Abstract
Dengue fever has been a major problem in hospital settings in Brazil for the past 15 years. The main concern has been the severe forms, i.e., dengue hemorrhagic fever and dengue shock syndrome. Hemorrhagic events of different degrees have also been a major concern. We report five cases of large vein thrombotic events associated with the acute phase of dengue fever, including a previously non-reported case of mesenteric vein thrombosis. Complications such as these could have been overlooked in the diagnosis of dengue fever, given that the major concern is the hemorrhagic event.
Dengue fever frequently affects Brazil, where thousands of cases have been diagnosed annually and all four dengue virus serotypes (DENV-1 through DENV-4) have been reported, sometimes concurrently in the same region.1,2 Hemorrhagic events of different degrees have often been described in dengue, but thrombotic events have not been extensively reported, despite the wide range of increased procoagulant activity during illness.1,3–8 During a recent outbreak, several cases of thrombotic events affected large veins in dengue fever patients. We report cases of unusual and overlooked complication of dengue fever.
From January 2011 through March 2011 during a local outbreak of dengue fever caused by DENV-1 and DENV-2 according to local health officials, five patients were given diagnoses by imaging techniques (pulmonary computed tomography angiography, cholangio-magnetic resonance imaging, and Doppler ultrasound of lower extremities) as having large vessel thrombosis. These patients were part of 92 serologically confirmed (by immunochromatographic strip test or IgM antigen-capture enzyme-linked immunosorbent assay) patients with dengue (60% women and 40% men, median age = 39 years, age range = 10–99 years) admitted to Monte Sinai Hospital (200 beds) in Juiz de Fora, (population = 500,000), Minas Gerais, Brazil. This study was approved by the Ethical Committee of Monte Sinai Hospital.
Twenty-three patients (25%) were classified as having dengue shock syndrome or dengue hemorrhagic fever and 4 deaths were recorded (case-fatality rate = 4.3%). These thrombotic patients represented 5.4% of all dengue inpatients. All thrombotic events were identified within the first five days of illness, and all patients had symptoms compatible with the reported thrombotic event at hospital admission. No thrombotic events were identified among the remaining patients during hospitalization, and none of the patients them received drugs for thrombosis prophylaxis, which is contraindicated in dengue.
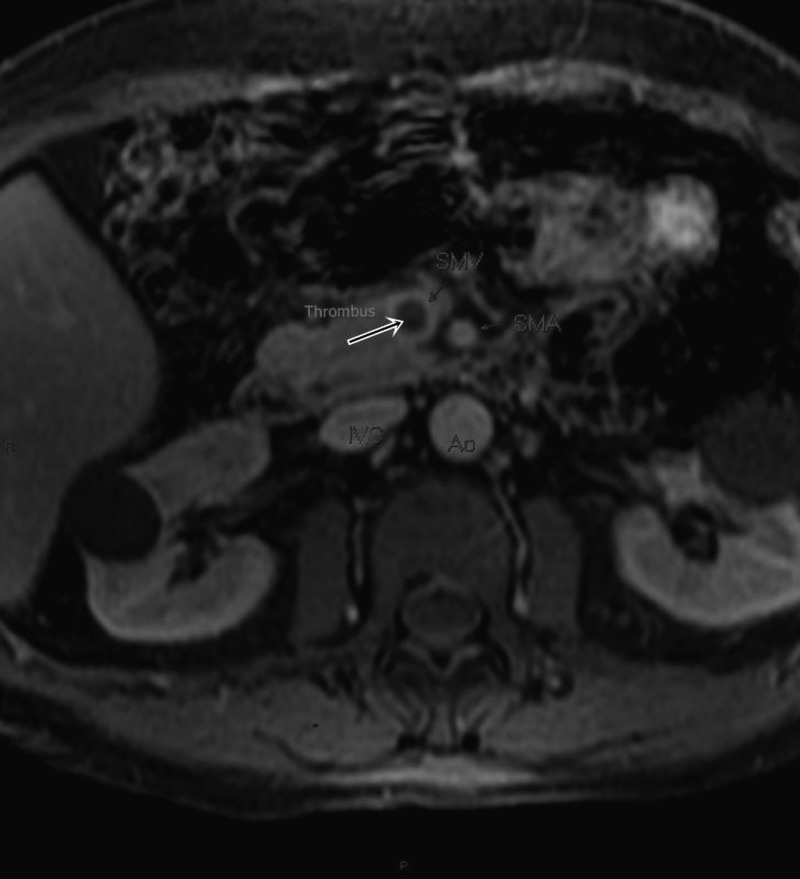
The demographic and clinical characteristics of the five patients are summarized in Table 1. Patients 1 and 2 had ileo-femoral deep vein thrombosis, patients 3 and 4 had pulmonary thromboembolism, and patient 5 was given a diagnosis of mesenteric vein thrombosis by cholangio-magnetic resonance imaging (Figure 1), which was associated with jaundice and severe sepsis by Escherichia coli demonstrated by blood culture. Known risk factors for thrombotic events such as smoking, use of oral contraceptives, and being overweight were absent in all patients and none had had any similar diagnosis or symptoms.
