Abstract
Background
Limited data on the incidence and clinical characteristics of adult pertussis infections are available in Korea.
Methods
Thirty-one hospitals and the Korean Centers for Disease Control and Prevention collaborated to investigate the incidence and clinical characteristics of pertussis infections among adults with a bothersome cough in non-outbreak, ordinary outpatient settings. Nasopharyngeal aspirates or nasopharyngeal swabs were collected for polymerase chain reaction (PCR) and culture tests.
Results
The study enrolled 934 patients between September 2009 and April 2011. Five patients were diagnosed as confirmed cases, satisfying both clinical and laboratory criteria (five positive PCR and one concurrent positive culture). Among 607 patients with cough duration of at least 2 weeks, 504 satisfied the clinical criteria of the US Centers for Disease Control and Prevention (i.e., probable case). The clinical pertussis cases (i.e., both probable and confirmed cases) had a wide age distribution (45.7±15.5 years) and cough duration (median, 30 days; interquartile range, 18.0~50.0 days). In addition, sputum, rhinorrhea, and myalgia were less common and dyspnea was more common in the clinical cases, compared to the others (p=0.037, p=0.006, p=0.005, and p=0.030, respectively).
Conclusion
The positive rate of pertussis infection may be low in non-outbreak, ordinary clinical settings if a PCR-based method is used. However, further prospective, well-designed, multicenter studies are needed.
Keywords: Adult, Cough, Incidence, Whooping Cough, Signs and Symptoms
Introduction
Pertussis infection is characterized by paroxysmal coughing, inspiratory whooping, and post-tussive vomiting and is also a bacterial cause of acute bronchitis requiring antibiotic treatment1. Although the incidence of pertussis infection in the United States has declined dramatically since the introduction of the inactivated whole-cell pertussis vaccine in the 1940s, the number of reported cases is again increasing, with a striking increase in adolescents and adults since 19762. This resurgence has also been observed in countries such as Canada and Argentina since the 1980s3-7. In a large European study (1998~2002), the incidence of pertussis infection did not decrease in children, but rather increased in adults3.
Multiple mechanisms may have caused this increase in the rate of pertussis infection: development of more sensitive diagnostic methods; changes in nationwide surveillance systems for communicable diseases; and waning immunity among adolescents and adults2,8. In particular, the clinical presentation of adults with pertussis infection is not typical, and symptoms are frequently less severe in this population. Therefore, pertussis can go undiagnosed in adults, and adults can be the primary source of pertussis infection in non-vaccinated infants, in whom infection is potentially fatal2.
In terms of vaccination schedule, a dose of tetanus and reduced dose of diphtheria and acellular pertussis (Tdap) is recommended for adolescents and adults by the US Advisory Committee on Immunization Practice and the Canada National Advisory Committee on Immunization. Tdap was introduced recently in Korea. However, contrary to the seriousness of adult pertussis infection in Western countries, data for Korea are limited; most reported pertussis cases have been in children. Therefore, a study of adult pertussis infection is urgently required to estimate the current burden of pertussis infection and facilitate a future booster vaccination program. This study investigated the incidence and clinical characteristics of adult pertussis infection in non-outbreak, ordinary clinical settings.
Materials and Methods
1. Sites and subjects
This study was conducted from September 2009 to April 2011 at 31 hospitals (14 primary care clinics, six secondary referral hospitals, and 11 tertiary referral hospitals) in eight South Korean provinces.
We enrolled only outpatients (≥18 years old) who presented with bothersome coughs. Exclusion criteria were a history of antibiotic treatment within 7 days; active lesions on the chest or paranasal sinus radiographs, if available; immunocompromised (e.g., acquired immune deficiency syndrome, leukemia, aplastic anemia, organ transplant, autoimmune diseases, or chemotherapy); or cough illness with a confirmed alternative cause (e.g., drugs [angiotensin-converting enzyme inhibitors], pneumonia, allergic rhinitis, sinusitis, or gastroesophageal reflux).
2. Clinical data and specimen collection
For all enrolled patients, the participating investigators at outpatient departments collected clinical information, including data on age, gender, chronic respiratory diseases, co-morbid illnesses, smoking status, cough duration, classic pertussis symptoms, other respiratory symptoms, history of diphtheria, tetanus, and pertussis or diphtheria, tetanus, and acellular pertussis (DTP or DTaP) vaccination; and a history of hospital visits.
