Abstract
Aim
The authors evaluate the results of mini-invasive therapy in patients diagnosed with upside-down stomach.
Material and methods
From 1998 to 2008, a total of 27 patients diagnosed with upside-down stomach were surgically treated at the 1st Department of Surgery, University Hospital Olomouc. Before the operation, patients were examined endoscopically and a barium swallow was performed. In all 27 patients (100%), the operation was performed electively laparoscopically. The principle of the operation in all cases was reposition of the stomach into the abdominal cavity, resection of the hernial sac and hiatoplasty. In addition, in 15 patients (56%) with reflux symptoms or endoscopic findings of reflux oesophagitis, fundoplication in Nissen's modification was also performed. Fundopexy was indicated in 12 patients (44%).
Results
In all patients (100%), the operation was performed mini-invasively; conversion to an open procedure was never necessary. In 3 cases (11%), the left pleural cavity was opened during the operation; this was treated by introducing a chest drain. The operation mortality in the patient set was zero; morbidity was 11%. A year after the operation, patients were re-examined, and follow-up endoscopy and barium swallow were performed.
Conclusions
In all patients diagnosed with upside-down stomach, surgical treatment is indicated due to the risk of developing severe complications. Mini-invasive surgical therapy in the hands of an experienced surgeon is a safe procedure which offers patients all the benefits of mini-invasive therapy with promising short- and long-term results.
Keywords: upside-down stomach, mini-invasive surgical therapy, complications of therapy
Introduction
Upside-down stomach is an extreme form of paraoesophageal hiatal hernia where the entire stomach is dislocated into the thoracic cavity [1, 2]. Other abdominal organs may be present in the large hernial sac, most often the spleen or part of the large intestine [3]. In patients diagnosed with upside-down stomach, there is a high risk of developing severe complications, which may have a fatal outcome for the patient. Surgical treatment is the only curative therapy and at the same time prevents the development of complications.
Our work presents elective surgical laparoscopic therapy in a set of patients diagnosed with upside-down stomach. Over a period of 10 years, perioperative and postoperative results were retrospectively evaluated, and one year following the operation, long-term results of surgical therapy were evaluated.
Material and methods
From 1998 to 2008, a total of 27 patients diagnosed with upside-down stomach were surgically treated at the 1st Department of Surgery, University Hospital Olomouc. The patient set included only patients with a chronic course of the disease and where the entire stomach was localized in the mediastinum, based on the X-ray barium swallow. The patient set consisted of 16 males (60%) and 11 females (40%). The age of the patients ranged from 43 years to 77 years; the average age was 63 years. The reported duration of symptoms ranged from 7 months to 4 years; the average duration was 26 months. Dominating symptoms included postprandial chest pressure and breathlessness, which were described in 21 cases (77%). Typical symptoms of oesophageal reflux disease such as pyrosis, epigastric pain and regurgitation, along with the aforementioned symptoms, were present in 11 patients (40%).
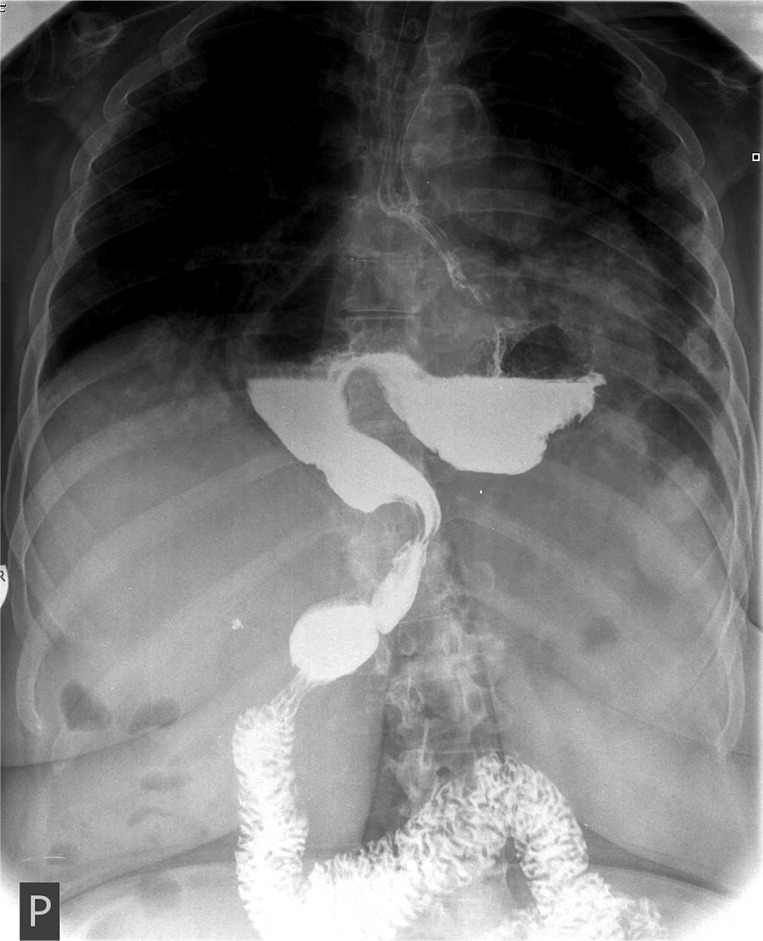
Diagnosis of the disease was based on endoscopic examination and barium swallow (Figure 1). To exclude a cardiac aetiology of chest pain, a cardiologic examination was performed.
