Lung transplantation has become an accepted treatment for many individuals with severe lung disease.1 It yields improvements in quality and/or quantity of life, depending on the underlying disease process leading to the transplant as well as many other pre- and posttransplant factors. Yet, transplant candidates and recipients experience a range of psychosocial issues that begin at the initiation of the transplant evaluation and continue throughout patients' wait for donor lungs, their perioperative recovery, and their long-term adjustment to posttransplant life. Psychosocial factors may comprise, be caused by, and result in changes to functional capacity, social roles and relationships, health maintenance behaviors, psychological status, perceptions of self, and life plans and goals. Quality of life has a strong association with these domains and their changes throughout the transplantation experience.
This article reviews the psychosocial factors implicated during the various phases of the lung transplantation experience. It will consider patients' perceptions of changes to quality of life and their reported well-being as they progress through each phase, with a focus on the following psychosocial domains: physical functioning, behavioral, psychological, and social. This article also highlights studies of interventions that aim to improve quality of care or reduce patient distress throughout the transplantation process. In addition, the authors address disease-specific differences in outcome, controversial issues in lung transplantation candidate selection, and palliative care for lung candidates and recipients. Lastly, they discuss some psychosocial effects of transplantation on patients' primary family caregivers, as caregivers play a major role in maintaining their loved ones' physical and mental health and also undergo significant exposure to the stressors of the transplantation experience.
Evaluation for Lung Transplantation
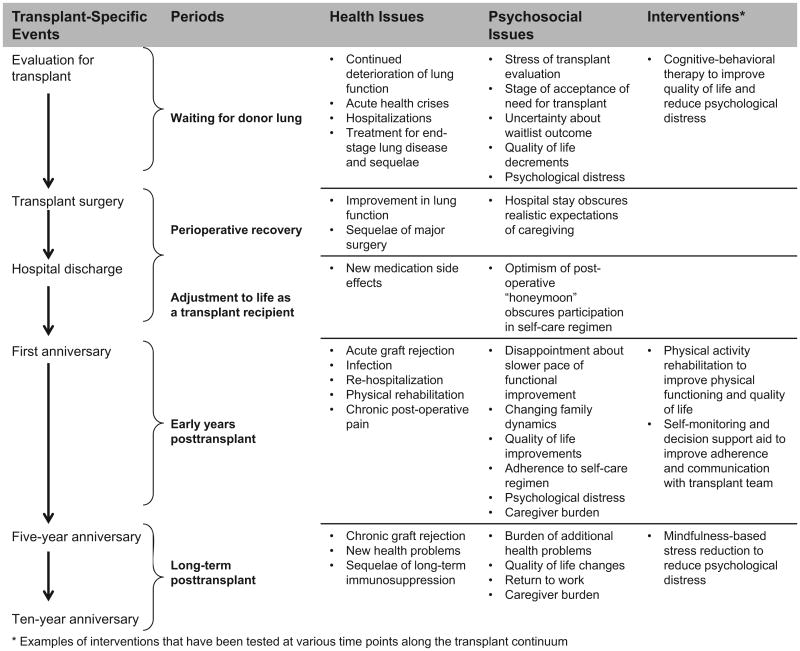
Similar to other types of solid organ transplantation, the lung transplantation process begins in earnest as patients and their families begin to consider the idea of transplantation. Patients undergo a transplant evaluation that encompasses both medical and psychosocial realms. Fig. 1 depicts examples of events and stressors that contribute to different phases of the transplantation experience, as well as some of the interventions that have demonstrated efficacy in reducing the impact of these stressors. Specific stressors associated with the evaluation include uncertainty about whether or not a transplant program will judge the potential transplant candidate as suitable for listing, fear of surgery, worry about changes to future life plans, financial strain, and conflicting feelings about treatment options.2,3 Even participating in the transplant evaluation may cause distress and tension for some patients. Patients may be uncomfortable with the questions asked during the psychosocial portion of the evaluation because they are less familiar than those asked during the more routine medical portion of the evaluation. Patients may also be conflicted about whether revealing personal information that exposes their vulnerabilities may jeopardize their ability to present themselves favorably to maximize their chances of receiving a lung transplant.3 Moreover, consideration of mental health in the transplant evaluation may engender stress due not only to the nature of the questions but also because the mental health professionals conducting the evaluation are focused on judging suitability for transplant rather than providing treatment.4
Fig. 1.
Lung transplant timeline: examples of events and stressors that contribute to different phases of the transplantation experience as well as interventions that have demonstrated efficacy in reducing the impact of these stressors.
Ultimately, transplant candidates are confronted with the reality, and underlying stressor, that they risk opening themselves to the possibility of an arduous treatment that may never finally materalize. For some patients who have already accepted their progressive disease state, the hope of transplant and subsequent letdown may cause more distress than the management of the physical and psychological aspects of the disease itself. Patients' stage of acceptance of their need for a transplant, which often depends on the acuity of their disease, affects the level of distress patients experience while considering whether or not to undergo transplantation.5 Patients with chronic, longstanding disease (eg, chronic obstructive pulmonary disease [COPD]) are more likely to have prepared themselves for the idea of a potentially long waiting period and the life changes that will ensue after the transplant than those patients with a more rapidly progressing illness and a shorter waiting time for transplant.
Patients with cystic fibrosis (CF)-associated lung disease are in a unique position with respect to accepting the idea of transplantation. Although disease counseling throughout their lifetime may have encouraged them to base life decisions on a projected rate of decline, transplantation represents a major change to their life timeline and simultaneously subjects them to stressors faced by all candidates about risks associated with the transplantation procedure.6 High levels of anxiety and decisional conflict about being listed for transplantation commonly affect patients with CF. A recent study demonstrated the potential value of a decision aid for these patients. The investigators found that a paper- and internet-based tool that directly addressed CF-specific issues, offered in addition to standard pretransplant educational sessions, made patients' expectations of potential surgical and posttransplant complications more realistic and reduced their feelings of decisional conflict about being listed for transplant.7 Similar decision aids might positively affect potential transplant candidates who may expect to experience quality but not quantity of life improvements from transplantation, including patients with COPD.
The Waiting Period for Lung Transplantation
Once listed as a candidate, patients and their families enter what may be the most stressful period of the entire transplantation experience. Candidates and their families must balance the reality that they may not survive to the point of transplantation with the desire to make plans for life after transplantation. Lung candidates have described feeling that they have no choice but to accept that they and their family members must simply put their lives on hold until after the transplant surgery.8 Transplant candidates in general experience persistent anxiety about when, if ever, the call will come that a donor organ has become available. In addition, they typically experience monotony and frustration about the physical functional limitations associated with advanced disease, especially if they require oxygen support, as do many lung candidates. Patients who live in geographically remote areas may need to relocate to undergo transplantation, which further disrupts a candidate's family and adds to the sense of feeling hostage to the waiting list. Throughout the waiting period, some candidates feel supported by interacting with transplant recipients who can provide hope and fellow candidates who can identify with their current stressors5; however, jealousy may arise if one candidate receives a transplant before another.9
The stressors associated with waiting for transplant have a cumulative effect on patients' generally poor quality of life. Lung candidates appear to have a lower quality of life than candidates for other types of transplantation,10,11 likely because of their illness burden and physical impairments. They tend to have lower emotional well-being and higher risk for psychiatric disorders compared with the general population.12–14 Anxiety and panic disorders are common in patients with lung disease, perhaps because of the shared mechanisms underlying dyspnea, hyperventilation, and symptoms and triggers of anxiety.14 Prevalence rates of mood and anxiety disorders in lung candidates are high, reportedly ranging from 20% to 47%.3,15 Comorbidity is also common: one study showed that more than 25% of candidates who met criteria for any psychiatric disorder actually met criteria for 2 disorders.14 Lung candidates (as well as heart candidates) have also been found to report elevated depressive symptom levels compared with liver candidates.16 Moreover, psychological distress has been reported to increase the frequency of physical symptoms among lung transplant candidates,14 which may contribute to candidates' low overall quality of life.