We collected laboratory specimens via nasopharyngeal aspiration (NPA, bulb aspiration kit prefilled with saline, N-Pak; M-Pro, Annandale, MN, USA) or nasopharyngeal swabbing (NPS, liquid Amies medium on flocked swabs; Copan Diagnostic, Murrieta, CA, USA), and the specimens were transferred at room temperature to the Department of Bacterial Respiratory Infection at the Korean Centers for Disease Control and Prevention (KCDC) within 24 hours. To ensure consistent specimen quality, independent personnel, usually a nurse, performed the sampling procedure in each hospital during the study period, and all microbiological tests were performed and validated by the KCDC.
3. Case definition
The US Centers for Disease Control and Prevention (CDC) clinical criteria for pertussis infection were defined as when patients presented with a cough illness for ≥2 weeks and had one of the following classical symptoms: 1) paroxysmal coughing, 2) inspiratory whooping, or 3) post-tussive vomiting9. The laboratory criteria for diagnosis were isolation of Bordetella pertussis or a positive polymerase chain reaction (PCR) assay. A "confirmed case" was diagnosed when a patient satisfied both the clinical and laboratory criteria and a "probable case" was diagnosed when a patient satisfied only the clinical criteria9.
4. Specimens and microbiologic tests
All specimens were subject to PCR and culture tests. Regan and Lowe agar medium (charcoal agar supplemented with 10% horse blood) with 40 mg/mL cephalexin was used for culture tests10. After inoculation, the plates were incubated for at least 7 days under humid conditions (35~36℃). Identification was based on both biological characteristics and PCR11.
A portion of each specimen was boiled for 5 minutes for PCR. After centrifugation, 1~2µL of the supernatant was used as the PCR template. Although no standard PCR method exists, the "repeated-insertion sequence" and "pertussis toxin promoter region" have been used most frequently as target regions12,13. We used the repeated-insertion sequence and primers BP1 (5'-GATTCAATAGGTTGTATGCATGGTT-3') and BP2 (5'-TTCAGGCACACAAACTTGATGGGCG-3'). In-house PCR was performed using a commercial pre-mixed Taq polymerase (AccuPower PCR PreMix; Bioneer, Daejeon, Korea).
The PCR conditions were 95℃ for 5 minutes, followed by 40 cycles at 95℃ for 5 seconds and 55℃ for 10 seconds. The PCR products were resolved by electrophoresis on 2% agarose gels, and identification of a 180-bp band was considered positive.
5. Data analyses
We investigated the incidence of confirmed cases and compared the clinical characteristics between the clinical cases of pertussis infection and other cases, among patients with a cough duration≥2 weeks. Data are expressed as the mean±standard deviation (or median and interquartile range) for continuous variables and as percentages for categorical variables, unless otherwise indicated. Student's t-tests or Mann-Whitney U-tests were performed for continuous data; whereas chisquare or Fisher's exact tests were used for categorical data. A p<0.05 was considered statistically significant, and all analyses were conducted using SAS statistical software, EG version (SAS Institute, Cary, NC, USA).
