Abstract
Background & objectives:
India contributes a significant number of deaths attributed to coronary artery disease (CAD) compared to the rest of the world. Data on catastrophic health expenditure (CHE) related to acute coronary syndrome (ACS), the major cause of deaths in CAD, are limited in the literature. We estimated the magnitude of CHE and studied the strategies used to cope with CHE.
Methods:
Two hundred and ten ACS patients (mean age 56 yr, 83% men) were randomly selected proportionately from six hospitals in Thiruvananthapuram district, Kerala, India. Information on demographics, ACS-related out-of-pocket expenditure and coping strategies was collected using a pre-tested structured interview schedule. CHE, defined as ACS-related expenditures exceeding 40 per cent of a household's capacity to pay, was estimated using the World Health Organization methods. Health security was defined as protection against out-of-pocket expenditure through an employer or government provided social security scheme. Socio-demographic variables, effect on participants’ employment, loans or asset sales for treatment purposes, health security coverage and type of treatment were considered as potential correlates of CHE. Multiple logistic regression analyses were conducted to identify the correlates of CHE.
Results:
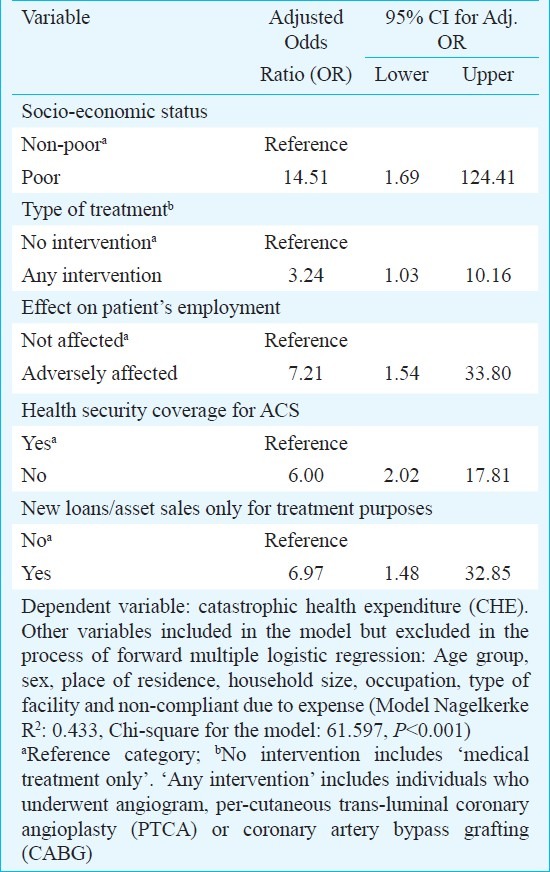
CHE was experienced by 84 per cent (95% CI: 79.04, 88.96) of participants as a consequence of treating ACS. Participants belonging to low socio-economic status (SES) were 15 times (odds ratio (OR): 14.51, 95% CI: 1.69-124.41), whose jobs were adversely affected were seven times (OR: 7.21, CI: 1.54-33.80), who had no health security were six times (OR: 6.00, CI: 2.02-17.81) and who underwent any intervention were three times (OR: 3.24, CI: 1.03-10.16) more likely to have CHE compared to their counterparts. The coping strategies adopted by the participants were loans (41%), savings (14%), health insurance (8%) and a combination of the above (37%).
Interpretation & conclusions:
Our findings show that viable financing mechanism for treating ACS is warranted to prevent CHE particularly among low SES participants, those having no health security, requiring intervention procedures and those with adversely affected employment.
Keywords: Cardiovascular diseases, catastrophic health expenditure, coping strategies, coronary artery disease, epidemiology, heart diseases, lifestyle, myocardial infarction
India contributed 1.5 million of the total 7.5 million deaths attributable to coronary artery disease (CAD) in 20021 and the trend is increasing2. Urbanization, stress, unhealthy diet, physical inactivity and increase in tobacco smoking had contributed substantially to this large number of CAD deaths3. Both CAD morbidity and mortality are seen at a much younger age in South Asia, compared to the west4.