Interventions aimed at improving psychosocial outcomes among lung transplant candidates have produced favorable results.17–19 Studies have generally structured their interventions as 8 to 12 weekly, telephone-based sessions that used cognitive behavioral strategies to improve coping skills, quality of life, mood symptoms, and relationships with caregivers. Compared to candidates who participated in control conditions, which varied between usual care and health education sessions depending on the study, candidates who received an intervention reported higher quality of life, fewer depressive and anxiety symptoms, lower perceived stress, and higher optimism and perceived social support.
Palliative Care Pretransplant
Although receiving no empirical evaluation to date, interventions that address symptom management, end-of-life care, and palliative care also have potential importance in this population. Patients, families, and their physicians may face difficult and complex decisions regarding the implementation of such strategies while they focus on the hope of eventual transplantation. However, the pace with which some individuals decompensate may drive the need to address end-of-life considerations and palliative care as part of their medical treatment. Among candidates with CF, studies have demonstrated that palliative care takes a secondary role to aggressive medical management that aims to sustain patients until transplantation20,21; as a result, CF candidates are often likely to die in the intensive care unit without ever having discussed end-of-life wishes.20 A case report of a candidate with COPD depicted the patient's and family's difficult decision to forego the curative-restorative care necessary to keep the patient listed for transplantation in favor of palliative care that strived to optimize her quality of life while dying.22 Although, in her case (as well as in many other anecdotal reports from practice), the decision to switch from curative-restorative to palliative care prompted a distinct change in treatment regimen and medical team composition, these 2 types of care do not necessarily need to be implemented separately and sequentially. According to the Clinical Practice Guidelines for Palliative Care (which states the goal of palliative care as being “to prevent and relieve suffering and to support the best possible quality of life for patients and their families, regardless of the stage of the disease or the need for other therapies”), palliative and restorative care are not at odds.23 By incorporating both types of care but changing the focus as patients move along their illness trajectory, clinicians may be able to address symptom management and palliative care while concurrently preparing lung candidates for transplantation.
Perioperative Recovery and Adjustment to Life as a Transplant Recipient
Most patients undergoing lung transplantation experience a rapid change in health soon after transplant. Often, they transit quickly from life with minimal lung function and maximal anxiety before the transplant to a posttransplant honeymoon period characterized by feelings of high optimism and anticipation of steadily improving lung function.24 Many patients and their families face hospital discharge buoyed by the success of transplant surgery and encouraged by early postoperative improvement in lung function.2 In addition, many families may have welcomed the respite from caring for their lung recipient during the postoperative hospital stay and have thus begun to think about posttransplant life, sometimes prematurely, without the burdens of caregiving. Consequently, they may begin to set unrealistic expectations about the recovery process and long-term posttransplant life.
This posttransplant optimism may present a barrier to patients' and their families' participation in self-management after the transplant. Patient education efforts may stall, as patients may not see the need to carry out self-care activities important for preventing posttransplant complications.2 A qualitative study of lung recipients described this initial phase as “naiveté”; after experiencing a positive postoperative experience and then beginning to see the normalization of pulmonary function tests and oxygen levels, many recipients felt immune to transplant-related complications.24 Although health care providers instructed recipients about the high incidence of acute graft rejection during the early postoperative phase, these lung recipients tended to attribute symptoms to non-transplant-related causes and opted to call their primary care provider instead of their transplant team about emergent symptoms. Only after recipients had developed rejection did they and their families become more vigilant of symptoms of potential rejection. However, although this adjustment reduced patients' initial sense of denial about their posttransplant medical vulnerabilities, it also prompted feelings of guilt for thinking they were uniquely exempt from complications that affect nearly all lung recipients.
The Early Years after Transplant
As recipients progress farther from their transplant surgery, they become increasingly reliant on themselves and their families to manage day-to-day posttransplant care, mainly because of longer periods between follow-up clinic appointments. Despite this positive achievement, recipients may feel anxious on realizing that their contact with the transplant team is diminishing. Family dynamics often remain in flux during the early months after transplant. As patients' steep rate of recovery during the early postoperative period begins to plateau, the slower pace of functional improvement may be disheartening even though patients generally have higher levels of posttransplant functional ability and quality of life compared to their pretransplant levels. It often takes several years after transplant for patients and their families to fully adjust to the new range of stressors associated with life posttransplant and to accept that, with the transplant, they have traded one chronic disease for another. Studies have observed posttransplant adjustment in multiple areas of psychosocial outcomes, which are discussed in the following sections.
Global Quality of Life
The most significant improvements in quality of life from pre- to posttransplant tend to occur during the early posttransplant phase and remain stable for several years thereafter.25–27 Although lung recipients' quality-of-life levels are typically lower than the general (nondiseased) population,25,28 they show dramatic improvements in health-related quality of life1,26,29,30 and feelings of well-being and life satisfaction28,31 when compared with their pretransplant ratings of these outcomes. Nevertheless, their rate of improvement in quality of life tends to be slower than that of heart recipients, for example, most likely because their physical recovery from surgery is more prolonged.31 In addition, improvements in quality of life tend to plateau between 6 and 7 months after transplant,27,31 with smaller gains observed thereafter.
Physical Functioning
Improvements in physical functioning show a slower trajectory of change than do recipients' perceptions of improvements in global quality of life. Whereas global quality of life has been shown to reach its plateau around 6 months posttransplant, physical functioning has been shown to improve throughout the first 2 years after transplant before leveling off.32 Similar to global quality-of-life ratings, physical functional status posttransplant does not reach that of the general population.33
Interventions that aim to improve physical functioning represent an important part of comprehensive posttransplant rehabilitation, particularly because transplantation has not been shown to bring about the same gains in exercise capacity that it does in lung function.34 Many transplant centers thus enroll or refer lung recipients to some form of exercise or pulmonary rehabilitation program. A review of 7 studies of aerobic and resistance exercise training programs for lung recipients showed that exercise training brought about improvements in maximal and functional exercise capacity, skeletal muscle function, and bone mineral density, all of which are impaired in lung recipients.35 Moreover, exercise training improved health-related quality of life over the course of each program. Studies published since the aforementioned review demonstrated improvements in lung function, functional exercise capacity,36 physical fitness indicators, blood pressure,33 and exercise tolerance37 among recipients who participated in exercise training. In studies that included a comparison group, greater improvements were seen in the intervention group relative to controls. Given the overall positive outcomes of empirically tested exercise training programs with varied structures, transplant centers have some flexibility around program location (eg, inpatient vs home-based) and program structure (eg, frequency, duration, and content of sessions).