Figure 1.
Barium swallow: image of upside-down stomach
Patients were operated on under general endotracheal anaesthesia. Patients were placed in a supine, anti-Trendelenburg position with abducted lower limbs. The operator stood between the lower limbs of the patient, first assistance to the left and second assistance to the right. Capnoperitoneum was introduced by way of a Veress needle; during the operation the pressure was set to 10 mmHg with a maximum of 12 mmHg. The operation was performed from five entries; the standard four 10 mm ports and one 5 mm port were used. A port introduced 10 cm below the xiphoid process was used to introduce the laparoscope with 30-degree optics. The operator used a 10 mm port left of the middle axial line, using the right hand to operate the dissector with monopolar coagulation, scissors and harmonic scalpel. The left hand worked with the Endoclinch in a 5 mm port, which was located below the right ribcage 5 cm from the linea alba. Another 10 mm port was introduced below the xiphoid process for the liver retractor to elevate the left liver lobe. The last 10 mm port was introduced below the left ribcage in the anterior axial line for the atraumatic Babcock. After introduction of the instruments, careful reposition of the stomach from the mediastinum back into the abdominal cavity was performed (Figure 2). Discision of the pars flaccida of the lesser omentum using the harmonic scalpel with interruption of the Leimer membrane followed. The next step included resection of the large hernial sac, which in some patients was difficult due to adherence to the parietal pleura. A nasogastric tube was always introduced into the stomach by the anaesthesiologist for better orientation of the oesophagus position and to prevent its injury. After isolation of the right and left crus of the diaphragm, the distal oesophagus was mobilized approximately 6 cm above the cardia (Figure 3). A Collis gastroplasty for short oesophagus was never performed; in all cases, it was possible to sufficiently mobilize the oesophagus below the diaphragm. The hiatoplasty was performed in all patients by individual Z stitches using the Endostitch with suture strength 0; on average 3 stitches were used. During construction of the hiatoplasty, a calibration probe of 42 F was introduced into the stomach. In 12 patients (44%) without reflux symptomatology, a fundopexy by three individual U stitches to the ventral peritoneum with suture strength 0 was performed. In 15 patients (56%) with reported reflux symptoms or with endoscopic findings of reflux oesophagitis a Nissen fundoplication was indicated. Construction of the fundoplication was done using four individual stitches with Endostitch 2-0 suture material. The last stitch was fixed to the distal oesophagus to prevent the telescopic phenomenon. Drainage was introduced individually in 13 patients (48%) based on blood loss during the operating procedure.
