Abstract
Mature outcomes from adjuvant endocrine therapy trials in estrogen receptor-positive breast cancer have enabled comparisons with neoadjuvant clinical trials that have parallel randomizations of treatment in terms of the response of disseminated disease versus the local response within the breast. Imprecise end points, such as ‘clinical response’, have produced inconsistent results regarding the relationship between neoadjuvant and adjuvant endocrine therapy outcomes. However, the proliferation marker Ki-67, measured during neoadjuvant treatment, has predicted accurately and consistently the results of much larger studies in the adjuvant setting. In this Review, we summarize these trials and discuss the implications for the design of future adjuvant endocrine therapy trials. We conclude that there is sufficient evidence supporting the view that the degree of Ki-67 suppression is a reliable short-term surrogate for the adjuvant potential of endocrine drugs, at least in postmenopausal women. We propose that adjuvant endocrine therapy trials should only be conducted once adequately-powered neoadjuvant studies have indicated superior Ki-67 suppression in patients receiving experimental endocrine treatment versus the standard treatment.
Introduction
Estrogen receptor-positive (ER+) breast cancer is a heterogeneous disease and, despite its reputation for a relatively benign course, most breast cancer-related deaths occur within this subset.1 Because the annual risk of relapse is low but risk persists over several decades and the differences in efficacy between endocrine therapy approaches are modest, the development of new adjuvant endocrine treatments requires protracted follow-up and very large sample sizes. Improvements in adjuvant therapy for ER+ breast cancer are, therefore, hard to demonstrate. 2–4 A surrogate end point biomarker that could examine reliably the potential efficacy of new endocrine treatments versus current standard treatments would be a significant advance that would promote the activation of adjuvant trials that are based on sound pharmacological superiority hypotheses and, therefore, are more likely to succeed.
As the efficacy of endocrine therapy in breast cancer relies largely on inducing cell-cycle arrest instead of on activation of apoptosis,5 it is logical to focus on proliferation as a relatively easy-to-measure biological end point as an assessment of the short-term effects of endocrine agents. The data from a number of studies comparing neoadjuvant and adjuvant endocrine treatments are now available (Table 1). These data may allow the proliferation biomarker Ki-67 to be recognized as a reliable surrogate, which would help to establish a paradigm whereby a positive neoadjuvant study based on Ki-67 data should be a mandatory prerequisite before adjuvant endocrine studies are carried out.
Table 1.
Clinical trials comparing endocrine agents conducted in the neoadjuvant and adjuvant settings
| Adjuvant trials |
Neoadjuvant trials (Ki-67 analysis) |
||
|---|---|---|---|
| Study (n) | Results (based on events) | Study (n with available Ki-67 data) |
Results (based on levels of Ki-67) |
| BIG 1-98 (8,010)16 | Letrozole > tamoxifen | P024 (185)13 | Letrozole > tamoxifen |
| ATAC (9,366)24 | Anastrozole > tamoxifen and anastrozole + tamoxifen | IMPACT (259)14 | Anastrozole > tamoxifen and anastrozole + tamoxifen |
| MA27 (7,576)28 | Anastrozole similar to exemestane | ACOSOG Z1031 (266*)29 | Anastrozole similar to exemestane |
| FACE trial (estimated 4,000)30 | Pending | ACOSOG Z1031 (266*)29 | Letrozole similar to anastrozole |
The number of patients with baseline and on-treatment Ki-67 values in the three-way comparison in the Z1031 trial were anastrozole, n = 86; exemestane, n = 91; and letrozole, n = 89. Abbreviation: > superior.
Ki-67 as a biomarker
First identified in the early 1980s by Gerdes et al.,6 the Ki-67 antigen is expressed during all cell-cycle phases except for G0, with levels peaking during mitosis. Although ASCO has yet to list Ki-67 as a required breast cancer biomarker for breast cancer management,7 the 2011 St Gallen International Expert Consensus meeting supported the use of a cutoff point of 14% of Ki-67 positive cells in the invasive portion of the tumor as a simple means to distinguish between the two ‘intrinsic’ subtypes of ER+ breast cancer: luminal A (better prognosis; <14% of Ki-67-positive cells) and luminal B (worse prognosis; >14% of Ki-67-positive cells).8,9 Resistance to the adoption of Ki-67 as a mandatory biomarker for clinical decision making in adjuvant therapy is largely due to the lack of a concerted effort to standardize the test,10,11 and not to a lack of evidence that Ki-67 is a prognostic factor in the setting of ER+ breast cancer.12 The focus of this Review, however, is not to discuss the status of baseline Ki-67 measurement in terms of its application as a routine clinical test, as this issue has been well covered by other publications,10 but rather as the basis for a centrally conducted and highly controlled pharmacodynamic assay that can be applied to ER+ breast cancer specimens accrued from patients who have been treated on neo-adjuvant endocrine therapy clinical trials. In this setting, the on-treatment levels of Ki-67 reflect the ability of the endocrine treatments to suppress proliferation.13,14 The decrease in levels of Ki-67 is rapid following treatment with either tamoxifen or an aromatase inhibitor, and the on-treatment levels at 2 weeks are already more prognostic than baseline levels.15 However, most of the data cited in this article are based on the levels of Ki-67 in biopsies obtained after 3–5 months of neoadjuvant endocrine treatment. We acknowledge that the optimal timing for when to measure the ‘on endocrine treatment’ Ki-67 value is an unsettled issue, partly because the patterns of Ki-67 response are very heterogeneous. Although most tumors exhibit a marked decrease in Ki-67 levels with endocrine treatment, some tumors exhibit a paradoxical increase in levels of Ki-67 from baseline and can even increase when the 2-week sample showed an initial decrease from baseline.5 Although our understanding of these patterns from a prognostic standpoint is incomplete, we propose that data from a Ki-67 value obtained from 3 to 5 months of treatment is a reasonable standard for clinical and research applications as the durability of the pharmacological effect is probably an important aspect of efficacy. However, further studies on the relationship between patient outcomes and the timing of the on-treatment biopsy are certainly warranted.
