which has been shown to be well correlated with QT intervals.[16,23]
Hypertension is therefore associated with prolonged maximum QT interval and increased QTc dispersion in a similar way it is associated with the increased risk of left ventricular hypertrophy and clustering of other cardiovascular risk factors. These newly diagnosed hypertensive subjects with prolonged QT interval and QT dispersion are therefore at an increased cardiovascular risk compared to others with normal QT intervals.
The consistency in the frequency of QTcd and prolonged QTc max suggests that there is a relationship between prolonged QTc max and increased QTcd in this study as both were well correlated to similar clinical and demographic factors. QT prolongation and increased QTc dispersion were not significantly associated with female gender in this study. Other studies however has shown that females tend to have more of prolonged QT intervals than their male counterparts.[24]
Prolonged QTc (Qtcmax≥440ms) and increased QTcd(QTcd≥80ms) have been observed to be good predictors of arrhythmia and sudden cardiac death in such conditions as long QT syndrome, hypertrophic cardiomyopathy, hypertension, chronic heart failure, post myocardial infarction patients,[25,26] and in diabetes mellitus patients.[27] Indeed some studies have suggested that prolonged QTcd is an independent and stronger risk factor for cardiac mortality in the elderly, stronger than left ventricular hypertrophy and systemic hypertension.[28]
Patients with prolonged QTc max >440ms and increased QTcd have an increased risk of dying from cardiovascular disease. Several studieshave associated this to an increasing ventricular inhomogeneity of the myocardium and associated predisposition to cardiac arrhythmias.[29–30] The pattern of QT parameters in this study population was similar to what was found among the Caucasians and similar studies reported among Nigerian subjects.[21,22,31] The fact that about half of newly diagnosed hypertensive subjects had prolonged QT intervals which is a noninvasive stratification tool highlight the enormous role of early implementation of total cardiovascular care including adequate stratification and management for newly diagnosed hypertensive subjects.
Hypertensive subjects with prolonged QT intervals in this study were of similar age with those with normal QT intervals. However, among normal controls, those with prolonged maximum QTc were well younger in age suggesting the possible contribution of congenital long QT syndrome and impact of drugs not reported by patients. None of these however reported associated ear or eye complaints.
In conclusion, maximum QTc prolongation and increased QTc dispersion are very prevalent among newly diagnosed hypertensive Nigerian subjects. Obesity seems to be well associated with prolonged QT intervals among them. Also, prolonged QT intervals and increased QTc dispersion can therefore serve as noninvasive marker of hypertensive with increased cardiovascular risk and can therefore be an effective screening for reduction of cardiovascular morbidity and mortality in the population. Therefore, aggressive control of blood pressure, appropriate lifestyle modification campaign to combat the rising frequency of obesity and the use of drugs such as angiotensin converting enzyme inhibitors (ACE-I) or angiotensin receptor blockers (ARB) may be the best form of preventive strategy to reduce the frequency of prolonged QTc and QTcd in subjects with hypertension. These drugs have been shown to regress LVH and also cause reversal of prolonged QT intervals in subjects with hypertension.[24,32–34]
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
REFERENCES
- 1.Akinkugbe OO. Current epidemiology of hypertension in Nigeria. Arch of Ibadan Med. 2001;1:3–4. [Google Scholar]
- 2.Cooper R, Rotimi C, Ataman S, McGee D, Osotimehin B, Kadiri S. The prevalence of hypertension in seven populations of West African origin. Am J Public Health. 1997;87:160–8. doi: 10.2105/ajph.87.2.160. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Kadiri S, Walker O, Salako BL, Akinkugbe O. Blood pressure, hypertension and correlates in urbanized workers in Ibadan, Nigeria: Arevisit. J Hum Hypertens. 1999;13:23–7. doi: 10.1038/sj.jhh.1000722. [DOI] [PubMed] [Google Scholar]
