Abstract
Objective: Computerized cognitive behavioral therapy (cCBT) and cognitive bias modification for interpretation (CBM-I) both have demonstrated efficacy in alleviating social anxiety, but how they compare with each other has not been investigated. The present study tested the prediction that both interventions would reduce anxiety relative to a no-intervention comparison condition, but CBM-I would be particularly effective at modifying threat-related cognitive bias under high mental load. Method: Sixty-three primarily Caucasian adults (mean age = 22.7, SD = 5.87; 68.3% female) with high social anxiety, randomly allocated to 3 groups: CBM-I (n = 21), cCBT (n = 21), and a no-intervention control group (n = 21) provided complete data for analysis. Pre- and postintervention (4 sessions lasting 2 weeks, control participants only attended the pre–post sessions) self-report measures of anxiety, depression, attentional control, and threat-related interpretive bias were completed. In addition, interpretive bias under high versus low cognitive load was measured using the Scrambled Sentences Test. Results: Both CBM-I and cCBT groups reported significantly reduced levels of social anxiety, trait anxiety, and depression and improved attentional control, relative to the control group, with no clear superiority of either active intervention. Although both active conditions reduced negative bias on the Scrambled Sentences Test completed under mental load, CBM-I was significantly more effective at doing so. Conclusions: The results suggest that although not differing in therapeutic efficacy, CBM-I and cCBT might differ in the resilience of their effects when under mental load.
Keywords: anxiety, cognitive bias modification, computerized cognitive behavioral therapy, interpretive bias, attentional control
Social anxiety (or social phobia) is characterized by an intense and a persistent fear of being negatively evaluated in social or performance situations (Diagnostic and Statistical Manual of Mental Disorders, fourth edition [DSM–IV]; American Psychiatric Association, 1994). Ranked among the most common psychiatric disorders (Fehm, Pelissolo, Furmark, & Hans-Ulrich, 2005), social phobia subsists even though most individuals with the condition are regularly exposed to some of their feared situations without receiving negative feedback (Clark & McManus, 2002). Cognitive theories (e.g., Beck & Clark, 1997; Mathews & Mackintosh, 1998) suggest that threat-related information-processing biases are an important maintaining factor within the disorder. Numerous studies have supported cognitive models of social anxiety, demonstrating that socially anxious individuals preferentially attend to negative social cues, such as angry faces (attention bias; e.g., for a review, see Bar-Haim, Lamy, Pergamin, Bakermans-Kranenburg, & van IJzendoorn, 2007) and perceive emotionally aversive meanings in ambiguous social situations (interpretation bias; e.g., Stopa & Clark, 2000).
On the basis of cognitive models of psychopathology, cognitive behavioral therapy (CBT) works on the premise that maladaptive information processing (e.g., attention and interpretation biases) has a causal role in anxiety and that when this thinking is corrected, anxiety will be attenuated (Beck & Clark, 1997; DeRubeis, Siegle, & Hollon, 2008). Engagement in CBT explicitly requires participants to consciously identify their negative thought processes and challenge the validity of their beliefs, often through behavioral experiments that expose them to their feared situations (DeRubeis et al., 2008; Mathews, 2006). Randomized controlled trials (RCTs) have shown that CBT can be efficacious in reducing symptoms of anxiety (Hofmann & Smits, 2008) and threat-related bias (e.g., Tobon, Ouimet, & Dozois, 2011). Given the intensive practitioner involvement required in traditional CBT, novel computer-aided versions of CBT (cCBT) have been developed that can be delivered online and require minimal face-to-face contact time (Andersson, Carlbring, Berger, Almlov, & Cuijpers, 2009). Such Internet-delivered self-help can lead to large posttreatment within group reductions in social phobia symptoms (Cohen's d = 1.38–1.64), with improvements maintained at both 6-month (ds = 1.35–1.65) and 30-month follow-up (ds = 1.10–1.71; Berger et al., 2011; Carlbring, Nordgren, Furmack, & Andersson, 2009). Interestingly, these more economic approaches have been shown to be just as effective as therapist-led care for social phobia, generalized anxiety, and mild to moderate depression, despite their self-help format (Andersson et al., 2009; Kaltenthaler et al., 2006; Nordgreen et al., 2012; Proudfoot et al., 2004).
Provision of such computer-administered interventions is vital given that many people who might profit from treatment for psychiatric disorders (primarily anxiety and depression) are unable or unwilling to seek it out (Kessler et al., 2005), particularly in the context of social anxiety disorder (Mobini, Reynolds, & Mackintosh, 2012). In Europe, only one quarter of those affected by mental illness are in any form of treatment, indicating considerable unmet need (Wittchen & Jacobi, 2005). One factor involved is a reluctance to attend mental health clinics for conditions seen as stigmatizing; increasing availability of computer-based therapy that can be accessed at home will help to address this need. In addition, although CBT has a promising evidence base, a broader repertoire of cognitive therapies available could be beneficial in meeting different patient needs. For instance, some people may be unwilling or unable to reflectively think about their own thinking patterns, or be reluctant to disclose intimate thoughts and feelings either in person (as in traditional CBT) or online (as in cCBT). Consequently, there is a need for new treatments that do not require explicit discussion of sensitive issues, and can be delivered in an easy and a cost-effective way, such as online or via a CD. One potential candidate is cognitive bias modification (CBM), a newly emerging technique that implicitly retrains threat-related cognitive biases. Rather than requiring individuals to engage in reflective thinking about their own thought patterns (as in cCBT), CBM instead erodes threat-related cognitive biases by repeated computer-based practice in disengaging from threat-related stimuli using a visual probe task (cognitive bias modification for attention; CBM-A), or interpreting emotional ambiguity in a positive direction (cognitive bias modification for interpretation; CBM-I). Initial studies suggest this approach can be efficacious in reducing social anxiety. For example, CBM-A has been shown to reduce symptoms of social phobia over the time of training (50% vs. 14% in the trained vs. control condition no longer meeting diagnosis), with effects maintained at a 4-month follow-up (Amir et al., 2009). Consistent with this, Schmidt, Richey, Buckner, and Timpano (2009) demonstrated that eight sessions of CBM-A reduces social and trait anxiety in individuals with generalized social anxiety disorder (72% vs. 11% in the CBM-A vs. control condition no longer meeting DSM–IV diagnosis criteria), with effects maintained at 4-month follow-up.
CBM-I is showing similar successes. In a typical CBM-I session, participants are asked to read and imagine themselves in a series of emotionally ambiguous scenarios. Each scenario remains ambiguous until the final word, which is presented as an incomplete word that has only one meaningful solution. Completing the final word resolves the scenario in a positive direction. This encourages the participant to form positive images of the emotionally ambiguous scenarios (cf. Holmes, Mathews, Dalgleish, & Mackintosh, 2006), thus training them to disambiguate emotional ambiguity in a positive way in order to do well on the task. Mathews, Ridgeway, Cook, and Yiend (2007) showed that four sessions of CBM-I can reduce trait anxiety in a high-anxious population; similarly, Salemink, van den Hout, and Kindt (2009) demonstrated reductions in trait anxiety, state anxiety, and general psychopathology through multiple CBM-I sessions. Murphy, Hirsch, Mathews, Smith, and Clark (2007) reported that highly socially anxious individuals were trained to interpret novel stimuli benignly, interpreted new situations less negatively, and self-reported less anxiety about upcoming social events, compared with a control group. Using a slightly different interpretive training paradigm, Beard and Amir (2008) showed a drop in self-reported social anxiety symptoms in a highly socially anxious population, whereas Amir and Taylor (2012b) demonstrated reductions in clinician-rated social anxiety symptoms compared with placebo-interpretive training.
Finally, two studies have evaluated a combined CBM-A plus CBM-I intervention. Beard, Weisberg, and Amir (2011) provided preliminary indication that combined training can reduce self-reported symptoms of social anxiety in a highly socially anxious population compared with a control group. Similarly, Brosan, Hoppitt, Shelfer, Sillence, and Mackintosh (2011) found combined CBM-I and CBM-A led to reductions in state and trait anxiety over four sessions in a diagnosed, clinical sample of individuals with social phobia/generalized anxiety disorder.
The logical next step given these promising early findings is for investigation into how CBM compares with other established therapies (Bar-Haim, 2010). Surprisingly, as yet, we know of no published studies comparing the efficacy of CBM against presently recommended low-intensity therapies for anxiety (such as cCBT). Therefore, the main aim of the present study was to conduct the first assessment of the efficacy of CBM (in this case, CBM for interpretation) versus a presently recommended treatment (cCBT) at reducing threat-related interpretive bias (as assessed by the Ambiguous Social Situations Interpretation Questionnaire [ASSIQ] and Scrambled Sentences Test [SST]) and symptoms of social anxiety, general anxiety, and depression relative to a no-intervention comparison condition, in a sample of socially anxious individuals.