The BIG 1-98 and P024 trials
The Breast International Group (BIG) 1-9816 trial is a randomized, phase III, double-blind four-arm adjuvant study that compared letrozole and tamoxifen administered either as monotherapy or in sequence for 5 years in post-menopausal women with early-stage hormone receptor-positive breast cancer.16 From 1998 to 2003, 8,010 patients were enrolled, 4,922 of whom received monotherapy for 5 years (letrozole arm: n = 2,463; tamoxifen arm: n = 2,459). Data from this study were reported 13 years after trial initiation with a median follow-up of 8.1 years (range 0–12.4 years). The letrozole arm was associated with improved disease-free survival (DFS; hazard ratio [HR] = 0.82; 95% CI = 0.74–0.92; P = 0.0002) and a reduced risk of death (HR = 0.79; 95% CI = 0.69–0.90; P = 0.0006) compared with the tamoxifen arm.17
Nearly a decade before letrozole was finally shown to improve survival in breast cancer,17 a prescient study with 337 patients had already revealed the superior efficacy of letrozole versus tamoxifen against primary breast cancer in a neoadjuvant protocol.13 The P024 trial was a randomized, double-blind, multicenter study that compared the efficacy of 4 months of treatment with letrozole or tamoxifen as neoadjuvant therapy for postmenopausal women with locally advanced-stage breast cancer (clinical stage II or III) positive for ER and/or progesterone receptor (PR).18 None of the patients was considered to be a candidate for breast-conserving surgery at baseline, and 14% of the patients were considered inoperable. Letrozole was found to be superior to tamoxifen in terms of clinical response rate (55% versus 36%, P = 0.001), ultrasound response rate (35% versus 25%, P = 0.042; Table 1), mammographic response rate (34% versus 16%, P = 0.001) and breast conservation rate (45% versus 35%, P = 0.022).18 These results were even more marked in the patients included in the ER+ subset classified by the central testing laboratory.19 In addition to improved clinical response, the superiority of letrozole was further demonstrated by a higher treatment-induced reduction of the levels of Ki-67 in the tumor at surgery (87% reduction in the letrozole arm versus 75% in the tamoxifen arm; analysis of covariance P = 0.0009) based on the 185 specimens with available data on Ki-67.13 Thus, the P024 trial13 first demonstrated the potential of small neo-adjuvant protocols to identify new adjuvant endocrine agents that would ultimately prove superior to a previous standard therapy, once follow-up had been achieved in a sufficiently large cohort of patients. This study also demonstrated interactions between HER2 status and Ki-67, revealing that HER2 amplification reduces the anti-proliferative effects of endocrine drugs.20 Thus, a relatively unexplored area of research is the use of Ki-67 as a discovery tool to identify the mechanisms of resistance to endocrine drugs.
The P024 trial13 also contributed to the observation that favorable short-term response to endocrine therapy is prognostic of superior long-term survival; an observation that had not been demonstrated before although there were hints from a UK study that, a decade earlier, had assessed tamoxifen alone as primary treatment.21 A prognostic model was developed within the P024 trial database based on biomarker and routine pathological staging of the tumor excision specimen after neoadjuvant endocrine therapy, with the objective of developing guidance for further therapeutic decision making after the completion of neoadjuvant endocrine treatment.22 At a median follow-up of 61.2 months, low levels of Ki-67 in the biopsy were significantly associated with relapse-free survival (RFS; HR = 1.4, per natural log increase in the Ki67 value 95% CI = 1.2–1.6 P <0.001), and breast cancer-specific survival (HR = 1.4, 95% CI = 1.1–1.7; P = 0.009).22 In addition to Ki-67, pathological tumor size (T1 or T2 versus T3 or T4), node status (positive or negative) and the ER status (positive Allred score 3–8 versus negative Allred score 0–2) of the biopsy were determined to also have independent prognostic value for relapse and death after relapse (Table 2).22 A prognostic score—the preoperative endocrine prognostic index (PEPI), which weights each of these factors according to their associated hazard ratios—was developed (Table 3). PEPI was then validated in an independent data set from the IMPACT trial.22 No relapses were recorded in either trial in patients with tumors classified as T1, N0 and with a PEPI score of 0 (residual tumor with a Ki-67 level ≤2.7% with maintained ER expression) or in the rare patient with a pathologic complete response.22 Although the PEPI score was primarily developed as a prognostic tool, it is now being applied as the primary end point in a neoadjuvant endocrine therapy protocol to be executed by the US cooperative groups. This makes sense, as a more-effective endocrine agent would be expected to achieve higher PEPI-0 rates through greater anti-proliferative effects combined with greater pathological tumor down-staging. 18 Regarding the use of PEPI score in clinical practice, this remains subject to a number of caveats concerning the analytical consistency of Ki-67 analysis that have been recently reviewed by the International Ki-67 Working Group.23 Unresolved issues include optimal assay conditions, reagents and scoring approaches.