The southern most Indian State of Kerala, reported the highest proportion of CAD (rural - 7.5%, urban - 12%) based on epidemiological studies from various parts of India during 1965 to 20055. A twenty-fold increase in admissions due to acute myocardial infarction (MI) was recorded in a single medical college hospital from 1966 to 19885. Kerala also has high prevalence of most known risk factors: current smoking: men-39.7 per cent, women-0.4 per cent, overweight (BMI > 25.0 kg/m2): men-23.9 per cent, women-37.5 per cent, unhealthy diet (< five servings of fruits and vegetables/day): men-42.9 per cent, women-50.9 per cent, diabetes (fasting blood sugar > 126 mg/dl or on medication): men-14.3 per cent, women-17.8 per cent, hypercholesterolaemia (total cholesterol > 200 mg/dl): men-51.4 per cent, women-61.5 per cent and hypertension (JNC VII): men-33.9 per cent, women-31.6 per cent6. CAD being a chronic illness with catastrophically high cost of care drives, individuals and their families below poverty line if they are not supported by public funding7. However, the per capita public health expenditure as a proportion of the State Domestic Product (SDP) in Kerala, which was one among the highest for any Indian State, decreased by 35 per cent between 1990 and 2002 making it, one of the States with the highest reduction in public contribution and the highest increase in private funding for health care8. Currently, in terms of health financing Kerala State has the highest private expenditure compared to any other State in India (90.3%)9.
While the term coronary artery disease covers a wide variety of acute and chronic cardiac manifestations of atherosclerosis, this study deals with acute coronary syndrome (ACS), which encompasses ST-segment and non-ST-segment elevation myocardial infarction and unstable angina10. The treatment of acute coronary syndrome could be disastrously expensive, a phenomenon termed as ‘catastrophic health expenditure (CHE)7. Expenditures greatly affect compliance when the ideal drug therapy is unaffordable for most, health insurance is virtually non-existent, majority of the expenses are borne out-of-pocket and public provisioning of health care is inadequate11,12. In such circumstances, it is not the ‘willingness to pay’ that plays the crucial role, rather the ‘ability to pay’. Unregulated health care markets such as India tend to favour the affluent when the determining factor of treatment option offered to the participants is not the real treatment indication but the need to enhance hospital performance through procedure volumes13. Consequently, the poor either do not reach the health system or receive sub-standard care14. Protecting people from catastrophic health expenditure is both a function of health systems and a ‘desirable objective of health policy’15,16.
While cost estimations have been done for CAD in general, no data on out-of-pocket expenditure were available for ACS17. The available estimations are done from the health system point of view, in terms of ‘costs of production’ of care and services. This macro-level approach where everything is viewed as cost to the State machinery, may hide micro-level consequences to the individuals and households, hence this exploratory study was carried out to identify the various correlates of CHE through the use of primary data and to address the following questions: (i) What proportion of ACS patients experience catastrophic health expenditure as a consequence of treating acute coronary syndrome and what are its predictors?, and (ii) Which coping mechanisms do households employ to manage the expenses?
Material & Methods
The cross-sectional survey was conducted during June - September 2008 in Thiruvananthapuram district of Kerala that had a human development index of 0.773, which was same as that of the State as a whole making it fairly comparable18.
Assuming an α-error of five per cent and power of 90 per cent, the required minimum sample size, to detect a difference of Indian rupees  50,000 in mean ACS-related expenditure between two groups with a standard deviation of
50,000 in mean ACS-related expenditure between two groups with a standard deviation of  60,000 was calculated to be 30. To consider a total of six such groups, i.e., three income groups and two age-groups, the sample size was estimated to be 180. The sample size was increased to 210 in order to account for non-response, change of address and death.
60,000 was calculated to be 30. To consider a total of six such groups, i.e., three income groups and two age-groups, the sample size was estimated to be 180. The sample size was increased to 210 in order to account for non-response, change of address and death.
