Abstract
Objectives. We assessed the effect of a telemedicine model providing medical abortion on service delivery in a clinic system in Iowa.
Methods. We reviewed Iowa vital statistic data and billing data from the clinic system for all abortion encounters during the 2 years prior to and after the introduction of telemedicine in June 2008 (n = 17 956 encounters). We calculated the distance from the patient’s residential zip code to the clinic and to the closest clinic providing surgical abortion.
Results. The abortion rate decreased in Iowa after telemedicine introduction, and the proportion of abortions in the clinics that were medical increased from 46% to 54%. After telemedicine was introduced, and with adjustment for other factors, clinic patients had increased odds of obtaining both medical abortion and abortion before 13 weeks’ gestation. Although distance traveled to the clinic decreased only slightly, women living farther than 50 miles from the nearest clinic offering surgical abortion were more likely to obtain an abortion after telemedicine introduction.
Conclusions. Telemedicine could improve access to medical abortion, especially for women living in remote areas, and reduce second-trimester abortion.
Medical abortion involves the use of medication to induce an abortion nonsurgically, and the regimen used most commonly in the United States involves oral mifepristone followed by misoprostol administered vaginally, orally, buccally, or sublingually.1 The mifepristone–misoprostol regimen is highly effective up to 9 weeks’ gestation and has been found to be very safe.2,3 Studies in the United States and elsewhere have found that women are very satisfied with this abortion method, and some women prefer it to vacuum aspiration.4,5 Medical abortion is not a surgical procedure and can be offered by nonphysician clinicians or by physicians who do not perform surgical abortion.6 However, US clinicians outside of abortion clinics do not appear to have adopted the technology in large numbers. An analysis of data from 2007 found that almost all medical abortion–only providers were located within 50 miles of a large-volume surgical abortion provider.7
One factor limiting the uptake of medical abortion is the restriction that most states impose regarding who can provide the service. As of 2009, only 15 states allowed advanced practice clinicians to provide medical abortion; the remainder required that a physician provide the service.8 Iowa is one such state where a physician must provide medical abortion.
Telemedicine is the delivery of health care services at a distance through information and communication technology. A recent systematic review of economic analyses of telemedicine services found that this care model was cost effective for a range of services.9 In June 2008, Planned Parenthood of the Heartland in Iowa launched a telemedicine program to allow physicians to provide medical abortion to patients at clinic sites not staffed by a physician to improve access to early abortion and reduce physician travel to outlying clinics. Prior to introducing telemedicine, the network had 17 clinic sites. Two clinics had an on-site physician and offered both medical and surgical abortion, 2 sites offered surgical and medical abortion when a physician traveled there, and 2 additional sites offered only medical abortion when the physician traveled there. The remaining 11 clinics did not provide abortions. A recently published cohort study found that the telemedicine model provided by this clinic system was as effective as a model involving an in-person visit with a physician; telemedicine was also found to be highly acceptable to women, with a low rate of adverse events.10
We examined how the clinic system’s service delivery patterns changed after the introduction of telemedicine. In particular, we asked whether the proportion of abortions that were medical abortion and second-trimester abortion changed, as well as whether there were changes in the geographical patterns of service delivery.
METHODS
Telemedicine was launched on June 25, 2008, by Planned Parenthood of the Heartland and phased in over the following 21 months. By June 30, 2010, abortion care was being provided at 15 clinic sites. The 4 original surgical abortion sites remained the only sites providing surgical abortion at the end of this period, and all new abortion sites provided medical abortion through telemedicine. The sites to which the physician previously traveled to offer medical abortion began offering telemedicine services after the launch. The telemedicine model used in this clinic system was previously described.10 For our analysis, we compared data between 2 periods: 2 years prior to telemedicine introduction versus 2 years after.
We used vital statistics records to analyze birth, medical abortion, and surgical abortion data for the state of Iowa during July 2006 to June 2008 versus July 2008 to June 2010.11 For each period, we calculated the total number of births, abortions, medical abortions, and surgical abortions; the abortion ratio per 100 live births; and the abortion rate per 1000 females aged 15 to 44 years. To calculate the abortion rate for each period, we averaged the annual number of females aged 15 to 44 years. We performed a χ2 test to assess statistical differences in the proportion of abortions that were medical versus surgical before and after telemedicine introduction.