Table 2.
Multivariable analysis of post-neoadjuvant tumor factors in P024 trial22
| Post-therapy factors | RFS | Breast cancer-specific survival |
||
|---|---|---|---|---|
| HR (95% CI) | P | HR (95% CI) | P | |
| Tumor stage (T1 or 2 vs T3 or 4) | 2.8 (1.4–5.4) | 0.003 | 4.4 (1.7–11.2) | 0.002 |
| Node status (+ versus −) | 3.2 (1.5–6.9) | 0.004 | 3.9 (1.1–13.7) | 0.04 |
| Ki-67 levels per 2.7-fold increase | 1.3 (1.1–1.6) | 0.003 | 1.4 (1.07–1.9) | 0.01 |
| ER, Allred score (0–2 versus 3–8) | 2.8 (1.2–6.4) | 0.02 | 7.0 (2.4–20.9) | <0.001 |
Abbreviations: ER, estrogen receptor; HR, hazard ratio; RFS, recurrence-free survival. Permission obtained from National Cancer Institute © Ellis, M. J. et al. J. Natl Cancer Inst. 100, 1380–1388 (2008).22
Table 3.
The components of PEPI
| Pathology and biomarker status |
Relapse-free survival |
Breast cancer- specific survival |
||
|---|---|---|---|---|
| HR | Points | HR | Points | |
| Tumor size | ||||
| T1 or T2 | N/A | 0 | N/A | 0 |
| T3 or T4 | 2.8 | 3 | 4.4 | 3 |
| Node status | ||||
| Negative | N/A | 0 | N/A | 0 |
| Positive | 3.2 | 3 | 3.9 | 3 |
| Ki-67 level | ||||
| 0–2.7% | N/A | 0 | N/A | 0 |
| >2.7–7.3% | 1.3 | 1 | 1.4 | 1 |
| >7.3–19.7% | 1.7 | 1 | 2.0 | 2 |
| 19.7–53.1% | 2.2 | 2 | 2.7 | 3 |
| >53.1% | 2.9 | 3 | 3.8 | 3 |
| ER, Allred score | ||||
| 0–2 | 2.8 | 3 | 7.0 | 3 |
| 3–8 | N/A | 0 | N/A | 0 |
Abbreviations: ER, estrogen receptor; HR, hazard ratio; NA, not applicable; PEPI, preoperative endocrine prognostic index. Permission obtained from National Cancer Institute © Ellis, M. J. et al. J. Natl Cancer Inst. 100, 1380–1388 (2008).22
The ATAC and IMPACT trials
Anastrozole was compared with tamoxifen in a large, randomized, phase III, adjuvant trial (ATAC) that randomly assigned 9,366 postmenopausal women with hormone receptor-positive breast cancer to receive anastrozole or tamoxifen, alone or in combination.24 After 10 years of follow-up, patients assigned to the anastrozole group had a statistically significant increase in DFS (HR = 0.86, P = 0.003) and a longer time to recurrence (HR = 0.79, P = 0.0002) compared with the tamoxifen group.25 The combination arm was dropped early because the efficacy of this regimen was not likely to exceed the efficacy of tamoxifen alone. In parallel to the ATAC trial, the IMPACT (Immediate Preoperative Anastrozole, Tamoxifen, or Combined with Tamoxifen) trial26 treated 330 patients with locally advanced-stage disease for a comparison of the two agents—used either alone or in combination—in the neoadjuvant setting.26 Overall, there was no significant difference in the clinical response rates between the two arms. However, the superiority of anastrozole over tamoxifen was demonstrated after detecting a greater reduction in Ki-67 levels after 2 weeks and 12 weeks of therapy (P = 0.013 and 0.0006, respectively) in the 259 patients for whom Ki-67 data were available.14 There were no significant differences in Ki-67 suppression between tamoxifen and the combination arm at either time point, which mirrored the DFS result in the ATAC trial. Thus, although the IMPACT trial, unlike P024, did not show differences in clinical response rates, both studies showed consistent reductions in Ki-67 levels. Importantly, IMPACT predicted the futility of the anastrozole and tamoxifen combination and the investigators contended that, had the Ki-67 results been known in advance, the ATAC investigators would not have included the combination arm in their protocol.14
A strong contribution of the IMPACT trial was the collection of tumor specimens 2 weeks after the initiation of therapy. This led to the observation that, at this very early time point, Ki-67 expression was significantly associated with RFS (HR = 1.95; 95% CI = 1.23–3.07; P = 0.004) after adjusting for ER levels and tumor size. The 5-year RFS rates were 85%, 75%, and 60% for the lowest, middle, and highest tertiles of 2-week Ki-67 expression, respectively.15 The hypothesis that Ki-67 levels—established as soon as 2 weeks after the initiation of therapy—act as a better prognostic factor than the baseline levels is being tested in the 4,000 patient POETIC (Peri Operative Endocrine Therapy for Individualizing Care) trial in the UK.27 A caveat regarding the POETIC approach is that measuring Ki-67 after 2 weeks of treatment will not identify tumors with a propensity to show delayed or acquired resistance. This fact argues for a longer period of observation in the preoperative setting for a completely accurate readout of biological efficacy of the endocrine treatment under investigation. The prediction, based on Ki-67 levels, of late relapse due to acquired resistance is hypothetically more likely to be more accurate with sample analysis at 4 months or even 6 months after the initiation of endocrine treatment. Proving this point will require a large number of patients, early time points and biopsy Ki-67 values, as well as long-term follow up. This all will be addressed in the near future in the ALTERNATE trial.