A second aim was to investigate the underlying mechanisms of both active treatments. Greater understanding of mechanisms underpinning the efficacy of these interventions is important in helping to streamline delivery and maximize utility. We first consider the role of attentional control. Clinical and nonclinical anxiety is associated with poor attentional control assessed using self-report and imaging methods (e.g., Bishop, Duncan, Brett, & Lawrence, 2004; Derryberry & Reed, 2002). CBT is thought to increase inhibitory executive control and appears to improve functions of the prefrontal cortex that are impaired in anxiety, such as directing attention away from threat distractors, volitional regulation of emotional responses, and reappraisal of meaning (DeRubeis et al., 2008). Emerging evidence from the CBM-A (attention retraining) literature suggests that it could impact on top-down control. Browning, Holmes, Murphy, Goodwin, and Harmer (2010) demonstrated that following a single session of avoid-threat CBM-A, there was greater activation in prefrontal areas associated with control mechanisms when participants were required to attend to threat-relevant stimuli. In addition, Eldar and Bar-Haim (2010) found that anxious participants trained to disengage their attention from threat images displayed increased N2 amplitude (an event-related potential component that is associated with increases in attentional control). Indeed, there has been some speculation that CBM for attention might have its effects via training general attentional control capacities, regardless of its valenced direction (Bar-Haim, 2010). To date, one study has indicated that CBM for interpretation might influence highly socially anxious participants' ability to disengage their attention from threat (Amir, Bomyea, & Beard, 2010). To further interrogate this possible mechanism of action, in the present study we asked participants to complete a self-report measurement of attentional control (the Attentional Control Scale [ACS]; Derryberry & Reed, 2002) pre- and postintervention.
Second, we considered the hypothesis that CBM-I might improve positive bias (and reduce anxiety) via promotion of a more habitual way of responding, whereas cCBT might encourage change in bias via a more explicit, controlled, deliberate process of reappraisal. We hypothesized that, whereas cCBT would rely on adequate cognitive resources available to enact the modified cognitive style, change induced via CBM-I would be less reliant on having cognitive resources available. As such, these changes might be more resilient in stressful situations when cognitive resources are depleted (Baert, De Raedt, & Koster, 2011). To investigate this possibility, we used the SST, which allows the measurement of emotional information processing under conditions of high versus low mental load. In the SST, participants are presented with a number of sentences in which the order of words is scrambled (e.g., “others foolish I to sensible appear”). Their task (under a strict time limit) is to unscramble the word order in each sentence to create a meaningful resolution, but without necessarily using all of the words provided. Each sentence can be unscrambled to create a sentence with either a positive or a negative meaning (e.g., “I appear sensible to others”, or “I appear foolish to others”). The number of negative resolutions that the participants make is taken to reflect the degree of negative interpretive bias. Asking participants to hold a six-digit number in mind while unscrambling the sentences allows researchers to investigate interpretive bias while cognitive resources are depleted (meaning that any effortful processing required to maintain a positive bias would be less effective). For example, Watkins and Moulds (2007) investigated the use of effortful strategies in recovery from depression by comparing how scrambled sentences were resolved with concurrent load (participants were asked to remember a number while working on the sentences) versus no load (participants were not asked to remember a number, thus freeing up executive resources to allow more effortful processing of the task). The generation of more negative sentences in the load condition indicated that negative depressogenic constructs remained accessible in this recovered depressed sample, suggesting that their activation was being effortfully down-regulated in the no-load condition. Standage, Ashwin, and Fox (2010) administered the SST with mental load before and after an interpretation bias modification intervention (in a healthy sample) to examine the effect of CBM-I on interpretive bias when cognitive resources were depleted and found that CBM successfully modified interpretive bias under these conditions. In the present study, the SST assessed the impact of each intervention on interpretive bias under conditions of high versus low cognitive load and how bias assessed with or without load mediated change in symptoms.
To summarize, to our knowledge this is the first study comparing CBM-I with cCBT, relative to a no-intervention control condition. We predicted that both CBM-I and cCBT would reduce anxiety and depressive symptoms and improve attentional control compared with the control group. As this was the first time that cCBT had been compared with CBM-I, we did not have any strong predictions regarding whether one or the other would be more efficacious in terms of their superiority over the control condition. However, we predicted that the effects of CBM-I on interpretive bias under load would be greater than the effects of cCBT on interpretive bias under load.
Method
Participants
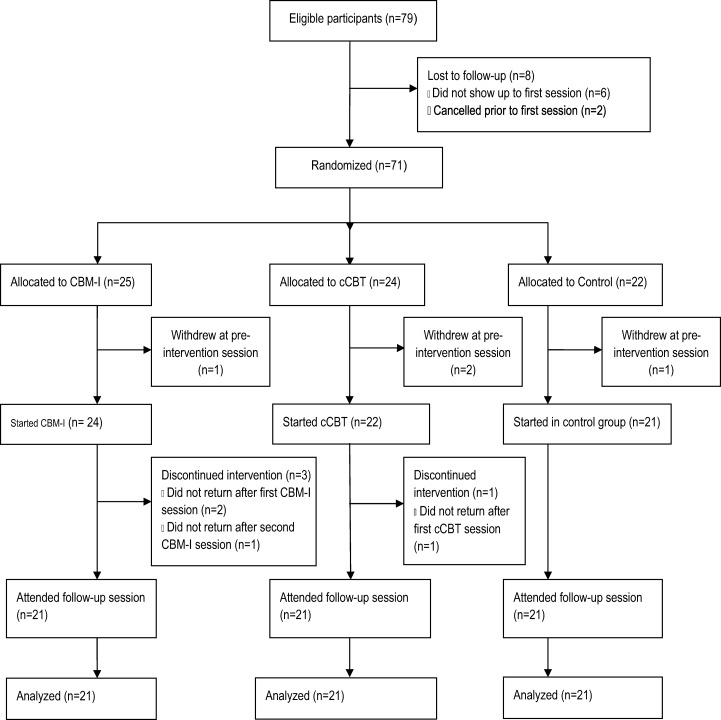
A CONSORT diagram (Schulz, Altman, Moher, & the CONSORT group, 2010) illustrating participant flow throughout the study is presented in Figure 1. A total of 71 participants were recruited via a poster and an e-mail campaign at the University of East Anglia (UEA), which specifically asked for people who felt they were experiencing social anxiety. Individuals who expressed interest were screened, and only those who scored ≥ 17 on the Fear of Negative Evaluation Scale (FNE; Watson & Friend, 1969) were invited to take part. The 71 participants were randomly allocated to one of three conditions—interpretation bias modification (CBM-I; n = 25), cCBT (n = 24), or a control condition not involving any intervention (n = 22). Randomization was subject to the restriction that group sizes were approximately equal. All participants were native English speakers and had not received psychological help for anxiety or depression within the past 6 months. Of the 71 participants who were randomized, eight (11.27%) subsequently dropped out (see Figure 1). Sixty-three participants (20 men and 43 women, mean age = 22.7, SD = 5.87, range = 18–48) therefore completed the study and provided complete data. They were paid £30 (approximately $45 U.S.) for taking part. Overall, this final sample had a mean trait anxiety score of 52.1, approximately two standard deviations above the State–Trait Anxiety Inventory–Trait (STAI-T) reported norms (Spielberger, Gorsuch, Lushene, Vagg, & Jacobs, 1983). Mean Beck Depression Inventory–II (BDI-II) scores of 17.3 indicated mild depression (Beck, Steer, & Brown, 1996), and mean Social Phobia Inventory (SPIN) scores of 33.5 signified a moderate level of social anxiety (Connor et al., 2000; see Table 1). The majority of participants in each group in the final sample fell above the recommended clinical cutoff score of 19 for social phobia on the SPIN (CBM-I: 90.5%; cCBT: 76.2%; control: 81.0%). On the BDI-II, 38.10% of participants in the CBM-I group fell above the cut-off score of 20 for moderate depression; 23.8% were similarly depressed in the cCBT group, along with 52.4% in the control group (Beck et al., 1996).
Figure 1. Consolidated Standards of Reporting Trials (CONSORT) diagram illustrating flow of participants through the study. CBM-I = cognitive bias modification for interpretation; cCBT = computer-aided version of cognitive behavioral therapy.
Table 1. Means of Age, FNE, Trait Anxiety, Social Anxiety, Depression, Attentional Control, and Interpretation Bias With Standard Deviations and Gender Ratio.
