Abstract
Laparoscopic adjustable gastric banding (LAGB) is one of the most frequently used minimally invasive and reversible procedures for the treatment of morbid obesity. Migration of the gastric band into the gastric lumen is a rare late complication of LAGB. Previous attempts at endoscopic removal of migrated bands have included the use of endoscopic scissors, laser ablation and argon plasma coagulation (APC). We report two cases of successful endoscopic management of gastric band migration using a gastric band cutter.
Keywords: band, cutter, laparoscopic adjustable gastric banding, migration
Introduction
Laparoscopic adjustable gastric banding (LAGB) is one of the most frequently used minimally invasive and reversible procedures for the treatment of morbid obesity [1, 2].The LAGB operation requires application of a silicon band containing an elastic balloon, that can be regulated by a port located subcutaneously, enabling injection and extraction of fluid. The band is applied around the upper part of the stomach and in this way two reservoirs are created – a smaller, superior one of 20 ml volume, and a significantly larger, inferior one [3, 4].
The main complications associated with LAGB include gastric perforation, migration of the band into the gastric lumen and band displacement, with resultant pouch enlargement [5]. Band migration is a long-term complication of unclear mechanism. Suggested aetiological factors of this complication are rejection reaction against the silicon band, external pressure applied to the gastric wall by an overfilled band, and internal pressure applied as a result of ingestion of excessively large food boluses [6]. Previous attempts at endoscopic removal of migrated bands have included the use of endoscopic scissors, laser ablation and argon plasma coagulation (APC) [7, 8].
Case reports
Case 1
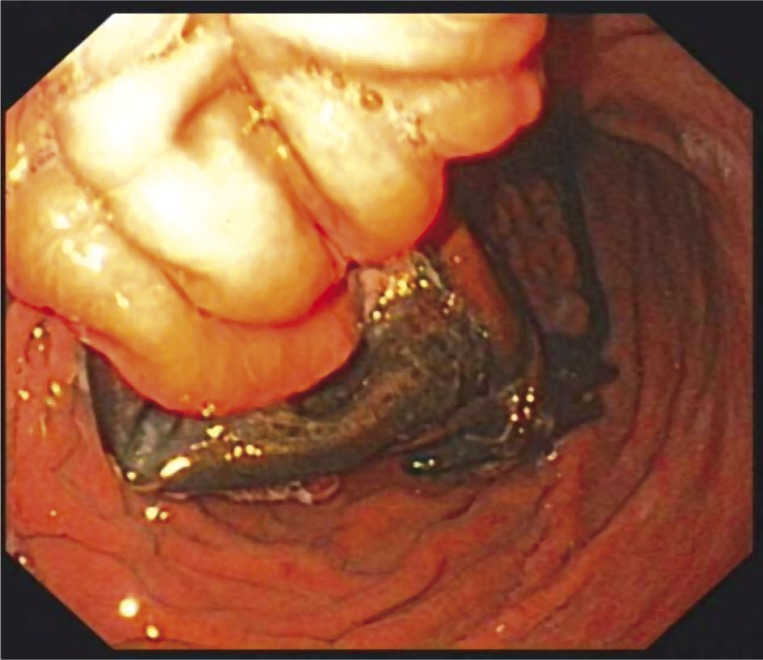
A 47-year-old woman with morbid obesity (body mass index [BMI] 45 kg/m2) underwent LAGB (gastric band manufacturer – Johnson&Johnson®) 3 years earlier and had effectively lost 18.5% of weight (BMI reduction of 8.02 kg/m2). The band filling was maximally 8 ml. The weight gain of 14.9% (BMI gain of 5.25 kg/m2) was observed 2 years after LAGB. Gastroscopy revealed almost total migration of the band into the gastric lumen and there was a tissue bridge that held the band to the gastric wall (Figure 1).
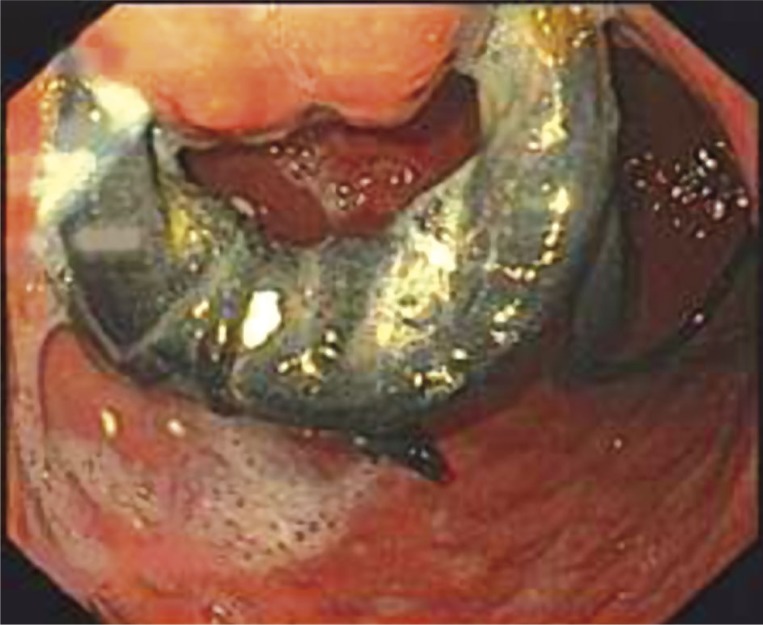
Figure 1.