The MA.27 and ACOSOG Z1031 trials
The MA.27 trial28 is a phase III study that, between June 2003 and July 2008, randomly assigned 7,576 postmenopausal women to receive two aromatase inhibitors—exemestane (steroidal) or anastrozole (non-steroidal) in the adjuvant setting. The primary end point was event-free survival and the secondary objectives included overall survival, distant recurrence, incidence of contralateral breast cancer and safety. Although the final results are currently unpublished, in a recent meeting Paul E. Goss, principal investigator of the study, reported no significant differences between the two arms for any of the trial end points and patients are no longer being followed.28 MA.27 was designed to prove the superiority of exemestane, and the question remains: could a neoadjuvant endocrine therapy trial have refuted this hypothesis and prevented the activation of such a large trial that was ultimately destined to be negative?
The phase II ACOSOG Z1031 trial29 randomly assigned 374 postmenopausal women between January 2006 and January 2009 with clinical stage II or III ER+ breast cancer to receive anastrozole, exemestane or letrozole for 16–18 weeks before surgery. The primary end point was clinical response rate. Clinical response rates were not statistically different between the arms: 69.1% (95% CI = 60.1–77.1%) for patients treated with anastrozole, 62.9% (95% CI = 53.8–71.4%) for patients treated with exemestane and 74.8% (95% CI = 66.3–82.15%) for treatment with letrozole; however, the randomized phase II selection design indicated that the non-steroidal aromatase inhibitors letrozole and anastrozole should be taken forward for further testing. Importantly, there were no significant differences in Ki-67 levels after treatment between the treatment arms based on the 266 cases with Ki-67 data available (P = 0.45). Geometric mean percentage change in Ki-67 was 78% with anastrozole, 81.2% with exemestane and 87.1% with letrozole.29 According to the Ki-67 analysis, the three drugs have biologically equivalent effects; thus, it could be argued that the ACOSOG Z1031 predicted that MA.27 was a futile study. Because the results from the FACE trial,30 a comparison between anastrozole and letrozole in high-risk women, have not been reported, we cannot comment yet on the parallel results from ACOSOG Z1031 and FACE. This is of considerable interest from the perspective of estradiol suppression as letrozole is a more-effective aromatase inhibitor.31 However, because no difference in Ki-67 suppression between the two drugs was observed in the ACOSOG Z1031 trial, it is possible that the pharmacodynamic differences in estradiol and estrone sulfate suppression observed by Dixon et al.31 do not translate into efficacy differences at the level of Ki-67.
The ACOSOG Z1031 trial analysis29 made an additional contribution with respect to the interaction between baseline (pre-treatment) tumor predictors of long-term outcome and the PEPI model, which is based on tumor characteristics after neoadjuvant treatment. In a univariate analysis, levels of Ki-67 ≤10% (P = 0.018) at baseline and luminal A subtype status (P = 0.004) were both significantly associated with an increased likelihood of a PEPI score of 0. Thus, Ki-67 or a gene-expression profile can be used to identify patients at baseline who are certainly suitable for neoadjuvant endocrine therapy because a significant proportion of the patients do not require chemotherapy. Nevertheless, the molecular testing approach, if available, would capture a greater population of patients with low-risk breast cancer.29 Regarding the optimal time point for measuring Ki-67 to predict adjuvant effects, it is noteworthy that 12% of luminal A breast cancers showed >5% increase in levels of Ki-67 from baseline. This result, again, argues for longer periods (months rather than weeks) of neoadjuvant treatment so that resistant subpopulations of tumors initially categorized as low risk can be correctly identified.
