Abstract
BACKGROUND
Despite numerous advances in resuscitation care in recent years, it remains unknown whether survival and neurological function after in-hospital cardiac arrest has improved over time.
METHODS
We identified all adults with an index in-hospital cardiac arrest at 374 hospitals in the Get With The Guidelines-Resuscitation registry between 2000 and 2009. Using multivariable regression, we examined temporal trends in risk-adjusted rates of survival to discharge. Additional analyses explored whether trends: (1) were due to improved survival during the acute resuscitation or post-resuscitation care and (2) occurred at the expense of greater neurological disability among survivors.
RESULTS
Among 84,625 hospitalized patients with cardiac arrest, 67,135 (79.3%) had an initial rhythm of asystole or pulseless electrical activity while 17,490 (20.7%) had ventricular fibrillation or pulseless ventricular tachycardia. The proportion of cardiac arrests due to asystole or pulseless electrical activity increased over time (P for trend <0.001). Risk-adjusted rates of survival to discharge in the overall cohort increased from 13.7% in 2000 to 22.4% in 2009 (adjusted rate-ratio per 1-year: 1.04, 95% CI [1.02–1.05]; P for trend <0.001). Survival improvement was similar in both rhythm groups and largely due to improved survival from the acute resuscitation (risk-adjusted rates: 42.7% in 2000, 54.1% in 2009; adjusted rate-ratio per 1-year: 1.03, 95% CI [1.02–1.04]; P for trend <0.001). Importantly, rates of neurological disability among survivors decreased over time (risk-adjusted rates: 32.9% in 2000, 28.1% in 2009; P for trend=0.02).
CONCLUSIONS
Both survival and neurological outcomes after in-hospital cardiac arrest have improved over the past decade.
INTRODUCTION
Advances in resuscitation care over the last decade have led to higher rates of survival for patients with out-of-hospital cardiac arrest.1–4 In the in-hospital setting, quality improvement efforts have included the use of routine mock codes, post-resuscitation debriefing, defibrillation by non-medical personnel, and participation in quality improvement registries, such as Get with the Guidelines–Resuscitation (GWTG-Resuscitation).5–9 Whether overall survival for patients with in-hospital cardiac arrest has improved with these efforts remains unknown.
To date, only one study has examined temporal trends in survival after in-hospital cardiac arrests. This study found no change in survival to discharge among hospitalized Medicare patients undergoing cardiopulmonary resuscitation (CPR) from 1992 through 2005.10 Although large and nationally representative, this study used administrative claims data and may have included patients without cardiac arrest (e.g., patients undergoing CPR for bradycardia) or excluded patients for whom a procedure code for CPR was not submitted. Moreover, information on the initial cardiac arrest rhythm, which has likely changed over time, was not available. This is important because advances in the management of acute myocardial infarction and heart failure may have led to a decline in the proportion of in-hospital cardiac arrests due to ventricular fibrillation (VF) and pulseless ventricular tachycardia (VT). Since these rhythms are associated with better survival, 9, 11, 12 it is possible that overall survival in that study did not change, even as rhythm-specific survival improved.
Therefore, we examined temporal trends in rates of survival to hospital discharge within a large, national quality improvement registry of in-hospital cardiac arrests. Because improved survival in these patients may occur at the expense of worsened neurological function, we also explored temporal trends in rates of neurological disability among survivors at discharge. Understanding how outcomes are changing over time in this population has important implications for improving resuscitation care at hospitals across the United States.
METHODS
Data Source and Study Population
Formerly known as the National Registry of Cardiopulmonary Resuscitation (NRCPR), GWTG-Resuscitation is a large, prospective, hospital-based, clinical registry of patients with in-hospital cardiac arrests in the U.S. The design of the registry has been previously described in detail.9 Briefly, all hospitalized patients with a confirmed cardiac arrest (defined as the absence of a palpable central pulse, apnea, and unresponsiveness), without Do-Not-Resuscitate (DNR) orders, and who received cardiopulmonary resuscitation are identified and enrolled by specially trained personnel. To ensure that all cases in a hospital are captured, multiple case finding approaches are used including centralized collection of cardiac arrest flow sheets, review of hospital page system logs, and routine checks of code carts, pharmacy tracer drug records, and hospital billing charges for use of resuscitation medications.13 The registry uses standardized Utstein-style definitions for defining clinical variables and outcomes.14, 15 Data completeness and accuracy is ensured by rigorous training and certification of hospital staff, use of standardized software with internal data checks and a periodic re-abstraction process.
