Abstract
Purpose
To determine whether a visual aid improves the understanding and retention of information presented during informed consent for rural, indigent patients presenting for cataract surgery.
Materials and Methods
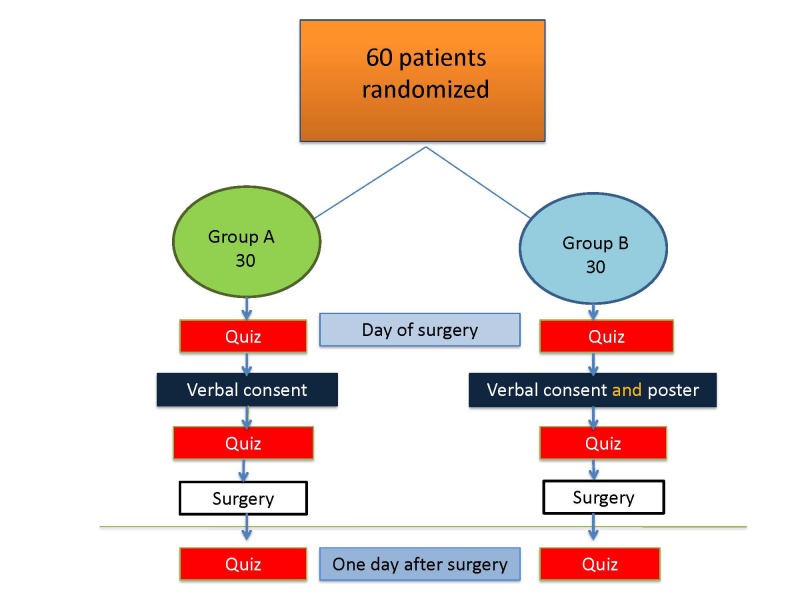
This was a randomized, unmasked, interventional study. We recruited patients who presented to the Hande Surgical Hospital in Chennai, India, for cataract surgery. Patients were randomized into two groups: verbal consent alone (group A) and verbal consent plus a poster (group B). Both groups completed an 11-question true/false quiz immediately before and after informed consent and one day after surgery.
Results
A total of 60 patients were recruited for the study, with 30 randomly assigned to each group; 23 patients from group A and 17 from group B completed the study. Informed consent improved patient scores in both groups; however, group B had significantly higher mean scores on postoperative day 1 (7.4 vs 8.7, P = 0.005) and significantly greater improvement in mean scores from pre–informed consent to postoperative day 1 (1.3 vs 3.6, P = 0.002).
Conclusions
Informed consent improves patient understanding of cataract surgery. Using a visual aid during informed consent for cataract surgery improves understanding and retention of information more than verbal consent alone in a rural South Indian population.
Multiple barriers to high-quality care exist for millions of indigent patients with pressing medical conditions.1–4 Ineffective communication between health care providers and patients is a major factor in reduced care.5–7 Roadblocks to effective communication can include limited formal education, illiteracy, and misinformation or misunderstanding among the population being served regarding medical interventions.5,7 Informed consent is a critical component of invasive medical procedures, helping to establish a healthy doctor-patient relationship by educating patients about the methods, risks, and benefits of procedures.8 Moseley et al9 examined the use of a poster and video presentation combined with a verbal informed consent in a highly educated population and demonstrated a significant increase in patient understanding of cataract surgery. In another study, the use of written pamphlets in addition to verbal discussion prior to cataract surgery showed an increase in information retention among patients.10 Methods used to communicate with patients in developed countries such as graphic tools and electronic multimedia–based programs may not be applicable to indigent populations in the developing world.11,12 In addition, written pamphlets and electronic programs can be prohibitively expensive in financially limited clinics. We aimed to determine whether a poster presentation combined with a verbal informed consent would be an effective means for educating cataract patients in rural South India.