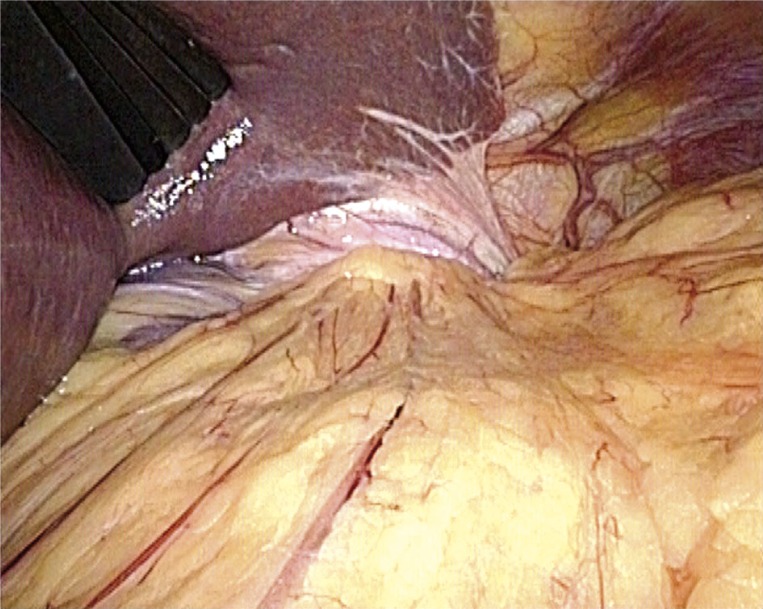
Figure 2.
Laparoscopic image of the abdominal cavity in patients with upside-down stomach
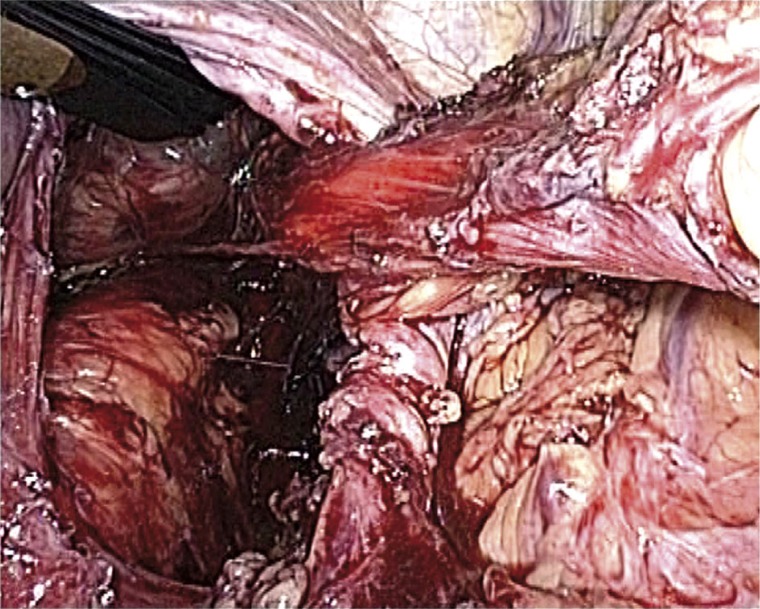
Figure 3.
Dissected diaphragmatic crus with the distal oesophagus prior to hiatoplasty and fundoplication
Results
In all 27 patients (100%) the operation was performed laparoscopically; conversion to a classical operation from laparotomy was never necessary. All the patients were operated on by surgeons with many years’ experience in mini-invasive surgical treatment of oesophageal reflux disease. The average operation time was 135 min; the range in operation time was 107 min to 182 min. In 3 cases (11%), during preparation of the stomach in the mediastinum, the left thoracic cavity was iatrogenically opened with development of pneumothorax, which was treated by chest drainage. No other severe perioperative complication was seen. Blood loss during the procedure ranged from 20 ml to 85 ml; the average was 51 ml. Drainage of the abdominal cavity was removed on the 2nd postoperative day at the latest; the secretion never surpassed 50 ml. Postoperative pain was treated by analgesic therapy. No serious complications were observed immediately following the operation. Mortality in our set of patients was zero, morbidity 11%. On average, patients were released from the surgery department into the care of their general practitioners 5.4 days postoperatively.
To evaluate long-term results of the surgical treatment, patients were invited for follow-up one year following the operation. A total of 21 patients (77%) attended the follow-up. Upon endoscopy and barium swallow, no patients showed recurrence of hiatal hernia or other pathology of the oesophagus or stomach. Subjectively, 16 patients (76%) evaluated their condition as very favourable, without presence of preoperative symptoms or other problems. In 2 patients (9%), minimal intermittent dysphagia without weight loss was present. Three patients (14%) reported postprandial dyspepsia; after administration of prokinetics their condition partially improved. In 1 case (4%), dislocation of the fundoplication into the mediastinum occurred 17 months following the operation, which was confirmed endoscopically and by barium swallow. Reoperation was performed in this patient laparoscopically; the fundoplication was repositioned back into the abdominal cavity with a new hiatoplasty.