Another important element of physical functional status, chronic postoperative pain, affects 18% to 49% of lung recipients during the first several years posttransplant.38,39 One study identified the pre-transplant diagnosis of emphysema as the strongest correlate of pain in lung recipients at least 3 months after transplant. Correlates of pain at this time point included older age, having had a single lung transplant, higher levels of depression symptoms, and lower health-related quality of life in areas other than pain.38 Another study of lung recipients who had survived, on average, 3.5 years posttransplant showed that more than half of patients with chronic pain believed that it had a major impact on their quality of life and, depending on the intensity of the activity, reported pain to be a limiting factor in their daily social activities.39
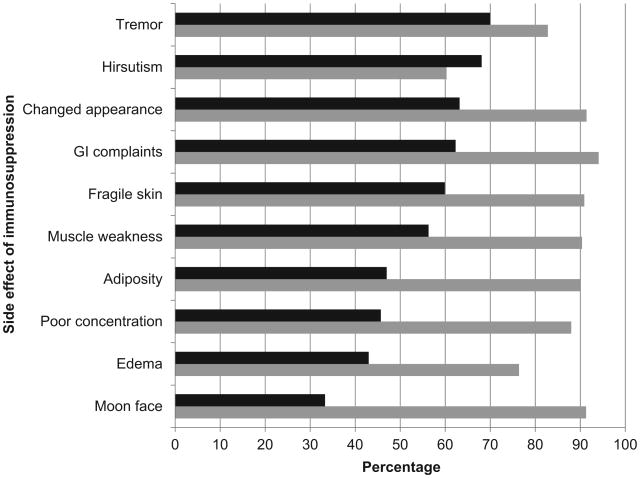
Side effects of maintenance immunosuppression also factor into patients' overall physical functional status. These side effects range from transient to permanent, and they vary with respect to the distress they produce. Because lung recipients receive higher doses of immunosuppression medications than any other solid organ recipients, they tend to experience the most side effects.40 A study of 287 lung recipients showed that the most common side effects were tremor, hirsutism, changed appearance, gastrointestinal complaints, and fragile skin, whereas the most common moderately-to-severely distressing side effects were gastrointestinal complaints, changed appearance, moon face, fragile skin, and muscle weakness (Fig. 2). A review of psychiatric considerations when treating transplant recipients in a critical care context noted that the most common neurotoxic side effects of immunosuppressants include tremors, headache, restlessness, insomnia, vivid dreams, photophobia, hyperesthesia, anxiety, and agitation, all of which affected 40%to 60% of those on immunosuppressive medication.9 In addition to causing discomfort and pain, studies have demonstrated that these symptoms affect patients' adherence to their medication regimen.41,42
Fig. 2.
Side effects of immunosuppression. Dark-shaded bars represent the prevalence of each symptom; light-shaded bars represent the percentage of those experiencing each symptom who found it moderately-to-severely distressing. (Data from Kugler C, Geyer S, Gottlieb J, et al. Symptom experience after lung transplantation: impact on quality of life and adherence. Clin Transplant 2007;21:590–6.)
Posttransplant Adherence to the Medical Regimen
Lung recipients must follow a complex self-management regimen as part of their posttransplant care. Adherence to this regimen is particularly important for lung recipients because, relative to recipients of other solid organs, lung recipients have higher rates of infection and acute and chronic rejection.43,44 The regimen includes taking immunosuppressants; monitoring spirometry, vital signs, weight, and symptoms; communicating effectively with the transplant care team; attending clinic appointments; getting regular blood work, pulmonary function testing, chest X-rays, and bronchoscopies; and following diet and exercise guidelines. One study found wide variability in lung recipients' adherence across these components of their regimen. Out of 178 recipients observed for the first 2 years after transplant, only 13% of recipients were nonadherent to immunosuppressants (based on a combination of self- and family caregiver-report).43 In contrast, 26% were nonadherent to clinical appointments, 62% were nonadherent to required spirometry, and 70% failed to monitor their blood pressure as required. In general, adherence declined over time.
University of Pittsburgh investigators recently developed an intervention that uses a handheld device called Pocket Personal Assistant for Tracking Health (Pocket PATH) to assist lung recipients with monitoring data related to their self-care behaviors and reporting potentially concerning values to the transplant team.45 After 2 months of participation in a randomized controlled trial of Pocket PATH versus standard paper-and-pencil monitoring methods, recipients in the Pocket PATH group reported higher self-care agency, adherence to self-care behaviors, and quality of life than the other group. These findings support the need for further study of interventions to improve adherence to self-care behaviors, especially as recipients progress farther beyond the point of transplant. The University of Pittsburgh group is currently conducting a randomized trial to evaluate these long-term issues.
Aside from interventions that focus directly on adherence-related behaviors themselves, identification of risk factors for nonadherence after lung transplantation may allow for more targeted education of patients and their families. Risk factors identified to date include pretransplant nonadherence to medications, less social support, and lower conscientiousness46; more side effects from immunosuppressants41; and younger age.47 Patients who considered themselves to have little influence over their health reported a higher rate of nonadherence to self-monitoring activities.43 Similarly, patients with weaker beliefs in medications' ability to prevent rejection and stronger concerns about adverse effects of medication reported a higher rate of non-adherence to medication taking.48 Although not yet used in lung transplant recipients, interventions that address patient knowledge about the role of self-management have improved adherence in non-transplant chronic disease populations.49,50
Psychiatric Status
Lung transplant recipients have reported prevalence rates of up to 30% for depression or anxiety disorders during the first year posttransplant, and these disorders are highly comorbid.13,51 One study showed that despite similar rates of depression, posttraumatic stress disorder related to the transplant, and generalized anxiety disorder in lung and heart recipients, lung recipients had a significantly higher rate of panic disorder than heart recipients, with prevalence reaching 18% for lung recipients (relative to 8% in heart recipients).13 Major risk factors for depression and/or anxiety included having a history of these disorders, female gender, spending a longer time on the waiting list, having early posttransplant complications, and having poor caregiver support. Awareness of these predictors may allow clinicians to recognize patients at high risk for posttransplant psychiatric distress.
Despite the high rates of diagnosable psychiatric disorders, it is noteworthy that most patients do not experience such disorders.12,13,25,28,51–53 Moreover, subclinical depression and anxiety symptoms tend to decline from pre- to posttransplant,52 as recipients experience dramatic improvements in physical functioning and optimism about their recovery. Nevertheless, a significant minority may not show this improving pattern. In a study of lung, heart, liver, and kidney recipients, 40% showed declining levels of emotional well-being from pretransplant across the first 2 years posttransplant.25 These individuals reported poorer pretransplant emotional well-being and a higher burden adhering to the posttransplant immunosuppressant regimen when compared with patients who had a more favorable pre- to posttransplant mental health profile. They may thus warrant additional support from the transplant team to avert a continued pattern of decline posttransplant.
