Abstract
Using data from a randomized, controlled feeding study, which aimed to recruit 88 participants (including 22 Hispanics and 22 African Americans), we examined strategies for recruiting individuals from underrepresented groups into research trials. Study eligibility criteria included participants who 1) were 18–45 years old; 2) had a body mass index (BMI) >18 < 24.9 or BMI > 28.0 <40.0; 3); had no preexisting health conditions; 4) were non-smoking; 5) had normal fasting blood glucose level (< 100 mg/dL); and 6) spoke English. Participants were recruited using two overarching methods: media-based strategies (flyers and posters, email announcements, announcements in local and campus newspapers, and the Internet) and in-person strategies (presentations in university classes and community events). Participants were enrolled March 2006–March 2009. We present the numbers of individuals requesting study information, completing pre-enrollment screening questionnaires, and enrolling in the study. A total of 1036 individuals requested study information, and 396 completed a pre-enrollment screening questionnaire; 90 enrolled in the study (22 Hispanics and 18 African Americans). Among enrolled participants, in-person recruitment strategies were reported by 39% of African Americans, 73% of Hispanics, and 30% of non-Hispanic Whites (P <0.001). In-person recruitment strategies were successful among Hispanics. Mass media recruitment strategies were successful among non-Hispanic Whites but enlisted relatively few Hispanic participants. Both strategies recruited nearly equal percentages of African Americans. These data suggest that different strategies are needed to effectively recruit racial/ethnic population subgroups into intervention studies.
Keywords: Patient recruitment, carbohydrate metabolism, Hispanic American, African American
INTRODUCTION
Racial/ethnic minority groups are underrepresented in research trials.[1;2] National Institutes of Health (NIH) study participant enrollment data show that in 2005, 10% of study participants were African American, and 8% were Hispanic.[3] In the same year, African Americans and Hispanics represented 12.8% and 14%, respectively, of the total U.S. population.[4] Data from 75,215 participants enrolled in a nonsurgical National Cancer Institute Clinic Trial Cooperative Group breast, colorectal, lung, and prostate cancer clinical trial from 2000–2002 provide further support for this claim; Compared to non-Hispanic whites, the odds of being enrolled if Hispanic or African American were 0.71 (0.68, 0.77) and 0.72 (0.68, 0.74), respectively. [5]
The underrepresentation of members of racial and ethnic minority groups can be attributed to many factors, including the historical low prioritization of these groups by research funding agencies. In 1993, the NIH passed the Revitalization Act, mandating the inclusion of women and racial/ethnically underrepresented groups into research studies, unless the researcher could justify exclusion.[6] However, Burchard and others note that since the passage of the Revitalization Act, little has changed with regard to the inclusion of underrepresented groups into research trials.[1] NIH minority enrollment data from 1995 to 2006 support this claim.[3]
Other factors that may explain underrepresentation include cultural misunderstandings that stem from researchers’ unfamiliarity with specific cultural/social norms, participants’ fears or mistrust of physicians and research based on prior deception or mistreatment, [7] inadequate access to medical care, and lack of awareness of available trials.[8] Individuals facing economic hardship may experience barriers related to lack of childcare or transportation or competing work-family obligations. Cultural and religious beliefs that emphasize non-intervention may discourage some individuals from enrolling in research studies.[8]
Nonetheless, research participation by individuals from underrepresented racial and ethnic groups is vital for several reasons. First, it increases generalizability: Study findings are less generalizable when a major proportion of a population is inadequately represented. Second, it broadens our understanding of genetic influences on disease: Research in population genetics has suggested great genetic variation throughout racial/ethnic subpopulations,[1] which may explain why disease outcomes vary across subpopulations with otherwise similar socio-economic characteristics and demographics. Third, it may improve access to health services for minority groups[2] and mitigate health disparities.[9]
Yancey et al. and others have identified a variety of strategies to recruit underrepresented groups into research studies. These include creating partnerships with key stakeholders and community organizations to disseminate information about a given research study,[9–11] training health care providers to deliver culturally relevant care and build patient trust,[11] integrating cultural components (relevant images and wording) into recruitment material (such as flyers, brochures, and personalized letters),[10] recruiting through family and friends, and conducting in-person recruitment.[10]
While strategies have been identified, few investigations have evaluated their success. As a result, the relative merits of specific recruitment approaches remain poorly understood. To examine the effectiveness of strategies for enlisting underrepresented individuals into cancer prevention trials, we used data from a Seattle-based randomized, controlled feeding study, Carbohydrates and Related Biomarkers (CARB). CARB aimed to recruit 88 participants and had a 50% minority recruitment goal. Our analysis contributes to the existing literature by assessing the effectiveness of strategies to recruit diverse groups into intervention studies. Given the vast amounts of time and research dollars dedicated to identifying and recruiting study participants, such information is critical to effective project planning and coordination.
