Abstract
Intra-abdominal cysts and pseudocysts are rarely occurring lesions. Their incidence is reported to be 1 per 100 000-250 000 hospitalizations. The lesions’ rarity and their mostly asymptomatic development causes troubles in early recognition and treatment. The patients’ complaints are unspecific and mostly occur when the cysts are enlarged. Sometimes these entities may cause signs of peritoneal irritation and be the reason for immediate operation. It may happen in the event of cyst rupture, torsion, haemorrhages into the lesion or signs of compression of neighbouring structures. Many radiological methods are helpful in revealing intra-abdominal cysts. Unfortunately they cannot accurately distinguish the character of the lesion. The most common surgical procedure of treatment is excision during laparotomy. However, in some cases the laparoscopic approach can be equal to open surgery. This article presents a case of a young woman with a large intra-abdominal pseudocyst treated with laparoscopy.
Keywords: mesenteric cyst, mesenteric pseudocyst, laparoscopy
Introduction
Mesenteric cysts are very rare tumours occurring in the abdomen. Kurtz et al. report their incidence to be about 1/100 000 but other authors record lower frequency, about 1/250 000 hospital admissions [1, 2]. In children under the age of 10 years the lesions are more frequent, with incidence of 1 patient per 4000-34 000 hospital admissions [3, 4]. In adults mesenteric cysts occur especially in the fourth decade of life [5]. When considering the relationship between their incidence in a given gender, Kurtz et al. noted equal occurrence of the lesion among males and females [1]. A similar observation was made by Akinola et al., and in addition there was no difference according to race [6]. In contrast to those reports Maliszewski et al. found a higher incidence in females [7]. The studies on mesenteric cysts revealed that the majority of these lesions are benign and the incidence of malignancy is about 3% [1].
Mesenteric or retroperitoneal cysts do not cause specific symptoms [1, 8]. The occurrence of patient's symptoms depends on the size of the lesion. Small cysts often remain asymptomatic. Taking into account the above, we explain why the lesions are often diagnosed accidentally during abdominal ultrasonography, computed tomography (CT) or magnetic resonance imaging (MRI) scanning for other medical reasons [9]. Usually these patients complain of commonly encountered symptoms such as abdominal pain, distension, abdominal discomfort, nausea, vomiting, flatulence, constipation or diarrhoea [10]. In the event of rupture of the cyst, its infection, haemorrhage, torsion or ileus caused by compression, these patients will require immediate surgical intervention. Enlarged cysts may also compress the ureter or the bladder. In these situations a correct clinical and radio-logical diagnosis is difficult and rarely possible [1, 11].
Most often cysts are present in the small bowel mesentery (50-80%), next in the large bowel mesentery (15-30%) and also in the retroperitoneal space (7-20%) [12]. They contain fat, lymphatic vessels, blood vessels, scant muscle fibres and neural tissue. The cysts may develop when the mesenteric leaves fail to fuse and can also arise as a consequence of lymph node degeneration or malformation, as well as malposition or obstruction of lymphatic vessels [13]. According to Beahrs et al. there are four categories of mesenteric cysts: embryonic and developmental, traumatic and acquired, infective and degenerative and finally neoplastic [14].
A new classification of intra-abdominal cysts was proposed in 2000 by de Perrot et al. It is based on the histological identity of the internal epithelium and consists of 6 groups: 1) lymphatic cysts (simple cyst and lymphangioma), 2) mesothelial cysts (simple cyst, benign mesothelioma, malignant mesothelioma), 3) enteric cysts (including enteric duplication), 4) urogenital cysts, 5) mature cystic teratoma (dermoid cysts), 6) pseudocysts (infectious, traumatic and degenerative) [15].
The differential diagnosis, required prior to each operation, includes: peritoneal cyst, lymphangioma, endometriosis, ascites, pancreatic pseudocyst, haemangioma, cystic mesenteric panniculitis, hydatid cyst, cystic teratoma and urogenital cyst [5, 16–19].
In the literature the advised surgical procedure is excision of the tumour. The first surgeons who described the successful mesenteric cyst operation were Tillaux in 1880 and Pean, who did so 3 years later, but the operations were not total excisions [3, 20]. For many years the mesenteric cyst operation was performed with laparotomy. This changed in 1993, when Mackenzie performed laparoscopic excision [21].