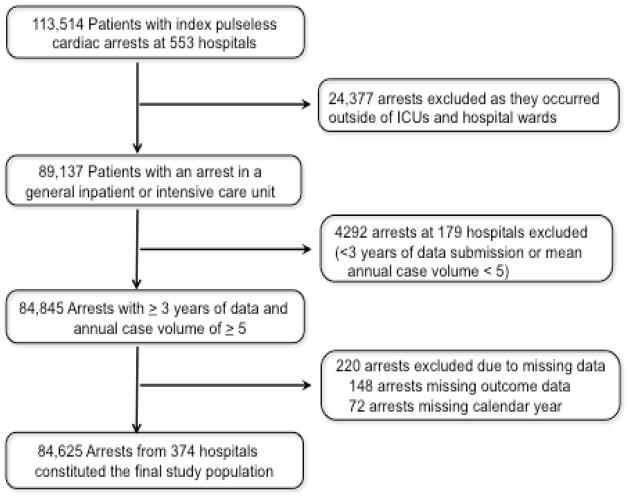
We identified 113,514 adults at 553 hospitals who were 18 years of age or older with an index cardiac arrest event between January 1, 2000 and November 19, 2009 (Figure 1). We restricted our sample to cardiac arrests occurring in an intensive care unit or inpatient ward and excluded 24,377 arrests from operating rooms, procedural suites or emergency departments, as this latter group represents distinct clinical circumstances and outcomes. As we were interested in examining trends in survival over time, we also excluded 4292 patients from 179 hospitals with fewer than 3 years of data submission or low case volumes (< 5 per year). Finally, we excluded patients missing information on survival (n=148) and calendar year (n=72). Our final sample comprised 84,625 patients from 374 hospitals (see eTable 1 for hospital characteristics).
Figure 1.
Study Cohort
Study Outcome
The primary outcome was survival to discharge. As survival from a VF or pulseless VT cardiac arrest differs from asystole or pulseless electrical activity (PEA),9, 11, 12 all analyses are reported for the overall cohort and separately by rhythm type. To better understand which specific phase of resuscitation care may have led to improvement in survival, we separately examined rates of acute resuscitation survival (defined as return of spontaneous circulation for at least 20 contiguous minutes at any time from the initial pulseless arrest) and post-resuscitation survival (defined as survival to hospital discharge among patients who survived the acute resuscitation). We also examined temporal trends in time to defibrillation in VF and pulseless VT patients.16
To confirm that any temporal trend in survival was clinically important, we also examined rates of neurological disability among survivors. This was assessed using previously developed cerebral performance category (CPC) scores.17 A CPC score of 1 denotes patients with mild to no neurological disability, 2 for moderate neurological disability, 3 for severe neurological disability, and 4 for coma or vegetative state. We examined temporal trends for significant (discharge CPC score of > 1) and severe neurological disability (discharge CPC score ≥2). 16, 18
Statistical Analyses
To evaluate changes in baseline characteristics by calendar year, we used the Mantel-Haenszel test of trend for categorical variables and linear regression for continuous variables. To assess whether survival to discharge has improved over time, multivariable regression models using generalized estimation equations (GEE) were constructed for the overall cohort and by rhythm type. These models account for clustering of patients within hospitals. Since survival exceeded 10%, we used Zou’s methodology to directly estimate rate-ratios instead of odds ratios by specifying a Poisson distribution and including a robust variance estimate in our models. 19, 20 Our independent variable, calendar year, was included as a categorical variable, with year 2000 as the reference year. We multiplied the adjusted rate-ratios for each year (2001 through 2009) with the observed survival rate for the reference year (2000) to obtain yearly risk-adjusted survival rates for the study period. These rates represent what the survival would be for each year if the patient case-mix were identical to the baseline year (i.e. 2000). We also evaluated calendar year as a continuous variable to obtain adjusted rate-ratios for year-over-year survival trends.
In our models, we adjusted for age, sex, race [white, black, other], co-morbidities (congestive heart failure; myocardial infarction; diabetes mellitus; renal, hepatic, or respiratory insufficiency; admission CPC score [neurological status pre-arrest]; baseline evidence of motor; cognitive, or functional deficits [CNS depression]; acute stroke; pneumonia; hypotension; arrhythmia; sepsis; trauma; metabolic or electrolyte abnormality; cancer), therapeutic interventions in place at the time of cardiac arrest (use of mechanical ventilation; anti-arrhythmic drugs; intravenous vasopressors; dialysis; pulmonary artery catheter, intra-aortic balloon pump), cardiac arrest characteristics (initial cardiac arrest rhythm; hospital location [ICU, monitored, non-monitored]; time [work hours: 7am–10:59pm vs. after hours: 11pm–6:59am] and day [weekday vs. weekend] of cardiac arrest; use of a hospital-wide cardiopulmonary arrest alert [i.e., “Code Blue”], amiodarone use during resuscitation, time to defibrillation [only for VF and VT arrests]) and select hospital characteristics (geographic region [Northeast, Southeast, Midwest, Southwest, West], urban vs. rural hospital, ownership [private, government, not-profit], hospital bed size [<250, 250–499, ≥ 500], teaching status [major, minor, none]). To confirm that any survival trends were independent of the duration of a hospital’s participation in the registry, we adjusted for the number of years a hospital had participated within GWTG-Resuscitation for each arrest. We also examined whether survival trends differed by age group (≥ 65 years vs. < 65 years), race, and sex by including an interaction term with calendar year in the model. Lastly, to exclude the possibility that our findings were due to enrollment of better-performing hospitals over time, we performed these analyses only for patients at hospitals with at least 8 years of registry participation.