METHODS
Overview
The overall goal of the CARB study is to understand the relationship between physiologic responses to specific dietary patterns and biological mechanisms related to carcinogenesis. The intervention is described elsewhere; in brief, participants received all meals and beverages for two 28-day feeding periods, completed blood draws and urine and feces collections, and completed questionnaires on appetite, depression, mood, and satiety. Participants were enrolled March 2006–March 2009.
Study eligibility criteria
CARB participants 1) were aged 18–45; 2) had a body mass index (BMI) >18 and < 24.9, or BMI > 28.0 and <40.0; 3) had no preexisting health conditions that would interfere with study procedures; 4) were non-smokers; 5) had a normal fasting blood glucose level (< 100 mg/dL); and 6) spoke English. Participants were ineligible if they took daily medications, used any type of recreational drug, drank alcohol more than four times each week, were pregnant or breastfeeding, or were allergic to/intolerant of any study foods.
Participants completed a screening questionnaire that assessed eligibility. In addition to medical history and other anthropometric and diet-related factors, the questionnaire asked about gender, race (Caucasian, African American, Asian/Pacific Islander, American Indian, multiple races, and other), and ethnicity (Hispanic yes/no). Potentially eligible participants were invited to attend a screening appointment to measure fasting glucose levels.
Enrollment targets
The study aimed to recruit 88 participants with 50% minority recruitment, including 22 African-Americans and 22 Hispanics; the remaining 44 participants could be any other race/ethnicity. In addition, there was block randomization on BMI such that half of the participants were normal weight (BMI >18 and < 24.9) and half were overweight or obese (BMI > 28.0 and <40.0). Individuals with borderline BMI (> 25 and < 27.9) were specifically not eligible because we wanted to achieve sufficient contrast between the two BMI groups with respect to study outcomes.
Setting
A convenience sample of participants was recruited from the greater Seattle area of Washington State. Some recruitment activities were undertaken at the University of Washington (UW), the state’s largest public university. In 2008, UW enrolled a student body of 38,415—including 1,193 (3.1%) African-American and 1,744 (4.5%) Hispanic students.[12]
Recruitment strategies
We used two overall recruitment approaches: in-person and media-based approaches. We developed several types of print materials for recruitment, including a multi-color poster (8-1/2 X 11), a multi-color tri-fold flyer, an 8-page booklet, and a study menu. We created multi-color and black-and-white announcements for newspapers and magazines, an email announcement, and a project website. These collateral contained information about the study’s purpose and requirements and participant eligibility criteria and incentives.
In-person recruitment: Presentations and community events
Two in-person recruitment strategies were undertaken to identify potential participants, primarily Hispanic and African-American participants. The first in-person strategy involved presentations in classrooms and at student groups at the UW. Project staff sought permission from professors and student group leaders to present in their classroom or student group. During a typical recruitment event, a project staff presented information about the study, including its purpose, the eligibility criteria, and the study procedures, and invited questions from potential respondents. A second in-person strategy involved staffing booths at community events. These events included Hispanic Sea Fair, Fiestas Patrias, and the Central Area Community Festival, among others. Wherever possible, Hispanic and African-American students and staff participated in recruitment, and we tried to match their ages and race/ethnicity to that of the target population. For both types of in-person strategies, potential participants were provided a study brochure and menu and were asked to provide their name and contact information (either a phone number or email address) for further project information.
Media-based recruitment: print ads, email, posters, and flyers
Several media-based strategies were used, including paid announcements in weekly city periodicals, campus newspapers and local magazines, and email announcements sent to university-based list-serves and community organizations serving Hispanics and African Americans. Project posters and flyers were displayed at libraries, community centers, various university campus locations, and local businesses. In addition to mainstream media channels, we also used media that targeted African Americans and Hispanics. In Western Washington, Colors Northwest magazine is dedicated to all communities of color and has an estimated monthly readership of 62,000. In limited cases, the study coordinator emailed former Fred Hutchinson Cancer Research Center (FHCRC) study participants (who had previously agreed to be contacted about future studies) inviting their participation.