This report presents a case of a young woman with a huge intra-abdominal cyst and unspecific symptoms, who was operated on with the laparoscopic approach.
Case report
A 25-year old woman was admitted to the Department of General and Thoracic Surgery with four-day history of pain in the upper quadrants of the abdomen. The pain was increasing over the few days prior to her admission and eventually became severe. Additionally, the patient complained of loss of appetite and nausea. She was not menstruating and pregnancy was excluded (β-HCG 2.39 mIU/ml). An increase of her abdominal girth was noticed over the year leading up to this admission, and was connected with obesity.
At the time of admission the patient's temperature was 37°C, her blood pressure was 120/70 mmHg and the heart rate was 100 beats per minute. Palpation revealed abdomen distension, mild tenderness and dullness was present upon percussion. Peristalsis was normal. There were no signs of peritoneum irritation in the physical examination.
Her blood tests revealed elevated inflammatory parameters (CRP 143.8 mg/l, and fibrinogen 762 mg/dl), but normal white blood cell count (5.62 th/µl) with decreased eosinophilic leucocytes (1.4%). Additionally the haemoglobin level was slightly decreased (11 g/dl). It was noted that the common neoplastic markers were all within the normal range (AFP: 0.9 ng/ml, CEA: 1.5 ng/ml, CA 15-3: 7.5 U/ml, Ca 19-9: 5.8 U/ml, CA 125: 19.2 U/ml).
Ultrasonography revealed an intra-abdominal hypoechogenic tumour located in the upper and middle part of the abdomen. Its size was 20 cm × 20 cm × 11 cm. Only the hypogastrium and both iliac fossae were free of the tumour. The lesion moulded and pushed neighbouring structures. US did not reveal any signs of cholelithiasis, free intra-abdominal fluid, or pathologies of the liver, pancreas or spleen. There were no signs of ileus or free gas in the abdomen in the X-ray.
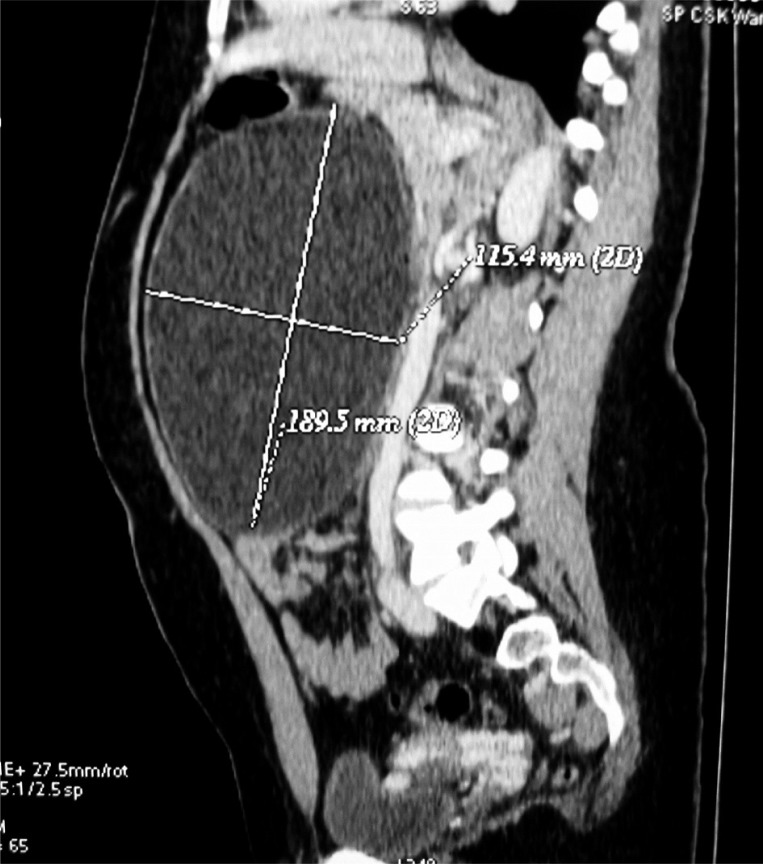
Computed tomography confirmed the presence of a huge cyst (18 cm × 20 cm × 11 cm), located symmetrically to the midline, between the navel and xiphoid process, with smooth walls and homogeneous contents (density – 22 Hu), well separated from the neighbouring vessels and organs (Figures 1, 2). It was not possible to assess the place of the cyst's origin. The lesion compressed the aorta and part of the portal and splenic veins, which were widened before compression. The impact on the left renal vein and distal part of the right ovarian vein (close to the vena cava) caused widening of both ovarian veins and the varices of the perimetrium. Other organs of the abdomen and pelvis were free of abnormalities.
