Abstract
Aim
The aim of the study was to compare the number of nodes dissected during laparoscopic and open radical cystoprostatectomy in men or anterior exenteration in women due to muscle invasive bladder urothelial cancer (IBC).
Material and methods
Fifty-one patients treated with laparoscopic radical cystectomy (LRC) and 63 with open radical cystectomy (ORC) were compared. The LRC group consisted of 47 pT2 tumours and 4 pT3, while the ORC group was composed of 27 pT2 tumours and 36 pT3. During ORC external, internal, common iliac and obturator lymph nodes were removed separately, but were added and analysed together for each side. Nodes dissected from one side during ORC were compared to en bloc dissected nodes in the LRC group.
Results
There were no complications associated with extended pelvic lymph node dissection during LRC or ORC. There were significant differences in the mean number of resected lymph nodes between LRC and ORC for pT2 tumours. The laparoscopic approach allowed about 8-9 more lymph nodes to be removed than open surgery in the pT2 group. In 15% of patients with pT2 disease treated with open radical cystectomy node metastases were observed. Active disease was detected in 18% of nodes resected laparoscopically due to pT2 disease. Fourty-seven percentage of patients with pT3 disease treated with open surgery were diagnosed as harbouring metastatic lymph nodes. The laparoscopic group with pT3 disease was too small to analyse.
Conclusions
We have found that laparoscopic radical cystectomy can be performed without any compromise in lymph node dissection. The technique of lymph node dissection (LND) during laparoscopic cystectomy (LRC) resulted in sufficient resected lymphatic tissue, especially in patients with bladder-confined tumours with a low volume of lymph nodes.
Keywords: laparoscopic radical cystectomy, open radical cystectomy, lymph node dissection
Introduction
Lymph node dissection (LND) is an important part of all oncological procedures. Properly and extensively performed LND can influence survival. Oncological results and good outcome of radical procedures are strongly dependent on the number of removed nodes [1–3]. The first experiences with laparoscopic cystectomies started in the early nineties [4–7]. In 2004 Finelli et al. presented the laparoscopic technique of extended lymph node dissection for muscle invasive bladder cancer [8]. This technique was improved, and now we can observe its rejuvenation as robot-assisted radical cystectomy [9].
Aim
The aim of the study was to compare the number of nodes dissected during laparoscopic and open radical cystoprostatectomy in men or anterior exenteration in women due to muscle invasive bladder urothelial cancer (TCC).