Subjects and Methods
Patients from rural villages around Chennai, India, were recruited to participate in the study on the day they presented for scheduled cataract surgery. The Yale Human Subjects Committee approved the study, granting the project exemption from full review by the Institutional Review Board of Yale University under 45 CFR 46.101(b)(2). Moreover, the Uma Eye Clinic/Vision Foundation of Chennai, India, which is a partner organization to the Hande Surgical Hospital approved the conduct of the study via an informal review committee. A total of 60 participants were randomized into two study groups of 30 each (Figure 1). All patients verbally consented to participate in the study. Patients were informed that they were participating in a study that was being conducted to improve methods of informed consent for surgery. The concept of informed consent was also explained since many patients were unaware of their rights to presurgical information. Patients were not told they were being randomized into different groups. The informed consent procedure followed a standardized protocol that emulated an ideal clinical experience as closely as possible. Patients were informed that they would be quizzed multiple times at the start, but they were not told the number of times or time-points at which they would be quizzed. Permission was obtained before each quizzing session.
Figure 1.
Organization of study subjects. Participants were divided into two groups for verbal consent, with and without a visual aid.
A pilot quiz was administered to a small group of patients (n = 5) one week before the study began. This quiz involved using an oral, 11-question, multiple choice quiz (4–5 choices/question) that covered concepts regarding the risks, benefits, and side effects of cataract surgery. We adopted the concept of a multiple choice quiz from Moseley et al,9 but it proved unfeasible in this population since patients could not readily understand the format or keep track of answer choices. We opted for a simpler, true/false/don’t know, format, which was also piloted with a small group of patients (n = 8) and proved to be more easily understandable.
Prior to being provided any preoperative information, patients in both groups were given an oral, 11-question, true/false quiz, which covered the causes and effects of cataracts, the basic surgical methods, as well as the risks and benefits of surgery (Appendix 1). The quiz was developed by the authors according to essential aspects of cataract surgery informed consent as practiced in US clinics. The wording of the verbal consent and the quiz questions was simplified since most patients had only three years of formal education and less than half in either group were literate. Because the majority of patients were illiterate, a translator read the questions from a translated script in an unbiased voice. All other documents, such as the demographic questions and informed consent for the study, were also translated from English to Tamil. To avoid guessing, patients were given the option of answering, “I don’t know.”
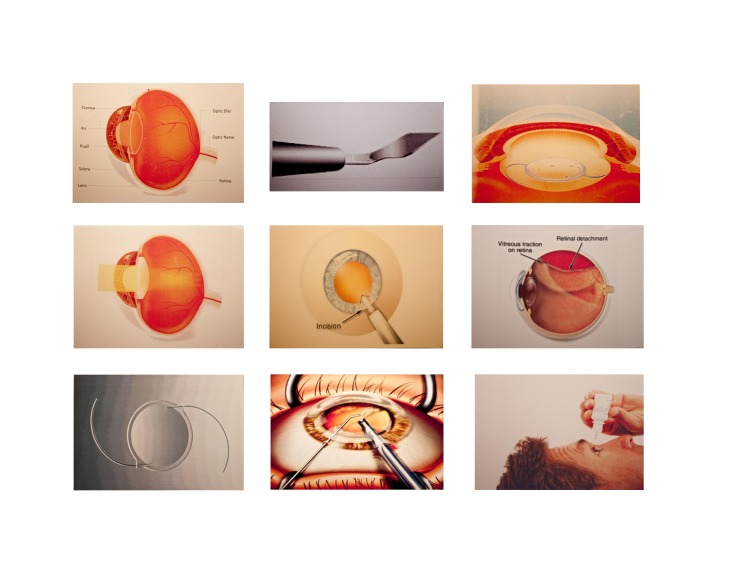
Patients in group A (n = 30) listened to a scripted informed consent (Appendix 2) read by a native Tamil speaker. Patients in group B (n = 30) listened to the same scripted informed consent but were also presented a 24″ × 36″ poster displaying nine images (Figure 2). Images included the following: a diagram of the normal eye, a parallel diagram of an eye with a cataract, an image of an intraocular lens, a close-up image of the surgical blade, a picture of the actual surgical incision, an image of the lens disassembly by phacoemulsification, an image of the intraocular lens (IOL) placed within the eye, a picture indicating a possible complication (in this case a retinal detachment), and lastly an image indicating the use of postoperative eyedrops.
Figure 2.
Visual aid for informed consent.