The lung transplant literature lacks data regarding the impact of posttransplant psychiatric status on medical outcomes. A prospective study of 177 lung recipients found that depression and anxiety disorders did not predict mortality at up to 10 years posttransplant.53 However, these disorders were associated with posttransplant morbidities, although in diverging directions. The study found that depression was associated with increased risk for bronchiolitis obliterans syndrome (BOS; the clinical correlate of chronic rejection), and lymphocytic bronchiolitis (the small airway disease that often precedes acute rejection), whereas anxiety was associated with decreased risk for graft loss and BOS. Adherence and frequency of screening (eg, pulmonary function tests and biopsies) did not mediate the relationship for either depression or anxiety.
The Long-Term Years after Transplant
After reaching plateaus in physical functioning and psychological adjustment to the transplant around the end of the first year posttransplant, lung transplant recipients tend to have more stability in medical and psychosocial outcomes during the subsequent years.2,27 Recipients and their families shift their focus from preventing and caring for acute transplant-related complications to reestablishing normalcy in everyday life. Yet, the risk of medical complications does not disappear. Long-term survivors of lung transplantation develop chronic rejection and sequelae of prolonged immunosuppression (eg, diabetes,2 renal failure,54 osteoporosis,55 malignancy,56,57 neurologic complications, and opportunistic infections58). Some of these post-transplant complications, specifically, infections, rejections, and BOS, have been associated with reduced health-related quality of life59 and an increased risk for anxiety and negative emotional well-being during the later posttransplant years.60
Indeed, the threat of BOS remains a predominant concern for recipients and their families, with impacts on many psychosocial domains. International transplant registry data suggest that BOS occurs in 49% of recipients by 5 years posttransplant and in 75% by 10 years.61 Because BOS is largely unresponsive to treatment, mortality from BOS remains high among recipients who survive at least one year. One study reported frequent hospitalizations, emergency department visits, and intensive care unit admissions following the onset of chronic rejection.62 The intense medical treatment required to manage BOS may explain the negative impact BOS has on multiple domains of psychosocial outcomes, including physical functional and emotional well-being.27,63,64 Further, a qualitative study of family caregivers of lung recipients with chronic rejection showed that caregivers considered the incidence of BOS “inevitable” and were distraught by what they perceived as recipients' regression to their pretransplant state.65
Additional correlates of quality-of-life outcomes among long-term lung transplant survivors sometimes differ per outcome domain and time since transplant. Some studies showed a negative association between length of time since transplant and low quality of life in physical functioning domains in cohorts assessed at both 3 and 10 years posttransplant.66,67 These recipients had lower quality-of-life scores than those of population norms and nontransplant chronic disease patients at 10 years. Conversely, another study found a positive association between length of time since transplant and mental health domains of quality of life, with quality-of-life scores equivalent to those of nontransplant populations at 10 years posttransplant.67
Predictors of low physical quality of life appear to differ according to time since transplant. In one study of recipients at 3 years posttransplant, some clinical events such as hospitalization predicted low physical quality of life.66 Another study of recipients at 5 years posttransplant identified marital status and return to work as the strongest predictors.27 At 10 years posttransplant, the strongest predictors of low physical quality of life were BOS, pretransplant physical quality of life, age, and gender.63
Predictors of psychosocial domains of quality of life differ from predictors of physical quality of life. Regarding psychological quality of life, BOS and pretransplant depression predicted posttransplant depression, whereas BOS and age predicted post-transplant anxiety, in a cohort of recipients at 10 years posttransplant.63 In the social domain of quality of life, return to work has been considered one of the main indicators of success of transplantation, although only 28% to 39% of recipients have been found to be employed posttransplant.27 Studies have shown that predictors of posttransplant employment include younger age, greater mobility, having had a previous occupation, having been off work for less than 2 years pretransplant, and having identified return to work as a main motivator for transplant.68–70
These findings underscore the need for psychosocial interventions that support recipients throughout the later-term posttransplant years. The only intervention study to date randomized solid organ recipients (including lung) to an 8-week long, weekly mindfulness-based stress reduction program, a peer-led health education program, or a standard care control.71 One year after the end of the intervention, recipients who had received the intervention reported less anxiety and better sleep quality than recipients who had received the health education control and less depression and better sleep quality than recipients who had received the standard care control. Moreover, those who had received the intervention also reported increasing quality of life over the 8 weeks of the intervention. The study did not show differential effects of the intervention based on time since transplant.
Controversial Populations in Lung Transplantation Candidate Selection
Transplant programs strive to carefully select transplant candidates to optimize outcomes for patients and for the program. Such selectivity often leads to the exclusion of controversial patient populations. In many of these populations, psychosocial issues and outcomes may factor largely into the benefit they receive from transplantation, as is the case with older adults, or may complicate the decision to transplant them, as is the case with psychotic patients.
Older adults have demonstrated positive psychosocial outcomes after transplantation. A review of solid organ transplantation in older adults reported that older recipients have equivalent, and sometimes better, adherence, mental health outcomes, and quality of life relative to younger recipients.72 Similarly, a study that compared lung recipients of various age groups showed that older recipients did not experience more posttransplant complications or worse hospital-related outcomes than younger recipients.73 Moreover, the few studies that have considered the impact of age on posttransplant psychosocial outcomes have not found any predictive relationship.72 Relative to the general population, however, older recipients reported higher rates of psychiatric disorders and lower rates of employment. Despite these favorable data regarding lung transplant outcomes in older adults, studies cannot fully adjust for the other factors that may lead transplant programs to screen out older candidates.
Transplant programs have traditionally considered patients with psychotic disorders to be questionable candidates for transplantation because of fears that the stress of transplantation or side effects from steroids will destabilize their psychotic disorder and subsequently cause nonadherence to the posttransplant regimen.60 Across all organs, a survey of transplant programs' experiences with patients with psychotic disorders reported incidence rates of rejection and nonadherence to immunosuppressants that were consistent with rates seen in nonpsychotic organ recipients.74 Specific to lung transplantation, one case report of a lung recipient with schizophrenia described favorable respiratory and psychiatric outcomes after lung transplantation, as well as consistent attendance at monthly visits to the psychiatric clinic.75
Palliative Care Posttransplant
The decision to initiate palliative care after transplant is complex because patients, families, and their clinicians may consider palliative care to conflict with the life-sustaining goals of transplantation. However, palliative care is not, by definition, end-of-life care; rather, it aims to optimize quality of life throughout patients' illness trajectory. In a study of palliative care referrals after lung transplantation, the misconception that palliative care is end-of-life care was endorsed by most transplant and palliative care clinicians as a barrier to initiating palliative care.76 An additional barrier noted by transplant clinicians was uncertainty about patients' prognosis, which often prevented the initiation of palliative care until patients were ill enough to require stopping life-sustaining treatment. Moreover, the prospect of retransplantation makes the decision to stop aggressive treatment measures even more difficult for many patients and their families.65 It may be ideal for palliative care and restorative care to proceed in parallel, with the focus of care shifting as patients' illness trajectory and treatment options change over time.