The STAGE study and the ABCSG 12 trial
The value of the on-treatment Ki-67 level or the PEPI score as prognostic tools are not established in premenopausal women with ER+ breast cancer. Indeed there is an emerging inconsistency. The ABCSG 12 trial32 established that, in the presence of the luteinizing hormone–releasing hormone analog (LHRH) agonist goserelin, anastrozole was not superior to tamoxifen.32 However, the Japanese STAGE study showed clear superiority—for both clinical outcomes and Ki-67 suppression—of anastrozole versus tamoxifen when given with goserelin in the neoadjuvant setting.33,34 The basis for this discrepancy is unclear but one hypothesis, suggested by a careful examination of the STAGE data, is that gradual tachyphylaxis occurs with time with the estrogen suppressing effects of combined goserelin and anastrozole treatment. As a result, a significant number of patients are experiencing insufficient adjuvant endocrine therapy on the aromatase inhibitor arm of goserelin-based clinical trials. For example, in the supplementary data provided by Masuda et al.,33 the confidence intervals for the estradiol levels at 16 weeks of neoadjuvant therapy widely overlap between the goserelin–tamoxifen group and the goserelin–anastrozole group, implying failure of anastrozole to suppress estradiol over that achieved by goserelin and tamoxifen. By contrast, in the data provided at the presentation of the study at ASCO in 2011,34 a greater estradiol suppression for the anastrozole versus tamoxifen arm was observed at 4 weeks. If true in large populations, the failure of anastrozole and goserelin to fully suppress estradiol levels in all patients in the longer term could explain the discrepancy between the STAGE data and the ABCSG 12 data and has immense implications for the use of LHRH agonist–aromatase inhibitor combined therapy for premenopausal women. Long term estradiol monitoring maybe necessary to ensure that individual patients receiving aromatase inhibitor–LHRH agonist therapy are experiencing adequate estradiol suppression.
Studies with rapamycin analogs
A new suite of neoadjuvant endocrine therapy trials assessing an endocrine agent in combination with a signal transduction inhibitor is underway. A trial that examined the mTOR inhibitor everolimus in combination with letrozole demonstrated superior anti-proliferative effects over letrozole alone and, therefore, suggested that this combination should be considered for an adjuvant therapy trial.35 Although an adjuvant program has not been activated yet, the recent results in the metastatic setting were also positive for combining an aromatase inhibitor with everolimus.36 These studies point towards a new phase in neoadjuvant investigation that will also explore combinations of other kinds of signal transduction inhibitor—such as PI3K inhibitors—with an endocrine approach, following up on the synthetic-lethal hypothesis that has been developed preclinically for this pathway combination.37,38
Future trials
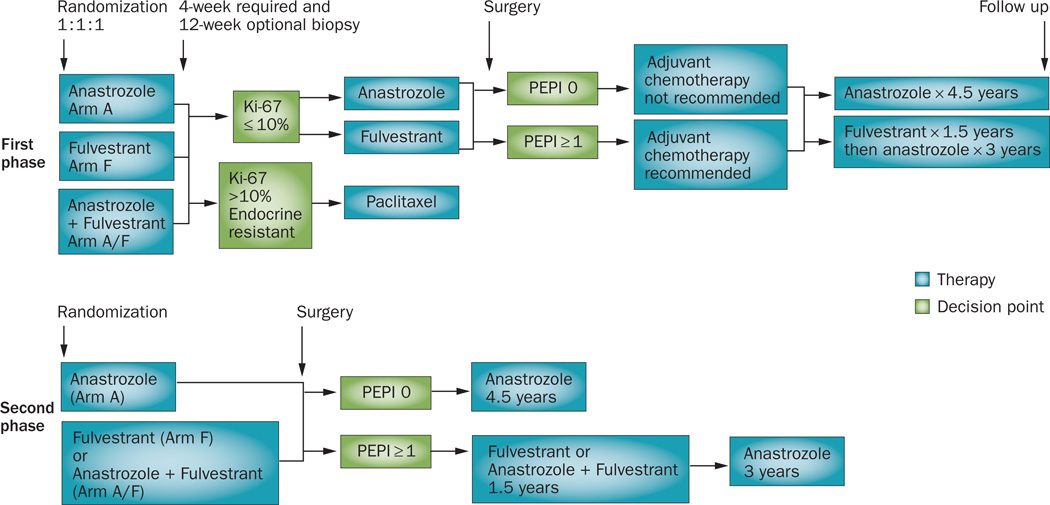
To prospectively validate the utility of neoadjuvant endocrine trials for the prediction of long-term outcomes, a randomized phase III study named ALTERNATE (ALTernate approaches for clinical stage II and III Estrogen Receptor positive breast cancer NeoAdjuvant TrEatment) is being conducted by the ACTION (Alliance for Clinical Trials In ONcology) cooperative group (Figure 1). The overarching goal of this trial is to develop a biomarker strategy based on Ki-67 levels in the neoadjuvant setting to predict long-term outcome of patients with ER+ breast cancer. In the three-arm neoadjuvant comparison phase (first phase of the study), patients will be randomly assigned to receive either the ER antagonist fulvestrant, or anastrozole, or the combination of fulvestrant and anastrozole. The primary objective for the first phase of the trial is to compare the PEPI-0 rate between anastrozole and the two fulvestrant arms to determine if one of the fulvestrant arms should be considered for the second phase of the study for PEPI-0 validation and for an adjuvant endocrine therapy trial in the future. In the PEPI-0 validation phase (second phase of the study), the long-term outcome of patients who achieved a PEPI score of 0 will be assessed. The primary objective for the second phase of the trial is to validate a PEPI score of 0 as a surrogate marker—after treatments with neoadjuvant anastrozole or one of the superior fulvestrant arms—for low-risk breast cancer so that tumors with this characteristic can be treated without chemotherapy, based on an excellent prognosis. In both phases of the trial, a mandatory and an optional biopsy are performed at 4 weeks and 12 weeks, respectively, for the evaluation of tumor Ki-67. On the basis of an analysis of the IMPACT data,15 endocrine resistant tumors identified by Ki-67 levels >10% on these tumor biopsies will be switched to treatment with neoadjuvant paclitaxel administered weekly with the primary objective to determine the rate of pathologic complete response after 12 weeks of neoadjuvant paclitaxel in patients with endocrine-resistant disease, so that future trials can be powered against these control data. Other objectives of ALTERNATE trial include a well-powered comparison between Ki-67 values at baseline, 4 weeks and 24 weeks for the prediction of long-term outcomes. The design of the ALTERNATE trial is intended to definitively establish the neoadjuvant endocrine therapy paradigm.