During the enumeration it was found that the smallest hospital where the service of a cardiologist was available had at least 100 beds. The district had 16 hospitals with a cardiologist, of which nine had cardiac catheterization facilities. Among these nine hospitals two were government hospitals and both consented for the study. Among the seven private hospitals with cardiac catheterization facility only two consented. Of the seven private hospitals without cardiac catheterization facilities only two consented making a total of six hospitals participating in the study. All men and women aged 25 to 70 yr who had their acute event, defined as first episode of ACS after March 1, 2007 and at least six months before the date of interview, and diagnosed as ACS with chest pain and either electrocardiograph changes or enzyme elevation (Cardiac Troponin I or T / Creatine Kinase MB)15 and admitted in these six hospitals, were included in the sampling frame (N=650). Deaths, pregnant women, patients with co-morbidities like stroke and peripheral vascular disease and prior documented myocardial infarction were excluded. From each hospital, participants were selected proportional to the patient load and within each hospital proportional to the income categories so that the sample was self-weighting.
Ethical clearance was obtained from the Institutional Ethics Committee (IEC) of the Sree Chitra Tirunal Institute for Medical Sciences and Technology, Thiruvananthapuram. Permission from the hospitals and written informed consent from all participants were obtained.
Using a pre-tested structured interview schedule, the first author (MD) collected the data at the residence of the study participants. All the diagnoses were confirmed by discharge summaries. Expenditure data were collected as reported by the participants and 80 per cent of the hospitalization expenditures were verified by either hospital bills or written expenditure statements and these were found to be comparable with the reported expenditure. Total household expenditure (THHE) defined as the sum total of a household's consumption expenditure excluding the ACS-related expenditure was collected using mixed recall period i.e., a 12-month recall period for six infrequently purchased non-food items, namely clothing, footwear, durable goods, education, institutional medical expenses and insurance premiums and a 30-day recall period for the frequent expenses including food19.
ACS-related expenditure (both direct and indirect) was collected for three months pre-event and six months post-event. Direct expenditure included expenses related to hospitalization, medication, treatment and procedures, investigations, follow up consultations, informal payments, travel, food and lodging and expenses related to bystanders. Indirect expenditure included expenses incurred due to loss of income due to loss of job, change of job, denial of promotion and wage loss due to hospitalization, medically advised rest and follow up.
Expenses incurred in the pre-event period were related to any ACS-related symptomatic treatment/visits to multiple providers, and treatment and management of diabetes, hypertension or dyslipidaemias. The post-event period were expenses related to each of the hospitalization episodes including informal payments to doctors and other staff and any expenses pertaining to travel, food and lodging for both patient and bystanders; any expenses incurred after the acute event and in between the various hospitalization episodes including those incurred for follow up, medication or employment of extra help as a consequence of this illness; and income/wage loss to the patient, primary care giver or any other household member resulting from a shortfall in working days, change in nature of job or loss of job.
All hospitalization and follow up expenses excluding the expenses incurred for employment of extra help were considered as direct expenditure. Income or wage loss and the expenses incurred for employment of extra help were considered as indirect expenditure. All expenditures including THHE were adjusted for household size and duration of illness by calculating the respective per capita per month figures.
In the present study, out-of-pocket expenditure (OPE) was defined as the sum total of all ACS-related expenditures excluding any reimbursements. Catastrophic health expenditure was defined as ACS-related expenditures exceeding 40 per cent of a household's capacity to pay (CTP). Capacity to pay refers to the non-subsistence expenditure which is the difference between the THHE of a household and their subsistence expenditure (SE).
The catastrophic health expenditure was calculated as follow:
Step 1: Calculation of subsistence expenditure (SE)
Calculate food expenditure (FE)/total household expenditure (THHE)
Identify the 45th - 55th percentile of FE/THHE
SE = Mean FE of 45th - 55th of FE/THHE
Step 2: Calculation of capacity to pay (CTP)
CTP = THHE – SE (if FE > SE)
CTP = THHE – FE (if FE < SE)
Step 3: Calculation of catastrophic health expenditure (CHE)
CHE is present if out-of-pocket expenditure (OPE) is more than 40 per cent of a household's capacity to pay
Socio-economic status (SES) was based on tertiles of THHE, households were categorized into three SES groups; low, middle and high at the time of analysis.