Impact on Caregivers of Transplant Recipients
Family caregivers provide crucial supports for maintaining patients' physical and mental health throughout the transplantation process. During phases of the process in which patients may experience severe illness and disability, caregivers carry out practical activities that patients often take for granted in daily life. Exposure to the chronic stresses of transplantation may cause caregivers of both lung candidates and recipients to experience a lower quality of life than noncaregiving adults.77 Moreover, up to 30% of caregivers for lung candidates reported clinically significant levels of depression and anxiety, both of which were associated with a higher perceived burden of caregiving.78,79 Caregivers may feel confined and inconvenienced by having to be available to help their loved one at any time, and they may also feel disappointment that the illness has substantially changed their loved one.77 One qualitative study determined that 30% of caregivers' daily activities during the first 6 months after transplant were related to supporting their loved one's health.80 Although performing these activities can often be gratifying, adjusting to the changing family dynamics, household responsibilities, and job-related capacities associated with transplant may compound the discrete burdens of caregiving, as evidenced by caregivers reportedly spending less of their day in a positive mood than did the lung recipients for which they care.80 At the same time, however, caregivers also reported positive outcomes of caregiving, such as discovering inner strength and support from others and realizing the important things in life.77
Interventions to improve caregivers' quality of life may have benefits for both patients' and caregivers' health. Evidence from nontransplant populations show that psychological interventions for caregivers of patients with a chronic illness may improve caregivers' mental health and coping skills.81 The only such study in lung transplantation that evaluated the effect of a psychological intervention on caregivers' quality of life showed that caregivers of lung candidates who received the psychological therapy reported better quality of life, fewer mood disturbances, and higher social intimacy than caregivers of patients who did not receive the therapy.82
Summary and Treatment Implications
The process of lung transplantation brings with it a range of successes and stressors from the time a patient contemplates undergoing evaluation to the years beyond the transplant. Although transplantation may improve quality of life, physical functioning, and psychiatric status, not all patients experience the same degree of improvements; moreover, benefits do not always occur as quickly as many patients anticipate. Patients often expect that the transplant will restore their health and quality of life to a level comparable to levels before they ever became ill. Instead, adjustment to life after transplant often requires coming to terms with ongoing medical illness burden and continued reliance on caregivers. After experiencing improvements in pre- to posttransplant psychosocial status (eg, global quality of life, physical functioning, and mental health), patients' levels of psychosocial outcomes typically plateau and do not return to levels equivalent to the general population. Nevertheless, because patients may still experience dramatic pre- to posttransplant improvements in psychosocial status, clinicians should work with lung recipients and their families, particularly their caregivers, to find ways to sustainor increase those gains, such as by optimizing adherence, symptom management, and complication prevention.
Transplant programs could consider incorporating elements from the evidence-based interventions reviewed here into care of both candidates and recipients. Because most recipients and their families cite the waiting period as the most distressing part of the transplantation experience, pretransplant psychosocial interventions could include those that aim to ease the stresses related to the uncertainty of being on the waiting list while simultaneously managing a deteriorating condition. Immediately after transplant, although recipients and their families optimistically enjoy the successes of the surgery and patients' marked gains in physical functioning, interventions could focus on education about the risks of posttransplant complications and the importance of self-monitoring in order to involve patients in the prevention of infections and complications. During the years beyond the transplant, interventions could aim to improve quality of life (in both recipients and their caregivers), physical functioning, and adherence to the medical regimen. Although it is sometimes challenging to reconcile the treatment goals of patients, families, and the transplant team, evidence suggest that deliberate and preemptive integration of palliative care and restorative care maximizes quality of life over the course of the pre- to posttransplant illness trajectory; transplant programs could thus strive to offer palliative and restorative care in parallel.
To meet the broad needs of lung recipients and their families, clinicians must remain aware of the many psychosocial issues lung recipients face throughout the transplantation process. At the same time, clinicians should address the many psychosocial benefits recipients may experience, as a means of acknowledging progress and facilitating greater grains. An understanding of these psychosocial issues over the course of the transplantation timeline and an inclusion of approaches to improve various posttransplant issues based on evidence-based interventions may aid transplant programs in improving the care of their lung recipients.
Key Points.
Lung transplant candidates and recipients experience a range of psychosocial stressors throughout the transplant evaluation, waiting period, perioperative recovery, early years, and late-term years after transplantation.
The lung transplantation process and its associated stressors affect a range of patient psychosocial outcomes, including global quality of life, physical functioning, psychiatric status, and adherence to the medical regimen.
Lung recipients experience pre-to posttransplant gains in many psychosocial domains, although most gains plateau during the first posttransplant year at levels lower than those of the general population.
Lung transplant candidates' and recipients' family caregivers are also exposed to stressors associated with the transplantation process, and their global quality of life and physical and emotional well-being may be affected as well.
Transplant programs should incorporate evidence-based interventions to improve psychosocial outcomes and a combination of palliative and restorative care strategies that shift with patients' changing medical needs.
Acknowledgments
Funding support: Funded, in part, through the following grants from the National Institutes of Health: TL1 TR000145, R01 NR010711 and R01 HL083067.
Footnotes
Financial disclosures and/or conflicts of interest: The authors have nothing to disclose.