The pictures were large and clear and were held approximately one meter away from the patients. Patients in the intervention group were shown the poster during verbal informed consent, and the presenter paused as appropriate to refer to the pictures. The presentation was standardized across intervention group patients. Immediately after provision of this information, the quiz was readministered to each group. Patients were administered the same quiz for a third time on postoperative day one. To minimize information bias being introduced through extraordinary attention to the informed consent material presented, participants were not informed that there was a post-test or that they would be retested on postoperative day 1. Patients were asked permission before being administered the postoperative quiz. Relatives and friends who accompanied patients were asked not to aid the patient in answering questions.
The average numbers of questions marked correct, incorrect, and “I don’t know” were calculated for both groups at each of the three time points. The scores were compared within and between group A and group B to determine statistically significant differences. Only patients who completed all three quizzes (group A, 23 patients; group B, 17 patients) were included in the statistical analysis.
In order to detect a difference of one question correct between groups A and B, a sample size of 34 (17 in each group) would be required to obtain a power of 80%, assuming a standard deviation of one for each group. A power of 90% would require a sample size of 44, and 95% would require a sample size of 54. A total sample size of 60 was selected and expected to provide sufficient power while accounting for attrition during the study.
Comparisons of total scores between individuals in group A and group B were made using unpaired, two-sample t tests in the R programming language. Comparisons of differences in scores between different time points (eg, change in scores from before the informed consent to after the operation) were similarly made using paired two-sample t tests. The effects of covariates were analyzed using multiple linear regression models.
Results
Each group consisted of patients from 23 different villages. No significant differences existed between groups in terms of formal education, literacy, number of patients with previous cataract surgery, or number of patients with acquaintances with previous cataract surgery (Table 1). All 60 patients completed the pre– and post–informed consent quizzes.
Table 1.
Patient Baseline Characteristics
| Characteristic | Group A | Group B | P value |
|---|---|---|---|
| Verbal Consent Alone (n = 30) | Verbal Consent and Poster (n = 30) | ||
| Age (years) ± SD | 60.96 ± 10.88 | 65.23 ± 8.88 | 0.1017 |
| Women | 22 | 19 | 0.4051a |
| Men | 8 | 11 | |
| Formal education in years (mean ± SD) | 3.1 ± 3.9 | 2.8 ± 3.6 | 0.7578 |
| Literate patients | 12 | 10 | 0.5921 |
| Previous cataract surgery | 10 | 12 | 0.5921 |
| Accompanied by friend/family | 16 | 12 | 0.3006 |
| Friend or family with previous surgery | 10 | 5 | 0.136 |
P value for sex as a whole; the numbers for men and women cannot be tested separately since the total number of individuals is fixed.
There was no statistically significant difference in the pre–informed consent scores or the post–informed consent scores between the two groups. However, group B’s improvement in the mean score was greater than group A’s after the informed consent, and this difference in improvement persisted one day postoperatively ( Figure 3). Group B’s mean improvement from pre–informed consent to postoperative day 1 was significantly higher than group A’s (1.3 vs 3.6, P = 0.002). In addition, group B’s mean score on postoperative day 1 was significantly higher than group A’s (7.4 vs 8.7, P = 0.005), despite group A’s higher mean scores at the beginning of the study (Tables 2 and 3). A χ2 test for trend in proportions on the number of correct responses for each group at each time point indicated a value of 3.8882 with a P value of 0.04863.
Figure 3.