Table I.
Results of surgical therapy in patients diagnosed with upside-down stomach
| Patients | (n = 27) |
| Sex (males: females) | 16 (60%): 11 (40%) |
| Mini-invasive procedure | 27 (100%) |
| Average operation time | 135 min |
| Morbidity | 3 (11%) – left-sided pneumothorax |
| Mortality | 0 |
| Reoperation | 1 (4%) – hernia recurrence |
Discussion
Upside-down stomach is an extreme form of hiatal hernia with organoaxial torsion of the stomach and its localization in the thoracic cavity; the hernial sac may also contain other abdominal organs [4]. The diagnosis of upside-down stomach was first described by Berti during autopsy in 1866, the first mention of surgical therapy in 1896 by Berg [5].
Major symptoms of the disease include postprandial chest discomfort, breathlessness, dysphagia, vomiting and anaemia [5]. Typical symptoms of oesophageal reflux disease may not be present [6]. In most cases, the course of the disease is chronic. It is manifested acutely in case of complications, which include strangulation, stomach obstruction, and acute bleeding from ulceration [3, 7]. Strangulation may even lead to stomach gangrene with subsequent perforation and the development of mediastinitis. In cases of obstruction, aspiration of stomach contents into the respiratory tract may occur [4, 8]. All of these cases are severe complications, which if not diagnosed in time and immediately treated may be life-threatening for the patient [4, 9].
Diagnosis is established based on X-ray examination (barium swallow) and endoscopic examination. The radiological image shows the entire stomach in the chest and the GE junction is in close proximity to the oesophageal hiatus [3].
All patients with upside-down stomach are indicated for surgical treatment [1, 3]. In patients with acute symptoms of the disease, an urgent surgical procedure is indicated; the type of procedure is modified based on perioperative findings [3, 7, 10]. In the remaining patients, an elective procedure is performed. Laparoscopic operation of paraoesophageal hernia was first described by Cushieri in 1992 [5]. Works published in the last decade regarding large paraoesophageal hernias clearly prefer the elective mini-invasive surgical approach [5, 8, 11, 12]. Works published in the last three years mention using the robotic system during operations of paraoesophageal hernias. Hartman reports on operations of upside-down stomach using the Da Vinci robotic system. Oesophageal preparation around the hiatus is considered to be the primary advantage; the cost of the procedure and educating time of the operation team are disadvantages [13]. Individual authors all agree on the principle of the surgical procedure (stomach reposition back into the abdominal cavity, resection of the hernia sac, hiatoplasty and fundoplication) [6, 11, 14, 15]. A short oesophagus may present a problem, and is defined as being at least 5 cm distant from the GE junction above the diaphragm. Swanstrom reports this finding in 14% of patients, and in 30% of these patients the oesophagus was mobilized laparoscopically without complications. In the remaining cases where the oesophagus could not be mobilized, a Collis gastroplasty was performed, where 20-70% of patients report its benefit in minimal incidence of postoperative dysphagia, acid reflux to the oesophagus and hernia recurrence [16]. The literature reports performance of a Collis gastroplasty for short oesophagus ranging from 0% (Ponsky) to 20% (Yano) [11, 12, 17]. In our set of patients, it was always possible to mobilize the distal oesophagus to a sufficient extent with placement of the GE junction below the diaphragm. Hiatoplasty is always part of the surgical procedure. Gantert prefers its performance without using a mesh, while Zehetner and Oelschlanger report a lower percentage of hernia recurrence after implantation of a mesh into the oesophageal hiatus [1, 14, 18]. In our set of patients, hiatoplasty was performed using individual cross stitches with Endostitch. Fundoplication is included in the procedure for low percentage of hernia recurrence and optimal prevention of acid reflux into the oesophagus in the postoperative period [19]. In over 90% of cases, fundoplication is performed in the Nissen modification [4, 6, 12, 20]. Other presented possibilities include Toupet or Dorr plasty [5, 8, 20]. Gastropexy is reported as another possibility to prevent hiatal hernia recurrence [7, 21]. In our set of patients, we preferred gastropexy in patients without reflux symptomatology with a promising endoscopic finding without reflux oesophagitis. Perioperative complications of mini-invasive therapy for upside-down stomach are comparable to the incidence of complications in patients operated for gastroesophageal reflux disease (bleeding, injury to the liver, spleen, stomach and oesophagus). Operation conversion is most often due to injury to the oesophagus, bleeding, or unclear operating field [1, 5, 12, 22]. When comparing with results of patients with other types of hiatal hernia, there is a higher incidence of injury to the pleura and opening of the thoracic cavity with development of pneumothorax during preparation of the large hernial sac [5, 23]. In terms of long-term results, the most common complication is hernia recurrence, which in large patient sets is reported as being up to 10% [11, 14, 21]. Reoperations are indicated for symptomatic hernia recurrence or return of reflux symptoms; Gantert and Andujar report a rate of 4% to 6% [11, 14].