We performed a more in-depth analysis on de-identified billing data from all abortion encounters at Planned Parenthood of the Heartland clinics in Iowa between June 20, 2006, and June 30, 2010, (n = 17 956 encounters). This clinic network provided 74% of all abortions in Iowa in 2008.11 The data set comprised the following variables: date of service; clinic site where abortion was performed; patient age, race and ethnicity, education level, and residential zip code; whether the patient received financial assistance at the clinic to pay for her abortion; gestational age (for surgical abortion gestational age was recorded as ≤ 13 weeks' or > 13 weeks' gestation; by definition, medical abortion was performed at ≤ 9 weeks' gestation); and type of abortion (medical vs surgical).
We analyzed these data to determine the effect of telemedicine introduction on the following outcomes: the proportion of all abortions that were medical abortion (vs surgical abortion), the proportion of all abortions performed at ≤ 13 weeks (vs abortion > 13 weeks), distance traveled to clinic (approximated with straight-line calculations between clinic and patient residential zip codes), and distance of patient to the nearest clinic that offered surgical abortion, to assess whether women came from more remote areas of the state following the introduction of telemedicine. Women whose reported residential zip code was more than 500 miles from the clinic were excluded from the distance analyses because the location data for these women was assumed to be permanent residence information, such as parents’ home address, rather than the woman’s local address. After we excluded these cases, the final data set for the geographical analyses comprised 17 801 abortion encounters.
We conducted χ2 analyses to compare patient characteristics before and after telemedicine introduction. To evaluate the impact of telemedicine on our outcomes of interest, we used the t test and linear regression for continuous distance variables and logistic regression for categorical variables (medical abortion provision, abortion ≤ 13 weeks’ gestation, and categorical distance variables). We conducted additional pre–post distance analyses among medical abortion patients only. The predictor variable in each model was telemedicine introduction (1 = patient attended a clinic after telemedicine introduction; 0 = patient attended a clinic before). All sociodemographic covariates from the clinic billing data set were selected a priori in the multivariate models. We performed all statistical tests with Stata 12 (StataCorp LP, College Station, TX).
We matched patients’ residential zip codes to polygons in US Census shape files for Iowa and surrounding states. For each zip code, we calculated Z (number of abortion patients before − number of abortion patients after telemedicine introduction). We used the centroids of zip code areas as approximate (X,Y) = (longitude, latitude) locations for patients to produce a set {X,Y,Z} of locations and changes, with zip codes as the unit of observation. We then smoothed this {(X,Y,Z)} map through inverse-distance weighting with the krige() function in R’s gstat package (R Foundation for Statistical Computing, Vienna, Austria) to find spatial clusters of increased and decreased numbers of abortion cases after the introduction of telemedicine. We performed similar analyses for medical abortions and surgical abortions separately.
RESULTS
Table 1 shows the comparative data on births and abortions for the state of Iowa for the 2-year periods before and after telemedicine was introduced at Planned Parenthood of the Heartland. The number of both births and abortions declined in the state between these periods; however, the reduction in abortions was larger, with a decrease in both abortion ratio and abortion rate for the state. The proportion of medical abortions among all abortions increased significantly, from 33.4% to 45.3% (P < .001).
TABLE 1—
Births and Abortions in Iowa Before and After Introduction of Telemedicine Service at Planned Parenthood Clinics in Iowa in June 2008
| Variable | July 2006–June 2008 | July 2008–June 2010 |
| Average female population aged 15–44 y, no. | 583 180 | 577 876 |
| Births, no. | 81 501 | 79 198 |
| Abortions, no. | 13 264 | 11 762 |
| Abortion type, no. (%) | ||
| Medical | 4432 (33.4) | 5326 (45.3)* |
| Surgical | 8832 (66.6) | 6436 (54.7) |
| Abortions/100 births | 16.3 | 14.9 |
| Average annual abortions/1000 females aged 15–44 y | 11.4 | 10.2 |
*P < .001. P values were determined by the χ2 test.