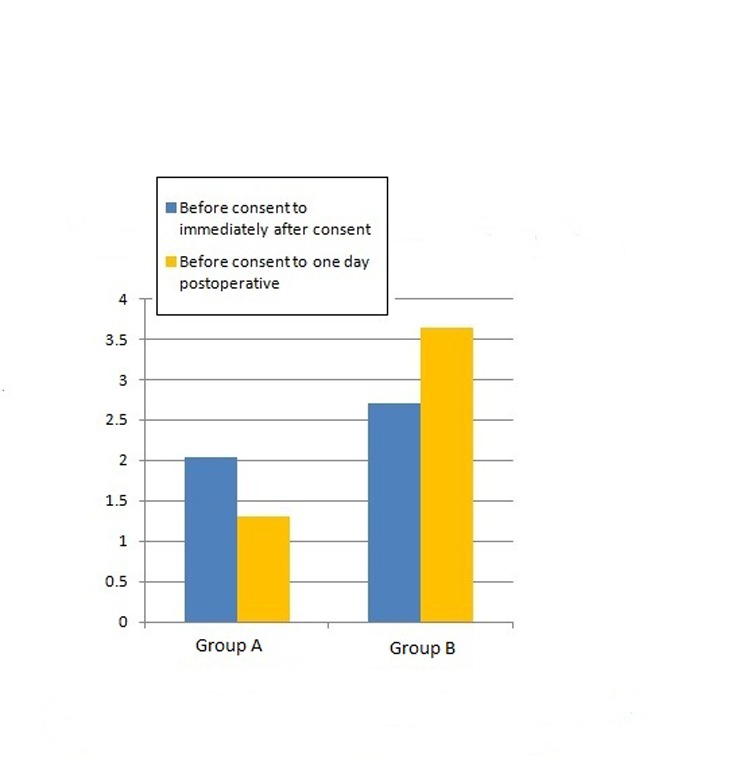
Change in scores between testing sessions. Quiz score improvement was significantly higher in group B (verbal consent plus a poster) than in group A (verbal consent alone).
Table 2.
Average Number of Correct Responses (of 11)*
| Group | Pre–Informed Consent Mean (SD) |
Post–Informed Consent Mean (SD) |
Postoperative Day 1 Mean (SD) |
|---|---|---|---|
| A (n = 23) | 6.0870 (2.026) | 8.1304 (1.359) | 7.391 (1.305) |
| B (n = 17) | 5.0588 (1.298) | 8.1765 (2.038) | 8.706 (1.404) |
| P value for difference between groups | 0.0581 | 0.9362 | 0.0049 |
Calculations made using unpaired, two-sample t tests
Table 3.
Change in Number of Correct Responses*
| Group | Pre–Informed Consent to Post–Informed Consent Mean (SD) |
Pre–Informed Consent to Postoperative Mean (SD) |
|---|---|---|
| A | 2.043 (2.233) | 1.304 (2.636) |
| B | 3.118 (2.142) | 3.647 (1.801) |
| P value for difference between groups | 0.1353 | 0.001909 |
Calculations made using paired two-sample t tests
To assess the possible influence of covariates on these results, a series of linear regression models was fit to the data, with differences in scores between time points as the dependent variables. Independent variables in the full model were group membership (group A or group B), age, gender, highest educational level, literacy, previous surgery, prior knowledge of the surgery (collected as a binary), and visual acuity (taken as the better visual acuity of the patient’s two eyes). The R2 value for the model predicting improvement from pre–informed consent to post–informed consent was 0.4873. When comparing pre–informed consent to post–informed consent improvement and post–informed consent to postoperative improvement, neither group A nor B stratification was statistically significant in the presence of the other covariates. However, when improvement from pre–informed consent to postoperative day 1 was used as the dependent variable, patients in group B scored an additional 4.0523 points higher on the quiz, as measured by its coefficient in the linear model, with an associated P value of 0.00819.
Discussion
In a study by Scanlan et al10 regarding attitudes toward informed consent, 90% of cataract patients who participated stated informed consent was an important process, and 89% reported that there is a need to have all information explained to them. In some developing countries, the value patients place on informed consent is often not paralleled by physicians, and medical paternalism is especially prevalent among those working with illiterate populations.13–15 A review article by Bastia attempted to clarify common misconceptions among Indian physicians regarding what constitutes appropriate informed consent.16
In our study, a detailed, comprehensive, and patient-appropriate informed consent with or without a visual aid resulted in significantly higher scores from pre–informed consent to post–informed consent. Though there was no immediate difference when patients were exposed to a visual aid, there was a statistically significant improvement on postoperative day 1 in information retention in the group that was exposed to a visual aid.
Limitations to this study included the potential for statistical artifacts due to low patient numbers. We were unable to control for patient attrition on postoperative day 1 due to variable times at which patients would leave after surgery. Some patients did not remain at the hospital after surgery and could not be contacted for follow-up. The use of a translator resulted in some unintended variance in the consent process; for example, some patients tried to ask questions during the consent process while others did not. Many patients had extremely poor vision in each eye, limiting the efficacy of a visual aid in these surgical candidates, although this was not identified as a significant factor during the multivariate analysis.