Results
1. Demographics and clinical symptoms
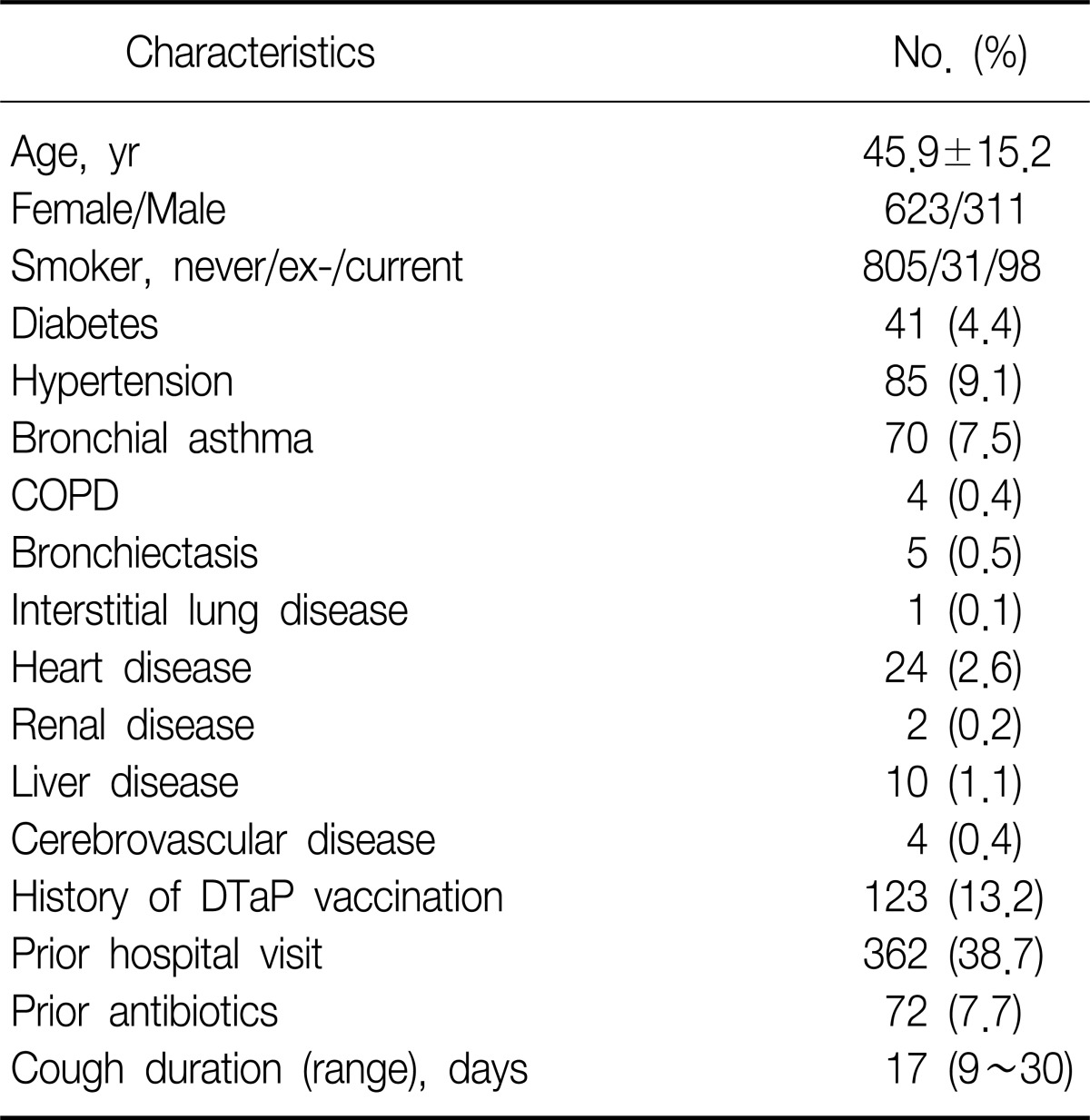
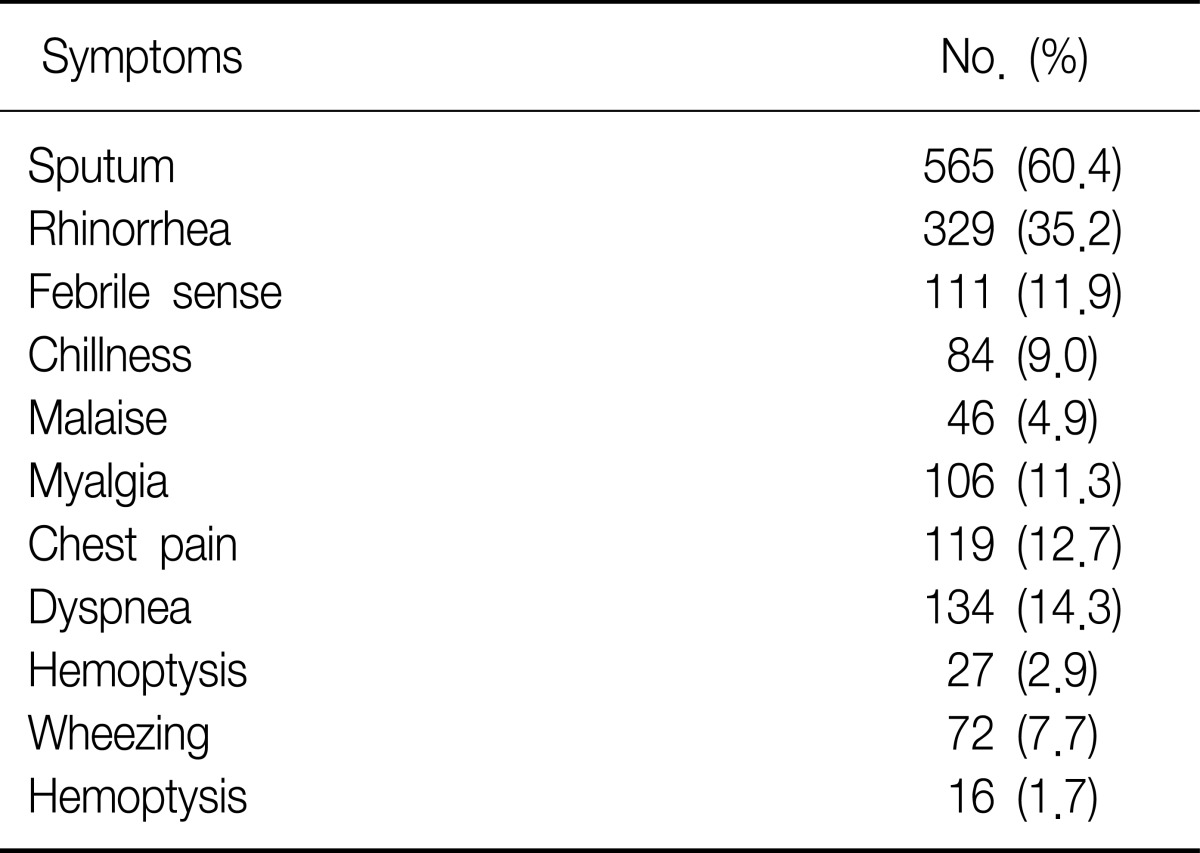
In total, 938 patients were initially enrolled, and four with incomplete clinical data were excluded (primary care clinics, 157 patients; secondary referral hospitals, 214 patients; and tertiary referral hospitals, 563 patients). The mean age of the patients (n=934) was 45.9±15.2 years, and 66.7% were female (Table 1). The patient's ages were distributed evenly, and 30~39 years was the most frequent age group. The median cough duration was 17 days (range, 9~30 days). Hypertension and bronchial asthma were the most common co-morbid illnesses, and sputum and rhinorrhea were the most frequent symptoms, except for coughing (Table 2). Only 13.2% (123/934) of the patients were able to recall if they had received the DTP (or DTaP) vaccine; the rest were uncertain.
Table 1.
Baseline characteristics (n=934)
COPD: chronic obstructive pulmonary disease; DTaP: diphtheria, tetanus, and acellular pertussis.
Table 2.
Symptoms and signs (n=934)
In total, 607 patients presented with a cough duration ≥2 weeks: four (0.7%) were diagnosed as confirmed cases and 504 (83.0%) as probable cases. Another patient with a cough duration of 8 days was also diagnosed as a confirmed case because he was culture-positive for B. pertussis. Therefore, there were 509 clinical cases of pertussis infection.
2. Microbiologic data
We collected 568 NPA and 366 NPS samples during the study period. Five patients were PCR positive, and one was also culture positive. NPS and NPA had positive rates of 1.1% (4/366) and 0.2% (1/568), respectively.