The Planned Parenthood of the Heartland clinic system recorded 8902 abortion encounters during the 2 years before and 9054 abortion encounters during the 2 years after telemedicine was introduced. Demographic characteristics of the Planned Parenthood patients are shown in Table 2. Age and race/ethnicity of abortion patients did not differ in the 2 periods; however, we observed slight differences by education level (P < .001). More women received financial assistance during the period after telemedicine was introduced because a new program was started in 2008 to provide such support.12
TABLE 2—
Abortion Patient Characteristics and Service Delivery Statistics From Planned Parenthood of the Heartland (Iowa) Before and After Introduction of Telemedicine Service in June 2008
| Variable | July 2006–June 2008 (n = 8902), No. (%), Mean, or Median | July 2008–June 2010 (n = 9054), No. (%), Mean, or Median | P |
| Patient characteristics | |||
| Age, y | .53 | ||
| 9–20 | 2225 (25) | 2331 (26) | |
| 21–24 | 2505 (28) | 2475 (27) | |
| 25–29 | 2085 (23) | 2104 (23) | |
| 30–49 | 2087 (23) | 2144 (24) | |
| Race/ethnicity | .07 | ||
| Non-Hispanic White | 6505 (73) | 6583 (73) | |
| Non-Hispanic Black | 826 (9) | 922 (10) | |
| Hispanic | 729 (8) | 725 (8) | |
| Asian/Pacific Islander | 347 (4) | 323 (4) | |
| > 1 race | 144 (2) | 178 (2) | |
| Other racea or unknown race | 351 (4) | 323 (4) | |
| Highest grade of education completed | <.001 | ||
| < 9 | 177 (2) | 166 (2) | |
| 9–12 | 4541 (51) | 4711 (52) | |
| ≥ 13 | 3298 (37) | 2827 (31) | |
| Unknown | 886 (10) | 1350 (15) | |
| Received financial assistance to pay for abortion | 903 (10) | 4506 (50) | <.001 |
| Service delivery statistics | |||
| Abortion type | <.001 | ||
| Medical | 4095 (46) | 4850 (54) | |
| Surgical, ≤ 13 wk | 4464 (50) | 3886 (43) | |
| Surgical, > 13 wk | 343 (3.9) | 318 (3.5) | |
| Distance traveled by patient from residence to clinic,b miles | |||
| Mean | 33.2 | 30.7 | <.001 |
| Median | 12.6 | 12.6 | |
| 0–25 | 5271 (60) | 5470 (61) | .01 |
| 25.1–50 | 1353 (15) | 1454 (16) | |
| > 50 | 2184 (25) | 2069 (23) | |
| Distance between residential zip code of patient and nearest clinic providing surgical abortion,b miles | |||
| Mean | 29.9 | 31.6 | .002 |
| Median | 12.6 | 16.7 | |
| 0–25 | 5287 (60) | 5079 (56) | <.001 |
| 25.1–50 | 1437 (16) | 1532 (17) | |
| > 50 | 2084 (24) | 2382 (26) | |
American Indian, Alaskan Native, and other.
Patients who traveled < 500 miles only (n = 17 801; before, n = 8808; after, n = 8993).
The proportion of abortions that were medical abortion at Planned Parenthood of the Heartland clinics increased from 46% to 54% after telemedicine introduction, and the proportion of abortions performed after 13 weeks’ gestation decreased slightly from 3.9% to 3.5% (Table 2). After we controlled for financial assistance, age, race/ethnicity, and education level, we found that women obtaining services after the introduction of telemedicine had a 51% greater likelihood of having a medical abortion (adjusted odds ratio [AOR] = 1.51; 95% confidence interval [CI] = 1.41, 1.61). With adjustment for the same covariates, women obtaining services after telemedicine introduction had a 46% greater likelihood of having an abortion at or before 13 weeks’ gestation (AOR = 1.46; 95% CI = 1.22, 1.75).
The average distance that women traveled from their home to the clinic decreased slightly, from 33.2 miles before telemedicine introduction to 30.7 miles after (P < .001). The proportion of patients who traveled more than 50 miles to the clinic also declined slightly, from 25% to 23% (Table 2). The median distance traveled did not change. In regression analysis, women obtaining services after the introduction of telemedicine had a 3.16-mile decrease in average distance traveled to the clinic, after adjustment for sociodemographic factors (95% CI = −4.51, −1.80). Women presenting after telemedicine introduction also had a 12% reduced likelihood of traveling more than 50 miles to the clinic, after adjustment for sociodemographic factors (AOR = 0.88; 95% CI = 0.81, 0.95). We obtained similar results when we restricted this analysis to medical abortion patients.
Abortion access for women living in more remote parts of the state increased with telemedicine: the proportion of patients who lived more than 25 miles and more than 50 miles from a surgical abortion clinic increased from 40% to 44% and from 24% to 26%, respectively (P < .001; Table 2). After adjustment for sociodemographic factors, patients were 12% more likely to reside more than 50 miles from a clinic that provided surgical abortion after than before telemedicine was introduced (AOR = 1.12; 95% CI = 1.03, 1.20). When we restricted this analysis to medical abortion patients (n = 8860) and controlled for sociodemographic factors, we found that after telemedicine introduction, medical abortion patients had a 16% greater likelihood of residing more than 50 miles from a clinic providing surgical abortion (AOR = 1.16; 95% CI = 1.05, 1.28).