Endoscopic view of migrated gastric band (patient 1)
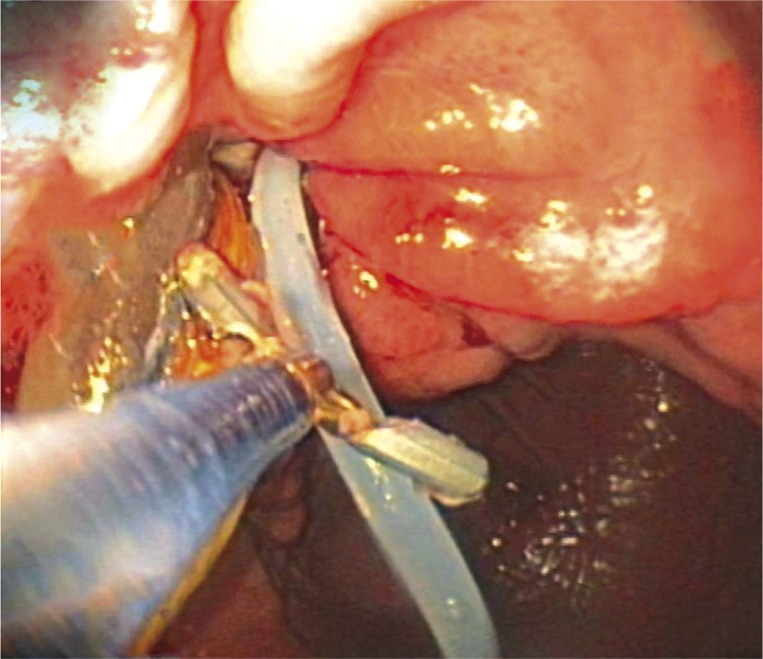
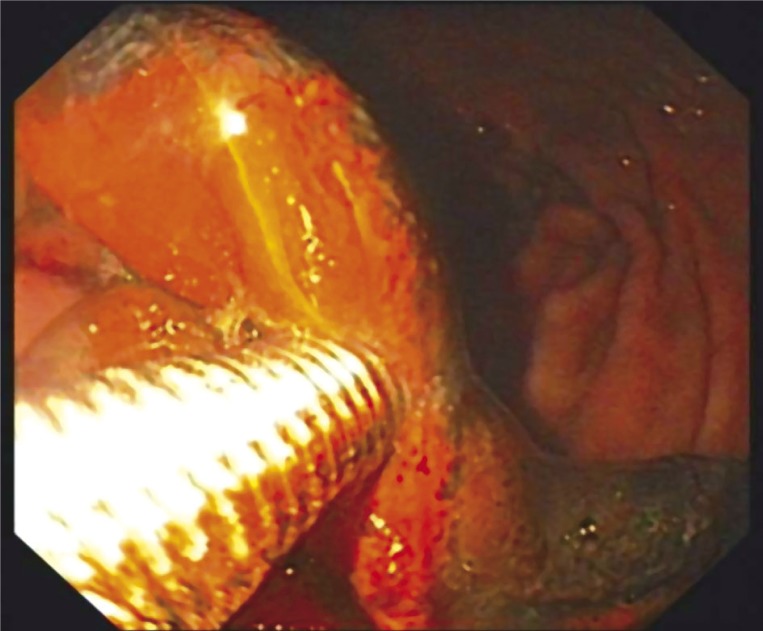
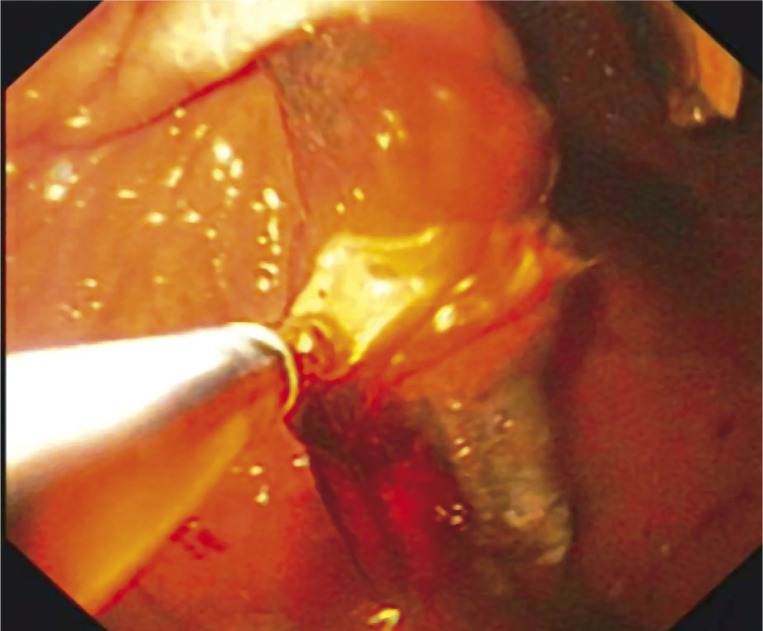
The port system was removed surgically with the patient under local anaesthesia. The connecting tube was cut and the rest of the tube was left inside the peritoneal cavity. It was pulled with forceps into the gastric lumen during endoscopy a few weeks later (Figure 2). Endoscopic extraction of the band was performed with surgical standby a few months after removal of the port system. The band was cut using an A.M.I.® Aigner Gastric Band Cutter and extracted with forceps (Figures 3, 4). There were no complications of the procedure and the patient was discharged the next day.