Recruitment survey
Interested participants chose either to phone the project office to have the study information packet and screening questionnaire mailed to them or to download the same information from the study website. The questionnaire asked participants how they were recruited: 1) enrolled participant, 2) friend or relative, 3) flyer or poster, 4) letter or email, 5) newspaper, 6) newsletter, 7) radio, 8) television, 9) class or meeting, 10) public event or fair, 11) unknown, or 12) other.
Participants who met initial eligibility criteria (based on survey responses) were contacted by phone and asked to come to the Prevention Clinic at FHCRC, where they were administered informed consent and asked to provide a blood sample to check their blood glucose levels. Only those with normal blood glucose levels were eligible.
Statistical analysis
For the purposes of statistical analysis, we grouped individuals based on self-reported race and ethnicity classifications. African Americans were those who reported African-American race, irrespective of ethnicity. Hispanics were those who reported Hispanic ethnicity and any race (no participant reported Hispanic ethnicity and African-American race). All other individuals included non-Hispanic Whites (n = 194), Asians (n = 54), Native Hawaiian/Pacific Islanders (n = 5), American Indian/Alaskan natives (n = 3), and multiple or unknown races (n = 12). We limited observations to the African-American, Hispanic Americans, and non-Hispanic White groups.
We calculated the frequency of each reported recruitment method (word-of-mouth; flyer or poster; letter or email; newspaper or newsletter; Internet; community festival or class presentation; other; and unknown) across the three racial and ethnic groups (African American, Hispanic, and non-Hispanic White). To distinguish media and in-person recruitment strategies, we grouped flyer or poster, letter or email, newspaper or newsletter, and Internet into a “mass media” category, and word-of-mouth and community festivals and class presentations into an “in-person” category. Differences in reported frequencies across racial/ethnic groups were estimated using the Pearson chi-square test.
RESULTS
Screening and enrollment
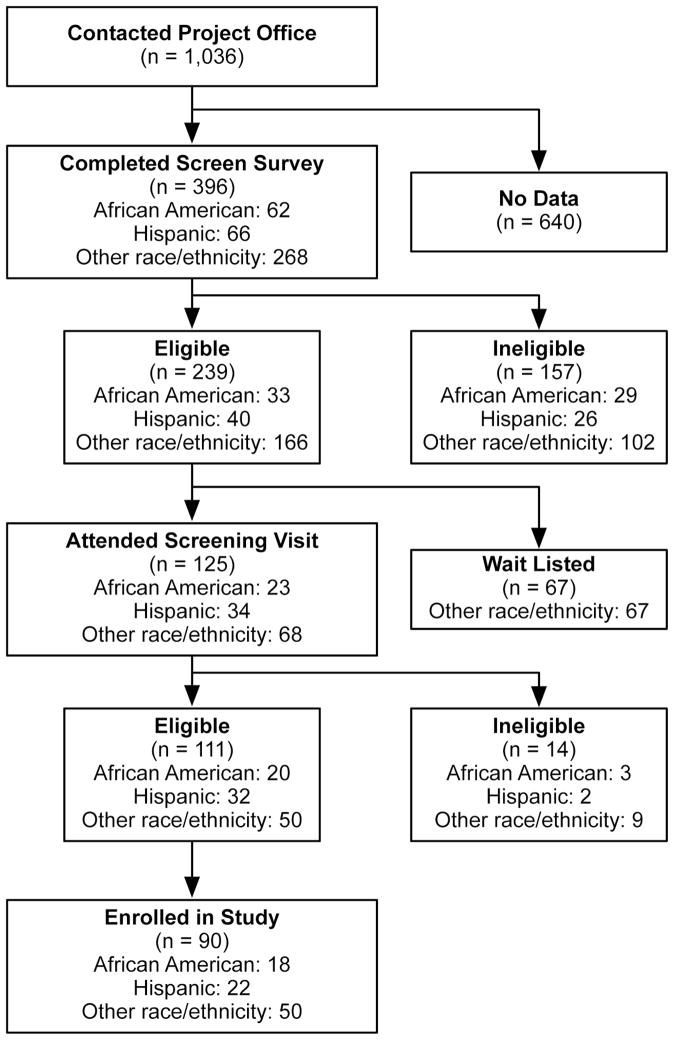
Figure 1 shows the number of individuals by racial and ethnic group (African Americans, Hispanics, and other races and ethnicities) who participated at several steps in the research study. A total of 1036 individuals (all races and ethnicities) requested study information, including 396 (231 females, 165 males) who completed a pre-enrollment screening questionnaire. Of those, 66 were Hispanic and 62 were African American. Half of those who completed the screening questionnaire did not meet the BMI criteria and were ineligible (51%); 22% were ineligible because of medical reasons (use of prescription medications, chronic or current illness); 18% for dietary reasons (allergies, intolerances, dislikes including vegan and vegetarian, no red meat, etc.). A total of 239 were eligible based on screening data (40 Hispanics and 33 African Americans); of these 172 were invited to attend a screening visit, and 67 were waitlisted (as target numbers in the “other races/ ethnicities” strata had been recruited, and subsequent enrollment would occur only if insufficient numbers were recruited in other strata). A total of 125 (74% of eligible) attended the screening visit (34 Hispanics and 23 African Americans), and 90 enrolled in the study (22 Hispanics and 18 African Americans).