3. Clinical characteristics
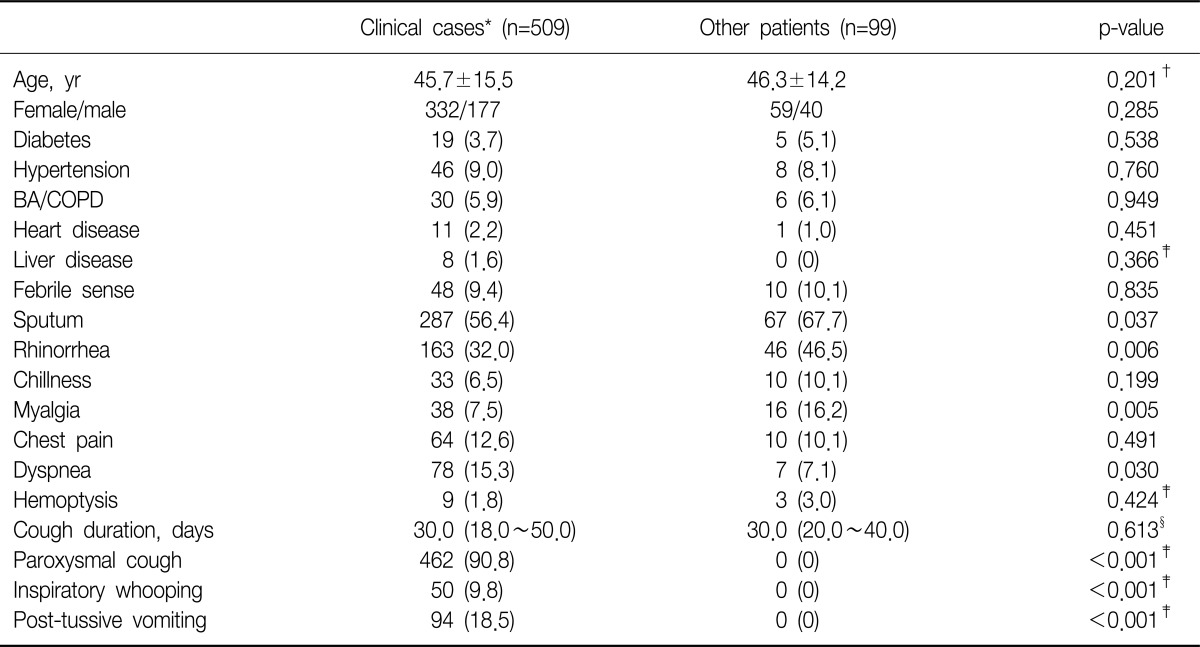
We investigated the clinical characteristics of 509 clinical cases (i.e., five confirmed and 504 probable cases). Both the age distribution and cough duration of the clinical cases were diverse (45.7±15.5 years and 30 [18.0~ 50.0] days, respectively), and 462 (90.8%) patients complained of paroxysmal cough, 9.8% of inspiratory whooping, and 18.5% of post-tussive vomiting.
The characteristics of the clinical cases are compared to other cases in Table 3. No significant differences between the two groups were observed among the comorbid illnesses. In terms of clinical symptoms, sputum, rhinorrhea, and myalgia were less frequent and dyspnea was more frequent in the clinical cases compared to other cases (p=0.037, p=0.006, p=0.005, and p=0.030, respectively).
Table 3.
Comparisons of the clinical characteristics between clinical cases and other patients
Values are represented as number (% or range).
*Confirmed (n=5) and probable (n=504) cases defined by the US Centers for Disease Control and Prevention's criteria. †Student's t-tests. ‡Fisher's exact test. §Mann-Whitney U-tests.
BA: bronchial asthma; COPD: chronic obstructive pulmonary disease.
4. Close contacts
In terms of close contacts, we investigated only three contacts of one confirmed case. All had cough illness days before the confirmed patient, but none was PCR or culture positive. We could not investigate the close contacts of the remaining confirmed patients due to their refusal (n=2) or loss to follow-up (n=2).
Discussion
In this study, the positive PCR rate for B. pertussis among all enrolled patients in a non-outbreak, ordinary clinical setting was 0.5% (5/934), and it was 0.7% among the patients with a cough duration≥2 weeks.
This low positive rate can be explained by several factors. First, we recruited patients complaining of cough of any duration, regardless of whether they presented with classical pertussis symptoms. Therefore, many patients with upper respiratory viral infections may have been included. Second, we did not perform serologic testing. Third, false-positive PCR results were possible. Fourth, several other factors might have been possible causes, such as specimen quality, the time taken to transfer specimens to the central laboratory, and prior antibiotic use. However, our objective was to determine the clinical features and incidence of pertussis infection in an ordinary outpatient setting; therefore, the threshold for seeking medical care and performing tests may have been different from that during outbreaks.