Data were complete for all covariates, except race (6.6%), admission CPC score (14.6%), time of cardiac arrest (0.9%) and hospital variables (4.5%). Missing patient-level data were assumed to be missing at random and were imputed using multiple imputation.21 Results with and without imputation were not meaningfully different, so only the former are presented.
All statistical analyses were conducted using SAS Version 9.1.3 (SAS Institute, Cary, NC), IVEWARE (University of Michigan, MI), and R Version 2.6.0 (Free Software Foundation, Boston, MA). All hypothesis tests were 2-sided with a significance level of 0.05. The Institutional Review Board at University of Iowa approved the study.
Author contributions were as follows: study design (SG, PSC); data acquisition (PSC); data analysis and interpretation (SG, BKN, JAS, YL, HMK, PSC); drafting the manuscript (SG, PSC); and critical revision of the manuscript (SG, BKN, JAS, YL, HMK, PSC). Dr. Saket Girotra vouches for the integrity of the data and accuracy of the results. All authors have approved the manuscript for publication. Although the American Heart Association oversees GWTG-Resuscitation, it had no role in the study design, data analysis or interpretation, or manuscript preparation.
RESULTS
Among 84,625 patients, the initial cardiac arrest rhythm was asystole or PEA in 67,135 (79.3%) and VF or pulseless VT in 17,490 (20.7%). Over the study period, the proportion of cardiac arrests due to asystole or PEA increased from 68.7% in 2000 to 82.4% in 2009 (eFigure 1, P for trend <0.001). Table 1 describes temporal trends in patient characteristics. While there was a trend for younger age and less baseline neurological disability, illness severity increased over time with a higher prevalence of sepsis, use of mechanical ventilation, and intravenous vasopressors before the arrest event (P for trend <0.001 for all comparisons).
Table 1. Trends in Baseline Characteristics in Patients with an In-hospital Cardiac Arrest.
For illustrative purposes, trends in baseline characteristics are presented as 3 time periods. The P for trend is for temporal changes in these characteristics by calendar year.
| Year Groups | ||||
|---|---|---|---|---|
| 2000–2003 n= 23,633 | 2004–2006 n= 32,603 | 2007–2009 n= 28,389 | P for Trend | |
| Demographics | ||||
| Age, Mean (SD) | 67.3 (15.4) | 66.5 (15.6) | 65.9 (15.8) | < 0.001 |
| Male Sex, % | 13,582 (57.5) | 19,050 (58.4) | 16,546 (58.3) | 0.07 |
| Black Race, % | 4723 (21.8) | 6581 (21.4) | 6048 (22.7) | < 0.001 |
| Cardiac Arrest Characteristics, % | ||||
| Initial Cardiac Arrest Rhythm | < 0.001 | |||
| Asystole | 9423 (39.9) | 12,576 (38.6) | 9915 (34.9) | |
| Pulseless Electrical Activity | 8663 (36.7) | 13,343 (40.9) | 13,215 (46.5) | |
| Ventricular Fibrillation | 3999 (16.9) | 3878 (11.9) | 2952 (10.4) | |
| Pulseless Ventricular Tachycardia | 1548 (6.6) | 2806 (8.6) | 2307 (8.1) | |
| Amiodarone Use in Resuscitation | 3290 (13.9) | 5275 (16.2) | 5169 (18.2) | < 0.001 |
| Assessed with AED | 1094 (4.6) | 3545 (10.9) | 5169 (18.2) | < 0.001 |
| Arrest at Night (11pm to 7am) | 8369 (35.9) | 11,410 (35.3) | 9880 (35.1) | 0.09 |
| Arrest on Weekend | 7570 (32.0) | 10,470 (32.1) | 9049 (31.9) | 0.12 |
| Hospital Location of Arrest | < 0.001 | |||
| Intensive Care Unit | 13,189 (55.8) | 18,852 (57.8) | 16,859 (59.4) | |
| Monitored unit | 4735 (20.0) | 7269 (22.3) | 7160 (25.2) | |
| Non-monitored unit | 5709 (24.2) | 6482 (19.9) | 4370 (15.4) | |