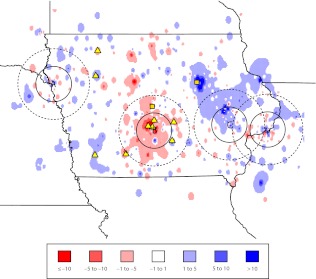
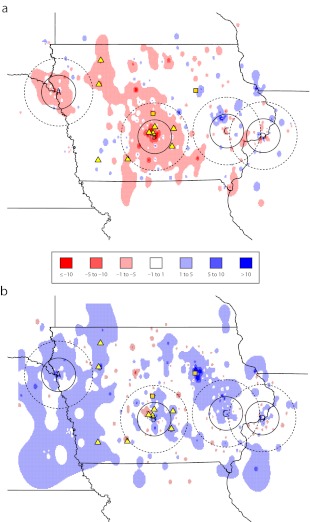
Figure 1 shows the smoothed mapping results for the changes in the number of abortions after telemedicine introduction according to patient residential zip code, and Figure 2 shows the same mapping results for surgical abortions (panel a) and for medical abortions (panel b). The data showed a reduction in the number of abortions among women residing around Des Moines and an increase in the number of abortions performed on women living in the western and eastern portions of the state (Figure 1). The number of surgical abortions decreased among women residing throughout the state, but especially for those living in the central and western portions of the state (Figure 2a). The number of medical abortions increased among women residing throughout the state, but especially among residents of the western and eastern portions of the state. Most of the increase in the number of medical abortions after telemedicine introduction occurred among women living more than 50 miles from one of the surgical abortion clinics, especially in more remote parts of Iowa, as well as in eastern Nebraska and northwest Illinois. In most cases, the increases occurred in areas surrounding telemedicine sites. The data showed scattered areas where fewer women obtained medical abortions (shown in red), but no clear pattern emerged.
FIGURE 1—
Change in total number of abortions by residential zip code for 2 years before (June 20, 2006–June 24, 2008) and after (June 25, 2008–June 30, 2010) telemedicine was introduced in Planned Parenthood of the Heartland clinics in Iowa.
Note. Mapping results are smoothed. A, B, C, and D = clinics that provide surgical abortion (solid and broken rings indicate distances of 25 and 50 miles, respectively). Yellow squares = clinics that intermittently offered medical abortion before telemedicine was introduced when a doctor traveled to the clinic and later became telemedicine sites. Yellow triangles = clinics that began offering medical abortion after telemedicine was introduced.
FIGURE 2—
Change in number of abortions by residential zip code for 2 years before (June 20, 2006–June 24, 2008) and after (June 25, 2008–June 30, 2010) telemedicine was introduced in Planned Parenthood of the Heartland clinics in Iowa that were (a) surgical and (b) medical.
Note. Mapping results are smoothed. A, B, C, and D = clinics that provide surgical abortion (solid and broken rings indicate distances of 25 and 50 miles, respectively). Yellow squares = clinics that intermittently offered medical abortion before telemedicine was introduced when a doctor traveled to the clinic and later became telemedicine sites. Yellow triangles = clinics that began offering medical abortion after telemedicine was introduced.
DISCUSSION
After the introduction of telemedicine in a Planned Parenthood clinic system, the proportion of medical abortions performed increased in both the system and the state of Iowa. After adjustment for other factors, including financial assistance, we found that women presenting after telemedicine introduction were significantly more likely to receive a medical abortion. This finding is not surprising because the clinic sites that began offering abortion care after telemedicine introduction only provided medical abortion. Although the increase in medical abortion might be attributable to a time trend unrelated to telemedicine introduction, it is unlikely that the observed increase in medical abortion from 46% to 54% of all Planned Parenthood of the Heartland abortions would have occurred without telemedicine. In a national census of abortion providers, the proportion of nonhospital abortions that were medical abortions only increased from 14% to 17% between 2005 and 2008.13 It is particularly interesting that the increase in medical abortion occurred in the context of decreasing abortion numbers statewide, reflecting an overall reduction in the number of surgical abortions.