Interpretation bias modification procedure
Given the importance of developing an intervention that is cost-effective and highly accessible, we opted to select as small a number of sessions as could be justified based on the previous research. Studies to date have yielded favorable results in anxious populations using only four sessions (e.g., Brosan et al., 2011; Mathews et al., 2007), and so we decided to implement four sessions of CBM-I in the laboratory using E-Prime (Schneider, Eschman, & Zuccolotto, 2002) software. A researcher was present at sessions to ensure participant attendance and general task compliance. A single session comprised 40 different scenarios related to issues that might concern socially anxious individuals such as making a phone call (presented in random order). On the basis of Mathews and Mackintosh (2000), each scenario had the final word missing and was emotionally ambiguous up to this point (e.g., “As you are walking down a crowded street in Norwich, you see your new flatmate on the other side. You call out but your flatmate does not answer. You think that this was because they were—”). The final word always resolved the ambiguity in a benign way and was presented in an incomplete form on the screen after the participant had read the preceding scenario (e.g., pr—c-upi-d—“preoccupied”).
Participants were asked to imagine themselves in the situation and to use their image to identify what the incomplete word was (pressing the down-arrow key as soon as they knew). They were then prompted to type in the first missing letter of this word before the correct complete word (e.g., “preoccupied”) was presented, and a comprehension question asked them to confirm the interpretation of the scenario (e.g., “Did your flatmate deliberately ignore your call to her in the street?”). Participants used the arrow keys to answer yes or no to this question, and they were given feedback (a “Correct!” or an “Incorrect” message) that reinforced a positive interpretation. The next scenario then followed.
cCBT procedure
A course of cCBT for social anxiety was delivered using the e-couch website. E-couch materials were developed by the e-hub group at the Australian National University, who have produced two other successful cCBT websites for depression and generalized anxiety, “Blue Pages” and “MoodGYM.” A clustered RCT has demonstrated the efficacy of MoodGYM in successfully reducing symptoms of depression and anxiety (Calear, Christensen, Mackinnon, Griffiths, & O'Kearney, 2009).
In the present study, participants accessed the e-couch social anxiety program online over four sessions in the laboratory. A researcher ensured participant attendance and general compliance with the module. The cCBT program contained informational and CBT modules for social anxiety. In the first computer session, participants completed the psychoeducational subsection, which contained information on the nature of social anxiety, and in the next three sessions accessed the toolkits that targeted typical thinking in social anxiety. Toolkits completed were “exposure practice,” “modifying your thinking,” “attention practice,” and “social skills training.” Exposure practice looked at overcoming avoidance and safety behaviors; modifying your thinking targeted negative automatic thoughts; attention practice focused on turning attention outward rather than inward with a view to increasing confidence; and social skills training addressed particular skills useful in social situations, such as maintaining eye contact appropriately during conversations. During the course, participants completed two pieces of homework concerning exposure practice and social skills practice, respectively.
Self-Report Measures
Participants were given a pack of six questionnaires. The first four of these questionnaires measured symptoms of social anxiety and depression. Social anxiety was assessed using the FNE (Watson & Friend, 1969) and the SPIN (Connor et al., 2000). The Trait scale of the Spielberger State–Trait Anxiety Inventory (Spielberger et al., 1983) was used to measure general anxiety, and the BDI-II was selected as the self-report measure of depression (Beck et al., 1996).
Attentional control was assessed using the ACS (Derryberry & Reed, 2002). This is a 20-item self-report questionnaire measuring two types of attention: attention focusing (e.g., “When I need to concentrate and solve a problem, I have trouble focusing my attention”) and attention shifting (e.g., “I can quickly switch from one task to another”). Items are scored on a 4-point scale ranging from 1 (almost never) to 4 (always). After reverse scoring inversely coded items, a total score is summed across all items, with higher scores indicating greater attentional control. Reliability and validity of the measure has been demonstrated by Derryberry and Reed (2002).
The ASSIQ (Stopa & Clark, 2000) was used as a measure of interpretive bias. This is a 24-item questionnaire that incorporates two classes of ambiguous events: social situations (n = 14; e.g., “You go into a shop and the assistant ignores you”) and control situations (n = 10; e.g., “A letter marked ‘urgent’ arrives”). Each situation is followed by the question “Why?” and participants are required to write down the first explanation that comes to mind and then rank three provided explanations (one negative and two benign) in order of likelihood of coming to mind in real life. Finally, they rate belief (where 0 = not at all likely to be true and 8 = extremely likely to be true) in each outcome. Rankings are given a score of 3 if the negative interpretation is ranked first, 2 if it is ranked second, and 1 if it is ranked last. The open-ended questions were classified according to a predetermined set of categories provided by the questionnaire author: negative social, negative nonsocial, anxiety related, neutral, and unclassifiable.
To check present category reliability of the ASSIQ, a second rater independently categorized items from seven participants in each group. The intraclass correlation coefficient (ICC) was very good for categorization of baseline responses as negative social (ICC = 0.94), negative nonsocial (ICC = 1), anxiety related (ICC = 1), and neutral (ICC = 0.9). For negative social responses at follow-up, the ICC was 0.97, and for neutral items it was 0.96. Neither judge categorized follow-up responses as negative nonsocial or anxiety related.
The SST
The SST (Wenzlaff, 1993) was used to assess the predictions regarding the effect of CBM-I versus cCBT on interpretive bias under conditions of high versus low mental load. In each test session, participants unscrambled two lists of 20 scrambled sentences (e.g., others is hard speaking easy with). Every scrambled sentence contained six words and had one possible negative interpretation (e.g., speaking with others is hard) and one positive interpretation (e.g., speaking with others is easy). Participants were required to unscramble one list with cognitive load (i.e., while remembering a six-digit number; the load condition) in 4 min and one without load (the no-load condition), also in 4 min. Instructions were to “Unscramble the sentences to form the first statement that comes to mind” and to do this “as quickly and accurately as possible.” In the load condition, they were given 10 s to look at the number before completing the sentences, and at the end of the 4 min or at the end of the task, they were asked to write down the number in the box provided. Forty sentences were taken from Standage et al. (2010), and 40 additional sentences were developed in the same way for the present study.
Unscrambled sentences were scored by calculating the proportion of grammatically correct sentences completed in accordance with instructions that had a negative valence. To check scoring reliability, a second judge independently scored all the sentences. Judges' correlations were high at baseline (r = .99, p < .001) and follow-up (r = .96, p < .001).
Procedure
Ethical approval for the study was obtained from the UEA School of Social Work and Psychology Research Ethics committee. After giving informed written consent, participants completed paper versions of the questionnaire measures (baseline). Questionnaires were always presented in the same order (FNE, STAI-T, SPIN, BDI-II, ACS, ASSIQ). The SST was then administered with order of sentence set and load and no-load versions each counterbalanced across participants within conditions. Next, participants completed the first session of either the CBM-I or the cCBT, depending on condition. Control participants were thanked and asked to return to the laboratory in 2 weeks' time. All study sessions were completed in the same computer laboratory on campus.
Of the 63 participants who completed the study, 59 (93.7%) completed the follow-up session exactly 2 weeks after the preintervention session. Two participants returned on the 15th day (cCBT) and two on the 18th day (CBM-I). At the postintervention session, the SST was administered first, followed by the six questionnaires, after which participants were debriefed. Control participants were given the opportunity to register with e-couch and begin the social anxiety module if they so wished.
Results
Participants
As shown in Table 1, all three groups were comparable at baseline on all measures of anxiety, depression, attentional control, interpretation bias (as assessed by the ASSIQ and the SST), age, and gender ratios (ps > .2).
Data Analytic Approach
A complete-case analysis approach, where only participants with all data points complete are included, was the primary approach used to analyze the data due to the small number of cases who dropped out (see Figure 1) and because it was reasonable to assume that the data were missing at random (Little & Rubin, 1987). In addition, for the symptom outcomes we also report intent-to-treat (ITT) analyses, and the pattern of results was unaltered. For the mechanism outcomes and associated mediation analyses, we did not compute ITT analyses, as adherence to protocol is necessary in order for putative treatment mechanisms to take effect (e.g., Kuyken et al., 2010).