Data analysis was done using SPSS for Windows, version 15.0. CHE was estimated using the 40 per cent threshold methodology that has been used by the World Health Organization16,19. Analyses were performed on log transformed outcome variables due to the skewed nature of the distributions. Bivariate analysis (Chi-square/Fisher's exact test) was used to compare proportions of CHE between groups. Forward step-wise multiple logistic regression (Likelihood ratio method) was used with probability for entry as 0.05 and removal as 0.10.
Results
The mean age of the study population (n=210) was 55.6 ± 8.9 yr, (range 25, 70 yr) and the mean household size was 4.0 ± 1.6, (range 1 - 13). The median per capita monthly household expenditure was  3051 (range 263 - 95,203). Women comprised only 16.7 per cent of the sample and 55 per cent resided in rural areas. Around half (48%) of the study participants had more than secondary education and 68 per cent were employed at the time of the survey. Half (51%,) of the participants reported having existing loans availed prior to their illness while only 29 per cent had some form of health security coverage, (partial or complete) for their ACS episode(s). The main co-morbidities reported were dyslipidaemia (67.6%), hypertension (56.7%) and diabetes (54.3%).
3051 (range 263 - 95,203). Women comprised only 16.7 per cent of the sample and 55 per cent resided in rural areas. Around half (48%) of the study participants had more than secondary education and 68 per cent were employed at the time of the survey. Half (51%,) of the participants reported having existing loans availed prior to their illness while only 29 per cent had some form of health security coverage, (partial or complete) for their ACS episode(s). The main co-morbidities reported were dyslipidaemia (67.6%), hypertension (56.7%) and diabetes (54.3%).
The summary estimates describing the distribution of ACS-related out-of-pocket expenditure in the sample population is shown in the Figure. All participants had out-of-pocket expenditure related to ACS in varying degrees. Even individuals with health security had some degree of OPE, mainly for follow up medication/investigations. CHE was experienced by 84 per cent (n=176) (95% CI: 79.04, 88.96). Direct health expenditure ranged from 8-100 per cent (median: 92%) of the total out-of-pocket expenditure.
Fig.
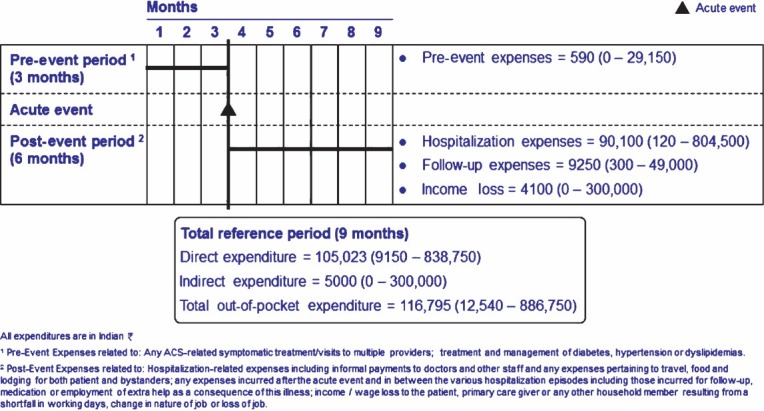
Median out-of-pocket expenditures in Indian rupees  (Minimum - Maximum) related to acute coronary syndrome. This figure describes the various expenditures in
(Minimum - Maximum) related to acute coronary syndrome. This figure describes the various expenditures in  , median (minimum - maximum) associated with acute coronary syndrome related to the acute event itself, the pre-event period (three months before the acute event) and the post-event period (till six months after the acute event).
, median (minimum - maximum) associated with acute coronary syndrome related to the acute event itself, the pre-event period (three months before the acute event) and the post-event period (till six months after the acute event).
In bivariate analysis, CHE was significantly more often (P < 0.01) in rural participants than urban participants (90% of 115 compared to 76% of 95); in poor socio-economic status subjects (99% compared to 76% in others); in less educated subjects (90% compared to 76% in others); in those with no health security coverage (93% compared to 62% in others); in those who were non-compliant (94% compared to 80% in others); in those whose employment status was adversely affected (97% compared to 76% in others): in those with loans/asset sales (93% than in others 57%) and in those with new loans/assets for sale (97% than in others 76%).