Figure 1.
Diagram of Study Enrollment
Table 1 enumerates who participated at several steps in the research study, this time grouped as non-Hispanic White, African American, and Hispanic. Because the study endeavored to recruit equal numbers of males and females, we display the numbers of males and females within the race/ethnicity categories. Notably, among those eligible based on screening visit data, 90% of African Americans, 69% of Hispanics, and 85% of non-Hispanic Whites enrolled in the study. The study was considered a recruitment success, having reached the overall goal of 88 participants. The goal for Hispanic recruitment was reached (n = 22), and the goal for African Americans was nearly reached (n = 18; the goal was 22).
TABLE 1.
Number of screened, eligible, and enrolled study participants, by race and ethnicity
| Completed screening survey N = 396* | Eligible N = 239 N (%)† | Attended screening appointment N = 125‡ | Eligible N = 111 N (%)§ | Enrolled in study N = 90 N (%)= | |
|---|---|---|---|---|---|
| Non-Hispanic Whites | |||||
| Females | 115 | 41 (35.7) | 28 | 26 (92.8) | 22 (84.6) |
| Males | 80 | 38 (47.5) | 25 | 21 (84.0) | 18 (72.0) |
|
| |||||
| African Americans | |||||
|
| |||||
| Females | 40 | 19 (47.5) | 14 | 12 (85.7) | 10 (83.3) |
| Males | 22 | 14 (63.6) | 9 | 8 (88.9) | 8 (100.0) |
|
| |||||
| Hispanics | |||||
|
| |||||
| Females | 32 | 18 (56.3) | 15 | 14 (93.3) | 9 (64.3) |
| Males | 34 | 22 (64.7) | 19 | 18 (94.7) | 13 (72.2) |
Included 54 Asian, 5 Native Hawaiian/Pacific Islanders, 3 American Indian/ Alaskan Natives, and 11 who were multiple or unknown race.
Percentages based on number who completed screening survey; includes 20 “other races and ethnicities” and 67 non-Hispanic Whites who were wait-listed.
Includes 15 “other races and ethnicities.”
Percentages based on number who attended screening appointment; includes 12 “other races and ethnicities.”
Percentages based on number eligible based on screening appointment; includes 10
other races and ethnicities.”
Recruitment methods
We examined self-reported recruitment methods of individuals who completed the screening survey and those who enrolled in the study (Table 2). Overall, among individuals who completed the screening questionnaire, the most commonly reported sources of study information were newspaper or newsletter (29%), word-of-mouth (26%), and Internet (14%). Nevertheless, differences were observed across racial/ethnic groups, with Hispanics commonly reporting word of mouth (38%), community festivals and classes (23%), and newspaper or newsletter (17%); African Americans reporting newspaper or newsletter (34%), word-of-mouth (23%), or community festival or class (13%); and non-Hispanic Whites reporting newspaper or newsletter (34%), word-of-mouth (21%), and Internet (21%).
TABLE 2.