- 4.Ulasi II, Ijoma CK, Onwubere BJ, Arodiwe E, Onodugo O, Okafor C. High prevalence and low awareness of hypertension in a market population in enugu, Nigeria. Int J Hypertens. 2011;2011:869675. doi: 10.4061/2011/869675. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Isezuo SA. Systemic hypertension in blacks:An overview of current concepts of pathogenesis and management. Niger PostgradMed J. 2003;10:144–53. [PubMed] [Google Scholar]
- 6.Chobanian AV, Bakris GL, Black HR, Cushman WC, Green LA, Izzo JL., Jr For the National high Blood Pressure Education program coordinating committee. Seventh report of the Joint National committee on prevention, detection, evaluation and treatment of high blood pressure JNC VII. Hypertens. 2003;12:1206–52. doi: 10.1161/01.HYP.0000107251.49515.c2. [DOI] [PubMed] [Google Scholar]
- 7.Yusuf S, Reddy S, Ounpuu S, Anand S. Global burden of cardiovascular diseases: Part 1: General considerations, the epidemiologic transition, risk factors and impact of urbanization. Circulation. 2001;104:2746–53. doi: 10.1161/hc4601.099487. [DOI] [PubMed] [Google Scholar]
- 8.European Society of Hypertension–European Society of Cardiology Guidelines Committee. 2003 European Society of Hypertension-European Society of Cardiology guidelines for the management of arterial hypertension. J Hypertens. 2003;21:1011–53. doi: 10.1097/00004872-200306000-00001. [DOI] [PubMed] [Google Scholar]
- 9.Cooper R, Rotimi C. Hypertension in blacks. AmJHypertens. 1997;10:804–12. doi: 10.1016/s0895-7061(97)00211-2. [DOI] [PubMed] [Google Scholar]
- 10.Haider AW, Larson MG, Benjamin EJ, Levy D. Increased left ventricular mass and hypertrophy are associated with increased risk for sudden death. J Am CollCardiol. 1998;32:1454–9. doi: 10.1016/s0735-1097(98)00407-0. [DOI] [PubMed] [Google Scholar]
- 11.August P. Initial management of hypertension. N Engl J Med. 2003;348:610–7. doi: 10.1056/NEJMcp010357. [DOI] [PubMed] [Google Scholar]
- 12.MacMahon S, Peto R, Cutler J, Collins R, Sorlie P, Neaton J, et al. Blood pressure, stroke and coronary heart disease. Part 1,Prolonged differences in blood pressure: Prospective observational studies corrected for the regression dilution bias. Lancet. 1990;335:774–85. doi: 10.1016/0140-6736(90)90878-9. [DOI] [PubMed] [Google Scholar]
- 13.Salako BL, Ogah OS, Adebiyi AA, Adedapo KS, Bekibele CO, Oluleye TS. Unexpectedly high prevalence of target-organ damage in newly diagnosed Nigerians with hypertension. Cardiovasc J Afr. 2007;18:77–83. [PubMed] [Google Scholar]
- 14.Ayodele OE, Alebiosu CO, Salako BL, Awoden OG, Adigun AD. Target organ damage and associated clinical conditions among Nigerians with treated Hypertension. CardiovascJ SAfr. 2005;16:89–93. [PubMed] [Google Scholar]
- 15.Kuo CS, Reddy CP, Munakata K, Surawicz B. Mechanism of ventricular arrhythmias caused by increased dispersion of repolarization. Eur Heart J. 1985;6:63–70. doi: 10.1093/eurheartj/6.suppl_d.63. [DOI] [PubMed] [Google Scholar]
- 16.Festa A, D’Agostino R, Jr, Rautaharju P, Mykkänen L, Haffner SM. Relation of blood pressure, left ventricular mass, insulin sensitivity, and coronary artery disease to QT interval duration in nondiabetic and type 2 diabetic subjects. Am JCardiol. 2000;86:1117–22. doi: 10.1016/s0002-9149(00)01170-x. [DOI] [PubMed] [Google Scholar]
- 17.Prochnau D, Kuehnert H, Figulla HR, Surber R. QRS duration and QTc interval are predictors of risk for ventricular arrhythmias during cardiac resynchronization therapy. ActaCardiol. 2011;66:415–20. doi: 10.1080/ac.66.4.2126587. [DOI] [PubMed] [Google Scholar]
- 18.Barr CS, Naas A, Freeman M, Lang CC, Struthers AD. QT dispersion and sudden unexpected death in chronic heart failure. Lancet. 1994;343:327–9. doi: 10.1016/s0140-6736(94)91164-9. [DOI] [PubMed] [Google Scholar]