Conclusions
Surgical treatment is the only curative therapy in patients with upside-down stomach. Operation is preferred even in patients with minimal symptoms of the disease to prevent the development of serious complications of the disease. An elective laparoscopic operation in the hands of an experienced surgeon is a safe procedure which brings the patient all the benefits of a minimally invasive procedure with a minimal number of perioperative and postoperative complications and promising long-term results [24–27].
References
- 1.Zehetner J, Lipham JC, Ayazi S, et al. A simplifield technique for intrathoracic stomach repair: laparoscopic fundoplication with Vicryl mesh and BioGlue crural reinforcement. Surg Endosc. 2010;24:675–9. doi: 10.1007/s00464-009-0662-5. [DOI] [PubMed] [Google Scholar]
- 2.Šerý Z, Králík J. Příspěvky k anatomii, histologii, fyziologii hiátové části bránice. Frenoesofageální membrána. Acta Palack Olomouc. 1956;11:257–61. [Google Scholar]
- 3.Cherukupalli C, Khaneja S, Bankulla P, Schein M. CT diagnosis of acute gastric volvulus. Die Surg. 2003;20:497–9. doi: 10.1159/000073536. [DOI] [PubMed] [Google Scholar]
- 4.Katkhouda N, Mavor E, Achanta K, et al. Laparoscopic repair of chronic intrathoracic gastric volvulus. Surgery. 2000;128:784–90. doi: 10.1067/msy.2000.108658. [DOI] [PubMed] [Google Scholar]
- 5.Yano F, Stadlhuber RJ, Tsuboi K, et al. Outcomes of surgical treatment of intrathoracic stomach. Dis Esophagus. 2009;22:284–8. doi: 10.1111/j.1442-2050.2008.00919.x. [DOI] [PubMed] [Google Scholar]
- 6.Krahenbuhl L, Schafer M, Farhadi, et al. Laparoscopic treatment of large paraesophageal hernia with totally intrathoracic stomach. J AM Coll Surg. 1998;187:231–7. doi: 10.1016/s1072-7515(98)00156-2. [DOI] [PubMed] [Google Scholar]
- 7.Ekelund M, Ribbe E, Willner J, Zilling T. Perfored peptic ulcer in paraesophageal hernia – a case report of a rare surgical emergency. BMC Surg. 2006;6:1. doi: 10.1186/1471-2482-6-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Athanasakis H, Tzortzinis A, Tsiaoussis J, et al. Laparoscopic repair of paraesophageal hernia. Endoscopy. 2001;33:590–4. doi: 10.1055/s-2001-15306. [DOI] [PubMed] [Google Scholar]
- 9.Duda M, Dlouhý M, Gryga A, et al. Langzeitige Beobachtung der webem paraosophagealen und gemischten Hiatushernien operierten Krankem. Erfahrungen mit mehr als 100 Operierten. Zent Bli Chir. 1991;116:729–36. [PubMed] [Google Scholar]
- 10.Rapant V. K. strategii chirurgického výkonu po druhotných komplikacích hiátových kýl. Acta Univ Olomouc Fac Med. 1961;23:253–56. [Google Scholar]
- 11.Andujar JJ, Papasavas PK, Birdas T, et al. Laparoscopic repair of large paraesophageal hernia is associated with low incidence of recurrence and reoperation. Surg Endosc. 2004;18:444–7. doi: 10.1007/s00464-003-8823-4. [DOI] [PubMed] [Google Scholar]
- 12.Wiechmann RJ, Ferguson MK, Naunheim KS, et al. Laparoscopic managment of giant paraesophageal herniation. Ann Thorac Surg. 2001;71:1080–6. doi: 10.1016/s0003-4975(00)01229-7. [DOI] [PubMed] [Google Scholar]