Effects of CBM-I and cCBT on Self-Report Measures of Anxiety and Depression
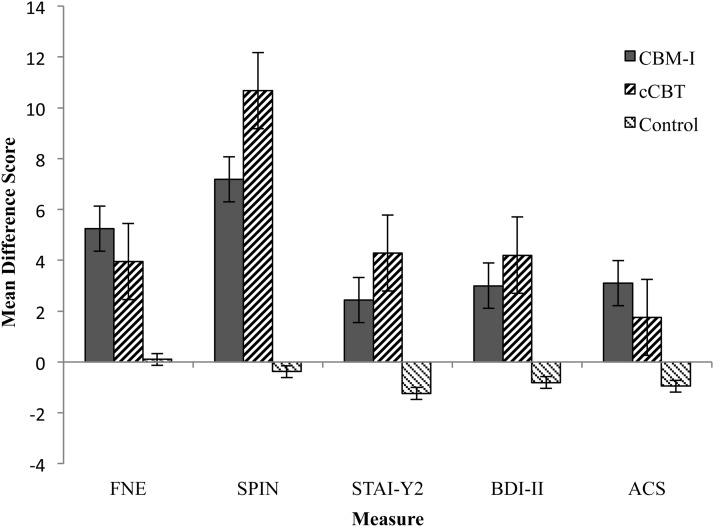
All participants who completed interpretation bias training (n = 21) fell within three standard deviations of the mean accuracy on comprehension question input, indicating good task compliance. We did not have a comparable measure of cCBT compliance, although all 21 participants attended all four cCBT sessions. We performed separate mixed model analyses of variance (ANOVAs), with time (pre–post) entered as the within-subjects factor and group (CBM-I, cCBT, or control) entered as the between-subjects factor for each of the self-report measures. Results revealed a significant Time × Group interaction on all four measures, FNE, F(2, 60) = 3.84, p = .03, η2 = .11; SPIN, F(2, 60) = 7.55, p = .001, η2 = .20; STAI-Trait, F(2, 60) = 6.71, p = .002, η2 = .18; BDI-II, F(2, 59) = 3.95, p = .03, η2 = .12. These findings were followed up with three 2-way mixed model ANOVAs (CBM-I vs. control, cCBT vs. control, and CBM-I vs. cCBT) for each scale. In terms of social anxiety (FNE and SPIN), significant main effects of time (largest p = .014) were found in all cases, indicating that social anxiety improved overall. These main effects were qualified by the predicted Time × Group interactions when comparing CBM-I with the control group: FNE, F(1, 40) = 6.10, p = .02, η2 = .13; SPIN, F(1, 40) = 8.13, p = .007, η2 = .17, and cCBT with the control group: FNE, F(1, 40) = 6.69, p = .01, η2 = .14; SPIN, F(1, 40) = 18.09, p < .001, η2 = .31, indicating relatively greater reductions in social anxiety in the intervention groups as compared with controls (see Figure 2). When comparing the two intervention groups (CBM-I vs. cCBT), there was no significant Time × Group interaction for FNE (F < 1) or SPIN, F(1, 40) = 1.05, p = .31, η2 = .03, suggesting that the two interventions did not significantly differ in reducing social anxiety.
Figure 2. Mean difference scores (pre- minus postintervention) for the Fear of Negative Evaluation Scale (FNE), Social Phobia Inventory (SPIN), Trait scale of the Spielberger State–Trait Anxiety Inventory (STAI), Beck Depression Inventory–II (BDI-II), and Attentional Control Scale (ACS; post- minus preintervention) by group (a higher score indicates greater improvement in anxiety, depression, and attentional control). Error bars represent ± 1 standard error. CBM-I = cognitive bias modification for interpretation; cCBT = computer-aided version of cognitive behavioral therapy.
We analyzed trait anxiety (STAI) and depression (BDI-II) in a similar way (with comparisons between CBM-I vs. control, cCBT vs. control, and CBM-I vs. cCBT). There were no significant main effects of time for the comparison of CBM-I versus control group or cCBT versus control group (smallest p = .06). However, the predicted Time × Group interactions were evident when comparing CBM-I with the control group: STAI, F(1, 40) = 5.64, p = .02, η2 = .12; BDI-II, F(1, 40) = 4.50, p = .04, η2 = .10, and cCBT with the control group: STAI, F(1, 40) = 11.93, p = .001, η2 = .23; BDI-II, F(1, 39) = 7.22, p = .01, η2 = .16, indicating relatively greater reductions in trait anxiety and depression in the intervention groups as compared with the control group. When comparing CBM-I directly with cCBT, there was a highly significant main effect of time for both trait anxiety and depression, suggesting a decrease in trait anxiety and depression in the intervention groups overall: STAI, F(1, 40) = 21.24, p < .001, η2 = .35; BDI-II, F(1, 39) = 13.96, p = .001, η2 = .26, but there was no interaction between time and group: STAI, F(1, 40) = 1.63, p = .21, η2 = .04; BDI-II, F < 1, indicating that the interventions did not significantly differ in reducing trait anxiety and depression.
We also conducted ITT analyses for the four symptom outcome measures. For the five participants who dropped out of the trial following baseline assessment (see Figure 1), we imputed postintervention scores using the baseline-observation-carried-forward method (Little & Rubin, 1987). This is a conservative approach in trials such as the present one in which scores on the outcome variables generally improve over the intervention period. The three participants who signed up online for the study but did not attend baseline assessment were set aside from the ITT because we have no data on them and because they opted out of the trial prior to receiving their allocation of treatment condition. Treatment allocation therefore could not have influenced their choice to no longer attend. The ITT analyses revealed a comparable pattern of results as the complete-case analysis. Specifically, for all four symptom outcome measures, there was a significant Time × Group interaction (all Fs > 3.44, all ps < .04, all ηp2s > .10). Follow-up analyses revealed that both CBM-I and cCBT, analysed separately, were more efficacious than the control condition (all Fs > 4.23, all ps < .05, all ηp2s > .08). However, there was no significant difference in efficacy on any measure in a comparison of CBM-I and cCBT (all Fs < 2.11, all ps > .15, all ηp2s < .05).
Clinical change
Our primary standardized outcome measure for clinical change in social anxiety, the primary therapeutic target of the intervention, was the SPIN, as it is the clinically recommended measure of choice for social anxiety (Department of Health/Improving Access to Psychological Therapies [DH/IAPT], 2011). In accordance with the approach described by Jacobson and Truax (1991), clinically significant change was considered to have occurred if (a) the participant's score fell within the range of the functional population (in Connor et al., 2000), (b) the posttraining level of functioning was closer to the mean of the functional population than the mean of the dysfunctional population, and (c) the participant exhibited a statistically reliable reduction in scores from pre- to posttraining using the reliable change index (RCI; Jacobson & Truax, 1991). Using a cutoff value of 26.6 (the point that lies between the functional and dysfunctional means as outlined by Jacobson & Truax) in the complete-case-analysis, 13 participants had a baseline score above the cutoff in the CBM-I group, 14 in the cCBT group, and 13 in the control group. Of these, five CBM-I participants (38.5%), six cCBT participants (42.9%), and zero control participants displayed a reliable reduction in scores (RCI > 1.96) from above to below the cutoff value. The ITT analysis delivered comparable findings except there were 16 participants who scored above cutoff in the CBM-I group, five (31.3%) of whom displayed a reliable reduction. Proportions for the other groups were the same.
In summary, both the CBM-I and cCBT were efficacious at reducing social anxiety (as assessed by the FNE and the SPIN), trait anxiety (as assessed by the STAI), and depression (as assessed by the BDI-II), relative to the no-intervention comparison condition.
Effects of CBM-I and cCBT on Attentional Control
We performed a mixed model ANOVA on the attentional control scale scores, with time as the within-subjects factor and group as the between-subjects factor. As predicted, a significant Group × Time interaction was revealed, F(2, 60) = 4.88, p = .01, η2 = .14. To follow this up, three separate mixed model ANOVAs compared CBM-I with the control group, cCBT with the control group, and cCBT with CBM-I. In the comparisons of CBM-I with the control group and cCBT with the control group, there was no main effect of time: CBM-I, F(1, 40) = 2.27, p = .14, η2 = .05; cCBT, F < 1, but the predicted significant interactions between time and group indicated a greater improvement in attentional control in the CBM-I condition as compared with the control group: F(1, 40) = 8.11, p = .007, η2 = .17, and in the cCBT condition as compared with the control group, F(1, 40) = 5.79, p = .02, η2 = .13. A further mixed ANOVA with only the two intervention conditions showed a main effect of time, F(1, 40) = 12.18, p < .001, η2 = .23, indicating an overall improvement in attentional control, but the lack of a significant interaction between time and group, confirming that they did not differ in modifying perceived attentional control (F < 1) (see Figure 2). In summary, the intervention groups did not differ significantly in changes in attentional control as measured by the ACS, and they were each individually superior to the control group.