The predictors of CHE are shown in the Table. Being poor, employment being adversely affected, availing loans, having no health security coverage and undergoing any intervention were identified as predictors of CHE.
Table.
Correlates of catastrophic health expenditure: Results of multiple logistic regression analysis
Different coping strategies (defined as measures used by households to alleviate the out of pocket expenses that could not be managed from their regular income or savings) adopted by the participants to meet the expenses were analyzed. Loans were found to be the predominant coping strategy and were not confined to any particular socio-economic strata. Fourteen per cent (n=30) had financed their treatment exclusively from savings and of these 70 per cent (n=21) experienced CHE. Forty one per cent (n=85) of the study participants had financed their treatment solely from loans while 37 per cent (n=78) used a combination of loans, savings, gifts, insurance, etc. Seventeen participants (8%) had 62-98 per cent of their OPE covered by health insurance. Of these, 6 participants (35%) experienced CHE. Thirty six per cent (n=75) of previously loan-free households had to avail new loans for treatment over these nine months. In spite of this, 41 per cent (n=31) among those who availed new loans were non-compliant due to a lack of financial resources. Forty-seven per cent (n=30) of those who were non-compliant belonged to the low SES compared to only 13 per cent (n=8) from the high SES. Among daily-wage earners, 55 per cent (n=12) were non-compliant, as treatment was unaffordable.
Apart from these ‘obvious’ strategies to increase the household reserve, some households were also found to employ ‘masked’ strategies to check the drain on household reserves. Children discontinued their education, got transferred from private schools to free government schools and families moved out of expensive rental accommodation to cheaper ones or even moved in with willing relatives to cut expenditure. Among the fourteen primary care givers who reported an adverse impact of the illness on their employment, thirteen (93%) had taken up a job for the very first time to support their families.
Discussion
All participants had to meet their expenses with varying degrees of out-of-pocket expenditure; 84 per cent ending in CHE. As recommended interventions for diseases like ACS are known to be catastrophically expensive, this is not comparable to the CHE associated with general illnesses. Xu et al19 estimated CHE for all health-related expenses using national household income and expenditure surveys from 89 countries. It ranged form virtually zero per cent in countries like Czech Republic, Slovakia and United Kingdom to more than 10 per cent in Vietnam and Brazil19. This is likely to conceal the magnitude of CHE for diseases such as ACS. The overall positive relationship between proportion of households experiencing CHE and the share of OPE in total health expenditure has been well established16. Three key pre-conditions reported for CHE include health services that require payment, low capacity to pay and lack of prepayment or health financing mechanism16.
Out-of-pocket health expenditure leading to impoverishment is well known20. One-quarter of those hospitalized in India are impoverished due to OPE20. This is particularly relevant as low SES was found to be a major predictor of CHE and the poor have higher risk, tend to be less able to access timely medical care and develop rapidly progressive disease with early and sudden fatal outcomes21.
One of the predictors of CHE in our study was effect of participants’ employment. When an earning member becomes ill and employment is adversely affected, the family still has to survive and in addition take care of medical bills. In India, the share of informal employment (with no social security) was 76.7 per cent in urban areas and 94.8 per cent in rural areas in 1999-200022.
Taking loans and selling assets for treatment purposes was another major predictor for CHE. This was due to lack of free treatment in public sector hospitals for diseases such as ACS. In Kerala where proportion of public spending on health care is less than 10 per cent9 focusing on infectious diseases and maternal and child health problems, patients have no other choice other than to take loans or sell their assets for treatment of ACS.