Recruitment methods among participants who completed screening survey and enrolled in study, by race and ethnicity
| Recruitment Methods | Completed screening survey N=396* | Enrolled in study N=90† | ||||||
|---|---|---|---|---|---|---|---|---|
| Non-Hispanic Whites N =195 | African American N =62 N | Hispanic N =66 N | P value ‡ | Non-Hispanic Whites N =40 | African American N =18 | Hispanic N =22 | P value ‡ | |
|
| ||||||||
| N (%) | (%) | (%) | N (%) | N (%) | N (%) | |||
| Media-based (overall) | 133 (68.2) | 36 (58.0) | 20 (30.3) | 0.02 | 25 (62.5) | 8 (44.4) | 5 (22.7) | NS |
| Flyer or poster | 25 (12.8) | 7 (11.3) | 4 (6.1) | 5 (12.5) | 2 (11.1) | 0 (0.0) | ||
| Letter or email | 2 (1.0) | 2 (3.2) | 1 (1.5) | 0 (0.0) | 0 (0.0) | 1 (4.8) | ||
| Newspapers or newsletter | 66 (33.9) | 22 (33.9) | 11 (16.7) | 15 (37.5) | 4 (16.7) | 2 (4.8) | ||
| Internet | 40 (20.5) | 5 (8.1) | 4 (6.1) | 5 (12.5) | 2 (11.1) | 2 (9.5) | ||
| In-person (overall) | 51 (26.2) | 22 (35.5) | 40 (60.6) | <0.0001 | 12 (30.0) | 7 (38.9) | 16 (72.7) | 0.004 |
| Word-of-mouth | 41 (21.0) | 14 (22.6) | 25 (37.8) | 9 (22.5) | 2 (11.1) | 10 (47.6) | ||
| Consented participant in prior study | 6 (3.1) | 0 (0) | 0 (0) | 3 (7.5) | 0 (0) | 0 (0) | ||
| Community festivals or presentation in classes / student organizations | 4 (2.1) | 8 (12.9) | 15 (22.7) | 0 (0.0) | 5 (27.8) | 6 (28.6) | ||
| Other or unknown § | 11 (5.6) | 4 (6.5) | 6 (9.1) | 3 (7.5) | 3 (16.7) | 1 (4.8) | ||
Included 54 Asian, 5 Native Hawaiian/Pacific Islanders, 3 American Indian/Alaskan Natives and 11 who were multiple or unknown race.
Included 6 Asians, 2 Native Hawaiian/Pacific Islander, 1 American Indian/Alaska Natives, and 1 of unknown race.
Based on chi-square test
Includes TV/radio
When we examined recruitment methods among those who successfully enrolled in the study, we observed important differences by race and ethnicity. Having heard of the study by word-of-mouth was reported by nearly half of Hispanics but only 23% and 11% of non-Hispanic Whites and African Americans, respectively. Flyers and posters were reported as the primary recruitment method by more than 10% of African Americans and non-Hispanic Whites, but by no Hispanics. The proportion of respondents recruited by newspaper or newsletter (38% of non-Hispanic Whites, less than one-quarter of African-Americans, and less than 5% of Hispanics) also varied by race and ethnicity.
DISCUSSION
Studying recruitment into a controlled cancer prevention feeding trial, our findings suggest certain strategies more commonly reported across racial/ethnic groups. Media-based strategies successfully recruited most non-Hispanic Whites, while in-person strategies recruited 73% of the Hispanics; both strategies recruited nearly equal percentages of African Americans. These data suggest that different strategies are needed to effectively recruit racial/ethnic population subgroups into intervention studies. As previously noted, representative inclusion of such groups can broaden generalizability of findings and potentially lessen the disproportionate burden of certain diseases. Understanding and employing effective strategies to identify and enlist members of population subgroups into research trials can minimize time and associated costs of study recruitment and can lead to more effective project planning.
Our study employed a variety of creative recruitment strategies. Furthermore, several Hispanic and African-American students and staff assisted with the recruitment, generally matching the age and race/ethnicity of the target population. As a result, they were aware of cultural norms and fears that can impede study participation, a factor noted by Stark and others as key to successful recruitment of underrepresented populations.[8;13] However, the extent to which this factor facilitated successful recruitment remains unclear.