Effects on Ambiguous Social Scenario Interpretation Questionnaire
Open-ended questions responses and rankings
Due to the high percentage of open-ended question (OEQ) responses (73% at baseline and follow-up) falling into the negative social interpretation category, we used this measure as the dependent variable. Five participants could not be included in the analysis of rankings data because they failed to rank outcomes. We calculated difference scores (pre- minus postintervention) and performed separate mixed model ANOVAs on the OEQ and rankings data, with scenario type (social, control) as the within-subjects factor and group (CBM-I, cCBT, control) as the between-subjects factor for each. Results indicated there were main effects of scenario type; OEQ, F(1, 59) = 27.41, p < .001, η2 = .32; rankings, F(1, 55) = 11.56, p = .001, η2 = .17, and main effects of group; OEQ, F(2, 59) = 7.08, p = .002, η2 = .19; rankings, F(2, 55) = 3.43, p = .039, η2 = .11, together with the predicted significant Type × Group interactions, OEQ, F(2, 59) = 6.65, p = .002, η2 = .18; rankings, F(2, 55) = 4.96, p = .01, η2 = .15. Separate mixed model ANOVAs conducted on each scenario type revealed significant Time × Group interactions for social scenarios, OEQ, F(2, 59) = 7.21, p = .002, η2 = .20; rankings, F(2, 55) = 5.05, p = .01, η2 = .16, and not control scenarios (OEQ and rankings, Fs < 1). Follow-up least significant difference (LSD) tests on the OEQ responses to social scenarios suggested that the CBM-I group experienced a greater reduction in number of negative interpretations produced as compared with the control group (p < .001, 95% CI = [1.62, 5.28]), and a similar trend when compared with the cCBT group (p = .14, 95% CI = [−.48, 3.23]) (see Table 2). For rankings, compared with the control group, both the CBM-I group and cCBT group became significantly less likely to think that a negative interpretation of an ambiguous social situation would come to mind first in real life (CBM-I vs. control, p = .003, 95% CI = [.15, .71]; cCBT vs. control, p = .03, 95% CI = [.03, .62]). There was no difference in rankings between the CBM-I and cCBT groups (p = .49, 95% CI = [−.19, .39]).
Table 2. Mean ASSIQ Difference Scores by Group for Negative Social Interpretations of Open-Ended Questions With Standard Deviations.
Belief in negative and neutral interpretations
Five participants could not be included in the analysis because they failed to produce belief ratings. We performed a mixed model ANOVA on the difference scores, with scenario type (social, control) and valence (neutral, negative) as the within-subjects factors and group (CBM-I, cCBT, control) as the between-subjects factor. Results indicated there was a near significant main effect of scenario type, F(1, 55) = 3.86, p = .054, η2 = .07, and main effect of valence, F(1, 55) = 14.23, p < .001, η2 = .21, which was qualified by a significant Valence × Group interaction, F(2, 55) = 4.96, p = .010, η2 = .15. Investigative separate mixed model ANOVAs conducted for each category of belief (negative social, neutral social, negative control, neutral control) revealed a significant Time × Group interaction for belief in negative social situations only, F(2, 56) = 3.80, p = .028, η2 = .12. Follow-up LSD tests on the change-in-belief ratings suggested that the CBM-I group had become significantly less likely to believe negative interpretations of social situations compared with the control group (p = .008, 95% CI = [.33, 2.15]) but that there was no significant difference in change-in-belief ratings between the cCBT and control group (p = .11, 95% CI = [−.17, 1.75]) or the CBM-I and cCBT groups (p = .35, 95% CI = [−.51, 1.41]).
In summary, both the CBM-I and cCBT groups became significantly less likely to rank negative interpretations of ambiguous social situations as coming to mind first in real life. However, only the CBM-I group showed a reduction in the free generation of negative interpretations of ambiguous scenarios, and in the belief that the negative events would happen.
The SST
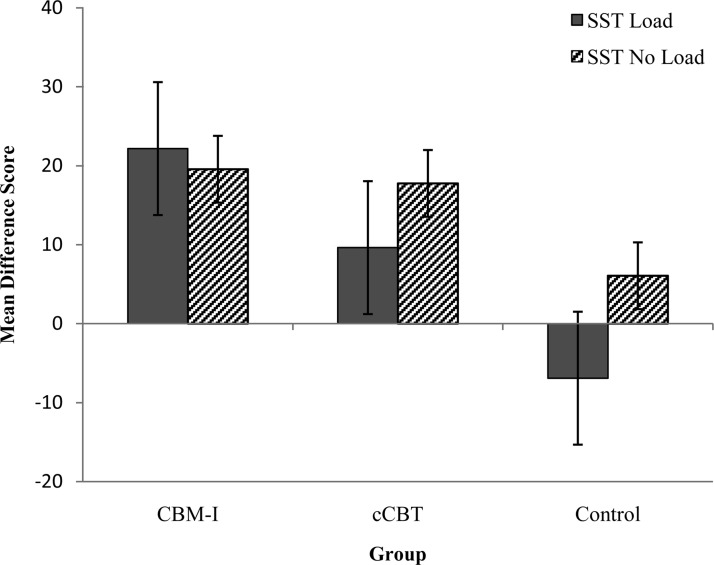
Two participants (one in the cCBT group and one in the control group) were excluded from the analysis because they did not follow instructions correctly. As noted by Wenzlaff, Rude, Taylor, Stultz, and Sweatt (2001), a potential complicating factor of the SST paradigm would occur if the groups differed in the effort they applied in remembering the six-digit number in the load condition. To assess this possibility, participants were assigned a recall score of 1 if they had correctly remembered the number and 0 if they had not. Overall, all participants wrote down a six-digit number as requested, and of these 69.8% had recalled the number correctly at baseline and 71.4% at follow-up. A chi-square analysis of recall scores at baseline indicated no reliable differences among the three groups of participants (χ2 < 1), and all participants were included in the final analyses. We conducted a mixed model ANOVA on the difference scores (pre- minus postintervention), with load condition (load, no load) as the within-subjects factors and group (CBM-I, cCBT, control) as the between-subjects factor. Results revealed a significant main effect of load, F(1, 58) = 5.95, p = .02, η2 = .09, and group, F(2, 58) = 6.34, p = .003, η2 = .18, and the predicted significant Load × Group interaction, F(2, 58) = 3.36, p = .042, η2 = .10. One-way ANOVAs showed that there was no significant main effect of group on change in negative interpretations when not under load, F(2, 58) = 1.99, p = .15, η2 = .06 (see Figure 3); however, there was a significant main effect of group on change in negative interpretations when under load, F(2, 58) = 10.81, p < .001, η2 = .27. Follow-up LSD tests revealed that both the CBM-I and cCBT groups displayed a greater drop in their negativity score under load as compared with the control condition (CBM-I vs. control, p < .001, 95% CI = [16.53, 41.61]; cCBT vs. control, p = .012, 95% CI = [3.85, 29.23]). To assess our prediction that CBM should be more effective than cCBT when under load, we directly compared CBM with cCBT. As predicted, participants in the CBM group had a greater drop in their negativity score under load as compared with the cCBT group (p = .05, 95% CI = [−.005, 25.07]) (see Figure 3).
Figure 3. Mean difference scores (pre- minus postintervention) for the Scrambled Sentences Test (SST) by group (a more positive score indicates a greater reduction in the proportion of negative resolutions generated). Error bars represent ± 1 standard error. CBM-I = cognitive bias modification for interpretation; cCBT = computer-aided version of cognitive behavioral therapy.
Mediation Analysis
We used the multiple mediation procedure developed by Preacher and Hayes (2008) to examine whether change in symptoms in the two active interventions was driven by change in interpretive bias or attentional control. Mediation is indicated by the z test of the indirect effect being significant and zero not falling in the 95% confidence interval of the bootstrapped indirect effect distribution. We ran each simulation 5,000 times, conducting separate analyses for cCBT and CBM-I (relative to the control) conditions. In each analysis, the predictor variable was group status (dummy coded as one for the control condition and zero for the active condition), and overall change across the symptom scales (FNE, BDI-II, STAI, and SPIN; z-transformed and then averaged) was the outcome measure. The mediator variables were change in perceived attentional control, change in sentence task performance in the load condition, and change in sentence task performance in the no-load condition (entered simultaneously into each model; all z-transformed).
Results indicated a significant overall mediating relationship for both CBM-I and cCBT (see Table 3). Consistent with the idea that changing interpretative bias contributes to symptom improvement, increasing performance on the SST under load mediated symptom improvement in the CBM-I and the cCBT conditions. In contrast, performance on the no-load version of the SST did not mediate the effects of either cCBT or CBM-I, relative to the control condition.
Table 3. Mediation Analyses With Mean Standardized Change From Pre–Post Intervention Across the Four Study Symptom Outcomes as the Dependent Variable, Group as the Independent Variable, and the Study Mechanism Measures as Mediators.
Although changes in perceived attentional control did not significantly mediate the relationship between symptom improvement and CBM-I, there was a significant mediation for cCBT. Inspection of the contrasts showed that the mediation effect was of a trend of greater magnitude in the load than the no-load analyses for both CBM-I and cCBT. There was also a trend for load to show a greater mediating effect than ACS scores in the CBM-I condition, but this did not hold in the cCBT analysis.
In summary, these data are consistent with the view that training anxious individuals to interpret information in a positive fashion partly contributes to symptom improvement in CBM-I, particularly when concurrent load is present. This mechanism also appears to be active in cCBT, and in addition changes in perceived attentional control contributed to symptom improvement following cCBT.