Studies have found that those who are uninsured not only tend to have higher OPE, but are also less likely to seek medical care23. We identified lack of health security as a predictor for CHE which can be resolved by the implementation of social security measures as reported in Thailand. They saw a reduction in CHE from 31 per cent in 2000 to 14.6 per cent in 2004 among those using in-patient services after the introduction of universal coverage24. The provision of a health security measure has a dual advantage in that households especially the most vulnerable can not only avail treatment which otherwise they may not seek due to financial inaccessibility, but can also be spared from resorting to debt or asset financing thereby securing them against future risks as well. However, health-financing mechanism should not be considered synonymously with private health insurance and projected as the solution for CHE16,25. Private health insurance schemes often cover specific expenditure items related to treatment, mostly in-patient services, which form only a part of the expenditure for diseases such as ACS. It also leads to serious equity compromises without significant reductions in public health expenditure26. Pre-payment mechanisms most definitely seem to offer maximum protection, but it is the ‘social security’ type that has been the most promising26. Countries like Slovakia and Czech Republic finance 87 and 90 per cent of their total health expenditure, respectively through social security have virtually zero per cent catastrophic health expenditure16,27. A financially accessible health system with zero user fees and co-payments is possibly the best form of secure health financing.
As expected any intervention required for ACS resulted in CHE because of its higher costs compared to medical treatments resulting in reduced access and outcome for the poor, which was already reported from India28. The pattern of coping strategies was similar across other studies though the magnitude is higher in the present study owing to the higher expenditure involved25.
In conclusion, 84 per cent of the households across all socio-demographic strata experienced catastrophic health expenditure as a result of treating acute coronary syndrome. Being poor, employment being adversely affected, availing loans, having no health security coverage and undergoing any intervention were identified as predictors of CHE. Public facilities did not afford any kind of protection against catastrophic health expenditure.
On the policy front, the findings of this study highlight three major concerns. First, Kerala health system which is the most advanced in India is not geared towards the management of non-communicable diseases and is unable to mitigate the consequences of health shocks such as acute coronary syndrome. With deaths from chronic diseases projected to increase substantially, the scale of CHE is likely to be alarming. Second, the budgetary provision for health in the State is grossly inadequate. With a conservative estimate of 150,000 individuals developing acute myocardial infarction (a major proportion of ACS) in Kerala every year, the six month hospitalization expenditures alone work out to 13,515 million  , which is 105 per cent of the total public sector medical and public health expenditure for the State in 2007-085,29. As feared earlier, Kerala has started to sacrifice the welfare gains of the past and the market is gradually taking over the health sector in Kerala. While, individuals and households are largely burdened with this cost of care, the cost to the State machinery can only be staggering when the loss of production and productivity are also included. It becomes imperative to increase budgetary allocation to the health sector focusing on prevention of chronic diseases including ACS. Third, a viable financing mechanism for treating ACS is warranted to prevent CHE particularly among low SES participants, those having no health security, requiring intervention procedures and those with adversely affected employment.
, which is 105 per cent of the total public sector medical and public health expenditure for the State in 2007-085,29. As feared earlier, Kerala has started to sacrifice the welfare gains of the past and the market is gradually taking over the health sector in Kerala. While, individuals and households are largely burdened with this cost of care, the cost to the State machinery can only be staggering when the loss of production and productivity are also included. It becomes imperative to increase budgetary allocation to the health sector focusing on prevention of chronic diseases including ACS. Third, a viable financing mechanism for treating ACS is warranted to prevent CHE particularly among low SES participants, those having no health security, requiring intervention procedures and those with adversely affected employment.
Apart from the limitations of a cross-sectional survey, the sample size was small limiting the ability to look at sub-groups and interactions. The proportion of women in the sample was only 17 per cent. However, this was similar to the CREATE registry on ACS from India that had 23.6 per cent women28 and the ACS registry of Kerala that had 22.6 per cent of women30. Acute coronary syndrome patients are predominantly men in India. Also, cases in the community who may not seek care due to various reasons were totally excluded. However, this is unlikely to undermine the results of this study. Female participants were few, ruling out an in-depth analysis of gender-based differences. Only those hospitals which gave consent were included in the study. This might have led to a selection bias as it is possible that hospitals which refused permission were different from those who did not in terms of expenditure to the patient.
Acknowledgment
The authors acknowledge the Asia-Pacific Academic Consortium for Public Health (APACPH) Mini Grants 2008, Round 1 for providing the financial support, Dr T.K. Sundari Ravindran, Honorary Professor, AMCHSS, SCTIMST, Thiruvananthapuram for help in developing the tools for the study, Dr V. Raman Kutty, Professor, AMCHSS, SCTIMST, for his contributions in preparation and review of manuscript.