References
- 1.Yusen RD. Survival and quality of life of patients undergoing lung transplant. Clin Chest Med. 2011;32:253–64. doi: 10.1016/j.ccm.2011.02.006. [DOI] [PubMed] [Google Scholar]
- 2.Dew MA, DiMartini AF, Kormos RL. Stress of organ transplantation. In: Fink G, editor. Encyclopedia of stress. 2nd. Oxford, UK: Academic Press (Elsevier); 2007. pp. 35–44. [Google Scholar]
- 3.Barbour KA, Blumenthal JA, Palmer SM. Psychosocial issues in the assessment and management of patients undergoing lung transplantation. Chest. 2006;129:1367–74. doi: 10.1378/chest.129.5.1367. [DOI] [PubMed] [Google Scholar]
- 4.Olbrisch ME, Benedict SM, Ashe K, et al. Psychological assessment and care of organ transplant patients. J Consult Clin Psychol. 2002;70:771–83. doi: 10.1037//0022-006x.70.3.771. [DOI] [PubMed] [Google Scholar]
- 5.Ivarsson B, Ekmehag B, Sjoberg T. Recently accepted for the waiting list for heart or lung transplantation - patients' experiences of information and support. Clin Transplant. 2011;25:E664–71. doi: 10.1111/j.1399-0012.2011.01511.x. [DOI] [PubMed] [Google Scholar]
- 6.Adler FR, Aurora P, Barker DH, et al. Lung transplantation for cystic fibrosis. Proc Am Thorac Soc. 2009;6:619–33. doi: 10.1513/pats.2009008-088TL. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Vandemheen KL, O'Connor A, Bell SC, et al. Randomized trial of a decision aid for patients with cystic fibrosis considering lung transplantation. Am J Respir Crit Care Med. 2009;180:761–8. doi: 10.1164/rccm.200903-0421OC. [DOI] [PubMed] [Google Scholar]
- 8.Naef R, Bournes DA. The lived experience of waiting: a Parse method study. Nurs Sci Q. 2009;22:141–53. doi: 10.1177/0894318409331932. [DOI] [PubMed] [Google Scholar]
- 9.DiMartini AF, Crone C, Fireman M, et al. Psychiatric aspects of organ transplantation in critical care. Crit Care Clin. 2008;24:949–81. doi: 10.1016/j.ccc.2008.05.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Ortega T, Deulofeu R, Salamero P, et al. Health-related quality of life before and after a solid organ transplantation (kidney, liver, and lung) of four Catalonia hospitals. Transplant Proc. 2009;41:2265–7. doi: 10.1016/j.transproceed.2009.06.175. [DOI] [PubMed] [Google Scholar]
- 11.Myaskovsky L, Dew MA, Switzer GE, et al. Quality of life and coping strategies among lung transplant candidates and their family caregivers. Soc Sci Med. 2005;60:2321–32. doi: 10.1016/j.socscimed.2004.10.001. [DOI] [PubMed] [Google Scholar]
- 12.Dew MA, DiMartini AF. Psychological disorders and distress after adult cardiothoracic transplantation. J Cardiovasc Nurs. 2005;20:S51–66. doi: 10.1097/00005082-200509001-00007. [DOI] [PubMed] [Google Scholar]
- 13.Dew MA, DiMartini AF, DeVito Dabbs AJ, et al. Onset and risk factors for anxiety and depression during the first two years after lung transplantation. Gen Hosp Psychiatry. 2012;34:127–38. doi: 10.1016/j.genhosppsych.2011.11.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Parekh PI, Blumenthal JA, Babyak MA, et al. Psychiatric disorder and quality of life in patients awaiting lung transplantation. Chest. 2003;124(5):1682–8. doi: 10.1378/chest.124.5.1682. [DOI] [PubMed] [Google Scholar]
- 15.Erim Y, Beckmann M, Marggraf G, et al. Psychosomatic evaluation of patients awaiting lung transplantation. Transplant Proc. 2009;41:2595–8. doi: 10.1016/j.transproceed.2009.06.125. [DOI] [PubMed] [Google Scholar]
- 16.Dobbels F, Vanhaecke J, Nevens F, et al. Liver versus cardiothoracic transplant candidates and their pretransplant psychosocial and behavioral risk profiles: good neighbors or complete strangers? Transpl Int. 2007;20:1020–30. doi: 10.1111/j.1432-2277.2007.00527.x. [DOI] [PubMed] [Google Scholar]
- 17.Blumenthal JA, Babyak MA, Keefe FJ, et al. Telephone-based coping skills training for patients awaiting lung transplantation. J Consult Clin Psychol. 2006;74:535–44. doi: 10.1037/0022-006X.74.3.535. [DOI] [PubMed] [Google Scholar]
- 18.Rodrigue JR, Baz MA, Widows MR, et al. A randomized evaluation of quality-of-life therapy with patients awaiting lung transplantation. Am J Transplant. 2005;5:2425–32. doi: 10.1111/j.1600-6143.2005.01038.x. [DOI] [PubMed] [Google Scholar]
- 19.Napolitano MA, Babyak MA, Palmer S, et al. Effects of a telephone-based psychosocial intervention for patients awaiting lung transplantation. Chest. 2002;122:1176–84. doi: 10.1378/chest.122.4.1176. [DOI] [PubMed] [Google Scholar]
- 20.Sands D, Repetto T, Dupont LJ, et al. End of life care for patients with cystic fibrosis. J Cyst Fibros. 2011;10:S37–44. doi: 10.1016/S1569-1993(11)60007-6. [DOI] [PubMed] [Google Scholar]
- 21.Robinson WM. Palliative and end-of-life care in cystic fibrosis: what we know and what we need to know. Curr Opin Pulm Med. 2009;15:621–5. doi: 10.1097/MCP.0b013e3283304c29. [DOI] [PubMed] [Google Scholar]
- 22.Janssen DJ, Spruit MA, Does JD, et al. End-of-life care in a COPD patient awaiting lung transplantation: a case report. BMC Palliat Care. 2010;9:6. doi: 10.1186/1472-684X-9-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.National Consensus Project for Quality Palliative Care. Clinical Practice Guidelines for Palliative Care. 2009 Available at http://www.nationalconsensusproject.org/guideline.pdf.
- 24.DeVito Dabbs A, Hoffman LA, Swigart V, et al. Striving for normalcy: symptoms and the threat of rejection after lung transplantation. Soc Sci Med. 2004;59:1473–84. doi: 10.1016/j.socscimed.2004.01.013. [DOI] [PubMed] [Google Scholar]
- 25.Goetzmann L, Ruegg L, Stamm M, et al. Psychosocial profiles after transplantation: a 24-month follow-up of heart, lung, liver, kidney and allogeneic bone-marrow patients. Transplantation. 2008;86:662–8. doi: 10.1097/TP.0b013e3181817dd7. [DOI] [PubMed] [Google Scholar]
- 26.Goetzmann L, Sarac N, Ambuhl P, et al. Psychological response and quality of life after transplantation: a comparison between heart, lung, liver and kidney recipients. Swiss Med Wkly. 2008;138:477–83. doi: 10.4414/smw.2008.12160. [DOI] [PubMed] [Google Scholar]
- 27.Kugler C, Tegtbur U, Gottlieb J, et al. Health-related quality of life in long-term survivors after heart and lung transplantation: a prospective cohort study. Transplantation. 2010;90:451–7. doi: 10.1097/TP.0b013e3181e72863. [DOI] [PubMed] [Google Scholar]
- 28.Goetzmann L, Klaghofer R, Wagner-Huber R, et al. Quality of life and psychosocial situation before and after a lung, liver or an allogeneic bone marrow transplant. Swiss Med Wkly. 2006;136:281–90. doi: 10.4414/smw.2006.11362. [DOI] [PubMed] [Google Scholar]