Material and methods
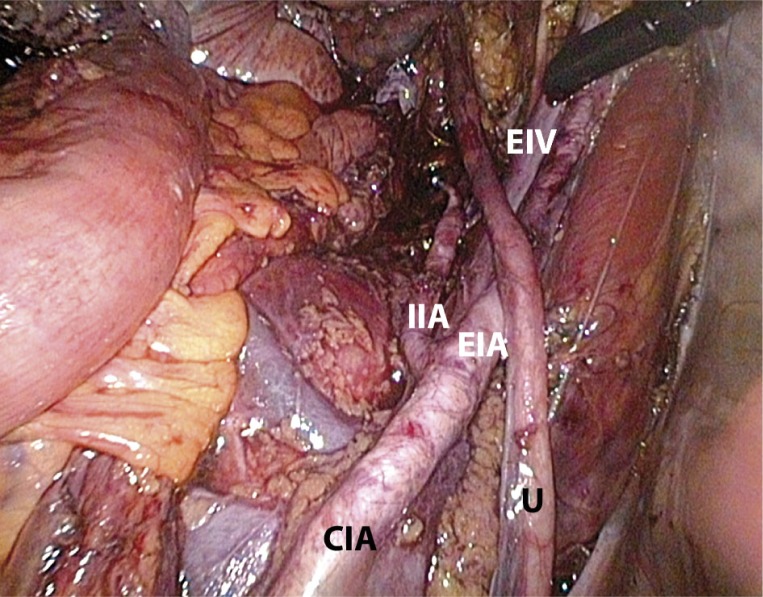
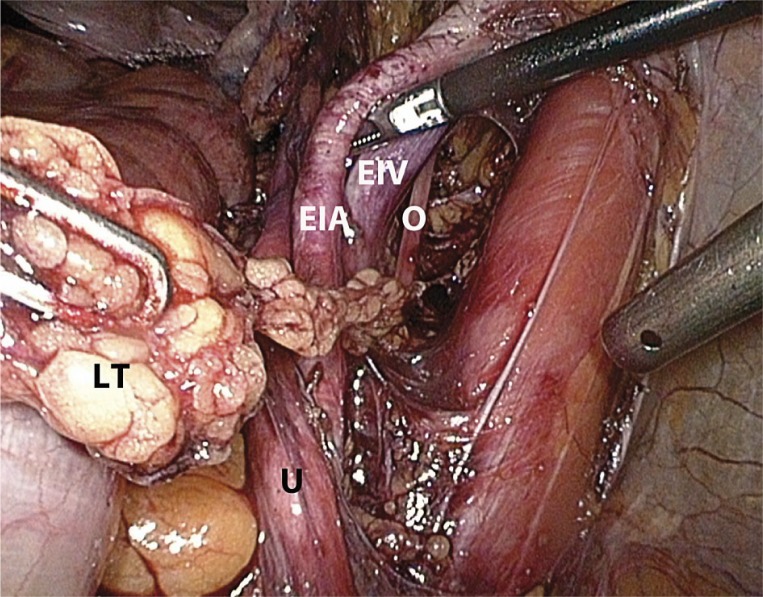
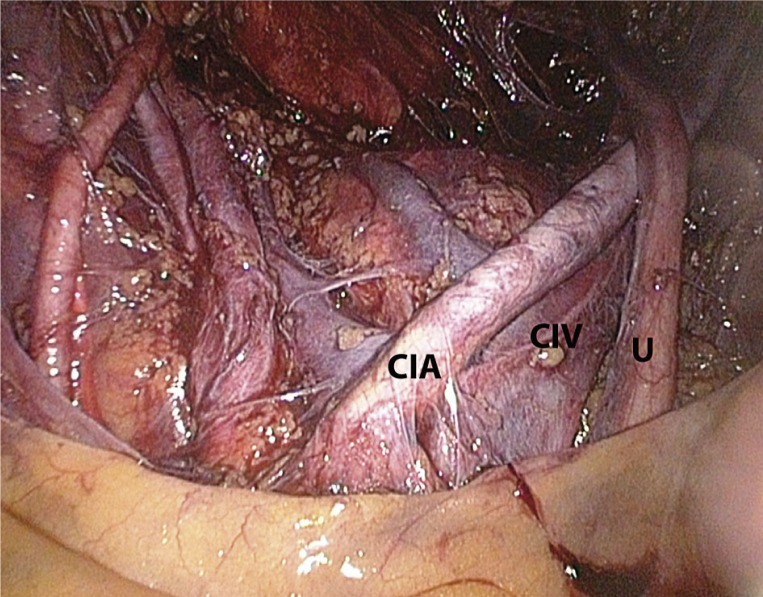
Numbers of lymph nodes dissected during laparoscopic and open radical cystectomies were compared. Material was collected between 2008 and 2010. Data used for analysis came from two oncological centres. In one centre patients underwent only open procedures; the second team usually operated laparoscopically. We compared 51 patients treated with laparoscopic radical cystectomy (LRC) and 63 with open radical cystectomy (ORC). The LRC group consisted of 47 pT2 tumours and 4 pT3, while the ORC group was composed of 27 pT2 tumours and 36 pT3 (Table I). The method of lymph node dissection (LND) during LRC differs from LND during ORC. Lymph node dissection during LRC was started after bladder excision. The procedure is performed with two 5 mm trocars and 3 trocars of 10 mm. 0° and 30° laparoscopes were used. Before lymph node dissection, the ureter was divided above the iliac vessels to the posterior bladder wall. Lymph node dissection was usually started from the right side (Figure 1). Dissection of all lymphatic tissue was along the external and internal iliac region and obturator fossa, and next along the common iliac region, with the aortic bifurcation and presacral region (Figure 1). The cranial margin of lymphadenectomy was always the region above the aorta and vena cava inferior bifurcation (Figure 1). During this part of the procedure two working bipolar graspers, monopolar scissors, a suction pump and a harmonic scalpel were used. External, internal, common iliac and obturator lymph nodes were dissected en bloc and analysed together. During the open procedure (ORC) external, internal, common iliac and obturator lymph nodes were removed separately, but were added and analysed together for each side. Nodes dissected from one side during ORC were together compared to en bloc dissected nodes in the laparoscopic (LRC) group. The key point of LND during LRC was dissection performed on the external sides of the both iliac vessels coming deeply into the obturator fossa (Figure 2). This manoeuvre can help to remove much more lymphatic tissue, which resulted in excellent surgical exposure of all pelvic vessels and nerves (Figure 3). Statistical analysis was performed for the group characterized with normal distribution. Mean numbers of removed nodes were compared; p > 0.05 was considered as important. Survival analysis was not done due to the short observation period.
Table I.