In conclusion, a careful and comprehensive process of obtaining informed consent improves patients’ understanding of the risks, benefits, alternatives, and side effects of surgery, as seen in previous informed consent studies. In this rural, largely illiterate population, the addition of a visual aid during the informed consent process improved information retention on postoperative day 1.
Appendix 1 Cataract Surgery Questionnaire
State whether the following is True or False. If you are not sure, say I Don’t Know
A cataract is the clouding of the lens.
Lack of certain vitamins, exposure to sunlight, and old age can all cause cataracts.
Wearing strong glasses can remove a cataract.
If you do not remove a mature cataract, you will suffer irreversible blindness.
During cataract surgery, the surgeon makes an incision in the eye with a special blade.
The way the surgeon removes the cataract is by breaking apart and removing the lens and placing a new, artificial lens in the eye.
Everyone will have improved vision after cataract surgery.
There are no risks involved with cataract surgery.
Benefits of cataract surgery include never needing glasses again.
The normal postoperative course is typically that vision will be perfect the next day.
Postoperative drops are used to prevent infection and inflammation.
Appendix 2 Informed Consent Procedure
Control Group
Patients were presented with a standardized verbal informed consent read aloud by a translator:
“A cataract forms in the part of the eye called the lens. When we are young the lens is clear and as we age the lens gets cloudier. The cataract can also grow and become more cloudy for other reasons such as if the eye is injured, if too much sunlight enters the eye, if one does not eat a healthy diet or if one smokes cigarettes. The cataract can become so large and cloudy that it blocks light from getting back to the retina, the part of the eye that senses the light, and vision will be blurry. Most cataracts are not dangerous, your doctors only consider removing the cataracts when they are causing vision to be decreased and the patient is unable to do his or her normal daily activities like walking, eating, reading, and seeing people’s faces. Glasses and drops cannot improve the cloudiness of a mature cataract, only surgery can correct the cloudiness from a cataract.
“Cataract surgery is a real surgery. The surgeon makes a small incision on the eye and uses a special instrument to break apart the cataract and vacuum the cataract out of the eye. The surgeon will then place a new plastic artificial lens inside the eye. Now light can get back to the retina for good vision.
“Problems that can happen during or because of cataract surgery include: scarring or clouding of the clear cornea, high pressure inside the eye called glaucoma, a change in the shape or color of the iris, the whole lens or a piece of the lens may fall to the back of the eye and require a second surgery to remove it, you could develop a retinal tear or detachment, or there could be bleeding or infection in the eye. Most of these problems are rare, but any of these complications could result in a loss of vision or loss of the eye (though most people experience an improvement in vision). Occasionally a person may have a film that forms over the artificial lens months to years after cataract surgery. This film may be called a secondary cataract. If that film forms it can often be removed with a laser.
“During the surgery you will be awake. The surgeon will use medication to numb the eye, so you should not have any pain. The surgery usually takes about 20 minutes. You will need to use eyedrops after surgery to prevent infection and control inflammation inside the eye.
“After surgery, it is normal for your vision to be blurry. You should notice your vision improves a little every day. Your vision will usually be improved by one month. Most people require glasses for near vision, distance vision, or both. It is important that you follow up with your eye doctor after surgery to make sure the eye is healthy and there are no problems developing.”
Intervention Group
Patients were presented with a standardized verbal informed consent (presented above) read aloud by a translator as well as the poster (Figure 2).
Footnotes
The authors have no proprietary or commercial interest in any materials discussed in this article.
The authors acknowledge the Unite for Sight NGO for support in completing this study and providing access to patients, hospital contacts, and physicians. Financial support was provided by the Yale College Sunrise Foundation Research and Travel Grant, the John E. Linck Fellowship, and the Research to Prevent Blindness organization.