| Hospital-wide response activated | 21,013 (88.9) | 28,182 (86.4) | 23,559 (83.0) | < 0.001 |
| CPC Category on Admission | ||||
| 1 | 9769 (50.8) | 14,524 (49.8) | 12,902 (54.2) | |
| 2 | 5882 (30.6) | 9047 (31.0) | 6496 (27.3) | |
| 3 | 2531 (13.2) | 4090 (14.0) | 3004 (12.6) | |
| 4 or 5 | 1042 (5.4) | 1529 (5.2) | 1413 (5.9) | |
| Pre-Existing Conditions, % | ||||
| Heart Failure, this admission | 4919 (20.8) | 6702 (20.6) | 5113 (18.0) | < 0.001 |
| Prior Heart Failure | 6131 (25.9) | 7305 (22.4) | 5743 (20.2) | < 0.001 |
| Myocardial Infarction, this admission | 4602 (19.5) | 5792 (17.8) | 4263 (15.0) | < 0.001 |
| Prior Myocardial Infarction | 5000 (21.2) | 5771 (17.7) | 4261 (15.0) | < 0.001 |
| Arrhythmia | 7850 (33.2) | 12,052 (37.0) | 8887 (31.3) | < 0.001 |
| Hypotension | 6353 (26.9) | 10,065 (30.9) | 7566 (26.7) | < 0.001 |
| Respiratory Insufficiency | 9799 (41.5) | 14,930 (45.8) | 11,943 (42.1) | < 0.001 |
| Renal Insufficiency | 8076 (34.2) | 11,999 (36.8) | 10,062 (35.4) | < 0.001 |
| Hepatic Insufficiency | 1771 (7.5) | 2947 (9.0) | 2342 (8.2) | < 0.001 |
| Metabolic or Electrolyte Abnormality | 4601 (19.5) | 6646 (20.4) | 4367 (15.4) | < 0.001 |
| Diabetes Mellitus | 7183 (30.4) | 10,550 (32.4) | 8944 (31.5) | < 0.001 |
| Baseline Depression in CNS Function | 3216 (13.6) | 4706 (14.4) | 3347 (11.8) | < 0.001 |
| Acute Stroke | 1037 (4.4) | 1454 (4.5) | 1155 (4.1) | 0.148 |
| Pneumonia | 3591 (15.2) | 5015 (15.4) | 4239 (14.9) | < 0.001 |
| Septicemia | 3367 (14.2) | 6037 (18.5) | 5363 (18.9) | < 0.001 |
| Major Trauma | 693 (2.9) | 1164 (3.6) | 1121 (3.9) | < 0.001 |
| Cancer | 2909 (12.3) | 4529 (13.9) | 3846 (13.5) | < 0.001 |
| Interventions in Place Prior to the Arrest, % | ||||
| Mechanical Ventilation | 6388 (27.0) | 10,300 (31.6) | 9702 (34.2) | < 0.001 |
| Intravenous Vasopressor Medication | 6804 (28.8) | 9175 (28.1) | 9060 (31.9) | < 0.001 |
| Intravenous Antiarrhythmic Therapy | 1435 (6.1) | 1944 (6.0) | 1953 (6.9) | < 0.001 |
| Dialysis | 897 (3.8) | 1421 (4.4) | 1118 (3.9) | < 0.001 |
| Intra-Aortic Balloon Pump | 394 (1.7) | 534 (1.6) | 449 (1.6) | 0.651 |
| Pulmonary Artery Catheter | 1346 (5.7) | 1534 (4.7) | 869 (3.1) | < 0.001 |
| Hospital Characteristics, % | ||||
| Geographic Region* | < 0.001 | |||
| Northeast | 2536 (11.7) | 4616 (14.7) | 3531 (12.7) | |
| Southeast | 6604 (30.5) | 8549 (27.2) | 7828 (18.2) | |
| Midwest | 5782 (26.7) | 7694 (24.5) | 6186 (22.3) | |
| Southwest | 3524 (16.3) | 5022 (16.0) | 5874 (21.2) | |
| West | 3215 (14.8) | 5522 (17.6) | 4329 (15.6) | |
| Location* | ||||
| Urban | 20,320 (93.8) | 29,722 (94.6) | 26,387 (95.1) | < 0.001 |
| Rural | 1341 (6.2) | 1681 (5.4) | 1361 (4.9) | |
| Ownership* | < 0.001 | |||
| Private | 1768 (8.2) | 3213 (10.2) | 3547 (12.8) | |
| Government | 3493 (16.1) | 5205 (16.6) | 4919 (17.7) | |
| Non-profit | 16,400 (75.7) | 22,985 (73.2) | 19,282 (69.5) | |
| Hospital Bed Size** | < 0.001 | |||
| < 250 | 5074 (23.0) | 6649 (20.9) | 4916 (17.5) | |
| 250–499 | 8546 (38.7) | 13,573 (42.6) | 12,250 (43.6) | |
| ≥ 500 | 8443 (38.3) | 11,607 (36.5) | 10,920 (38.9) | |
| Academic Hospital** | < 0.001 | |||
| Hospital with fellowship program (Major) | 6278 (28.5) | 10,794 (33.9) | 11,241 (40) | |
| Hospital with residency program (Minor) | 7485 (33.9) | 10,674 (33.5) | 8445 (30.1) | |
| Non-teaching hospital | 8300 (37.6) | 10,361 (32.6) | 8400 (29.9) | |
Abbreviations: AED, automated external defibrillator; CNS, central nervous system; CPC, cerebral performance category; SD, standard deviation.