Discussion
Our first aim was to assess the relative efficacy of CBM-I and cCBT for improving anxiety and depression as compared with a control group. The results suggested that, in line with previous studies demonstrating the therapeutic efficacy of these low-intensity computer-assisted interventions (e.g., CBM-I; Blackwell & Holmes, 2010; cCBT; Proudfoot et al., 2004), both CBM-I and cCBT produced significant reductions in symptoms of social anxiety, trait anxiety, and depression, relative to the control group. Crucially, however, this is the first time that it has been demonstrated within a single study that CBM-I and cCBT are both efficacious in a high socially anxious population, and we found no support for a clear superiority of either active intervention over the other. Participants began the study with high self-reported fear of negative evaluation, and upon completion of either the CBM-I or the cCBT programs, this had dropped to within the range of average scorers (Watson & Friend, 1969). Similarly, on the clinically recommended SPIN (Connor et al., 2000; DH/IAPT, 2011), both intervention groups dropped over 7 points from a start point of moderate social anxiety, representing a clinically significant reduction in anxiety-related symptoms (Connor et al., 2000). In conjunction with past results, these findings suggest that CBM-I might represent a well-founded, short-course intervention for social anxiety disorder that has comparable efficacy with present low-intensity therapies such as cCBT. The ASSIQ provided a self-report measurement of interpretive bias when cognitive resources were relatively high. In line with predictions, both the CBM-I and cCBT groups showed a greater decrease in their tendency to rank negative explanations as likely to occur as compared with the control group. However, only the CBM-I group was better able to freely generate positive outcomes in the face of emotional ambiguity and had greater belief in that outcome as compared with controls (with the cCBT group not differing significantly from the control group).
Our second aim was to assess the effects of the interventions on attentional control and interpretive bias with and without load, and their influence as mediators. In terms of attentional control, CBM-I and cCBT resulted in increases in perceived attentional control as compared with the control group (with no significant differences between CBM-I and cCBT). However, changes in perceived attentional control only significantly mediated symptomatic improvement (relative to the control condition) in the cCBT and not in the CBM-I condition. This is consistent with the hypothesis that CBT works through enhancing intentional inhibitory control of threat-related information (e.g., DeRubeis et al., 2008). As a result of exposure and reflection regarding alternative viewpoints, cCBT imparts the skill, impaired in anxiety, of deploying central resources to processing benign objects of attention in favor of threatening contents (DeRubeis et al., 2008; Teasdale, Segal, & Williams, 1995). The present improvement in attentional control in the CBM-I condition suggests that, following CBM-I, individuals also feel better able to control their attention but that this may not be a key active ingredient of the intervention, clearly warranting further research.
Second, we assessed how well each intervention modified interpretive bias under conditions of presence versus absence of explicit cognitive load and whether this change mediated symptom improvement. The SST was used to directly test the prediction that when cognitive resources are depleted (the load condition), CBM-I might be more effective than cCBT in maintaining a positive cognitive bias. The results indicated that although both CBM-I and cCBT were effective at reducing negative bias under load as compared with the control group, CBM-I was significantly more effective than cCBT. This finding fits with prior studies and models that have claimed cognitive bias modification techniques could be more data driven and automated (e.g., Mathews & Mackintosh, 2000) and that participants are not necessarily conscious of resultant changes (Hertel & Mathews, 2011). In accordance with the implicit production rule hypothesis (e.g., Hoppitt, Mathews, Yiend, & Mackintosh, 2010; Wilson, MacLeod, Mathews, & Rutherford, 2006), the present results suggest that selection of the benign option is favored following CBM even when mechanisms of cognitive control are taken up with other processing activities (Mathews & Mackintosh, 2000; Mathews et al., 2007). Interestingly, the degree of change in bias under the load (but not the no-load) condition predicted overall symptom improvement following both CBM-I and cCBT, relative to the control condition. Moreover, contrasts revealed that the magnitude of the load mediation effect tended to be greater than the no-load mediation effect for both the CBM-I and cCBT analyses. Overall, these findings are consistent with the notion that one active ingredient of both interventions is changing interpretive bias when cognitive resources are limited. However, we tentatively suggest that the greater change under load in the CBM-I condition than the cCBT condition suggests that CBM-I might be more effective in this respect.
The present study is not without its limitations. First, our sample is primarily Caucasian and relatively young (mean age = 22.7), and so our results may not be generalizable to the broader population. In order to definitively compare the efficacy of CBM-I versus cCBT, the results from this study would need to be replicated in a suitably powered later phase RCT, preferably with a clinical sample, and against other versions of cCBT. Importantly, however, the present population reflects the people who are likely to use low-intensity computerized interventions, for which diagnosis is not routine. Second, the e-couch website has not yet been formally evaluated, although an RCT is presently assessing its efficacy (Christensen et al., 2010). Third, the self-report nature of the measure of attentional control leaves open the possibility that, rather than improving actual attentional control, we have instead increased individual perception of, or optimism related to, attentional control. A replication of these effects with more objective measures of attentional control is therefore essential. Fourth, we relied on self-report symptom outcomes and did not include a clinician-administered or objective behavioral assessment of clinical change; future research should include more objective measures of symptoms. Fifth, there is some potential for demand effects in both treatment arms because these participants knew they were receiving an intervention (although the rationale behind CBM-I was not explained to them), whereas control participants knew they were not. Finally, we only assessed outcomes at pre- and postintervention. It would be important to assess how enduring these effects are, and also whether positive bias in the cCBT condition when tested under conditions of high cognitive load improves over time after the intervention. It is possible that after further real-life practice of making positive interpretations, cCBT might become as effective as CBM-I in this respect. Alternatively, it may be the case that any benefits accruing from the bias modification resulting from CBM-I will further accumulate with time.
From a therapeutic perspective, these findings have a number of implications. First, they provide a preliminary indication that CBM-I could be used as an alternative to cCBT in situations in which having a different tool might be beneficial. For example, CBM-I might be a more helpful option for those who either do not want to spend time engaging in thoughtful reflection of their own thinking styles or find this particularly difficult. Second, the results allow us to speculate that, at the more severe end of anxiety and depression, CBM-I and CBT-based interventions have the potential to work effectively side by side in a complementary fashion. Alongside working in a conscious, deliberate way on reversing negative thinking styles during CBT, CBM-I could be used to further aid the modification of cognitive bias at a more habitual level to assist transfer of positive bias to real-life situations when under stress or pressure. Combining the two interventions could therefore produce better outcomes than relying on either alone. Indeed, initial work using different CBM paradigms in the treatment of alcoholism suggests that a combination of CBT and CBM is significantly more effective at improving treatment outcome than CBT alone (Wiers, Eberl, Rinck, Becker, & Lindenmeyer, 2011) and is feasible in generalized anxiety disorder (Amir & Taylor, 2012a). Finally, like CBT, CBM-I involves the systematic exposure to potentially adverse and problematic circumstances, which in training have a consistently innocuous resolution. Although such repeated computer-based practice leaves little room for empathic reflection or for adapting to individual concerns as in CBT, the efficacy of CBM-I suggests that its format is advantageous in that feared situations no longer need to be actualized in practice for changes in cognitive bias and emotion to take place (Hertel & Mathews, 2011). Thus, CBM-I could be particularly effective for individuals initially unwilling to engage in exposure to their feared situations, and as such could be used prior to CBT. Engaging in CBT may be more beneficial for individuals who wish to better understand their thought processes and behavior and who particularly want or need to increase their ability to use effortful control over unhelpful thoughts and emotions. Interestingly, CBM also has the potential to encourage effortful control through the addition of explicit instructions (cf. Krebs, Hirsch, & Mathews, 2010), although exactly how this may impact on the presently understood mechanisms of action would require further investigation.
In summary, the present study has suggested that CBM-I represents a viable intervention that has broadly comparable therapeutic effects as another computer-assisted therapy, cCBT. The two approaches do not differ significantly in their ability to reduce symptoms of anxiety and depression or to increase perceived attentional control, and both were superior to a no-intervention comparison condition. Where the two active interventions do differ is in how well the effects of positive bias modification endure when generating outcomes of emotionally ambiguous scenarios, and under conditions of high cognitive load, with CBM-I showing superior performance. Furthermore, changes in attentional control significantly mediate symptom improvement in cCBT but not in CBM-I. We conclude that these two approaches could be used as alternative or complementary interventions to reduce anxiety.
Acknowledgments
Bundy Mackintosh is now at the Department of Psychology, University of Essex. Barnaby Dunn is now at the Mood Disorders Centre, University of Exeter.