Figure 1.
Schematic representation for the ALTERNATE Trial. Postmenopausal women with clinical stage II or III ER-positive, HER2-negative breast cancer are eligible for the study. In the first phase (neoadjuvant comparison phase), patients are randomized at 1:1:1 ratio (n = 400 in each arm) to receive neoadjuvant endocrine therapy with either anastrozole (Arm A) or fulvestrant (Arm F), or the combination of anastrozole and fulvestrant (Arm A/F) for 24 weeks. Tumor biopsy for Ki-67 assessment is performed at the end of week 4 (mandatory) and then week 12 (optional, recommended if the clinical response is less than a partial response). If Ki-67 >10%, patients are recommended to switch to 12 weeks of weekly paclitaxel for the determination of the pathologic complete response rate in this population. Patients with Ki-67 <10% will continue their assigned regimen to complete 24 weeks of treatment followed by surgery and PEPI score calculation. Adjuvant chemotherapy is not recommended for patients in the PEPI-0 group. Patients will continue their assigned regimen in the adjuvant setting for another 1.5 years followed by anastrozole for 3 more years. On completion of accrual for the first phase of the trial, enrollment for the two fulvestrant arms will not be done until a decision is made that either none (if neither treatment yield a PEPI-0 rate at least 10% higher than with anastrozole) or one (the superior fulvestrant arm) of these arms will proceed to the second phase of the study for PEPI-0 validation on the fulvestrant regimen. Abbreviations: ER, estrogen receptor; PEPI, preoperative endocrine prognostic index.
Conclusions
For postmenopausal women, there are three examples of large adjuvant endocrine therapy clinical trials whose final outcome were predicted by Ki-67 analyses conducted within the context of small neoadjuvant studies involving less than 400 patients. 13,22,26,29 The ALTERNATE trial is the logical next step and, if this trial fails to show that high-dose fulvestrant either alone or in combination with anastrozole is more effective at suppressing levels of Ki-67 than anastrozole, it is very unlikely that a fulvestrant adjuvant study will be approved. In the current era of genome sequencing, neoadjuvant endocrine therapy trials will also prove to be a very effective and resource-conserving approach to the design of studies with mutation-driven therapeutic hypotheses as early information on the activity of drugs within predefined subsets can be efficiently obtained.
Key points.
-
▪
In postmenopausal women, on-treatment Ki-67 levels are more predictive of long-term outcome than baseline levels; studies validating the clinical value of this assessment as a prognostic tool are underway
-
▪
Ki-67 values in three small neoadjuvant trials predicted outcomes of large adjuvant trials; future adjuvant designs should be based on a biological superiority hypothesis generated by a neoadjuvant study
-
▪
The use of on-treatment Ki-67 and the preoperative endocrine prognostic index (PEPI) in premenopausal women with estrogen receptor-positive breast cancer requires further investigation
-
▪
High Ki-67 values can identify endocrine therapy-resistant tumors as early as 2 weeks after neoadjuvant endocrine therapy; ongoing trials are investigating the utility of this observation
Acknowledgments
This work was supported by R01 CA095614 awarded to M. J. Ellis, a 2011 AVON Foundation research grant to support R. Goncalves and CALGB Clinical Scholar Award to C. Ma. The ACOSOG Z1031 trial was supported by grants by the National Cancer Institute to the American College of Physicians Oncology Group (U24 CA114736 and U10 076,001).
Footnotes
Competing interests
M. J. Ellis declares an association with the following companies: Astra Zeneca, Bioclassifier LLC, Novartis, Pfizer. The other authors declare no competing interests.
Author contributions
J. Luo researched the data for the article and reviewed the manuscript before submission. All the other authors researched the data for the manuscript, made a substantial contribution to discussion of the content, wrote, and edited and revised the manuscript before submission.
