Abstract
A 34 year-old male patient presented with recurrent attack of palpitation and chest pain due to Wolf Parkinson White syndrome (WPWS). Two dimensional echocardiography demonstrated features of Ebstein's anomaly along with biventricular non compaction. Color flow Doppler studies confirmed the presence of blood flow within the trabeculations. Biventricular myocardial non-compaction associated with Ebstein's anomaly who presented with WPWS is a very rare association. So far, Medline search revealed only three reported cases in the literatures. The patient was treated with radiofrequency ablation of right sided posteroseptal accessory pathway of WPWS and was asymptomatic in further follow-up.
Keywords: Ebstein's anomaly, Non compaction of myocardium, Radiofrequency ablation, Wolf Parkinson White syndrome
INTRODUCTION
Ebstein's anomaly is a rare congenital heart malformation affecting about 1 in 200,000 live births.[1] It is characterized by apical displacement and adherence of the septal and posterior leaflets of the tricuspid valve to the underlying myocardium, thereby displacing the functional tricuspid orifice apically and dividing the right ventricle into two portions.[1] The main hemodynamic abnormality which leads to symptoms is tricuspid valve incompetence. These patients may be asymptomatic or experience right-sided heart failure, cyanosis, arrhythmias and sudden cardiac death (SCD).[1] Associated abnormalities of left ventricular morphology and function including left ventricular non compaction (LVNC) have been reported.[2–7] Non-compaction of the ventricular myocardium is also a rare congenital cardiomyopathy, presumably resulting from an arrest in normal endomyocardial embryogenesis.[2] The myocardium of the left ventricle is most often affected, but biventricular non-compaction is also possible. Non-compaction of the ventricular myocardium is characterized by numerous excessively prominent trabeculations and deep inter trabecular recesses.[2] Recently, mutations in the sarcomeric protein gene β-myosin heavy chain (MYH7) were described in patients with Ebstein's anomaly associated with LVNC.[1] Interestingly, a higher incidence of WPWS was found in children with isolated non compaction of the ventricular myocardium and in patients with Ebstein's malformation.[6] So far, there have been only two reports of three cases on biventricular non compaction of the ventricular myocardium associated with Ebstein's malformation.[3,8]
We are reporting this case who presented to us with WPWS and after investigations, found to have biventricular non compaction associated with Ebstein's anomaly.
CASE REPORT
A 31-year-old male presented to our hospital for evaluation of recurrent palpitation and chest pain over the past two years. The patient didn’t have symptoms like exertional dyspnoea, orthopnoea, effort intolerance or fatigue. He was completely asymptomatic before this period. His family history was also uneventful. On general physical examination, he was looking healthy with normal built and there was absence of clinical cyanosis (oxygen saturation- 97% on room air), pedal edema, and clubbing or engorged neck vein. On examination, his blood pressure was 120/78 mm Hg; pulse 74 beat per minute. Cardio vascular examination revealed an ejection systolic heart murmur grade 2/6 present in the left inferior parasternal area. Other systemic examinations didn’t reveal any abnormality. Chest X-ray revealed there was no cardiomegaly and cardiothoracic ratio was 0.45 with no pulmonary congestion. The laboratory examinations revealed normal complete blood count, blood sugar, renal and liver function. The electrocardiogram revealed right postero-septal accessory pathway of WPWS. Transthoracic echocardiography (TTE) revealed numerous large trabeculations and deep intra-trabecular recesses at the apex, lateral wall, and the apical part of the inter-ventricular septum of left ventricles along with hyper trabeculation of right ventricle [Figure 1]. Color flow Doppler examination confirmed the presence of blood flow within the trabeculae. The size and ejection fraction (60%) of the LV was normal. The ratio between non-compacted and compacted area in the parasternal short axis view was 2.5. About ten segments of LV were affected by non-compaction. The attached margins of the septal and inferior leaflets of the tricuspid valve were apically displaced and color flow Doppler showed mild tricuspid regurgitation. The apical displacement of septal leaflet of tricuspid valve was 13.6 mm/m2 and the distance between the mitral and tricuspid annuli was 23.7 mm [Figure 2]. There was absence of any atrial and ventricular septal defect, patent ductus arteriosus, coarctation of aorta or left ventricular outflow tract obstruction. Though the right ventricle showed increased trabeculations but there was no dilatation. It had normal systolic function and the pulmonary artery systolic pressure was only 24 mm of Hg. The right atrium was moderately enlarged. As the patient had recurrent palpitation and WPWS, he was treated with radiofrequency ablation of the accessory pathway. On follow-up up to six months, he was asymptomatic and the biventricular systolic function was preserved.