Figure 1.
Computed tomography – reconstruction of the intra-abdominal cyst (front)
Figure 2.
Computed tomography – reconstruction of the intra-abdominal cyst (side view)
After puncture of the cyst we obtained a milky, muddy fluid with a pH of 7.0. It contained a high concentration of proteins, high density lipid (HDL), triglycerides and cholesterol, which might suggest its chylous nature. No cells suspicious for neoplastic transformation were found. The microbiological tests and cultures were also negative.
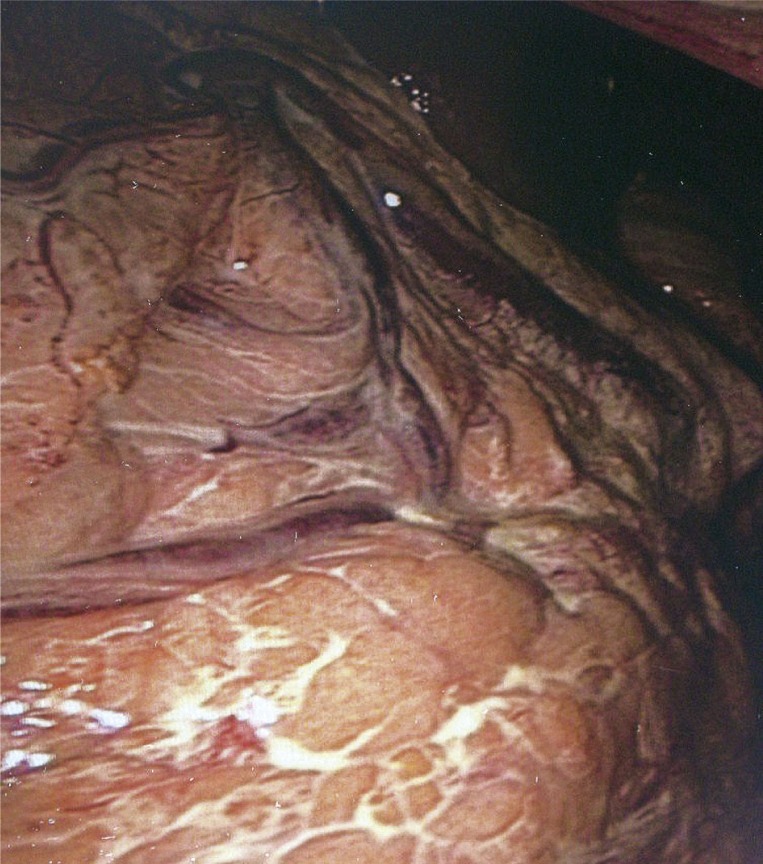
After taking a history and physical examination, blood tests, radiological investigations and diagnostic and partly therapeutic puncture of the cyst we proposed laparoscopy to the patient. We started the operation by placing the first 10 mm trocar under the navel and the huge cyst, which was covered with omentum containing widened vessels, became apparent (Figures 3, 4). The small bowel was covered and the transverse colon and stomach were displaced and compressed by the cyst. We gently shifted the omentum and transverse colon upward to the epigastrium to reveal the lesion. We grasped the wall, tapped it and sucked out approximately 2 l of milky-brown liquid. Total emptying of the cyst was not possible due to cheese-like formations. After decreasing the cyst size, we started to free its adhesions to the bowel, omentum and transverse colon. This did not prove problematic until we approached the root of the lesion. It was located in the mesentery of the first loop of the jejunum. The root of the cyst neighboured vessels of the jejunum and manipulation of the root was creating small haemorrhages. These haemorrhages were successfully coagulated. Due to the large size of the cyst its extraction through the trocar was difficult. That is why we decided to perform a minilaparotomy (about 3 cm long) in the navel area, and next we removed the cyst (Figure 5). The operation lasted 150 min.
Figure 3.
The omentum with widened vessels revealed during laparoscopic investigation
Figure 4.