- 29.Yusen RD. Technology and outcomes assessment in lung transplantation. Proc Am Thorac Soc. 2009;6:128–36. doi: 10.1513/pats.200809-102GO. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Eskander A, Waddell TK, Faughnan ME, et al. BODE index and quality of life in advanced chronic obstructive pulmonary disease before and after lung transplantation. J Heart Lung Transplant. 2011;30:1334–41. doi: 10.1016/j.healun.2011.06.006. [DOI] [PubMed] [Google Scholar]
- 31.Myaskovsky L, Dew MA, McNulty ML, et al. Trajectories of change in quality of life in 12-month survivors of lung or heart transplant. Am J Transplant. 2006;6:1939–47. doi: 10.1111/j.1600-6143.2006.01395.x. [DOI] [PubMed] [Google Scholar]
- 32.Bossenbroek L, ten Hacken NH, van der Bij W, et al. Cross-sectional assessment of daily physical activity in chronic obstructive pulmonary disease lung transplant patients. J Heart Lung Transplant. 2009;28:149–55. doi: 10.1016/j.healun.2008.11.905. [DOI] [PubMed] [Google Scholar]
- 33.Langer D, Gosselink R, Pitta F, et al. Physical activity in daily life 1 year after lung transplantation. J Heart Lung Transplant. 2009;28:572–8. doi: 10.1016/j.healun.2009.03.007. [DOI] [PubMed] [Google Scholar]
- 34.Bartels MN, Armstrong HF, Gerardo RE, et al. Evaluation of pulmonary function and exercise performance by cardiopulmonary exercise testing before and after lung transplantation. Chest. 2011;140(6):1604–11. doi: 10.1378/chest.10-2721. [DOI] [PubMed] [Google Scholar]
- 35.Wickerson L, Mathur S, Brooks D. Exercise training after lung transplantation: a systematic review. J Heart Lung Transplant. 2010;29:497–503. doi: 10.1016/j.healun.2009.12.008. [DOI] [PubMed] [Google Scholar]
- 36.Munro PE, Holland AE, Bailey M, et al. Pulmonary rehabilitation following lung transplantation. Transplant Proc. 2009;41:292–5. doi: 10.1016/j.transproceed.2008.10.043. [DOI] [PubMed] [Google Scholar]
- 37.Vivodtzev I, Pison C, Guerrero K, et al. Benefits of home-based endurance training in lung transplant recipients. Respir Physiol Neurobiol. 2011;177:189–98. doi: 10.1016/j.resp.2011.02.005. [DOI] [PubMed] [Google Scholar]
- 38.Girard F, Chouinard P, Boudreault D, et al. Prevalence and impact of pain on the quality of life of lung transplant recipients: a prospective observational study. Chest. 2006;130:1535–40. doi: 10.1378/chest.130.5.1535. [DOI] [PubMed] [Google Scholar]
- 39.Wildgaard K, Iversen M, Kehlet H. Chronic pain after lung transplantation: a nationwide study. Clin J Pain. 2010;26:217–22. doi: 10.1097/AJP.0b013e3181b705e4. [DOI] [PubMed] [Google Scholar]
- 40.Floreth T, Bhorade SM. Current trends in immunosuppression for lung transplantation. Semin Respir Crit Care Med. 2010;31:172–8. doi: 10.1055/s-0030-1249112. [DOI] [PubMed] [Google Scholar]
- 41.Kugler C, Geyer S, Gottlieb J, et al. Symptom experience after lung transplantation: impact on quality of life and adherence. Clin Transplant. 2007;21:590–6. doi: 10.1111/j.1399-0012.2007.00693.x. [DOI] [PubMed] [Google Scholar]
- 42.Dobbels F, Vanhaecke J, Desmyttre A, et al. Prevalence and correlates of self-reported pretransplant nonadherence with medication in heart, liver, and lung transplant candidates. Transplantation. 2005;79:1588–95. doi: 10.1097/01.tp.0000158430.06507.87. [DOI] [PubMed] [Google Scholar]
- 43.Dew MA, DiMartini AF, DeVito Dabbs A, et al. Adherence to the medical regimen during the first two years after lung transplantation. Transplantation. 2008;85:193–202. doi: 10.1097/TP.0b013e318160135f. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.De Geest S, Dobbels F, Fluri C, et al. Adherence to the therapeutic regimen in heart, lung, and heart-lung transplant recipients. J Cardiovasc Nurs. 2005;20:S88–98. doi: 10.1097/00005082-200509001-00010. [DOI] [PubMed] [Google Scholar]
- 45.DeVito Dabbs A, Dew MA, Myers B, et al. Evaluation of a hand-held, computer-based intervention to promote early self-care behaviors after lung transplant. Clin Transplant. 2009;23:537–45. doi: 10.1111/j.1399-0012.2009.00992.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Dobbels F, Vanhaecke J, Dupont L, et al. Pretransplant predictors of posttransplant adherence and clinical outcome: an evidence base for pretransplant psychosocial screening. Transplantation. 2009;87:1497–504. doi: 10.1097/TP.0b013e3181a440ae. [DOI] [PubMed] [Google Scholar]
- 47.Bosma OH, Vermuelen KM, Verschurren EA, et al. Adherence to immunosuppression in adult lung transplant recipients: prevalence and risk factors. J Heart Lung Transplant. 2011;30:1275–80. doi: 10.1016/j.healun.2011.05.007. [DOI] [PubMed] [Google Scholar]
- 48.Kung M, Koschwanez HE, Painter L, et al. Immunosuppressant nonadherence in heart, liver, and lung transplant patients: associations with medication beliefs and illness perceptions. Transplantation. 2012;93:958–63. doi: 10.1097/TP.0b013e31824b822d. [DOI] [PubMed] [Google Scholar]
- 49.Bodenheimer T, Lorig K, Holman H, et al. Patient self-management of chronic disease in primary care. JAMA. 2002;288:2469–75. doi: 10.1001/jama.288.19.2469. [DOI] [PubMed] [Google Scholar]
- 50.Holman H, Lorig K. Patient self-management: a key to effectiveness and efficiency in care of chronic disease. Public Health Rep. 2004;119:239–43. doi: 10.1016/j.phr.2004.04.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Goetzmann L, Scheuer E, Naef R, et al. Psychosocial situation and physical health in 50 patients > 1 year after lung transplantation. Chest. 2005;127:166–70. doi: 10.1378/chest.127.1.166. [DOI] [PubMed] [Google Scholar]
- 52.Vermeulen KM, Ouwens JP, van der Bij W, et al. Long-term quality of life in patients surviving at least 55 months after lung transplantation. Gen Hosp Psychiatry. 2003;25:95–102. doi: 10.1016/s0163-8343(03)00007-0. [DOI] [PubMed] [Google Scholar]
- 53.Rosenberger EM, DiMartini AF, Toyoda Y, et al. Psychiatric predictors of 10-year outcomes after lung transplantation [abstract 374] J Heart Lung Transplant. 2012;31(4S):S132–3. [Google Scholar]
- 54.Mason DP, Solovera-Rozas M, Feng J, et al. Dialysis after lung transplantation: prevalence, risk factors and outcome. J Heart Lung Transplant. 2007;26:1155–62. doi: 10.1016/j.healun.2007.08.006. [DOI] [PubMed] [Google Scholar]
- 55.Kulak CA, Borba VZ, Kulak J, Jr, et al. Transplantation osteoporosis. Arq Bras Endocrinol Metabol. 2006;50:783–92. doi: 10.1590/s0004-27302006000400023. [DOI] [PubMed] [Google Scholar]