Geographic Region, Location and Ownership data were missing for 3813 (4.5%) patients.
Hospital Bed Size and Academic Status data were missing for 2647 (3.1%) patients.
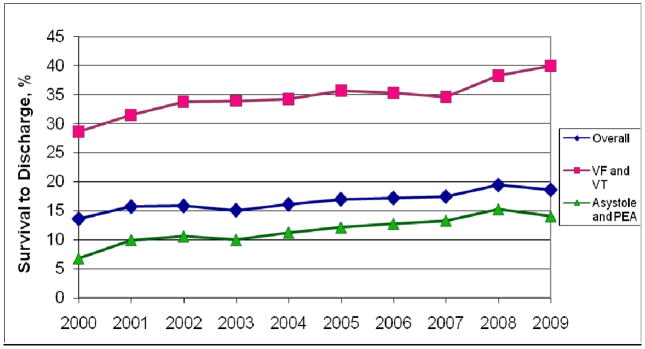
Survival to Discharge
The overall rate of survival to discharge was 17.0% (14,357/84,625), which improved significantly during the study period (Figure 2; eTable 2). After adjusting for temporal trends in patient and hospital characteristics, overall survival increased from 13.7% in 2000 to 22.3% in 2009 (adjusted rate-ratio per 1-year, 1.04; 95% confidence interval [CI], 1.02–1.05; P for trend <0.001; Table 2). Full model results are displayed in eTable 3. The temporal trends in survival were consistent in both rhythm groups (eTable 4) and were similar by age group (≥ 65 years vs. < 65 years), race (black vs. white) and sex (male vs. female) (P for all interactions > 0.10). Importantly, our findings were unchanged when we restricted the analyses to the 85 hospitals (33,464 patients) that participated in GWTG-Resuscitation for at least 8 years (eTable 5).
Figure 2. Unadjusted Rates of Survival to Hospital Discharge By Calendar Year.
Observed (crude) rates for survival to discharge are displayed for the overall cohort and separately for shockable (ventricular fibrillation [VF] and pulseless ventricular tachycardia [VT]) and non-shockable (asystole and pulseless electrical activity [PEA]) cardiac arrest rhythms. The P for trend was <0.001 for each survival curve.
Table 2. Trends in Survival and Neurological Outcomes.
Risk-adjusted rates of survival to discharge, acute resuscitation survival, post-resuscitation survival, and neurological disability for each calendar year are reported for the overall cohort. Rates are adjusted for temporal changes in patient and hospital characteristics [see eTable 3 for all model covariates].
| Risk-Adjusted Rates* | Adjusted RR per 1-year** (95% CI) | P for Trend** | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 2000 | 2001 | 2002 | 2003 | 2004 | 2005 | 2006 | 2007 | 2008 | 2009 | |||
| OVERALL | ||||||||||||
| Survival to Discharge, % | 13.7 | 17.1 | 18.2 | 17.8 | 18.9 | 20.0 | 20.5 | 21.2 | 23.3 | 22.3 | 1.04 (1.03, 1.06) | <0.001 |
| Acute Resuscitation Survival†, % | 42.7 | 45.1 | 45.4 | 46.0 | 47.0 | 48.6 | 49.7 | 52.5 | 55.2 | 54.1 | 1.03 (1.02, 1.04) | <0.001 |
| Post-Resuscitation Survival‡, % | 32.0 | 38.3 | 40.0 | 39.0 | 40.8 | 42.1 | 42.4 | 41.5 | 43.6 | 42.9 | 1.02 (1.01, 1.03) | 0.001 |
| Neurological Outcome in Survivors, % | ||||||||||||
| Significant Disability# (CPC > 1), % | 32.9 | 35.7 | 31.9 | 34.3 | 34.0 | 33.1 | 33.0 | 32.7 | 31.8 | 28.1 | 0.98 (0.97, 1.00) | 0.02 |
| Severe Disability¶ (CPC > 2), % | 10.1 | 10.5 | 9.8 | 10.5 | 11.5 | 11.5 | 9.7 | 12.2 | 11.7 | 10.7 | 1.01 (0.98, 1.04) | 0.37 |
Abbreviations: CI, confidence interval; CPC, cerebral performance category; RR, rate-ratio.
Risk-adjusted rates for each calendar year were obtained by multiplying the observed rate for the reference year (2000) by the corresponding rate-ratios for 2001 through 2009 from a model evaluating calendar year as a categorical variable
Determined from a model evaluating calendar year as a continuous variable
Acute Resuscitation Survival was determined by the number of patients with return of spontaneous circulation for at least 20 minutes divided by the number of patients with a cardiac arrest.