Number of resected lymph nodes during open radical cystectomy (ORC) and laparoscopic radical cystectomy (LRC) are presented as mean ± standard deviation (SD)
| Mean ± SD (left side) | Mean ± SD (right side) | % of patients with positive lymph nodes | |
|---|---|---|---|
| ORC, pT2 (n = 27) | 4.7 ±2.4 | 5.4 ±3.1 | 15 |
| ORC, pT3 (n = 36) | 6.1 ±3.9 | 6.2 ±3.5 | 47 |
| LRC, pT2 (n = 47) | 9.3 ±2.2 | 9.2 ±1.7 | 18 |
| LRC, pT3 (n = 4) | 7.3 ±1.5 | 10.5 ±1.5 | 0 |
p < 0.0001 for ORC, pT2 vs. LRC, pT2 (left side), p < 0.0001 for ORC, pT2 vs. LRC, pT2 (right side), p = 0.37 for LRC pT2 (right side) vs. LRC, pT2 (left side), p = 0.83 for ORC pT2 (right side) vs. ORC, pT2 (left side). LRC, pT3 was not analysed due to small patient group (n = 4)
Figure 1.
View of the right side of the pelvic wall. Vessels are prepared as during an open procedure
CIA – common iliac artery, IIA – internal iliac artery, EIA – external iliac artery, U – ureter, EIV – external iliac vein
Figure 2.
Preparation of the external side of iliac vessels enables one to obtain all lymphatic tissue (LT) from obturator fossa
EIA – external iliac artery, U – ureter, EIV – external iliac vein, O – obturator nerve
Figure 3.
Panoramic view of the pelvis after vessel skeletonization
CIA – common iliac artery, CIV – common iliac vein, U – ureter
Results
In all patients treated with LRC the procedure of extended lymph node dissection was performed without conversion to the standard open technique. There were no complications associated with extended pelvic lymph node dissection during LRC or ORC. Open and laparoscopic radical cystectomies were performed without any significant problems. There were significant differences in the mean number of resected lymph nodes between LRC and ORC for pT2 tumours, regardless of the analysed side (Table I). Generally in pT2 disease, a laparoscopic approach allowed about 8-9 more lymph nodes to be removed than open surgery. Only comparative analysis was done for pT3 disease due to the small number of patients (n = 4) in the LRC group. For this small group (pT3, LRC) the difference in number of resected lymph nodes between the left and right side was considerable: 7.3 ±1.5 vs. 10.5 ±1.5, respectively. In 15% of patients with pT2 disease treated with open radical cystectomy node metastases were observed. Active disease was detected in 18% of nodes resected laparoscopically due to pT2 disease. Fourty-seven percentage of patients with pT3 disease were diagnosed as harbouring metastatic lymph nodes, but these data came only from the open radical cystectomy group. The laparoscopic group for pT3 disease was too small to obtain any significant results (Table I). Lymphatic leak occurred in a minority of patients treated conservatively.
Discussion
Radical cystectomy with lymph node dissection is the reference treatment for invasive, high grade bladder cancer. Controlling cancer progression, rapid postoperative recovery and satisfactory quality of life are the 3 goals of oncological surgery [10]. Laparoscopic surgery has been shown to provide significant benefits in various urological procedures. Guillotreau et al. compared in a non-randomized prospective study 38 laparoscopic radical cystectomies to 30 open approaches. They showed that laparoscopic radical cystectomy is associated with decreased intraoperative and postoperative morbidity and mortality, lower opioid consumption and shorter hospital stay [11].
The aim of this study was to document the number of resected lymph nodes during radical cystoprostatectomy in men or anterior exenteration in women treated due to muscle invasive bladder urothelial cancer (TCC). The period of observation (2008-2010) was short, so long-term oncological results, such as overall survival and cancer-specific survival, could not be established. Pathological examination revealed that tumour characteristics and the number of excised lymph nodes were not the same for both groups of patients. Patients treated with the laparoscopic approach had lower staging (the majority of cancers were described as pT2), while in the open group approximately half of cancers were pT2 and half pT3. This can be explained with more careful patient selection for laparoscopic procedures. We did not include pT4 cancers, which are very often treated with open radical cystectomy, and so far are very rarely treated with a laparoscopic approach. It usually happens as a result of understaging. In fact, only patients with pT2 cancers can be compared in our study. We have found that the technique of lymph node dissection (LND) during laparoscopic cystectomy (LRC) resulted in a higher number of resected lymph nodes than during the open procedure. Two explanations can be given. The first is the technique of LND during the laparoscopic procedure. The lymphatic tissue is resected en bloc and descending from the iliac to obturator vessels with good vision of the resected area due to magnification (Figure 1). The second reason is that the 30° degree camera enables one to see the external part of iliac vessels and dissection of lymphatic tissue located in the obturator fossa can be performed from this side (Figure 2).