Figure 1.
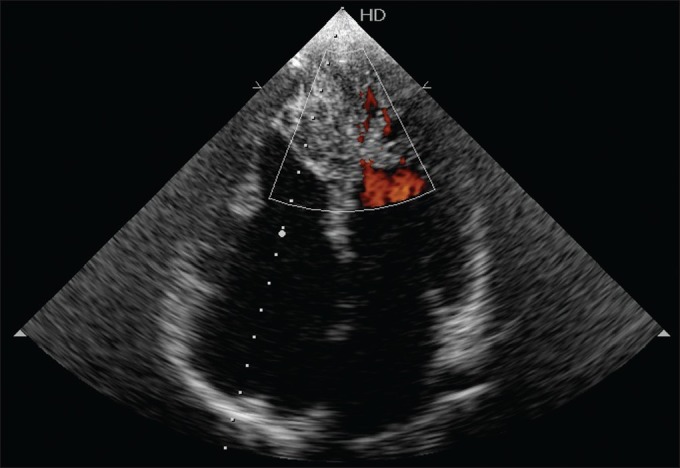
TTE image showing numerous large trabeculations and deep intra trabecular recesses at the apex, lateral wall, and the apical part of the inter ventricular septum of left ventricle along with right ventricular hyper trabeculation
Figure 2.
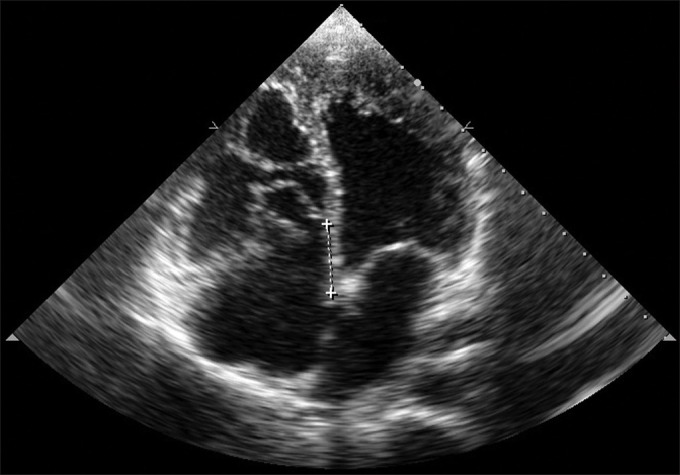
TTE reveal apical displacement of septal and inferior leaflets of the tricuspid valve and color flow Doppler showed mild tricuspid regurgitation. The distance between the mitral and tricuspid annuli was 2.37 cm
DISCUSSION
Ventricular non-compaction is categorized as an unclassified cardiomyopathy by the World Health Organization.[2] It is a result of an arrest in myocardial morphogenesis and is characterized by excessively prominent trabeculations in ventricular wall segments and deep inter trabecular recesses.[2] The myocardium of the left ventricle is most often affected, mainly affecting the apex and mid-apical portions of the lateral and inferior walls of the LV, but biventricular non compaction is also possible.[6] Echocardiography is the diagnostic modality of choice for non-compaction.[6] The evidence for direct blood flow from the ventricular cavity into deep intra-trabecular recesses by color Doppler echocardiography, and a two-layered structure of the LV wall, with a thin compacted epicardial, and much thicker non-compacted endocardial zones are needed for diagnosis.[3] In order to obtain a more accurate diagnosis, calculation of the ratio of non-compacted to compacted zones at end-systole and end-diastole is recommended. A ratio of >2 is considered to be diagnostic for non-compaction.[3] Although there are no established criteria for non-compaction in the right ventricle, right ventricular non-compaction (RVNC) has been reported in some cases in whom the diagnosis of RVNC were pretty dependent on TTE.[5] The most common finding is an LV myocardial abnormality resembling mild non-compaction,[6] like in our case. Recent studies have identified MYH7 mutations as a cause of Ebstein's anomaly associated with LVNC and other congenital heart disease (CHD).[1] So far, there were only three reported cases of biventricular non-compaction associated with Ebstein's malformation.[3,8] All these cases had LV dilatation and reduced systolic function in varying degrees. The poor prognosis in ventricular non-compaction has been associated with poor functional capacity and systolic dysfunction of LV.[3] In contrast, patients without heart failure can remain asymptomatic for a long period as in our patient who had a favourable long term follow-up.[7] The prompt recognition of non-compaction is extremely important because of its high mortality and morbidity due to progressive heart failure, thromboembolism and malignant arrhythmias.[6]