- 56.Anile M, Venuta F, Diso D, et al. Malignancies following lung transplantation. Transplant Proc. 2007;39:1983–4. doi: 10.1016/j.transproceed.2007.05.036. [DOI] [PubMed] [Google Scholar]
- 57.Kremer BE, Reshef R, Misleh JG, et al. Post-transplant lymphoproliferative disorder after lung transplantation: a review of 35 cases. J Heart Lung Transplant. 2012;31:296–304. doi: 10.1016/j.healun.2011.10.013. [DOI] [PubMed] [Google Scholar]
- 58.Zivkovic SA, Jumaa M, Barisic N, et al. Neurologic complications following lung transplantation. J Neurol Sci. 2009;280:90–3. doi: 10.1016/j.jns.2009.02.308. [DOI] [PubMed] [Google Scholar]
- 59.Kugler C, Tegtbur U, Gottlieb J, et al. Health-related quality of life in two hundred-eighty lung transplant recipients. J Heart Lung Transplant. 2005;24:2262–8. doi: 10.1016/j.healun.2005.07.005. [DOI] [PubMed] [Google Scholar]
- 60.Rosenberger EM, Dew MA, Crone C, et al. Psychiatric disorders as risk factors for adverse medical outcomes after solid organ transplantation. Curr Opin Organ Transplant. 2012;17:188–92. doi: 10.1097/MOT.0b013e3283510928. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Christie JD, Edwards LB, Kucheryavaya AY, et al. The Registry of the International Society for Heart and Lung Transplantation: twenty-eighth adult lung and heart-lung transplant report–2011. J Heart Lung Transplant. 2011;30:1104–22. doi: 10.1016/j.healun.2011.08.004. [DOI] [PubMed] [Google Scholar]
- 62.Song MK, DeVito Dabbs A, Studer SM, et al. Course of illness after the onset of chronic rejection in lung transplant recipients. AmJ Crit Care. 2008;17:246–53. [PubMed] [Google Scholar]
- 63.Vermuelen KM, van der Bij W, Erasmus ME, et al. Long-term health-related quality of life after lung transplantation: different predictors for different dimensions. J Heart Lung Transplant. 2007;26:188–93. doi: 10.1016/j.healun.2006.11.006. [DOI] [PubMed] [Google Scholar]
- 64.van den Berg JW, Geertsma A, van der Bij W, et al. Bronchiolitis obliterans syndrome after lung transplantation and health-related quality of life. Am J Re-spir Crit Care Med. 2000;161:1937–41. doi: 10.1164/ajrccm.161.6.9909092. [DOI] [PubMed] [Google Scholar]
- 65.Song MK, DeVito Dabbs A, Studer SM, et al. Exploring the meaning of chronic rejection after lung transplantation and its impact on clinical management and caregiving. J Pain Symptom Manage. 2010;40:246–55. doi: 10.1016/j.jpainsymman.2009.12.014. [DOI] [PubMed] [Google Scholar]
- 66.Vasiliadis HM, Collet JP, Poirier C. Health-related quality-of-life determinants in lung transplantation. J Heart Lung Transplant. 2006;25:226–33. doi: 10.1016/j.healun.2005.08.008. [DOI] [PubMed] [Google Scholar]
- 67.Rutherford RM, Fisher AJ, Hilton C, et al. Functional status and quality of life in patients surviving 10 years after lung transplantation. Am J Transplant. 2005;5:1099–104. doi: 10.1111/j.1600-6143.2004.00803.x. [DOI] [PubMed] [Google Scholar]
- 68.Petrucci L, Ricotti S, Michelini I, et al. Return to work after thoracic organ transplantation in a clinically stable population. Eur J Heart Fail. 2007;9:1112–9. doi: 10.1016/j.ejheart.2007.08.002. [DOI] [PubMed] [Google Scholar]
- 69.Cicutto L, Braidy C, Moloney S, et al. Factors affecting attainment of paid employment after lung transplantation. J Heart Lung Transplant. 2004;23:481–6. doi: 10.1016/S1053-2498(03)00226-2. [DOI] [PubMed] [Google Scholar]
- 70.De Baere C, Delva D, Kloeck A, et al. Return to work and social participation: does type of organ transplantation matter? Transplantation. 2010;89:1009–15. doi: 10.1097/TP.0b013e3181ce77e5. [DOI] [PubMed] [Google Scholar]
- 71.Gross CR, Kreitzer MJ, Thomas W, et al. Mindfulness-based stress reduction for solid organ transplant recipients: a randomized controlled trial. Altern Ther Health Med. 2010;6:30–8. [PMC free article] [PubMed] [Google Scholar]
- 72.Abecassis MM, Bridges ND, Clancy CJ, et al. Solid organ transplantation in older adults: current status and future research. Am J Transplant. 2012;12:2608–22. doi: 10.1111/j.1600-6143.2012.04245.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Vadnerkar A, Toyoda Y, Crespo M, et al. Age-specific complications among lung transplant recipients 60 years and older. J Heart Lung Transplant. 2011;30:273–81. doi: 10.1016/j.healun.2010.08.032. [DOI] [PubMed] [Google Scholar]
- 74.Coffman KL, Crone C. Rational guidelines for transplantation in patients with psychotic disorders. Curr Opin Organ Transplant. 2002;7:385–8. [Google Scholar]
- 75.Okayasu H, Ozeki Y, Chida M, et al. Lung transplantation in a Japanese patient with schizophrenia from brain-dead donor. Gen Hosp Psychiatry. 2012 Apr 26; doi: 10.1016/j.genhosppsych.2012.03.013. Epub ahead of print. [DOI] [PubMed] [Google Scholar]
- 76.Song MK, DeVito Dabbs A, Studer SM, et al. Palliative care referrals after lung transplantation in major transplant centers in the United States. Crit Care Med. 2009;37:1288–92. doi: 10.1097/CCM.0b013e31819cec62. [DOI] [PubMed] [Google Scholar]
- 77.Rodrigue JR, Baz MA. Waiting for lung transplantation: quality of life, mood, caregiving strain and benefit, and social intimacy of spouses. Clin Transplant. 2007;21:722–7. doi: 10.1111/j.1399-0012.2007.00729.x. [DOI] [PubMed] [Google Scholar]
- 78.Goetzinger AM, Blumenthal JA, O'Hayer CV, et al. Stress and coping in caregivers of patients awaiting solid organ transplantation. Clin Transplant. 2012;26:97–104. doi: 10.1111/j.1399-0012.2011.01431.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Claar RL, Parekh PI, Palmer SM, et al. Emotional distress and quality of life in caregivers of patients awaiting lung transplant. J Psychosom Res. 2005;59:1–6. doi: 10.1016/j.jpsychores.2005.03.007. [DOI] [PubMed] [Google Scholar]
- 80.Xu J, Adeboyejo O, Wagley E, et al. Daily burdens of recipients and family caregivers after lung transplant. Prog Transplant. 2012;22:41–7. doi: 10.7182/pit2012815. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Selwood A, Johnston K, Katona C, et al. Systematic review of the effect of psychological interventions on family caregivers of people with dementia. J Affect Disord. 2007;101:75–89. doi: 10.1016/j.jad.2006.10.025. [DOI] [PubMed] [Google Scholar]
- 82.Rodrigue JR, Widows MR, Baz MA. Caregivers of lung transplant candidates: do they benefit when the patient is receiving psychological services? Prog Transplant. 2006;16:336–42. doi: 10.1177/152692480601600409. [DOI] [PubMed] [Google Scholar]