- 19.Crawford MH, Bernstein SJ, Deedwania PC, DiMarco JP, Ferrick KJ, Garson A, Jr, et al. ACC/ AHA guidelines for ambulatory electrocardiography: Executive summary and recommendations. A report of the American College of Cardiology/American Heart Association task force on practice guidelines (committee to revise the guidelines for ambulatory electrocardiography) Circulation. 1999;100:886–93. doi: 10.1161/01.cir.100.8.886. [DOI] [PubMed] [Google Scholar]
- 20.Bazett HC. An analysis of the time-relations of electrocardiograms. Heart. 1920;7:353–70. [Google Scholar]
- 21.Familoni OB, Odusan O, Ogun SA. The pattern and prognostic features of QT intervals and Dispersion in patients with acute ischaemic stroke. J Natl Med Assoc. 2006;98:1758–62. [PMC free article] [PubMed] [Google Scholar]
- 22.Sani IM, Solomon DS, Imhogene OA, Ahmad AM, Bala GS. QT Dispersion in AdultHypertensives. JNatlMedAssoc. 2006;98:631–6. [PMC free article] [PubMed] [Google Scholar]
- 23.Clarkson PB, Naas AA, McMahon A, MacLeod C, Struthers AD, MacDonald TM. QT dispersion in essentialhypertension. QJM. 1995;88:327–32. [PubMed] [Google Scholar]
- 24.Matsuno Y, Minatoguchi S, Fujiwara H GIFU Substudy Group of the Case-J Trial. Effect of candersartan versus amlodipine on home-measured blood pressure, QT dispersion and left ventricular hypertrophy in high-risk hypertensive patients. Blood Press Suppl. 2011;1:12–9. doi: 10.3109/08037051.2010.532339. [DOI] [PubMed] [Google Scholar]
- 25.Mayet J, Shahi M, McGrath K, Poulter NR, Sever PS, Foale RA, et al. Left ventricular hypertrophy and QT dispersion in hypertension. Hypertension. 1996;28:791–6. doi: 10.1161/01.hyp.28.5.791. [DOI] [PubMed] [Google Scholar]
- 26.Saadeh A, Evan S, James M, Jones J. QTc dispersion and complex ventricular arrhythmias in untreated newly presenting hypertensive patients. J Hum Hypertens. 1999;13:665–9. doi: 10.1038/sj.jhh.1000908. [DOI] [PubMed] [Google Scholar]
- 27.Linneman B, Jankea HU. Prolonged QTc interval and elevated heart rate identify the type 2 diabetic patient at high risk for cardiovascular death: The Bremman Diabetes Study. Exp Clin Endocrinol Diabetes. 2003;111:215–22. doi: 10.1055/s-2003-40466. [DOI] [PubMed] [Google Scholar]
- 28.deBruyne MC, Hoes AW, Kors JA, Hofman A, van Bemmel JH, Grobbee DE. QTc dispersion predicts cardiac mortality in the elderly: The Rotterdam study. Circulation. 1998;97:467–72. doi: 10.1161/01.cir.97.5.467. [DOI] [PubMed] [Google Scholar]
- 29.Opadijo OG, Omotosho AB, Araoye MA. Ventricular arrhythmias: QT Prolongation and left ventricular hypertrophy in adult Nigerians with hypertensive heart disease. Niger Postgrad MedJ. 2003;10:76–8. [PubMed] [Google Scholar]
- 30.Robbins J, Nelson JC, Rahtaharju PM, Gottdiener JS. The association between the length of the QT interval and mortality in the Cardiovascular Health Study. AmJMed. 2003;115:689–94. doi: 10.1016/j.amjmed.2003.07.014. [DOI] [PubMed] [Google Scholar]
- 31.Peng S, Yu V, Han K, Xing H, Li D, Chen C, et al. Heart rate corrected QT interval duration is significantly associated with blood pressure in Chinese population. J Electrocardiol. 2006;39:206–10. doi: 10.1016/j.jelectrocard.2005.08.007. [DOI] [PubMed] [Google Scholar]
- 32.Karjalainen J, Reunanen A, Ristola P, Viitasalo M. QT interval as a Cardiac risk factor in a middle aged population. Heart. 1997;77:543–8. doi: 10.1136/hrt.77.6.543. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Elming H, Holm E, Jun L, Torp-Pedersen C, Køber L, Kircshoff M, et al. The prognostic value of the QT interval and QT interval dispersion in all cause and cardiac mortality and morbidity in a population of Danish citizens. Eur Heart J. 1998;19:1391–400. doi: 10.1053/euhj.1998.1094. [DOI] [PubMed] [Google Scholar]
- 34.Poirier P, Giles TD, Bray GA, Hong Y, Stern JS, Pi-Sunyer FX, et al. Obesity and Cardiovascular disease: Pathophysiology, evaluation and effect of weight loss. An Update of the 1997 American Heart Association Scientific Statement on Obesity and Heart Disease from the Obesity Committee of the Council on Nutrition, Physical Activity, and Metabolism. Circulation. 2006;113:898–918. doi: 10.1161/CIRCULATIONAHA.106.171016. [DOI] [PubMed] [Google Scholar]