Culture has been considered the gold-standard method of laboratory diagnosis. It is highly specific, but has varying sensitivity depending on factors such as age, vaccination status, and transfer time14. Culture is rarely useful for the prompt diagnosis and treatment of an adult pertussis infection due to the long turnaround time. However, serology has proven useful for diagnosis in adolescents and adults, particularly in the late period (i.e., after 3~4 weeks), when the results of both PCR and culture are frequently negative. Many studies have shown that 13~32% of adolescents and adults with cough illness are serologically positive for pertussis infection15-20. Therefore, we may have underestimated the incidence of pertussis infection. Due to the high sensitivity of PCR (70~99%)14, the US CDC and the World Health Organization include the test in the diagnostic criteria for pertussis infection. We used a method similar to that used in Loeffelholz et al.21, in which the sensitivity and specificity of a PCR test were 93.5% and 97.1%, respectively. However, although PCR can detect patients with an atypical presentation, there is no standardized PCR kit, and it still has the risk of false positives.
Despite the high vaccination coverage in many industrialized countries, a worldwide resurgence of pertussis infection has been reported in recent years2,3. This significant increase has led to much research on immunity, leading to the revelation that neither vaccination nor natural infection guarantees life-long immunity22,23. Contrary to the pre-vaccine era when the majority of pertussis infection occurred in children and adults could maintain their boosted immunity by recurrent exposure, in the post-vaccine era the risk of pertussis infection can increase among adolescents and adults when their vaccine-induced immunity diminishes.
Surveillance of pertussis infection in Korea relies mostly on clinical notification systems, and most reported cases are in children24. Adult patients often do not seek medical care until several weeks after the onset of their illness and frequently present with mild symptoms. Therefore, disease surveillance and control may not be possible using only a clinical notification system. In 2005, Park et al.25 reported an incidence of 2.9% among Korean adults with cough≥1 week. The median age of patients in their study was 30 years, and 65.7% had a paroxysmal cough. However, theirs was a small study, including only two centers (n=102)25.
Among patients with a cough duration≥2 weeks, 90.8% of patients had a paroxysmal cough, 88 (17.3%) presented with two classical symptoms, and 14 (2.8%) had all three classical symptoms, but none of those with three symptoms were both PCR and culture negative. In a study of immunized children and adults in Israel, who were serologically confirmed to have pertussis infection, all patients had a cough (4±3.6 weeks), but only 6% had classical whooping. Most had atypical and mild symptoms26. Although several studies have demonstrated the high diagnostic sensitivity of paroxysmal cough, the diagnostic accuracy of the three classical symptoms remains questionable25-27. In this study, we also investigated other clinical symptoms, and found that sputum, rhinorrhea, and myalgia were less frequent and dyspnea was more frequent in clinical cases compared to those in other patients. Despite the small number of laboratory-confirmed cases, we think that these are interesting findings worthy of reevaluation in a future study. Our results may assist in excluding patients who are less likely to have pertussis infection.
Many patients could not recall whether they had received a pertussis vaccine in their childhood. Therefore, we could not evaluate the clinical implication of prior vaccination on adult pertussis infection. However, since the DTP vaccine was introduced in 1958, the incidence of pertussis in South Korea has been low. The DTaP vaccination rate of infants and children in the early 2000s was over 98.0% in two metropolitan cities in South Korea28. In our study, four of five confirmed patients were born after 1958 and had most likely received either the DTP or DTaP vaccine.
This study had several limitations including a lack of serologic testing. However, the study also had several strengths. This is the first large-scale, prospective study performed in non-outbreak, ordinary settings. This study encompassed primary care clinics and secondary and tertiary referral hospitals nationwide. Although the positivity rate was low, we think that our findings are important, because this is the first multicenter study of adult patients to tackle an important epidemic issue. As such, it represents the groundwork for a future study intended to provide evidence for a booster vaccination program.
In conclusion, the positive rate of pertussis infection may be low in non-outbreak, ordinary clinical settings if a PCR-based method is used. Further prospective, well-designed, multicenter studies should be performed to define precisely the incidence and clinical implications of adult pertussis infection.