Post-resuscitation Survival was determined by the number surviving to hospital discharge divided by the number surviving the acute resuscitation.
Significant Disability was defined as the proportion of patients surviving to hospital discharge with a CPC Score of > 1.
Severe Disability was defined as the proportion of patients surviving to hospital discharge with a CPC Score of > 2.
Secondary Outcomes
Rates of acute resuscitation survival also improved substantially in the overall cohort (risk-adjusted rate: 42.7% in 2000, 54.1% in 2009; adjusted rate-ratio per 1-year, 1.03; 95% CI, 1.02–1.04; P for trend <0.001; Table 2) and by rhythm type (eTable 4). In contrast, temporal improvement in post-resuscitation survival was much smaller (Table 2; eTable 4). In patients with VF and pulseless VT, there was no change in time to defibrillation (eFigure 2).
While rates of survival to discharge increased, rates of significant neurological disability (discharge CPC score >1) among survivors decreased over time in the overall cohort (risk-adjusted rate: 32.9% in 2000, 28.1% in 2009; adjusted rate-ratio per 1-year, 0.98; 95% CI, 0.97–1.00; P for trend=0.02; Table 2) and in patients with VF and pulseless VT (eTable 4). Rates of severe neurological disability (discharge CPC score >2), however, were unchanged over time (Table 2; eTable 4).
DISCUSSION
During the past decade, survival from in-hospital cardiac arrest has improved substantially among patients at hospitals enrolled in a national quality improvement registry. These gains have been achieved primarily through increased survival during the acute resuscitation event and have been accompanied by a decrease in the rate of significant neurological disability among survivors. Using a conservative estimate of 200,000 in-hospital cardiac arrests annually in the U.S.,22 our findings suggest that an additional 17,200 patients would have survived to hospital discharge in 2009, compared to 2000 (based on 8.6% absolute improvement in risk-adjusted survival during this period). We also estimate that over 3500 cases of significant neurological disability would have been avoided.
To our knowledge, this is the first study to document temporal trends for higher survival following in-hospital cardiac arrest. The unadjusted survival rate of 17.0% in our study was lower than the 18.3% survival found in a recent study of Medicare patients10 largely because we excluded cardiac arrests in the emergency room and procedural areas - which are known to have higher survival.23, 24 Although the Medicare study did not detect survival trends,10 several factors likely explain our different findings. Since that study used procedure codes for CPR to identify cardiac arrest patients, it is possible that some patients who received CPR for bradycardia (and not cardiac arrest) were included. Moreover, the Medicare study was unable to adjust for initial cardiac arrest rhythm, which we found has changed over time. Finally, although we adjusted for the duration of a hospital’s participation within GWTG-Resuscitation, we cannot distinguish whether our findings are a consequence of motivated hospitals participating in a quality improvement registry or part of a nationwide trend arising from other factors (such as changes in clinical practice, equipment, early recognition of illness acuity, etc).
We found that improvement in cardiac arrest survival was largely driven by increased survival from the acute resuscitation, and this trend was seen regardless of whether the initial cardiac arrest rhythm was treatable by defibrillation or not. In patients with VF or pulseless VT, improvement in survival over time was not accompanied by shorter defibrillation times suggesting that other factors during resuscitation may have accounted for this improvement. These factors may include earlier recognition of cardiac arrest, shorter response times, greater availability of trained personnel, and provision of higher quality chest compressions with fewer interruptions. In fact, many of these processes have been emphasized in the American Heart Association Guidelines for CPR over the past decade.25, 26 Future studies are needed to better understand which specific factors are responsible for improvements in cardiac arrest survival so that survival gains can be consolidated and expanded to all hospitals.
Several issues also merit further discussion. First, the increase in survival may simply reflect a decrease in baseline risk over time. However, we found little evidence that this was occurring. Although patients in our study were younger by 1.5 years at the end of the decade compared to the beginning, they were also sicker, with higher rates of sepsis, mechanical ventilation, and use of vasopressor medications prior to the arrest. Moreover, our results were consistent even after adjustment for temporal changes in patient factors over time, including age. Second, increasing use of advanced directives and DNR orders could have introduced selection bias in the patients who undergo resuscitation for a cardiac arrest over time. Yet again, our observed temporal increase in the proportion of patients on mechanical ventilation and vasopressor medications prior to cardiac arrest makes this less likely. Moreover, a recent study found that the proportion of in-hospital deaths that are preceded by CPR has actually increased over time.10 Lastly, our findings are unlikely due to enrollment of better-performing hospitals over time, since we found similar results when we restricted our analyses to hospitals that participated in GWTG-Resuscitation for 8 years or longer.