Table 1.
Demographic, clinical, and laboratory characteristics of five dengue fever patients with thrombotic events, Brazil*
| Patient/age (years)/sex | Platelets (× 109/L)† | Hematocrit, %‡ | Antibodies against phospholipid§ | Imaging | Manifestations | Thrombotic event | Illness day of thrombosis diagnosis |
|---|---|---|---|---|---|---|---|
| 1/89/F | 113 | 33 | IgG 4.5, IgM 17.6 | Doppler US | Leg pain and edema | DVT | 2 |
| 2/41/F | 112 | 32.9 | IgG 7.9, IgM 1.9 | Doppler US | Leg pain and edema | DVT | 3 |
| 3/89/F | 52 | 45 | IgG 32.8, IgM 14.2 | CTA | Dyspnea | PTE | 1 |
| 4/51/F | 45 | 41 | IgG 0.6, IgM 12.0 | CTA | Dyspnea | PTE | 2 |
| 5/61/M | 37 | 42 | IgG 6.1, IgM 11.3 | C-MRI | SIRS | MVT | 5 |
US = ultrasound; DVT = deep vein thrombosis; CTA = computed tomography angiography; PTE = pulmonary thromboembolism; C-MRI = cholangio-magnetic resonance imaging; SIRS = systemic inflammatory response syndrome; MVT = mesenteric vein thrombosis.
Reference value = 140–400 × 109 /L (sample obtained on hospital day 1).
Reference values: males = 41–53%; females = 36–46% (sample obtained on hospital day 1).
Reference value < 10 IgMPL/IgGPL (IgM phospholipid units, 1 IgMPL unit = 1 μg of IgM); IgGPL (IgG phospholipid units, 1 GPL unit = 1 μg of IgG).
Figure 1.
T1-weighted cholangio-magnetic resonance image with contrast of dengue patient 5 showing the superior mesenteric vein (SMV) with a large thrombus (arrow) occupying the vein lumen. SMA = superior mesenteric artery; IVC = inferior vena cava; Ao = aorta.
Increased levels of IgM against phospholipids were detected in four patients, but levels of IgG against phospholipids above the reference level were detected in only one patient (by enzyme immunoassay), and this was the only positive result in thrombophilia screening. Although most of the patients were dehydrated, severe hemoconcentration was not observed. Leukocyte counts were within the reference range and levels of D-dimer were increased in all patients. The international normalized ratio (prothrombin time) was normal or slightly prolonged in all patients and none had hemorrhagic events. None of the thrombotic patients were classified as having dengue shock syndrome or dengue hemorrhagic fever. All patients were treated with low molecular weight heparin and recovered. Although not completely understood, low platelet counts and function, increased vascular permeability, increased thrombomodulin, increased tissue plasminogen activator, and antibody cross-reactivity with endothelial cells and with specific coagulation proteins are among the suggested mechanisms responsible for hemorrhagic phenomena in dengue fever.3–8
Myriad factors, including cytokines, fibrinolysis, and the complement system, might increase thrombotic risk in dengue fever patients.3–5 Increased PAI-1 plasma levels seem to be common in DENV infection and have been associated with greater risk for thrombosis.7 Disseminated intravascular coagulation and consequent microthombi formation have also been reported in dengue fever but have not been associated with large vessel thrombosis.5 Low concentrations of plasma anticoagulant proteins C and S and antithrombin III have also been detected in severe dengue but have not been associated with clinical thrombosis.4
Increased levels of IgM against phospholipids were detected in all but one patient in this series, but these levels are of low clinical significance for thrombosis. Thus, except for increased levels of IgG against phospholipids in one patient, no other procoagulant risk factor was identified in this case series.9 Antibodies against phospholipids and increased lupus anticoagulant have been anecdotally associated with thrombotic events in peripheral arteries and cerebral vasculature in dengue fever patients.10,11 Venous cerebral vasculature thrombosis and ischemic stroke not associated with antibodies against phospholipids or other risk factors have been rarely reported in dengue fever patients.12
Severe dehydration, a well known condition associated with thrombotic events, was not detected in any patient. All but one of the patients was > 50 years of age. Thus, the role of older age in thrombotic events in dengue fever should be considered. It is noteworthy that none of the thrombosis cases occurred in patients with dengue shock syndrome or dengue hemorrhagic fever, but the small number of patients with these conditions is not a reasonable explanation.