Huge intra-abdominal cyst reaching downward to the infraumbilical regions of the peritoneal cavity (laparoscopic investigation)
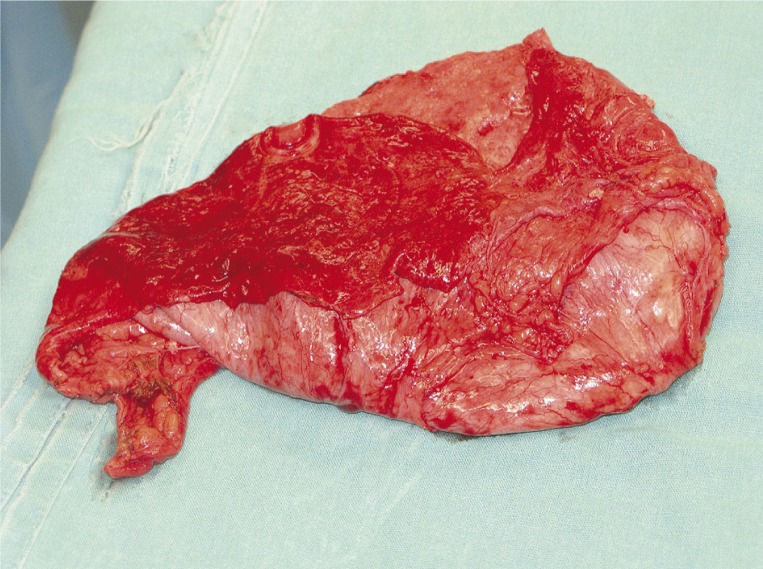
Figure 5.
The surgical specimen – completely excised pseudocyst
The patient's postoperative hospital stay was uneventful. She was discharged in good condition 7 days after the operation and stayed under our department's control. The follow-up clinical and US examination performed 6 months after her surgery did not reveal any abnormalities.
Microscopic examination of the excised cyst was performed 7 days after the operation. It demonstrated a pseudocyst with a wall containing connective tissue with inflammatory infiltrations and foci composed of histiocytic cells. On the internal surface the haemorrhages and yellowish deposits were visible.
Discussion
Large intra-abdominal cysts occur rarely. Only 15 cases of non-pancreatic pseudocyst have been noted in Japan up until 2003, and were more frequent in women [7, 22]. A few intra-abdominal cyst classifications are present in the literature, for example by Beahrs et al., Ros et al. and de Perrot et al. [14, 15, 23]. According to these classifications our patient suffered from non-pancreatic pseudocyst. Most such lesions are posttraumatic or infectious, but in our patient trauma of the abdomen was not apparent [23, 24]. In addition she categorically denied signs and symptoms of any possible abdominal inflammatory diseases, which may have been present previously. The above information allowed us to recognise the cyst as a degenerative pseudocyst [15]. In our case the cyst was filled with chylous fluid and cheese-like formations. Such contents are not unique in pseudocystic lesions, which may be serous, chylous, gelatinous, sanguineous or mixed [22, 25].
Patients with suspicion of mesenteric cyst can have the following imaging studies: ultrasonography, computed tomography or magnetic resonance. In the case of a large lesion it is often difficult to establish the origin [11]. Some authors emphasize the usefulness of ultrasonography, which may reveal details suggesting the character of the lesion. The occurrence of septa implies that the entity ought to be considered as a pseudocyst. Moreover, the existence of a thick-walled cyst merged with the muscle layer of the bowel may suggest enteric duplication. Internal echoes are present in mucous or infectious cysts [11]. In contrast, other investigators consider MRI to be more accurate in the imaging diagnostic process of locating the origin of the cyst [26]. In our case we performed ultrasonography and CT. Both methods gave us adequate knowledge about the size and topography of the cystic lesion, as well as helping to distinguish the content as liquid versus solid. Both modalities proved to be very useful. The CT scan additionally aided in assessment of the state of the pelvis. Unfortunately both methods failed to find the place of the lesion's origin. The majority of authors regard computed tomography as the modality of choice [7].
In the differential diagnosis it was very important to exclude the possibility that the cystic lesion was malignant, haemorrhagic, inflammatory, parasitic or infected by other microorganisms. We recognized a benign cyst, free of haemorrhage, infection and neoplastic process. We hoped that after reduction of the cyst size, easier preparation would be possible. We also wanted to lower the risk of intraoperative bleeding. A similar approach to this problem was noted in a previous article by Shamiyeh et al. [27].