References
- 1.Anderson WF, Chen BE, Jatoi I, Rosenberg PS. Effects of estrogen receptor expression and histopathology on annual hazard rates of death from breast cancer. Breast Cancer Res. Treat. 2006;100:121–126. doi: 10.1007/s10549-006-9231-y. [DOI] [PubMed] [Google Scholar]
- 2.Howell A, et al. Results of the ATAC (Arimidex, Tamoxifen, Alone or in Combination) trial after completion of 5 years’ adjuvant treatment for breast cancer. Lancet. 2005;365:60–62. doi: 10.1016/S0140-6736(04)17666-6. [DOI] [PubMed] [Google Scholar]
- 3.Mouridsen H, et al. Letrozole therapy alone or in sequence with tamoxifen in women with breast cancer. N. Engl. J. Med. 2009;361:766–776. doi: 10.1056/NEJMoa0810818. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Coombes RC, et al. A randomized trial of exemestane after two to three years of tamoxifen therapy in postmenopausal women with primary breast cancer. N. Engl. J. Med. 2004;350:1081–1092. doi: 10.1056/NEJMoa040331. [DOI] [PubMed] [Google Scholar]
- 5.Dowsett M, et al. Biomarker changes during neoadjuvant anastrozole, tamoxifen, or the combination: influence of hormonal status and HER-2 in breast cancer—a study from the IMPACT trialists. J. Clin. Oncol. 2005;23:2477–2492. doi: 10.1200/JCO.2005.07.559. [DOI] [PubMed] [Google Scholar]
- 6.Gerdes J, Schwab U, Lemke H, Stein H. Production of a mouse monoclonal antibody reactive with a human nuclear antigen associated with cell proliferation. Int. J. Cancer. 1983;31:13–20. doi: 10.1002/ijc.2910310104. [DOI] [PubMed] [Google Scholar]
- 7.Harris L, et al. American Society of Clinical Oncology 2007 update of recommendations for the use of tumor markers in breast cancer. J. Clin. Oncol. 2007;25:5287–5312. doi: 10.1200/JCO.2007.14.2364. [DOI] [PubMed] [Google Scholar]
- 8.Goldhirsch A, et al. Strategies for subtypes —dealing with the diversity of breast cancer: highlights of the St. Gallen International Expert Consensus on the Primary Therapy of Early Breast Cancer 2011. Ann. Oncol. 2011;22:1736–1747. doi: 10.1093/annonc/mdr304. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Cheang MC, et al. Ki67 index, HER2 status, and prognosis of patients with luminal B breast cancer. J. Natl Cancer Inst. 2009;101:736–750. doi: 10.1093/jnci/djp082. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Dowsett M, et al. Assessment of Ki67 in breast cancer: recommendations from the International Ki67 in Breast Cancer Working Group. J. Natl Cancer Inst. 2011;103:1656–1664. doi: 10.1093/jnci/djr393. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Colozza M, Sidoni A, Piccart-Gebhart M. Value of Ki67 in breast cancer: the debate is still open. Lancet Oncol. 2010;11:414–415. doi: 10.1016/S1470-2045(10)70089-9. [DOI] [PubMed] [Google Scholar]
- 12.Luporsi E, et al. Ki-67: level of evidence and methodological considerations for its role in the clinical management of breast cancer: analytical and critical review. Breast Cancer Res. Treat. doi: 10.1007/s10549-011-1837-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Ellis MJ, et al. Letrozole inhibits tumor proliferation more effectively than tamoxifen independent of HER1/2 expression status. Cancer Res. 2003;63:6523–6531. [PubMed] [Google Scholar]
- 14.Dowsett M, et al. Short-term changes in Ki-67 during neoadjuvant treatment of primary breast cancer with anastrozole or tamoxifen alone or combined correlate with recurrence-free survival. Clin. Cancer Res. 2005;11:951s–958s. [PubMed] [Google Scholar]
- 15.Dowsett M, et al. Prognostic value of Ki67 expression after short-term presurgical endocrine therapy for primary breast cancer. J. Natl Cancer Inst. 2007;99:167–170. doi: 10.1093/jnci/djk020. [DOI] [PubMed] [Google Scholar]
- 16.Thürlimann B, et al. A comparison of letrozole and tamoxifen in postmenopausal women with early breast cancer. N. Engl. J. Med. 2005;353:2747–2757. doi: 10.1056/NEJMoa052258. [DOI] [PubMed] [Google Scholar]
- 17.Regan MM, et al. Assessment of letrozole and tamoxifen alone and in sequence for postmenopausal women with steroid hormone receptor-positive breast cancer: the BIG 1-98 randomised clinical trial at 8.1 years median follow-up. Lancet Oncol. 2011;12:1101–1108. doi: 10.1016/S1470-2045(11)70270-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Eiermann W, et al. Preoperative treatment of postmenopausal breast cancer patients with letrozole: A randomized double-blind multicenter study. Ann. Oncol. 2001;12:1527–1532. doi: 10.1023/a:1013128213451. [DOI] [PubMed] [Google Scholar]
- 19.Ellis MJ, et al. Letrozole is more effective neoadjuvant endocrine therapy than tamoxifen for ErbB-1- and/or ErbB-2-positive, estrogen receptor-positive primary breast cancer: evidence from a phase III randomized trial. J. Clin. Oncol. 2001;19:3808–3816. doi: 10.1200/JCO.2001.19.18.3808. [DOI] [PubMed] [Google Scholar]