The laparoscopic procedure has to be performed without any compromise in tumour cure to avoid local recurrence and nerve damage [1–3, 8–11]. Haber et al. stated that LRC with extracorporeally constructed urinary diversion is a safe and effective operation for appropriate patients with bladder cancer. Perioperative and functional outcomes are comparable with open surgery. They emphasized that more focus on extended lymphadenectomy is necessary to routinely achieve higher node yields [12]. We have shown in this study that laparoscopic lymph node dissection can be performed even better than during an open procedure. Rassweiler suggested that laparoscopic radical cystectomy has to prove its superiority versus the open approach. Since this is still not clear, this procedure seems to be ideal for a randomized prospective study. This could take place in Europe, where the expertise of laparoscopic pelvic surgeons is equivalent to the expertise with open radical cystectomy [13]. Our study is not a randomized study, but tries to answer the basic question on oncological results. The presented surgical technique is an effective and considerably less invasive procedure than standard, open radical cystectomy. Laparoscopic radical cystectomy makes it possible to perform efficient and safe radical excision of the bladder with extended pelvic lymph node dissection, especially in cases of absence of extravesical cancer expansion (pT2) and no great volume of metastatic nodes. Using the harmonic scalpel and bipolar instruments for both surgeon and assistant facilitates extended pelvic lymph node dissection during laparoscopic radical cystectomy. Invasive bladder cancer can be treated with the laparoscopic technique, but despite the increasing number of centres adopting minimally invasive approaches for radical cystectomy, the long-term effectiveness of these techniques has not yet been proven [14].
References
- 1.Ścierski A, Roechte F. Laparoskopowe leczenie uchyłkowatości i schorzeń nowotworowych jelita grubego i odbytnicy. Videosurgery and other miniinvasive techniques. 2007;2:108–18. [Google Scholar]
- 2.Piątkowski J, Jackowski M. Laparoscopic colon resections – own experience report. Videosurgery and other miniinvasive techniques. 2009;4:135–7. [Google Scholar]
- 3.Belák J, Kudláč M, Šimon R. Video-assisted thoracoscopic surgery lobectomy – early experience. Videosurgery and other miniinvasive techniques. 2010;5:100–3. [Google Scholar]
- 4.Parra RO, Andrus CH, Jones JP, Boullier JA. Laparoscopic cystectomy: Initial report on a new treatment for the retained bladder. J Urol. 1992;148:1140–4. doi: 10.1016/s0022-5347(17)36843-x. [DOI] [PubMed] [Google Scholar]
- 5.Kozminski M, Partamian KO. Case report of laparoscopic ileal conduit. J Endourol. 1992;6:147–50. [Google Scholar]
- 6.Puppo P, Perachino M, Ricciotti G, et al. Laparoscopically assisted transvaginal radical cystectomy. Eur Urol. 1995;27:80–4. doi: 10.1159/000475130. [DOI] [PubMed] [Google Scholar]
- 7.Sanchez de Badajoz E, Gallego Perales JL, Reche Rosado A, et al. Laparoscopic cystectomy and ileal conduit: case report. J Endourol. 1995;9:59–62. doi: 10.1089/end.1995.9.59. [DOI] [PubMed] [Google Scholar]
- 8.Finelli A, Gill IS, Desai MM, et al. Laparoscopic extended pelvic lymphadenectomy for bladder cancer: technique and initial outcomes. J Urol. 2004;172:1809–12. doi: 10.1097/01.ju.0000140994.72981.20. [DOI] [PubMed] [Google Scholar]
- 9.Murphy DG, Challacombe BJ, Elhage O, et al. Robotic-assisted laparoscopic radical cystectomy with extracorporeal urinary diversion: initial experience. Eur Urol. 2008;54:570–80. doi: 10.1016/j.eururo.2008.04.011. [DOI] [PubMed] [Google Scholar]
- 10.Chlosta P, Drewa T, Dobruch , et al. Is pure laparoscopic radical cystectomy still an attractive solution for the treatment of muscle-invasive bladder cancer? Urol Int. 2010;85:291–5. doi: 10.1159/000310349. [DOI] [PubMed] [Google Scholar]
- 11.Guillotreau J, Gamz X, Mouzin M, et al. Radical cystectomy for bladder cancer: morbidity of laparoscopic versus open surgery. J Urol. 2009;181:554–9. doi: 10.1016/j.juro.2008.10.011. [DOI] [PubMed] [Google Scholar]
- 12.Haber GP, Crouzet S, Gill IS. Laparoscopic and robotic assisted radical cystectomy for bladder cancer: a critical analysis. Eur Urol. 2008;54:54–64. doi: 10.1016/j.eururo.2008.03.076. [DOI] [PubMed] [Google Scholar]
- 13.Rassweiler J. Laparoscopic radical cystectomy. Where are we really? Eur Urol. 2008;54:19–20. doi: 10.1016/j.eururo.2008.03.081. [DOI] [PubMed] [Google Scholar]
- 14.Chade DC, Laudone VP, Bochner BH, Parra RO. Oncological outcomes after radical cystectomy for bladder cancer: open versus minimally invasive approaches. J Urol. 2010;183:862–70. doi: 10.1016/j.juro.2009.11.019. [DOI] [PubMed] [Google Scholar]