We detected a relatively high motivation to participate among eligible individuals, although eligible Hispanics had a slightly lower rate of participation. Among participants who attended the screening visit and were eligible, relatively large proportions enrolled; 90% of African Americans, 69% of Hispanics, and 85% of non-Hispanic Whites.
We found that media-based strategies enlisted relatively few Hispanic participants; this is especially notable because all Hispanics in our study spoke English and presumably had just as much access to English-language media as did our non-Hispanic White and African-American participants. Media-based strategies successfully recruited a relatively higher proportion of African Americans, which may suggest broader readership of such media compared to Hispanics. Alternatively other factors not measured in this study (e.g., reluctance to participate in a “study” or work or childcare constraints [14]) may account for the differences observed in these groups.
The stringent eligibility criteria and extensive study procedures meant that the “hit rate” (the number who enrolled in the study divided by the number who initially contacted the project office) was relatively low (9%). Participants had to fall within a certain BMI range, excluding the moderately overweight. Also excluded were individuals taking daily medication. Finally, despite the incentive of free meals and $750, participants faced two inconveniences that may have been prohibitive: eating all weekday dinners at the Human Nutrition Laboratory during the feeding periods and providing multiple blood and urine samples. From a practical standpoint, a low hit rate directly increases recruitment costs; therefore, we uphold the value of targeting recruitment efforts to identify individuals most likely meeting eligibility requirements. Our observation that the majority of individuals who completed the screening questionnaire were ineligible due to BMI (51%), may underscore the challenge of targeting recruitment on BMI, or other criteria for which there is limited personal awareness of one’s scores.
Another notable finding is that across all racial and ethnic groups in our analysis, in-person strategies appeared more effective than media-based strategies at identifying individuals who were eligible and motivated to participate. Of 361 who completed the screening questionnaire, 40% reported having been recruited by an in-person strategy; this percentage rose to 55% among those who enrolled in the study (data not shown). In-person strategies allow potential study participants to assess their eligibility; thus those who did not meet criteria may have opted not to complete the screening questionnaire. In contrast, those who learned of the study through media strategies may have paid less attention to eligibility criteria and were more likely to complete the questionnaire (and later learn of their ineligibility). Alternatively, in-person recruitment may have served as an effective motivator for study participation among individuals who were eligible.
Among Hispanic participants in particular, individuals commonly reported joining the study after having spoken with a friend who had participated; this suggested that word-of-mouth information may have helped some individuals overcome cultural biases against participation. Since word-of-mouth was reported as the source of study information by 25% of those who completed the screening survey and 28% of those who enrolled in the study, efforts to promote “talking to your friends and family” about participating may have been useful.
Limitations
This study had several weaknesses. Recruitment activities were undertaken non-systematically, in that media advertisement (the least labor intensive) was attempted first; if that failed to recruit a sufficient number of Hispanic and African Americans, then we tried other activities. Also, the study criteria required that all participants, irrespective of race and ethnicity, spoke English, and we did not have reason to believe that English-language media would result in differential recruitment. Nevertheless, the non-systematic nature of recruitment means that the findings should be interpreted with caution.
It is possible that strategies successful in our region may be unsuccessful elsewhere and certain recruitment strategies we employed (such as in-person recruitment at community events and classrooms) may be unnecessary in regions with higher percentages of eligible participants. Moreover, our study required that participants come to the Human Nutrition Laboratory at the FHCRC, which in may have been prohibitively inconvenient; and no food was provided to non-participant family members. These factors suggest limited generalizability.
Nonetheless, while the data we present do not suggest a definitive strategy for recruiting underrepresented individuals into a highly controlled feeding study, this observational study can inform future recruitment efforts and may allow other investigators to plan certain recruitment strategies a priori.
CONCLUSION
In an observational study of recruitment of underrepresented groups into a feeding study, we found that in-person approaches were more effective than mass-media methods for recruiting Hispanics. Mass media and in-person strategies appeared to be similarly effective in recruiting African Americans. Recruitment efforts can be aided by clear information about the effectiveness of a given approach for a given group.
Acknowledgments
The authors would like to acknowledge Leonor Lara, Timnit Tekeste, Ruby Godina, and Norma Mariscal for their help in recruiting participants for the study. This project was funded by NCI U54 CA116847 (Transdisciplinary Research on Energetics and Cancer) and 5 U54 CA132381 (FHCRC) and 5 U54 CA 132383 (NMSU) both from the National Cancer Institute, Department of Health and Human Services.