Although the magnitude of the reduction was small, we also found that women were less likely to have a second-trimester abortion in this clinic system after telemedicine introduction. Previous research found that logistical factors, such as difficulty finding a provider, distance from the clinic, and difficulty with transportation, were reported significantly more frequently by women seeking second-trimester abortion than by those seeking first-trimester abortion.14 Telemedicine may reduce some of these barriers to earlier abortion. In light of the evidence documenting the higher risk of complications and mortality associated with second-trimester than with early first-trimester abortion,15 the effect of telemedicine on gestational age at time of abortion should be evaluated over a longer period and in other settings to confirm our findings. It would be interesting to evaluate whether telemedicine availability also reduces surgical abortion at 9 to 13 weeks' gestation; unfortunately our data set did not allow us to explore this hypothesis.
Access to care has been defined as the degree of fit between patients and the health care system in 5 specific areas: availability, accessibility, accommodation, affordability, and acceptability.16 In this clinic system, availability of abortion services certainly increased after telemedicine introduction, because the number of clinics providing abortion care increased. Accessibility is defined as the relationship between the location of supply and the location of patients,16 and this also clearly increased, as can be seen in Figures 1 and 2. The increase in use of abortion services—especially medical abortion—among women living in more remote parts of Iowa, which we defined as living more than 50 miles from a clinic offering surgical abortion, also suggests that accessibility improved.
Accommodation is the relationship between the way supply resources are organized to accept patients and the patients’ ability to accommodate to these factors and their perception of their appropriateness.16 One measure of accommodation is satisfaction with clinic wait time, which was shown to be significantly higher among telemedicine patients in this system.10 Affordability was not specifically measured in our study, although it is possible that women’s out-of-pocket expenditures related to time away from work, child care, and travel costs may be reduced with telemedicine abortion provision. The final dimension of access—acceptability—has been shown to be significantly higher among telemedicine patients for some measures.10 Taken together, our analyses suggest that access to abortion care improved after the introduction of telemedicine in this clinic system. They also highlight the need to examine access from a variety of vantage points, including that of patients, rather than simply considering the number and location of service delivery points.
In our geographic analysis, we found an overall reduction in the number of abortions in the central part of the state around Des Moines. The reasons for this decline are not clear. One hypothesis is that a promotional campaign increased uptake of contraception, including long-acting methods, in this area. The reduction in births in Iowa during the same period also supports this hypothesis. In 2009, the Iowa Initiative to Reduce Unintended Pregnancies began several community- and clinic-focused interventions aimed at improving contraceptive use.17 These interventions may have been particularly effective in urban areas of the state, although additional research would be required to confirm this hypothesis.
Despite this apparent improvement in access to abortion care, we observed a relatively small reduction in the distance women traveled from their home to the clinic. Although this finding may seem surprising, distance to the clinic is only one of several factors women consider when choosing where to obtain the service.10 Some women may choose to travel farther to get an appointment sooner, and abortion stigma may lead some women in a small community to go to a clinic in another town to avoid being seen by someone they know. Previous research in Iowa found that travel time was not a predictor of women’s preference for obtaining abortion services with their regular physician; some women preferred not to obtain care with their regular physician because of concerns about privacy and confidentiality.18 The decrease in abortion that we observed in the Des Moines area after telemedicine introduction also likely affected distance traveled, because this population lives close to several of the abortion clinics. It will be interesting to see whether distance traveled by patients in this clinic system continues to decrease in the coming years.
Our study had several limitations. Because it was an observational study, we cannot infer causality from our results, and factors other than telemedicine and the variables we were able to control for may have contributed to our findings. It would be challenging to study the impact of telemedicine with a cluster-randomized design because the clusters would have to be sufficiently far apart to be able to assess distance traveled and to avoid contamination. Another limitation is that we only examined the first 2 years after telemedicine introduction. The telemedicine sites that began offering services later in the study period had small volumes of patients, and these numbers might increase over time. In addition, our findings are specific to the service delivery model implemented in this clinic system and cannot be generalized to other models in other settings. Our study also had several strengths, including the ability to analyze the entire universe of abortion encounters in this clinic system over a 4-year period and the novel spatial mapping techniques we used to determine access to abortion care.
Access to abortion services remains limited in the United States, with 35% of women of reproductive age living in counties without an abortion provider.13 Telemedicine provision of medical abortion has been shown to be safe, effective, and acceptable to women.10 Our results suggest that it promotes earlier abortion and improves access to care for rural women. Recent legislation to ban telemedicine abortion19 may adversely affect public health by preventing women from accessing abortion earlier in pregnancy, when it is safer.15
Acknowledgments
The study was funded by a grant from an anonymous donor.