- 13.Hartmann J, Jacobi CA, Menenakos C, et al. Surgical treatment of gastroesophageal reflux disease and upside-dowm stomach using the Da Vinci robotic system. A prospective study. J Gastrointest Surg. 2008;12:504–9. doi: 10.1007/s11605-007-0400-z. [DOI] [PubMed] [Google Scholar]
- 14.Gantert WA, Patti MG, Arcerito M, et al. Laparoscopic repair of paraesophageal hiatal hernias. J Am Coll Surg. 1998;186:428–32. doi: 10.1016/s1072-7515(98)00061-1. [DOI] [PubMed] [Google Scholar]
- 15.Migaczewski M, Budzynski A, Rembiasz K, Choruz R. Quality of life of patients with gastroesophageal reflux disease after laparoscopic Nissen fundoplication. Videosurgery and Other Miniinvasive Techniques. 2008;3:119–25. [Google Scholar]
- 16.Swanstrom LL, Marcus DR, Gallowa GQ. Laparoscopic Collis gastroplasty is treatment of choise for the shortened esophagus. Am J Surg. 1996;171:477–81. doi: 10.1016/S0002-9610(96)00008-6. [DOI] [PubMed] [Google Scholar]
- 17.Ponsky J, Rosen M, Fanning A, Malm J. Anterior gastropexy may reduce reccurence rate after laparoscopic paraesophageal hernia repair. Surg Endosc. 2003;17:1036–41. doi: 10.1007/s00464-002-8765-2. [DOI] [PubMed] [Google Scholar]
- 18.Oelschlanger BK, Pellegrini CA, Hunter J, et al. Biologic prosthesis reduced recurrence after laparoscopic paraesophageal hernia repair: a multicenter, prospective, randomized trial. Ann Surg. 2006;244:481–90. doi: 10.1097/01.sla.0000237759.42831.03. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Neoral C, Král V. Laparoscopic fundoplication. Rozhl Chir. 1996;7:345–8. [PubMed] [Google Scholar]
- 20.Livingston CD, Jones HL, Jr, Askew RE, Jr, et al. Laparoscopic hiatal hernia repair in patients with poor esophageal motility or paraesophageal herniation. Am Surg. 2001;67:987–91. [PubMed] [Google Scholar]
- 21.Boushey RP, Moloo H, Burpee S, et al. Laparoscopic repair of paraesophageal hernias: a Canadian experience. Can J Surg. 2008;51:355–60. [PMC free article] [PubMed] [Google Scholar]
- 22.Rembiasz K, Bobrzynski A, Budzynski A, et al. Analysis of complications of laparoscopic management of abdominal disease related to extended indications. Videosurgery and Other Miniinvasive Techniques. 2010;5:53–9. [Google Scholar]
- 23.Hohmann U, Jahnichen A, Schramm H. The upside-down stomach. Laparoscopic treatment is possible. Zentrlbl Chir. 2001;125:394–7. [PubMed] [Google Scholar]
- 24.Stylopoulos N, Gazelle GS, Rattner DW. Paraesophageal hernias: operation or observation? Ann Surg. 2002;236:492–500. doi: 10.1097/00000658-200210000-00012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Edye MB, Canin-Endres J, Gattorno F, Salky BA. Durability of laparoscopic repair of large type III hiatal hernia: objective follow up reveals high recurrence rate. J Am Col Surg. 2000;190:553–60. doi: 10.1016/s1072-7515(00)00260-x. [DOI] [PubMed] [Google Scholar]
- 26.Mattar SG, Bowers SP, Galloway KD, et al. Long-term outcome of laparoscopic repair of paraesophageal hernia. Surg Endosc. 2002;16:745–9. doi: 10.1007/s00464-001-8194-7. [DOI] [PubMed] [Google Scholar]
- 27.Huntington TR. Short-term outcome of laparoscopic paraesophageal hernia repair. A case series of 58 consecutive patients. Surg Endosc. 1997;11:894–8. doi: 10.1007/s004649900481. [DOI] [PubMed] [Google Scholar]