ABBREVIATIONS
- NIH
National Institutes of Health
- CARB
Carbohydrates and Related Biomarkers
- BMI
Body Mass Index
- UW
University of Washington
- FHCRC
Fred Hutchinson Cancer Research Center
Footnotes
No conflicts of interest are reported.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
REFERENCE LIST
- 1.Burchard EG, Ziv E, Coyle N, Gomez SL, Tang H, Karter AJ, et al. The importance of race and ethnic background in biomedical research and clinical practice. The New England journal of medicine. 2003;348:1170–5. doi: 10.1056/NEJMsb025007. [DOI] [PubMed] [Google Scholar]
- 2.Bolen S, Tilburt J, Baffi C, Gary TL, Powe N, Howerton M, et al. Defining “success” in recruitment of underrepresented populations to cancer clinical trials: moving toward a more consistent approach. Cancer. 2006;106:1197–204. doi: 10.1002/cncr.21745. [DOI] [PubMed] [Google Scholar]
- 3.National Institutes of Health. Monitoring adherence to the NIH policy on the inclusion of women and minorities as subjects in clinical research. 2007 Available from: URL: http://orwh.od.nih.gov/inclusion/FinalAnnualReport2006.pdf.
- 4.US Census Bureau. Race and Hispanic Origin 2005. US Census Bureau; 2009. Available from: URL: http://www.census.gov/population/www/pop-profile/files/dynamic/RACEHO.pdf. [Google Scholar]
- 5.Murthy VH, Krumholz HM, Gross CP. Participation in cancer clinical trials: race-, sex-, and age-based disparities. JAMA. 2004;291:2720–6. doi: 10.1001/jama.291.22.2720. [DOI] [PubMed] [Google Scholar]
- 6.National Institutes of Health. NIH policy and Guidelines on the Inclusion of Women and Minorities as Subjects in Clinical Research-Amended. 2001 Oct; Available from: URL: http://grants.nih.gov/grants/funding/women_min/guidelines_amended_10_2001.htm.
- 7.Corbie-Smith G, Thomas SB, Williams MV, Moody-Ayers S. Attitudes and beliefs of African Americans toward participation in medical research. J Gen Intern Med. 1999;14:537–46. doi: 10.1046/j.1525-1497.1999.07048.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Daunt DJ. Ethnicity and recruitment rates in clinical research studies. Appl Nurs Res. 2003;16:189–95. doi: 10.1016/s0897-1897(03)00042-9. [DOI] [PubMed] [Google Scholar]
- 9.Sheppard VB, Cox LS, Kanamori MJ, Canar J, Rodriguez Y, Goodman M, et al. Brief report: if you build it, they will come: methods for recruiting Latinos into cancer research. J Gen Intern Med. 2005;20:444–7. doi: 10.1111/j.1525-1497.2005.0083.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Yancey AK, Ortega AN, Kumanyika SK. Effective recruitment and retention of minority research participants. Annu Rev Public Health. 2006;27:1–28. doi: 10.1146/annurev.publhealth.27.021405.102113. [DOI] [PubMed] [Google Scholar]
- 11.Hussain-Gambles M, Atkin K, Leese B. Why ethnic minority groups are under-represented in clinical trials: a review of the literature. Health Soc Care Community. 2004;12:382–8. doi: 10.1111/j.1365-2524.2004.00507.x. [DOI] [PubMed] [Google Scholar]
- 12.Washington U. University of Washington Admissions Factbook. 2007 Available from: URL: http://www.washington.edu/admin/factbook/taba5.pdf.
- 13.Stark N, Paskett E, Bell R, Cooper MR, Walker E, Wilson A, et al. Increasing participation of minorities in cancer clinical trials: summary of the “Moving Beyond the Barriers” Conference in North Carolina. J Natl Med Assoc. 2002;94:31–9. [PMC free article] [PubMed] [Google Scholar]
- 14.Brewster WR, Anton-Culver H, Ziogas A, Largent J, Howe S, Hubbell FA, et al. Recruitment strategies for cervical cancer prevention study. Gynecol Oncol. 2002;85:250–4. doi: 10.1006/gyno.2002.6592. [DOI] [PubMed] [Google Scholar]