Our findings should be interpreted in light of the following potential limitations. First, although data in GWTG-Resuscitation allowed us to adjust for a number of key variables, the possibility of residual confounding still remains. Second, we did not have detailed information on specific resuscitation process variables (e.g., quality of chest compressions), treatments (e.g., use of hypothermia or cardiac catheterization) and quality improvement initiatives at hospitals (e.g., use of routine mock codes) to better understand the reasons for improved rates of survival. These are often difficult to document accurately and future studies are required to examine the role of these factors in explaining the temporal increase in survival. Third, our neurological assessments at discharge may not predict long-term quality of life since neurological function may evolve after discharge.27 Lastly, although we found that improved survival trends were independent of the duration of a hospital’s participation within GWTG-Resuscitation, our study cohort was likely comprised of hospitals motivated for quality improvement; therefore, our findings may not be generalizable to all U.S. hospitals.
In conclusion, we found that survival after in-hospital cardiac arrest has improved significantly over the past decade at hospitals participating in a large, national quality improvement registry. This improvement was largely attributed to increased survival during acute resuscitation and was accompanied by a parallel decrease in rates of neurological disability over time. Identifying the factors responsible for these improved trends and expanding these processes to other facilities is warranted.
Supplementary Material
References
- 1.Rea TD, Crouthamel M, Eisenberg MS, Becker LJ, Lima AR. Temporal patterns in long-term survival after resuscitation from out-of-hospital cardiac arrest. Circulation. 2003;108:1196–201. doi: 10.1161/01.CIR.0000087403.24467.A4. [DOI] [PubMed] [Google Scholar]
- 2.Hinchey PR, Myers JB, Lewis R, et al. Improved out-of-hospital cardiac arrest survival after the sequential implementation of 2005 AHA guidelines for compressions, ventilations, and induced hypothermia: the Wake County experience. Ann Emerg Med. 2003;56:348–57. doi: 10.1016/j.annemergmed.2010.01.036. [DOI] [PubMed] [Google Scholar]
- 3.Pell JP, Corstorphine M, McConnachie A, et al. Post-discharge survival following pre-hospital cardiopulmonary arrest due to cardiac aetiology: temporal trends and impact of changes in clinical management. Eur Heart J. 2006;27:406–12. doi: 10.1093/eurheartj/ehi604. [DOI] [PubMed] [Google Scholar]
- 4.Aufderheide TP, Yannopoulos D, Lick CJ, et al. Implementing the 2005 American Heart Association Guidelines improves outcomes after out-of-hospital cardiac arrest. Heart Rhythm. 2010;7:1357–62. doi: 10.1016/j.hrthm.2010.04.022. [DOI] [PubMed] [Google Scholar]
- 5.Hunt EA, Walker AR, Shaffner DH, Miller MR, Pronovost PJ. Simulation of in-hospital pediatric medical emergencies and cardiopulmonary arrests: highlighting the importance of the first 5 minutes. Pediatrics. 2008;121:e34–43. doi: 10.1542/peds.2007-0029. [DOI] [PubMed] [Google Scholar]
- 6.Abella BS, Edelson DP, Kim S, et al. CPR quality improvement during in-hospital cardiac arrest using a real-time audiovisual feedback system. Resuscitation. 2007;73:54–61. doi: 10.1016/j.resuscitation.2006.10.027. [DOI] [PubMed] [Google Scholar]
- 7.Edelson DP, Litzinger B, Arora V, et al. Improving in-hospital cardiac arrest process and outcomes with performance debriefing. Arch Intern Med. 2008;168:1063–9. doi: 10.1001/archinte.168.10.1063. [DOI] [PubMed] [Google Scholar]
- 8.Tai CK, Cattermole GN, Mak PSK, Graham CA, Rainer TH. Nurse-initiated defibrillation: are nurses confident enough? Emergency Medicine Journal. 2010 doi: 10.1136/emj.2009.084848. [DOI] [PubMed] [Google Scholar]
- 9.Peberdy MA, Kaye W, Ornato JP, et al. Cardiopulmonary resuscitation of adults in the hospital: a report of 14720 cardiac arrests from the National Registry of Cardiopulmonary Resuscitation. Resuscitation. 2003;58:297–308. doi: 10.1016/s0300-9572(03)00215-6. [DOI] [PubMed] [Google Scholar]
- 10.Ehlenbach WJ, Barnato AE, Curtis JR, et al. Epidemiologic study of in-hospital cardiopulmonary resuscitation in the elderly. N Engl J Med. 2009;361:22–31. doi: 10.1056/NEJMoa0810245. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Nadkarni VM, Larkin GL, Peberdy MA, et al. First documented rhythm and clinical outcome from in-hospital cardiac arrest among children and adults. JAMA. 2006;295:50–7. doi: 10.1001/jama.295.1.50. [DOI] [PubMed] [Google Scholar]
