One of the concerns often raised about genetic testing is the possibility that a positive result (or even disclosing that the test has been taken) may result in difficulty in obtaining life assurance. Currently the UK insurance industry has declared a moratorium on requiring genetic tests from applicants,1 but since DNA based tests offer a definitive, highly specific diagnosis they are likely eventually to replace less specific clinical diagnostic criteria for many inherited disorders. Early, presymptomatic treatment may increase life expectancy by preventing or reducing the risk of developing the disease or associated complications. However, if life assurance policy premiums do not adequately reflect the reduction in mortality with treatment relatives of affected probands may be deterred from being tested. We examined how life assurance companies have responded to the improvement in the prognosis of heterozygous familial hypercholesterolaemia with statin treatment.2
Familial hypercholesterolaemia is an autosomal dominant disorder, inherited on average by one in two children of an affected parent. The prevalence in the United Kingdom is about 1:500, but at least three quarters of cases remain undiagnosed.3 It is usually caused by mutations in the gene for the low density lipoprotein (LDL) receptor that result in accumulation of plasma cholesterol and substantially increased coronary mortality. Without effective treatment the cumulative risk of a coronary event is at least 50% in men and 30% in women by the age of 60 years.4 With statin treatment, however, the standardised mortality ratio for coronary heart disease for such patients aged 20-59 years has more than halved over the past decade.2
Participants, methods, and results
We conducted a survey of 41 life assurance companies in 19905 and repeated it in 2002 by sending the same questionnaire to 26 companies still underwriting term life assurance. They were asked to assess a fictional proposal for a 20 year policy (paying benefit only on death) by applying an excess mortality rating defined as the percentage increase over the assumed rate of mortality. In the follow up survey companies were asked to assess the rating before and after statin treatment. The applicant was a normotensive (120/80 mm Hg), non-smoking, 30 year old man taking no medication, with a body mass index of 22.1 kg/m2 and a normal resting electrocardiogram, whose father had had a non-fatal myocardial infarction aged 45 years. He had no other family history of heart disease, other medical history of note, or tendon xanthomata on examination. The results of the lipid profile (mmol/l) were total cholesterol 11.4, high density lipoprotein (HDL) cholesterol 1.7, triglycerides 1.3, and calculated LDL cholesterol 9.1; and the presumptive diagnosis was familial hypercholesterolaemia. On treatment with atorvastatin 80 mg daily his total cholesterol concentration was 6.2 mmol/l (compared with 10.7 mmol/l on cholestyramine prescribed in 1990).
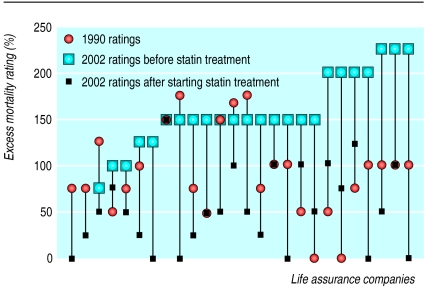
The figure shows the excess mortality ratings applied. Because two companies would assess proposals only from patients receiving statin treatment statistical comparisons were restricted to 24 companies. The mean excess rating increased from 89% (SD 52) in 1990 to 158% (SD 40) in 2002 (difference 69%, 95% confidence interval 41 to 97; P < 0.000, paired t test), but fell to 56% (SD 43) on treatment (102%, 79 to 126; P < 0.000), which was 33% lower (5 to 61; P = 0.022) than the original rating in 1990.
Figure 1.
Percentage excess mortality ratings applied by life assurance companies in 1990 and 2002, before and after starting statin treatment
Comment
The increase in mortality rating in the second survey, together with the substantial reduction in the excess applied to patients taking statins show that underwriters now assess risk more realistically and recognise that the prognosis for familial hypercholesterolaemia has improved with more effective treatment.2 Nevertheless variability in the rating applied was considerable, and patients could usefully be advised to shop around for the most competitive premium. The results of the survey, however, are reassuring and should encourage relatives of probands to be tested rather than being deterred by concerns about life assurance.
We thank the life assurance companies for participating in the study.
Contributors: HAWN and DM designed the study, TH conducted the survey, HAWN undertook the analysis, SEH and HAWN wrote the paper. All authors participated in the interpretation and critical revision of the paper. HAWN is the guarantor.
Funding: This work was supported by a grant from the British Heart Foundation (PG2000/015) and was carried out in part with support from the Department of Health and the Department of Trade and Industry for the IDEAS Genetics Knowledge Park.
Competing interests: None declared.
References
- 1.Mayor S. UK insurers agree five-year ban on using genetic tests. BMJ 2001;323: 1021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Scientific Steering Committee on behalf of the Simon Broome Register Group. Mortality in treated heterozygous familial hypercholesterolaemia: implications for clinical management. Atherosclerosis 1999;142: 105-12. [PubMed] [Google Scholar]
- 3.Neil HAW, Hammond T, Huxley R, Matthews DR, Humphries SE. Extent of underdiagnosis of familial hypercholesterolaemia in routine practice: prospective registry study. BMJ 2000;321: 148. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Stone NJ, Levy RI, Fredrickson DS, Verter J. Coronary artery disease in 116 kindred with familial type II hyperlipoproteinaemia. Circulation 1974;49: 476-488. [DOI] [PubMed] [Google Scholar]
- 5.Neil HAW, Mant D. Cholesterol screening and life assurance. BMJ 1991;302: 891-3. [DOI] [PMC free article] [PubMed] [Google Scholar]