Our case presents another association of Ebstein's anomaly with biventricular non-compaction. Biventricular systolic and diastolic functions were normal. This finding shows that he has mild type anomaly. But he was symptomatic due to WPWS. Ebstein's anomaly is a congenital cardiac disorder that is not confined to the right heart. We recommend patients with Ebstein's anomaly to be carefully evaluated for LVNC, and if present, early treatment of patients at risk for complications of LVNC.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
REFERENCES
- 1.Van Engelen K, Postma AV, van de Meerakker JB, Roos-Hesselink JW, Helderman-van den Enden AT, Vliegen HW, et al. Ebstein's anomaly may be caused by mutations in the sarcomere protein gene MYH7. Neth Heart J. 2011 doi: 10.1007/s12471-011-0141-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Attenhofer Jost CH, Connolly HM, Warnes CA, O’leary P, Tajik AJ, Pellikka PA, et al. Non compacted myocardium in Ebstein's anomaly: Initial description in three patients. J Am Soc Echocardiogr. 2004;17:677–80. doi: 10.1016/j.echo.2004.02.013. [DOI] [PubMed] [Google Scholar]
- 3.Sinkovec M, Kozelj M, Podnar T. Familial biventricular myocardial non-compaction associated with Ebstein's malformation. Int J Cardiol. 2005;102:297–302. doi: 10.1016/j.ijcard.2004.05.033. [DOI] [PubMed] [Google Scholar]
- 4.Arslan S, Gurlertop HY, Gundogdu F, Senocak H. Left ventricular non-compaction and mid-caviter narrowing associated with Ebstein's anomaly: Three-dimensional transthoracic echocardiographic image. Int J Cardiol. 2007;115:e52–5. doi: 10.1016/j.ijcard.2006.07.117. [DOI] [PubMed] [Google Scholar]
- 5.Song ZZ. A combination of right ventricular hyper trabeculation/non-compaction and Ebstein's anomaly. Int J Cardiol. 2010;143:e30–3. doi: 10.1016/j.ijcard.2008.12.024. [DOI] [PubMed] [Google Scholar]
- 6.Attenhofer Jost CH, Connolly HM, O’Leary PW, Warnes CA, Tajik AJ, Seward JB. Left heart lesions in patients with Ebstein's anomaly. Mayo Clin Proc. 2005;80:361–8. doi: 10.4065/80.3.361. [DOI] [PubMed] [Google Scholar]
- 7.Saltik L, Eroğlu E, Bayrak F, Değertekin M. Left ventricular non-compaction associated with Ebstein's anomaly. Turk Kardiyol Dern Ars. 2009;37:269–72. [PubMed] [Google Scholar]
- 8.Baysan O, Yokuşoğlu M, Bugan B, Demirkol S. E-page original images. A case of Ebstein's anomaly and biventricular non-compaction. Anadolu Kardiyol Derg. 2010;10:E26. doi: 10.5152/akd.2010.178. [DOI] [PubMed] [Google Scholar]