- 12.Meaney PA, Nadkarni VM, Kern KB, Indik JH, Halperin HR, Berg RA. Rhythms and outcomes of adult in-hospital cardiac arrest. Crit Care Med. 2010;38:101–8. doi: 10.1097/CCM.0b013e3181b43282. [DOI] [PubMed] [Google Scholar]
- 13.Peberdy MA, Ornato JP, Larkin GL, et al. Survival from in-hospital cardiac arrest during nights and weekends. JAMA. 2008;299:785–92. doi: 10.1001/jama.299.7.785. [DOI] [PubMed] [Google Scholar]
- 14.Cummins RO, Chamberlain D, Hazinski MF, et al. Recommended guidelines for reviewing, reporting, and conducting research on in-hospital resuscitation: the in-hospital ‘Utstein style’. American Heart Association. Circulation. 1997;95:2213–39. doi: 10.1161/01.cir.95.8.2213. [DOI] [PubMed] [Google Scholar]
- 15.Jacobs I, Nadkarni V, Bahr J, et al. Cardiac arrest and cardiopulmonary resuscitation outcome reports: update and simplification of the Utstein templates for resuscitation registries: a statement for healthcare professionals from a task force of the International Liaison Committee on Resuscitation (American Heart Association, European Resuscitation Council, Australian Resuscitation Council, New Zealand Resuscitation Council, Heart and Stroke Foundation of Canada, InterAmerican Heart Foundation, Resuscitation Councils of Southern Africa) Circulation. 2004;110:3385–97. doi: 10.1161/01.CIR.0000147236.85306.15. [DOI] [PubMed] [Google Scholar]
- 16.Chan PS, Krumholz HM, Nichol G, Nallamothu BK. Delayed time to defibrillation after in-hospital cardiac arrest. N Engl J Med. 2008;358:9–17. doi: 10.1056/NEJMoa0706467. [DOI] [PubMed] [Google Scholar]
- 17.Jennett B, Bond M. Assessment of outcome after severe brain damage. Lancet. 1975;1:480–4. doi: 10.1016/s0140-6736(75)92830-5. [DOI] [PubMed] [Google Scholar]
- 18.Chan PS, Krumholz HM, Spertus JA, et al. Automated external defibrillators and survival after in-hospital cardiac arrest. JAMA. 2010;304:2129–36. doi: 10.1001/jama.2010.1576. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Greenland S. Model-based estimation of relative risks and other epidemiologic measures in studies of common outcomes and in case-control studies. Am J Epidemiol. 2004;160:301–5. doi: 10.1093/aje/kwh221. [DOI] [PubMed] [Google Scholar]
- 20.Zou G. A modified poisson regression approach to prospective studies with binary data. Am J Epidemiol. 2004;159:702–6. doi: 10.1093/aje/kwh090. [DOI] [PubMed] [Google Scholar]
- 21.Raghunathan TESP, Van Hoeyk J. IVEware: Imputation and Variance Estimation Software - User Guide. Michigan: Survey Research Center, Institute for Social Research University of Michigan; 2002. [Google Scholar]
- 22.Merchant RM, Yang L, Becker LB, et al. Incidence of treated cardiac arrest in hospitalized patients in the United States. Crit Care Med. 2011 doi: 10.1097/CCM.0b013e3182257459. Published ahead of print, 23 June 2011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Kayser RG, Ornato JP, Peberdy MA. Cardiac arrest in the Emergency Department: a report from the National Registry of Cardiopulmonary Resuscitation. Resuscitation. 2008;78:151–60. doi: 10.1016/j.resuscitation.2008.03.007. [DOI] [PubMed] [Google Scholar]
- 24.Mhyre JM, Ramachandran SK, Kheterpal S, Morris M, Chan PS. Delayed time to defibrillation after intraoperative and periprocedural cardiac arrest. Anesthesiology. 2010;113:782–93. doi: 10.1097/ALN.0b013e3181eaa74f. [DOI] [PubMed] [Google Scholar]
- 25.2005 American Heart Association Guidelines for Cardiopulmonary Resuscitation and Emergency Cardiovascular Care. Circulation. 2005;112:IV1–203. doi: 10.1161/CIRCULATIONAHA.105.166550. [DOI] [PubMed] [Google Scholar]
- 26.Field JM, Hazinski MF, Sayre MR, et al. Part 1: Executive Summary: 2010 American Heart Association Guidelines for Cardiopulmonary Resuscitation and Emergency Cardiovascular Care. Circulation. 2010;122:S640–56. doi: 10.1161/CIRCULATIONAHA.110.970889. [DOI] [PubMed] [Google Scholar]
- 27.Hsu JWY, Madsen CD, Callaham ML. Quality-of-Life and Formal Functional Testing of Survivors of Out-of-Hospital Cardiac Arrest Correlates Poorly With Traditional Neurologic Outcome Scales. Annals of Emergency Medicine. 1996;28:597–605. doi: 10.1016/s0196-0644(96)70080-x. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.