This study was supported by Wellcome Trust Grant 083475 awarded to Laura Hoppitt and Bundy Mackintosh. Barnaby D. Dunn and the penultimate author's involvement was additionally supported by the Medical Research Council (U U1055.02.002.00001.01). We thank Lusia Stopa for providing the Ambiguous Social Situations Interpretation Questionnaire and Helen Standage for stimuli used in the Scrambled Sentences Test. We are grateful to Emily Drake for her help with the data collection and scoring. We are also thankful to Kathy Griffiths and Helen Christensen at the e-hub group at the Australian National University for kindly permitting use of the e-couch website in this study.
References
- American Psychiatric Association. (1994). Diagnostic and statistical manual of mental disorders (4th ed.). Washington, DC: Author. [Google Scholar]
- Amir N., Beard C., Taylor L. T., Klumpp H., Elias J., Burns M., & Chen X. (2009). Attention training in individuals with generalized social phobia: A randomized controlled trial. Journal of Consulting and Clinical Psychology, 77, 961–973. doi:10.1037/a0016685 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Amir N., Bomyea J., & Beard C. (2010). The effect of a single-session interpretation modification on attention bias in socially anxious individuals. Journal of Anxiety Disorders, 24, 178–182. doi:10.1016/j.janxdis.2009.10.005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Amir N., & Taylor C. T. (2012a). Combining computerized home-based treatments for generalized anxiety disorder: An attention modification program and cognitive behavioral therapy. Behavior Therapy, 43, 546–559. doi:10.1016/j.beth.2010.12.008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Amir N., & Taylor C. T. (2012b). Interpretation training in individuals with generalized social anxiety disorder: A randomized controlled trial. Journal of Consulting and Clinical Psychology, 80, 497–511. doi:10.1037/a0026928 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Andersson G., Carlbring P., Berger T., Almlov J., & Cuijpers P. (2009). What makes internet therapy work? Cognitive Behaviour Therapy, 38, 55–60. doi:10.1080/16506070902916400 [DOI] [PubMed] [Google Scholar]
- Baert S., De Raedt R., & Koster E. H. W. (2011). Modification of information processing biases in emotional disorders: Clinically relevant developments in experimental psychopathology. International Journal of Cognitive Therapy, 4, 205–219. doi:10.1521/ijct.2011.4.2.208 [Google Scholar]
- Bar-Haim Y. (2010). Research review: Attention bias modification (ABM): A novel treatment for anxiety disorders. The Journal of Child Psychology and Psychiatry, 51, 859–870. doi:10.1111/j.1469-7610.2010.02251.x [DOI] [PubMed] [Google Scholar]
- Bar-Haim Y., Lamy D., Pergamin L., Bakermans-Kranenburg M. J., & van IJzendoorn M. H. (2007). Threat-related attentional bias in anxious and nonanxious individuals: A meta-analytic study. Psychological Bulletin, 133, 1–24. doi:10.1037/0033-2909.133.1.1 [DOI] [PubMed] [Google Scholar]
- Beard C., & Amir N. (2008). A multi-session interpretation modification program: Changes in interpretation and social anxiety symptoms. Behaviour Research and Therapy, 46, 1135–1141. doi:10.1016/j.brat.2008.05.012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Beard C., Weisberg R. B., & Amir N. (2011). Combined cognitive bias modification treatment for social anxiety disorder: A pilot trial. Depression and Anxiety, 28, 981–988. doi:10.1002/da.20873 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Beck A. T., & Clark D. A. (1997). An information processing model of anxiety: Automatic and strategic processes. Behaviour Research and Therapy, 35, 49–59. [DOI] [PubMed] [Google Scholar]
- Beck A. T., Steer R. A., & Brown G. K. (1996). Beck Depression Inventory–II (BDI-II). Manual for the Beck Depression Inventory–II. San Antonio, TX: Psychological Corporation. [Google Scholar]
- Berger T., Caspar F., Richardson R., Kneubühler B., Sutter D., & Andersson G. (2011). Internet-based treatment of social phobia: A randomized controlled trial comparing unguided with two types of guided self-help. Behaviour Research and Therapy, 49, 158–169. doi:10.1016/j.brat.2010.12.007 [DOI] [PubMed] [Google Scholar]
- Bishop S., Duncan J., Brett M., & Lawrence A. D. (2004). Prefrontal cortical function and anxiety: Controlling attention to threat-related stimuli. Nature Neuroscience, 7, 184–188. doi:10.1038/nn1173 [DOI] [PubMed] [Google Scholar]
- Blackwell S. E., & Holmes E. A. (2010). Modifying interpretation and imagination in clinical depression: A single case series using cognitive bias modification. Applied Cognitive Psychology, 24, 338–350. doi:10.1002/acp.1680 [Google Scholar]
- Brosan L., Hoppitt L., Shelfer L., Sillence A., & Mackintosh B. (2011). Cognitive bias modification for attention and interpretation reduces trait and state anxiety in anxious patients referred to an out-patient service: Results from a pilot study. Journal of Behavior Therapy and Experimental Psychiatry, 42, 258–264. doi:10.1016/j.jbtep.2010.12.006 [DOI] [PubMed] [Google Scholar]
- Browning M., Holmes E. A., Murphy S. E., Goodwin G. M., & Harmer C. (2010). Lateral prefrontal cortex mediates the cognitive modification of attentional bias. Biological Psychiatry, 67, 919–925. doi:10.1016/j.biopsych.2009.10.031 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Calear A. L., Christensen H., Mackinnon A., Griffiths K. M., & O'Kearney R. (2009). The YouthMood Project: A cluster randomized controlled trial of an online cognitive behavioral program with adolescents. Journal of Consulting and Clinical Psychology, 77, 1021–1032. doi:10.1037/a0017391 [DOI] [PubMed] [Google Scholar]
- Carlbring P., Nordgren L. B., Furmack T., & Andersson G. (2009). Long-term outcome of Internet-delivered cognitive–behavioural therapy for social phobia: A 30-month follow-up. Behaviour Research and Therapy, 47, 848–850. doi:10.1016/j.brat.2009.06.012 [DOI] [PubMed] [Google Scholar]
- Christensen H., Guastella A. J., Mackinnon A. J., Griffiths K. M., Eagleson C., Batterham P. J., & Hickie I. B. (2010). Protocol for a randomised controlled trial investigating the effectiveness of an online e-health application compared to attention placebo or sertraline in the treatment of generalised anxiety disorder. Trials, 11(48), 1–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Clark D. M., & McManus F. (2002). Information processing in social phobia. Biological Psychiatry, 51, 92–100. doi:10.1016/S0006-3223(01)01296-3 [DOI] [PubMed] [Google Scholar]
- Connor K. M., Davidson J. R. T., Churchill L. E., Sherwood A., Foa E., & Weisler R. H. (2000). Psychometric properties of the Social Phobia Inventory (SPIN): New self-rating scale. British Journal of Psychiatry, 176, 379–386. doi:10.1192/bjp.176.4.379 [DOI] [PubMed] [Google Scholar]
- Department of Health/Improving Access to Psychological Therapies. (2011). The IAPT data handbook: Guidance on recording and monitoring outcomes to support local evidence-based practice, Version 2.0.1. Retrieved from http://www.iapt.nhs.uk/silo/files/iapt-data-handbook-v2.pdf [Google Scholar]
- Derryberry D., & Reed M. A. (2002). Anxiety-related attentional biases and their regulation by attentional control. Journal of Abnormal Psychology, 111, 225–236. doi:10.1037/0021-843X.111.2.225 [DOI] [PubMed] [Google Scholar]
- DeRubeis R. J., Siegle G. R., & Hollon S. D. (2008). Cognitive therapy versus medication for depression: Treatment outcomes and neural mechanisms. Nature Reviews Neuroscience, 9, 788–796. doi:10.1038/nrn2345 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Eldar S., & Bar-Haim Y. (2010). Neural plasticity in response to attention training in anxiety. Psychological Medicine, 40, 667–677. doi:10.1017/S0033291709990766 [DOI] [PubMed] [Google Scholar]
- Fehm L., Pelissolo A., Furmark T., & Hans-Ulrich W. (2005). Size and burden of social phobia in Europe. European Neuropsychopharmacology, 15, 453–462. doi:10.1016/j.euroneuro.2005.04.002 [DOI] [PubMed] [Google Scholar]