Note. The findings and conclusions in this article are those of the authors and do not necessarily represent the views of Planned Parenthood Federation of America, Inc.
Human Participant Protection
The study was approved by the Allendale investigational review board.
References
- 1.Wiegerinck MM, Jones HE, O’Connell K, Lichtenberg ES, Paul M, Westhoff CL. Medical abortion practices: a survey of National Abortion Federation members in the United States. Contraception. 2008;78(6):486–491 [DOI] [PubMed] [Google Scholar]
- 2.Kulier R, Kapp N, Gülmezoglu AM, Hofmeyr GJ, Cheng L, Campana A. Medical methods for first trimester abortion. Cochrane Database Syst Rev. 2011;(11):CD002855. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Fjerstad M, Trussell J, Sivin I, Lichtenberg ES, Cullins V. Rates of serious infection after changes in regimens for medical abortion. N Engl J Med. 2009;361(2):145–151 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Winikoff B, Ellertson C, Elul B, Sivin I. Acceptability and feasibility of early pregnancy termination by mifepristone-misoprostol. Results of a large multicenter trial in the United States. Mifepristone Clinical Trials Group. Arch Fam Med. 1998;7(4):360–366 [DOI] [PubMed] [Google Scholar]
- 5.Ho PC. Women’s perceptions on medical abortion. Contraception. 2006;74(1):11–15 [DOI] [PubMed] [Google Scholar]
- 6.Yarnall J, Swica Y, Winikoff B. Non-physician clinicians can safely provide first trimester medical abortion. Reprod Health Matters. 2009;17(33):61–69 [DOI] [PubMed] [Google Scholar]
- 7.Finer LB, Wei J. Effect of mifepristone on abortion access in the United States. Obstet Gynecol. 2009;114(3):623–630 [DOI] [PubMed] [Google Scholar]
- 8.Berer M. Provision of abortion by mid-level providers: international policy, practice and perspectives. Bull World Health Organ. 2009;87(1):58–63 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Wade VA, Karnon J, Elshaug AG, Hiller JE. A systematic review of economic analyses of telehealth services using real time video communication. BMC Health Serv Res. 2010;10:233. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Grossman D, Grindlay K, Buchacker T, Lane K, Blanchard K. Effectiveness and acceptability of medical abortion provided through telemedicine. Obstet Gynecol. 2011;118(2 pt 1):296–303 [DOI] [PubMed] [Google Scholar]
- 11.Iowa Department of Public Health, Bureau of Vital Statistics Vital statistics of Iowa. Available at: http://www.idph.state.ia.us/apl/vital_stats.asp. Accessed May 24, 2012
- 12.CAIR Project Fast facts about abortion funding. Available at: http://www.prochoicewashington.org/assets/files/fastfacts.pdf. Accessed April 4, 2012
- 13.Jones RK, Kooistra K. Abortion incidence and access to services in the United States, 2008. Perspect Sex Reprod Health. 2011;43(1):41–50 [DOI] [PubMed] [Google Scholar]
- 14.Drey EA, Foster DG, Jackson RA, Lee SJ, Cardenas LH, Darney PD. Risk factors associated with presenting for abortion in the second trimester. Obstet Gynecol. 2006;107(1):128–135 [DOI] [PubMed] [Google Scholar]
- 15.Bartlett LA, Berg CJ, Shulman HBet al. Risk factors for legal induced abortion-related mortality in the United States. Obstet Gynecol. 2004;103(4):729–737 [DOI] [PubMed] [Google Scholar]
- 16.Penchansky R, Thomas JW. The concept of access: definition and relationship to consumer satisfaction. Med Care. 1981;19(2):127–140 [DOI] [PubMed] [Google Scholar]
- 17. The Iowa Initiative to Reduce Unintended Pregnancies. Available at: http://www.iowainitiative.org/research_program/research_program.php. Accessed April 4, 2012.
- 18.Shochet T, Trussell J. Determinants of demand: method selection and provider preference among US women seeking abortion services. Contraception. 2008;77(6):397–404 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Gold RB, Nash E. Troubling trend: more states hostile to abortion rights as middle ground shrinks. Guttmacher Pol Rev. 2012;15(1):14–19 [Google Scholar]