Excision or enucleation is the procedure of choice in patients with a mesenteric cyst [28]. Sometimes additional resection of neighbouring organs is needed [11]. Other possible therapeutic procedures are drainage and marsupialisation of a cyst. Drainage is no longer advised due to the high rate of recurrence and infection [29, 30]. A similar situation is seen after marsupialisation, which would be performed in the event of an increased risk of wide adjacent organ resection [1, 31]. Knowing the benefits of laparoscopy such as lower postoperative pain, lower perioperative mortality, better cosmetic effect, faster recovery and in consequence shorter postoperative hospitalization, we decided to choose a laparoscopic approach [29, 30, 32]. However, sometimes the necessity of conversion to open surgery occurs. In our patient intra-abdominal preparation, exploration and freeing of adhesions was possible during the laparoscopic procedure. Unfortunately, due to the large size and only partial emptying of the lesion, it was not possible to remove the excised cyst through the trocar, and therefore a small minilaparotomy (about 3 cm) was needed.
We achieved a very good early clinical effect, and no signs or symptoms of recurrence or other intra-abdominal complications were observed at the 6-month follow-up.
There are few reports about mesenteric cysts in the literature. That is why it is hard to create a standardised method of treatment. Recent studies show that laparoscopy could be a good alternative to open surgery, but it should always be performed with caution.
References
- 1.Kurtz RJ, Heimann TM, Beck AR, Holt J. Mesenteric and retroperitoneal cysts. Ann Surg. 1986;203:109–12. doi: 10.1097/00000658-198601000-00017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Vaughn AM, Lees WM, Henry JW. Mesenteric cysts. Surgery. 1948;23:13–9. [PubMed] [Google Scholar]
- 3.Slocum MA. Chylous mesenteric cyst. Am J Surg. 1948;41:463–73. [Google Scholar]
- 4.Steinreich OS. The diagnosis of mesenteric cysts. Ann Surg. 1955;142:889–94. doi: 10.1097/00000658-195511000-00018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Pantanowitz L, Botero M. Giant mesenteric cyst: a case report and rewiev of the literature. The Internet Journal of Pathology. 2001;1:2. [Google Scholar]
- 6.Akinola O, Adejuyigbe O, Dare F. Mesenteric cysts in Nigerians. Centr Afr J Med. 1989;35:513–7. [PubMed] [Google Scholar]
- 7.Maliszewski D, Polec T, Jastrzębski T. Classic resection of mesenteric cyst – case report and literature rewiev. Pol J Surg. 2009;81:410–3. [Google Scholar]
- 8.Walker AR, Putman TC. Omental, mesenteric and retroperitoneal cysts: a clinical study of 33 new cases. Ann Surg. 1973;178:13–9. doi: 10.1097/00000658-197307000-00003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Duldulao MP, Thiruchitrambalam A, Kaul A. Mesenteric cyst: a rare cause of lower abdominal pain; 2008. Apr 7th Monday, Published Online: [Google Scholar]
- 10.Dulger C, Adali E, Avcu S, Kurdoglu Z. Large mesenteric cyst mimicking tuberculous ascites. Case Report Med 2010. 2010:725050. doi: 10.1155/2010/725050. Epub 2010 Jun 8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Chou YH, Tiu CM, Lui WY, Chang T. Mesenteric and omental cysts: an ultrasonographic and clinical study of 15 patients. Gastrointest Radiol. 1991;16:311–4. doi: 10.1007/BF01887376. [DOI] [PubMed] [Google Scholar]
- 12.Saviano MS, Fundaro S, Gelmini R, et al. Mesenteric cystic neoformations: report of two cases. Surgery Today. 1999;29:174–7. doi: 10.1007/BF02482245. [DOI] [PubMed] [Google Scholar]