- 20.Chin SF, et al. Using array-comparative genomic hybridization to define molecular portraits of primary breast cancers. Oncogene. 2007;26:1959–1970. doi: 10.1038/sj.onc.1209985. [DOI] [PubMed] [Google Scholar]
- 21.Horobin JM, Preece PE, Dewar JA, Wood RA, Cuschieri A. Long-term follow-up of elderly patients with locoregional breast cancer treated with tamoxifen only. Br. J. Surg. 1991;78:213–217. doi: 10.1002/bjs.1800780228. [DOI] [PubMed] [Google Scholar]
- 22.Ellis MJ, et al. Outcome prediction for estrogen receptor-positive breast cancer based on postneoadjuvant endocrine therapy tumor characteristics. J. Natl Cancer Inst. 2008;100:1380–1388. doi: 10.1093/jnci/djn309. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Dowsett M, et al. Assessment of Ki67 in breast cancer: Recommendations from the International Ki67 in Breast Cancer Working Group. J. Natl Cancer Inst. 2011;103:1656–1664. doi: 10.1093/jnci/djr393. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Baum M, et al. Anastrozole alone or in combination with tamoxifen versus tamoxifen alone for adjuvant treatment of postmenopausal women with early breast cancer: first results of the ATAC randomised trial. Lancet. 2002;359:2131–2139. doi: 10.1016/s0140-6736(02)09088-8. [DOI] [PubMed] [Google Scholar]
- 25.Cuzick J, et al. Effect of anastrozole and tamoxifen as adjuvant treatment for early-stage breast cancer-10-year analysis of the ATAC trial. Lancet Oncol. 2010;11:1135–1141. doi: 10.1016/S1470-2045(10)70257-6. [DOI] [PubMed] [Google Scholar]
- 26.Smith IE, et al. Neoadjuvant treatment of postmenopausal breast cancer with anastrozole, tamoxifen, or both in combination: the Immediate Preoperative Anastrozole, Tamoxifen, or Combined with Tamoxifen (IMPACT) multicenter double-blind randomized trial. J. Clin. Oncol. 2005;23:5108–5116. doi: 10.1200/JCO.2005.04.005. [DOI] [PubMed] [Google Scholar]
- 27.Dowsett M, et al. Endocrine therapy, new biologicals, and new study designs for presurgical studies in breast cancer. J. Natl Cancer Inst. Monogr. 2011;2011:120–123. doi: 10.1093/jncimonographs/lgr034. [DOI] [PubMed] [Google Scholar]
- 28.Goss PE, et al. 33rd Annual San Antonio Breast Cancer Symposium. San Antonio, Texas: 2010. Final analysis of NCIC CTG MA.27: a randomized phase III trial of exemestane versus anastrozole in postmenopausal women with hormone receptor positive primary breast cancer [abstract] p. S1-1. [Google Scholar]
- 29.Ellis MJ, et al. Randomized phase II neoadjuvant comparison between letrozole, anastrozole, and exemestane for postmenopausal women with estrogen receptorrich stage 2 to 3 breast cancer: clinical and biomarker outcomes and predictive value of the baseline PAM50-based intrinsic subtype— ACOSOG Z1031. J. Clin. Oncol. 2011;29:2342–2349. doi: 10.1200/JCO.2010.31.6950. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.US National Library of Medicine. ClinicalTrials.gov [online] doi: 10.1080/15360280801989377. http://clinicaltrials.gov/ct2/show/NCT00248170. [DOI] [PubMed]
- 31.Dixon JM, et al. Letrozole suppresses plasma estradiol and estrone sulphate more completely than anastrozole in postmenopausal women with breast cancer. J. Clin. Oncol. 2008;26:1671–1676. doi: 10.1200/JCO.2007.13.9279. [DOI] [PubMed] [Google Scholar]
- 32.Gnant M, et al. Adjuvant endocrine therapy plus zoledronic acid in premenopausal women with early-stage breast cancer: 62-month follow-up from the ABCSG-12 randomised trial. Lancet Oncol. 2011;12:631–641. doi: 10.1016/S1470-2045(11)70122-X. [DOI] [PubMed] [Google Scholar]
- 33.Masuda N, et al. Neoadjuvant anastrozole versus tamoxifen in patients receiving goserelin for premenopausal breast cancer (STAGE): a double-blind, randomised phase 3 trial. Lancet Oncol. doi: 10.1016/S1470-2045(11)70373-4. [DOI] [PubMed] [Google Scholar]
- 34.Kinoshita T, et al. Neoadjuvant anastrozole or tamoxifen for premenopausal breast cancer: Ki67 expression data from the STAGE study. J. Clin. Oncol. 2011;29(Suppl. 15):501. [Google Scholar]
- 35.Baselga J, et al. Phase II randomized study of neoadjuvant everolimus plus letrozole compared with placebo plus letrozole in patients with estrogen receptor-positive breast cancer. J. Clin. Oncol. 2009;27:2630–2637. doi: 10.1200/JCO.2008.18.8391. [DOI] [PubMed] [Google Scholar]
- 36.Baselga J, et al. Everolimus in postmenopausal hormone-receptor-positive advanced breast cancer. N. Engl. J. Med. 2011 doi: 10.1056/NEJMoa1109653. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Crowder RJ, et al. PIK3CA and PIK3CB inhibition produce synthetic lethality when combined with estrogen deprivation in estrogen receptor-positive breast cancer. Cancer Res. 2009;69:3955–3962. doi: 10.1158/0008-5472.CAN-08-4450. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Sanchez CG, et al. Preclinical modeling of combined phosphatidylinositol-3-kinase inhibition with endocrine therapy for estrogen receptor-positive breast cancer. Breast Cancer Res. 2011;13:R21. doi: 10.1186/bcr2833. [DOI] [PMC free article] [PubMed] [Google Scholar]