References
- 1.Satyanarayana K, Srivastava S. Poverty, health & intellectual property rights with special reference to India. Indian J Med Res. 2007;126:390–406. [PubMed] [Google Scholar]
- 2.O’Donnell O. Access to health care in developing countries: breaking down demand side barriers. Cad Saude Publica. 2007;23:2820–34. doi: 10.1590/s0102-311x2007001200003. [DOI] [PubMed] [Google Scholar]
- 3.Finger RP. Cataracts in India: current situation, access, and barriers to services over time. Ophthalmic Epidemiol. 2007;14:112–8. doi: 10.1080/09286580601114967. [DOI] [PubMed] [Google Scholar]
- 4.Strasser R. Rural health around the world: challenges and solutions. Fam Pract. 2003;20:457–63. doi: 10.1093/fampra/cmg422. [DOI] [PubMed] [Google Scholar]
- 5.Chang MA, Congdon NG, Baker SK, Bloem MW, Savage H, Sommer A. The surgical management of cataract: barriers, best practices and outcomes. Int Ophthalmol. 2008;28:247–60. doi: 10.1007/s10792-007-9121-2. [DOI] [PubMed] [Google Scholar]
- 6.Mahendradhata Y, Ahmad RA, Lefèvre P, Boelaert M, Van der Stuyft P. Barriers for introducing HIV testing among tuberculosis patients in Jogjakarta, Indonesia: a qualitative study. BMC Public Health. 2008;8:385. doi: 10.1186/1471-2458-8-385. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Manafa O, Lindegger G, Ijsselmuiden C. Informed consent in an antiretroviral trial in Nigeria. Indian J Med Ethics. 2007;4:26–30. doi: 10.20529/IJME.2007.009. [DOI] [PubMed] [Google Scholar]
- 8.Bernat JL, Peterson LM. Patient-centered informed consent in surgical practice. Arch Surg. 2006;141:86–92. doi: 10.1001/archsurg.141.1.86. [DOI] [PubMed] [Google Scholar]
- 9.Moseley TH, Wiggins MN, O’Sullivan P. Effects of presentation method on the understanding of informed consent. Br J Ophthalmol. 2006;90:990–3. doi: 10.1136/bjo.2006.092650. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Scanlan D, Siddiqui F, Perry G, Hutnik CM. Informed consent for cataract surgery: what patients do and do not understand. J Cataract Refract Surg. 2003;29:1904–12. doi: 10.1016/s0886-3350(03)00234-7. [DOI] [PubMed] [Google Scholar]
- 11.Panton RL, Downie R, Truong T, Mackeen L, Kabene S, Yi QL, et al. A visual approach to providing prognostic information to parents of children with retinoblastoma. Psychooncology. 2009;18:300–4. doi: 10.1002/pon.1397. [DOI] [PubMed] [Google Scholar]
- 12.Bollschweiler E, Apitzsch J, Obliers R, Koerfer A, Mönig SP, Metzger R. Improving informed consent of surgical patients using a multimedia-based program: results of a prospective randomized multicenter study of patients before cholecystectomy. Ann Surg. 2008;248:205–11. doi: 10.1097/SLA.0b013e318180a3a7. [DOI] [PubMed] [Google Scholar]
- 13.Humayun A, Fatima N, Naqqash S, Hussain S, Rasheed A, Imtiaz H, et al. Patients’ perception and actual practice of informed consent, privacy and confidentiality in general medical outpatient departments of two tertiary care hospitals of Lahore. BMC Med Ethics. 2008;9:14. doi: 10.1186/1472-6939-9-14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Yousuf RM, Fauzi AR, How SH, Rasool AG, Rehana K. Awareness, knowledge and attitude toward informed consent among doctors in two different cultures in Asia: a cross-sectional comparative study in Malaysia and Kashmir, India. Singapore Med J. 2007;48:559–65. [PubMed] [Google Scholar]
- 15.Luna F. Paternalism and the Argument from Illiteracy. Bioethics. 1995;9:283–90. doi: 10.1111/j.1467-8519.1995.tb00363.x. [DOI] [PubMed] [Google Scholar]
- 16.Bastia BK. Consent to treatment: practice vis-à-vis principle. Indian J Med Ethics. 2008;5:113–4. doi: 10.20529/IJME.2008.041. [DOI] [PubMed] [Google Scholar]