- 13.Rauch RF. Retroperitoneal lymphangiom. Arch Surg. 1959;78:45–50. doi: 10.1001/archsurg.1959.04320010049008. [DOI] [PubMed] [Google Scholar]
- 14.Beahrs OM, Judd ES, Jr, Dockerty MD. Chylous cysts of the abdomen. Surg Clin North Am. 1950;30:1081–96. doi: 10.1016/s0039-6109(16)33090-0. [DOI] [PubMed] [Google Scholar]
- 15.de Perrot M, Bründler MA, Totsch M, et al. Mesenteric cysts. Toward less confusion? Dig Surg. 2000;17:323–8. doi: 10.1159/000018872. [DOI] [PubMed] [Google Scholar]
- 16.Johnson LA, Longacre TA, Wharton KA, Jeffrey RB. Multiple mesenteric lymphatic cysts: an unusual feature of mesenteric panniculitis (sclerosingmesenteritis) J Comp Assist Tomography. 1997;21:103–5. doi: 10.1097/00004728-199701000-00019. [DOI] [PubMed] [Google Scholar]
- 17.Rathnaraj S, Aggarwal S, Verhese M. Giant mesenteric hemangioma. Indian J Gastroenterol. 1995;14:113. [PubMed] [Google Scholar]
- 18.Takiff H, Calabria R, Yin L, Stabile BE. Mesenteric cyst anad intra-abdominal cystic hemangiomas. Arch Surg. 1985;120:1266–9. doi: 10.1001/archsurg.1985.01390350048010. [DOI] [PubMed] [Google Scholar]
- 19.Clement PB. Tumors of the peritoneum. In: Fletcher CDM, editor. Diagnostic histopathology of tumors. Vol. 1. 2nd ed. Vol. 15. London: Churchil Livingstone; 2000. pp. 839–64. [Google Scholar]
- 20.Tillaux PJ. Cyste du mesentere un homme: ablation par la gastromie. Revue de Therapeutiques Medico-Chirurgicale Paris. 1880;40:479. [Google Scholar]
- 21.Mackenzie DJ, Shapiro SJ, Gordon LA, Ress R. Laparoscopic excision of a mesenteric cyst. J Laparoendosc Surg. 1993;3:295–9. doi: 10.1089/lps.1993.3.295. [DOI] [PubMed] [Google Scholar]
- 22.Iida T, Suenaga M, Takeuchi Y, et al. Mesenteric pseudocyst of sigmoid colon. J Gastroenterol. 2003;38:1081–5. doi: 10.1007/s00535-003-1200-1. [DOI] [PubMed] [Google Scholar]
- 23.Ros PR, Olmsted WW, Moser PR, Jr, et al. Mesenteric and omental cysts: histologic classification with imaging correlation. Radiology. 1987;164:327–32. doi: 10.1148/radiology.164.2.3299483. [DOI] [PubMed] [Google Scholar]
- 24.Stoupis C, Ros PR, Abbitt PL, et al. Bubbles in the belly: imaging of cystic mesenteric or omental masses. Radiographics. 1994;14:729–37. doi: 10.1148/radiographics.14.4.7938764. [DOI] [PubMed] [Google Scholar]
- 25.Cizginer S, Tatli S, Snyder EL, et al. CT and MR imaging features of non-pancreatic pseudocyst of the mesentery. Eur J Gyn Med. 2009;6:49–51. [Google Scholar]
- 26.Miliaras S, Trygonis S, Papandoniou A, et al. Mesenteric cyst of the descending colon: report of a case. Acta Chir Belg. 2006;106:714–6. doi: 10.1080/00015458.2006.11679990. [DOI] [PubMed] [Google Scholar]
- 27.Shamiyeh A, Rieger R, Schrenk P, Wayand W. Role of laparoscopic surgery in treatment of mesenteric cysts. Surg Endosc. 1999;13:937–9. doi: 10.1007/s004649901140. [DOI] [PubMed] [Google Scholar]
- 28.Trompetas V, Varsamidakis N. Laparoscopic management of mesenteric cysts. Surg Endosc. 2003;17:2036. doi: 10.1007/s00464-002-9265-0. [DOI] [PubMed] [Google Scholar]
- 29.Vu JH, Thomas EL, Spencer DD. Laparoscopic management of mesenteric cyst. Am Surg. 1999;65:264–5. [PubMed] [Google Scholar]
- 30.Polat C, Ozacmak D, Yucel T, et al. Laparoscopic resection of giant mesenteric cyst. J Laparoendosc Adv Surg Tech A. 2000;10:337–9. doi: 10.1089/lap.2000.10.337. [DOI] [PubMed] [Google Scholar]
- 31.Alwan MH, Eid AS, Alsharif IM. Retroperitoneal and mesenteric cysts. Singapore Med J. 1999;40:160–4. [PubMed] [Google Scholar]
- 32.Al-Haifi MB, Abdulsamad AM, Juma T. Laparoscopic excision of mesenteric cyst: case report. Kuweit Medical Journal. 2007;39:167–9. [Google Scholar]