Acknowledgements
The authors would like to thank Dong-Gyu Kim, Mi-Ok Kim, Seung Hun Jang, Yong-Il Hwang, Ji-Yong Choi, Jong-Wook Yun, Jong-Woo Lee, Jun-Wook Ha, Tae-Gyeong Lim, and Hee-Suck Jeon for their contribution to this nationwide surveillance.
References
- 1.Gonzales R, Sande MA. Uncomplicated acute bronchitis. Ann Intern Med. 2000;133:981–991. doi: 10.7326/0003-4819-133-12-200012190-00014. [DOI] [PubMed] [Google Scholar]
- 2.Hewlett EL, Edwards KM. Clinical practice. Pertussis: not just for kids. N Engl J Med. 2005;352:1215–1222. doi: 10.1056/NEJMcp041025. [DOI] [PubMed] [Google Scholar]
- 3.Celentano LP, Massari M, Paramatti D, Salmaso S, Tozzi AE EUVAC-NET Group. Resurgence of pertussis in Europe. Pediatr Infect Dis J. 2005;24:761–765. doi: 10.1097/01.inf.0000177282.53500.77. [DOI] [PubMed] [Google Scholar]
- 4.de Melker HE, Versteegh FG, Schellekens JF, Teunis PF, Kretzschmar M. The incidence of Bordetella pertussis infections estimated in the population from a combination of serological surveys. J Infect. 2006;53:106–113. doi: 10.1016/j.jinf.2005.10.020. [DOI] [PubMed] [Google Scholar]
- 5.Hozbor D, Mooi F, Flores D, Weltman G, Bottero D, Fossati S, et al. Pertussis epidemiology in Argentina: trends over 2004-2007. J Infect. 2009;59:225–231. doi: 10.1016/j.jinf.2009.07.014. [DOI] [PubMed] [Google Scholar]
- 6.Mayet A, Brossier C, Haus-Cheymol R, Verret C, Meynard JB, Migliani R, et al. Pertussis surveillance within the French armed forces: a new system showing increased incidence among young adults (2007-2009) J Infect. 2011;62:322–324. doi: 10.1016/j.jinf.2011.02.005. [DOI] [PubMed] [Google Scholar]
- 7.Skowronski DM, De Serres G, MacDonald D, Wu W, Shaw C, Macnabb J, et al. The changing age and seasonal profile of pertussis in Canada. J Infect Dis. 2002;185:1448–1453. doi: 10.1086/340280. [DOI] [PubMed] [Google Scholar]
- 8.Cherry JD. The science and fiction of the "resurgence" of pertussis. Pediatrics. 2003;112:405–406. doi: 10.1542/peds.112.2.405. [DOI] [PubMed] [Google Scholar]
- 9.Tiwari T, Murphy TV, Moran J National Immunization Program, CDC. Recommended antimicrobial agents for the treatment and postexposure prophylaxis of pertussis: 2005 CDC Guidelines. MMWR Recomm Rep. 2005;54:1–16. [PubMed] [Google Scholar]
- 10.Regan J, Lowe F. Enrichment medium for the isolation of Bordetella. J Clin Microbiol. 1977;6:303–309. doi: 10.1128/jcm.6.3.303-309.1977. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Lautrop H. Laboratory diagnosis of whooping-cough or Bordetella infections. Bull World Health Organ. 1960;23:15–35. [PMC free article] [PubMed] [Google Scholar]
- 12.Glare EM, Paton JC, Premier RR, Lawrence AJ, Nisbet IT. Analysis of a repetitive DNA sequence from Bordetella pertussis and its application to the diagnosis of pertussis using the polymerase chain reaction. J Clin Microbiol. 1990;28:1982–1987. doi: 10.1128/jcm.28.9.1982-1987.1990. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Houard S, Hackel C, Herzog A, Bollen A. Specific identification of Bordetella pertussis by the polymerase chain reaction. Res Microbiol. 1989;140:477–487. doi: 10.1016/0923-2508(89)90069-7. [DOI] [PubMed] [Google Scholar]
- 14.Zouari A, Smaoui H, Kechrid A. The diagnosis of pertussis: which method to choose? Crit Rev Microbiol. 2012;38:111–121. doi: 10.3109/1040841X.2011.622715. [DOI] [PubMed] [Google Scholar]