- Hertel P. T., & Mathews A. (2011). Cognitive bias modification: Past perspectives, current findings, and future applications. Perspectives on Psychological Science, 6, 521–536. doi:10.1177/1745691611421205 [DOI] [PubMed] [Google Scholar]
- Hofmann S. G., & Smits J. A. J. (2008). Cognitive-behavioral therapy for adult anxiety disorders: A meta-analysis of randomized placebo-controlled trials. Journal of Clinical Psychiatry, 69, 621–632. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Holmes E. A., Mathews A., Dalgleish, & Mackintosh B. (2006). Positive interpretation training: Effects of mental imagery versus verbal training on positive mood. Behavior Therapy, 37, 237–247. doi:10.1016/j.beth.2006.02.002 [DOI] [PubMed] [Google Scholar]
- Hoppitt L., Mathews A., Yiend J., & Mackintosh B. (2010). Cognitive bias modification: The critical role of active training in modifying emotional responses. Behavior Therapy, 41, 73–81. doi:10.1016/j.beth.2009.01.002 [DOI] [PubMed] [Google Scholar]
- Jacobson N. S., & Truax P. (1991). Clinical significance: A statistical approach to defining meaningful change in psychotherapy research. Journal of Consulting and Clinical Psychology, 59, 12–19. doi:10.1037/0022-006X.59.1.12 [DOI] [PubMed] [Google Scholar]
- Kaltenthaler E., Brazier J., De Nigris E., Tumur I., Ferriter M., Beverley C., & Sutcliffe P. (2006). Computerised cognitive behaviour therapy for depression and anxiety update: A systematic review and economic evaluation. Health Technology Assessment, 10(33). [DOI] [PubMed] [Google Scholar]
- Kessler R. C., Berglund P., Demler O., Jin R., Merikangas K. R., & Walters E. E. (2005). Lifetime prevalence and age-of-onset distributions of DSM–IV disorders in the National Comorbidity Survey Replication. Archives of General Psychiatry, 62, 593–602. doi:10.1001/archpsyc.62.6.593 [DOI] [PubMed] [Google Scholar]
- Krebs G., Hirsch C. R., & Mathews A. (2010). The effect of attention modification with explicit vs. minimal instructions on worry. Behaviour Research and Therapy, 48, 251–256. doi:10.1016/j.brat.2009.10.009 [DOI] [PubMed] [Google Scholar]
- Kuyken W., Watkins E., Holden E., White K., Taylor R. S., Byford S., & Dalgleish T. (2010). How does mindfulness-based cognitive therapy work? Behaviour Research and Therapy, 48, 1105–1112. doi:10.1016/j.brat.2010.08.003 [DOI] [PubMed] [Google Scholar]
- Little R. J. A., & Rubin D. B. (1987). Statistical analysis with missing data. New York, NY: Wiley. [Google Scholar]
- Mathews A. (2006). Towards an experimental science of CBT. Behavior Therapy, 37, 314–318. doi:10.1016/j.beth.2006.02.004 [DOI] [PubMed] [Google Scholar]
- Mathews A., & Mackintosh B. (1998). A cognitive model of selective processing in anxiety. Cognitive Therapy and Research, 22, 539–560. doi:10.1023/A:1018738019346 [Google Scholar]
- Mathews A., & Mackintosh B. (2000). Induced emotional interpretation bias and anxiety. Journal of Abnormal Psychology, 109, 602–615. doi:10.1037/0021-843X.109.4.602 [PubMed] [Google Scholar]
- Mathews A., Ridgeway V., Cook E., & Yiend J. (2007). Inducing a benign interpretational bias reduces trait anxiety. Journal of Behaviour Therapy and Experimental Psychiatry, 38, 225–236. doi:10.1016/j.jbtep.2006.10.011 [DOI] [PubMed] [Google Scholar]
- Mobini S., Reynolds S., & Mackintosh B. (2012). Clinical implications of cognitive bias modification for interpretive biases in social anxiety: An integrative literature review. Cognitive Therapy and Research. doi:10.1007/s10608-012-9445-8 [Google Scholar]
- Murphy R., Hirsch C. R., Mathews A., Smith K., & Clark D. M. (2007). Facilitating a benign interpretation bias in a highly socially anxious population. Behaviour Research and Therapy, 45, 1517–1529. doi:10.1016/j.brat.2007.01.007 [DOI] [PubMed] [Google Scholar]
- Nordgreen T., Havik O. E., Öst L. G., Furmark T., Carlbring P., & Andersson G. (2012). Outcome predictors in guided and unguided self-help for social anxiety disorder. Behaviour Research and Therapy, 50, 13–21. doi:10.1016/j.brat.2011.10.009 [DOI] [PubMed] [Google Scholar]
- Preacher K. J., & Hayes A. F. (2008). Asymptotic and resampling strategies for assessing and comparing indirect effects in multiple mediator models. Behavior Research Methods, 40, 879–891. doi:10.3758/BRM.40.3.879 [DOI] [PubMed] [Google Scholar]
- Proudfoot J., Ryden C., Everitt B., Shapiro D. A., Goldberg D., Mann A., & Gray J. A. (2004). Clinical efficacy of computerised cognitive-behavioural therapy for anxiety and depression in primary care: Randomised controlled trial. The British Journal of Psychiatry, 185, 46–54. doi:10.1192/bjp.185.1.46 [DOI] [PubMed] [Google Scholar]
- Salemink E., van den Hout M., & Kindt M. (2009). Effects of positive interpretive bias modification in highly anxious individuals. Journal of Anxiety Disorders, 23, 676–683. doi:10.1016/j.janxdis.2009.02.006 [DOI] [PubMed] [Google Scholar]
- Schmidt N. B., Richey J. A., Buckner J. D., & Timpano K. R. (2009). Attention training for generalized social anxiety disorder. Journal of Abnormal Psychology, 118, 5–14. doi:10.1037/a0013643 [DOI] [PubMed] [Google Scholar]
- Schneider W., Eschman A., & Zuccolotto A. (2002). E-Prime user's guide. Pittsburgh, PA: Psychology Software Tools. [Google Scholar]
- Schulz K. F., Altman D. G., Moher D., & the CONSORT Group. (2010). CONSORT 2010 statement: Updated guidelines for reporting parallel group randomised trials. PLoS Med, 7(3): e1000251. doi:10.1371/journal.pmed.1000251 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Spielberger C. D., Gorsuch R. L., Lushene R., Vagg P. R., & Jacobs G. A. (1983). Manual for the State–Trait Anxiety Inventory. Palo Alto, CA: Consulting Psychologists Press. [Google Scholar]
- Standage H., Ashwin C., & Fox E. (2010). Is manipulation of mood a critical component of cognitive bias modification procedures? Behaviour Research and Therapy, 48, 4–10. doi:10.1016/j.brat.2009.08.005 [DOI] [PubMed] [Google Scholar]
- Stopa L., & Clark D. M. (2000). Social phobia and interpretation of social events. Behaviour Research and Therapy, 38, 273–283. doi:10.1016/S0005-7967(99)00043-1 [DOI] [PubMed] [Google Scholar]
- Teasdale J. D., Segal Z., & Williams J. M. G. (1995). How does cognitive therapy prevent depressive relapse and why should attentional control (mindfulness) training help? Behaviour Research and Therapy, 33, 25–39. doi:10.1016/0005-7967(94)E0011–7 [DOI] [PubMed] [Google Scholar]
- Tobon J. I., Ouimet A. J., & Dozois D. J. A. (2011). Attentional bias in anxiety disorders following cognitive behavioral treatment. Journal of Cognitive Psychotherapy, 25, 114–129. doi:10.1891/0889-8391.25.2.114 [Google Scholar]
- Watkins E. R., & Moulds M. (2007). Revealing negative thinking in recovered major depression: A preliminary investigation. Behaviour Research and Therapy, 45, 3069–3076. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Watson D., & Friend R. (1969). Measurement of social-evaluative anxiety. Journal of Consulting and Clinical Psychology, 33, 448–457. doi:10.1037/h0027806 [DOI] [PubMed] [Google Scholar]
- Wenzlaff R. M. (1993). The mental control of depression: Psychological obstacles to emotional well-being. In Wegner D. M. & Pennebaker J. W. (Eds.), Handbook of mental control (pp. 239–257). Englewood Cliffs, NJ: Prentice Hall. [Google Scholar]
- Wenzlaff R. M., Rude S. S., Taylor C. J., Stultz C. H., & Sweatt R. A. (2001). Beneath the veil of thought suppression: Attentional bias and depression risk. Cognition & Emotion, 15, 435–452. [Google Scholar]
- Wiers R. W., Eberl C., Rinck M., Becker E. S., & Lindenmeyer J. (2011). Retraining automatic action tendencies changes alcoholic patients' approach bias for alcohol and improves treatment outcome. Psychological Science, 22, 490–497. doi:10.1177/0956797611400615 [DOI] [PubMed] [Google Scholar]
- Wilson E., MacLeod C., Mathews A., & Rutherford E. M. (2006). The causal role of interpretive bias in vulnerability to anxiety. Journal of Abnormal Psychology, 115, 103–111. [DOI] [PubMed] [Google Scholar]
- Wittchen H.-U., & Jacobi F. (2005). Size and burden of mental disorders in Europe—A critical review and appraisal of 27 studies. European Neuropsychopharmacology, 15, 357–376. doi:10.1016/j.euroneuro.2005.04.012 [DOI] [PubMed] [Google Scholar]