Figure 2.
Pulling of the connecting tube into the gastric lumen with forceps (patient 1)
Figure 3.
Cutting of the gastric band using the gastric band cutter (patient 1)
Figure 4.
Extraction of the gastric band with forceps (patient 1)
Case 2
A 34-year-old man with morbid obesity (body mass index 50 kg/m2) underwent LAGB (gastric band manufacturer – A.M.I.®) 5 years earlier and had successfully lost 20.68% of weight (BMI reduction of 9.54 kg/m2). The maximal band filling was 8 ml. Weight gain of 13.04% (BMI gain of 5.05 kg/m2) was observed during the last 6 months. There were no other symptoms. Gastroscopy and abdomen computed tomography (CT) imaging revealed almost total migration of the band into the gastric lumen (Figures 5, 6). The port system was removed surgically with the patient under local anaesthesia. The connecting tube was cut and the rest of the tube was left inside the peritoneal cavity. It slipped spontaneously into the stomach during the next 6 months. Endoscopic extraction of the band was performed with surgical standby a few months after removal of the port system. The band was cut using an A.M.I.® Aigner Gastric Band Cutter and extracted with a polypectomy snare (Figure 7). There were no complications of the procedure. The patient was discharged the next day.
Figure 5.
Endoscopic view of migrated gastric band (patient 2)
Figure 6.
Computed tomography scan showing migrated gastric band with connection tube inside the stomach (patient 2)
Figure 7.
The gastric band after successful endoscopic extraction from the stomach
Discussion
Between May 2005 and December 2010, 105 consecutive patients had an adjustable gastric band implanted in our institution. Intragastric band migration occurred in 2 patients (1.9%).
Migration of the gastric band into the gastric lumen is a rare late complication of LAGB. The main symptoms suggesting gastric band migration are weight gain and epigastric pain. Migrated gastric bands should be retrieved from the stomach to preclude obstruction. The risk of gastric perforation after an endoscopic procedure is higher in patients with partial penetration of the gastric band. Thus, in patients who are asymptomatic, according to the available literature data and our experience we suggest waiting for almost complete migration and endoscopic removal of the penetrated gastric band after previous surgical extraction of the port system [6].
References
- 1.Bobowicz M, Michalik M, Orłowski M, Frask A. Bariatric single incision laparoscopic surgery – review of initial experience. Videosurgery and Other Miniinvasive Techniques. 2011;6:48–52. [Google Scholar]
- 2.Kirshtein B, Lantsberg L, Mizrahi S, Avinoach E. Bariatric emergencies for non-bariatric surgeons: complications of laparoscopic gastric banding. Obes Surg. 2010;20:1468–78. doi: 10.1007/s11695-009-0059-5. [DOI] [PubMed] [Google Scholar]
- 3.Dadan J, Iwacewicz P, Razak Hady H. Quality of life evaluation after selected bariatric procedures using the Bariatric Analysis and Reporting Outcome System. Videosurgery and Other Miniinvasive Techniques. 2010;5:93–9. [Google Scholar]
- 4.Stanowski E, Paśnik K. Bariatric surgery – the current state of knowledge. Videosurgery and Other Miniinvasive Techniques. 2008;3:71–86. [Google Scholar]
- 5.Blanco Engert R, Gascon M, Weiner R, et al. Video-laparoscopic placement of adjustable gastric banding in the treatment of morbid obesity. Preliminary results after 407 interventions. Gastroenterol Hepatol. 2001;24:381–6. doi: 10.1016/s0210-5705(01)70205-1. [DOI] [PubMed] [Google Scholar]
- 6.Baldinger R, Mluench R, Steffen R, et al. Conservative management of intragastric migration of Swedish adjustable gastric band by endoscopic retrieval. Gastrointest Endosc. 2001;53:98–101. doi: 10.1067/mge.2001.111392. [DOI] [PubMed] [Google Scholar]
- 7.Lunde OC. Endoscopic laser therapy for band penetration of the gastric wall after gastric banding for morbid obesity. Endoscopy. 1991;23:100–1. doi: 10.1055/s-2007-1010625. [DOI] [PubMed] [Google Scholar]
- 8.Meyenberger C, Gubler C, Hengstler PM. Endoscopic management of a penetrated gastric band. Gastrointest Endosc. 2004;60:480–1. doi: 10.1016/s0016-5107(04)01736-5. [DOI] [PubMed] [Google Scholar]