- 15.Birkebaek NH, Kristiansen M, Seefeldt T, Degn J, Moller A, Heron I, et al. Bordetella pertussis and chronic cough in adults. Clin Infect Dis. 1999;29:1239–1242. doi: 10.1086/313448. [DOI] [PubMed] [Google Scholar]
- 16.Cattaneo LA, Reed GW, Haase DH, Wills MJ, Edwards KM. The seroepidemiology of Bordetella pertussis infections: a study of persons ages 1-65 years. J Infect Dis. 1996;173:1256–1259. doi: 10.1093/infdis/173.5.1256. [DOI] [PubMed] [Google Scholar]
- 17.Miller E, Fleming DM, Ashworth LA, Mabbett DA, Vurdien JE, Elliott TS. Serological evidence of pertussis in patients presenting with cough in general practice in Birmingham. Commun Dis Public Health. 2000;3:132–134. [PubMed] [Google Scholar]
- 18.Mink CM, Cherry JD, Christenson P, Lewis K, Pineda E, Shlian D, et al. A search for Bordetella pertussis infection in university students. Clin Infect Dis. 1992;14:464–471. doi: 10.1093/clinids/14.2.464. [DOI] [PubMed] [Google Scholar]
- 19.Nennig ME, Shinefield HR, Edwards KM, Black SB, Fireman BH. Prevalence and incidence of adult pertussis in an urban population. JAMA. 1996;275:1672–1674. [PubMed] [Google Scholar]
- 20.Wright SW, Edwards KM, Decker MD, Zeldin MH. Pertussis infection in adults with persistent cough. JAMA. 1995;273:1044–1046. [PubMed] [Google Scholar]
- 21.Loeffelholz MJ, Thompson CJ, Long KS, Gilchrist MJ. Comparison of PCR, culture, and direct fluorescent-antibody testing for detection of Bordetella pertussis. J Clin Microbiol. 1999;37:2872–2876. doi: 10.1128/jcm.37.9.2872-2876.1999. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.van Boven M, de Melker HE, Schellekens JF, Kretzschmar M. Waning immunity and sub-clinical infection in an epidemic model: implications for pertussis in The Netherlands. Math Biosci. 2000;164:161–182. doi: 10.1016/s0025-5564(00)00009-2. [DOI] [PubMed] [Google Scholar]
- 23.Wendelboe AM, Van Rie A, Salmaso S, Englund JA. Duration of immunity against pertussis after natural infection or vaccination. Pediatr Infect Dis J. 2005;24(5 Suppl):S58–S61. doi: 10.1097/01.inf.0000160914.59160.41. [DOI] [PubMed] [Google Scholar]
- 24.Sentinal surveillance systems for communicable infectious diseases [Internet] Cheongwon: Korean Centers for Disease Control and Prevention; [cited 2011 Oct 1]. Korean Centers for Disease Control and Prevention. Available from http://www.cdc.go.kr. [Google Scholar]
- 25.Park WB, Park SW, Kim HB, Kim EC, Oh M, Choe KW. Pertussis in adults with persistent cough in South Korea. Eur J Clin Microbiol Infect Dis. 2005;24:156–158. doi: 10.1007/s10096-005-1277-y. [DOI] [PubMed] [Google Scholar]
- 26.Yaari E, Yafe-Zimerman Y, Schwartz SB, Slater PE, Shvartzman P, Andoren N, et al. Clinical manifestations of Bordetella pertussis infection in immunized children and young adults. Chest. 1999;115:1254–1258. doi: 10.1378/chest.115.5.1254. [DOI] [PubMed] [Google Scholar]
- 27.Strebel P, Nordin J, Edwards K, Hunt J, Besser J, Burns S, et al. Population-based incidence of pertussis among adolescents and adults, Minnesota, 1995-1996. J Infect Dis. 2001;183:1353–1359. doi: 10.1086/319853. [DOI] [PubMed] [Google Scholar]
- 28.Lee JJ, Yang JH, Hwang IS, Chun BY, Kam S, Lee KS, et al. The BCG, DTaP and IPV vaccination rate and the proportion of vaccination in the public health centers: demonstration project for expansion of national immunization program coverage in Deagu Metropolitan City. J Korean Soc Matern Child Health. 2007;11:33–43. [Google Scholar]