References
- 1.Atlas of heart disease and stroke. Chapter 14 - Deaths from coronary heart disease. Geneva: WHO; 2004. World Health Organization; pp. 48–9. [Google Scholar]
- 2.Prabhakaran D, Singh K. Premature coronary heart disease risk factors and reducing the CHD burden in India. Indian J Med Res. 2011;134:8–9. [PMC free article] [PubMed] [Google Scholar]
- 3.Yusuf S, Hawken S, Ounpuu S, Dans T, Avezum A, Lanas F, et al. Effect of potentially modifiable risk factors associated with myocardial infarction in 52 countries (the INTERHEART study): case-control study. Lancet. 2004;364:937–52. doi: 10.1016/S0140-6736(04)17018-9. [DOI] [PubMed] [Google Scholar]
- 4.Joshi P, Islam S, Pais P, Reddy S, Dorairaj P, Kazmi K, et al. Risk factors for early myocardial infarction in South Asians compared with individuals in other countries. JAMA. 2007;297:286–94. doi: 10.1001/jama.297.3.286. [DOI] [PubMed] [Google Scholar]
- 5.Cardiology Society of India, Kerala chapter. ACS Registry: Background information and rationale: Kerala Scenario. [accessed on March 2, 2009]. Available from: http://www.csikerala.org/acsregistry.php .
- 6.Thankappan KR, Shah B, Mathur P, Sarma PS, Srinivas G, Mini GK, et al. Risk factor profile for chronic non-communicable diseases: Results of a community-based study in Kerala, India. Indian J Med Res. 2010;131:53–63. [PubMed] [Google Scholar]
- 7.Preventing chronic diseases: a vital investment: WHO global report. Geneva: WHO; 2005. World Health Organization. Part 2-Chapter 2: Chronic diseases and poverty. [Google Scholar]
- 8.Levesque JF, Haddad S, Narayana D, Fournier P. Affording what's free and paying for choice: comparing the cost of public and private hospitalizations in urban Kerala. Int J Health Plann Manage. 2007;22:159–74. doi: 10.1002/hpm.879. [DOI] [PubMed] [Google Scholar]
- 9.Siva Kumar AK, Chen LC, Choudhury M, Ganju S, Mahajan V, Sinha A, et al. Financing health care for all: challenges and opportunities. Lancet. 2011;377:668–79. doi: 10.1016/S0140-6736(10)61884-3. [DOI] [PubMed] [Google Scholar]
- 10.Lloyd-Jones D, Adams R, Carnethon M, De Simone G, Ferguson TB, Flegal K, et al. American Heart Association Statistics Committee and Stroke Statistics Subcommittee. Heart Disease and Stroke Statistics-2009 Update: a report from the American Heart Association Statistics Committee and Stroke Statistics Subcommittee. Circulation. 2009;119:e21–e181. doi: 10.1161/CIRCULATIONAHA.108.191261. [DOI] [PubMed] [Google Scholar]
- 11.Nishtar S. Prevention of coronary heart disease in south Asia. Lancet. 2002;360:1015–8. doi: 10.1016/S0140-6736(02)11088-9. [DOI] [PubMed] [Google Scholar]
- 12.Mendis S, Fukino K, Cameron A, Laing R, Filipe A, Jr, Khatib O, et al. The availability and affordability of selected medicines for chronic diseases in six low- and middle-income countries. Bull World Health Organ. 2007;85:279–88. doi: 10.2471/BLT.06.033647. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Karthikeyan G, Xavier D, Dorairaj P, Pais P. Perspectives on the management of coronary artery disease in India. Heart. 2007;93:1334–8. doi: 10.1136/hrt.2007.131193. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Musgrove P, editor. Health economics in development. Washington DC: The World Bank; 2004. [Google Scholar]
- 15.The World Health Report 2000 - Health systems: improving performance. Geneva: WHO; 2000. World Health Organization. Chapter 2: How well do health systems perform? pp. 21–46. [Google Scholar]