The involved mechanism seems to be related to events that occurred during the early phase of the disease because the thrombotic events were clinically detected at admission and no episode of thrombosis was detected among the remaining dengue fever patients throughout hospitalization or during outpatient follow-up. Loss of endothelium non-thrombogenic protective factors has been identified in severe dengue early in the course of the disease.1
To our knowledge, deep vein thrombosis, pulmonary thromboembolism, and mesenteric vein thrombosis have not been reported in direct association with dengue fever.1,11,12 Mesenteric vein thrombosis was an unusual complication of DENV infection, and was erroneously diagnosed in an imaging study of suspected cholangitis in a patient with clinical sepsis without a primary source. Awareness for these kinds of complications should be recommended to all practitioners who treat patients with dengue fever, particularly in hospital settings.
Footnotes
Authors' addresses: Paulo Sérgio Gonçalves da Costa, Geyza Machado Ribeiro, Cleber Soares Junior, and Lenilton da Costa Campos, Hospital Monte Sinai, Juiz de Fora, Minas Gerais, Brazil, E-mails: psgcosta@acessa.com, geyza@laboratoriomontesinai.com.br, cleberdoc@ig.com.br, and leniltoncampos@yahoo.com.br.
References
- 1.Cavalcanti LP, Coelho IC, Vilar DC, Holanda SG, Escóssia KN, Souza-Santos R. Clinical and epidemiological characterization of dengue hemorrhagic fever cases in northeastern, Brazil. Rev Soc Bras Med Trop. 2010;43:355–358. doi: 10.1590/s0037-86822010000400003. [DOI] [PubMed] [Google Scholar]
- 2.Vilela AP, Figueiredo LB, dos Santos JR, Eiras AE, Bonjardin CA, Ferreira PC, Kroon EG. Dengue virus 3 genotype I in Aedes aegypti mosquitoes and eggs, Brazil 2005–2006. Emerg Infect Dis. 2010;16:989–992. doi: 10.3201/eid1606.091000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Mairuhu AT, Mac Gillavry MR, Setiati TE, Soemantri A, ten Cate H, Brandjes DP, van Gorp EC. Is clinical outcome of dengue-virus infections influenced by coagulation and fibrinolysis? A critical review of the evidence. Lancet Infect Dis. 2003;3:33–41. doi: 10.1016/s1473-3099(03)00487-0. [DOI] [PubMed] [Google Scholar]
- 4.Wills BA, Oragui EE, Stephens AC, Daramola OA, Dung NM, Loan HT, Chau NV, Chambers M, Stepniewska K, Farrar JJ, Levin M. Coagulation abnormalities in dengue hemorrhagic fever: serial investigations in 167 Vietnamese children with dengue shock syndrome. CID. 2002;35:277–285. doi: 10.1086/341410. [DOI] [PubMed] [Google Scholar]
- 5.Martina BE, Koraka P, Osterhaus AD. Dengue virus pathogenesis: an integrated view. Clin Microbiol Rev. 2009;22:564–581. doi: 10.1128/CMR.00035-09. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Krishnamurti C, Peat RA, Cutting MA, Rothwell SW. Platelet adhesion to dengue-2 virus-infected endothelial cells. Am J Trop Med Hyg. 2002;66:435–441. doi: 10.4269/ajtmh.2002.66.435. [DOI] [PubMed] [Google Scholar]
- 7.Mairuhu AT, Setiati TE, Koraka P, Hack CE, Leyte A, Faradz SM, ten Cate H, Brandjes DP, Osterhaus AD, Reitsma PH, van Gorp EC. Increased PAI-1 plasma levels and risk of death from dengue: no association with the 4G/5G promoter polymorphism. Thromb J. 2005;3:17. doi: 10.1186/1477-9560-3-17. doi:10.1186/1477-9560-3-17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Basu A, Chaturvedi UC. Vascular endothelium: the battlefield of dengue viruses. FEMS Immunol Med Microbiol. 2008;53:287–299. doi: 10.1111/j.1574-695X.2008.00420.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Miesbach W, Scharrer I, Asherson RA. High titres of IgM-antiphospholipid antibodies are unrelated to pathogenicity in patients with non-Hodgkin's lymphoma. Clin Rheumatol. 2007;26:95–97. doi: 10.1007/s10067-006-0328-9. [DOI] [PubMed] [Google Scholar]
- 10.Chen WH. An unusual transitory increase of lupus anticoagulant in dengue virus infection complicated with cerebral ischaemia. J Infect. 2006;52:e87–e91. doi: 10.1016/j.jinf.2005.06.003. [DOI] [PubMed] [Google Scholar]
- 11.Karunatilaka DH, De Silva JR, Ranatunga PK, Gunasekara TM, Faizal MA, Malavige GN. Idiopathic purpura fulminans in dengue hemorrhagic fever. Indian J Med Sci. 2007;61:471–473. [PubMed] [Google Scholar]
- 12.Gulati S, Maheshwari A. Atypical manifestations of dengue. Trop Med Int Health. 2007;12:1087–1095. doi: 10.1111/j.1365-3156.2007.01891.x. [DOI] [PubMed] [Google Scholar]