- 16.Xu K, Evans DB, Kawabata K, Zeramdini R, Klavus J, Murray CJL. Household catastrophic health expenditure: a multicountry analysis. Lancet. 2003;362:111–7. doi: 10.1016/S0140-6736(03)13861-5. [DOI] [PubMed] [Google Scholar]
- 17.Liu JLY, Maniadakis N, Gray A, Rayner M. The economic burden of coronary heart disease in the UK. Heart. 2002;88:597–603. doi: 10.1136/heart.88.6.597. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Human Development Report 2005. Thiruvananthapuram, India: Centre for Development Studies; 2006. Government of Kerala; p. 60. [Google Scholar]
- 19.Xu K, Evans DB, Carrin G, Aguilar-Rivera AM, Musgrove P, Evans T. Protecting households from catastrophic health spending. Health Aff (Millwood) 2007;26:972–83. doi: 10.1377/hlthaff.26.4.972. [DOI] [PubMed] [Google Scholar]
- 20.Van Doorslaer E, O’Donnell O, Rannan-Eliya RP. Paying outof-pocket for health care in Asia: Catastrophic and poverty impact. EQUITAP Project: Working Paper # 2. [accessed on September 12, 2009]. Available from: http://www.ahrn.net/library_upload/uploadfile/file2979.pdf .
- 21.Yu Z, Nissinen A, Vartiainen E, Song G, Guo Z, Zheng G, et al. Associations between socioeconomic status and cardiovascular risk factors in an urban population in China. Bull World Health Organ. 2000;78:1296–305. [PMC free article] [PubMed] [Google Scholar]
- 22.Kucera D, Roncolato L. Informal employment: Two contested policy issues. Int Labour Rev. 2008;147:321–48. [Google Scholar]
- 23.Hwang W, Weller W, Ireys H, Anderson G. Out-of-pocket medical spending for care of chronic conditions. Health Aff (Millwood) 2001;20:267–78. doi: 10.1377/hlthaff.20.6.267. [DOI] [PubMed] [Google Scholar]
- 24.Limwattanonon S, Tangcharoensathien V, Prakongsai P. Catastrophic and poverty impacts of health payments: results from national household surveys in Thailand. Bull World Health Organ. 2007;85:600–6. doi: 10.2471/BLT.06.033720. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Flores G, Krishnakumar J, O’Donnell O, Van Doorslaer E. Coping with health-care costs: implications for the measurement of catastrophic expenditures and poverty. Health Econ. 2008;17:1393–412. doi: 10.1002/hec.1338. [DOI] [PubMed] [Google Scholar]
- 26.Paris: OECD; 2004. [accessed on October 10, 2008]. Organization for Economic Co-operation and Development - OECD. The OECD Health Project Summary Report - Towards high-performing health systems. Available from: http://www.oecd.org/ dataoecd/15/23/31737305.pdf . [Google Scholar]
- 27.World Health Statistics 2007. Geneva: World Health Organization; 2007. World Health Organization. Health System: Expenditures in health (2004) pp. 64–73. [Google Scholar]
- 28.Xavier D, Pais P, Devereaux PJ, Xie C, Prabhakaran D, Reddy KS, et al. Treatment and outcome of acute coronary syndromes in India (CREATE): a prospective analysis of registry data. Lancet. 2008;371:1435–42. doi: 10.1016/S0140-6736(08)60623-6. [DOI] [PubMed] [Google Scholar]
- 29.Thiruvananthapuram, India: 2009. [accessed on May 14, 2009]. Government of Kerala. Budget in brief: 2009-10. Available from: http://www.kerala.gov.in/ budget2009_10/budget_part_a.pdf . [Google Scholar]
- 30.Mohanan PP, Mathew R, Harikrishnan S, Krishnan MN, Zachariah G, Joseph J, et al. Presentation, management, and outcomes of 25 748 acute coronary syndrome admissions in Kerala, India: results from the Kerala ACS Registry. Eur Heart J. 2012 Sep 7; doi: 10.1093/eurheartj/ehs219. doi:10.1093/eurheartj/ehs219. [DOI] [PMC free article] [PubMed] [Google Scholar]


